Abstract
Hepatitis C virus (HCV) is the leading cause of death from infectious disease in Canada. Immigrants are an important group who are at increased risk for HCV; they account for a disproportionate number of all HCV cases in Canada (~30%) and have approximately a twofold higher prevalence of HCV (~2%) than those born in Canada. HCV-infected immigrants are more likely to develop cirrhosis and hepatocellular carcinoma and are more likely to have a liver-related death during a hospitalization than HCV-infected non-immigrants. Several factors, including lack of routine HCV screening programs in Canada for immigrants before or after arrival, lack of awareness on the part of health practitioners that immigrants are at increased risk of HCV and could benefit from screening, and several patient- and health system–level barriers that affect access to health care and treatment likely contribute to delayed diagnosis and treatment uptake. HCV screening and engagement in care among immigrants can be improved through reminders in electronic medical records that prompt practitioners to screen for HCV during clinical visits and implementation of decentralized community-based screening strategies that address cultural and language barriers. In conclusion, early screening and linkage to care for immigrants from countries with an intermediate or high prevalence of HCV would not only improve the health of this population but will be key to achieving HCV elimination in Canada. This article describes the unique barriers encountered by the foreign-born population in accessing HCV care and approaches to overcoming these barriers.
Keywords: Canada, foreign-born, hepatitis C, immigrants
Introduction
The health care burden from, cost of, and mortality from hepatitis C (HCV) infection are increasing in Canada because of asymptomatic undetected or untreated infections that progress to chronic liver disease and hepatocellular carcinoma (HCC) (1–8). Newly available, short-course, well-tolerated direct-acting antiviral (DAA) therapies that cure HCV in more than 95% of cases and that decrease liver-related morbidity and mortality provide an opportunity to reverse this trend (9). Canada has endorsed and is committed to the World Health Organization (WHO) goal of eliminating hepatitis C as a public health threat by 2030 (10–12). To achieve WHO goals, high uptake along all steps of the HCV care cascade (diagnosis, linkage to care, treatment, and cure) will be required for all at-risk populations (13,14).
Immigrants are an important group at increased risk for HCV; they account for a disproportionate number of hepatitis C cases in Canada (~30%), have an approximately twofold higher prevalence of HCV (~2%), and are more likely to develop HCC and to have a liver-related death in hospital than people born in Canada (15–22). The long delay to HCV diagnosis (mean 10 years) and linkage to liver-related care (mean 15 years) after arrival in Canada are likely responsible for these poor liver-related outcomes (17,23). To achieve HCV elimination in Canada, it will be imperative to focus more attention on and effort in improving HCV screening and treatment among the Canadian foreign-born population. This article focuses on hepatitis C in the immigrant population in Canada in the context of the global hepatitis C epidemic and outlines the diversity of the immigrant population in Canada, changing flows and patterns of migration over time, the prevalence and burden of HCV among those who are foreign-born, barriers they encounter in accessing HCV screening and care, and approaches to overcoming these barriers.
Global Epidemiology of Hepatitis C
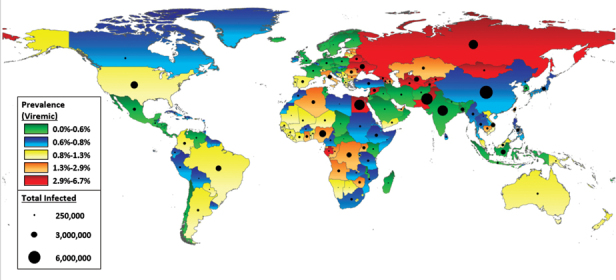
The majority of immigrants arriving in Canada over the past four decades have originated from countries in which HCV is endemic, and their HCV risk reflects that in their country of birth (15,24). Worldwide, 71 million people are living with chronic HCV, and 399,000 die from it annually (25). The majority of the global burden of HCV is borne by low- and middle-income countries in which the primary mode of transmission is through transfusion of unscreened blood products; the use of unsterilized or inadequately sterilized medical, dental, and surgical equipment; and unsafe injections (25–28). This is in contrast to high-income countries in which the majority of new infections are transmitted through injection drug use (29,30). Globally, HCV infection is unevenly distributed. Countries are classified by HCV prevalence and are considered to be low (anti-HCV antibody prevalence <2%; viremic prevalence <1.5%), intermediate (anti-HCV antibody prevalence ≥2%–5%; viremic prevalence ≥1.5%–3.75%), or high (anti-HCV antibody prevalence ≥5%; viremic prevalence ≥3.75%) prevalence (31–33) (Table 1;Figure 1). Countries in Central Asia, Eastern Europe, North Africa and the Middle East, and sub-Saharan Africa have the highest prevalence of HCV infection, whereas countries in North America, Latin America, and Western Europe have low HCV prevalence (31). Globally, Egypt has the highest prevalence, with 6.3% (5.6 million) of the population having viremic infection. These high rates are due to initial transmission from the late 1950s through the early 1980s through reuse of unsterilized needles during schistosomiasis treatment campaigns and to ongoing transmission through improperly sterilized medical equipment and intrafamilial spread (27,35,36). Although viremic prevalence is much lower than in Egypt (<1.2%), the largest number of HCV cases (almost 30 million) are found in East Asia and the Indian subcontinent (Table 1). China (9.8 million), Pakistan (7.2 million), and India (6.2 million) have the highest number of cases globally and are among the top source countries for new immigrants arriving in Canada (24,31). The primary mode of transmission in these regions is also iatrogenic, but intravenous drug use is increasing.
Table 1:
Reported HCV seroprevalence and viremic infections by global region
| %, CI | ||
|---|---|---|
| Region | Anti-HCV prevalence (34) | Viremic infections (31) |
| Asia Pacific, high income | 1.1 (0.5 to 1.7) | 0.6 (0.3 to 0.7) |
| Asia, Central | 5.4 (3.5 to 6.8) | 3.6 (2.8 to 3.9) |
| Asia, East | 1.2 (0.4 to 1.8) | 0.7 (0.5 to 0.8) |
| Asia, South | 1.1 (0.7 to 1.5) | 0.9 (0.7 to 1.3) |
| Asia, Southeast | 1.0 (0.8 to 1.8) | 0.7 (0.5 to 0.8) |
| Australasia | 1.4 (1.0 to 1.5) | 1.0 (0.8 to 1.0) |
| Caribbean | 0.8 (0.2 to 1.3) | 0.5 (0.4 to 0.8) |
| Europe, Central | 1.3 (1.1 to 1.6) | 1.0 (0.8 to 1.0) |
| Europe, Eastern | 3.3 (1.6 to 4.5) | 3.3 (2.1 to 3.4) |
| Europe, Western | 0.9 (0.7 to 1.5) | 0.5 (0.4 to 0.8) |
| Latin America, Andean | 0.9 (0.4 to 1.3) | 0.5 (0.3 to 0.6) |
| Latin America, Central | 1.0 (0.8 to 1.4) | 0.5 (0.4 to 0.5) |
| Latin America, Southern | 1.2 (0.5 to 2.1) | 0.6 (0.3 to 0.9) |
| Latin America, Tropical | 1.2 (0.9 to 1.2) | 0.9 (0.6 to 0.9) |
| North Africa/Middle East | 3.1 (2.5 to 3.9) | 1.7 (1.4 to 1.9) |
| North America, high income | 1.0 (1.0 to 1.9) | 0.9 (0.7 to 1.1) |
| Oceania | 0.1 (0.1 to 0.6) | 1.1 (0.8 to 3.7) |
| Sub-Saharan Africa, Central | 4.2 (2.4 to 9.2) | 2.1 (0.1 to 6.9) |
| Sub-Saharan Africa, East | 1.0 (0.6 to 3.1) | 0.5 (0.4 to 0.7) |
| Sub-Saharan Africa, Southern | 1.3 (0.8 to 2.5) | 0.7 (0.4 to 0.9) |
| Sub-Saharan Africa, West | 5.3 (2.9 to 9.1) | 1.3 (1.1 to 1.4) |
| Total | 1.6 (1.3 to 2.1) | 1.0 (0.8 to 1.1) |
Figure 1:
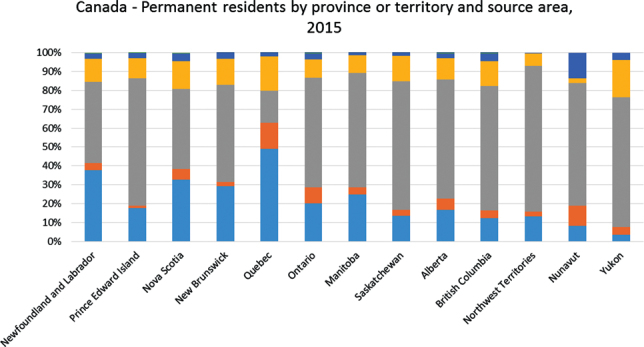
Region of origin of immigrants in Canada by province: 2015 (37).
