Abstract
Background
The SARS-CoV-2 pandemic is still ongoing and a major challenge for health care services worldwide. In the first WSES COVID-19 emergency surgery survey, a strong negative impact on emergency surgery (ES) had been described already early in the pandemic situation. However, the knowledge is limited about current effects of the pandemic on patient flow through emergency rooms, daily routine and decision making in ES as well as their changes over time during the last two pandemic years. This second WSES COVID-19 emergency surgery survey investigates the impact of the SARS-CoV-2 pandemic on ES during the course of the pandemic.
Methods
A web survey had been distributed to medical specialists in ES during a four-week period from January 2022, investigating the impact of the pandemic on patients and septic diseases both requiring ES, structural problems due to the pandemic and time-to-intervention in ES routine.
Results
367 collaborators from 59 countries responded to the survey. The majority indicated that the pandemic still significantly impacts on treatment and outcome of surgical emergency patients (83.1% and 78.5%, respectively). As reasons, the collaborators reported decreased case load in ES (44.7%), but patients presenting with more prolonged and severe diseases, especially concerning perforated appendicitis (62.1%) and diverticulitis (57.5%). Otherwise, approximately 50% of the participants still observe a delay in time-to-intervention in ES compared with the situation before the pandemic. Relevant causes leading to enlarged time-to-intervention in ES during the pandemic are persistent problems with in-hospital logistics, lacks in medical staff as well as operating room and intensive care capacities during the pandemic. This leads not only to the need for triage or transferring of ES patients to other hospitals, reported by 64.0% and 48.8% of the collaborators, respectively, but also to paradigm shifts in treatment modalities to non-operative approaches reported by 67.3% of the participants, especially in uncomplicated appendicitis, cholecystitis and multiple-recurrent diverticulitis.
Conclusions
The SARS-CoV-2 pandemic still significantly impacts on care and outcome of patients in ES. Well-known problems with in-hospital logistics are not sufficiently resolved by now; however, medical staff shortages and reduced capacities have been dramatically aggravated over last two pandemic years.
Keywords: COVID-19, SARS-CoV-2, Pandemic, Emergency surgery, Emergency, Appendicitis, WSES, Time to intervention, Capacity, Quarantine
Background
Since the World Health Organization has declared SARS-CoV-2 as a worldwide pandemic in early 2020, it dominates daily life and influences political decisions as well as daily therapeutic practices in various medical disciplines. Global or local lockdown policies and recommendations regarding postponement of elective therapies during the last two pandemic years aim at providing necessary health care capacities especially during wave-like outbreaks of different variants of SARS-CoV-2. Therefore, the discussion behind postponements of elective surgical therapies is primarily to hold up bed, intensive care as well as operating room capacities available during the pandemic and secondarily to preserve patients and medical staff from nosocomial infection with SARS-CoV-2 [1–4]. However, postponement of elective surgical therapies might not be detrimental in the short-term follow-up upon diagnosis, but delayed treatments might have some harmful effects beyond that short range in the longer-term outcome [2]. This it is quite clear for surgical oncology, because delays in cancer-specific therapy might result in severely impaired oncologic outcome [2, 5–7].Even patient outcome is impaired through postponements of elective surgical therapy of other non-malignant diseases during the pandemic [8]. The situation is dramatically different in emergency patients. Postponement of urgent therapies is not allowed in the emergency setting and can rapidly result in detrimental outcome [9, 10]. However, local hospital management for maintaining an adequate emergency surgical service during wave-like SARS-CoV-2 outbreaks with high incidences of severely-ill COVID-19 patients and limited intensive care capacities is challenging. Policies, health care providers and hospital management have to balance the necessity of strong SARS-CoV-2 measures on the one hand and the maintenance of surgical emergency services on the other hand, which both compete with critical hospital resources including normal ward, intensive care and operating room capacities as well as personnel required for an adequate therapy and additional expenses for quarantine measures.
Since the rapid spread of the SARS-CoV-2 around the world in late 2019, a high amount of research had been published regarding the pandemic, the characteristics of the virus and treatment modalities of COVID-19, which are urgently needed [4]. However, the literature reveals some evidence about dramatic negative effects of the pandemic on various medical fields and health care services, e.g., in oncology, cardiovascular diseases, etc., as well as on the outcome of respective patients [5, 11–14]. By now, this list is endless and the SARS-CoV-2 pandemic has obviously a negative impact on emergency surgery worldwide: Although case load decreases, patients present with more severe and prolonged surgical emergencies, and thus, treatment is more complex and surgery is more complicated during the pandemic [3, 15, 16].
As a consequence, these pandemic-driven factors uncertainly influence not only the entire spectrum of elective patient care, but also have a significant effect on daily routine patient care in emergency rooms and particularly in emergency surgery. However, the knowledge is limited about the impact of the pandemic on patient flow through emergency rooms, clinical daily routine and clinical decision making in emergency surgery as well as their changes over time during the last two years of the pandemic. In our first WSES COVID-19 emergency surgery survey from June 2020, we have described a strong impact of the pandemic on emergency surgery services worldwide due to potential harmful delays in time-to-diagnosis (TTD) and time-to-intervention (TTI), and the need of triage of emergency surgical patients [3]. Data analysis revealed that structural problems like in-hospital logistics were predominantly responsible for negative effects of SARS-CoV-2 on emergency surgical patient care [3]. This new second WSES COVID-19 emergency surgery survey investigates the impact of the SARS-CoV-2 pandemic on patients and their diseases requiring emergency surgery, on TTD and TTI in emergency departments as well as relevant causes for a delayed surgical therapy during the course of the pandemic. Two years after the initial survey structural rearrangement, new in-hospital standard operating procedures and integration of SARS-CoV-2 into the everyday clinicians’ work should have led to an improvement of emergency care. If the initial problems persist, this must lead to a radical and immediate improvement of surgical emergency care worldwide.
Methods
An online survey was designed by a core group of investigators of the study group. Google Forms (Google LLC, Mountain View, California, USA) was used as the platform for the survey.
The survey was designed, the survey study was conducted, and the results were analyzed and reported following the CHERRIES statement [17].
The survey consists of multiple-choice and single-choice items as well as open-answer questions. In the style of the first WSES COVID-19 emergency surgery survey study from June 2020, published in December 2020 [3], the items of the present questionnaire are organized in five sections: (1) recording the characteristics of collaborators and their affiliated hospitals, (2) evaluating the experiences of the study group with emergency surgery in COVID-19-infected patients, (3) investigating the ongoing impact of SARS-CoV-2 pandemic on patients requiring emergency surgery as well as (4) ongoing structural problems caused by the pandemic and leading to substantial barriers across emergency surgical pathways and quality loss in emergency patient treatment. Furthermore, (5) individual experiences with septic diseases potentially requiring intensive care, interventional emergency therapy and/or emergency surgery as well as (6) potential paradigm shifts from a standard operative therapy before the pandemic situation to a non-operative (conservative) treatment approach during the pandemic and (7) preventive, quarantine and SARS-CoV-2 testing strategies are part of the survey.
After the survey was approved by the World Society of Emergency Surgery (WSES) project steering committee, this cross-sectional survey study was distributed on January 17, 2022, to the global mailing list of WSES members and beyond, as addressees were invited to distribute the survey to their colleagues. The survey was closed after four weeks on February 11, 2022.
After closing the survey, the results were checked for duplicates. Results are presented descriptively within the present manuscript.
Results of items, that were comparable with our previous WSES COVID-19 emergency surgery survey study from June 2020 [3], were conducted to statistical analyses, which allowed us to investigate changes in responses over time during the pandemic situation. Statistical analyses were performed using GraphPad Prism (Version 9 for Windows, GraphPad Software, San Diego, CA, USA, www.graphpad.com). For descriptive statistics, categorical data were analyzed using Fishers exact test or Pearson’s X2 test. p values ≤ 0.05 were considered to indicate statistical significance. Because of the exploratory character of the study, no adjustments of p values were performed.
Data are given as n collaborators and/or percentages of the collaborators.
Results
Characteristics of participants and their affiliated hospitals
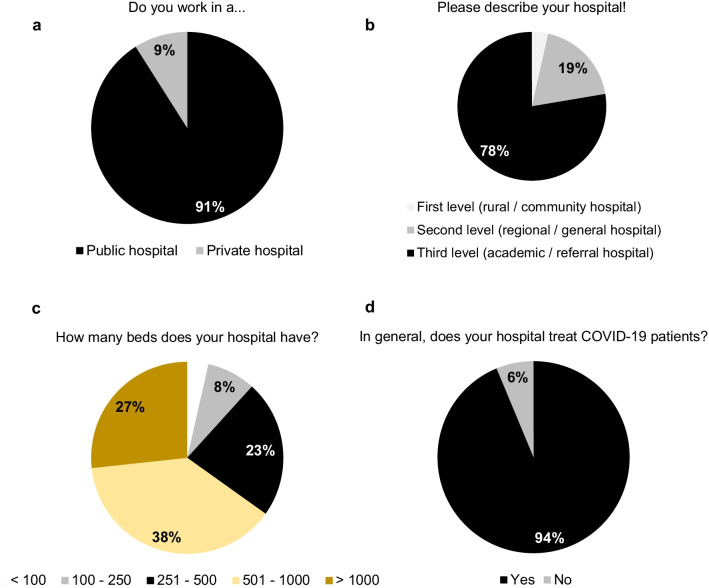
367 health care specialists in emergency medicine and emergency surgical patient care from 59 countries around the world, i.e., 5 continents, completed the survey study (Fig. 1). Most participants work in a larger public, third-level (academic/referral) hospital with more than 500 beds (Fig. 2) which includes a dedicated emergency department (96.2% of the cases) and more precisely a dedicated acute care surgery or emergency surgery unit at the own hospital (71.9% of the cases). With 86.9% and 15%, most collaborators came from general/abdominal surgery and trauma surgery/orthopedics, respectively, but representatives of other medical disciplines, which are involved in emergency surgical patient care, were also represented in the study cohort including internal medicine, anesthesiology, vascular surgery, thoracic surgery and gynecology (all < 5%). Therefore, most of the collaborators are well-experienced personnel with being senior consultants and heads of the departments in 48.0% and 19.3%, respectively, or at least board-certified staff in 18.3% (Fig. 1).
Fig. 1.
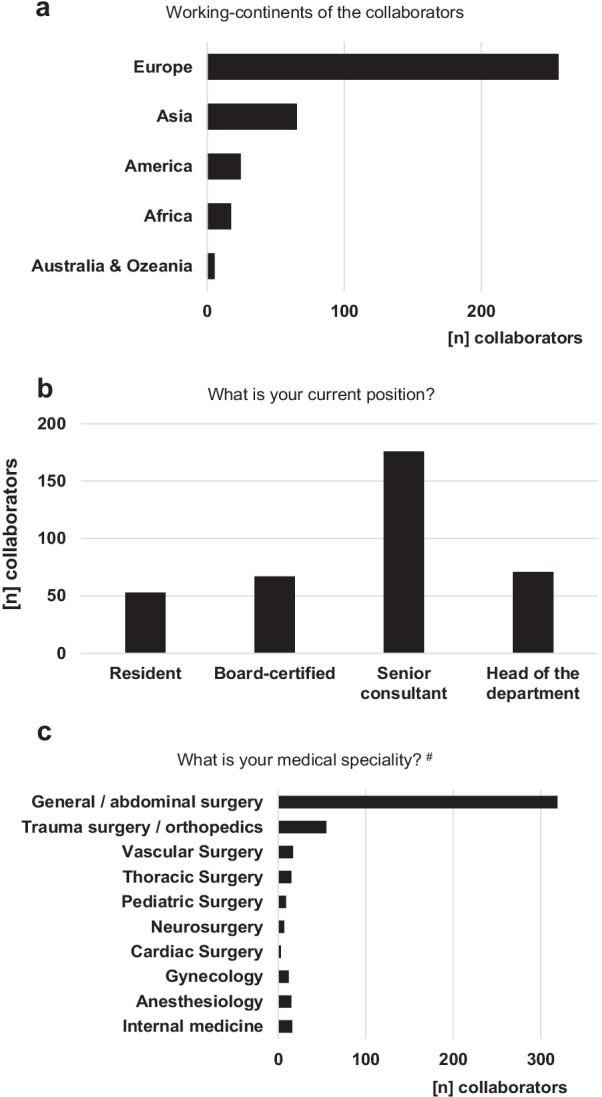
Characteristics of the collaborators. Working continents of the WSES COVID-19 emergency surgery survey collaboration group (a). Experience and position (b) as well as medical speciality (c) of the collaborators. #multiple answers possible
Fig. 2.
