Abstract
Background
Delivery of hepatitis C virus (HCV) care to people in prison is essential to HCV elimination. We aimed to describe current HCV care practices across Canada’s adult provincial prisons.
Methods
One representative per provincial prison health care team (except Ontario) was invited to participate in a web-based survey from January to June 2020. The outcomes of interest were HCV screening and treatment, treatment restrictions, and harm reduction services. The government ministry responsible for health care was determined. Non-nominal data were aggregated by province and ministry; descriptive statistical analyses were used to report outcomes.
Results
The survey was completed by 59/65 (91%) prisons. On-demand, risk-based, opt-in, and opt-out screening are offered by 19 (32%), 10 (17%), 18 (31%), and 9 (15%) prisons, respectively; 3 prisons offer no HCV screening. Liver fibrosis assessments are rare (8 prisons access transient elastography, and 15 use aspartate aminotransferase to platelet ratio or Fibrosis-4); 20 (34%) prisons lack linkage to care programs. Only 32 (54%) prisons have ever initiated HCV treatment on site. Incarceration length and a fibrosis staging of ≥F2 are the most common eligibility restrictions for treatment. Opioid agonist therapy is available in 83% of prisons; needle and syringe programs are not available anywhere. Systematic screening and greater access to treatment and harm reduction services are more common where the Ministry of Health is responsible.
Conclusions
Tremendous variability exists in HCV screening and care practices across Canada’s provincial prisons. To advance HCV care, adopting opt-out screening and removing eligibility restrictions may be important initial strategies.
Keywords: elimination, hepatitis C virus (HCV), linkage to care, prison, screening, treatment
Introduction
The prevalence of chronic hepatitis C virus (HCV) infection in correctional settings is disproportionately higher than in the general population, in part because of the overrepresentation of people who inject drugs (PWID) among those experiencing incarceration (1,2). Modelling studies have shown that people in prison play a major role in driving HCV epidemics, particularly once released, and should thus be prioritized if HCV elimination is to be achieved by 2030 (3–6). However, countries’ responses to the needs of this population vary significantly. As of April 2019, fewer than 25% of countries with viral hepatitis plans had outlined specific interventions for people experiencing incarceration (7). In Canada, one in nine Canadians infected with HCV spends time in a correctional facility each year, and most recent estimates by the Public Health Agency of Canada (PHAC) have indicated that 25% of incarcerated Canadians have been exposed to HCV, suggesting that Canadian correctional settings represent unique public health opportunities to engage high-risk individuals in care (8,9). Consequently, the Canadian Network on Hepatitis C appropriately identified ‘people with experience in the prison system’ as one of six priority populations for the elimination of HCV in Canada (10).
Despite the prioritization of incarcerated persons as a key population for the elimination of HCV in Canada, very little research has focused on understanding current HCV care practices at the correctional level to determine feasibility. The Canadian correctional system is divided into 43 federal and 99 provincial and territorial prisons, and major disparities in the provision of HCV care exist depending on the type of prison (11–26). The median incarceration time in provincial and territorial prisons is 28 days, meaning that progression along the HCV cascade of care cannot be completed during incarceration for many of those sentenced in these prisons (27). This has important implications for the overall care provided at the institutional level and suggests that HCV micro-elimination efforts may be particularly challenging in these facilities (28). This is in contrast to federal correctional facilities, where individuals serve sentences of 2 years or more. As a result, all individuals incarcerated in federal facilities can complete their HCV care trajectories while incarcerated, including confirmation of cure, or sustained virologic response (SVR). Long sentences in federal prisons have thus facilitated the standardization of HCV care by Correctional Service Canada. In fact, all those incarcerated in federal facilities are systematically offered opt-out HCV screening on admission, a course of direct-acting antivirals (DAAs) if diagnosed with chronic HCV infection, and they are re-treated if they fail or are reinfected (29).
Although federal corrections may be on track for HCV elimination, provincial and territorial corrections lag behind. However, little is known regarding the HCV care provided at the provincial and territorial correctional level. We thus aimed to understand current HCV screening and care practices across all Canadian provincial prisons and, secondarily, to outline important barriers to HCV elimination.
Methods
Design
We conducted a cross-sectional study of Canadian provincial prisons from January to June 2020. For the purpose of this study, we included adult provincial prisons with internet access. We excluded youth and territorial prisons because they represent a minority of the overall incarcerated population in Canada (30) and federal prisons because of the standardization of HCV care across all facilities (26). We surveyed all provinces (British Columbia, Alberta, Saskatchewan, Manitoba, Quebec, New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland and Labrador) with the exception of Ontario. Ontario was excluded because approval from the Ministry of the Solicitor General (responsible for research in Ontario’s provincial correctional facilities) was required and could not be obtained as a result of the cessation of research activity secondary to the severe acute respiratory syndrome coronavirus 2 pandemic.
One key informant per prison health care team, identified by our research team, was invited via email to participate in a survey. The participant selected to complete the survey was the health care professional overseeing or having the greatest knowledge vis-à-vis HCV care services at each provincial institution. When answers were unknown, participants could seek the assistance of other prison personnel. To maximize the response rate, bimonthly emails were sent to participants who had not yet completed the survey. English and French versions of the survey were created. Consent to study participation was implicit on the basis of survey completion, and participants were not compensated for their time. The study was approved by the McGill University Health Centre Research Ethics Board (REB no. 2020-6196).
Survey
The web-based survey consisted of 41 response-guided questions involving yes-or-no, multiple-choice, and short-answer responses. All data were collected through LimeSurvey (31). Although participants were required to provide the name of the correctional facility and their occupation, no personal identifying information was collected. The survey instrument was pilot tested with a small group of respondents (n = 4), and feedback was incorporated before the survey was disseminated.
The outcomes of interest were HCV screening and care practices. Participants were asked to report on the current HCV care practices in their correctional facilities, including HCV screening, linkage to care, treatment, and harm reduction strategies. HCV screening was classified into four categories: (1) on-demand testing, whereby individuals must request screening; (2) risk-based testing, whereby individuals at risk of HCV infection are screened; (3) opt-in testing, whereby individuals are systematically offered screening, but individuals must accept before undergoing screening; and (4) opt-out testing, whereby individuals are informed that screening is part of standard of care, and screening is performed unless declined (32,33). Information regarding the ministry responsible for health care delivery and HCV care services in respective correctional facilities was also obtained.
Perceived barriers to the provision of HCV care in correctional settings were also explored as secondary outcomes with multiple-choice answers derived from published studies. Barriers to HCV screening in correctional facilities include screening strategy, lack of provider–patient knowledge, limited staff and resources, and HCV-related stigma (34–36). Barriers to overall HCV care in correctional settings include limited staff and resources, lack of provider–patient knowledge, treatment restrictions and costs, perceived high risk of reinfection, and absence of formal linkage to care programs on release (36–38).
Analysis
Overall and stratified (province, ministry) descriptive statistical analyses were used to summarize current HCV care practices as well as potential barriers to care. Cross-tabulation analysis was used to report the number and proportion of correctional facilities for each step along the HCV care cascade (from screening to treatment initiation in prison). The most common barriers to HCV care during screening and overall care were also reported.
Results
Study sites and participants
Of the 90 adult provincial prisons in Canada, the survey was distributed to 65 prisons after excluding Ontario (n = 25) (Supplemental Table 1). The response rate was 91% (59/65). Among the 59 provincial prisons, 37 (63%) were all-male, 6 (10%) were all-female, and 16 (27%) were mixed. The average daily incarcerated population varied between 12 and 1,546 individuals. The delivery of health care services fell under the Ministry of Health (MOH) for 35 (59%) prisons and under the Ministry of Justice and Public Security (MOJPS), or its equivalent in each province, for the remaining 24 (41%) facilities. The majority of participants were nurses or nurse practitioners (43/59; 73%); health care managers (10/59; 17%), physicians (3/59; 5%), and correctional (2/59; 3%) and administrative staff (1/59; 2%) made up the minority of participants.
