Introduction:
The purpose of this study was to identify common complications and the rates of readmission and revision in total knee arthroplasty (TKA) patients younger than 65 years.
Methods:
Using the American Joint Replacement Registry, we conducted a retrospective review of all TKAs done in patients aged 18 to 65 years from 2012 to 2020. Demographic factors such as age, sex, Charlson Comorbidity Index (CCI), and preoperative Veterans RAND 12-Item Health Survey Physical Component Summary (VR-12 PCS) scores were collected. We excluded patients older than 65 years and revision, oncologic, and nonelective cases. Primary outcomes included cumulative revision rate, 90-day readmission rate, and reason for revision. Univariate analysis and the Kaplan-Meier method were used.
Results:
Six thousand one hundred seventy-nine patients were included. The average age was 58.8 years (SD 5.5 years), 61% were female, 82% were White, and 88% had a CCI of 0 (1 = 8% and ≥2 = 4%). The mean follow-up was 42.51 months. Seventy-four patients (1.2%) underwent revision. Sixty-nine patients (1.1%) were readmitted within 90 days. No factors assessed increased revision rates. Revision-free survivorship was 98.7% (95% CI 98.4 to 99.0) and 98.6% (95% CI 98.2 to 99.0) at 5 and 8 years, respectively. Infection (15%), aseptic loosening (14%), and instability (12%) were the most common indications for revision.
Conclusion:
TKA done in young and presumed active patients has excellent survivorship. Long-term follow-up is needed to assess survival trends in this growing population.
The demand for total knee arthroplasty (TKA) in the United States is anticipated to increase 673% from 2005 to 2030, with 5.28 million TKAs to be done annually.1 As average life expectancy increases, younger and more active patients are undergoing TKAs. Long-term outcomes have shown increased failure rates due to mechanical failure, polyethylene wear, instability, and infection in this patient population.2,3 However, these long-term studies fail to account for improvements in implant design and surgical techniques largely used today.
Several authors reported good survivorship of TKA in young and active patients at 30 years.4,5 The generalizability of these studies is limited because of data being supplied from only few institutions. Currently, no study has analyzed the American Joint Replacement Registry (AJRR) database for outcomes of young and presumed active patients who have undergone primary TKA. This registry provides robust data on hip and knee arthroplasties done in the United States and offers trends in outcome measures. By collecting procedural, postoperative, and patient-reported outcome measures, the AJRR database provides a standardized metric to analyze surgical trends and patient outcomes across the country.
This study analyzed the AJRR database for patients younger than 65 years who underwent TKA. The objective was to investigate the overall survivorship of these patients with revision for any reason as the end point.
Methods
An application was submitted to AJRR in 2020 to analyze all TKAs done in patients aged 18 to 65 years from 2012 to 2020 and had documented preoperative VR-12 PCS scores. The main purpose of this study was to determine whether improved preoperative patient factors were associated with improved outcomes. Therefore, only patients who had documentation of all the above variables were included in the analysis. The AJRR collects knee and hip arthroplasty data, including procedural, postoperative, and patient-reported outcome measures, and contains 1,897,050 procedures from hospitals, ambulatory surgery centers, and private practice groups in the United States. Collected patient demographic factors were age, sex, Charlson Comorbidity Index (CCI), and preoperative Veterans RAND 12-Item Health Survey Physical Component Summary (VR-12 PCS) scores. The VR-12 PCS is derived from a patient-reported questionnaire that measures physical function, mental health, pain, energy, social interaction, and overall health.6 The Charlson Comorbidity Index is a method for evaluating comorbid conditions that might affect mortality and assigns an objective score to a patient.7
Age was stratified into four groups: 18 to 34 years, 35 to 44 years, 45 to 54 years, and 55 to 65 years. Sex was either male or female, and race was Black, White, or other. CCI was stratified into three groups: zero, 1, or ≥2, with each integer representing the number of medical conditions associated with morbidity.