Hospital characteristics of the collaboration group. Volume and academic affiliation (a–c) of the hospitals as well as reported treatment capacities of COVID-19 patients (d)
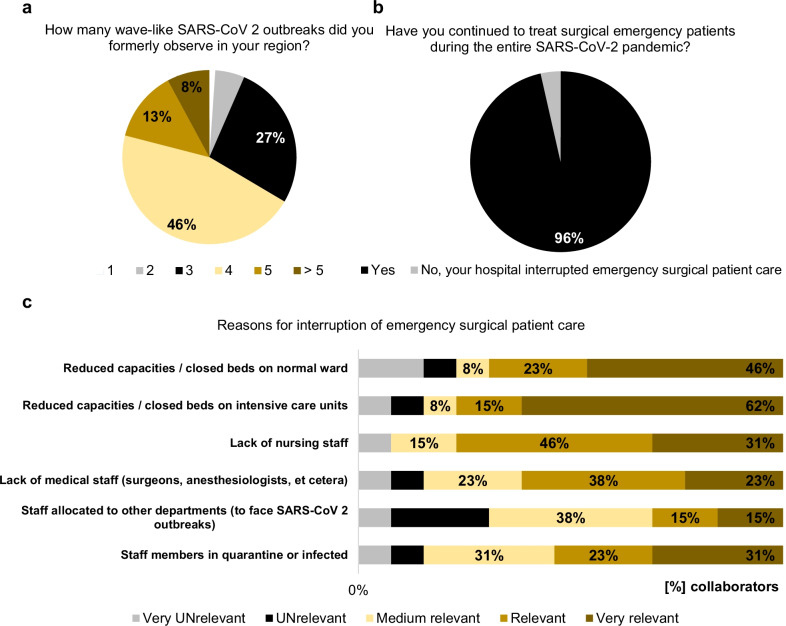
93.5% of the participants stated that they formally experienced three or more SARS-CoV-2 outbreaks in their region since the beginning of the pandemic situation in early 2020 (Fig. 3) and almost all collaborators (94%) stated that their region currently (from October 2021 to February 2022) suffers from a wave-like SARS-CoV-2 outbreak. In general, COVID-19 patients are treated in hospitals of 93.7% of the collaborators (Fig. 2) and almost all of the collaborators (88%) had performed emergency surgery in patients, acutely infected with SARS-CoV-2, which represents a significant increase over time compared with the situation in June 2020 (versus 62.2%, p < 0.0001 [3]). Interestingly, in hospitals of 13 participants (3.5%) emergency surgical patient care was interrupted due to the pandemic. Relevant or very relevant reasons for a discontinuous emergency surgery service among these participants were: reduced capacities on normal ward (69.2%) and intensive care units (76.9%), lack of nursing (76.9%) and medical staff (61.5%) as well as staff members being in quarantine or infected (53.8%, Fig. 3).
Fig. 3.
SARS-CoV-2 outbreaks and emergency surgery. Interruption of surgical emergency patient care in response to SARS-CoV-2 outbreaks (a, b) as well as reasons for interruption of surgical emergency patient care during the pandemic (c)
Ongoing impact of the pandemic on capacities and quality indicators of emergency surgery
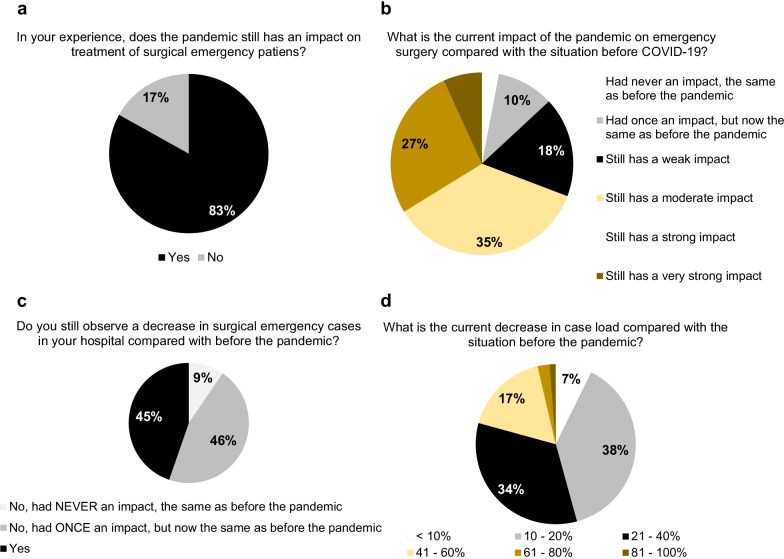
In the previous WSES COVID-19 emergency surgery survey in June 2020, we reported that the SARS-CoV-2 pandemic negatively influences the treatment of surgical emergency patients strongly [3]. Therefore, 83.1% of the collaborators indicated now that the pandemic still has an impact on treatment of surgical emergency patients and estimated this impact as being strong or very strong in 33.8% of the cases (Fig. 4). Interestingly, 18 of the 23 participants, from hospitals, which are not involved in care of SARS-CoV-2 positive patients, also observe these negative effects. However, the negative impact of the SARS-CoV-2 pandemic on emergency surgical services due to the pandemic was fortunately reduced over time compared with answers from the first WSES COVID-19 emergency surgery survey in June 2020, where almost 65.5% of the participants estimated it as being strong or very strong (p < 0.0001 [3]). Overall 44.7% of the participants still observe a decrease in emergency surgical cases in their hospitals compared with the situation before the pandemic (versus 86.2% of the collaborators from the previous WSES COVID-19 emergency surgery survey in June 2020, p < 0.0001 [3]). However, 74.1% of the participants reported this effect being mostly obvious during local lockdown policies.
Fig. 4.
The impact of the pandemic situation on emergency surgery. The estimated “global” impact of the pandemic on emergency surgery (a, b) and the effect of the pandemic situation on emergency surgical case load (c, d)
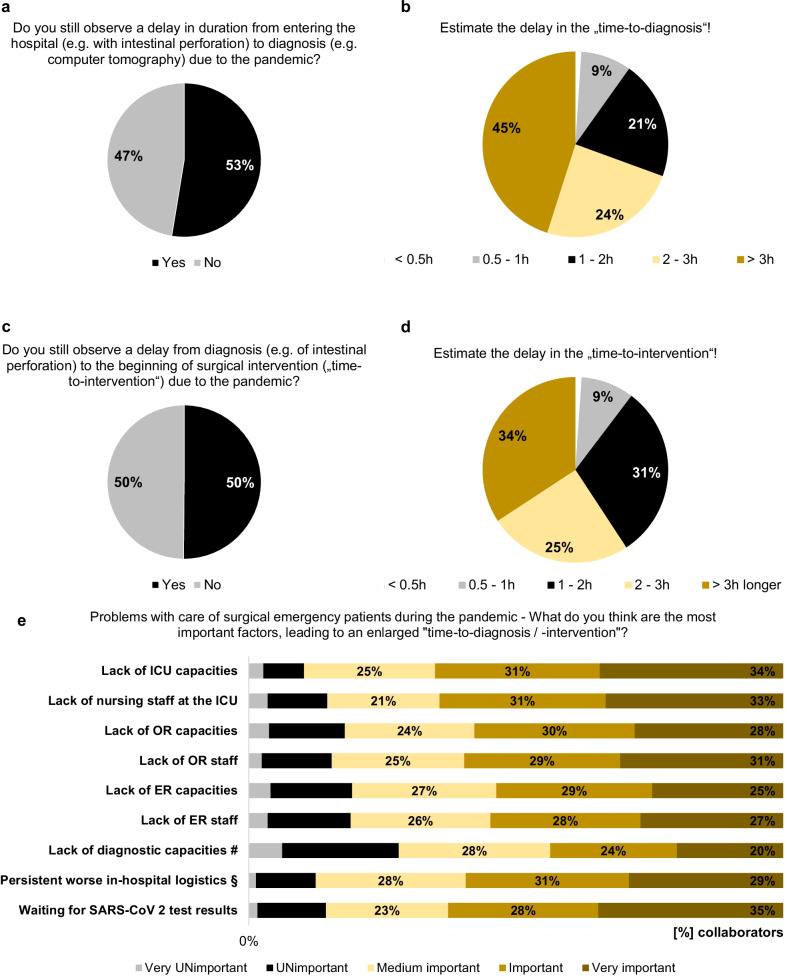
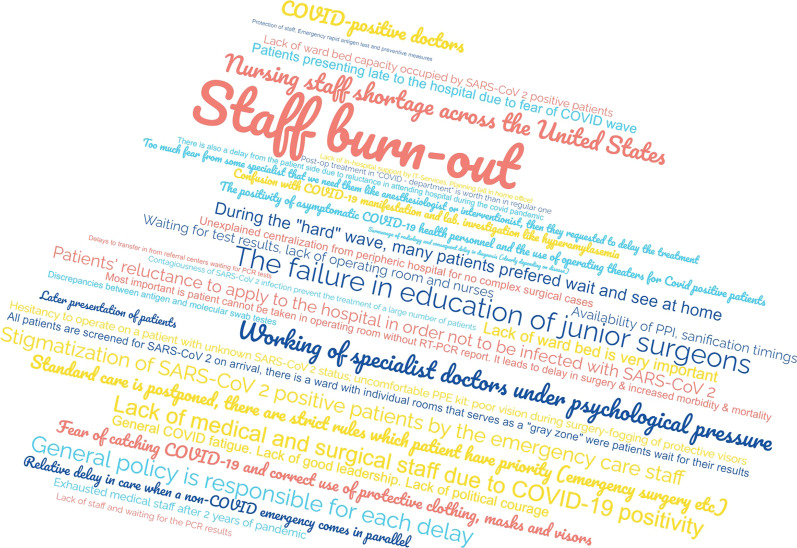
Important quality indicators for emergency patient care are TTD and TTI. In the current survey, 52.6% and 50.1% of the participants still observe a delay in TTD and consecutively in TTI, respectively, due to the pandemic, which was comparable with the situation in June 2020 (p = 0.0734 and p = 0.2331 [3]). Even no obvious differences were seen in the estimated delays in TTD (p = 0.3763 [3]) and TTI (p = 0.0582 [3]) over time during the SARS-CoV-2 pandemic. To evaluate relevant factors being critical in the therapy of surgical emergency patients and why the SARS-CoV-2 pandemic might have an ongoing impact on emergency room and emergency surgical pathways, the collaborators of the study were asked for the most important factors that still lead to an enlarged TTD and TTI as well as problems with capacities concerning emergency surgery during the pandemic situation. The answers are summarized in Figs. 5e and 6. Interestingly, we did not observe improvements in in-hospital logistics, e.g., for transport of emergency patients or separated pathways for SARS-CoV-2-infected patients, reported over time from the previous WSES COVID-19 emergency surgery survey in June 2020 until now (p = 1 [3]), which is until now one of the most important problems for delays in TTD and TTI. Vice versa, significantly more collaborators currently report a dramatic lack in medical staff, especially in the operating room, leading to both unavailable operating room and intensive care unit capacities (all of them p < 0.0001 in comparison with the responses from the first WSES COVID-19 emergency surgery survey in June 2020 [3]), indicating that staff shortages and reduced capacities, relevant for emergency surgery, are dramatically aggravated during the course of the SARS-CoV-2 pandemic over the last two years. These problems with limited local capacities continuously result in a relevant need of triage or transferring surgical emergency patients to other hospitals for further therapy, reported by 64% and 48.8% of the collaborators, respectively. Figure 6 reports free-text answers from the collaborators collecting further factors, which lead to problems with surgical emergency patient care during the pandemic.