HCV screening
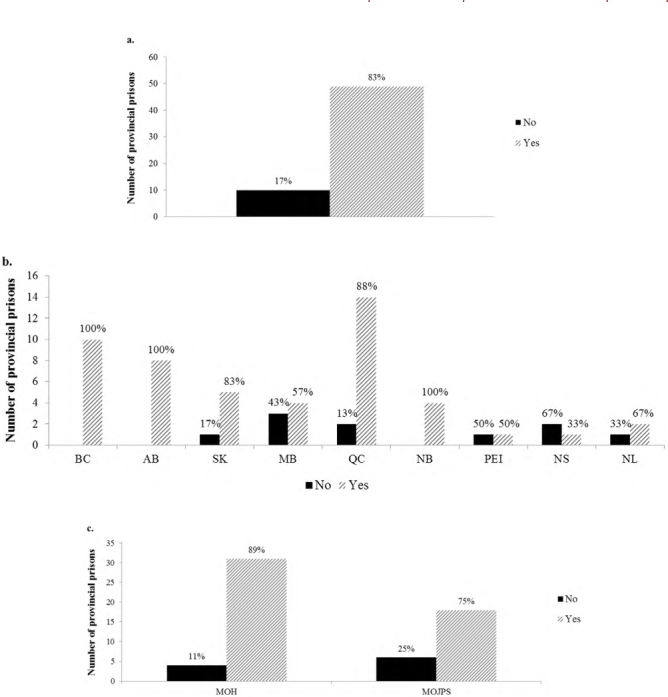
HCV antibody (HCV-Ab) screening is offered in all but three provincial prisons. On-demand, risk-based, opt-in, and opt-out screening are offered by 19 (32%), 10 (17%), 18 (31%), and 9 (15%) prisons, respectively (Figure 1a). Alberta is the only province offering opt-out HCV screening in all provincial prisons (Figure 1b). The majority of remaining provinces offer a variety of screening strategies. When stratified by ministry (Figure 1c), opt-in or opt-out screening is more common in MOH than in MOJPS prisons (51% versus 37%). HCV-Ab testing via venipuncture is the standard of care in all Canadian correctional facilities; the median turn-around-time (TAT) for HCV-Ab test results is 48–72 hours (range <24 h to >5 d; results by prison not shown). Among those who are HCV-Ab-positive, most (64% for MOH prisons, 54% for MOJPS prisons) undergo confirmatory HCV RNA testing within 1 week of test disclosure. The median TAT for HCV RNA test results is 7–14 days (range <7 d to >21 days; results by prison not shown).
Figure 1:
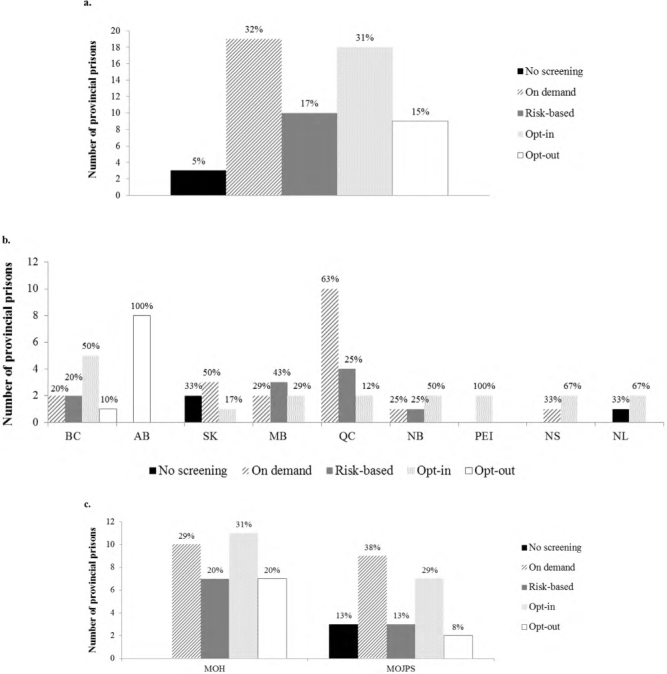
HCV-antibody screening overall (a), by province (b), and by ministry responsible for the delivery of health care services (c)
HCV = Hepatitis C virus; MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Fibrosis staging
Liver fibrosis is rarely assessed in Canadian provincial prisons; 8/59 (14%) prisons perform transient elastography (TE), 15/59 (25%) use aspartate aminotransferase-to-platelet ratio index (APRI) or Fibrosis-4 (FIB-4) scores, and the remaining 36/59 (61%) prisons do not perform any assessments (Figure 2a). Of the 8 prisons that perform TE, only 1 has access to on-site TE. Nova Scotia and Newfoundland and Labrador are the only two Canadian provinces that do not routinely assess for liver fibrosis (Figure 2b). A comparably low number of provincial prisons, under either the MOH or the MOJPS (3 versus 5, respectively), perform TE (Figure 2c).
Figure 2:
Fibrosis staging overall (a), by province (b), and by ministry responsible for the delivery of health care services (c)
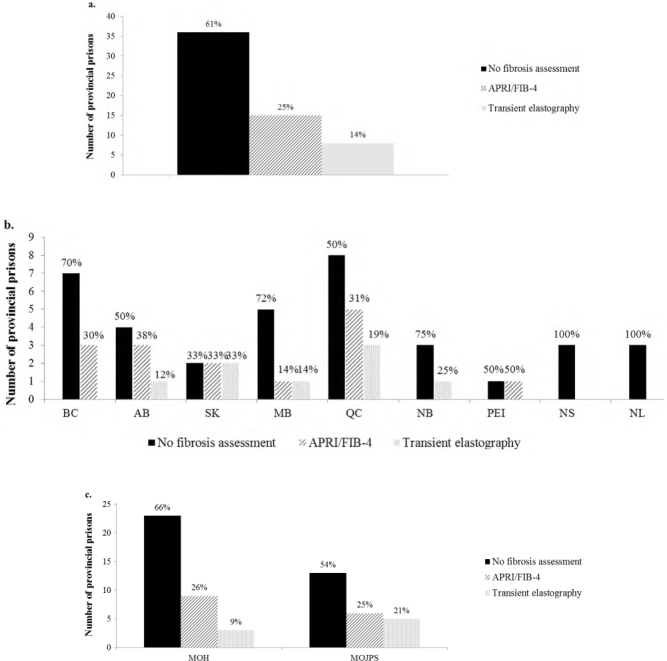
APRI = Aspartate aminotransferase-to-platelet ratio index; FIB-4 = Fibrosis-4 index; MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Linkage to HCV care
Two-thirds (39/59; 66%) of provincial prisons refer those who are newly diagnosed with chronic HCV for further evaluations (results not shown). Conversely, provincial prisons less often (28/59; 48%) refer individuals admitted with known chronic HCV for further evaluation. These assessments are provided by either on-site family physicians (67%) or off-site specialists (33%). Nurse-led HCV care is not the standard of practice. Although on-site physicians are available in two-thirds (39/59; 66%) of facilities, their presence is not necessarily associated with access to HCV care. Only 18/39 (46%) prisons reported the provision of HCV care by their on-site physician; that is, more than half of all MOH or MOJPS prisons have on-site physicians who do not provide HCV care to those who are incarcerated. Physician presence differs slightly between MOH and MOJPS prisons; on-site physicians are present for a median of 2 days/week in MOH prisons versus 1 day/week in MOJPS prisons.