Source: Statistics Canada (http://www.statcan.gc.ca/daily-quotidien/171025/dq171025b-eng.htm). Reproduced and distributed on an “as-is” basis with the permission of Statistics Canada.
Immigration Patterns in Canada
One-fifth (21%) of the Canadian population in 2016 was foreign born, and Canada receives more than 250,000 new immigrants annually (24). In 2016, almost half (48.1%) of the immigrants living in Canada were born in Asia (including the Middle East), 8.5% were born in Africa, and fewer than one-third (27.7%) were born in Europe. The proportion of immigrants from high-HCV-burden countries living in Canada has increased from 10.9% (1971 Census) to almost 70% (2016 Census) over the past 50 years (24) (Figure 2). The pattern of top source countries of immigrants living in each province and city varies and is driven by linguistic preferences, cultural links, and job availability. Quebec selects and attracts immigrants primarily from French-speaking countries, British Columbia has a large South Asian and Southeast Asian diaspora, and Ontario attracts a very diverse sample of immigrants from English-speaking source countries (37) (Figure 3). Ontario, British Columbia, and Quebec are home to more than two-thirds of all immigrants in Canada, but more recent immigrants are settling in the Prairie and Atlantic provinces. Immigrant-focused programming for prevention and care, therefore, will be needed in all Canadian provinces (24).
Figure 2:
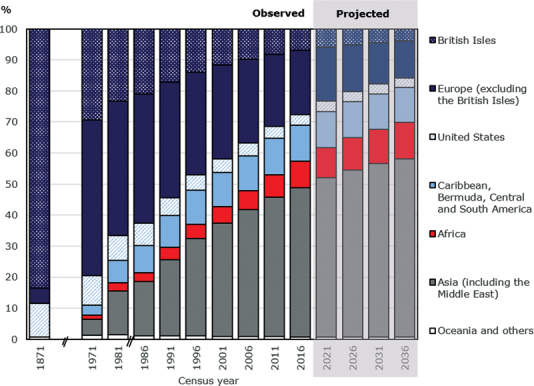
Distribution of foreign-born population by region of birth, Canada 1821–2026.
Source: Statistics Canada (http://www.statcan.gc.ca/daily-quotidien/171025/dq171025b-eng.htm). Reproduced and distributed on an “as-is” basis with the permission of Statistics Canada
Figure 3:
Prevalence of HCV viremia and number of HCV viremic individuals globally in 2016.
HCV = Hepatitis C virus.
Courtesy of H. Razavi.
Source: The Polaris Observatory HCV Collaborators (http://cdafound.org/polaris/)
Prevalence of and Risk Factors for Hepatitis C
Immigrants from intermediate- and high-HCV-prevalence countries have higher anti-HCV prevalence (1.9% vs. 0.8%) than the Canadian population (15,16). A systematic review of the anti-HCV prevalence in immigrants living in low-HCV-prevalence host countries found that HCV prevalence in the country of origin was a good proxy for the expected prevalence in the immigrant population (15). (SeeAppendix 1for prevalence and distribution by country.) The foreign-born population often does not have the traditional percutaneous HCV risk factors with which Canadian practitioners are familiar, and this is likely a barrier to HCV screening among immigrants (17,19,20). The difference in HCV risk factor profiles was demonstrated in a cohort of HCV-infected individuals in Quebec. In this study, nonimmigrants were significantly more likely to be male (68.3% vs. 53.6%), were younger (43.2 years vs 47.5 years), and had higher rates of problematic drug use (23.9% vs 2.5%), alcohol use (12.8% vs 1.5%), and HIV infection (4.6% vs. 1.2%) than immigrants (17,21). Similar results were also reported in another Canadian study (23). These differences are due to different modes of transmission of HCV in high- and low-resource countries (25–27). Additional modes of transmission among immigrants may occur because of community exposure in their countries of origin or through specific cultural practices. Shaving at community barber shops is a risk factor for acquiring HCV in studies from India and Pakistan, where razors are reused without sterilization and where a potash alum stone is rubbed on facial shaving cuts and reused on many people (38,39). Alternative medicine practices such as wet cupping, a blood-drawing technique that lacerates the skin through traction using a cup, are common in many Muslim countries, and acupuncture is an important HCV risk factor among East Asian populations (27,40,41).
Burden and Health Outcomes Related to HCV
Several studies show that HCV-infected immigrants bear a disproportionate burden of liver-associated complications compared with host populations. HCV-infected immigrants are older and more likely to have HCC at the time of diagnosis. Unadjusted analyses show that they are twice as likely to develop HCC during follow-up than host populations (17,18,20). In multivariate analyses, however, the increased risk among immigrants of developing HCC is found to be due to older age and diabetes rather than to immigrant status (17–19). Furthermore, immigrants from intermediate- and high-HCV-prevalence countries are also more likely to be admitted with an HCV-related hospitalization and to die from HCC during a liver-related hospitalization than those born in Canada (21,22). These data, taken together with the long delays to diagnosis and linkage to care after arrival, suggest that the observed advanced liver disease among immigrants is a missed opportunity for early screening and engagement in care and treatment (17,23).
Health of Immigrants and Barriers to Accessing HCV Screening and Treatment
Eliminating hepatitis C will require a comprehensive approach along the entire care continuum (diagnosis, linkage to care, treatment, and cure) and provision of services tailored to the needs of high-risk and vulnerable populations. Barriers to accessing HCV care and achieving sustained virologic response for all HCV-infected persons occur at the patient, provider, and health system levels (42). At the patient level, barriers include lack of awareness of HCV and poor treatment completion because of fear of side effects, poor adherence to treatment, and comorbid conditions such as mental illness or substance use. For providers, limited knowledge of HCV screening processes and treatment and communication difficulties with patients may be problematic. At the health system level, the lack of promotion and surveillance programs and funding for HCV treatment are limitations (42). Immigrants have additional unique barriers to accessing health care that may contribute to further gaps along the HCV care continuum, particularly among vulnerable subgroups. These multiple factors will further challenge HCV elimination efforts in Canada (43–46).