Fig. 5.
Delays in surgical emergency patient care. Do the collaborators still observe delays in time-to-diagnosis (a, b) and time-to-intervention (c, d) in emergency surgery and the reasons behind these observations (e). #Lack of diagnostic capacities (e.g., computed tomography, endoscopy, etc.). §Persistent worse in-hospital logistics (e.g., transport of patients, closed normal wards, etc.)
Fig. 6.
Factors leading to problems with surgical emergency patient care during the pandemic. Free-text answers in a word cloud from the collaborators collecting relevant factors, which lead to problems with surgical emergency patient care during the pandemic
Ongoing impact of SARS-CoV-2 pandemic on diseases requiring critical care, emergency therapy, emergency surgery
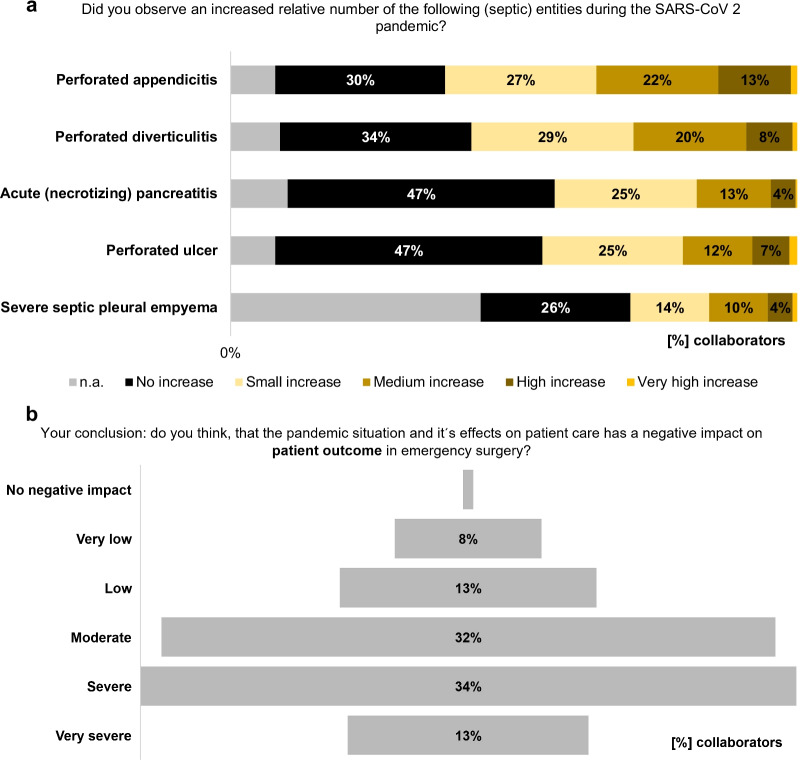
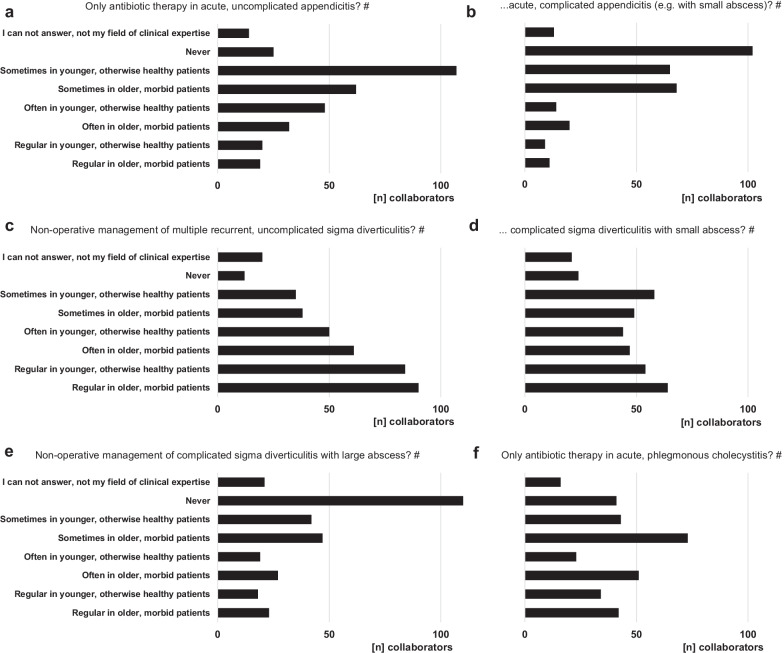
The collaborators of the current WSES COVID-19 emergency surgery survey observed an ongoing medium, high or very high increase in relative numbers of severe (septic) abdomino-thoracic diseases, especially of perforated appendicitis and diverticulitis, during the pandemic in comparison with the situation before (Fig. 7a); however, this was comparable with the estimation of the participants from June 2020 (perforated appendicitis: p = 0.5586 and perforated diverticulitis: p = 1328 [3]). Contrastingly, two-thirds of the collaborators (67.3%) reported their experience that the pandemic situation (with reduced capacities, higher perioperative risk, etc.) led to a paradigm shift in the treatment of more uncomplicated infectious diseases to a non-operative approach. These findings are underlined by the reports upon the questions, which non-operative treatment options the participants recommend to their patients during the ongoing pandemic situation. This was mostly obvious for acute, uncomplicated infectious diseases including appendicitis and diverticulitis, but also more complicated diseases were considered to more conservative treatment modalities during the pandemic by a remarkable proportion of participants. Therefore, patient characteristics play an important role in these treatment considerations (Fig. 8).
Fig. 7.
The effect of the pandemic on patient outcome. The impact of the SARS-CoV-2 pandemic on diseases requiring emergency surgery (a) and on outcome of surgical emergency patients (b)
Fig. 8.
Paradigm shift in treatment modalities. Shift of treatment modalities due to the pandemic from a frequently intended surgical therapy before to a non-operative approach during the pandemic situation in patients with appendicitis (a, b), diverticulitis (c–e) and cholecystitis (f). #multiple answers possible
In a conclusion, most of the collaborators think that the pandemic situation and its effects on emergency surgical patient care have a moderate (31.9%), severe (34.1%) or very severe (12.5%) negative impact on emergency surgical patient outcome. Only 13.4%, 7.6% and 0.5% of the participants think that this negative impact on patient outcome in the surgical emergency setting due to pandemic-driven changes is low, very low or zero, respectively (Fig. 7b). Interestingly, all participants, from hospitals, which are not involved in care of SARS-CoV-2 positive patients (n = 23), also estimated a moderate (n = 12), severe (n = 9) or very severe (n = 2) negative impact on the outcome of emergency surgical patients.
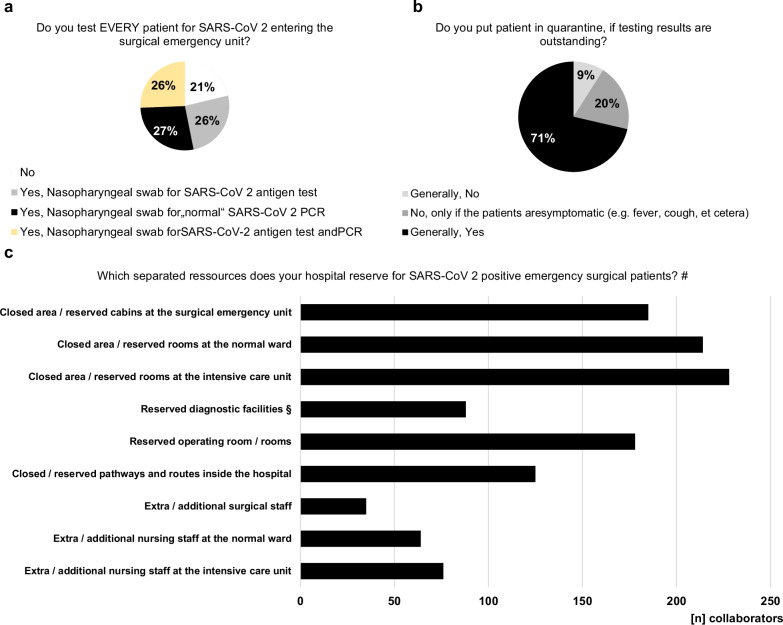
Preventive and testing strategies
In the hospitals of 78.7% of the collaborators, every patient entering the surgical emergency unit undergoes SARS-CoV-2 testing and 71.4% put patients in quarantine generally, if testing results are outstanding (Fig. 9). Therefore, “rapid” SARS-CoV-2-PCR is available at the surgical emergency unit of 76.3% of the participants for urgent results within one hour. 89.4% of the collaborators reported that their hospitals provide separated pathways for SARS-CoV-2 positive patients to minimize contact with uninfected patients. The most commonly used measures are closed areas and reserved rooms at the emergency unit, normal wards and intensive care units as well as reserved operating theatres for SARS-CoV-2 positive patients.
Fig. 9.
Testing and quarantine strategies. Local testing (a) and quarantine strategies (b) varying strongly. (c) Which separated pathways are useful and which resources are provided by hospital management to separate SARS-CoV-2 positive from uninfected patients. #multiple answers possible. §Reserved diagnostic facilities (e.g., computed tomography scanner, ultrasonography, etc.)
Discussion
The SARS-CoV-2 pandemic has still devastating effects on surgical emergency services worldwide. Our initial WSES COVID-19 emergency surgery survey from June 2020 revealed in the very early pandemic phase that there is a strong impact of the pandemic situation on surgical emergency patient care including potential harmful delays in TTD and TTI. This led either to a delayed therapy or the urge of triage of surgical emergency patients in a relevant proportion worldwide [3]. At that early time point, structural problems with in-hospital logistics were mainly responsible for these problems in patient care, whereas medical staff shortages previously did not play a major role contributing to these challenges in emergency surgery [3]. The current cross-sectional survey reflects the situation with emergency surgical patient care presently, approximately 2 years after. By now, the pandemic is still ongoing and various regions of the world suffered from numerous wave-like outbreaks of diverse variants of SARS-CoV-2. However, beyond several heterogeneous strategies to maintain global health care during the pandemic including social lockdown policies, adjusted treatment recommendations and in-hospital quarantine measures, the negative effect of the pandemic situation on surgical emergency patient care and on patient outcome is still significant. These alarming findings are underlined by persistent delays in TTD and TTI for emergency surgical patients during the last two years of the pandemic, which had been reported by approximately 50% of the collaborators. Therefore, it is well known that rapid initiation of diagnostics and therapy especially for patients with septic diseases in emergency surgery and trauma patients is mandatory for good treatment quality [9, 10, 18–20]. Furthermore, the collaborators were asked for relevant reasons causing the significant impact of the pandemic situation on emergency surgery: Persistent problems with in-hospital logistics are still major factors making an adequate surgical emergency treatment impossible. Obviously, these problems could not be resolved during the two-year lasting pandemic situation. Based on the results of the first WSES COVID-19 emergency surgery survey in 2020, we declared critical impairments in the diagnostic and therapeutic work-up of surgical emergency patients as a worldwide issue and postulated that improvements in care of surgical emergency patients like tailored solutions for in-hospital logistics are urgently necessary [3, 21]. Furthermore, we then hypothesized that proactive provision of resources to enhance medical staff, operating room capacities, intensive care capacities from policies, medical societies and local health care providers are mandatory for future patient care during the pandemic [3, 21]. In contrast, the situation in surgical emergency units worldwide is aggravated by dramatic shortages in medical staff, capacities and resources, which consecutively deteriorates the problematic situation with surgical emergency patients during the pandemic. Both the well-known logistic problems paired with the “new” lack of (human) resources summit in an enlarged TTD and TTI in many cases and finally to impaired outcome of our patients by now. Nevertheless, one has to keep in mind that some of these culprits, especially those logistic ones, might be modifiable easily, which might lead to significant improvements in in-hospital emergency patient care.