Access to DAAs and treatment eligibility restrictions
Just more than half (32/59; 54%) of prisons have ever initiated a course of DAAs on-site (Figure 3a). DAAs have never been initiated in any provincial prison in New Brunswick or Newfoundland and Labrador (Figure 3b). Conversely, British Columbia and Prince Edward Island are the only two provinces in which DAAs have been initiated in all of their respective provincial prisons. MOH prisons are more likely to provide DAAs during incarceration than are MOJPS prisons (60% versus 46%) (Figure 3c).
Figure 3:
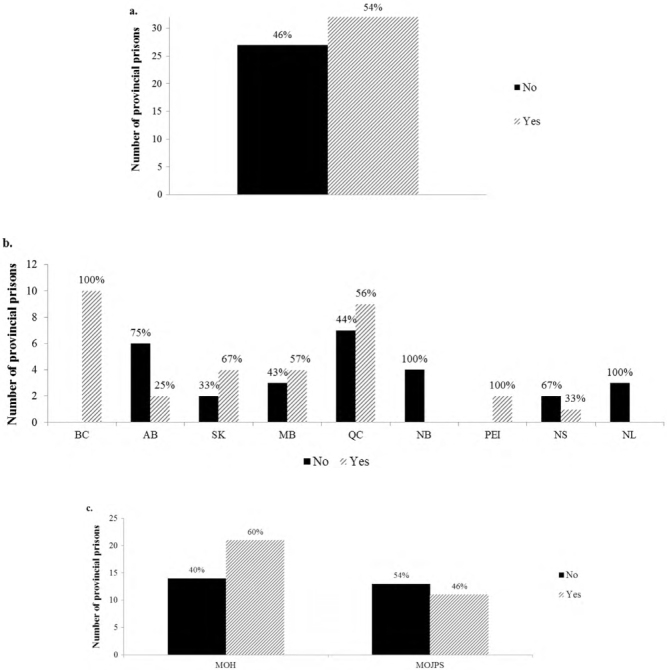
Access to HCV treatment overall (a), by province (b), and by ministry responsible for the delivery of health care services (c)
HCV = Hepatitis C virus; MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Fewer than half (25/59; 42%) of provincial prisons have no eligibility restrictions vis-à-vis HCV treatment initiation during incarceration (Figure 4a). Incarceration length (11/59; 19%) and a fibrosis staging of greater than or equal to F2 (11/59; 19%) are the most common eligibility criteria. DAAs or a qualified prescriber are lacking in 11 (19%) provincial prisons. Four provinces (Alberta, Manitoba, New Brunswick, and Newfoundland and Labrador) have at least one HCV treatment eligibility restriction in each of their correctional facilities (Figure 4b). MOJPS prisons are more likely to have eligibility restrictions on HCV treatment than are MOH facilities (75% versus 46%, respectively) (Figure 4c).
Figure 4:
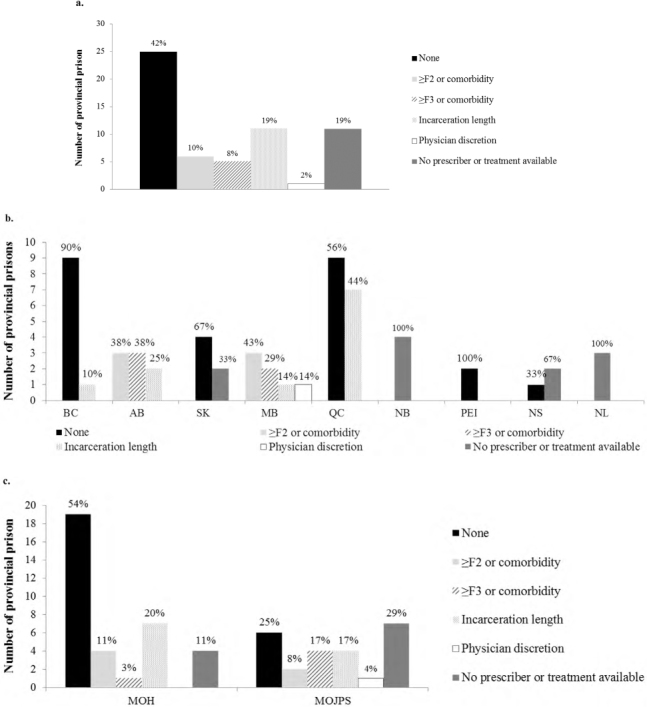
HCV treatment restrictions overall (a), by province (b), and by ministry responsible for the delivery of health care services (c)
HCV = Hepatitis C virus; MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Harm reduction services
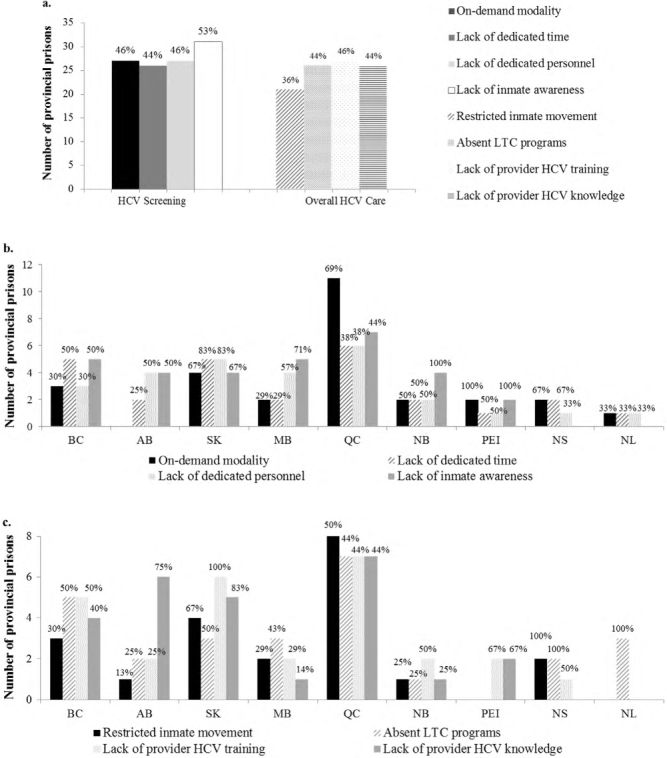
Although opioid agonist therapy (OAT) is available in the majority of prisons (49/59; 83%) (Figure 5a), just more than half (29/49; 59%) of provincial prisons have ever initiated OAT among individuals not admitted on methadone (results not shown). OAT is offered in all provincial prisons in British Colombia, Alberta, and New Brunswick (Figure 5b). OAT is more readily available in MOH than in MOJPS prisons (31/35 [89%] versus 18/24 [75%]) (Figure 5c). Similarly, OAT is more likely to be initiated among individuals not admitted on methadone in MOH versus MOJPS prisons (22/31 [71%] versus 7/18 [39%]; results not shown).
Figure 5:
Availability of opioid agonist therapy overall (a), by province (b), and by ministry responsible for the delivery of health care services (c)
MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Not a single Canadian provincial prison offers prison-based needle and syringe programs (PNSPs). Support services provided to patients with chronic HCV infection are similarly available in MOH and MOJPS prisons. These services include referrals to community organizations (34% in MOH prisons versus 38% in MOJPS prisons, respectively), access to an addiction worker (34% versus 50%, respectively), education on harm reduction measures (49% versus 38%, respectively), and discharge planning (29% versus 26%, respectively).