Immigrants are in better health when they arrive in Canada, a phenomenon described as the healthy immigrant effect, but this diminishes over time (47,48). This health decline is due to several factors, including linguistic barriers or cultural differences, discrimination and racism, poor socio-economic status, and barriers to accessing and navigating the health care system (43–46). Certain subgroups of immigrants are particularly at risk for deteriorating health status and include refugees (odds ratio [OR] 2.31), those with low income (OR 1.5; 95% CI 1.3 to 1.7), and those of non-European origin (OR 2.3; 95% CI 1.6 to 3.3) (49). Illegal migrants and those with temporary status (such as those on work visas and students) face additional challenges because they are not entitled to health care benefits (50). Specific barriers to accessing HCV screening and care among immigrants are described later and need to be addressed to optimize the HCV care cascade for this population.
Individual barriers
Knowledge of the importance of hepatitis C, its consequences, and the risk factors for transmission are low among certain immigrant populations and are significantly lower than among nonimmigrants living in the same country (51,52). Immigrants with a higher level of education, who are employed full time, and who are highly acculturated (adapted to the host culture), however, had better knowledge of HCV than other immigrants (52,53). Cultural differences resulting from religious beliefs; attitudes toward health, illness, and medicine; and disease-associated stigma are important barriers in the uptake of screening and treatment of other infectious diseases such as tuberculosis and blood-borne infections such as HIV (50,54–56). These barriers influence the health-seeking behaviour of affected individuals, who might choose not to seek treatment or not to disclose symptoms to their health care practitioner to avoid stigmatization (50). In addition, individuals may seek care from traditional healers from their own cultural communities (50,54). There are no specific data on the impact of these factors among HCV-infected immigrants, but they are also likely important barriers. Socio-economic factors such as precarious employment with the risk of lost wages, lack of insurance coverage, lack of transportation, or lack of child care lead to poor clinic appointment attendance or treatment completion (55,56).
Provider barriers
There are several physician-level barriers to identifying and managing patients with HCV infection (42,57). In the United States, ethnic minorities are less likely than Caucasians to be tested for HCV in the presence of HCV risk factors or to be referred for subspecialty care and treatment (58,59). Physicians are frequently unaware of or incorrectly identify traditional risk factors for acquiring HCV in both the general and immigrant populations (42,57). Many practitioners are also unaware that immigrants may have additional HCV risk factors as a result of exposure in their country of origin from iatrogenic procedures or receipt of screened blood products (42,57,60). Language and cultural discordance between physicians and patients leads to poor communication and low quality of care. A lack of interpreters is associated with reduced satisfaction with clinician communication, lower overall satisfaction with health care, poor patient comprehension of care received, poor compliance with treatment recommendations, reduced medication adherence, and missed follow-up visits (61–63). As highlighted earlier, immigrants from endemic countries are settling in all provinces; hence, there is a need for awareness among practitioners that being an immigrant from an endemic country is an important HCV risk factor and a criterion for screening.
Health system barriers
Health system barriers affect all steps along the HCV care cascade. Immigrants are not routinely screened for viral hepatitis before or after arrival in Canada. During the mandated prelanding medical exam, routine viral hepatitis screening is not performed (64). Only applicants with viral hepatitis risk factors; evidence of liver disease on history or physical exam; or those found to have HIV, tuberculosis, or syphilis on exam are required to undergo hepatitis B and hepatitis C testing. Those who test positive for hepatitis B virus or HCV are permitted to enter Canada, but there is no procedure to ensure linkage to care after arrival (64). The Canadian Task force recommend HCV screening for all those with HCV risk factors such as current or prior injection drug use, incarceration, receipt of blood products before 1992, and having been born in an HCV-endemic country (≥2% anti-HCV prevalence) (65).
Despite these recommendations, there are no systematic, targeted HCV screening or health promotion programs for immigrants after arrival in Canada (56,66). Many clinics and hospitals across Canada lack interpreter services and culturally adapted programs despite the fact that providing interpreters increases screening and compliance with medications and decreases costs (63,67,68). Although health services in Canada are universally provided to all those with legal status, DAA therapy has been restricted to those with advanced liver disease and has been an important barrier to accessing HCV therapy for all HCV-infected individuals (69,70). Canada has recently negotiated lower prices for DAA medications (71). Expanded public funding of these treatments is, therefore, expected to cover all infected persons in most provinces in the near future (71). Migrants without legal status or health insurance will not benefit from these changes because they are not entitled to free access to either health care or medications.
Increasing Uptake of Hepatitis C Screening and Treatment
Several outreach programs for immigrants have been developed that address the unique individual and health system barriers they encounter in accessing HCV care. Studies show that HCV screening uptake and linkage to care can be improved among immigrants by implementing decentralized community-based screening strategies that are culturally and linguistically adapted and developed in collaboration with community-based organizations (72–76). Furthermore, point-of-care testing integrated with testing for other infections in the primary care setting has been shown to increase HCV testing uptake (72,77). When HCV care is delivered by a multidisciplinary team, with provision of interpreters as needed and staff sensitive to cultural differences, immigrants are as likely to be offered HCV treatment, to adhere to treatment, and to achieve a sustained virologic response as those born in Canada (23,78).
The US Centers for Disease Control and Prevention Hepatitis Testing and Linkage to Care program and the Hepatitis Outreach Network program in New York City are examples of programs that achieve high levels of screening (50%–60%) and linkage to care (65%) of individuals from several immigrant communities. These programs engage community-based organizations, use outreach workers of the same culture and language, facilitate appointments with reminders, publicize events in the native languages of the target communities, and reach out to nontraditional venues such as religious institutions and community centers (74,75,79,80). Similarly, the EU-HEP-SCREEN program was a pilot project conducted between 2012 and 2014 among immigrants in Spain, Hungary, and the United Kingdom that used different screening approaches including community outreach, opportunistic screening during primary care visits, and the addition of HCV screening to existing public health programs (72). The highest screening uptake occurred in settings in which screening was offered opportunistically or where existing programs were extended (70%–78% uptake).
Initiatives are underway to improve screening, diagnosis, and linkage to care and treatment among immigrant groups in Canada. Example programs are those developed by CATIE (Canada’s source for HIV and hepatitis C information;www.catie.ca) and Hepatitis Education Canada (http://hepatitiseducation.ca/). CATIE introduced a Hepatitis C Ethnocultural Educational, Outreach and Social Marketing pilot program in 2010 (81). The objective of the program is to increase knowledge and awareness of HCV and to improve screening uptake among immigrants. This program, focused on the largest immigrant communities in Ontario (Chinese, Punjabi, Pakistani, and Filipino), has conducted community education and outreach, developed and distributed linguistically and culturally adapted resources, and has conducted media campaigns concerning hepatitis C. The community outreach workshops have taken place in local community centers, schools, and places of worship and have reached 10,000 immigrants and newcomers living in Ontario (81).