Another important aspect of the pandemic situation are changes in patient flow into the surgical emergency departments and changes in the disease quality requiring emergency surgery over the last two years. Overall a decreasing case load of emergency surgical patients is reported since the beginning of the pandemic in both WSES COVID-19 emergency surgery surveys [3]. But, an increase in more severe and prolonged diseases, including perforated appendicitis and diverticulitis, requiring more complex surgical or multimodal treatment strategies has been observed. Although it is a subjective estimation from the participants of the present survey, this finding is not entirely novel and had also been described by other authors from larger scaled cross-sectional studies involving patient data in the literature before. Although overall patient numbers are decreasing, especially patients with bowel diseases including appendicitis and diverticulitis present in the emergency rooms with more severe, prolonged and even perforated diseases [3, 8, 15, 16]. Besides that, Tebala et al. showed in their international retrospective cohort audit correlations of hospital admissions with general patient condition and physical health [22]. These changes in patient flow into surgical emergency departments as well as the observation of higher proportion of patients with more severe and prolonged diseases might be an expression of ongoing changes in medical evaluation and decision-making processes and a kind of pandemic-driven fear reactions of patients and referring physicians against SARS-CoV-2 infection [23]. Other issues, indicating changes in medical evaluation and particularly in decision-making processes, are paradigm shifts in the treatment modalities of frequent infectious diseases, which classically require (general) emergency surgery. Particularly in acute appendicitis, multiple recurrent and symptomatic non-complicative diverticulitis and cholecystitis a great proportion of participants would refer on a non-operative management, which—vice versa—was not regularly the case before the pandemic [24]. Additionally, some participants of the survey stated to apply non-operative therapeutic strategies for other severe septic diseases, including primary drainage therapy for perforated peptic ulcer in higher aged and polymorbid patients and prolonged drainage therapy to avoid—if possible—decortication for pleural empyema. If these circumstances will change treatment perceptions and therapeutic standards beyond the special situation during the pandemic remains to be seen in the future, however, emergency surgeons have to be aware that discussions are ongoing regarding more conservative treatment strategies in selected cases especially with appendicitis and diverticulitis.
In contrast, patients with traumatic emergencies frequently do not tolerate treatment postponements or conservative therapy attempts. The estimation of the collaborators, that the pandemic results in impaired outcomes of emergency surgical patients, underlines the essential necessity to maintain adequate and continuous patient care within the emergency setting including sufficient in-hospital and personnel capacities as well as appropriate in-hospital logistics. The latter includes fast SARS-CoV-2 testing (79% of the participants are testing every patient entering the surgical emergency room) and consequent quarantine measures with closed and reserved areas for patients with doubted or confirmed SARS-CoV-2 infection as highly important strategies on the one hand to prevent patients from misdiagnosis and delayed initiation of adequate therapy. On the other hand, these measures are mandatory to prevent patients and medical staff from nosocomial SARS-CoV-2 infection during high-incidence periods, which would worsen shortages in emergency surgical patient care, exhaustion and psychological pressure of personnel dramatically.
Conclusions
In conclusion, the current study demonstrates that the SARS-CoV-2 pandemic still has a significant and global impact on care and outcome of surgical emergency patients. Well-known problems with in-hospital logistics are not sufficiently resolved by now; however, medical staff shortages and reduced capacities have been dramatically aggravated during the pandemic situation over the last two years. Global strategies to maintain adequate emergency surgical patient care are urgently needed from policies and hospital management [21]. These measures are not only mandatory during the ongoing SARS-CoV-2 pandemic and future outbreaks of virus variants but also for prospective disaster management protocols.
Acknowledgements
The authors sincerely thank all collaborators of the study for participation in the survey.
The WSES COVID-19 emergency surgery survey collaboration group (only those who agree are listed as collaborators)
Adam Peckham-Cooper, Leeds Teaching Hospitals NHS Trust, United Kingdom
Adrian Camacho-Ortiz, Hospital Epidemiology and Infectious diseases, Hospital Universitario Dr. José Eleuterio Gonzalez, Monterrey, Mexico
Aikaterini T. Mastoraki, National and Kapodistrian University of Athens, Laikon Hospital, Greece
Aitor Landaluce-Olavarria, Alfredo Espinosa Urduliz Hospital, Spain
Ajay Kumar Pal, King George's Medical University, India
Akira Kuriyama, Kurashiki Central Hospital, Japan
Alain Chichom-Mefire, Faculty of Health Sciences, University of Buea, Cameroon
Alberto Porcu, Università degli Studi di Sassari, Italy
Aleix Martínez-Pérez, Department of General and Digestive Surgery, Hospital Universitario Doctor Peset, Valencia, Spain
Aleksandar R. Karamarkovic, Surgical Clinic "Nikola Spasic" - UCC Zvezdara Belgrade, Faculty of Medicine University of Belgrade, Serbia
Aleksei V. Osipov, Department of urgent surgery, Scientific research institute of emergency medicine, Saint-Petersburg, Russia
Alessandro Coppola, General Surgery, Fondazione Policlinico Universitario Campus Bio-Medico, Italy
Alessandro Cucchetti, Department of Medical and Surgical Sciences - DIMEC; University of Bologna, Italy
Alessandro Spolini, UOC Chirurgia Generale Sondrio ASST Valtellina-Alto Lario, Italy
Alessio Giordano, General Surgery unit, Nuovo Ospedale S. Stefano, Prato, Italy
Alexander Reinisch-Liese, Department of General, Viszeral and Oncologic Surgery, Klinikum Wetzlar,Teaching Hospital of JLU Giessen, Wetzlar, Germany
Alfie J. Kavalakat, Jubilee Mission Medical College & RI, Thrissur, India
Alin Vasilescu, Department of Surgery, St Spiridon University Hospital, “Grigore T Popa” University of Medicine and Pharmacy, Iasi, Romania
Amin Alamin, General surgery department, Ealing Hospital, London North West University Healthcare NHS Trust, United Kingdom
Amit Gupta, Department of Surgery, All India Institute of Medical Sciences Rishikesh, Rishikesh, India
Ana Maria Dascalu, Faculty of Medicine, Carol Davila University of Medicine and Pharmacy Bucharest, Romania
Ana-Maria Musina, University of Medicine and Pharmacy Grigore T. Popa Iasi/ Regional Institute of Oncology Iasi, Romania
Anargyros Bakopoulos, Department of Surgery, Attikon University Hospital, University of Athens, Athens, Greece
Andee Dzulkarnaen Zakaria, Department of Surgery, School of Medical Sciences & Hospital USM, Universiti Sains Malaysia, Malaysia
Andras Vereczkei, Department of Surgery, Medical Center, University of Pécs, Hungary
Andrea Balla, UOC of General and Minimally Invasive Surgery, Hospital “San Paolo”, Largo Donatori del Sangue 1, Civitavecchia, Rome, Italy
Andrea Bottari, Chirurgia dell'Apparato Digerente, Azienda Ospedaliero-Universitaria Careggi, Firenze, Italy
Andreas Baumann, Neurosurgical Department, Cologne Merheim Medical Center, Universitiy of Witten Herdecke, Germany
Andreas Fette, PS_SS, Weissach im Tal, Germany
Andrey Litvin, Immanuel Kant Baltic Federal University, Regional Clinical Hospital, Kaliningrad, Russia
Aniella Katharina Reichert, Department of Gynaecology and Obstetrics, University Hospital of Giessen, Giessen, Germany
Anna Guariniello, Emergency Surgery Ravenna Hospital, Italy
Anna Paspala, Evgenideio Hospital, Athens, Greece
Anne-Sophie Schneck, Centre Hospitalier Universitaire de la Guadeloupe, Guadeloupe
Antonio Brillantino, Emergency Surgery Department, "A. Cardarelli" hospital, via Cardarelli 9, 80131 Naples, Italy
Antonio Pesce, AUSL of Ferrara - University of Ferrara, Italy
Arda Isik, Istanbul medeniyet university, Turkey
Ari Kalevi Leppäniemi, Helsinki University Hospital and University of Helsinki, Finland
Aristeidis Papadopoulos, General Hospital of Nikaia, Greece
Aristotelis Kechagias, Department of General Surgery, Kanta-Häme Central Hospital, Finland
Ashraf yehya abdalla Mohamed, General Surgery Department, Buraimi Hospital, Buraimi, Oman
Ashrarur Rahman Mitul, Bangladesh Shishu Hospital & Institute, Bangladesh
Athanasios Marinis, Third Department of Surgery, Tzaneio General Hospital, Piraeus, Greece
Athanasios Syllaios, Laiko General Hospital, Greece
Baris Mantoglu, Sakarya Medical Faculty, Turkey
Belinda De Simone, Department of Emergency, digestive and metabolic minimally invasive surgery, Poissy and Saint Germain en Laye Hospitals, France
Benjamin Stefan Weiss, Department for Adult and Pediatric Cardiovascular Surgery, University Hospital of Giessen, Giessen, Germany
Bernd Pösentrup, Department of Pediatric Surgery and Pediatric Urology, Children´s Hospital, Klinikum Dortmund, Dortmund, Germany
Biagio Picardi, San Filippo Neri ASL Roma 1, Italy
Biagio Zampogna, Department of Orthopaedic and Trauma Surgery, Campus Bio-Medico University of Rome, Rome, Italy
Boris Eugeniev Sakakushev, Research Institute at Medical University of Plovdiv, Medical University of Plovdiv, Department of Surgical Propedeutics, Section of General Surgery, UMHAT St George Plovdiv, First Clinic of General Surgery, Bulgaria
Boyko Chavdarov Atanasov, Umhat Eurohospital, Medical university of Plovdiv, Bulgaria
Bruno Nardo, Annunziata Hospital, Unversity of Calabria, Italy
Bulent Calik, University of Healthy Sciences Izmir Bozyaka Education and Research Hospital, General Surgery Department, Turkey
Camilla Cremonini, Pisa university hospital, Italy
Carlos A. Ordoñez, Division of Trauma and Acute Care Surgery, Department of Surgery, Fundacion Valle del Lili, Cali, Colombia
Charalampos Seretis, General University Hospital of Patras, Greece
