Abstract
Age-associated cardiovascular (CV) dysfunction increases the risk for CV diseases. Aerobic exercise training can improve CV function, but only a minority of adults meet aerobic exercise guidelines. High-resistance inspiratory muscle strength training (IMST) is a time-efficient lifestyle intervention that may promote adherence and improve CV function. However, further investigation is needed to translate IMST into the public health domain.
Keywords: Blood pressure, endothelial function, aging, aerobic exercise, dissemination and implementation, digital health
Summary for TOC:
Time-efficient, high-resistance inspiratory muscle strength training, a novel lifestyle intervention for improving cardiovascular aging, holds translational potential for improving public health.
INTRODUCTION
Aging is the primary risk factor for cardiovascular diseases (CVD), the leading cause of death in developed and developing societies (1). The number of older adults in the United States and other countries is expected to significantly increase in the coming years, leading to an increased burden of CVD (2). The increased risk for CVD with aging is attributable, in large part, to age-related changes in CV function (Figure 1). Key changes in CV function with advancing age include increases in blood pressure (BP), primarily systolic BP (SBP) after age 50 years, vascular endothelial dysfunction, and stiffening of the large elastic (carotid and aorta) arteries (3). The primary mechanisms underlying these age-related changes in CV function are oxidative stress and chronic low-grade inflammation (4–7).
Figure 1.
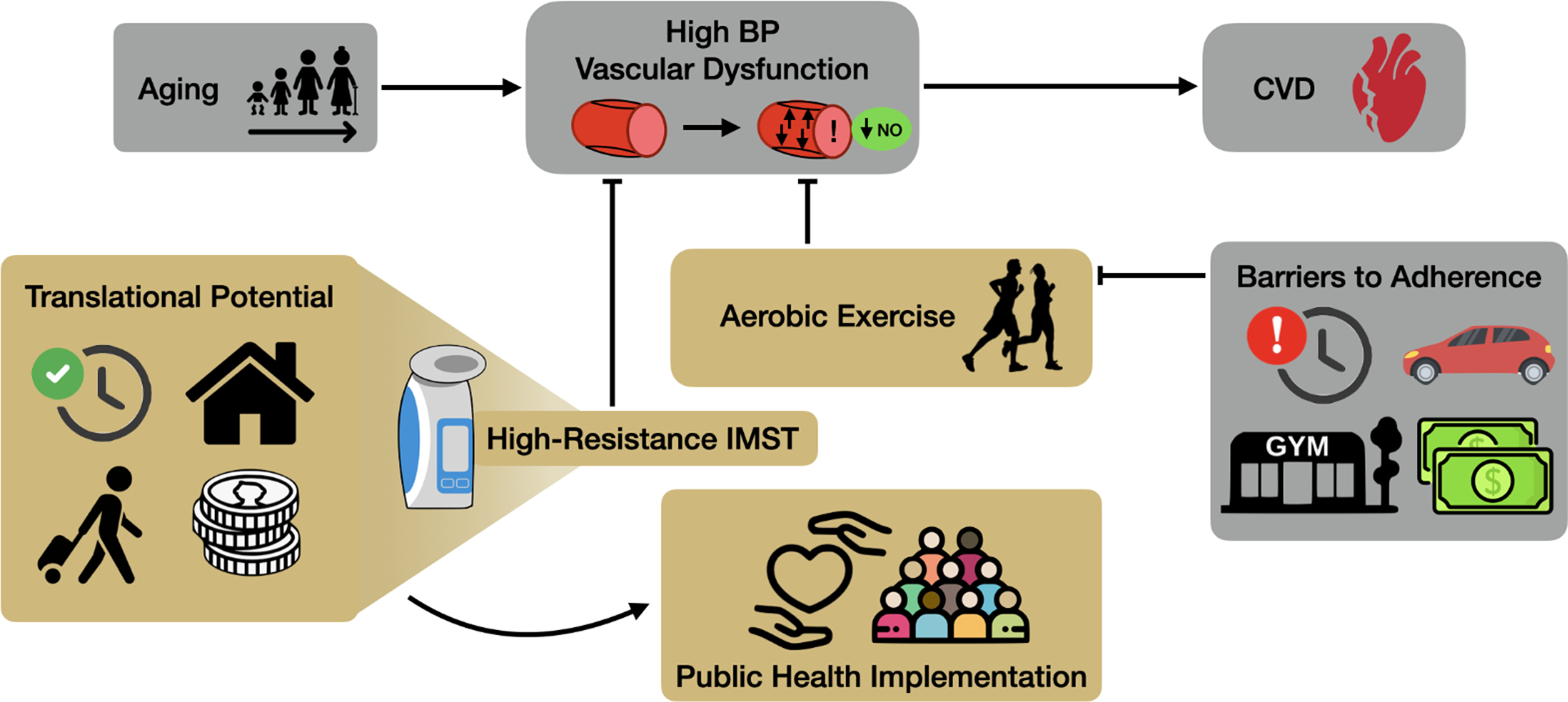
Conceptual model outlining the barriers for adhering to aerobic exercise and the potential characteristics of high-resistance inspiratory muscle strength training (IMST) that make it a promising intervention for public health implementation. Blood pressure (BP), cardiovascular diseases (CVD).
Oxidative stress is caused by excessive production of reactive oxygen species (ROS), particularly superoxide, in the face of an inadequate (or complete lack of a) compensatory increase in antioxidant defenses, most importantly antioxidant enzyme abundance (6, 8). The excessive superoxide directly reacts with nitric oxide (NO), a key vasodilatory and athero-protective molecule produced by the vascular endothelium (5, 8, 9), to form peroxynitrite (10). Thus, excess superoxide bioactivity leads to a reduction in NO bioavailability and an impairment in endothelial function. Excessive superoxide-induced oxidative stress also stimulates remodeling of the arterial extracellular matrix causing fragmentation of elastin fibers with compensatory deposition of collagen and the formation of structural protein crosslinking molecules, such as advanced glycation end products (3, 11).
Inflammation involves a chronic, low-grade increase in pro-inflammatory cytokines, such as C-reactive protein (CRP) and interleukin (IL)-6 (12, 13). A key mechanism contributing to chronic low-grade inflammation is the continuous activation of the pro-inflammatory transcription factor and master regulator of inflammation, nuclear factor κB (NFκB) (5, 6, 14).
Collectively, the changes in oxidative stress and inflammation with aging induce increases in SBP, vascular endothelial dysfunction, and large elastic artery stiffening. Age-related changes in SBP, vascular function and the associated mechanisms can be mitigated by so called “first-line” lifestyle strategies. Most prominent among these strategies is regular aerobic exercise training (5, 15). However, as discussed below, only a minority (<40%) of midlife and older adults (i.e., adults aged 50 years and older) presently meet guidelines for aerobic exercise due to multiple barriers to adherence (16, 17). Therefore, there is a need for novel interventions that improve CV function with aging.
The purpose of this Perspective for Progress is to discuss the current knowledge and future research directions regarding high-resistance, low-repetition inspiratory muscle strength training (IMST), a novel, time-efficient form of physical activity that utilizes the respiratory muscles and may improve CV function with aging (18, 19). Because it poses a minimal time burden, high-resistance IMST holds particular promise for translation into the public health domain and for use in rehabilitation settings. To provide context and contrast for future research on IMST, we will start by briefly discussing aerobic exercise, an established form of physical activity that has been the subject of intense investigation along the entirety of the basic science-to-public health research spectrum. We will then review available evidence on high-resistance IMST for improving CV function with aging, before highlighting the potential synergy between IMST and digital health technologies for accelerating the translation of IMST into the public health domain. We will conclude by providing our view on important future research directions on this novel lifestyle intervention.
AEROBIC EXERCISE FOR IMPROVING CARDIOVASCULAR FUNCTION WITH AGING
Moderate-intensity continuous aerobic exercise is defined as sustained, rhythmic movements of large muscle groups resulting in increases in heart rate and respiration. Moderate-intensity aerobic exercise can maintain and improve CV health with aging, as well as decrease the risk for CVD across the lifespan (Figure 1). On average, aerobic exercise lowers SBP by 2 to 8 mmHg, with the largest effect evident in those individuals with the highest initial SBP (i.e., stage II hypertension) (20, 21).
Regular aerobic exercise also improves vascular endothelial function in midlife and older men by increasing NO bioavailability, secondary to reductions in superoxide-associated suppression of endothelial function and decreased inflammation (22–25). However, estrogen-deficient postmenopausal women do not respond as consistently or robustly to aerobic exercise training for improving endothelial function as age-matched men (26). This is likely due, in part, to the significant reduction in circulating estrogen following the menopausal transition. As such, aerobic exercise trials that have assessed endothelial function via brachial artery flow-mediated dilation (FMDBA) typically demonstrate no benefit of physical activity on endothelial function in estrogen-deficient postmenopausal women, whereas the same exercise stimulus appears to evoke improvements in postmenopausal women with circulating estrogen similar to pre-menopausal concentrations as a result of sex hormone replacement (27–29).
Results from cross sectional studies comparing sedentary to endurance-trained middle-aged and older adults suggest that years of vigorous aerobic exercise training mitigates the age-related increase in arterial stiffness (30–33). However, results from aerobic exercise interventions initiated in midlife are somewhat less clear. Although aerobic exercise interventions in midlife/older men and postmenopausal women have demonstrated improvements in carotid artery compliance (30, 32), improvements in aortic stiffness measured via carotid-femoral pulse wave velocity have been less consistently documented (34–36). These inconsistencies may be due to differences in aerobic exercise interventions and study populations, though overall it appears aerobic exercise is modestly effective at reducing large elastic artery stiffness, especially aortic stiffness, in midlife and older adults (36, 37).