Hepatitis Education Canada is a project developed by the Hepatitis Services at the British Columbia Centre for Disease Control and funded by the Public Health Agency of Canada. They have developed linguistically and culturally adapted hepatitis C education resources for various population groups with the aim of increasing knowledge and awareness of hepatitis C disease and its screening and management. This program has focused on educational resources for South Asian and East Asian groups in Punjabi, Urdu, simplified Chinese, and Tagalog. Resources include print materials, a Web site, and short videos. The videos produced were based on requests from community groups to increase community reach. During this project, it was found that physicians did not routinely offer HCV testing to the South Asian population because their knowledge of how to screen and engage patients in care and HCV treatment was suboptimal. Educational programs for physicians were developed to address this issue, including a one-page screening and testing guide (82). The Public Health Agency of Canada Community Action Fund on Hepatitis C and HIV has also recently funded two community groups (Progressive Intercultural Society [http://pics.bc.ca/] and S.U.C.C.E.S.S. [http://www.successbc.ca/eng/]) to increase awareness, screening, and linkage to care for HCV and HIV among South Asian and East Asian immigrant groups in the Greater Vancouver Area. This program involves educational sessions at settlement services and other venues, screening for HCV and HIV, and linking those who test positive to the next level of services for further care.
Educating and engaging physicians in the care of immigrants with HCV is an important strategy to increase screening and treatment of this population. Primary care practitioners, who are often the first health professionals consulted, need to be aware of risk factors for HCV infection in this group and the influence of ethnicity and culture on the perception of disease so that they can conduct effective patient education and counselling. Among the underserved HCV-infected population in the United States, initiatives aimed at educating primary care providers to improve their knowledge and comfort with managing hepatitis C and its complications, such as the Extension for Community Healthcare Outcome project, have been successful in their goals (83). Clinician reminders to prompt HCV testing during clinical visits have been shown to increase HCV testing rates (OR 3.70; 95% CI 1.81 to 7.57) (84). Clinical care guidelines highlighting the unique health care needs of immigrants are important educational materials for practitioners. A few examples of published guidelines and online tools to aid in identifying country-of-origin-specific screening and testing needs of immigrants are those produced by the Canadian Collaboration for Immigrant and Refugee Health, the Canadian Pediatrics Society, Public Health England, and the British Columbia Centre for Disease Control (56,82,85–87). Finally, programs should be established that better respond to the linguistic, cultural, social, religious, and health status differences that are currently barriers to immigrants’ ability to effectively access and use health care services. One critical health system barrier is the lack of universal access to interpreter services across Canada (88).
Conclusion
Canada is a multicultural society with a large and growing diverse, foreign-born population. Immigrants from intermediate- and high-HCV-prevalence countries living in Canada are at increased risk for HCV and have poorer liver-associated outcomes than host populations. The long delay to diagnosis and linkage to care among the immigrant population is a missed opportunity to engage this population and treat and cure HCV before it progresses to the advanced stages of liver disease. Improving the HCV care continuum among Canadian immigrants will require addressing patient, practitioner, and health system barriers that lead to poor access to health care. Implementing culturally and linguistically adapted HCV screening for immigrants will not only benefit this population but will be key to eliminating hepatitis C in Canada.
Acknowledgments
Acknowledgements
This article is part of a special topic series commissioned by the Canadian Network on Hepatitis C (CanHepC). CanHepC is funded by a joint initiative of the Canadian Institutes of Health Research (NHC-142832) and the Public Health Agency of Canada.
Ethics Approval:
N/A
Informed Consent:
N/A
Registry and Registration No. of The Study/Trial:
N/A
Funding
No funding was received for this work.
Disclosures
The authors have nothing to disclose.
APPENDIX 1
Table A.1:
Reported HCV prevalence (antibody and viremia) distribution by country
| %, CI | ||
|---|---|---|
| Region and country | Anti-HCV prevalence (34) | Viremic prevalence (31) |
| Asia Pacific, high income | 1.1 (0.5 to 1.7) | 0.6 (0.3 to 0.7) |
| Japan | 1.5 (0.5 to 2.2) | 0.7 (0.3 to 0.8) |
| Korea, Republic of | 0.8 (0.2 to 2.1) | 0.5 (0.3 to 0.5) |
| Asia, Central | 5.4 (3.5 to 6.8) | 3.6 (2.8 to 3.9) |
| Azerbaijan | 3.1 (1.0 to 6.7) | 1.9 (1.3 to 2.1) |
| Georgia | 6.7 (5.6 to 7.3) | 4.2 (3.0 to 4.2) |
| Kazakhstan | 3.3 (1.0 to 6.7) | 2.8 (1.9 to 3.2) |
| Kyrgyzstan | 2.5 (1.6 to 6.7) | — |
| Mongolia | 10.8 (8.7 to 15.6) | 6.4 (4.3 to 7.9) |
| Tajikistan | 3.1 (1.1 to 6.7) | — |
| Turkmenistan | 5.6 (1.1 to 6.7) | — |
| Uzbekistan | 11.3 (6.4 to 13.1) | 4.3 (3.0 to 5.0) |
| Asia, East | 1.2 (0.4 to 1.8) | 0.7 (0.5 to 0.8) |
| China | 1.3 (0.4 to 2.0) | 0.7 (0.5 to 0.8) |
| Hong Kong | — | 0.2 (0.1 to 0.3) |
| Taiwan | 4.4 (2.5 to 6.3) | 2.1 (1.3 to 3.7) |
| Asia, South | 1.1 (0.7 to 1.5) | 0.9 (0.7 to 1.3) |