Chiara Cascone, Fondazione Policlinico Campus Bio-Medico di Roma, Italy
Christos Chouliaras, 1st Department of Surgery, General Hospital of Nikaia, Piraeus, Greece
Cino Bendinelli, John Hunter Hospital. Newcastle, NSW, Australia
Claudia Lopes, Hospital Universitario Donostia-Osakidetza, Spain
Claudio Guerci, Ospedale Luigi Sacco, Italy
Clemens Weber, Department of Neurosurgery, Stavanger University Hospital, Norway
Constantinos Nastos, Attikon University Hospital, Greece
Cristian Mesina, Emergency County Hospital of Craiova, Romania
Damiano Caputo, Department of Surgery University Campus Bio-Medico di Roma, Fondazione Policlinico Universitario Campus Bio-Medico, Italy
Damien Massalou, Acute care surgery, University Hospital of Nice, Centre Hospitalier Universitaire de Nice, Nice, France
Davide Cavaliere, Department of Surgery, Forlì Hospital - AUSL della Romagna, Italy
Deborah A McNamara, RCSI University of Medicine and Health Sciences, Ireland
Demetrios Demetriades, USC School of Medicine, Los Angeles, United States
Desirè Pantalone, Department of Experimental and Clinical Medicine University of Florence, University Hospital Careggi, Florence, Italy
Diego Coletta, AO Ospedali Riuniti Marche Nord, Department of General Surgery, Italy
Diego Sasia, General and Oncological Surgery Unit, Santa Croce and Carle Hospital, Cuneo, Italy
Diego Visconti, Chirurgia Generals d´Urgenza e PS, AOU Cittá della Salute e della Scienza, Turin, Italy
Dieter G. Weber, Department of General Surgery, Royal Perth Hospital & The University of Western Australia, Australia
Diletta Corallino, Department of General Surgery and Surgical Specialities „Paride Stefanini“, Sapienza, University of Rome, Italy
Dimitrios Chatzipetris, Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece
Dimitrios K. Manatakis, Department of Surgery, Athens Naval and Veterans Hospital, Athens, Greece
Dimitrios Ntourakis, School of Medicine, Division of Surgery, European University Cyprus, Greece
Dimitrios Papaconstantinou, Attikon University Hospital, 3rd Department of Surgery, Greece
Dimitrios Schizas, First Department of Surgery, National and Kapodistrian University of Athens, Athens, Greece
Dimosthenis Chrysikos, First Department of Propaedeutic Surgery, Hippocration Hospital, School of Medicine, University of Athens, Athens, Greece
Dmitry Mikhailovich Adamovich, Department of Surgical Diseases II, Gomel State Medical University, Gomel, Belarus
Doaa Elkafrawy, Kafersaad general hospital, Egypt
Dragos Seban, University of Medicine and Pharmacy, Carol Davila Bucharest & 4th Surgery Department of University Emergency Hospital Bucharest, Bucharest, Romania
Edgar Fernando Hernández García, Cirugía de trauma, Hospital Central Militar, Ciudad de México, Mexico
Edoardo Baldini, Ospedale Santa Maria delle Stelle, Melzo, Italy
Edoardo Picetti, Department of Anesthesia and Intensive Care, Parma University Hospital, Parma, Italy
Edward C.T.H. Tan, Radboud university medical center, Department of Surgery, Netherlands
Efstratia Baili, Guy's and St Thomas' NHS Foundation Trust, United Kingdom
Eftychios Lostoridis, Kavala General Hospital, Kavala, Greece
Elena Adelina Toma, Surgery Department, UMF Carol Davila Bucharest, Romania
Elif Colak, University of Samsun, Turkey
Elisabetta Cerutti, Department of Anesthesia and Transplant Surgical Intensive care, Ospedali Riuniti, Ancona, Italy
Elmin Steyn, Stellenbosch University and Tygerberg Hospital, South Africa
Elmuiz A. Hsabo, Manchester University NHS Foundation Trust, United Kingdom
Emmanouil Ioannis Kapetanakis, Department of Thoracic Surgery, “Attikon” University Hospital, National and Kapodistrian University of Athens, Athens, Greece
Emmanouil Kaouras, Department of Surgery, Metaxa Cancer Hospital, Piraeus, Greece
Emmanuel Schneck, Department of Anesthesiology, Operative Intensive Care Medicine and Pain Therapy, University Hospital of Giessen, Rudolf-Buchheim-Strasse 7, Giessen, Germany
Emrah Akin, Sakarya University Faculty of Medicine, Turkey
Emre Gonullu, General Surgery, Sakarya training and research hospital, Sakarya, Turkey
Enes çelik, Derik State Hospital, Turkey
Enrico Cicuttin, General, Emergency and Trauma Surgery, Pisa University Hospital, Pisa, Italy
Enrico Pinotti, Policlinico San Pietro, Italy
Erik Johnsson, Department of Surgery, Sahlgren University Hospital, Gothenburg, Sweden
Ernest E. Moore, Director of Research Ernest E Moore Shock Trauma Center at Denver Health, United States
Ervis Agastra, Regional Hospital of Korce, Albania
Evgeni Nikolaev Dimitrov, Department of Surgical Diseases, University Hospital "Prof. Dr. Stoyan Kirkovich" Stara Zagora, Bulgaria
Ewen A Griffiths, Department of Upper GI Surgery, Queen Elizabeth Hospital, Birmingham, United Kingdom
Fabrizio D'Acapito, Morgagni-Pierantoni Hospital, AUSL Romagna, Italy
Federica Saraceno, UOC of General and Minimally Invasive Surgery, Hospital „San Paolo“, Largo Donatori del Sangue 1, Civitavecchia, Rome, Italy
Felipe Alconchel, Virgen de la Arrixaca University Hospital (IMIB-Arrixaca), Spain
Felix Alexander Zeppernick, Department of Gynaecology and Obstetrics, University Hospital of Giessen, Giessen, Germany
Fernando Machado Rodríguez, Departamento de Emergencia, Hospital de Clínicas „Dr. Manuel Quintela“ - Facutad de Medicina de la UdelaR, Montevideo, Uruguay
Fikri Abu-Zidan, Department of Surgery, College of Medicine, UAE University, Al-Ain, United Arab Emirates
Francesca Pecchini, Division of General Surgery, Emergency and New Technologies, Ospedale Civile Baggiovara, AOU, Modena, Italy
Francesco Favi, UOC Chirurgia Generale e DÚrgenza Cesena Ausl della Romagna, Italy
Francesco Ferrara, Department of Surgery, San Carlo Borromeo Hospital, ASST Santi Paolo e Carlo, Milan, Italy
Francesco Fleres, Department of Human Pathology of the Adult and Evolutive Age “Gaetano Barresi”, Section of General and Emergency Surgery, University of Messina, Messina, Italy
Francesco Pata, Department of Surgery, Nicola Giannettasio Hospital, Corigliano-Rossano, Italy
Francesco Pietro Maria Roscio, ASST Valle Olona Busto Arsizio, Italy
Francesk Mulita, Department of Surgery, General University Hospital of Patras, Greece
Frank J. M. F. Dor, 1. Imperial College Renal and Transplant Centre, Hammersmith Hospital, Imperial College Healthcare NHS Trust, London, 2. Department of Surgery and Cancer, Imperial College, London, United Kingdom
Fredrik Linder, Department of Surgical Sciences, Emergency Surgery, Uppsala University, Uppsala, Sweden
Gabriel Dimofte, Institutul Regional de Oncologie Iasi, Universitatea de Medicina si Farmacie „Grigore T. Popa“ Iasi, Romania
Gabriel Rodrigues, General Surgery, Kasturba Medical College Hospital, Manipal Academy of Higher Education, Manipal, India
Gabriela Nita, Sant'Anna Hospital, AUSL Reggio Emilia, Italy
Gabriele Sganga, Emergency Surgery & Trauma, Fondazione Policlinico Universitario A. Gemelli IRCCS, Roma, Italy
Gennaro Martines, Azienda Ospedaliero Universitaria Policlinico Bari, Italy
Gennaro Mazzarella, Department of Emergency Surgery, Sapienza University of Rome, Rome, Italy
Gennaro Perrone, Department of emergency surgery, Parma Maggiore Hospital, Parma, Italy
George Velmahos, Massachusetts General Hospital and Harvard Medical School, Boston, Massachusetts, USA
Georgios D. Lianos, Department of Surgery, University Hospital of Ioannina, Greece
Gia Tomadze, Surgery Department of Tbilisi State Medical University, Georgia
Gian Luca Baiocchi, UOC General Surgery, ASST Cremona; Department of Clinical and Experimental Sciences, University of Brescia, Italy
Giancarlo D'Ambrosio, Policlinico Umberto I, Univeristà La Sapienza, Roma, Italy
Gianluca Pellino, Department of Advanced Medical and Surgical Sciences, Università degli Studi della Campania Luigi Vanvitelli, Naples, Italy
Gianmaria Casoni Pattacini, Division of General Surgery, Emergency and New Technologies, Ospedale Civile Baggiovara, AOU, Modena, Italy
Giorgio Giraudo, Department of Surgery ASO Santa Croce e Carle Cuneo, Italy
Giorgio Lisi, Department of Surgery, Sant'Eugenio Hospital, piazzale dell'umanesimo 10, Rome, Italy
Giovanni Domenico Tebala, Oxford University Hospitals NHS Foundation Trust, United Kingdom
Giovanni Pirozzolo, Ospedale dell'Angelo - ULSS3 Serenissima – Venice, Italy
Giulia Montori, General surgery, Vittorio Veneto hospital (TV), Italy
Giulio Argenio, UOC Chirurgia Generale ed Oncologica, AO San Pio, Benevento, Italy
Giuseppe Brisinda, Department of Surgery, Fondazione Policlinico Universitario A Gemelli IRCCS and Università Cattolica S. Cuore, Rome, Italy
Giuseppe Currò, AOU Mater Domini Catanzaro - Magna Graecia University of Catanzaro, Italy
Giuseppe Giuliani, Department of general and emergency surgery, Misericordia Hospital, Grosseto, Italy
Giuseppe Palomba, Università degli Studi di Napoli Federico II, Italy
Giuseppe Roscitano, University of Catania, Italy
Gökhan Avşar, Ankara university faculty of medicine department of surgical oncology, Turkey
Goran Augustin, University Hospital Centre Zagreb, Croatia
Guglielmo Clarizia, UOC Chirurgia Generale, PO Sondrio, ASST Valtellina e Alto Lario, Italy
Gustavo M. Machain Vega, University of Asuncion, Faculty of Medical Sciences, II Chair and Service of General Surgery Hospital de Clinicas FCM, Paraguay
Gustavo P. Fraga, Division of Trauma Surgery, University of Campinas (Unicamp), Brazil
Harsheet Sethi, Acute Surgical Unit, Princess Alexandra Hospital, Brisbane, QLD, Australia
Hazim Abdulnassir Eltyeb, General Surgery, Health Education North East, United Kingdom
Helmut A. Segovia Lohse, II Cátedra de Clínica Quirúrgica. Hospital de Clínicas. Universidad Nacional de Asunción. San Lorenzo, Paraguay
Herald René Segovia Lohse, II Cátedra de Clínica Quirúrgica, Hospital de Clínicas, Universidad Nacional de Asunción, San Lorenzo, Paraguay
Hüseyin Bayhan, Mardin Training and Research Hospital, Turkey
Hytham K. S. Hamid, Kuwaiti Specialized Hospital, Sudan
Igor A. Kryvoruchko, Kharkiv National Medical University, Ukraine
Immacolata Iannone, Azienda Ospedaliera Policlinico Umberto I, Roma, Italy
Imtiaz Wani, Govt Gousia Hospital, Srinagar, India
Ioannis I. Lazaridis, Clarunis, Department of Visceral Surgery, University Centre for Gastrointestinal and Liver Diseases, St. Clara Hospital and University Hospital Basel, Basel, Switzerland
