Abstract
Objective.
To evaluate communication training content fidelity included in a multifaceted intervention known to reduce antibiotic over-prescribing for pediatric acute respiratory illnesses (ARTIs), by examining the degree to which clinicians implemented the intended communication behavior changes.
Methods.
Parents were surveyed regarding clinician communication behaviors immediately after attending 1,026 visits by children 6 months to < 11 years old diagnosed with ARTIs by 53 clinicians in 18 pediatric practices. Communication outcomes analyzed were whether clinicians: (A) provided both a combined (positive + negative) treatment recommendation and a contingency plan (full implementation); (B) provided either a combined treatment recommendation or a contingency plan (partial implementation); or (C) provided neither (no implementation). We used mixed effects multinomial logistic regression to determine whether these 3 communication outcomes changed between baseline and the time periods following each of 3 training modules.
Results.
After completing the communication training, the adjusted probability of clinicians fully implementing the intended communication behavior changes increased by an absolute 8.1% compared to baseline (95% Confidence Interval [CI]: 2.4%, 13.8%, p=0.005).
Conclusions.
Our findings support the fidelity of the intervention’s communication training content.
Practical Implications.
Clinicians can be trained to implement communication behaviors that may aid in reducing antibiotic over-prescribing for ARTIs.
1. Introduction
Several randomized clinical trials have demonstrated intervention effectiveness for reducing antibiotic prescribing for acute respiratory tract infections (ARTIs) [1–8]. Successful interventions have been multifaceted and sustained improvement more likely when interventions included clinician communication training [3, 8, 9]. According to the Medical Research Council [10], multifaceted complex interventions should include analyses of intervention fidelity [11–13]. A key aspect of intervention fidelity is ‘receipt,’ or the degree to which those receiving the intervention have understood it and display the behavior change intended [11].
This study evaluates the receipt fidelity of the communication training included in the Dialogue Around Respiratory Illness Treatment (DART) program [14]. The DART program intervention trial decreased overall and inappropriate antibiotic prescribing for ARTIs by 7% and 40%, respectively [15]. While the DART program is multifaceted, it is unique in that its central intervention component focuses on two specific evidence-based communication behaviors that are discussed and modeled in different formats (i.e., online tutorials, webinars, and booster video vignettes).
The first communication behavior involves delivering a combined, two-part treatment recommendation that includes a negative recommendation, i.e., ruling out the need for antibiotics (e.g., “What we have here is a really bad cold, so nothing an antibiotic will help.”), and a positive recommendation, i.e., suggesting actions that parents can take to reduce their child’s symptoms (e.g., “Giving her an extra pillow at night can help with draining the congestion”). Providing both negative and positive treatment recommendations (versus one or none) is associated with decreased inappropriate antibiotic prescribing [16].
The second communication behavior involves ending visits with a contingency plan for what parents can do if their child gets worse or shows no improvement over the following 2–3 days (e.g., “Definitely call me if she starts having high fevers. I don’t expect that to happen, but that’s what you should watch for.”). Providing two-part, negative and positive treatment recommendations and contingency plans is positively associated with parents’ increased visit-satisfaction [16, 17].
Our main objective for this study was to evaluate the receipt fidelity of DART’s communication program content by examining whether or not clinicians changed their communication behaviors as intended.
2. Methods
This study was approved by the participating organizations’ institutional review boards (IRBs) and the Western IRB (See study protocol at ClinicalTrials.gov; Identifier: NCT02943551).
The DART intervention trial [15] was a cluster-randomized, stepped-wedge, clinical trial that allowed enrolled clinicians (i.e., pediatricians and pediatric nurse practitioners) to receive the intervention through staggered implementation across 19 United States primary care pediatric practices. Between 9/1/2016 and 1/30/2017, clinicians were recruited from the American Academy of Pediatrics Pediatric Research in Office Settings network [18] (n=11 practices from 9 states) and the NorthShore University Health System (n=8 practices in the Chicago, IL area). Practices were the unit of randomization and were allocated by random permutation to 4 wedges. Written informed consent was obtained from clinicians (n=57) prior to practice randomization. Enrolled clinicians received intervention modules according to their practice-assigned wedge (Figure 1).
Figure 1.