Current physical activity guidelines recommend that older adults participate in at least 150 minutes of moderate-intensity, or 75 minutes of vigorous intensity, aerobic exercise per week (38). Despite the efficacy of aerobic exercise for exerting numerous CV benefits, over 60% of midlife and older adults in the United States do not meet these physical activity guidelines (16, 17). The most cited barrier that prevents midlife/older adults from adhering to physical activity guidelines is lack of time (39–41). Other common barriers that limit adherence include physical limitations, financial cost, lack of appropriate exercise facilities or equipment, lack of intrinsic motivation, transportation limitations, knowledge gaps on how to implement aerobic exercise, and an overall aversion to aerobic exercise training (40–46) (Figure 1). As such, additional strategies are needed to promote adherence to aerobic exercise guidelines among midlife and older adults.
DIGITAL HEALTH TECHNOLOGIES AND AEROBIC EXERCISE
Given the considerable barriers for adherence to aerobic exercise guidelines, digital health technologies, such as wearable activity tracking devices and mobile health (mHealth) apps, have been pursued as potential tools to promote higher levels of physical activity among midlife and older adults. Digital health technologies are promising as they may overcome barriers to physical activity such as facility access, transportation, geographic location, and availability of community-based programs (47). Select exercise interventions administered via mHealth technologies increase physical activity levels and reduce sedentary behaviors in individuals across the lifespan (48, 49), as well as in older populations (50). There is a wide range of mHealth interventions for promoting physical activity in midlife/older adults. Examples of these diverse strategies include use of accelerometers and pedometers, text messaging reminders, internet-delivered interventions, interactive applications, exergaming, and online professional and peer support (51, 52).
In general, physical activity monitors, such as accelerometers and pedometers increase physical activity by 1000 to 1500 steps per day over short-term intervention periods (50). Accelerometers appear to increase physical activity to a greater extent than pedometers, which may be due to differences in the accuracy of step detection between these types of devices (53). Internet-based (eHealth) physical activity interventions also increase steps per day, minutes of moderate-to-vigorous physical activity per day, and overall minutes per week of physical activity (54). Importantly, theory-based interventions (e.g., those interventions that increase motivation and include behavior change techniques) are more effective, regardless of the method of administration (55).
Others have shown positive trends, but no significant effects, of app-based interventions on improving physical activity levels in older adults, likely due to the small sample sizes of most current trials (56, 57). App features such as syncing to smartwatches or activity monitors, instructions, goal setting, self-monitoring, and social support are commonly successful features in mHealth-based interventions in which trends for improving physical activity levels are observed (56, 57).
Overall, digital health technologies have shown benefits for promoting physical activity in older populations, increasing physical activity on average by 28% compared to control groups without digital health support tools (55). This has led certain working groups, such as the Community Preventive Services Task Force, to recommend the use of digital health technologies to deliver physical activity interventions in adults aged 55 years and older. However, even with the ability of digital health technologies to increase physical activity over initial levels, midlife and older adults still struggle to accrue enough activity to meet guideline recommendations (55). This indicates that there are additional barriers to performing adequate amounts of aerobic exercise, even when digital health technologies are in use.
Unexplained heterogeneity, bias, and lack of rigorous methodology limit the ability to compare studies and draw strong conclusions regarding the effectiveness of physical activity monitors and digital health technologies for increasing physical activity in older populations (57). Larger scale trials with longer-term intervention and follow-up durations are warranted to provide a better understanding of mHealth physical activity interventions for improving exercise adherence in midlife/older adults (53, 56). Additionally, studies that employ rigorous and objective measures of adherence to home-based mHealth exercise interventions for midlife/older adults are necessary.
HIGH-RESISTANCE INSPIRATORY MUSCLE STRENGTH TRAINING FOR IMPROVING CARDIOVASCULAR FUNCTION
IMST is an alternative form of physical training that isolates the inspiratory muscles by requiring individuals to perform repeated inhalations against an external resistance while exhalation is unimpeded. IMST primarily utilizes the diaphragm and accessory respiratory muscles including the intercostal, scalene and sternocleidomastoid muscles (Figure 2). IMST is distinct from other forms of breathing exercises, such as respiratory muscle training which involves resistance to both inhalation and exhalation, or pursed-lip breathing where resistance is self-produced by narrowing the airway.
Figure 2.
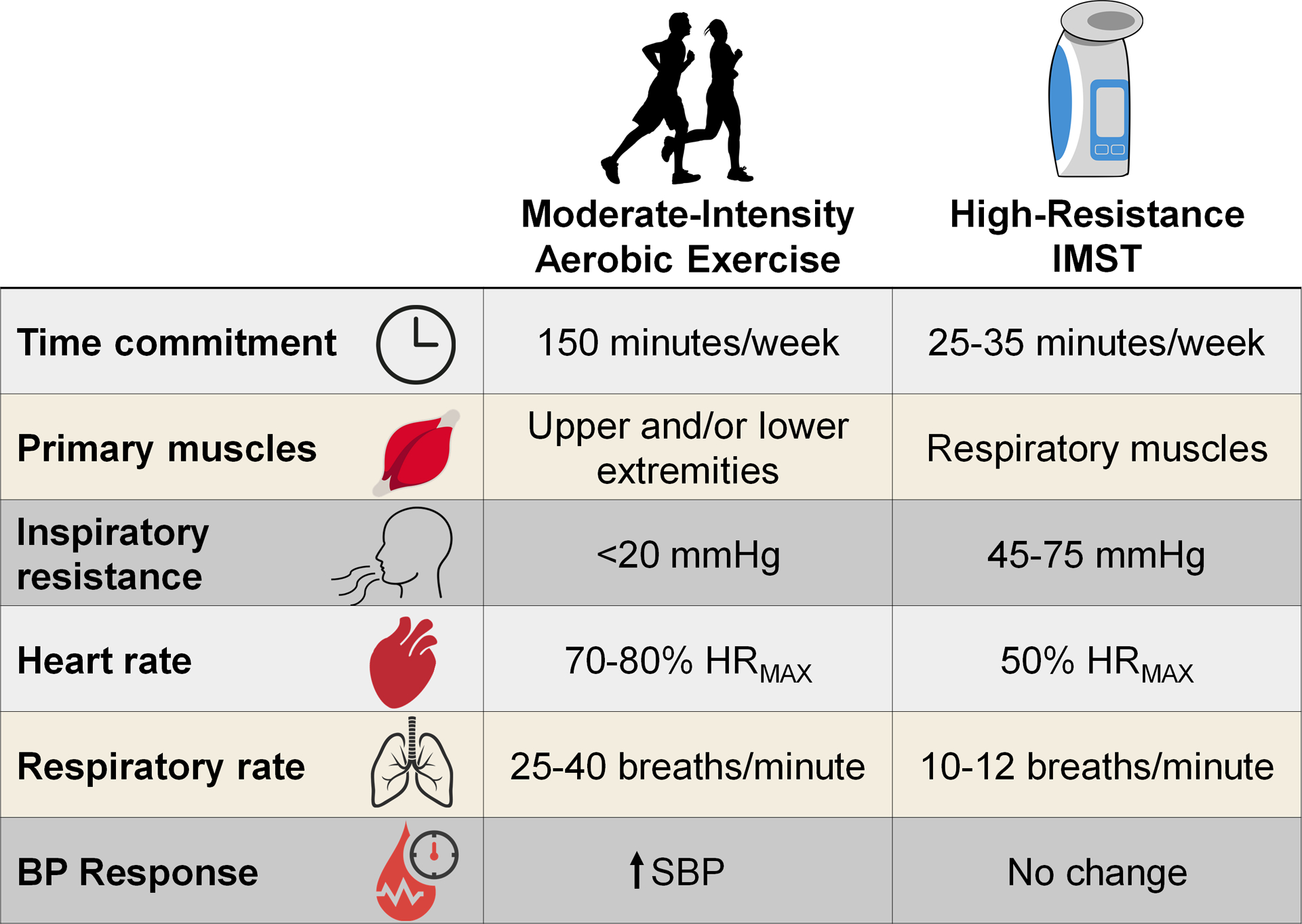
Training characteristics and cardiorespiratory responses to a single bout of high-resistance inspiratory muscle strength training (IMST) or moderate-intensity aerobic exercise. Maximal heart rate (HRMAX), systolic blood pressure (SBP).
Most studies investigating the CV health benefits of IMST have utilized low-resistance, high-repetition paradigms, in which users inspire against a resistance at or near 30% of their individual maximal inspiratory pressure (PIMAX) (18, 19). A primary weakness of low-resistance, high-repetition IMST is that it requires a similar overall time commitment to that of moderate-intensity physical activity guidelines (i.e., ~150 minutes/week). As time-availability is the most cited barrier to achieving healthy lifestyle strategies (39–41), low-resistance IMST interventions are unlikely to elicit high rates of adherence in a real-world setting. The purported CV health benefits of low-resistance IMST have been reviewed recently (18) and thus will not be discussed in further detail.
Given the important role of time-availability for meeting healthy lifestyle guidelines, the potential of time-efficient (i.e., ~30 minute/week time commitment) interventions for promoting healthy CV aging is becoming a topic of increasing interest (19). High-resistance, low-repetition IMST is an emerging variation of the traditional, low-resistance IMST paradigm that can be accomplished with minimal time burden.