Ioannis Katsaros, Department of Surgery, Metaxa Cancer Hospital, Pireaus, Greece
Ioannis Nikolopoulos, Lewisham & Greenwich NHS Trust, United Kingdom
Ionut Negoi, Carol Davila University of Medicine and Pharmacy Bucharest, Emergency Hospital of Bucharest, Romania
Isabella Reccia, Department of Surgery and Cancer, Hammersmith Hospital, Imerpial College Healthcare NHS Trust, London, United Kingdom
Isidoro Di Carlo, University of Catania, Italy
Iyiade Olatunde Olaoye, Surgery Department, University of Ilorin Teaching Hospital, Ilorin, Nigeria
Jacek Czepiel, Department of Infectious and Tropical Diseases, Jagiellonian University Medical College, Krakow, Poland
Jae Il Kim, Department of Surgery, Inje University Ilsan Paik Hospital, Goyang, South Korea
Jeremy Meyer, University Hospitals of Geneva, Geneva, Switzerland
Jesus Manuel Saenz Terrazas, Senior Surgeon for the International Committee of the Red Cross, Nigeria
Joel Noutakdie Tochie, Anaesthesiologist and Intensive Care Physician, Laquintinie Hospital of Douala, Douala, Cameroon
Joseph M. Galante, University of California, Davis, United States
Justin Davies, Cambridge University Hospitals NHS Foundation Trust, United Kingdom
Kapil Sugand, Imperial College London, United Kingdom
Kebebe Bekele Gonfa, Maddawalabu University Goba Referral Hospital, Ethiopia
Kemal Rasa, Anadolu Medical Center Hospital affiliated with Johns Hopkins Hospital, Kocaeli, Turkey
Kenneth Y. Y. Kok, Pengiran Anak Puteri Rashidah Saadatul Bolkiah Institue of Health Sciences, Universiti Brunei darussalam, Brunei
Konstantinos G. Apostolou, 1st Department of Surgery, National and Kapodistrian University of Athens, Laiko General Hospital, Athens, Greece
Konstantinos Lasithiotakis, Department of Surgery, University Hospital of Heraklion, Crete, Greece
Konstantinos Tsekouras, Sismanogleio General Hospital, Athens, Greece
Kumar Angamuthu, Department of Clinical Microbiology, Infection Prevention & Control, Almana General Hospital, Dammam, Saudi Arabia
Lali Akhmeteli, Tbilisi State Medical University, Georgia
Larysa Sydorchuk, Bukovinian State Medical University, Ukraine
Laura Fortuna, General Surgery, Azienda Ospedaliero-Universitaria Careggi (AOUC), Largo Giovanni Alessandro Brambilla, Firenze (FI), Italy
Leandro Siragusa, Department of Surgery, Università degli studi di Roma Tor Vergata, Italy
Leonardo Pagani, Antimicrobial Stewardship Program, Infectious Diseases Branch, Bolzano Central Hospital, Italy
Leonardo Solaini, Department of Medical and Surgical Sciences, University of Bologna, Morgagni Pierantoni Hospital, Forlì, Italy
Lisa A. Miller, Western Michigan University Homer Stryker, MD School of Medicine, United States
Lovenish Bains, Maulana Azad Medical College, New Delhi, India
Luca Ansaloni, San Matteo Hospital, Pavia, Italy
Luca Ferrario, General Surgery Trauma Team ASST-GOM Niguarda, Milan, Italy
Luigi Bonavina, Department of Biomedical Sciences for Health, IRCCS Policlinico San Donato, Division of General and Foregut Surgery, University of Milan, Italy
Luigi Conti, Acute care Surgery Unit , Department of Surgery, AUSL Piacenza, Italy
Luis Antonio Buonomo, Hospital Zonal de Agudos "Dr. Alberto Balestrini", Argentina
Luis Tallon-Aguilar, Virgen del Rocío University Hospital, Spain
Lukas Tomczyk, Department of general and visceral surgery, General Hospital Lich, Germany
Lukas Werner Widmer, Department of Visceral Surgery and Medicine, University Hospital of Bern, Bern, Switzerland
Maciej Walędziak, Military Institute of Medicine, Department of General Surgery, Poland
Mahir Gachabayov, Vladimir City Emergency Hospital, Russia
Maloni Bulanauca, Department of Surgery, Labasa Hospital, Fiji
Manu L.N.G. Malbrain, Intensive Care Medicine, International Fluid Academy, Lovenjoel, Belgium and First Department of Anaesthesiology and Intensive Therapy, Medical University of Lubin, Poland
Marc Maegele, Department for Trauma and Orthopedic Surgery, Cologne-Merheim Medical Center (CMMC), Institute for Research in Operative Medicine (IFOM), University Witten-Herdecke (UW/H), Campus Cologne-Merheim, Ostmerheimerstr. 200, Cologne, Germany
Marco Catarci, Ospedale Sandro Pertini, Roma, Italy
Marco Ceresoli, University of Milano-Bicocca, Italy
Maria Chiara Ranucci, Azienda ospedaliera Santa Maria di Terni, Italy
Maria Ioanna Antonopoulou, Naval and Veteran Hospital of Crete, Greece
Maria Papadoliopoulou, General University Hospital Attikon, Athens, Greece
Maria Rosaria Valenti, Policlinico di Catania, Italy
Maria Sotiropoulou, Evaggelismos General Hospital, Greece
Mario D'Oria, Division of Vascular and Endovascular Surgery, Cardiovascular Department, University Hospital of Trieste ASUGI, Italy
Mario Serradilla Martín, Instituto de Investigación Sanitaria Aragón, Department of Surgery, Miguel Servet University Hospital, Zaragoza, Spain
Markus Hirschburger, Department of General, Visceral and Thoracic Surgery, Hospital of Worms, Worms, Germany
Massimiliano Veroux, General Surgery, University Hospital of Catania, Department of Medical and Surgical Sciences and Advanced Technologies, University of Catania, Italy
Massimo Fantoni, Fondazione Policlinico Gemelli IRCCS - UNiversità Cattolica S. Cuore, Italy
Matteo Nardi, San Camillo Forlanini Hospital, Italy
Matti Tolonen, HUS Abdominal Center, Helsinki University Hospital and University of Helsinki, Finland
Mauro Montuori, Policlinico San Pietro - Department of Surgery - Via Carlo Forlanini 15 Ponte San Pietro, Italy
Mauro Podda, Department of Surgical Science, University of Cagliari, Cagliari, Italy
Maximilian Scheiterle, SOD Chirurgia d'Urgenza, Careggi, Italy
Maximos Frountzas, First Propaedeutic Department of Surgery, National and Kapodistrian University of Athens, Medical School, Hippocration General Hospital of Athens, Greece
Mehmet Sarıkaya, Mardin, Turkey
Mehmet Yildirim, University of Health Sciences İzmir Bozyaka Training and Research Hospital General Surgery Department, Turkey
Michael Bender, Department of Neurosurgery, University Hospital of Giessen, Germany
Michail Vailas, Laiko General hospital Athens, Greece
Michel Teuben, Cantonal Hospital Frauenfeld, Switzerland
Michela Campanelli, Emergency Surgery Unit, University Hospital of Tor Vergata, viale Oxford 81, Rome, Italy
Michele Ammendola, Health of Science Department, "Magna Graecia" University Medical School, Digestive Surgery Unit, "Mater Domini" Hospital, Catanzaro, Italy
Michele Malerba, Surgical Department ASL2 Savonese, Santa Corona Hospital, Pietra Ligure (SV), Italy
Michele Pisano, ASST Papa Giovanni Bergamo, Italy
Mihaela Pertea, Sf Spiridon Emegency Hospital Iasi, University of Medicine and Pharmacy "Grigore T Popa"Iasi, Romania
Mihail Slavchev, University Hospital Eurohospital, Plovdiv, Bulgaria
Mika Ukkonen, Tampere University Hospital, Finland
Miklosh Bala, Department of General Surgery, Hadassah Medical Center and Faculty of Medicine, Hebrew University of Jerusalem, Israel
Mircea Chirica, Service de chirurgie digestive, Centre hospitalier universitaire Grenoble Alpes, France
Mirko Barone, Department of Surgery, SS. Annunziata University Hospital of Chieti, Italy
Mohamed Maher Shaat, King Faisal Medical Complex in Taif, Saudi Arabia
Mohammed Jibreel Suliman Mohammed, Wirral University Teaching Hospital, United Kingdom
Mona Awad Akasha Abuelgasim, Kingston Hospital NHS foundation trust, United Kingdom
Monika Gureh, General surgery, AIIMS Bhuvneshwar, Bhuvneshwar, India
Mouaqit Ouadii, Hassan II hospital, Morocco
Mujdat Balkan, General Surgery, TOBB ETÜ Medical school, Ankara, Turkey
Mumin Mohamed, Queen Elizabeth Hospital Birmingham, United Kingdom
Musluh Hakseven, Ankara University School of Medicine Department of General Surgery, Surgical Oncology, Turkey
Natalia Velenciuc, University of Medicine and Pharmacy Grigore T. Popa Iasi/ Regional Institute of Oncology Iasi, Romania
Nicola Cillara, Chirurgia Generale PO Santissima Trinità Cagliari, Italy
Nicola de'Angelis, Henri Mondor University Hospital (AP-HP), Faculty of Medicine, University of Paris Est, UPEC, France
Nicolò Tamini, ASST MONZA - Ospedale San Gerardo, Italy
Nikolaos J. Zavras, Department of Pediatric Surgery-General University Hospital "ATTIKON", Greece
Nikolaos Machairas, General Hospital of Athens “Laiko”, Greece
Nikolaos Michalopoulos, General University Hospital Attikon, Athens, Greece
Nikolaos N. Koliakos, Univerisity Hospital Attikon, Athens, Greece
Nikolaos Pararas, Dr Sulaiman Al Habib Hospital, Saudi Arabia
Noel E. Donlon, Trinity college Dublin st James hospital, Ireland
Noushif Medappil, Aster Malabar Institute of Medical Sciences (Aster MIMS - Calicut), India
Offir Ben-Ishay, Surgical Oncology, Division of Surgery, Rambam Health Care Campus, Haifa, Israel
Stefano Olmi, General and Oncological Surgery Department, Senior Research Vita-Salute, San Raffaele University, Milan, San Marco Hospital GSD, Zingonia (BG), Italy
Omar Islam, Wirral university teaching hospital, United Kingdom
Ömer Tammo, Mardin training and research hospital, Turkey
Orestis Ioannidis, 4th Department of Surgery, Medical School, Aristotle University of Thessaloniki, General Hospital “George Papanikolaou”, Thessaloniki, Greece
Oscar Aparicio, Parc Tauli Hospital Universitari Sabadell, Spain
Oussama Baraket, Deprtement of surghery bizerte hospital, Faculty of medicine of Tunis, Tunisia
Pankaj Kumar, Department of General Surgery, Bhubaneswar, Odisha, India
Pasquale Cianci, Lorenzo Bonomo Hospital Andria-ASL BAT-University of Foggia, Italy
Per Örtenwall, Department of surgery, Sahlgrenska University Hospital, Gothenburg, Sweden
Petar Angelov Uchikov, Medical university of Plovdiv, Department of special surgery, Medical faculty, University hospital “St. George”, Plovdiv, Bulgaria
Philip de Reuver, Department of Surgery, Radboudumc, Nijmegen, Netherlands
Philip F. Stahel, Rocky Vista University College of Osteopathic Medicine, United States
Philip S. Barie, Department of Surgery, Weill Cornell Medicine, New York, NY, United States
Micaela Piccoli, Division of General Surgery, Emergency and New Technologies, Ospedale Civile Baggiovara, AOU, Modena, Italy
Piotr Major, Jagiellonian University Medical College, Poland
Pradeep H. Navsaria, Trauma Centre, Groote Schuur Hospital and University of Cape Town, South Africa
Prakash Kumar Sasmal, All India Institute of Medical Sciences, Bhubaneswar, India