Exclusion criteria included patients older than 65 years and revision and oncologic TKA cases. International Classification of Diseases 10th Revision (ICD-10) codes were used to stratify the type of case and reason for revision and readmission. Primary outcome measures included cumulative revision rate, 90-day readmission rate, and reason for revision.
Logistic regression analysis was used to evaluate the association between a preoperative VR-12 PCS and a subsequent revision or 90-day readmission adjusting for potential confounders. Statistical significance was set at P < 0.05. The Kaplan-Meier method was used to measure survivorship with revision for any reason as the end point.
Results
Of the 6,179 patients included in the analysis, 61% were female, 39% were male, and they had an average age of 58.8 ± 5.5 years (Table 1). The mean follow-up was 42.51 months. Seventy-four patients (1.2%) underwent revision. Sixty-nine patients (1.1%) were readmitted within 90 days (Table 2). Most common causes for revision were infection (14.9%), aseptic loosening (13.5%), and instability (12.2%). Most common reasons for 90-day readmission without revision were infection (34.8%), pain (8.7%), and extensor mechanism disruption (4.4%) (Table 2).
Table 1.
Demographic Summary
| Factors | TKA (N = 6,179) | |
| N | % | |
| Mean age (SD) | 58.8 (5.5) | |
| Age category | ||
| 18-34 | 24 | 0.4 |
| 35-44 | 89 | 1.4 |
| 45-54 | 1,049 | 17.0 |
| 55-65 | 5,017 | 81.2 |
| Sex | ||
| Male | 2,411 | 39.1 |
| Female | 3,755 | 60.9 |
| Race | ||
| White | 5,046 | 81.7 |
| Black | 300 | 4.9 |
| Other | 833 | 13.5 |
| Charlson comorbidity index | ||
| 0 | 5,440 | 88. |
| 1 | 475 | 7.7 |
| ≥2 | 264 | 4.3 |
TKA = total knee arthroplasty
Table 2.
TKA Outcomes and Top Diagnoses
| Revision and Readmission Rates | TKA (N = 6,179) | |
| Linked revisions | 74 | 1.2% |
| Linked 90-d readmissions (without revision) | 69 | 1.1% |
| Top 3 Reasons for Revision | TKA (N = 74) | |
| Infection | 11 | 14.9% |
| Aseptic loosening | 10 | 13.5% |
| Instability | 9 | 12.2% |
| Top 3 Reasons for 90-d Readmission w/o Revision | TKA (N = 69) | |
| Infection | 24 | 34.8% |
| Pain | 6 | 8.7% |
| Extensor mechanism disruption | 3 | 4.4% |
TKA = total knee arthroplasty
Readmission within 90 days requiring revision was more common in Black patients compared with White patients, although this did not reach statistical significance (P = 0.077) (Table 3). Age, sex, CCI, and preoperative VR-12 scores were not associated with increased early readmission requiring revision. Using the Kaplan-Meier method, patient survivorship free of revision was 99% (95% CI 99.06 to 99.49) at 2 years, 99% (95% CI 98.37 to 99.02) at 5 years, and 99% (95% CI 98.20 to 98.97) at 8 years (Figure 1).
Table 3.
Association Between Independent Factors and Linked Revisions Among Younger Patients (18 to 65 Years)
| Factors | TKA (N = 6,142) | |||
| Odds Ratio | Lower Limit | Upper Limit | P | |
| Preoperative VR-12 PCS | 0.981 | 0.954 | 1.008 | 0.159 |
| Age | 0.977 | 0.94 | 1.015 | 0.229 |
| Sex: female versus male | 1.212 | 0.744 | 1.973 | 0.44 |
| Race: Black versus White | 2.074 | 0.924 | 4.656 | 0.077 |
| Race: other versus White | 0.837 | 0.397 | 1.767 | 0.641 |
| Charlson comorbidity index | 0.851 | 0.555 | 1.305 | 0.459 |
TKA = total knee arthroplasty, PCS = Physical Component Summary Scores
Figure 1.