| Afghanistan | 1.1 (0.6 to 1.9) | 0.5 (0.3 to 0.8) |
| Bangladesh | 1.3 (0.2 to 2.2) | — |
| India | 0.8 (0.4 to 1.0) | 0.5 (0.4 to 0.8) |
| Pakistan | 6.7 (1.6 to 10.0) | 3.8 (2.8 to 3.9) |
| Asia, Southeast | 1.0 (0.8 to 1.8) | 0.7 (0.5 to 0.8) |
| Indonesia | 0.8 (0.4 to 2.0) | 0.5 (0.2 to 0.8) |
| Cambodia | 2.3 (2.3 to 14.7) | 1.6 (0.9 to 1.7) |
| Myanmar | 1.7 (1.0 to 2.7) | — |
| Malaysia | 1.5 (0.3 to 7.7) | 1.2 (0.8 to 1.3) |
| Philippines | 0.9 (0.3 to 2.0) | 0.6 (0.3 to 0.6) |
| Thailand | 2.7 (1.8 to 3.7) | 0.7 (0.4 to 0.7) |
| Vietnam | — | 1.1 (0.6 to 1.2) |
| Australasia | 1.4 (1.0 to 1.5) | 1.0 (0.8 to 1.0) |
| Australia | 1.7 (1.2 to 1.8) | 1.0 (0.7 to 1.0) |
| New Zealand | 1.9 (0.8 to 2.2) | 1.0 (0.6 to 1.3) |
| Caribbean | 0.8 (0.2 to 1.3) | 0.5 (0.4 to 0.8) |
| Cuba | — | 0.3 (0.1 to 0.7) |
| Dominican Republic | — | 0.6 (0.4 to 1.0) |
| Guadeloupe | — | 0.3 (0.2 to 0.6) |
| Europe, Central | 1.3 (1.1 to 1.6) | 1.0 (0.8 to 1.0) |
| Bulgaria | 1.1 (0.3 to 2.4) | 1.2 (0.7 to 1.6) |
| Czech Republic | 0.7 (0.2 to 0.7) | 0.4 (0.2 to 0.5) |
| Croatia | — | 0.6 (0.4 to 0.7) |
| Hungary | 0.8 (0.4 to 2.7) | 0.5 (0.3 to 0.6) |
| Poland | 0.9 (0.6 to 1.1) | 0.5 (0.4 to 0.6) |
| Romania | 3.2 (2.9 to 3.6) | 2.5 (1.8 to 2.6) |
| Slovakia | 1.4 (0.9 to 2.0) | 0.6 (0.4 to 0.7) |
| Slovenia | — | 0.3 (0.2 to 0.3) |
| Europe, Eastern | 3.3 (1.6 to 4.5) | 3.3 (2.1 to 3.4) |
| Belarus | 1.3 (0.9 to 2.9) | — |
| Estonia | — | 1.4 (0.9 to 1.6) |
| Lithuania | 2.9 (0.7 to 3.0) | 1.1 (0.7 to 1.3) |
| Latvia | 2.4 (1.7 to 3.3) | 2.2 (1.4 to 2.6) |
| Moldova | 4.5 (2.3 to 4.5) | — |
| Russia | 4.1 (1.2 to 5.6) | 3.3 (2.3 to 3.5) |
| Ukraine | 3.6 (0.9 to 4.5) | — |
| Europe, Western | 0.9 (0.7 to 1.5) | 0.5 (0.4 to 0.8) |
| Austria | 0.5 (0.1 to 0.7) | 0.2 (0.1 to 0.4) |
| Belgium | 0.9 (0.1 to 1.2) | 0.6 (0.2 to 0.7) |
| Switzerland | 1.5 (0.7 to 1.8) | 1.0 (0.6 to 1.1) |
| Cyprus | 0.6 (0.5 to 1.9) | — |
| Germany | 0.6 (0.3 to 0.9) | 0.3 (0.1 to 0.4) |
| Denmark | 0.7 (0.5 to 0.7) | 0.3 (0.3 to 0.3) |
| Spain | 1.7 (0.4 to 2.6) | 0.8 (0.3 to 1.2) |
| Finland | 0.7 (0.6 to 0.9) | 0.4 (0.3 to 0.5) |
| France | 0.6 (0.4 to 1.1) | 0.3 (0.1 to 0.3) |
| United Kingdom | 0.6 (0.4 to 1.2) | 0.3 (0.1 to 0.3) |
| Greece | 1.9 (0.5 to 2.6) | 1.1 (0.7 to 1.5) |
| Iceland | — | 0.3 (0.2 to 0.4) |
| Ireland | 1.1 (0.7 to 1.6) | 0.6 (0.4 to 0.9) |
| Israel | 2.0 (0.9 to 2.0) | 1.2 (0.7 to 1.3) |
| Italy | 2.0 (1.6 to 7.3) | 1.1 (0.7 to 2.7) |
| Luxembourg | 0.9 (0.6 to 0.9) | 0.9 (0.6 to 1.0) |
| Malta | — | 0.3 (0.2 to 0.4) |
| Netherlands | 0.2 (0.1 to 0.4) | 0.1 (0.0 to 0.2) |
| Norway | 0.7 (0.6 to 0.9) | 0.4 (0.3 to 0.5) |
| Portugal | 1.8 (0.5 to 2.9) | 0.8 (0.7 to 1.1) |
| Sweden | 0.7 (0.5 to 0.7) | 0.4 (0.3 to 0.4) |
| Latin America, Andean | 0.9 (0.4 to 1.3) | 0.5 (0.3 to 0.6) |
| Peru | 1.2 (0.4 to 1.6) | 0.5 (0.3 to 0.6) |
| Latin America, Central | 1.0 (0.8 to 1.4) | 0.5 (0.4 to 0.5) |
| Colombia | — | 0.8 (0.6 to 0.9) |
| Mexico | 1.4 (1.1 to 1.6) | 0.4 (0.3 to 0.5) |
| Panama | — | 0.3 (0.2 to 0.3) |
| Venezuela | 1.5 (0.3 to 2.6) | 0.4 (0.2 to 0.4) |
| Latin America, Southern | 1.2 (0.5 to 2.1) | 0.6 (0.3 to 0.9) |
| Argentina | 1.5 (0.5 to 2.5) | 0.8 (0.3 to 1.2) |
| Chile | — | 0.3 (0.2 to 0.5) |
| Latin America, Tropical | 1.2 (0.9 to 1.2) | 0.9 (0.6 to 0.9) |
| Brazil | 1.6 (1.1 to 1.6) | 0.9 (0.6 to 0.9) |
| North Africa and the Middle East | 3.1 (2.5 to 3.9) | 1.7 (1.4 to 1.9) |
| Algeria | 1.4 (0.2 to 2.5) | 1.0 (0.3 to 1.7) |
| Bahrain | — | 1.2 (0.8 to 1.3) |
| Egypt | 14.7 (10.3 to 18.0) | 6.3 (4.5 to 6.7) |
| Iran | 0.5 (0.2 to 1.0) | 0.2 (0.2 to 0.3) |
| Iraq | 3.2 (0.3 to 3.2) | 0.2 (0.2 to 0.3) |
| Jordan | — | 0.3 (0.1 to 0.4) |
| Lebanon | — | 0.2 (0.1 to 0.4) |
| Libya | 1.2 (1.2 to 2.3) | 0.7 (0.5 to 0.7) |
| Morocco | 1.6 (0.6 to 1.9) | 0.8 (0.5 to 0.9) |
| Oman | — | 0.4 (0.3 to 0.4) |
| Qatar | 0.9 (0.5 to 1.5) | 1.6 (1.3 to 1.8) |
| Saudi Arabia | 1.5 (0.6 to 7.3) | 0.3 (0.2 to 0.9) |
| Syria | — | 3.0 (1.3 to 3.5) |
| Tunisia | 1.3 (0.3 to 2.5) | 0.9 (0.2 to 1.1) |
| Turkey | 1.0 (0.6 to 2.1) | 0.6 (0.3 to 1.0) |
| United Arab Emirates | — | 1.3 (0.5 to 1.6) |
| Yemen | 2.2 (1.1 to 3.5) | 0.8 (0.5 to 0.9) |
| North America, high income | 1.0 (1.0 to 1.9) | 0.9 (0.7 to 1.1) |
| Canada | 1.1 (0.6 to 1.3) | 0.6 (0.4 to 0.7) |
| United States | 1.3 (1.2 to 2.4) | 0.9 (0.7 to 1.2) |
| Puerto Rico | 2.3 (1.3 to 4.2) | 1.0 (0.6 to 1.6) |
| Oceania | 0.1 (0.1 to 0.6) | 1.1 (0.8 to 3.7) |
| Samoa | 0.2 (0.2 to 0.9) | 0.1 (0.1 to 0.2) |
| Fiji | — | 0.1 (0.0 to 0.3) |
| Papua New Guinea | — | 1.2 (0.9 to 4.2) |
| Sub-Saharan Africa, Central | 4.2 (2.4 to 9.2) | 2.1 (0.1 to 6.9) |
| Central African Republic | — | 0.3 (0.2 to 0.4) |
| Congo, Democratic Republic of the | 4.3 (3.2 to 13.7) | — |
| Gabon | 11.2 (2.1 to 20.7) | 7.0 (5.1 to 7.3) |
| Sub-Saharan Africa, East | 1.0 (0.6 to 3.1) | 0.5 (0.4 to 0.7) |
| Burundi | — | 1.0 (0.8 to 4.0) |
| Ethiopia | 1.3 (0.7 to 5.8) | 0.6 (0.4 to 0.7) |
| Kenya | — | 0.2 (0.1 to 0.3) |
| Madagascar | 1.2 (0.8 to 1.7) | 0.2 (0.2 to 0.3) |
| Sub-Saharan Africa, Southern | 1.3 (0.8 to 2.5) | 0.7 (0.4 to 0.9) |
| South Africa | 1.7 (1.0 to 2.5) | 0.7 (0.4 to 0.9) |
| Zimbabwe | 1.6 (1.0 to 9.1) | — |
| Sub-Saharan Africa, West | 5.3 (2.9 to 9.1) | 1.3 (1.1 to 1.4) |
| Benin | 3.6 (3.6 to 12.8) | — |
| Burkina Faso | — | 1.3 (1.0 to 1.4) |
| Côte d’Ivoire | 3.3 (0.8 to 12.8) | — |
| Cameroon | 11.6 (4.3 to 29.7) | 0.7 (0.5 to 0.8) |
| Chad | — | 1.1 (0.8 to 1.3) |
| Ghana | — | 1.4 (1.1 to 3.4) |
| Gambia, The | 2.1 (1.4 to 2.9) | 0.8 (0.5 to 1.3) |
| Mauritania | 1.9 (1.1 to 10.7) | — |
| Nigeria | 8.4 (3.9 to 12.8) | 1.4 (1.0 to 1.4) |
Peer Review:
This article has been peer reviewed.