Though no standard definition has been established, high-resistance IMST most often refers to regimens utilizing a level of resistance equivalent to ~75% of an individual’s PIMAX (18). This level of intensity allows high-resistance IMST to be completed in as little as 5 minutes/day, making it a time-efficient intervention with the potential to promote adherence. IMST is performed with small, hand-held devices, which are ideal for use at home and during travel. There are consumer-available IMST devices that are relatively affordable when compared to gym memberships or other pieces of exercise equipment. Thus, high-resistance, low-repetition IMST has multiple characteristics that may help promote adherence (Figure 1). As such, high-resistance IMST for promoting healthy CV aging will be the focus of the remainder of this Perspective for Progress.
High-resistance IMST provides a physiological stimulus that is distinct from moderate-intensity aerobic exercise (Figure 2). Indeed, the level of inspiratory resistance attained during high-resistance IMST is ~2–4 times larger than those achieved during aerobic exercise, though the respiratory rate is appreciably lower during high-resistance IMST compared to aerobic exercise (58–61). Compared to aerobic exercise, a single bout of high-resistance IMST results in a smaller increase in heart rate and a minimal change in SBP (62–64). Therefore, high-resistance IMST is not simply mimicking the acute cardiorespiratory effects of moderate-intensity aerobic exercise but is instead a unique acute physiological stimulus and, when performed regularly, form of physical training.
High-resistance IMST for lowering blood pressure
The most established CV benefit of high-resistance IMST is for lowering casual (resting, seated) BP (Figure 3). Initial efficacy of high-resistance IMST for lowering BP was demonstrated by Bailey and colleagues, who demonstrated that 6 weeks of high-resistance IMST, consisting of 30 breaths (~5 minutes) per day, 5 days per week, at an intensity of 75% PIMAX, lowered casual SBP by 10 mmHg and casual diastolic BP (DBP) by 6 mmHg in young adults with normal BP at baseline (58). Importantly, in this same study, BP was unchanged in a group of young adults randomized to perform the same protocol but against a minimal inspiratory resistance (58). The study also demonstrated that large excursions in lung volume with low resistance, when employed with this 30-breaths per day protocol, are inadequate for lowering BP. Thus, the necessity of high inspiratory resistance to facilitate the benefits of IMST in a time-efficient manner were initially established.
Figure 3.
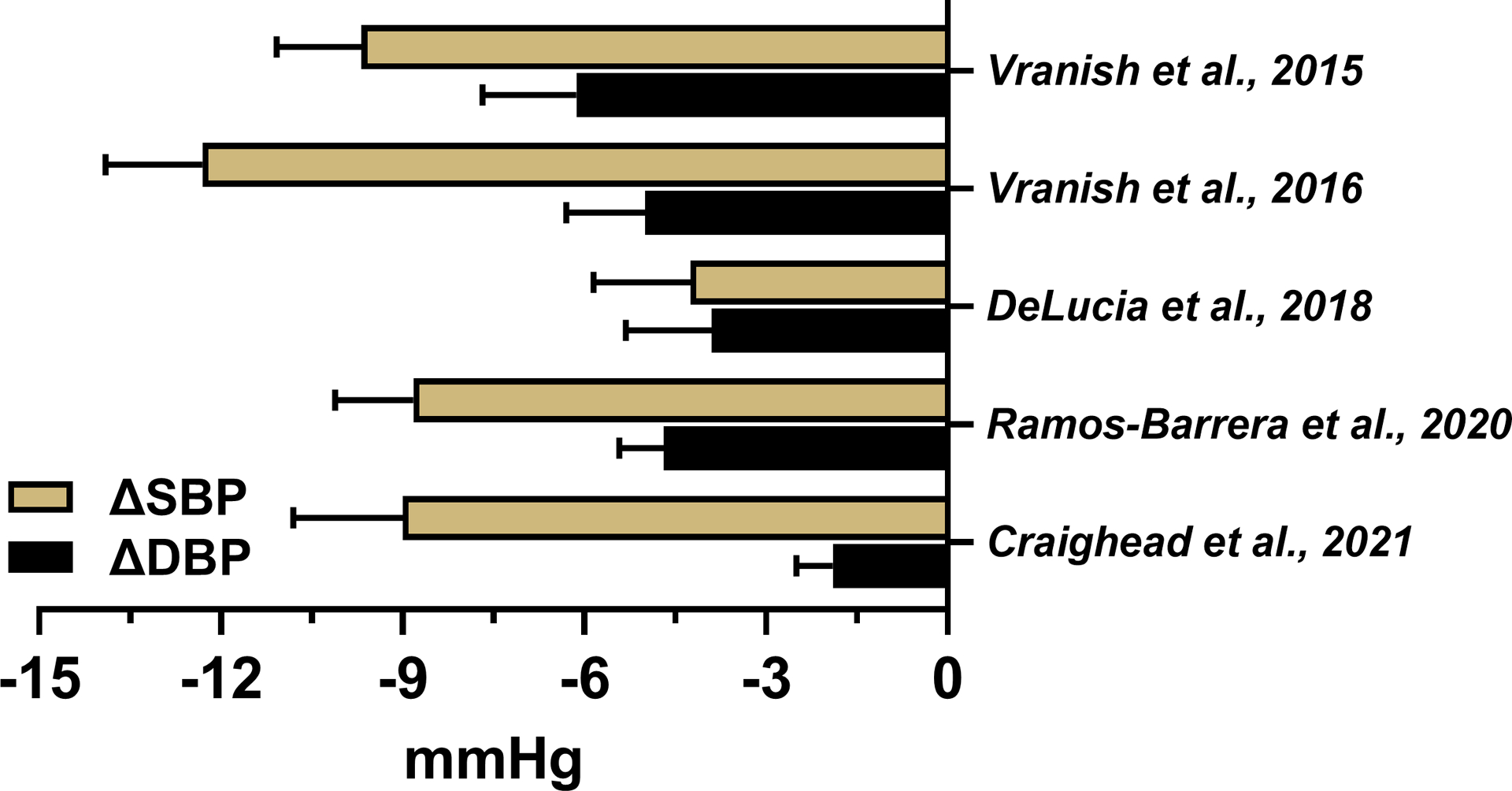
Summary of the changes in systolic blood pressure (SBP) and diastolic BP (DBP) in the high-resistance inspiratory muscle strength training groups from available randomized clinical trials.
Next, the Bailey laboratory translated their 30-breaths per day high-resistance IMST protocol to patients with obstructive sleep apnea. In these patients, 6 weeks of high-resistance IMST (75% PIMAX, 6 days per week) lowered SBP by 12 mmHg and DBP by 5 mmHg; no change was observed in the low-resistance (15% PIMAX) sham control group (65). Dr. Bailey’s group has since replicated their initial findings in additional 6-week long interventions in separate cohorts of young healthy adults (SBP −4 mmHg; DBP −4 mmHg) (66) and patients with obstructive sleep apnea (SBP −9 mmHg; DBP −5 mmHg) (67).
Using the protocol pioneered by Bailey and colleagues, our laboratory recently demonstrated that 6 weeks of high-resistance IMST (75% PIMAX, 30 breaths per day, 6 days per week) lowered casual SBP by 9 mmHg and DBP by 2 mmHg in a group of otherwise healthy midlife and older adults with an initial SBP above 120 mmHg (68). Importantly, casual BP was measured 24–48 hours following the last session of IMST, precluding acute effects from influencing our results. A unique feature of our study was that a majority of participants returned for reassessment after abstaining from IMST for 6 weeks in order to determine if there were any persistent effects of the intervention on BP. SBP remained 7 mmHg lower than baseline levels at this follow-up timepoint, suggesting the SBP-lowering effects of high-resistance IMST may be sustained at least for several weeks (68). BP tends to rise quickly after abstaining from aerobic exercise or withdrawing prescribed pharmacotherapy. Thus, if confirmed in additional studies, the persistent BP-lowering effects of high-resistance IMST may offer an additional advantage over other antihypertensive therapies as it may require only intermittent training periods, better promoting longer-term adherence.
The consistently observed reductions in casual BP across the 6-week high-resistance IMST interventions performed by Dr. Bailey and our laboratory (Figure 3) are similar or greater in magnitude than the changes in BP that tend to be observed following aerobic exercise training (20, 21). These reductions in BP were achieved with a much smaller time burden in comparison to standard aerobic exercise. The reductions in BP are also similar to those observed following treatment with first-line antihypertensive pharmacotherapies (69–71). Importantly, reductions in casual SBP (4–12 mmHg) and DBP (2–6 mmHg) observed across these studies are clinically significant, with an expected reduction in CVD risk of ~30% if sustained long-term (72). The ability of IMST to lower BP even in young adults with normal BP at baseline could be clinically meaningful as progressive, age-related increases in SBP begin in young adulthood and result in above-normal SBP in a majority of adults prior to midlife (20, 73, 74). Thus, the efficacy of IMST for lowering SBP in this group could help maintain normal SBP levels into later life.