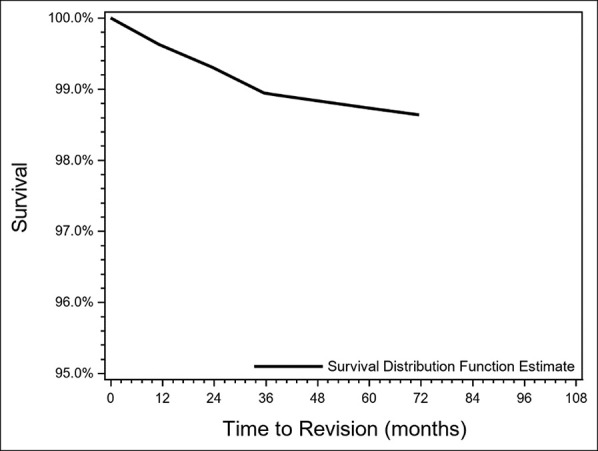
Graph showing Kaplan-Meier survivorship for total knee arthroplasty in patients yopunger than 65 years.
Readmission within 90 days not requiring revision was not associated with any variables analyzed in the database (Table 4). We did not find any correlation between age and VR-12 scores with readmissions.
Table 4.
Association Between Independent Factors and Linked 90-day Readmissions Without Revision Among Younger Patients (18 to 65 Years)
| Factors | TKA (N = 53) | |||
| Odds Ratio | Lower Limit | Upper Limit | P | |
| Preoperative VR-12 PCS | 0.913 | 0.785 | 1.062 | 0.238 |
| Age | 1.103 | 0.897 | 1.356 | 0.351 |
TKA = total knee arthroplasty, PCS = Physical Component Summary Scores
Discussion
With an increase in demand and broader indications for surgery, patients aged 65 years and younger are likely receiving TKAs more frequently than at any other time. Two nationwide database studies and a systematic review have evaluated the complication rates of TKA in this patient population and demonstrated similarly excellent survival rates in this patient population.8–10 However, these studies may not accurately reflect the advances made in implant design over the past several decades. In our analysis of the AJRR database, patient survivorship free of revision was 99% at 8 years with a 1.2% cumulative revision rate. Owing to inherent limitations of the database, these findings represent trends in data and cannot yet be used to make definitive conclusions on outcomes.
In a multicenter study by Parvizi et al,11 residual symptoms and functional deficits in 661 young patients with a mean age of 54 years were assessed at 1 to 4 years after primary TKA. They reported that 89% of the patients were satisfied with their capacity to do daily tasks and 91% of the patients were satisfied by the reduction in pain. Approximately 33% of these patients noted residual symptoms, including some degree of pain (33%), stiffness (41%), grinding noises (33%), and swelling and tightness (33%).11 Their analysis suggests that this patient population should carefully consider TKA because of the high likelihood of residual symptoms.
In a cohort of 44 TKAs, Meftah et al12 showed that the long-term follow-up of all-polyethylene tibial implants was 12.4 years (range 10 to 18 years) in patients aged 60 years or younger. Kaplan-Meier survivorship at 10 years was 99.7% for revision because of mechanical reasons and 95.5% for all failures.12 In another study by the same authors, patients aged 60 years and younger who underwent TKA with a posterior-stabilized implant design had a 99% survivorship at 12.3 years.13 The results of the present study show similar survivorship of TKA in young patients to the existing literature.