References
- 1.Canadian Liver Foundation. Liver Disease in Canada: A crisis in the making.Markham, Ontario:The Foundation. [Google Scholar]
- 2.Kwong JC,Ratnasingham S,Campitelli MA, et al. The impact of infection on population health: results of the Ontario Burden of Infectious Diseases study. PLoS One.2012;7(9):e44103. 10.1371/journal.pone.0044103.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schanzer DL,Paquette D,Lix LM.Historical trends and projected hospital admissions for chronic hepatitis C infection in Canada: a birth cohort analysis. CMAJ Open.2014;2:E139–44. 10.9778/cmajo.20130087.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Myers RP,Krajden M,Bilodeau M, et al. Burden of disease and cost of chronic hepatitis C infection in Canada. Can J Gastroenterol Hepatol.2014;28:243–50. 10.1155/2014/317623.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myers RP,Liu M,Shaheen AAM.The burden of hepatitis C virus infection is growing: a Canadian population-based study of hospitalizations from 1994 to 2004. Can J Gastroenterol.2008;22:381–7. 10.1155/2008/173153.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krajden M,Kuo M,Zagorski B, et al. Health care costs associated with hepatitis C: a longitudinal cohort study. Can J Gastroenterol.2010;24:717–26. 10.1155/2010/569692.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alavi M,Janjua NZ,Chong M, et al. The contribution of alcohol use disorder to decompensated cirrhosis among people with hepatitis C: An international study.J Hepatol.2018;68:393–401.Medline: [DOI] [PubMed] [Google Scholar]
- 8.Alavi M,Janjua NZ,Chong M, et al. Trends in hepatocellular carcinoma incidence and survival among people with hepatitis C: An international study. J Viral Hepat.2017. (ePub Ahead of Print).Medline: [DOI] [PubMed] [Google Scholar]
- 9.Falade-Nwulia O,Suarez-Cuervo C,Nelson DR, et al. Oral direct-acting agent therapy for hepatitis c virus infection: a systematic review. Ann Intern Med.2017;166:637–48. 10.7326/M16-2575.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organisation.Combating Hepatitis B and C to reach elimination by 2030.Geneva, Switzerland:WHO Press;2016. [Google Scholar]
- 11. World Health Organisation.Global Health Sector Strategy on Viral Hepatitis 2016–2021. Towards ending viral hepatitis.Geneva, Switzerland:WHO Press;2016. [Google Scholar]
- 12. Government of Canada. Message from the Minister of Health—World Hepatitis Day, Ottawa, Ontario: Government of Canada.https://www.canada.ca/en/health-canada/news/2016/07/message-from-the-minister-of-health-world-hepatitis-day.html?=undefined&wbdisable=true. [Google Scholar]
- 13.Janjua NZ,Kuo M,Yu A, et al. The population level cascade of care for hepatitis C in British Columbia, Canada: The BC Hepatitis Testers Cohort (BC-HTC). EBioMedicine.2016;12:189–95. 10.1016/j.ebiom.2016.08.035.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yehia BR,Schranz AJ,Umscheid CA, et al. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLoS One.2014;9(7):e101554. 10.1371/journal.pone.0101554.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Greenaway C,Thu Ma A,Kloda LA, et al. The seroprevalence of hepatitis C antibodies in immigrants and refugees from intermediate and high endemic countries: a systematic review and meta-analysis. PLoS One.2015;10(11):e0141715. 10.1371/journal.pone.0141715.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trubnikov M,Yan P,Archibald C. Estimated prevalence of Hepatitis C virus infection in Canada, 2011.CCDR.2014;40–19:421–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Greenaway C,Azoulay L,Allard R, et al. A population-based study of chronic hepatitis C in immigrants and non-immigrants in Quebec, Canada. BMC Infect Dis.2017;17(1):140. 10.1186/s12879-017-2242-y.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenaway C,Azoulay L,Akaberi A, et al.Liver related complications and all cause deaths in immigrants and non-immigrants with chronic hepatitis C infection: a population based study in Quebec, Paper presented at15th International Society for Travel Medicine Conference; 2017 May 15–18; Barcelona, Spain. [Google Scholar]
- 19.Chen W,Tomlinson G,Krahn M, et al. Immigrant patients with chronic hepatitis C and advanced fibrosis have a higher risk of hepatocellular carcinoma. J Viral Hepat.2012;19:574–80. 10.1111/j.1365-2893.2012.01583.x.Medline: [DOI] [PubMed] [Google Scholar]
- 20.Nguyen LH,Nguyen MH.Systematic review: Asian patients with chronic hepatitis C infection. Aliment Pharmacol Ther.2013;37(10):921–36. 10.1111/apt.12300.Medline: [DOI] [PubMed] [Google Scholar]
- 21.Kamstra R,Azoulay L,Steele R, et al. Hospitalizations in immigrants and nonimmigrants diagnosed with chronic hepatitis C infection in Quebec. Clin Infect Dis.2016;63:1439–48. 10.1093/cid/ciw540.Medline: [DOI] [PubMed] [Google Scholar]
- 22.Ng E,Myers RP,Manuel D, et al. Hospital stays for hepatitis B or C virus infection or primary liver cancer among immigrants: a census-linked population-based cohort study. CMAJ Open.2016;4(2):E162–8. 10.9778/cmajo.20150117.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper CL,Thavorn K,Damian E, et al. Hepatitis C virus infection outcomes among immigrants to Canada: a retrospective cohort analysis. Ann Hepatol.2017;16:720–6. 10.5604/01.3001.0010.2714.Medline: [DOI] [PubMed] [Google Scholar]
- 24. Statistics Canada. Immigration and ethnocultural diversity: key results from the 2016 Census.2017. http://www.statcan.gc.ca/daily-quotidien/171025/dq171025b-eng.htm(December 15, 2017).