Barriers to HCV screening and overall HCV care
Commonly perceived system-, provider-, and patient-level barriers to HCV screening include the screening strategy (eg, on-demand) (27/59; 46%), a lack of dedicated time (26/59; 44%) or personnel (27/59; 46%), and low inmate knowledge (31/59; 53%), respectively (Figure 6a). Commonly perceived system- and provider-level barriers to HCV care include restricted inmate movement (21/59; 36%) and deficient linkage to care programs (26/59; 44%) and a lack of training in (27/59; 46%) and knowledge of (26/59; 44%) HCV care, respectively (Figure 6a). Saskatchewan and Quebec, where HCV screening is primarily on-demand, reported that screening modality (ie, on-demand) was an important barrier to screening (Figure 6b). Conversely, no provincial prisons in Alberta, in which opt-out screening is the only screening modality, reported the screening strategy as a barrier to screening. Almost all provinces reported at least three perceived barriers to overall HCV care for people in prison (Figure 6c). MOJPS prisons were more likely than MOH prisons to report that HCV screening strategy (58% versus 37%, respectively), a lack of dedicated personnel (58% versus 37%, respectively), and low inmate awareness (63% versus 46%, respectively) were important barriers to HCV screening (Figure 6d). Similarly, MOJPS prisons were more likely than MOH prisons to report that restricted inmate movement (38% versus 34%, respectively), deficient linkage to care programs (46% versus 43%, respectively), and a lack of provider training in HCV (50% versus 43%, respectively) were important barriers to overall HCV care (Figure 6d).
Figure 6:
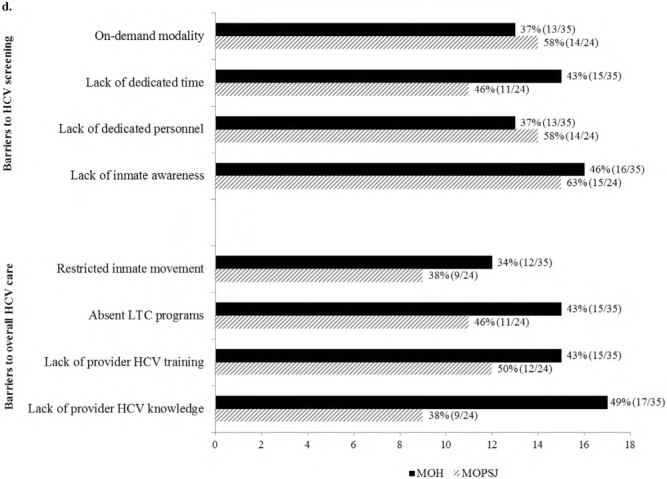
Commonly perceived barriers to HCV screening and overall care (a), to HCV screening by province (b), to overall HCV care by province (c), and to HCV screening and overall care by ministry responsible for the delivery of health care services (d)
HCV = Hepatitis C virus; LTC = Linkage to care; MOH = Ministry of Health; MOJPS = Ministry of Justice and Public Security
Discussion
Our cross-sectional study sought to characterize the spectrum of HCV care provided to individuals incarcerated in provincial prisons across Canada and to better understand key barriers along the HCV cascade of care that may prevent standardization of care. We found tremendous variability in HCV care practices within and across provinces and important system-, provider-, and patient-level barriers that may be important in the provision of HCV care. Our study reinforces the numerous challenges that must be overcome for HCV elimination to be considered feasible in Canada’s provincial prison system and underscores that initial strategies such as the adoption of opt-out screening practices should be considered as a starting point. In addition, given the success of Canada’s federal correctional system in the delivery of HCV care, important lessons could be drawn and applied when possible.
In the past decade, there has been a shift in the delivery of health care services in provincial prisons away from the MOJPS to the MOH. The province of Alberta was the first to fully transition to the MOH in 2010; Nova Scotia and British Columbia have since followed. We observed important differences in the delivery of HCV care based on the ministry overseeing prison health care, as has been reported elsewhere (39,40). First, where the MOH administers services, a higher proportion of provincial prisons offer systematic HCV screening (opt-out or opt-in). Alberta, for example, is the only province that universally offers opt-out HCV screening, and the majority of provincial prisons in Nova Scotia and British Columbia offer either opt-out or opt-in screening. This is contrast to Saskatchewan and Newfoundland and Labrador, where health services are administered by the MOJPS and where HCV screening is absent in several facilities. Second, a higher percentage of provincial prisons under the MOH offer DAAs to incarcerated individuals with chronic HCV; similarly, fewer eligibility restrictions exist for the initiation of treatment. Finally, OAT is more likely to be newly initiated and continued among those admitted on methadone in provincial prisons under the MOH. These findings suggest that access to health care in provincial prisons, including for HCV, is more likely to be prioritized or deemed “the responsibility of the state” (41 p1) if administered by the MOH, with a trend toward systematic screening and increased access to treatment and harm reduction services. Thus, HCV elimination for people in prison may be challenging unless a transfer of responsibility for the provision of health care to the MOH has occurred in all prisons.
Significant disparities exist in the type of HCV screening offered both within and between Canadian provincial prisons. We observed that approximately 40% of provincial prisons offer either no or on-demand screening, the latter of which is associated with screening rates of less than 10% in a Quebec provincial prison (28). Despite national and international recommendations to screen all people who experience incarceration, fewer than half (46%) of provincial prisons offer routine (either opt-out or opt-in) screening—a major barrier to HCV elimination (42–44). Moreover, all provincial prisons offer HCV antibody testing via venipuncture as the standard screening test, and although many correctional settings are moving toward point-of-care testing to facilitate engagement in care (45–48), the current approach seems reasonable pending cost-effectiveness analyses of various screening strategies and larger studies assessing the acceptability of point-of-care testing among people in prison (49). That said, the current approach could be considered both effective and cost-effective if paired with reflex RNA testing, as is the current standard of care in several provinces, including British Columbia as of January 2020 (50). Finally, although health care is provincially mandated and differences between provinces are expected, disparities in screening exist within provinces despite full onus by the MOH. This suggests that decisions regarding screening strategies may be being made at the institutional level depending on available resources or that a hierarchical prioritization of prisons may exist. These findings underscore that for HCV elimination to occur in Canada’s provincial prisons, moving toward systematic screening of all individuals on admission—as is done in Canadian federal prisons—is an imperative first step.
Access to DAAs remains an important barrier to HCV elimination in Canadian provincial prisons. Almost half (46%) of provincial prisons have never offered treatment to those who are incarcerated. Additional studies are thus needed to better understand the multi-level barriers that exist in expanding access to treatment at the provincial prison level. However, our study suggests that important system-level eligibility restrictions may be contributing. For example, fibrosis restrictions still exist in several provincial prisons despite their being lifted in all Canadian provinces by mid-2018 (51). Incarceration length was also reported to be a common restriction to treatment initiation. Although the ‘Blueprint to Inform Hepatitis C Elimination Efforts in Canada’ encourages ‘linkage to care upon release for those with short sentences’ (10 p29), others have advocated for treatment initiation irrespective of incarceration length, given evidence of high SVR rates despite suboptimal adherence (52,53) and the potential impact on community-level HCV prevalence, incidence, and transmission (5). That said, studies in the pre-DAA and DAA eras have suggested that SVR rates are significantly lower among incarcerated individuals who are released before the completion of therapy than among those who complete treatment during incarceration (54,55). Moreover, many provincial prisons do not benefit from the reduced DAA prices that were negotiated by the pan-Canadian Pharmaceutical Alliance, meaning that a course of DAAs could be several-fold more expensive per incarcerated individual if initiated in prison. Given the current realities, it seems reasonable to reserve treatment for those with advanced liver disease and those whose incarceration length allows for the completion of therapy until equivalently competitive pricing schemes or adequate linkage to care programs exist.
Our study demonstrates that linkage to care lacks standardization across Canada’s provincial prisons. Although this is likely due in part to limited resources, little research has also been dedicated to this field, and the most effective, acceptable, and sustainable interventions to maximize linkage to care after release have yet to be determined (56,57). As a result of short sentences, linkage to care is a crucial step along the HCV care cascade for those incarcerated in provincial prison and remains the subject of ongoing research. Although critical, HCV linkage to care is unlikely to be prioritized if systematic screening is not yet in place (58) and until more data accumulate regarding predictors of linkage to HCV care after incarceration.