A study by Della Valle et al showed a 92% survivorship free of aseptic revision in 298 TKAs in patients younger than 50 years.14 In addition, the most common reasons for revision were aseptic loosening (4.8%), deep infection (3.2%), and polyethylene wear (2.8%).14 The authors noted good implant durability, with increased revision rates if the tibial cut was in excessive varus (>4o) or slope (>10o). Their analysis provided encouraging data that TKA in young patients has excellent mid-term implant survivorship. In the AJRR database, 0.2% of all TKAs (11/6179) done in patients aged 65 years and younger required revision because of infection. Comparatively, the AJRR database showed improved infection rates in this age group than in previous studies. Moreover, 90-day readmission not requiring revision in this age group was 0.4% (24/6179). Improvements in current infection mitigation during the perioperative period may support these lower infection rates.
In our AJRR database analysis, there was a trend toward higher revision rates in Black patients compared with White patients (P = 0.077). Lavernia et al investigated pain, well-being, and function before and after TKA using self-administered questionnaires.15 The authors concluded that no preoperative differences existed between races but that Black patients had worse postoperative outcomes on the Quality of Well-Being questionnaire and 36-Item Short Form Health Survey Physical Component Summary (SF-36 PCS). Furthermore, Singh et al16 noted that Black patients younger than 65 years were up to 5 times more likely to be discharged to an inpatient rehabilitation facility when compared with their White counterparts. Moreover, young Black patients were more likely to have a readmission within 90 days than young White patients.16 A growing body of the literature, including the results of this study, has shown notable racial disparities in TKA patients. Additional studies should aim to identify quality improvement measures in minority orthopaedic populations.
Our study had several limitations. First, most of the patients had a CCI of zero. As a result, this study was not designed to determine statistical significance based on comorbidity. However, given the paucity of TKAs in young and presumed active patients, we think our study is the first to analyze the largest sample size in a cohort that is generally healthier than the elderly TKA population. Second, there was no standardization of the International Classification of Diseases 10th revision diagnosis codes for revision cases or readmissions entered into the database. As a result, diagnoses for a small percentage of cases could not be determined because of the ambiguity of the International Classification of Diseases code. Those that could not be identified are listed in Appendix Table 1, http://links.lww.com/JG9/A224. Third, additional surgeries not done at AJRR sites and patients lost to follow-up were not included in the database analysis. This is an inherent limitation of all registry studies based on institutional participation as compared with national registries. As a result, the revision rates may actually be higher than that reported in the AJRR data. Fourth, the data set does not capture whether patients choose different surgeons if they required a revision surgery. As a result, failure and infection rates may actually be higher than that reported in the AJRR data. Fifth, we limited to all-time revision in an effort to maximize outcome capture because AJRR cannot account for loss to follow-up in the younger-than-65-year-old population. Sixth, collection of data at irregular intervals and inconsistent data entry could have affected the Kaplan-Meier analyses. Finally, we were not able to account for patients lost to follow-up in the target population of those younger than 65 years. Despite these limitations, we think that most of the revisions and readmissions were captured correctly and provide the largest overview to date of this population.
Conclusion
TKA done in young and presumed active patients less than 65 years have excellent survivorship. Although racial disparities may exist with Black patients having higher revision rates than White patients, this difference did not reach statistical significance. Data from the AJRR show promising trends in TKA survivorship in this rapidly expanding patient population; however, long-term outcome studies are needed to confirm the validity of these findings and future utility of this comprehensive database.
Footnotes
Dr. Slover or an immediate family member is a member of a speakers' bureau or has made paid presentations on behalf of Pacira; serves as a paid consultant to Horizon Pharma; has received research or institutional support from Biomet and Smith & Nephew; and serves as a board member, owner, officer, or committee member of AAOS, AJRR Hip Society Steering Comm Member, American Association of Hip and Knee Surgeons, Hip Society, and PCORI Advisor Board Shared Decision Making. Dr. Schwarzkopf or an immediate family member has received IP royalties from Smith & Nephew; serves as a paid consultant to Intelijoint and Smith & Nephew; has stock or stock options held in Gauss surgical and Intelijoint; has received research or institutional support from Smith & Nephew; serves as a board member, owner, officer, or committee member of AAOS, and American Association of Hip and Knee Surgeons; and is on the editorial or governing board of Arthroplasty Today and Journal of Arthroplasty. Dr. Meftah or an immediate family member has received IP royalties from Innomed; serves as a paid consultant to Conformis and Intellijoint; has stock or stock options held in CAIRA surgical and Constance; serves as a board member, owner, officer, or committee member of ISTA; and is on the editorial or governing board of Orthopedics. Neither of the following authors nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Shah, and Mr. Cieremans.