- 25. World Health Organization.Global hepatitis report.Geneva, Switzerland:World Health Organization;2017. [Google Scholar]
- 26.Pépin J,Abou Chakra CN,Pépin E, et al. Evolution of the global burden of viral infections from unsafe medical injections, 2000-2010. PLoS One.2014;9(6):e99677. 10.1371/journal.pone.0099677.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.El-Ghitany EM,Abdel Wahab MM,Abd El-Wahab EW, et al. A comprehensive hepatitis C virus risk factors meta-analysis (1989-2013): do they differ in Egypt? Liver Int.2015;35:489–501. 10.1111/liv.12617.Medline: [DOI] [PubMed] [Google Scholar]
- 28.Janjua NZ,Butt ZA,Mahmood B, et al. Towards safe injection practices for prevention of hepatitis C transmission in South Asia: Challenges and progress. World J Gastroenterol.2016;22:5837–52. 10.3748/wjg.v22.i25.5837.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams IT,Bell BP,Kuhnert W, et al. Incidence and transmission patterns of acute hepatitis C in the United States, 1982-2006. Arch Intern Med.2011;171:242–8. 10.1001/archinternmed.2010.511.Medline: [DOI] [PubMed] [Google Scholar]
- 30.Cornberg M,Razavi HA,Alberti A, et al. A systematic review of hepatitis C virus epidemiology in Europe, Canada and Israel. Liver Int.2011;31(suppl 2):30–60. 10.1111/j.1478-3231.2011.02539.x.Medline: [DOI] [PubMed] [Google Scholar]
- 31.Blach S,Zeuzem S,Manns M,et al.;Polaris Observatory HCV Collaborators.Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol.2017;2:161–76. 10.1016/S2468-1253(16)30181-9.Medline: [DOI] [PubMed] [Google Scholar]
- 32. World Health Organization.Global hepatitis report.Geneva, Switzerland:WHO Press;2017. [Google Scholar]
- 33. World Health Organization.Guidelines on Hepatitis B and C testing.Geneva, Switzerland:WHO Press;2017. [Google Scholar]
- 34.Gower E,Estes C,Blach S, et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol.2014;61(1 suppl):S45–57. 10.1016/j.jhep.2014.07.027.Medline: [DOI] [PubMed] [Google Scholar]
- 35.Frank C,Mohamed MK,Strickland GT, et al. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet.2000;355:887–91. 10.1016/S0140-6736(99)06527-7.Medline: [DOI] [PubMed] [Google Scholar]
- 36.Sievert W,Altraif I,Razavi HA, et al. A systematic review of hepatitis C virus epidemiology in Asia, Australia and Egypt. Liver Int.2011;31(suppl 2):61–80. 10.1111/j.1478-3231.2011.02540.x.Medline: [DOI] [PubMed] [Google Scholar]
- 37. Government of Canada. Statistics and open data.2015.https://www.canada.ca/en/immigration-refugees-citizenship/corporate/reports-statistics/statistics-open-data.html(December 15, 2017).
- 38.Waheed Y,Safi SZ,Qadri I.Role of potash alum in hepatitis C virus transmission at barber’s shop. Virol J.2011;8(1):211. 10.1186/1743-422X-8-211.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Janjua NZ,Nizamy MA.Knowledge and practices of barbers about hepatitis B and C transmission in Rawalpindi and Islamabad. J Pak Med Assoc.2004;54:116–9.Medline: [PubMed] [Google Scholar]
- 40.Rehman A,Ul-Ain Baloch N,Awais M.Practice of cupping (hijama) and the risk of bloodborne infections. Am J Infect Control.2014;42(10):1139. 10.1016/j.ajic.2014.06.031.Medline: [DOI] [PubMed] [Google Scholar]
- 41.Kin KC,Lin B,Chaung KT, et al. Less-established risk factors are common in Asian Americans with hepatitis C virus: a case-controlled study. Dig Dis Sci.2013;58:3342–7. 10.1007/s10620-013-2884-6.Medline: [DOI] [PubMed] [Google Scholar]
- 42.McGowan CE,Fried MW.Barriers to hepatitis C treatment. Liver Int.2012;32(suppl 1):151–6. 10.1111/j.1478-3231.2011.02706.x.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmed S,Shommu NS,Rumana N, et al. Barriers to access of primary healthcare by immigrant populations in Canada: a literature review. J Immigr Minor Health.2016;18:1522–40. 10.1007/s10903-015-0276-z.Medline: [DOI] [PubMed] [Google Scholar]
- 44.Wu Z,Penning MJ,Schimmele CM.Immigrant status and unmet health care needs. Can J Public Health.2005;96:369–73.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simich L,Jackson B. Social determinants of immigrant health in Canada: what makes some immigrants healthy and others not? Health Policy Research Bulletin.2011(17):26–8. [Google Scholar]
- 46.McDermott S,Gupta S,Desmeules M,Kazanjian A,Vissandjée B,Ruddick E, et al. Health services use among immigrants and refugees to Canada. Health Policy Res Bull.2011(17):37–40. [Google Scholar]
- 47.Newbold K.Chronic conditions and the healthy immigrant effect: evidence from Canadian immigrants. J Ethn Migr Stud.2006;32:765–84. 10.1080/13691830600704149. [DOI] [Google Scholar]
- 48.Newbold KB,Danforth J.Health status and Canada’s immigrant population. Soc Sci Med.2003;57:1981–95. 10.1016/S0277-9536(03)00064-9.Medline: [DOI] [PubMed] [Google Scholar]
- 49.Ng E,Wilkins R,Gendron F.Dynamics of immigrants’ health in Canada: evidence from the National Population Health Survey, Statistics Canada.Ottawa:Government of Canada;2005. [Google Scholar]
- 50.Gushulak BD,Pottie K,Hatcher Roberts J,et al.;Canadian Collaboration for Immigrant and Refugee Health.Migration and health in Canada: health in the global village. CMAJ.2011;183(12):E952–8. 10.1503/cmaj.090287.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Caruana SR,Kelly HA,De Silva SL, et al. Knowledge about hepatitis and previous exposure to hepatitis viruses in immigrants and refugees from the Mekong Region. Aust N Z J Public Health.2005;29(1):64–8. 10.1111/j.1467-842X.2005.tb00751.x.Medline: [DOI] [PubMed] [Google Scholar]
- 52.O’Connor CC,Shaw M,Wen LM, et al. Low knowledge and high infection rates of hepatitis in Vietnamese men in Sydney. Sex Health.2008;5:299–302. 10.1071/SH07084.Medline: [DOI] [PubMed] [Google Scholar]
- 53.Rissel C.The development and application of a scale of acculturation. Aust N Z J Public Health.1997;21:606–13. 10.1111/j.1467-842X.1997.tb01764.x.Medline: [DOI] [PubMed] [Google Scholar]
- 54.Juckett G.Cross-cultural medicine. Am Fam Physician.2005;72:2267–74.Medline: [PubMed] [Google Scholar]
- 55.Abarca Tomás B,Pell C,Bueno Cavanillas A, et al. Tuberculosis in migrant populations. A systematic review of the qualitative literature. PLoS One.2013;8(12):e82440. 10.1371/journal.pone.0082440.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pottie K,Greenaway C,Feightner J, et al. Evidence-based clinical guidelines for immigrants and refugees. CMAJ.2011;183(12):E824–925. 10.1503/cmaj.090313.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McGowan CE,Monis A,Bacon BR, et al. A global view of hepatitis C: physician knowledge, opinions, and perceived barriers to care. Hepatology.2013;57:1325–32. 10.1002/hep.26246.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Trooskin SB,Navarro VJ,Winn RJ, et al. Hepatitis C risk assessment, testing and referral for treatment in urban primary care: role of race and ethnicity. World J Gastroenterol.2007;13:1074–8. 10.3748/wjg.v13.i7.1074.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Butt AA,Justice AC,Skanderson M, et al. Rate and predictors of treatment prescription for hepatitis C. Gut.2007;56:385–9. 10.1136/gut.2006.099150.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dev A,Sievert W.A survey of Australian general practice management of hepatitis C-infected patients from non-English-speaking backgrounds. J Gastroenterol Hepatol.2002;17:295–300. 10.1046/j.1440-1746.2002.02701.x.Medline: [DOI] [PubMed] [Google Scholar]
- 61.Karliner LS,Jacobs EA,Chen AH, et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res.2007;42:727–54. 10.1111/j.1475-6773.2006.00629.x.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Flores G.The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev.2005;62:255–99. 10.1177/1077558705275416.Medline: [DOI] [PubMed] [Google Scholar]
- 63.Jacobs EA,Sadowski LS,Rathouz PJ.The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J Gen Intern Med.2007;22(suppl 2):306–11. 10.1007/s11606-007-0357-3.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Government of Canada. Panel members handbook. Immigration medical examination instructions.2013.https://www.canada.ca/en/immigration-refugees-citizenship/corporate/partners-service-providers/panel-physicians.html(December 16, 2018).