Raul Coimbra, Riverside University Health System MEdical Center / Loma Linda University, United States
Razrim Rahim, Universiti Sains Islam Malaysia, Malaysia
Recayi Çapoğlu, General Surgery, Sakarya training and research hospital, Sakarya, Turkey
Renol M. Koshy, Luton & Dunstable University Hospital, United Kingdom
Ricardo Alessandro Teixeira Gonsaga, Centro Universitário Padre Albino, Catanduva (SP), Brazil
Riccardo Pertile, Department of Clinical and Evaluative Epidemiology, Health Service of Trento, Italy
Rifat Ramadan Mussa Mohamed, University Hospital Ayr, United Kingdom
Rıza Deryol, Department of General Surgery, Surgical Oncology Unit, Ankara University, School of Medicine, Ankara, Turkey
Robert G. Sawyer, Western Michigan University School of Medicine, United States
Roberta Angelico, HPB and Transplant Unit, University of Rome Tor Vergata, Italy
Roberta Ragozzino, General surgery and Trauma Team, ASST Niguarda, Milano, Piazza Ospedale Maggiore 3, Milan, Italy
Roberto Bini, ASST Niguarda Hospital, Italy
Roberto Cammarata, Campus Biomedico University of Rome, Italy
Rosa Scaramuzzo, General Surgery Unit, San Paolo Hospital, Rome, Italy
Rossella Gioco, General Surgery, Policlinico G. Rodolico Catania, Italy
Ruslan Sydorchuk, General Surgery Department, Regional Emergency Hospital Chernivtsi, Ukraine
Salma Ahmed, Wirral University Teaching Hospital, United Kingdom
Salomone Di Saverio, Ospedale Madonna del Soccorso San benedetto del Tronto, Italy
Sameh Hany Emile, Mansoura University Hospital, Egypt
Samir Delibegovic, Department of Surgery, University Clinical Center Tuzla, Tuzla, Bosnia and Herzegovina
Sanjay Marwah, Pt BDS Postgraduate Institute of Medical Sciences, Rohtak, Haryana, India
Savvas Symeonidis, General Hospital of Thessaloniki Georgios Papanikolaou, Greece
Scott G. Thomas, Trauma Services, Indiana University School of Medicine, Beacon Health System, Memorial Hospital South Bend, Indiana, United States
Sebahattin Demir, Turkey
Selmy S. Awad, Mansoura university hospitals, Mansoura University, Egypt
Semra Demirli Atici, University of Health Sciences Tepecik Training and Research Hospital, Turkey
Serge Chooklin, Lviv National Medical University, Ukraine
Serhat Meric, General surgery department, Bağcılar training and research hospital, Istanbul, Turkey
Sevcan Sarıkaya, Mardin Training and Research Hospital, Mardin, Turkey
Sharfuddin Chowdhury, King Saud Medical City, Riyadh, Saudi Arabia
Shaza Faycal Mirghani, Sandwell General Hospital, United Kingdom
Sherry M. Wren, Stanford University, United States
Simone Gargarella, University “G.D’Annunzio” Chieti – Pescara, Italy
Simone Rossi Del Monte, ASL Roma 1 - Ospedale San Filippo Neri, Italy
Sofia Esposito, General, emergency and new technology surgery Unit, Baggiovara General Hospital, Modena, Italy
Sofia Xenaki, Department of General Surgery, University Hospital of Heraklion Crete, Greece
Soliman Fayez Ghedan Mohamed, KFMC, Saudi Arabia
Solomon Gurmu Beka, Emergency Surgery, Professional Specialist at Ethiopian Air Force Hospital, President of Ethiopian Emergency Surgery Association, Bishoftu, Oromia, Ethiopia
Sorinel Lunca, University of Medecine "Gr.T.Popa" Iasi Second Oncology Surgery Clinic Regional Institute of Oncology Iasi, Romania
Spiros G. Delis, University of Athens, Greece
Spyridon Dritsas, Colorectal and Peritoneal Oncology Centre, The Christie NHS Foundation Trust, Manchester, United Kingdom
Stefan Morarasu, 2nd Department of Surgical Oncology, Regional Institute of Oncology, Iasi, Romania
Stefano Magnone, ASST Papa Giovanni XXIII Bergamo, Italy
Stefano Rossi, Emergency surgery San Filippo Neri hospital ASL Roma1, Italy
Stefanos Bitsianis, 4th Department of Surgery of Aristotle University of Thessaloniki, Greece
Stylianos Kykalos, 2nd Department of Propaedeutic Surgery, General Hospital Laiko, National and Kapodistrian University of Athens, Greece
Suman Baral, Dirghayu Pokhara Hospital, Pokhara, Nepal
Sumita A Jain, SMS MEedical College and Hospital Jaipur, India
Syed Muhammad Ali, Hamad Medical Corporation, Qatar
Tadeja Pintar, Surgery Department, UMC Ljubljana, Ljubljana, Sloviena
Tania Triantafyllou, Advanced Upper GI Surgical Fellow, Athens, Greece
Tarik Delko, University Center for Gastrointestinal and Liver Diseases, Basel, Switzerland
Teresa Perra, Università degli Studi di Sassari, Italy
Theodoros A. Sidiropoulos, Surgical Resident, 4th Surgical Department, Attikon University Hospital, Athens, Greece
Thomas M. Scalea, R Adams Cowley Shock Trauma Center, University of Maryland School of Medicine, United States
Tim Oliver Vilz, Department of Surgery, University Hospital Bonn, Venusberg Campus 1, Bonn, Germany
Timothy Craig Hardcastle, IALCH, Durban and University of KwaZulu-Natal, South Africa
Tongporn Wannatoop, Department of Surgery, Faculty of Medicine Siriraj hospital, Mahidol university, Bankok, Thailand
Torsten Herzog, Department of Surgery, St. Josef Hospital, Ruhr University Bochum, Germany
Tushar Subhadarshan Mishra, Department of Surgery, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India
Ugo Boggi, Division of General and Transplant Surgery, University of Pisa, Italy
Valentin Calu, Elias Emergency University Hospital, Romania
Valentina Tomajer, Ospedale San Raffaele Milan, Italy
Vanni Agnoletti, Azienda USL della Romagna – Cesena, Italy
Varut Lohsiriwat, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
Victor Kong, Department of Surgery, University of KwaZulu Natal, Durban, South Africa
Virginia Durán Muñoz-Cruzado, Virgen del Rocío University Hospital, Spain
Vishal G. Shelat, Department of General Surgery, Tan Tock Seng Hospital, Singapore
Vladimir Khokha, Department of surgery, Mozyr city hospital, Belarus
Wagih Mommtaz Ghannam, Mansoura Faculty of Medicine, Egypt
Walter L. Biffl, Scripps Clinic Medical Group, United States
Wietse Zuidema, Amsterdam University Medical Center, Amsterdam, Netherlands
Yasin Kara, Health Sciences University Kanuni Sultan Süleyman Training and Research Hospital General Surgery Clinic, Turkey
Yoshiro Kobe, Chiba Emergency Medical Center, Japan
Zaza Demetrashvili, Surgery Department, Tbilisi State Medical University, Georgia
Ziad A. Memish, Research and Innovation Center, King Saud Medical City, Ministry of Health & College of Medicine Alfaisal University, Saudi Arabia
Zoilo Madrazo, Bellvitge University Hospital, Barcelona, Spain
Zsolt J. Balogh, Department of Traumatology, John Hunter Hospital and University of Newcastle, Australia
Zulfu Bayhan, Sakarya University, Faculty of Medicine Department of General Surgery, Turkey
Martin Reichert, Massimo Sartelli, Markus A. Weigand, Matthias Hecker, Ingolf H. Askevold, Juliane Liese, Winfried Padberg and Andreas Hecker: core investigator.
Federico Coccolini and Fausto Catena: WSES project steering committee representative.
Abbreviations
- CHERRIES
The Checklist for Reporting Results of Internet E-Surveys
- COVID-19
Corona virus disease 2019
- PCR
Polymerase chain reaction
- SARS-CoV-2
Severe acute respiratory syndrome corona virus type 2
- TTD
Time-to-diagnosis
- TTI
Time-to-intervention
- WSES
World Society of Emergency Surgery
Author contributions
Each author had made substantial contributions to the present manuscript. MR, MS, MAW, MH, IHA, JL, WP, FCo, FCa and AH contributed to conception and design. MR, PUO, JN and AH were involved in acquisition and analysis of data. MR and AH interpreted data. MR, MH and AH contributed to writing first draft. MS, MAW, JL, WP, FCo and FCa were involved in critical revision of the manuscript. All authors read the final version of the manuscript and gave final approval for the submission.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding received for this work.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Martin Reichert, Email: martin.reichert@chiru.med.uni-giessen.de.
The WSES COVID-19 emergency surgery survey collaboration group:
Adam Peckham-Cooper, Adrian Camacho-Ortiz, Aikaterini T. Mastoraki, Aitor Landaluce-Olavarria, Ajay Kumar Pal, Akira Kuriyama, Alain Chichom-Mefire, Alberto Porcu, Aleix Martínez-Pérez, Aleksandar R. Karamarkovic, Aleksei V. Osipov, Alessandro Coppola, Alessandro Cucchetti, Alessandro Spolini, Alessio Giordano, Alexander Reinisch-Liese, Alfie J. Kavalakat, Alin Vasilescu, Amin Alamin, Amit Gupta, Ana Maria Dascalu, Ana-Maria Musina, Anargyros Bakopoulos, Andee Dzulkarnaen Zakaria, Andras Vereczkei, Andrea Balla, Andrea Bottari, Andreas Baumann, Andreas Fette, Andrey Litvin, Aniella Katharina Reichert, Anna Guariniello, Anna Paspala, Anne-Sophie Schneck, Antonio Brillantino, Antonio Pesce, Arda Isik, Ari Kalevi Leppäniemi, Aristeidis Papadopoulos, Aristotelis Kechagias, Ashraf Yehya Abdalla Mohamed, Ashrarur Rahman Mitul, Athanasios Marinis, Athanasios Syllaios, Baris Mantoglu, Belinda De Simone, Benjamin Stefan Weiss, Bernd Pösentrup, Biagio Picardi, Biagio Zampogna, Boris Eugeniev Sakakushev, Boyko Chavdarov Atanasov, Bruno Nardo, Bulent Calik, Camilla Cremonini, Carlos A. Ordoñez, Charalampos Seretis, Chiara Cascone, Christos Chouliaras, Cino Bendinelli, Claudia Lopes, Claudio Guerci, Clemens Weber, Constantinos Nastos, Cristian Mesina, Damiano Caputo, Damien Massalou, Davide Cavaliere, Deborah A. McNamara, Demetrios Demetriades, Desirè Pantalone, Diego Coletta, Diego Sasia, Diego Visconti, Dieter G. Weber, Diletta Corallino, Dimitrios Chatzipetris, Dimitrios K. Manatakis, Dimitrios Ntourakis, Dimitrios Papaconstantinou, Dimitrios Schizas, Dimosthenis Chrysikos, Dmitry Mikhailovich Adamovich, Doaa Elkafrawy, Dragos Seban, Edgar Fernando Hernandez García, Edoardo Baldini, Edoardo Picetti, Edward C. T. H. Tan, Efstratia Baili, Eftychios Lostoridis, Elena Adelina Toma, Elif Colak, Elisabetta Cerutti, Elmin Steyn, Elmuiz A. Hsabo, Emmanouil Ioannis Kapetanakis, Emmanouil Kaouras, Emmanuel Schneck, Emrah Akin, Emre Gonullu, Enes çelik, Enrico Cicuttin, Enrico Pinotti, Erik Johnsson, Ernest E. Moore, Ervis Agastra, Evgeni Nikolaev Dimitrov, Ewen A. Griffiths, Fabrizio D’Acapito, Federica Saraceno, Felipe Alconchel, Felix Alexander Zeppernick, Fernando Machado Rodríguez, Fikri Abu-Zidan, Francesca Pecchini, Francesco Favi, Francesco Ferrara, Francesco Fleres, Francesco Pata, Francesco Pietro Maria Roscio, Francesk Mulita, Frank J. M. F. Dor, Fredrik Linder, Gabriel Dimofte, Gabriel