Mean 24-hour, daytime and nighttime BP measured via ambulatory monitoring are additional CVD risk factors that offer insight into BP status beyond what is obtained through clinic-based casual BP measurements (75, 76). The effects of high-resistance IMST on ambulatory BP measures were assessed in two of the trials described above. First, Bailey and colleagues observed a nighttime-specific reduction in SBP of 12 mmHg following 6 weeks of high-resistance IMST in patients with obstructive sleep apnea (67). This patient group exhibits sleep-disordered breathing which leads to elevations in nighttime SBP. Thus, the nighttime-specific reduction in SBP in this group may reflect the influence of IMST on their unique pathophysiological state. Similarly, in our IMST pilot study in midlife/older adults, we observed a 4 mmHg reduction in mean 24-hour SBP, driven by equivalent reductions in daytime and nighttime SBP, such that 24-hour SBP was significantly lower compared to the low-resistance sham control group after 6 weeks of high-resistance IMST in our cohort of generally healthy midlife and older adults (68). Combined, these findings suggest high-resistance IMST may improve ambulatory measures of BP sampled over a 24-hour period in addition to improving casual BP assessed at a single point in time.
High-resistance IMST for improving vascular function
Vascular endothelial function tends to decline with aging and is associated with increased CVD risk (77, 78). To our knowledge, our pilot trial in midlife/older adults is the only trial to date to assess the effect of high-resistance IMST on endothelial function. We observed a 45% improvement in endothelial function, assessed via FMDBA, after 6 weeks of high-resistance IMST, with no change in the sham control group, in our study (68). In contrast to AE training (26, 27, 29), equivalent improvements in endothelial function were observed in the estrogen-deficient postmenopausal women and midlife/older men enrolled in our study (68). Though caution is warranted given the small subgroups, this finding suggests high-resistance IMST may overcome a limitation of aerobic exercise for improving vascular endothelial function in estrogen-deficient postmenopausal women, as discussed above. The magnitude of improvement in FMDBA we observed (~2.5Δ% units) is likely clinically significant, as a 1Δ% unit higher FMDBA is associated with an 8–13% lower risk for CVD (78–82).
High-resistance IMST does not appear to improve large elastic artery stiffness, measured either as carotid-femoral pulse wave velocity or carotid artery compliance, in young or midlife/older adults (68, 83). However, it usually takes a treatment period of at least 3 months for healthy lifestyle strategies to change large elastic artery stiffness (36). Current studies have only used 4- or 6-week intervention durations. Thus, large elastic artery stiffness should be assessed in longer duration trials of high-resistance IMST to further assess the efficacy of this intervention for improving this important measure of age-related vascular dysfunction.
Potential mechanisms of high-resistance IMST for improving CV function
Currently, there is limited information on potential mechanisms through which high-resistance IMST improves CV function, with available evidence coming from a heterogenous group of studies. In healthy young adults, IMST reduces BP by lowering systemic vascular resistance without changing resting heart rate or cardiac output (66). This suggests that high-resistance IMST likely lowers BP by acting primarily on the vasculature, but additional research is needed to confirm these observations in patient groups and older adults.
We used an innovative ex vivo cell culture technique to assess the effect of high-resistance IMST on oxidative stress and NO bioavailability. Endothelial cells were cultured in serum obtained from midlife/older adults before and after 6 weeks of high-resistance IMST or low-resistance sham training. Serum samples collected after IMST reduced endothelial cell superoxide production by ~25–35% relative to baseline and serum from the sham control group (68). In addition, serum obtained post-IMST increased markers of activation for the NO-producing enzyme, endothelial NO synthase, by ~75% compared to serum sampled pre-IMST (68). This increase in activation of endothelial NO synthase was associated with a corresponding ~10–15% increase in NO production in endothelial cells cultured with serum obtained following the high-resistance IMST intervention compared to pre-intervention and sham training (68). Combined, these ex vivo results from our pilot trial suggest high-resistance IMST may improve CV function, in part, by inducing beneficial changes to factors in the circulation that decrease oxidative stress and increase NO bioavailability. These findings remain to be confirmed, and expanded upon, in subsequent trials.
Results from multiple trials suggest IMST may reduce chronic, low-grade inflammation, though findings are varied. We observed reductions in plasma CRP, a marker of systemic inflammation, after 6 weeks of high-resistance IMST in our pilot trial in midlife and older adults (68). Similarly, moderate-intensity IMST (50% PIMAX) reduced plasma CRP and soluble TNFα receptor 2 in patients on hemodialysis (84, 85). Conversely, a similar 8-week, moderate-intensity IMST (50% PIMAX) trial in healthy older adults observed no changes in plasma cytokine concentrations (86). It is likely that larger sample sizes or more sensitive measures will be needed to interrogate the effects of high-resistance IMST on low-grade inflammation.
There also are inconsistent results on the effect of high-resistance IMST on sympathetic nervous system activity, an additional mechanism linked to above-normal BP. Bailey and colleagues observed that 6 weeks of high-resistance IMST was sufficient to lower sympathetic activity, measured either directly via muscle sympathetic nerve activity or indirectly using plasma concentrations of norepinephrine, in patients with obstructive sleep apnea (65, 67). However, 6 weeks of high-resistance IMST did not change plasma norepinephrine concentrations in our trial in generally healthy midlife/older adults (68). A potential explanation for these disparate findings is that obstructive sleep apnea is associated with elevated baseline sympathetic nervous system activity (87).
Additionally, some respiratory muscle strength training interventions (i.e., those not falling under the definition of high-resistance IMST) have reported reductions in sympathetic activity in other patient groups, such as patients with heart failure or diabetes mellitus, though these findings are inconsistent (88). Thus, the direct effect of IMST on the neural control of the circulation is unclear currently. It is possible that high-resistance IMST may only impact sympathetic nervous system activity in those with significantly elevated levels at baseline. Moreover, arterial baroreflex control of heart rate was unchanged following 6 weeks of high-resistance IMST in young adults (66) and patients with sleep apnea (67). These findings suggest high-resistance IMST does not influence cardiac baroreflex sensitivity in these select groups, though investigation in other populations is warranted.
Of note, the acute impact of a single bout of IMST or aerobic exercise on BP differ, as aerobic exercise is associated with a period of post-exercise hypotension (89) that is not observed with high-resistance IMST (62). This further suggests that IMST is a unique intervention with differing physiological effects from aerobic exercise. However, physical activity levels across high-resistance IMST interventions have not yet been documented. Thus, whether the benefits of IMST occur independent of changes in activity levels cannot be fully confirmed.
Overall, high-resistance IMST has shown promise for lowering casual BP and potentially improving other measures of CV function across multiple small-scale pilot trials. These encouraging early results have stimulated interest in IMST and led to the initiation of multiple larger randomized controlled trials across various populations with above-normal BP (e.g., NCT04848675, NCT05000515, NCT04932447 (61), NCT04911491). The results from these ongoing trials will greatly increase our understanding of the efficacy and mechanisms of action of IMST for improving CV function in the context of aging and common age-related diseases.
TRANSLATIONAL POTENTIAL OF HIGH-RESISTANCE INSPIRATORY MUSCLE STRENGTH TRAINING
The ability of high-resistance IMST to improve CV function while overcoming multiple barriers to adherence suggests it has potential for public health implementation. However, investigation of high-resistance IMST has been limited to the clinical research setting. Initial translational evidence for IMST outside of the controlled research environment is available for low- to moderate-resistance IMST protocols of various durations. Accordingly, for the purposes of this review, we will summarize findings on adherence, safety, tolerability, feasibility and/or implementation outcomes from home-based, low- or moderate-resistance IMST trials, as these studies provide key insights regarding potential efficacy and challenges for translating high-resistance IMST to the public health arena. We acknowledge that dissemination, implementation, and full-scale public health translation have their own frameworks and deep science structure. In this Perspective for Progress, the focus is on translating initial findings on physiological efficacy and providing a broad overview of future areas of research. As such, a full discussion of framework models is outside the scope of this review.
An important aspect of translating IMST out of the clinical setting and into the public health sector is an understanding of the methods by which investigators could track the progression of individuals through an IMST intervention without study team interaction. Some studies have had participants perform completely unsupervised, home-based IMST with adherence self-reported through diaries (90–93). Although a useful design in its simplicity, self-reporting adherence in physical diaries runs the risk of subjects losing their diaries, or incorrectly or incompletely filling them out, as has been reported in an IMST trial using this strategy (94). Other studies have scheduled weekly phone calls with subjects to track adherence, monitor progress, and assist with altering the training intensity for those in the experimental groups (92, 93, 95). Regular phone calls allow researchers to track participants more accurately through the intervention compared to training diaries. However, participants may feel more accountable when they are required to regularly report intervention adherence to investigators and therefore may be more motivated to adhere to IMST than they otherwise would under unsupervised settings. Accordingly, regular contact with the research team, even when done remotely, may bias participant adherence and limit the translational knowledge gained from this type of design.
To overcome these issues, IMST training devices that automatically record and store training data have been utilized. Internal data storage allows for objective recording of intervention adherence and progression (e.g., changes in training load or achieved inspiratory volumes during training sessions) (95, 96). Although these recordings overcome certain research limitations associated with self-reported information, objective documentation of training data does not help with IMST translation and implementation per se.
Web-based platforms have been utilized to implement IMST outside of the clinic. In one study, patients with chronic obstructive pulmonary disease (COPD) were assigned to 12 weeks of home-based IMST with or without internet-based feedback. After each training session, the internet-based feedback group self-reported their rating of perceived exertion; in response, these participants would receive suggestions for adjusting their training intensity. Participants in the no-feedback group reported adherence via paper diaries and did not receive training-related suggestions. Although no direct, verbal communication was made between participants and investigators, those in the web-based feedback group exhibited higher rates of adherence to IMST than those not receiving feedback (87% vs. 67% of prescribed training sessions completed) (97). This finding supports the role of accountability via eHealth strategies for promoting adherence to home-based IMST.