Although it has previously been reported that access to OAT is variable as a result of unique delivery methods, policies, and monitoring, we observed that OAT is provided to the majority (83%) of those in provincial prison who are admitted on methadone (59). Conversely, we found that those incarcerated are less likely to be initiated on OAT if needed. Although promising, these observations reflect the ongoing difficulties faced by people who use opioid drugs in accessing OAT while incarcerated in some Canadian provinces. PNSPs are currently being pilot tested in 11 federal prisons, and their availability has not yet expanded to provincial corrections, as evidenced by our findings (60). Moreover, we did not inquire about the availability of safer tattooing programs in our survey because they were terminated in Canadian correctional settings in 2007 (61). Although the availability of OAT is reassuring, it is only one component of a comprehensive harm reduction response. Until PNSPs and safer tattooing programs become routinely available, HCV elimination at the provincial prison level is unlikely to occur.
Several system-, provider-, and patient-level barriers could hinder the elimination of HCV in Canadian provincial prisons. A key barrier to the provision and receipt of HCV care for providers and patients, respectively, is a lack of HCV-related knowledge. Low HCV knowledge has been well documented among PWID (62–64). That said, a recent systematic review found that nurse-led education was associated with increased HCV screening among people in prison, underscoring the potential impact of education in changing behaviour (56). Furthermore, our study demonstrated that more than half of all on-site physicians fail to provide HCV care to those who are incarcerated. Although the reasons for this are likely multifactorial, a lack of HCV knowledge and training may contribute, further underscoring the importance of education for providers in addition to patients. Prison-based HCV education programs are the focus of intense study in Australian prisons (65) and, if associated with increased engagement along the HCV cascade of care, could be adapted to different settings, including prisons in low- and middle-income countries. Finally, decentralized nurse-led models of HCV care, which have been shown to be effective and safe in other prisons (66–67), could replace the current physician-centric models of care to accelerate engagement in care.
Our study has limitations. First, it was cross-sectional. Changes in HCV care practices over time were thus not captured; however, because these changes typically occur slowly, our results may be applicable for several years. Second, we restricted participation to one individual per provincial prison. Although participants were individually selected by the research team to represent those with the greatest knowledge vis-à-vis HCV care services at each provincial institution, this step was not internally validated. Consequently, we cannot rule out invalid responses or social desirability bias. We attempted to mitigate the latter by using a self-administered online anonymous survey. Moreover, we encouraged consultation with other prison personnel to improve response accuracy. Third, we did not account for prison size or HCV prevalence, financial budgets for HCV care, or on-site logistical considerations in the interpretation of our results. These factors may have influenced the availability of HCV care services at the provincial prison level. Despite these limitations, this is the first study describing current HCV care practices in Canada’s provincial prisons, to which all future efforts to achieve HCV elimination can be compared. Furthermore, given the large degree of heterogeneity in prison-based HCV policies and practices across and within provinces, this study underscores that correctional health policies need to be evaluated at the individual correctional centre level to provide an accurate assessment. These findings have important implications outside Canada and provide a framework for other jurisdictions and countries to replicate.
In conclusion, significant disparities in HCV care exist across Canada’s provincial prisons. Given the lack of care standardization, HCV elimination is unlikely to occur in the Canadian provincial prison system by 2030. To advance HCV care in provincial prisons, adopting opt-out screening, removing eligibility restrictions, and providing HCV educational programs to providers and people in prison could be considered important initial strategies.
Supplementary Information
Supplemental Table 1:
Participating adult provincial prisons in Canada
| Province | Adult provincial prison | Sex | Average daily inmate count |
|---|---|---|---|
| British Columbia (n = 10) | Alouette Correctional Centre for Women | Female | 158 |
| Ford Mountain Correctional Centre | Male | 98 | |
| Fraser Regional Correctional Centre | Male | 457 | |
| Kamloops Regional Correctional Centre | Male | 257 | |
| Nanaimo Correctional Centre | Male | 134 | |
| North Fraser Pretrial Centre | Male | 506 | |
| Okanagan Correctional Centre | Mixed | 26 | |
| Prince George Regional Correctional Centre | Mixed | 261 | |
| Surrey Pretrial Services Centre | Male | 524 | |
| Vancouver Island Regional Correctional Centre | Male | 311 | |
| Alberta (n = 8) | Calgary Correctional Centre | Mixed | 291 |
| Calgary Remand Centre | Mixed | 614 | |
| Edmonton Remand Centre | Mixed | 1,546 | |
| Fort Saskatchewan Correctional Centre | Mixed | 504 | |
| Lethbridge Correctional Centre | Mixed | 322 | |
| Medicine Hat Remand Centre | Mixed | 98 | |
| Peace River Correctional Centre | Mixed | 197 | |
| Red Deer Remand Centre | Mixed | 132 | |
| Saskatchewan (n = 6) | Pine Grove Correctional Centre | Female | 200 |
| Prince Albert Provincial Correctional Centre | Male | 500 | |
| Regina Provincial Correctional Center | Male | 800 | |
| Saskatoon Provincial Correctional Centre | Male | 500 | |
| White Birch Female Remand Unit | Female | 22 | |
| Whitespruce Provincial Training Centre | Male | 30 | |
| Manitoba (n = 7) | Brandon Correctional Centre | Male | 300 |
| Dauphin Correctional Centre | Male | 70 | |
| Headingley Correctional Centre | Male | 750 | |
| Milner Ridge Correctional Centre | Male | 420 | |
| Pas Correctional Centre | Mixed | 140 | |
| Winnipeg Remand Centre | Mixed | 282 | |
| Women’s Correctional Centre | Female | 200 | |
| Quebec (n = 16) | Établissement de détention d’Amos | Male | 136 |
| Établissement de détention de Baie-Comeau | Male | 82 | |
| Établissement de détention de Hull | Male | 231 | |
| Établissement de détention Leclerc de Laval | Mixed | 225 | |
| Établissement de détention de Montréal | Male | 1,377 | |
| Établissement de détention de New Carlisle et Havre-Aubert | Male | 85 | |
| Établissement de détention de Percé | Male | 42 | |
| Établissement de détention de Québec | Mixed | 724 | |
| Établissement de détention de Rimouski | Male | 121 | |
| Établissement de détention de Rivière-des-Prairies | Male | 578 | |
| Établissement de détention de Roberval | Male | 88 | |
| Établissement de détention de Sept-Îles | Male | 26 | |
| Établissement de détention de Sherbrooke | Male | 289 | |
| Établissement de détention de Sorel | Male | 87 | |
| Établissement de détention de St-Jérôme | Male | 435 | |
| Établissement de détention de Trois-Rivières | Male | 290 | |
| New Brunswick (n = 5) | Dalhousie Regional Correctional Centre | Male | 75 |
| Madawaska Regional Correctional Centre† | Male | 70 | |
| New Brunswick Women’s Correctional Centre | Female | 45 | |
| Southeast Regional Correctional Centre | Male | 160 | |
| Saint John Regional Correctional Centre | Male | 135 | |
| Nova Scotia (n = 4) | Cape Breton Correctional Facility | Male | 80 |
| Central Nova Scotia Correctional Facility | Mixed | 150 | |
| Northeast Nova Scotia Correctional Facility | Male | 90 | |
| Southwest Nova Scotia Correctional Facility† | Male | 38 | |
| Prince Edward Island (n = 2) | Prince County Correctional Centre, Summerside | Male | 12 |
| Provincial Correctional Centre, Charlottetown | Mixed | 85 | |
| Newfoundland and Labrador (n = 7) | Bishop’s Falls Correctional Centre | Male | 26 |
| Corner Brook Lockup† | Mixed | 17 | |
| Her Majesty’s Penitentiary | Male | 160 | |
| Labrador Correctional Centre† | Male | 38 | |
| Newfoundland & Labrador Correctional Centre for Women | Female | 25 | |
| St. John’s Lockup† | Mixed | 14 | |
| West Coast Correctional Institution† | Male | 50 |
Prison did not complete the survey
Acknowledgements:
The authors thank the participants for their time and participation in this study.