- 65.Grad R,Thombs BD,Tonelli M,et al.;Canadian Task Force on Preventive Health Care.Recommendations on hepatitis C screening for adults. CMAJ.2017;189(16):E594–604. 10.1503/cmaj.161521.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pottie K,Greenaway C,Feightner J,Welch V, et al. Evidence-based clinical guidelines for immigrants and refugees.CMAJ.2011;183(12):E861–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jacobs EA,Shepard DS,Suaya JA, et al. Overcoming language barriers in health care: costs and benefits of interpreter services. Am J Public Health.2004;94:866–9. 10.2105/AJPH.94.5.866.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Karliner LS,Pérez-Stable EJ,Gregorich SE.Convenient access to professional interpreters in the hospital decreases readmission rates and estimated hospital expenditures for patients with limited English proficiency. Med Care.2017;55:199–206. 10.1097/MLR.0000000000000643.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Saeed S,Strumpf EC,Moodie EE,et al.;Canadian Co-Infection Cohort Study.Disparities in direct acting antivirals uptake in HIV-hepatitis C co-infected populations in Canada. J Int AIDS Soc.2017;20(3):e25013. 10.1002/jia2.25013.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marshall AD,Saeed S,Barrett L,et al.;Canadian Network on Hepatitis C (CanHepC).Restrictions for reimbursement of direct-acting antiviral treatment for hepatitis C virus infection in Canada: a descriptive study. CMAJ Open.2016;4(4):E605–14. 10.9778/cmajo.20160008.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. PDCI Market Access Inc. The pan-Canadian Pharmaceutical Alliance (pCPA): negotiations status update.2017.http://www.pdci.ca/the-pan-canadian-pharmaceutical-alliance-pcpa-negotiations-status-update-5/(September 2, 2017).
- 72.Fernandez M,Manzanares S,Jacques C,et al. Screening for chronic viral hepatitis in migrant populations—Report on four HEPscreen pilot studies screening for chronic viral hepatitis in migrant populations. Rotterdam: HEPscreen;2014. [Google Scholar]
- 73.Jafferbhoy H,Miller MH,McIntyre P,Dillon JF.The effectiveness of outreach testing for hepatitis C in an immigrant Pakistani population. Epidemiol Infect.2012;140:1048–53. 10.1017/S095026881100152X.Medline: [DOI] [PubMed] [Google Scholar]
- 74.Perumalswami PV,DeWolfe Miller F,Orabee H, et al. Hepatitis C screening beyond CDC guidelines in an Egyptian immigrant community. Liver Int.2014;34(2):253–8. 10.1111/liv.12259.Medline: [DOI] [PubMed] [Google Scholar]
- 75.Perumalswami PV,Factor SH,Kapelusznik L, et al. Hepatitis Outreach Network: a practical strategy for hepatitis screening with linkage to care in foreign-born communities. J Hepatol.2013;58:890–7. 10.1016/j.jhep.2013.01.004.Medline: [DOI] [PubMed] [Google Scholar]
- 76.Zuure FR,Bouman J,Martens M, et al. Screening for hepatitis B and C in first-generation Egyptian migrants living in the Netherlands. Liver Int.2013;33:727–38. 10.1111/liv.12131.Medline: [DOI] [PubMed] [Google Scholar]
- 77.Bottero J,Boyd A,Gozlan J, et al. Simultaneous human immunodeficiency virus-hepatitis B-hepatitis C point-of-care tests improve outcomes in linkage-to-care: results of a randomized control trial in persons without healthcare coverage. Open Forum Infect Dis.2015;2(4):ofv162. 10.1093/ofid/ofv162.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Giordano C,Druyts EF,Garber G, et al. Evaluation of immigration status, race and language barriers on chronic hepatitis C virus infection management and treatment outcomes. Eur J Gastroenterol Hepatol.2009;21:963–8. 10.1097/MEG.0b013e328326f598.Medline: [DOI] [PubMed] [Google Scholar]
- 79.Linde AC,Sweet KA,Nelson K, et al. Impact of the Hepatitis Testing and Linkage to Care (HepTLC) initiative on linkage to care for Minnesota refugees with hepatitis B, 2012-2014. Public Health Rep.2016;131(suppl 2):112–8. 10.1177/00333549161310S217.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dang JH,Chen MS Jr.Increasing hepatitis B testing and linkage to care of foreign-born Asians, Sacramento, California, 2012-2013. Public Health Rep.2016;131(suppl 2):119–24. 10.1177/00333549161310S218.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. CATIE. Hepatitis C Ethnocultural Education, Outreach and Social Marketing Program.2015.http://www.catie.ca/en/pc/program/ethno(December 18, 2017).
- 82. BC Centre for Disease Control. Hepatitis C testing guide: quick reference guide for health care providers. Vancouver: The Centre;2017. [Google Scholar]
- 83.Arora S,Kalishman S,Thornton K, et al. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care. Hepatology.2010;52:1124–33. 10.1002/hep.23802.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhou K,Fitzpatrick T,Walsh N, et al. Interventions to optimise the care continuum for chronic viral hepatitis: a systematic review and meta-analyses. Lancet Infect Dis.2016;16:1409–22. 10.1016/S1473-3099(16)30208-0.Medline: [DOI] [PubMed] [Google Scholar]
- 85. Canadian Collaboration for Immigrant and Refugee Health. e-Clinical checklist for new immigrants and refugees.2017.http://ccirhken.ca/ccirh_main/sample-page/page3-2/(December 18, 2017).
- 86. Canadian Pediatrics Society. Caring for kids new to Canada.2013.https://www.kidsnewtocanada.ca/http://ccirhken.ca/ccirh_main/sample-page/page3-2/(December 18, 2017).
- 87. Public Health England. Migrant health guide London, England.2014.https://www.gov.uk/topic/health-protection/migrant-health-guidehttp://ccirhken.ca/ccirh_main/sample-page/page3-2/(December 18, 2017).
- 88.Walji M,Flegel K.Healthy interpretation. CMAJ.2017;189(41):E1273. 10.1503/cmaj.171117.Medline: [DOI] [PMC free article] [PubMed] [Google Scholar]