Currently, studies investigating the efficacy of time-efficient, high-resistance IMST have used either daily or weekly in-person instructional and supervised sessions (58, 65–68). These studies have all demonstrated the excellent safety and tolerability (i.e., ability to tolerate any side effects to maintain participation) profile of high-resistance IMST. However, due to the regular supervision of training sessions, the feasibility of users effectively progressing through an unsupervised home-based high-resistance IMST intervention is unknown.
Importantly, small feasibility trials for home-based, moderate-resistance IMST were performed in clinical populations (96, 98), and provided initial insight on the ability of individuals to perform an IMST intervention without researcher oversight. In one study, adults with stable COPD performed 8 weeks of moderate-resistance IMST (60% PIMAX, 30 breaths twice per day, 5 days per week), with one session supervised in person. Following this 8-week run in period, participants continued training completely unsupervised, 3 days per week, for an additional 18 weeks (96). Seven of the 10 subjects enrolled completed the entire intervention. IMST was found to be acceptable, with most participants expressing confidence in their skill and ability to use the IMST device and perform the intervention. Additionally, adherence during the unsupervised sessions was high (91% of prescribed training sessions completed), but ranged from 22–162% (96), indicating low use by certain participants but a desire to perform more than the prescribed number of training sessions by other participants. This suggests home-based IMST is feasible in this population and warrants a larger trial.
In another trial assessing the feasibility and tolerability of IMST in patients recovering from pneumonia, subjects performed IMST twice daily for 9 weeks at 50% PIMAX with weekly supervised training sessions. IMST was safe, with side effects of training reported in only 15 of 1183 training sessions. Importantly, side effects did not prevent further training, indicating the IMST intervention was tolerable. Patient-reported acceptability of IMST, i.e., finding IMST to be an attractive or agreeable intervention, was 99.4% (98).
In studies reporting adherence to home-based IMST interventions, participants in the experimental (IMST) groups completed 76–91% of assigned training sessions (90, 92, 94, 96, 97). Notably, the populations enrolled in these studies included healthy older adults, adults with stable COPD, patients with heart failure, and stroke survivors. This broad range of populations investigated suggests implementation of home-based IMST is feasible across groups with varying health statuses and physical limitations.
Finally, clinic-based studies assessing time-efficient, high-resistance IMST have reported high rates of adherence, with at least 94% of prescribed training sessions completed (58, 65–68). However, whether adherence to high-resistance IMST remains high when performed at-home, without regular supervision, requires investigation. Critically, whether unsupervised, high-resistance IMST programs can effectively improve CV function has not been determined.
Potential for digital health technologies to advance IMST
Although available studies support the translational potential of high-resistance IMST as an adherable intervention, a crucial limitation to date is that all current studies have used investigator-led instruction on how to perform IMST. Indeed, that there is no current route for administering and disseminating high-resistance IMST outside of the clinical research setting is a serious limiting factor for public health translation.
As discussed above, digital health technologies are effective for delivering aerobic exercise interventions and are acceptable for use by midlife and older populations (47). Though not yet tested, digital health technologies also are likely to be effective tools to deliver and monitor high-resistance IMST interventions. For example, a majority of adults in America, including over three quarters of midlife and older adults, own a smartphone (99), which is kept on their person at most times. As such, high-resistance IMST could effectively be delivered through a smartphone app without appreciably altering user burden.
However, even with increasing smartphone ownership, there will still be barriers to technology uptake among midlife/older adults. Internet connection issues could pose a barrier to adherence. In fact, ~25% of adults aged 50 years and older report having problems connecting to the internet. However, a greater proportion of adults under 50 years of age (33%) report internet connection issues (100). This suggests internet connection is a general infrastructure barrier and not an issue of aging per se. Barriers related to technology adoption, such as physical and mental challenges or lack of comfort or familiarity with technology, also can impact older adults (aged ≥65 years), with visual, cognitive, motor skills and literacy barriers becoming more prevalent with increasing age (101, 102). Recently, there has been a trend towards teaching older adults technology skills (103) and more focus has been placed on user-centered technology design for older adults (47, 104). Incorporating these steps focused on increasing usability by older adults will be critical in the app design phase.
IMST devices that wirelessly pair with a smartphone app to deliver a high-resistance IMST intervention could be developed. Such apps could include features such as video instructions for IMST device use and training technique, training prompts or reminders, wireless data transfer between the app and device, and a user-tailored algorithm to automatically instruct and guide users through a high-resistance IMST intervention for improving CV function. The app could also pair with wireless home BP monitors and integrate this information with the IMST data to track changes in BP across the intervention period and notify users if their BP classification changes (e.g., if SBP dropped from the stage 1 hypertension into the elevated range).
While such automated digital features will aid with effective uptake of high-resistance IMST, it is important to consider that reliance on expensive equipment has the potential to exacerbate current health disparities. Therefore, it will be crucial that any eventual app for delivering high-resistance IMST effectively works with more affordable, mechanical (i.e., non-digital) IMST devices that do not have the ability to automatically sync with a smartphone. Individuals utilizing a mechanical IMST device will have to manually input training information into the accompanying smartphone app, which may decrease convenience. However, the cost difference between digital and mechanical IMST devices can be substantial, so the ability to use more affordable, mechanical IMST devices in conjunction with an app will reduce overall financial burden and make IMST accessible to a broader range of users.
Overall, leveraging the growing field of digital health technologies is likely to be an effective way to speed the dissemination and implementation of high-resistance IMST from the clinical research setting into the public health domain as a feasible strategy for improving CV aging.
Future directions for translating IMST towards public health
Available evidence suggests high-resistance IMST performed in a clinical research setting is efficacious for improving CV function, particularly lowering SBP, and for promoting adherence in midlife and older adults. These encouraging initial results support initiating further translational research on high-resistance IMST with the ultimate goal of improving public health (Figure 4).
Figure 4.
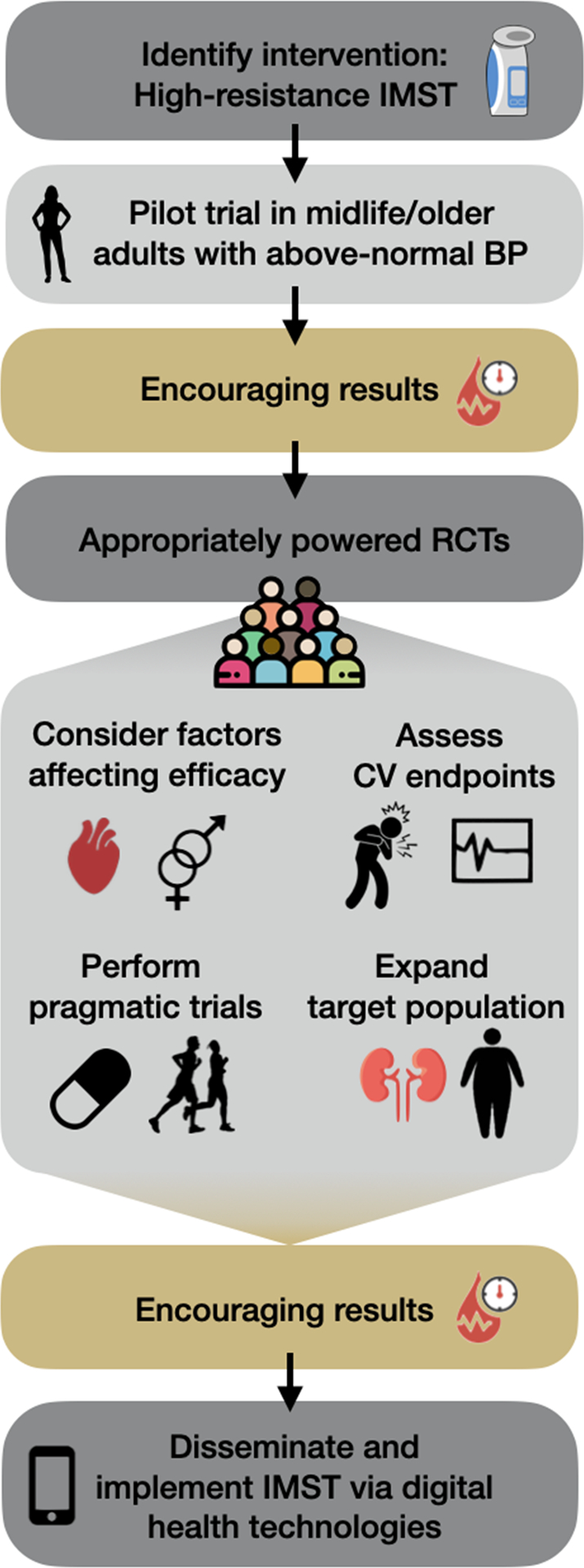
Translational potential for progress of high-resistance inspiratory muscle strength training (IMST) towards public health implementation. Blood pressure (BP), randomized controlled trial (RCT), cardiovascular (CV).