Funding Statement
NK is supported by a career award from the Fonds de Recherche Québec – Santé (FRQ-S; Junior 1).
Ethics Approval:
The study protocol was approved by an ethics committee and the ethics certificate information is available from the authors upon request.
Informed Consent:
Written informed consent or assent was implicit on the basis of survey completion.
Registry and Registration No. of the Study/Trial:
N/A
Funding:
NK is supported by a career award from the Fonds de Recherche Québec – Santé (FRQ-S; Junior 1).
Disclosures:
CD, BM, and CWN have no reported conflicts. NK has received research funding from Gilead Sciences, advisory fees from Gilead Sciences, ViiV Healthcare, Merck and Abbvie, and speaker fees from Gilead Sciences and Merck. SB is an (unpaid) non–executive director of Canadian registered charity Hepatitis Education and Prevention Society of British Columbia, an (unpaid) executive director of Papua New Guinean and Australian registered charity Grass Skirt Project Inc, and has received advisory fees from Gilead Sciences and speaker fees from Gilead Sciences (all personal fees given as unrestricted donations to BCCDC Foundation for Public Health). DF has received advisory fees from Gilead Sciences, Merck, and Abbvie. KK has received advisory fees from Gilead Sciences and Abbvie. KH has received research funding and speaker fees from Gilead Sciences and is employed by a non-profit funded in part by Gilead Sciences, Abbvie, and Merck. JC has received consulting fees from ViiV Healthcare and Gilead, grants from ViiV Healthcare, Merck, and Gilead; and payment for lectures from Gilead.
Peer Review:
This article has been peer reviewed
References
- 1.Dolan K, Wirtz AL, Moazen B, et al. Global burden of HIV, viral hepatitis, and tuberculosis in prisoners and detainees. Lancet. 2016;388(10049):1089–102. 10.1016/S0140-6736(16)30466-4. [DOI] [PubMed] [Google Scholar]
- 2.Larney S, Kopinski H, Beckwith CG, et al. Incidence and prevalence of hepatitis C in prisons and other closed settings: results of a systematic review and meta-analysis. Hepatology. 2013;58(4):1215–224. 10.1002/hep.26387. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone J, Fraser H, Lim AG, et al. Incarceration history and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis. Lancet Infect Dis. 2018;18(12):1397–409. 10.1016/S1473-3099(18)30469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stone J, Martin NK, Hickman M, et al. Modelling the impact of incarceration and prison-based hepatitis C virus (HCV) treatment on HCV transmission among people who inject drugs in Scotland. Addiction. 2017;112(7):1302–14. 10.1111/add.13783. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godin A, Kronfli N, Cox J, Alary M, Maheu-Giroux M. The role of prison-based interventions for hepatitis C virus (HCV) micro-elimination among people who inject drugs in Montréal, Canada. Int J Drug Policy. Forthcoming 2020. 10.1016/j.drugpo.2020.102738. Medline: [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Combating hepatitis B and C to reach elimination by 2030. 2016. https://www.who.int/hepatitis/publications/hep-elimination-by-2030-brief/en/ (July 15, 2020).
- 7.World Health Organization. Access to hepatitis C testing and treatment for people who inject drugs and people in prisons—a global perspective. 2019. https://www.who.int/hepatitis/publications/idu-prison-access-hepatitis-c/en/ (July 15, 2020).
- 8.Kouyoumdjian FG, McIsaac KE. Persons in correctional facilities in Canada: a key population for hepatitis C prevention and control. Can J Public Health. 2015;106(6):e454–6. 10.17269/cjph.106.5132. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trubnikov M, Yan P, Archibald C. Estimated prevalence of hepatitis C Virus infection in Canada, 2011. Can Communica Dis Rep. 2014;40(19):429–36. 10.14745/ccdr.v40i19a02. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canadian Network on Hepatitis C. Blueprint to inform hepatitis C elimination efforts in Canada. 2019. https://www.canhepc.ca/sites/default-/files/media/documents/blueprint_hcv_2019_05.pdf (July 15, 2020).
- 11.Correctional Service Canada. Facilities and security. 2018. https://www.csc-scc.gc.ca/facilities-and-security/index-eng.shtml (July 15, 2020).
- 12.Government of Alberta. Adult correctional and remand centres. 2020. https://www.alberta.ca/adult-correctional-remand-centres.aspx (July 15, 2020).
- 13.Government of British Columbia. Correctional centres. https://www2.gov.bc.ca/gov/content/justice/criminal-justice/corrections/correctional-centres (July 15, 2020).
- 14.Government of Manitoba. Adult correctional centres. https://www.gov.mb.ca/justice/commsafe/commsafediv/adult.html (July 15, 2020).
- 15.Government of New Brunswick. Justice and public safety: institutions. https://www2.gnb.ca/content/gnb/en/departments/public-safety/community_safety/content/corrections/institutions.html (July 15, 2020).
- 16.Government of Newfoundland and Labrador. Institutional services. https://www.gov.nl.ca/jps/corrections/institutional-services/ (July 15, 2020).
- 17.Government of Northwest Territories. Correctional facilities. https://www.justice.gov.nt.ca/en/correctional-facilities/ (July 15, 2020).
- 18.Government of Nunavut Department of Justice. Corrections. https://www.gov.nu.ca/justice/information/corrections (July 15, 2020).
- 19.Government of Ontario Ministry of the Solicitor General. Correctional services. 2019. https://www.mcscs.jus.gov.on.ca/english/corr_serv/CS_main.html (July 15, 2020).
- 20.Government of Prince Edward Island. Provincial custody programs. 2020. https://www.princeedwardisland.ca/en/information/justice-and-public-safety/provincial-custody-programs (July 15, 2020).
- 21.Government of Quebec Sécurité Publique du Québec. Bottin des établissements de détention du Québec. 2020. https://www.securitepublique.gouv.qc.ca/services-correctionnels/bottins/etablissements-de-detention.html (July 15, 2020).
- 22.Government of Saskatchewan. Saskatchewan correctional facilities. https://www.saskatchewan.ca/residents/justice-crime-and-the-law/correctional-facilities-and-probation/saskatchewan-correctional-facilities (July 15, 2020).
- 23.Government of Yukon. Department of Justice. 2016. http://www.justice.gov.yk.ca/prog/cor/ (July 15, 2020).
- 24.Province of Nova Scotia. Adult correctional facilities. 2018. https://novascotia.ca/just/Corrections/adult_facilities.asp (July 15, 2020).
- 25.Kronfli, N, Cox J. Care for people with hepatitis C in provincial and territorial prisons. CMAJ. 2018;190(4):E93–4. 10.1503/cmaj.171142. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kronfli N, Buxton JA, Jennings L, Kouyoumdjian F, Wong A. Hepatitis C virus (HCV) care in Canadian correctional facilities: where are we and where do we need to be? Can Liver J. 2019;4(2):171–83. 10.3138/canlivj.2019-0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reitano J. Adult correctional statistics in Canada, 2015/2016. 2017. https://www150.statcan.gc.ca/n1/en/pub/85-002-x/2017001/article/14700-eng.pdf?st=0fpGskxG (July 15, 2020).