Rodrigues, Gabriela Nita, Gabriele Sganga, Gennaro Martines, Gennaro Mazzarella, Gennaro Perrone, George Velmahos, Georgios D. Lianos, Gia Tomadze, Gian Luca Baiocchi, Giancarlo D’Ambrosio, Gianluca Pellino, Gianmaria Casoni Pattacini, Giorgio Giraudo, Giorgio Lisi, Giovanni Domenico Tebala, Giovanni Pirozzolo, Giulia Montori, Giulio Argenio, Giuseppe Brisinda, Giuseppe Currò, Giuseppe Giuliani, Giuseppe Palomba, Giuseppe Roscitano, Gökhan Avşar, Goran Augustin, Guglielmo Clarizia, Gustavo M. Machain Vega, Gustavo P. Fraga, Harsheet Sethi, Hazim Abdulnassir Eltyeb, Helmut A. Segovia Lohse, Herald René Segovia Lohse, Hüseyin Bayhan, Hytham K. S. Hamid, Igor A. Kryvoruchko, Immacolata Iannone, Imtiaz Wani, Ioannis I. Lazaridis, Ioannis Katsaros, Ioannis Nikolopoulos, Ionut Negoi, Isabella Reccia, Isidoro Di Carlo, Iyiade Olatunde Olaoye, Jacek Czepiel, Jae Il Kim, Jeremy Meyer, Jesus Manuel Saenz Terrazas, Joel Noutakdie Tochie, Joseph M. Galante, Justin Davies, Kapil Sugand, Kebebe Bekele Gonfa, Kemal Rasa, Kenneth Y. Y. Kok, Konstantinos G. Apostolou, Konstantinos Lasithiotakis, Konstantinos Tsekouras, Kumar Angamuthu, Lali Akhmeteli, Larysa Sydorchuk, Laura Fortuna, Leandro Siragusa, Leonardo Pagani, Leonardo Solaini, Lisa A. Miller, Lovenish Bains, Luca Ansaloni, Luca Ferrario, Luigi Bonavina, Luigi Conti, Luis Antonio Buonomo, Luis Tallon-Aguilar, Lukas Tomczyk, Lukas Werner Widmer, Maciej Walędziak, Mahir Gachabayov, Maloni M. Bulanauca, Manu L. N. G. Malbrain, Marc Maegele, Marco Catarci, Marco Ceresoli, Maria Chiara Ranucci, Maria Ioanna Antonopoulou, Maria Papadoliopoulou, Maria Rosaria Valenti, Maria Sotiropoulou, Mario D’Oria, Mario Serradilla Martín, Markus Hirschburger, Massimiliano Veroux, Massimo Fantoni, Matteo Nardi, Matti Tolonen, Mauro Montuori, Mauro Podda, Maximilian Scheiterle, Maximos Frountzas, Mehmet Sarıkaya, Mehmet Yildirim, Michael Bender, Michail Vailas, Michel Teuben, Michela Campanelli, Michele Ammendola, Michele Malerba, Michele Pisano, Mihaela Pertea, Mihail Slavchev, Mika Ukkonen, Miklosh Bala, Mircea Chirica, Mirko Barone, Mohamed Maher Shaat, Mohammed Jibreel Suliman Mohammed, Mona Awad Akasha Abuelgasim, Monika Gureh, Mouaqit Ouadii, Mujdat Balkan, Mumin Mohamed, Musluh Hakseven, Natalia Velenciuc, Nicola Cillara, Nicola de’Angelis, Nicolò Tamini, Nikolaos J. Zavras, Nikolaos Machairas, Nikolaos Michalopoulos, Nikolaos N. Koliakos, Nikolaos Pararas, Noel E. Donlon, Noushif Medappil, Offir Ben-Ishay, Olmi Stefano, Omar Islam, Ömer Tammo, Orestis Ioannidis, Oscar Aparicio, Oussama Baraket, Pankaj Kumar, Pasquale Cianci, Per Örtenwall, Petar Angelov Uchikov, Philip de Reuver, Philip F. Stahel, Philip S. Barie, Micaela Piccoli, Piotr Major, Pradeep H. Navsaria, Prakash Kumar Sasmal, Raul Coimbra, Razrim Rahim, Recayi Çapoğlu, Renol M. Koshy, Ricardo Alessandro Teixeira Gonsaga, Riccardo Pertile, Rifat Ramadan Mussa Mohamed, Rıza Deryol, Robert G. Sawyer, Roberta Angelico, Roberta Ragozzino, Roberto Bini, Roberto Cammarata, Rosa Scaramuzzo, Rossella Gioco, Ruslan Sydorchuk, Salma Ahmed, Salomone Di Saverio, Sameh Hany Emile, Samir Delibegovic, Sanjay Marwah, Savvas Symeonidis, Scott G. Thomas, Sebahattin Demir, Selmy S. Awad, Semra Demirli Atici, Serge Chooklin, Serhat Meric, Sevcan Sarıkaya, Sharfuddin Chowdhury, Shaza Faycal Mirghani, Sherry M. Wren, Simone Gargarella, Simone Rossi Del Monte, Sofia Esposito, Sofia Xenaki, Soliman Fayez Ghedan Mohamed, Solomon Gurmu Beka, Sorinel Lunca, Spiros G. Delis, Spyridon Dritsas, Stefan Morarasu, Stefano Magnone, Stefano Rossi, Stefanos Bitsianis, Stylianos Kykalos, Suman Baral, Sumita A. Jain, Syed Muhammad Ali, Tadeja Pintar, Tania Triantafyllou, Tarik Delko, Teresa Perra, Theodoros A. Sidiropoulos, Thomas M. Scalea, Tim Oliver Vilz, Timothy Craig Hardcastle, Tongporn Wannatoop, Torsten Herzog, Tushar Subhadarshan Mishra, Ugo Boggi, Valentin Calu, Valentina Tomajer, Vanni Agnoletti, Varut Lohsiriwat, Victor Kong, Virginia Durán Muñoz-Cruzado, Vishal G. Shelat, Vladimir Khokha, Wagih Mommtaz Ghannam, Walter L. Biffl, Wietse Zuidema, Yasin Kara, Yoshiro Kobe, Zaza Demetrashvili, Ziad A. Memish, Zoilo Madrazo, Zsolt J. Balogh, and Zulfu Bayhan
References
- 1.COVIDSurg Collaborative; GlobalSurg Collaborative Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021;2021(76):748–758. doi: 10.1111/anae.15458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moletta L, Pierobon ES, Capovilla G, Costantini M, Salvador R, Merigliano S, et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int J Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reichert M, Sartelli M, Weigand MA, Doppstadt C, Hecker M, Reinisch-Liese A, et al. Impact of the SARS-CoV-2 pandemic on emergency surgery services-a multi-national survey among WSES members. World J Emerg Surg. 2020;15:64. doi: 10.1186/s13017-020-00341-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Noll, J., Reichert, M., Dietrich, M. et al. When to operate after SARS-CoV-2 infection? A review on the recent consensus recommendation of the DGC/BDC and the DGAI/BDA. Langenbecks Arch Surg (2022). 10.1007/s00423-022-02495-8 [DOI] [PMC free article] [PubMed]
- 5.Kamarajah SK, Markar SR, Singh P, Griffiths EA. The influence of the SARS-CoV-2 pandemic on esophagogastric cancer services: an international survey of esophagogastric surgeons. Dis Esophagus. 2020. [DOI] [PMC free article] [PubMed]
- 6.Pellino G, Spinelli A. How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum United States. 2020;63:720–722. doi: 10.1097/DCR.0000000000001685. [DOI] [PubMed] [Google Scholar]
- 7.Stöss C, Steffani M, Pergolini I, Hartmann D, Radenkovic D, Novotny A, et al. Impact of the COVID-19 pandemic on surgical oncology in Europe: results of a European survey. Dig Surg. 2021;38:259–265. doi: 10.1159/000515186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willms A, Lock JF, Simbeck A, Thasler W, Rost W, Hauer T, et al. The impact of lockdown during the COVID-19 pandemic on care for elective patients (C-elective study)—results of a multicenter survey. Zentralbl Chir Germany. 2021;146:562–569. doi: 10.1055/a-1545-5065. [DOI] [PubMed] [Google Scholar]
- 9.Hecker A, Schneck E, Rohrig R, Roller F, Hecker B, Holler J, et al. The impact of early surgical intervention in free intestinal perforation: a time-to-intervention pilot study. World J Emerg Surg England. 2015;10:54. doi: 10.1186/s13017-015-0047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hecker A, Reichert M, Reuss CJ, Schmoch T, Riedel JG, Schneck E, et al. Intra-abdominal sepsis: new definitions and current clinical standards. Langenbeck’s Arch Surg. 2019;404:257–271. doi: 10.1007/s00423-019-01752-7. [DOI] [PubMed] [Google Scholar]
- 11.Nef HM, Elsässer A, Möllmann H, Abdel-Hadi M, Bauer T, Brück M, et al. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: an observational study. Clin Res Cardiol. 2021;110:292–301. doi: 10.1007/s00392-020-01780-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McIntosh A, Bachmann M, Siedner MJ, Gareta D, Seeley J, Herbst K. Effect of COVID-19 lockdown on hospital admissions and mortality in rural KwaZulu-Natal, South Africa: interrupted time series analysis. BMJ Open. 2021;11:e047961. doi: 10.1136/bmjopen-2020-047961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kocatürk E, Salman A, Cherrez-Ojeda I, Criado PR, Peter J, Comert-Ozer E, et al. The global impact of the COVID-19 pandemic on the management and course of chronic urticaria. Allergy Denmark. 2021;76:816–830. doi: 10.1111/all.14687. [DOI] [PubMed] [Google Scholar]
- 14.Biagioli V, Albanesi B, Belloni S, Piredda A, Caruso R. Living with cancer in the COVID-19 pandemic: an Italian survey on self-isolation at home. Eur J Cancer Care (Engl) 2021;30:e13385. doi: 10.1111/ecc.13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willms AG, Oldhafer KJ, Conze S, Thasler WE, von Schassen C, Hauer T, et al. Appendicitis during the COVID-19 lockdown: results of a multicenter analysis in Germany. Langenbeck’s Arch Surg. 2021;406:367–375. doi: 10.1007/s00423-021-02090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien CM, Jung K, Dang W, Jang H-J, Kielar AZ. Collateral damage: the impact of the COVID-19 pandemic on acute abdominal emergency presentations. J Am Coll Radiol. 2020;17:1443–1449. doi: 10.1016/j.jacr.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reichert M, Hecker M, Witte B, Bodner J, Padberg W, Weigand MA, et al. Stage-directed therapy of pleural empyema. Langenbeck’s Arch Surg Germany. 2017;402:15–26. doi: 10.1007/s00423-016-1498-9. [DOI] [PubMed] [Google Scholar]
- 19.Oppelt PU, Askevold I, Hörbelt R, Roller FC, Padberg W, Hecker A, et al. Trans-hiatal herniation following esophagectomy or gastrectomy: retrospective single-center experiences with a potential surgical emergency. Hernia. France; 2021. [DOI] [PMC free article] [PubMed]
- 20.Reichert M, Pösentrup B, Hecker A, Schneck E, Pons-Kühnemann J, Augustin F, et al. Thoracotomy versus video-assisted thoracoscopic surgery (VATS) in stage III empyema-an analysis of 217 consecutive patients. Surg Endosc Germany. 2018;32:2664–2675. doi: 10.1007/s00464-017-5961-7. [DOI] [PubMed] [Google Scholar]
- 21.Coccolini F, Sartelli M, Kluger Y, Pikoulis E, Karamagioli E, Moore EE, et al. COVID-19 the showdown for mass casualty preparedness and management: the Cassandra Syndrome. World J Emerg Surg. 2020;15:26. doi: 10.1186/s13017-020-00304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tebala GD, Milani MS, Bignell M, Bond-Smith G, Lewis C, Cirocchi R, et al. Emergency surgery admissions and the COVID-19 pandemic: did the first wave really change our practice? Results of an ACOI/WSES international retrospective cohort audit on 6263 patients. World J Emerg Surg. 2022;17:8. doi: 10.1186/s13017-022-00407-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Snapiri O, Rosenberg Danziger C, Krause I, Kravarusic D, Yulevich A, Balla U, et al. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672–1676. doi: 10.1111/apa.15376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reinisch A, Reichert M, Hecker A, Padberg W, Ulrich F, Liese J. Nonoperative antibiotic treatment of appendicitis in adults: a survey among clinically active surgeons. Visc Med. 2020;36:494–500. doi: 10.1159/000506058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.