As most studies to date have been small, proof-of-concept trials, the next step is to conduct larger, appropriately powered safety and efficacy trials to more definitively establish the CV health benefits of high-resistance IMST. Such larger trials in midlife and older adults (NCT05000515, NCT04848675), patients with obstructive sleep apnea (NCT04932447) (61), and patients with chronic kidney disease (NCT04911491) have recently begun and will start to fill this knowledge gap. However, trials in additional patient populations with BP-associated risk, such as patients with glaucoma or mild cognitive impairment, also are warranted. While the focus has primarily been on midlife and older adults, high-resistance IMST should also be considered for use in children with conditions associated with above-normal BP and increased lifetime risk of CVD, such as those with youth-onset type 2 diabetes mellitus. Additionally, as high-resistance IMST only requires use of the respiratory muscles, it may be accessible for groups with physical limitations that restrict whole body exercise. Accordingly, high-resistance IMST should be assessed for improving CV function in those with spinal cord injury, orthopedic injuries, frail older adults, adults with excessive adiposity, or other conditions associated with elevated risk for CVD due to increased sedentary behavior.
A majority of ongoing trials are all using a very similar high-resistance IMST paradigm (i.e., 30 breaths per day, 75% PIMAX, 5–6 days per week). However, whether this commonly prescribed protocol represents the most efficacious high-resistance, low-repetition IMST intervention for improving CV function has not been determined. Additional trials will be needed to identify the optimal high-resistance IMST protocol that elicits the greatest CV health benefits, or find the minimal effective dose of high-resistance IMST for improving CV function, by modulating the training frequency, training time of day, intensity, and number of breaths per session. The larger sample sizes afforded by these clinical trials will also provide key information on the effectiveness of high-resistance IMST for improving CV function in important subgroups. For example, larger clinical trials should enable us to gather evidence as to whether the effectiveness of IMST varies based on sex, initial BP, medication status, or whether other important subject characteristics influence responsiveness.
If the efficacy of high-resistance IMST for improving CV aging is established in these appropriately powered clinical trials, the next step would be to perform pragmatic studies examining the comparative or added effectiveness of IMST to established therapies. Indeed, it will be important to compare the BP-lowering effects of high-resistance IMST to established lifestyle strategies, such as aerobic exercise or dietary sodium restriction, and to approved pharmacotherapies, to determine the equivalence (or superiority/inferiority) of IMST to current interventions. As high-resistance IMST is a time-efficient intervention, it also holds promise as an additive therapy. Thus, similar trials where IMST is performed in addition to current lifestyle strategies to see if there are added CV health benefits, will be important. Additionally, trials adding IMST to pharmacotherapy regimens can determine whether IMST decreases the number of medications or dose necessary to achieve BP control.
Such pragmatic trials will pave the way for multisite clinical trials with longer follow-up periods assessing the impact of high-resistance IMST on CV events, such as myocardial infarction and all-cause mortality. Multisite trials should include both healthy adults and those with established CVD to determine the ability of high-resistance IMST to both prevent and treat CVD.
If the clinical efficacy of high-resistance IMST for improving CV function and decreasing disease risk is established, and the results of comparative effectiveness trials support equivalency (or better) vs. alternative strategies, uncovering effective avenues for dissemination and implementation of IMST will become important. As discussed above, high-resistance IMST has qualities that suggest it would be acceptable for uptake and to promote adherence in real world settings. However, minimal data supporting this hypothesis are available.
Digital health technologies are a promising strategy for dissemination and implementation of high-resistance IMST. However, before such tools can be made available to the public, the efficacy of high-resistance IMST delivered via digital health technologies for improving CV function will need to be established. This will require first collecting input from potential users on the appropriateness, feasibility, and acceptability of receiving high-resistance IMST through proposed digital health technologies, such as smartphone apps, to create a vehicle to deliver IMST that is usable by the target population. Next, high-resistance IMST delivered via the digital health approach will need to be compared to researcher-supervised, clinic-based IMST for lowering BP and improving vascular function to ensure efficacy.
Once the efficacy of technology-delivered, high-resistance IMST for improving CV function is established, dissemination and implementation research can begin. Of particular importance will be testing digital health technologies for delivering IMST in underserved populations, such as in urban/rural settings or to racial and ethnic minorities who do not traditionally receive equitable access to health care. Additionally, cost-benefit analyses will be needed to determine the healthcare and economic impact of uptake of high-resistance IMST. Such information will offer healthcare providers and insurance companies the information needed to determine the viability of providing free or reduced-price access to IMST devices and the accompanying digital health delivery system. Working with providers, along with underserved groups, will be critical for providing equal access to high-resistance IMST for all who may benefit from this promising lifestyle intervention.
CONCLUSIONS
High-resistance IMST is a novel form of physical training that promotes adherence and improves CV function in midlife/older adults and certain patient populations when assessed in a clinical research setting. While initial findings from small, proof-of-concept studies are promising, additional investigation along the translational research spectrum is needed to move high-resistance IMST from the research setting to use in the public health domain. A particularly promising strategy to speed the ultimate dissemination and implementation of IMST is to leverage digital health technologies to promote uptake among midlife/older adults and other populations at risk for CVD.
Key Points.
Adverse changes in cardiovascular function increase the risk for cardiovascular diseases with advancing age.
Aerobic exercise enhances CV function and decreases cardiovascular disease risk, but poor adherence to physical activity guidelines creates the need for alternative lifestyle interventions to combat age-related declines in cardiovascular health.
High-resistance inspiratory muscle strength training (IMST), a novel form of physical training, promotes adherence and improves cardiovascular function in midlife and older adults when studied in clinical research settings.
The efficacy of high-resistance IMST for improving cardiovascular function in other at-risk populations and when delivered in unsupervised, translational research settings is an important future research direction.
Digital health technologies are a promising avenue for the implementation and dissemination of IMST training to the community setting with important implications for public health.
Acknowledgments:
This work was supported by NIH Grants K01HL153326 (DHC) and F31HL154782 (KAF).
Footnotes
Conflicts of interest: None
REFERENCES
- 1.Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143(8):e254–743. [DOI] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. [DOI] [PubMed] [Google Scholar]
- 3.Lakatta EG, Levy D. Arterial and Cardiac Aging: Major Shareholders in Cardiovascular Disease Enterprises: Part I: Aging Arteries: A “Set Up” for Vascular Disease. Circulation. 2003;107(1):139–46. [DOI] [PubMed] [Google Scholar]
- 4.Craighead DH, Freeberg KA, Seals DR. Vascular Endothelial Function in Midlife/Older Adults Classified According to 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines. J Am Heart Assoc. 2020;9(17):e016625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seals DR. Edward F. Adolph Distinguished Lecture: The remarkable anti-aging effects of aerobic exercise on systemic arteries. J Appl Physiol. 2014;117(5):425–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donato AJ, Eskurza I, Silver AE, et al. Direct evidence of endothelial oxidative stress with aging in humans: relation to impaired endothelium-dependent dilation and upregulation of nuclear factor-kappaB. Circ Res. 2007;100(11):1659–66. [DOI] [PubMed] [Google Scholar]
- 7.Donato AJ, Black AD, Jablonski KL, Gano LB, Seals DR. Aging is associated with greater nuclear NF kappa B, reduced I kappa B alpha, and increased expression of proinflammatory cytokines in vascular endothelial cells of healthy humans. Aging Cell. 2008;7(6):805–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seals DR, Jablonski KL, Donato AJ. Aging and vascular endothelial function in humans. Clin Sci. 2011;120(9):357–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: testing and clinical relevance. Circulation. 2007;115(10):1285–95. [DOI] [PubMed] [Google Scholar]
- 10.Pacher P, Beckman JS, Liaudet L. Nitric oxide and peroxynitrite in health and disease. Physiol Rev. 2007;87(1):315–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lakatta EG. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part III: cellular and molecular clues to heart and arterial aging. Circulation. 2003;107(3):490–7. [DOI] [PubMed] [Google Scholar]
- 12.Danesh J, Wheeler JG, Hirschfield GM, et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. N Engl J Med. 2004;350(14):1387–97. [DOI] [PubMed] [Google Scholar]