- 28.Kronfli N, Dussault C, Klein MB, Lebouché B, Sebastiani G, Cox J. The hepatitis C virus cascade of care in a Quebec provincial prison: a retrospective cohort study. CMAJ Open. 2019;7(4):E674–9. 10.9778/cmajo.20190068. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Correctional Service Canada. Infectious disease surveillance 2014 hepatitis C virus (HCV). 2016. https://www.csc-scc.gc.ca/publications/005007-3038-eng.shtml (July 15, 2020).
- 30.Malakieh, J. Adult and youth correctional statistics in Canada, 2016/2017. 2018. https://www150.statcan.gc.ca/n1/en/pub/85-002-x/2018001/article/54972-eng.pdf?st=ZWqzfdqc (July 15, 2020).
- 31.LimeSurvey. Professional online surveys with LimeSurvey. https://account.limesurvey.org/ (July 15, 2020).
- 32.Galletly CL, Pinkerton SD, Petroll AE. CDC recommendations for opt-out testing and reactions to unanticipated HIV diagnoses. AIDS Patient Care STDs. 2008;22(3):189–93. 10.1089/apc.2007.0104. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Broeckaert L, Challacombe L. The routine offer of HIV testing in primary care settings: a review of the evidence. 2018. https://www.catie.ca/en/pif/spring-2018/routine-offer-hiv-testing-emergency-departments-review-evidence (July 27, 2020).
- 34.Swan D, Long J, Carr O, et al. Barriers to and facilitators of hepatitis C testing, management, and treatment among current and former injecting drug users: a qualitative exploration. AIDS Patient Care STDs. 2010;24(12):753–62. 10.1089/apc.2010.0142. Medline: [DOI] [PubMed] [Google Scholar]
- 35.Khaw F, Stobbart L. Murtagh MJ. ‘I just keep thinking I haven’t got it because I’m not yellow’: a qualitative study of the factors that influence the uptake of hepatitis C testing by prisoners. BMC Public Health. 2007;7:98. 10.1186/1471-2458-7-98. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crowley D, Van Hout MC, Murphy C, Kelly E, Lambert JS, Cullen W. Hepatitis C virus screening and treatment in Irish prisons from a governor and prison officer perspective—a qualitative exploration. Health Justice. 2018;6:23. 10.1186/s40352-018-0081-6. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lafferty L, Rance J, Grebely J, Lloyd AR, Dore GJ, Treloar C; SToP-C Study Group. Understanding facilitators and barriers of direct-acting antiviral therapy for hepatitis C virus infection in prison. J Viral Hepat. 2018;25(12):1526–32. 10.1111/jvh.12987. Medline: [DOI] [PubMed] [Google Scholar]
- 38.Papaluca T, Thompson A. HCV elimination: breaking down the barriers to prison based care. Hepatoma Res. 2018;4:64. 10.20517/2394-5079.2018.53. [DOI] [Google Scholar]
- 39.Webster PC. Integrating prison health care into public health care: the global view. CMAJ. 2013;185(7):E283. 10.1503/cmaj.109-4435. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pelletier L, MacFarlane A, Sharifi N. Correctional health services: transition to the provincial health services authority. 2018. https://cchl-ccls.ca/uploaded/web/BCHLC_2018/presentations/BCHLC2018_Pelletier-MacFarlane-Sharif.pdf (July 19, 2020). [Google Scholar]
- 41.Enggist S, Moller L, Galea G, Udesen C (eds.). Prisons and health. Copenhagen: World Health Organization; 2014. https://www.euro.who.int/_data/assets/pdf_file/0005/249188/Prisons-and-Health.pdf (July 19, 2020). [Google Scholar]
- 42.World Health Organization. Guidelines for the screening, care and treatment of persons with chronic hepatitis C infection. 2016. https://www.who.int/hepatitis/publications/hepatitis-c-guidelines-2016/en/ (July 19, 2020). [PubMed]
- 43.Canadian Task Force on Preventive Health Care. Recommendations on hepatitis C screening for adults. CMAJ. 2017;189(16):E594–604. 10.1503/cmaj.161521. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shah H, Bilodeau M, Burak KW, et al. The management of chronic hepatitis C: 2018 guideline update from the Canadian Association for the Study of the Liver. CMAJ. 2018;190(22):E677–87. 10.1503/cmaj.170453. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mohamed Z, Al-Kurdi D, Nelson M, et al. Time matters: point of care screening and streamlined linkage to care dramatically improves hepatitis C treatment uptake in prisoners in England. Int J Drug Policy. 2020;75:102608. 10.1016/j.drugpo.2019.102608. Medline: [DOI] [PubMed] [Google Scholar]
- 46.Morey S, Hamoodi A, Jones D, et al. Increased diagnosis and treatment of hepatitis C in prison by universal offer of testing and use of telemedicine. J Viral Hepat. 2019;26(1):101–8. 10.1111/jvh.13017. Medline: [DOI] [PubMed] [Google Scholar]
- 47.Beckwith CG, Kurth AE, Bazerman LB, et al. A pilot study of rapid hepatitis C virus testing in the Rhode Island Department of Corrections. J Public Health (Oxf). 2016;38(1);130–7. 10.1093/pubmed/fdv023. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rumble C, Pevalin DJ, O’Moore É. Routine testing for blood-borne viruses in prisons: a systematic review. Eur J Public Health. 2015;25(6):1078–88. 10.1093/eurpub/ckv133. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kronfli N, Dussault C, Chalifoux S, Kavoukian H, Klein MB, Cox J. A randomized pilot study assessing the acceptability of rapid point-of-care hepatitis C virus (HCV) testing among male inmates in Montreal, Canada. Int J Drug Policy. 2020;85:102921. 10.1016/j.drugpo.2020.102921. [DOI] [PubMed] [Google Scholar]
- 50.BCCDC Public Health Laboratory. BCCDC Public Health Laboratory update: hepatitis C reflex testing. 2020. Jan 16. https://smartsexresource.com/health-providers/blog/202001/bccdc-public-health-laboratory-update-hepatitis-c-reflex-testing (July 30, 2020).
- 51.Action Hepatitis Canada. Treatment access. https://www.actionhepatitiscanada.ca/treatment-access.html (July 15, 2020).
- 52.Cunningham EB, Amin J, Feld JJ, et al. Adherence to sofosbuvir and velpatasvir among people with chronic HCV infection and recent injection drug use: the SIMPLIFY study. Int J Drug Policy. 2018;62:14–23. 10.1016/j.drugpo.2018.08.013. Medline: [DOI] [PubMed] [Google Scholar]
- 53.Cunningham EB, Hajarizadeh B, Amin J, et al. Adherence to once-daily and twice-daily direct acting antiviral therapy for hepatitis C infection among people with recent injection drug use or current opioid agonist therapy. Clin Infect Dis. 2019;71(1):e115–24. 10.1093/cid/ciz1089. Medline: [DOI] [PubMed] [Google Scholar]
- 54.Aspinall EJ, Corson S, Doyle JS, et al. Treatment of hepatitis C virus infection among people who are actively injecting drugs: a systematic review and meta-analysis. Clin Infect Dis . 2013;57(Supplement 2):S80–9. 10.1093/cid/cit306. Medline: [DOI] [PubMed] [Google Scholar]
- 55.Chan J, Schwartz J, Kaba F, et al. Outcomes of hepatitis C virus treatment in the New York City jail population: successes and challenges facing scale up of care. Open Forum Infect Dis. 2020;7(7):ofaa263. 10.1093/ofid/ofaa263. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Akiyama MJ, Columbus D, MacDonald R, et al. Linkage to hepatitis C care after incarceration in jail: a prospective, single arm clinical trial. BMC Infect Dis.2019;19(1):703. 10.1186/s12879-019-4344-1. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kronfli N, Linthwaite B, Kouyoumdjian F, et al. Interventions to increase testing, linkage to care and treatment of hepatitis C virus (HCV) infection among people in prisons: a systematic review. Int J Drug Policy. 2018;57:95–103. 10.1016/j.drugpo.2018.04.003. Medline: [DOI] [PubMed] [Google Scholar]
- 58.Kronfli N, Nitulescu R, Cox J, et al. Previous incarceration impacts access to hepatitis C virus (HCV) treatment among HIV-HCV co-infected patients in Canada. J Int AIDS Soc. 2018;21(11):e25197. 10.1002/jia2.25197. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eibl JK, Morin K, Leinonen E, Marsh DC. The state of opioid agonist therapy in Canada 20 years after federal oversight. Can J Psychiatry. 2017;62(7):444–50. 10.1177/0706743717711167. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Correctional Service Canada. The prison needle exchange program. 2019. https://www.csc-scc.gc.ca/health/002006-2004-en.shtml (July 19, 2020).