Dr. Shah and Mr. Cieremans contributed equally to the manuscript as first authors.
Contributor Information
Akash Shah, Email: ak3shah@gmail.com.
James Slover, Email: james.slover@nyulangone.org.
Ran Schwarzkopf, Email: james.slover@nyulangone.org.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M: Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-785. [DOI] [PubMed] [Google Scholar]
- 2.Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T: Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. Acta Orthop 2010;81:413-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meehan JP, Danielsen B, Kim SH, Jamali AA, White RH: Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty. J Bone Joint Surg Am 2014;96:529-535. [DOI] [PubMed] [Google Scholar]
- 4.Long WJ, Bryce CD, Hollenbeak CS, Benner RW, Scott WN: Total knee replacement in young, active patients: Long-term follow-up and functional outcome: A concise follow-up of a previous report. J Bone Joint Surg Am 2014;96:e159. [DOI] [PubMed] [Google Scholar]
- 5.Mercuri JJ, Long WJ: What is the best option for young, active patients with knee arthritis? Ann Joint 2018;3:22. [Google Scholar]
- 6.Schalet BD, Rothrock NE, Hays RD, et al. : Linking physical and mental health summary scores from the veterans RAND 12-item health survey (VR-12) to the PROMIS(®) global health scale. J Gen Intern Med 2015;30:1524-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40:373-383. [DOI] [PubMed] [Google Scholar]
- 8.W-Dahl A, Robertsson O, Lidgren L: Surgery for knee osteoarthritis in younger patients. Acta Orthop 2010;81:161-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keeney JA: Total knee arthroplasty in the younger patient: Challenges and solutions. Orthop Res Rev 2015;7:33-38. [Google Scholar]
- 10.Argenson J-N, Boisgard S, Parratte S, et al. : Survival analysis of total knee arthroplasty at a minimum 10 years' follow-up: A multicenter French nationwide study including 846 cases. Orthop Traumatol Surg Res 2013;99:385-390. [DOI] [PubMed] [Google Scholar]
- 11.Parvizi J, Nunley RM, Berend KR, et al. : High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 2014;472:133-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meftah M, Ranawat AS, Sood AB, Rodriguez JA, Ranawat CS: All-polyethylene tibial implant in young, active patients a concise follow-up, 10 to 18 years. J Arthroplasty 2012;27:10-14. [DOI] [PubMed] [Google Scholar]
- 13.Meftah M, White PB, Ranawat AS, Ranawat CS: Long-term results of total knee arthroplasty in young and active patients with posterior stabilized design. Knee 2016;23:318-321. [DOI] [PubMed] [Google Scholar]
- 14.Karas V, Calkins TE, Bryan AJ, et al. : Total knee arthroplasty in patients less than 50 years of age: Results at a mean of 13 years. J Arthroplasty 2019;34:2392-2397. [DOI] [PubMed] [Google Scholar]
- 15.Zalavras CG, Lieberman JR: Osteonecrosis of the femoral head: Evaluation and treatment. J Am Acad Orthop Surg 2014;22:455-464. [DOI] [PubMed] [Google Scholar]
- 16.Singh JA, Kallan MJ, Chen Y, Parks ML, Ibrahim SA: Association of race/ethnicity with hospital discharge disposition after elective total knee arthroplasty. JAMA Netw Open 2019;2:e1914259. [DOI] [PMC free article] [PubMed] [Google Scholar]