- 13.Ershler WB. Interleukin-6: a cytokine for gerontologists. J Am Geriatr Soc. 1993;41(2):176–81. [DOI] [PubMed] [Google Scholar]
- 14.Lesniewski LA, Durrant JR, Connell ML, Folian BJ, Donato AJ, Seals DR. Salicylate treatment improves age-associated vascular endothelial dysfunction: potential role of nuclear factor kappaB and forkhead Box O phosphorylation. J Gerontol A Biol Sci Med Sci. 2011;66(4):409–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craighead DH, Freeberg KA, Seals DR. The protective role of regular aerobic exercise on vascular function with aging. Curr Opin Physiol. 2019;10:55–63. [Google Scholar]
- 16.Schoenborn CA, Stommel M. Adherence to the 2008 adult physical activity guidelines and mortality risk. Am J Prev Med. 2011;40(5):514–21. [DOI] [PubMed] [Google Scholar]
- 17.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 18.Craighead DH, Freeberg KA, McCarty NP, Seals DR. Time-efficient, high-resistance inspiratory muscle strength training for cardiovascular aging. Exp Gerontol. 2021;154:111515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craighead DH, Heinbockel TC, Hamilton MN, et al. Time-efficient physical training for enhancing cardiovascular function in midlife and older adults: promise and current research gaps. J Appl Physiol. 2019;127(5):1427–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–115. [DOI] [PubMed] [Google Scholar]
- 21.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. [DOI] [PubMed] [Google Scholar]
- 22.DeSouza CA, Shapiro LF, Clevenger CM, et al. Regular aerobic exercise prevents and restores age-related declines in endothelium-dependent vasodilation in healthy men. Circulation. 2000;102(12):1351–7. [DOI] [PubMed] [Google Scholar]
- 23.Eskurza I, Monahan KD, Robinson JA, Seals DR. Effect of acute and chronic ascorbic acid on flow-mediated dilatation with sedentary and physically active human ageing. J Physiol. 2004;556(Pt 1):315–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pierce GL, Donato AJ, LaRocca TJ, Eskurza I, Silver AE, Seals DR. Habitually exercising older men do not demonstrate age-associated vascular endothelial oxidative stress. Aging Cell. 2011;10(6):1032–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gano LB, Donato AJ, Pierce GL, et al. Increased proinflammatory and oxidant gene expression in circulating mononuclear cells in older adults: amelioration by habitual exercise. Physiol Genomics. 2011;43(14):895–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seals DR, Nagy EE, Moreau KL. Aerobic exercise training and vascular function with ageing in healthy men and women. J Physiol. 2019;597(19):4901–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pierce GL, Eskurza I, Walker AE, Fay TN, Seals DR. Sex-specific effects of habitual aerobic exercise on brachial artery flow-mediated dilation in middle-aged and older adults. Clin Sci. 2011;120(1):13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santos-Parker JR, Strahler TR, Vorwald VM, Pierce GL, Seals DR. Habitual aerobic exercise does not protect against micro- or macrovascular endothelial dysfunction in healthy estrogen-deficient postmenopausal women. J Appl Physiol. 2017;122(1):11–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moreau KL, Stauffer BL, Kohrt WM, Seals DR. Essential role of estrogen for improvements in vascular endothelial function with endurance exercise in postmenopausal women. J Clin Endocrinol Metab. 2013;98(11):4507–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka H, Dinenno FA, Monahan KD, Clevenger CM, DeSouza CA, Seals DR. Aging, habitual exercise, and dynamic arterial compliance. Circulation. 2000;102(11):1270–5. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka H, DeSouza CA, Seals DR. Absence of age-related increase in central arterial stiffness in physically active women. Arterioscler Thromb Vasc Biol. 1998;18(1):127–32. [DOI] [PubMed] [Google Scholar]
- 32.Moreau KL, Donato AJ, Seals DR, DeSouza CA, Tanaka H. Regular exercise, hormone replacement therapy and the age-related decline in carotid arterial compliance in healthy women. Cardiovasc Res. 2003;57(3):861–8. [DOI] [PubMed] [Google Scholar]
- 33.Pierce GL, Casey DP, Fiedorowicz JG, et al. Aortic pulse wave velocity and reflecting distance estimation from peripheral waveforms in humans: detection of age- and exercise training-related differences. Am J Physiol Heart Circ Physiol. 2013;305(1):H135–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oudegeest-Sander MH, Olde Rikkert MGM, Smits P, et al. The effect of an advanced glycation end-product crosslink breaker and exercise training on vascular function in older individuals: a randomized factorial design trial. Exp Gerontol. 2013;48(12):1509–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vogel T, Leprêtre P-M, Brechat P-H, et al. Effect of a short-term intermittent exercise-training programme on the pulse wave velocity and arterial pressure: a prospective study among 71 healthy older subjects. Int J Clin Pract. 2013;67(5):420–6. [DOI] [PubMed] [Google Scholar]
- 36.Pierce GL. Aortic Stiffness in Aging and Hypertension: Prevention and Treatment with Habitual Aerobic Exercise. Curr Hypertens Rep. 2017;19(11):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nowak KL, Rossman MJ, Chonchol M, Seals DR. Strategies for Achieving Healthy Vascular Aging. Hypertension. 2018;71(3):389–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Piercy KL, Troiano RP, Ballard RM, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320(19):2020–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.El Ansari W, Lovell G. Barriers to exercise in younger and older non-exercising adult women: a cross sectional study in London, United Kingdom. Int J Environ Res Public Health. 2009;6(4):1443–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and Facilitators to the Uptake and Maintenance of Healthy Behaviours by People at Mid-Life: A Rapid Systematic Review. PloS One. 2016;11(1):e0145074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stutts WC. Physical activity determinants in adults. Perceived benefits, barriers, and self efficacy. AAOHN J. 2002;50(11):499–507. [PubMed] [Google Scholar]
- 42.Babakus WS, Thompson JL. Physical activity among South Asian women: a systematic, mixed-methods review. Int J Behav Nutr Phys Act. 2012;9:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siddiqi Z, Tiro JA, Shuval K. Understanding impediments and enablers to physical activity among African American adults: a systematic review of qualitative studies. Health Educ Res. 2011;26(6):1010–24. [DOI] [PubMed] [Google Scholar]
- 44.Yarwood J, Carryer J, Gagan MJ. Women maintaining physical activity at midlife: contextual complexities. Nurs Prax N Z. 2005;21(3):24–37. [PubMed] [Google Scholar]
- 45.Leone LA, Ward DS. A Mixed Methods Comparison of Perceived Benefits and Barriers to Exercise Between Obese and Nonobese Women. J Phys Act Health. 2013;10(4):461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McIntosh T, Hunter DJ, Royce S. Barriers to physical activity in obese adults: A rapid evidence assessment. J Res Nurs. 2016;21(4):271–87. [Google Scholar]
- 47.Krishnaswami A, Beavers C, Dorsch MP, et al. Gerotechnology for Older Adults With Cardiovascular Diseases: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(22):2650–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Direito A, Carraça E, Rawstorn J, Whittaker R, Maddison R. mHealth Technologies to Influence Physical Activity and Sedentary Behaviors: Behavior Change Techniques, Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Behav Med Publ Soc Behav Med. 2017;51(2):226–39. [DOI] [PubMed] [Google Scholar]
- 49.Foster C, Richards J, Thorogood M, Hillsdon M. Remote and web 2.0 interventions for promoting physical activity. Cochrane Database Syst Rev. 2013;9:CD010395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Larsen RT, Christensen J, Juhl CB, Andersen HB, Langberg H. Physical activity monitors to enhance amount of physical activity in older adults - a systematic review and meta-analysis. Eur Rev Aging Phys Act. 2019;16:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jonkman NH, van Schooten KS, Maier AB, Pijnappels M. eHealth interventions to promote objectively measured physical activity in community-dwelling older people. Maturitas. 2018;113:32–9. [DOI] [PubMed] [Google Scholar]
- 52.Höchsmann C, Walz SP, Schäfer J, Holopainen J, Hanssen H, Schmidt-Trucksäss A. Mobile Exergaming for Health-Effects of a serious game application for smartphones on physical activity and exercise adherence in type 2 diabetes mellitus-study protocol for a randomized controlled trial. Trials. 2017;18(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cooper C, Gross A, Brinkman C, et al. The impact of wearable motion sensing technology on physical activity in older adults. Exp Gerontol. 2018;112:9–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Núñez de Arenas-Arroyo S, Cavero-Redondo I, Alvarez-Bueno C, Sequí-Domínguez I, Reina-Gutiérrez S, Martínez-Vizcaíno V. Effect of eHealth to increase physical activity in healthy adults over 55 years: A systematic review and meta-analysis. Scand J Med Sci Sports. 2021;31(4):776–89. [DOI] [PubMed] [Google Scholar]
- 55.Muellmann S, Forberger S, Möllers T, Bröring E, Zeeb H, Pischke CR. Effectiveness of eHealth interventions for the promotion of physical activity in older adults: A systematic review. Prev Med. 2018;108:93–110. [DOI] [PubMed] [Google Scholar]
- 56.Yerrakalva D, Yerrakalva D, Hajna S, Griffin S. Effects of Mobile Health App Interventions on Sedentary Time, Physical Activity, and Fitness in Older Adults: Systematic Review and Meta-Analysis. J Med Internet Res. 2019;21(11):e14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McGarrigle L, Todd C. Promotion of Physical Activity in Older People Using mHealth and eHealth Technologies: Rapid Review of Reviews. J Med Internet Res. 2020;22(12):e22201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vranish JR, Bailey EF. Daily respiratory training with large intrathoracic pressures, but not large lung volumes, lowers blood pressure in normotensive adults. Respir Physiol Neurobiol. 2015;216:63–9. [DOI] [PubMed] [Google Scholar]