- 61.Elliott R. Deadly disregard: government refusal to implement evidence-based measures to prevent HIV and hepatitis C virus infections in prisons. CMAJ. 2007;177(3): 262–4. 10.1503/cmaj.070854. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Childs E, Assoumou SA, Biello KB, et al. Evidence-based and guideline-concurrent responses to narratives deferring HCV treatment among people who inject drugs. Harm Reduct J. 2019;16(1):14. 10.1186/s12954-019-0286-6. Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Treloar C, Hull P, Bryant J, Hopwood M, Grebely J, Lavis Y. Factors associated with hepatitis C knowledge among a sample of treatment naive people who inject drugs. Drug Alcohol Depend. 2011;116(1–3):52–6. 10.1016/j.drugalcdep.2010.11.018. Medline: [DOI] [PubMed] [Google Scholar]
- 64.Treloar C, Hull P, Dore GJ, Grebely, J. Knowledge and barriers associated with assessment and treatment for hepatitis C virus infection among people who inject drugs. Drug Alcohol Rev. 2012;31(7):918–24. 10.1111/j.1465-3362.2012.00468.x. Medline: [DOI] [PubMed] [Google Scholar]
- 65.Dyer J, Tolliday L. Hepatitis C education and support in Australian prisons: preliminary findings of a nationwide survey. Health Promot J Austr. 2009;20(1):37–41. 10.1071/he09037. Medline: [DOI] [PubMed] [Google Scholar]
- 66.Overton K, Clegg J, Pekin F, et al. Outcomes of a nurse-led model of care for hepatitis C assessment and treatment with direct-acting antivirals in the custodial setting. Int J Drug Policy. 2019;72:123–8. 10.1016/j.drugpo.2019.02.013. Medline: [DOI] [PubMed] [Google Scholar]
- 67.Papaluca T, McDonald L, Craigie A, et al. Outcomes of treatment for hepatitis C in prisoners using a nurse-led, statewide model of care. J Hepatol. 2019;70(5):839–46. 10.1016/j.jhep.2019.01.012. Medline: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- BCCDC Public Health Laboratory. BCCDC Public Health Laboratory update: hepatitis C reflex testing. 2020. Jan 16. https://smartsexresource.com/health-providers/blog/202001/bccdc-public-health-laboratory-update-hepatitis-c-reflex-testing (July 30, 2020).
Supplementary Materials
Supplemental Table 1:
Participating adult provincial prisons in Canada
| Province | Adult provincial prison | Sex | Average daily inmate count |
|---|---|---|---|
| British Columbia (n = 10) | Alouette Correctional Centre for Women | Female | 158 |
| Ford Mountain Correctional Centre | Male | 98 | |
| Fraser Regional Correctional Centre | Male | 457 | |
| Kamloops Regional Correctional Centre | Male | 257 | |
| Nanaimo Correctional Centre | Male | 134 | |
| North Fraser Pretrial Centre | Male | 506 | |
| Okanagan Correctional Centre | Mixed | 26 | |
| Prince George Regional Correctional Centre | Mixed | 261 | |
| Surrey Pretrial Services Centre | Male | 524 | |
| Vancouver Island Regional Correctional Centre | Male | 311 | |
| Alberta (n = 8) | Calgary Correctional Centre | Mixed | 291 |
| Calgary Remand Centre | Mixed | 614 | |
| Edmonton Remand Centre | Mixed | 1,546 | |
| Fort Saskatchewan Correctional Centre | Mixed | 504 | |
| Lethbridge Correctional Centre | Mixed | 322 | |
| Medicine Hat Remand Centre | Mixed | 98 | |
| Peace River Correctional Centre | Mixed | 197 | |
| Red Deer Remand Centre | Mixed | 132 | |
| Saskatchewan (n = 6) | Pine Grove Correctional Centre | Female | 200 |
| Prince Albert Provincial Correctional Centre | Male | 500 | |
| Regina Provincial Correctional Center | Male | 800 | |
| Saskatoon Provincial Correctional Centre | Male | 500 | |
| White Birch Female Remand Unit | Female | 22 | |
| Whitespruce Provincial Training Centre | Male | 30 | |
| Manitoba (n = 7) | Brandon Correctional Centre | Male | 300 |
| Dauphin Correctional Centre | Male | 70 | |
| Headingley Correctional Centre | Male | 750 | |
| Milner Ridge Correctional Centre | Male | 420 | |
| Pas Correctional Centre | Mixed | 140 | |
| Winnipeg Remand Centre | Mixed | 282 | |
| Women’s Correctional Centre | Female | 200 | |
| Quebec (n = 16) | Établissement de détention d’Amos | Male | 136 |
| Établissement de détention de Baie-Comeau | Male | 82 | |
| Établissement de détention de Hull | Male | 231 | |
| Établissement de détention Leclerc de Laval | Mixed | 225 | |
| Établissement de détention de Montréal | Male | 1,377 | |
| Établissement de détention de New Carlisle et Havre-Aubert | Male | 85 | |
| Établissement de détention de Percé | Male | 42 | |
| Établissement de détention de Québec | Mixed | 724 | |
| Établissement de détention de Rimouski | Male | 121 | |
| Établissement de détention de Rivière-des-Prairies | Male | 578 | |
| Établissement de détention de Roberval | Male | 88 | |
| Établissement de détention de Sept-Îles | Male | 26 | |
| Établissement de détention de Sherbrooke | Male | 289 | |
| Établissement de détention de Sorel | Male | 87 | |
| Établissement de détention de St-Jérôme | Male | 435 | |
| Établissement de détention de Trois-Rivières | Male | 290 | |
| New Brunswick (n = 5) | Dalhousie Regional Correctional Centre | Male | 75 |
| Madawaska Regional Correctional Centre† | Male | 70 | |
| New Brunswick Women’s Correctional Centre | Female | 45 | |
| Southeast Regional Correctional Centre | Male | 160 | |
| Saint John Regional Correctional Centre | Male | 135 | |
| Nova Scotia (n = 4) | Cape Breton Correctional Facility | Male | 80 |
| Central Nova Scotia Correctional Facility | Mixed | 150 | |
| Northeast Nova Scotia Correctional Facility | Male | 90 | |
| Southwest Nova Scotia Correctional Facility† | Male | 38 | |
| Prince Edward Island (n = 2) | Prince County Correctional Centre, Summerside | Male | 12 |
| Provincial Correctional Centre, Charlottetown | Mixed | 85 | |
| Newfoundland and Labrador (n = 7) | Bishop’s Falls Correctional Centre | Male | 26 |
| Corner Brook Lockup† | Mixed | 17 | |
| Her Majesty’s Penitentiary | Male | 160 | |
| Labrador Correctional Centre† | Male | 38 | |
| Newfoundland & Labrador Correctional Centre for Women | Female | 25 | |
| St. John’s Lockup† | Mixed | 14 | |
| West Coast Correctional Institution† | Male | 50 |
Prison did not complete the survey