- 59.Harms CA, Wetter TJ, McClaran SR, et al. Effects of respiratory muscle work on cardiac output and its distribution during maximal exercise. J Appl Physiol. 1998;85(2):609–18. [DOI] [PubMed] [Google Scholar]
- 60.Johnson BD, Aaron EA, Babcock MA, Dempsey JA. Respiratory muscle fatigue during exercise: implications for performance. Med Sci Sports Exerc. 1996;28(9):1129–37. [DOI] [PubMed] [Google Scholar]
- 61.Tavoian D, Ramos-Barrera LE, Craighead DH, et al. Six Months of Inspiratory Muscle Training to Lower Blood Pressure and Improve Endothelial Function in Middle-Aged and Older Adults With Above-Normal Blood Pressure and Obstructive Sleep Apnea: Protocol for the CHART Clinical Trial. Front Cardiovasc Med. 2021;8:760203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.DeLucia CM, DeBonis DR, Schwyhart SM, Bailey EF. Acute cardiovascular responses to a single bout of high intensity inspiratory muscle strength training in healthy young adults. J Appl Physiol. 2021;130(4):1114–21. [DOI] [PubMed] [Google Scholar]
- 63.Sharman JE, LaGerche A. Exercise blood pressure: clinical relevance and correct measurement. J Hum Hypertens. 2015;29(6):351–8. [DOI] [PubMed] [Google Scholar]
- 64.Cornelissen VA, Verheyden B, Aubert AE, Fagard RH. Effects of aerobic training intensity on resting, exercise and post-exercise blood pressure, heart rate and heart-rate variability. J Hum Hypertens. 2010;24(3):175–82. [DOI] [PubMed] [Google Scholar]
- 65.Vranish JR, Bailey EF. Inspiratory Muscle Training Improves Sleep and Mitigates Cardiovascular Dysfunction in Obstructive Sleep Apnea. Sleep. 2016;39(6):1179–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.DeLucia CM, De Asis RM, Bailey EF. Daily inspiratory muscle training lowers blood pressure and vascular resistance in healthy men and women. Exp Physiol. 2018;103(2):201–11. [DOI] [PubMed] [Google Scholar]
- 67.Ramos-Barrera GE, DeLucia CM, Bailey EF. Inspiratory muscle strength training lowers blood pressure and sympathetic activity in older adults with OSA: A randomized controlled pilot trial. J Appl Physiol. 2020;129(3):449–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Craighead DH, Heinbockel TC, Freeberg KA, et al. Time-Efficient Inspiratory Muscle Strength Training Lowers Blood Pressure and Improves Endothelial Function, NO Bioavailability, and Oxidative Stress in Midlife/Older Adults With Above-Normal Blood Pressure. J Am Heart Assoc. 2021;10(13):e020980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Musini VM, Nazer M, Bassett K, Wright JM. Blood pressure-lowering efficacy of monotherapy with thiazide diuretics for primary hypertension. Cochrane Database Syst Rev. 2014;(5):CD003824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Heran BS, Wong MM, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin converting enzyme (ACE) inhibitors for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD003823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Heran BS, Wong MMY, Heran IK, Wright JM. Blood pressure lowering efficacy of angiotensin receptor blockers for primary hypertension. Cochrane Database Syst Rev. 2008;(4):CD003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13. [DOI] [PubMed] [Google Scholar]
- 73.Cheng S, Xanthakis V, Sullivan LM, Vasan RS. Blood pressure tracking over the adult life course: patterns and correlates in the Framingham heart study. Hypertension. 2012;60(6):1393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wills AK, Lawlor DA, Matthews FE, et al. Life course trajectories of systolic blood pressure using longitudinal data from eight UK cohorts. PLoS Med. 2011;8(6):e1000440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hansen TW, Kikuya M, Thijs L, et al. Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25(8):1554–64. [DOI] [PubMed] [Google Scholar]
- 76.Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51(1):55–61. [DOI] [PubMed] [Google Scholar]
- 77.Celermajer DS, Sorensen KE, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Deanfield JE. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J Am Coll Cardiol. 1994;24(2):471–6. [DOI] [PubMed] [Google Scholar]
- 78.Inaba Y, Chen JA, Bergmann SR. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int J Cardiovasc Imaging. 2010;26(6):631–40. [DOI] [PubMed] [Google Scholar]
- 79.Green DJ, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-mediated dilation and cardiovascular event prediction: does nitric oxide matter? Hypertension. 2011;57(3):363–9. [DOI] [PubMed] [Google Scholar]
- 80.Matsuzawa Y, Kwon T-G, Lennon RJ, Lerman LO, Lerman A. Prognostic Value of Flow-Mediated Vasodilation in Brachial Artery and Fingertip Artery for Cardiovascular Events: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2015;4(11) doi: 10.1161/JAHA.115.002270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ras RT, Streppel MT, Draijer R, Zock PL. Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int J Cardiol. 2013;168(1):344–51. [DOI] [PubMed] [Google Scholar]
- 82.Xu Y, Arora RC, Hiebert BM, et al. Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur Heart J Cardiovasc Imaging. 2014;15(7):736–46. [DOI] [PubMed] [Google Scholar]
- 83.Beltrami FG, Mzee D, Spengler CM. No Evidence That Hyperpnea-Based Respiratory Muscle Training Affects Indexes of Cardiovascular Health in Young Healthy Adults. Front Physiol. 2020;11:530218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Figueiredo PHS, Lima MMO, Costa HS, et al. Effects of the inspiratory muscle training and aerobic training on respiratory and functional parameters, inflammatory biomarkers, redox status and quality of life in hemodialysis patients: A randomized clinical trial. PloS One. 2018;13(7):e0200727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pellizzaro CO, Thomé FS, Veronese FV. Effect of Peripheral and Respiratory Muscle Training on the Functional Capacity of Hemodialysis Patients. Ren Fail. 2013;35(2):189–97. [DOI] [PubMed] [Google Scholar]
- 86.Mills DE, Johnson MA, Barnett YA, Smith WHT, Sharpe GR. The effects of inspiratory muscle training in older adults. Med Sci Sports Exerc. 2015;47(4):691–7. [DOI] [PubMed] [Google Scholar]
- 87.Narkiewicz K, Somers VK. Sympathetic nerve activity in obstructive sleep apnoea. Acta Physiol Scand. 2003;177(3):385–90. [DOI] [PubMed] [Google Scholar]
- 88.de Abreu RM, Rehder-Santos P, Minatel V, Dos Santos GL, Catai AM. Effects of inspiratory muscle training on cardiovascular autonomic control: A systematic review. Auton Neurosci Basic Clin. 2017;208:29–35. [DOI] [PubMed] [Google Scholar]
- 89.Halliwill JR. Mechanisms and clinical implications of post-exercise hypotension in humans. Exerc Sport Sci Rev. 2001;29(2):65–70. [DOI] [PubMed] [Google Scholar]
- 90.Ferraro FV, Gavin JP, Wainwright T, McConnell A. The effects of 8 weeks of inspiratory muscle training on the balance of healthy older adults: a randomized, double-blind, placebo-controlled study. Physiol Rep. 2019;7(9):e14076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Formiga MF, Dosbaba F, Hartman M, et al. Novel versus Traditional Inspiratory Muscle Training Regimens as Home-Based, Stand-Alone Therapies in COPD: Protocol for a Randomized Controlled Trial. Int J Chron Obstruct Pulmon Dis. 2020;15:2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fry DK, Pfalzer LA, Chokshi AR, Wagner MT, Jackson ES. Randomized control trial of effects of a 10-week inspiratory muscle training program on measures of pulmonary function in persons with multiple sclerosis. J Neurol Phys Ther. 2007;31(4):162–72. [DOI] [PubMed] [Google Scholar]
- 93.Pfalzer L, Fry D. Effects of a 10-week inspiratory muscle training program on lower-extremity mobility in people with multiple sclerosis: a randomized controlled trial. Int J MS Care. 2011;13(1):32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.de Menezes KKP, Ada L, Teixeira-Salmela LF, et al. Home-Based Interventions may Increase Recruitment, Adherence, and Measurement of outcomes in Clinical Trials of Stroke Rehabilitation. J Stroke Cerebrovasc Dis. 2021;30(10):106022. [DOI] [PubMed] [Google Scholar]
- 95.Nikoletou D, Man WD-C, Mustfa N, et al. Evaluation of the effectiveness of a home-based inspiratory muscle training programme in patients with chronic obstructive pulmonary disease using multiple inspiratory muscle tests. Disabil Rehabil. 2016;38(3):250–9. [DOI] [PubMed] [Google Scholar]
- 96.O’Connor C, Lawson R, Waterhouse J, Mills GH. Is inspiratory muscle training (IMT) an acceptable treatment option for people with chronic obstructive pulmonary disease (COPD) who have declined pulmonary rehabilitation (PR) and can IMT enhance PR uptake? A single-group prepost feasibility study in a home-based setting. BMJ Open. 2019;9(8):e028507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sørensen D, Svenningsen H. Adherence to home-based inspiratory muscle training in individuals with chronic obstructive pulmonary disease. Appl Nurs Res. 2018;43:75–9. [DOI] [PubMed] [Google Scholar]
- 98.Pick HJ, Faghy MA, Creswell G, et al. The feasibility and tolerability of using inspiratory muscle training with adults discharged from the hospital with community-acquired pneumonia. Adv Respir Med. 2021;89(2):216–20. [DOI] [PubMed] [Google Scholar]
- 99.Nelson Kakulla B. 2020 Tech Trends of the 50+. AARP Research; 2020. [cited 2021 Feb 9] Available from: https://www.aarp.org/research/topics/technology/info-2019/2020-technology-trends-older-americans.html. [Google Scholar]
- 100.Pew Research Center. Mobile technology and home broadband 2021. 2021.
- 101.Wagner N, Hassanein K, Head M. Computer use by older adults: A multi-disciplinary review. Comput Hum Behav. 2010;26(5):870–82. [Google Scholar]
- 102.Wildenbos GA, Peute L, Jaspers M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int J Med Inf. 2018;114:66–75. [DOI] [PubMed] [Google Scholar]
- 103.Betts LR, Hill R, Gardner SE. “There’s Not Enough Knowledge Out There”: Examining Older Adults’ Perceptions of Digital Technology Use and Digital Inclusion Classes. J Appl Gerontol. 2019;38(8):1147–66. [DOI] [PubMed] [Google Scholar]
- 104.Mitzner TL, Savla J, Boot WR, et al. Technology Adoption by Older Adults: Findings From the PRISM Trial. Gerontologist. 2019;59(1):34–44. [DOI] [PMC free article] [PubMed] [Google Scholar]