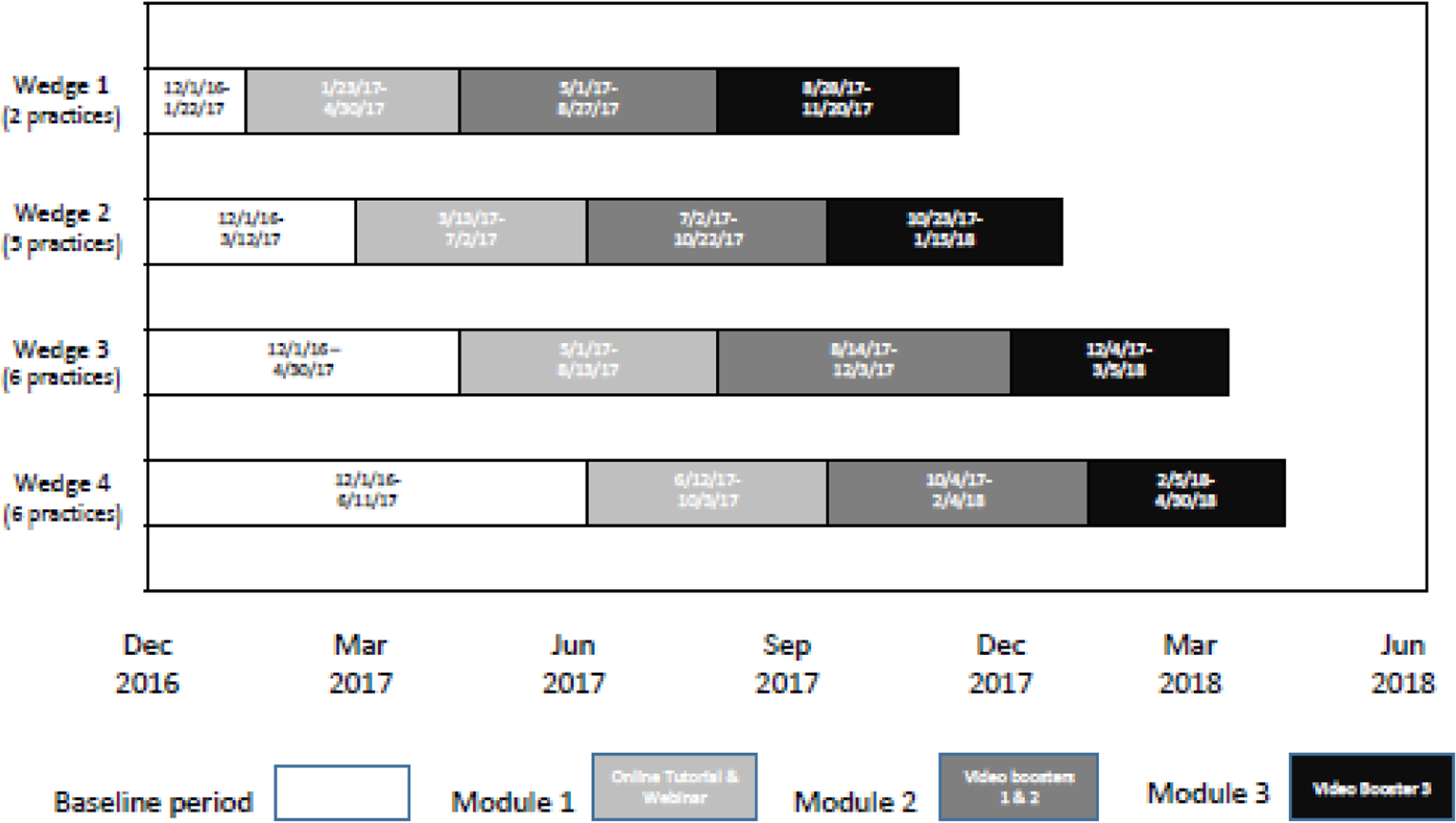
Study intervention and timing
The DART program communication content is evidence-based [16, 17, 19–21] with the training focused on two communication behaviors derived from formative research using Conversation Analysis [22] (1) the delivery of a treatment recommendation involving both negative and positive components (see introduction), and (2) a contingency plan. The training includes a 25-minute online tutorial, a 40-minute webinar, and three booster video-vignette sessions (recapping communication best practices followed by questions testing clinicians’ understanding) delivered in 3 modules over an 11-month period (Figure 1).
In participating practices, between 12/1/2016 and 4/30/18, survey data were collected anonymously from eligible parents of children presenting for ARTI visits during four time periods: a baseline (pre-intervention) period and three post-intervention periods occurring after clinicians completed each DART program module. Parents were eligible if their child was seen by an enrolled clinician, was 6 months to < 11 years old, had not received antibiotics in the previous two weeks, and was diagnosed during the visit with > 1 of 5 targeted ARTIs: acute otitis media, bronchitis, pharyngitis, sinusitis, or upper respiratory infection. Eligible parents completed surveys on tablet computers immediately after their child’s visit. Survey questions assessed parent/child demographics and clinician communication behaviors using the Provider Communication Behavior Inventory (PCBI; Table 1) [16].
Table 1.
PCBI* survey items assessing parent reports of clinician communication behaviors used during acute respiratory tract infection visits
| Clinician Communication Behavior | PCBI Survey Items Used to Assess Occurrence of Communication Behaviors |
|---|---|
| Negative Treatment Recommendation | Did the doctor tell you antibiotics will NOT help your child get better?
|
| Positive Treatment Recommendation | Did the doctor tell you things you can do to make your child feel better, for example, giving Tylenol for fevers or running a humidifier in your child’s bedroom at night?
|
| Contingency Plan: Visit-Based | Did the doctor ask you to come back if your child isn’t doing better in the next day or two?
Did the doctor tell you what to watch for so that you would know when to bring your child back in to be rechecked? For example, telling you to come back if your child has high fevers, or a cough that is lasting too many days?
|
| Contingency Plan: Telephone-Based | Did the doctor ask you to call on the phone if your child isn’t doing better in the next day or two?
Did the doctor tell you what to watch for so that you would know when to call about your child to get more help? For example, telling you to call if your child has high fevers, or a cough that is lasting too many days?
|
PCBI = Provider Communication Behavior Inventory
During the study, 1,288 eligible surveys were obtained from 18 of the 19 participating practices (range: 8–178). Four (7%) of the 57 enrolled clinicians had no eligible surveys. The 90th percentile for number of surveys obtained per clinician was 39. To avoid having a small number of clinicians overrepresented in the data, for clinicians with ≥ 39 surveys (5/53, 9%), we randomly selected 39 surveys for analysis. This yielded 1,026 surveys for analysis (80% of those collected, Figure 2).
Figure 2.
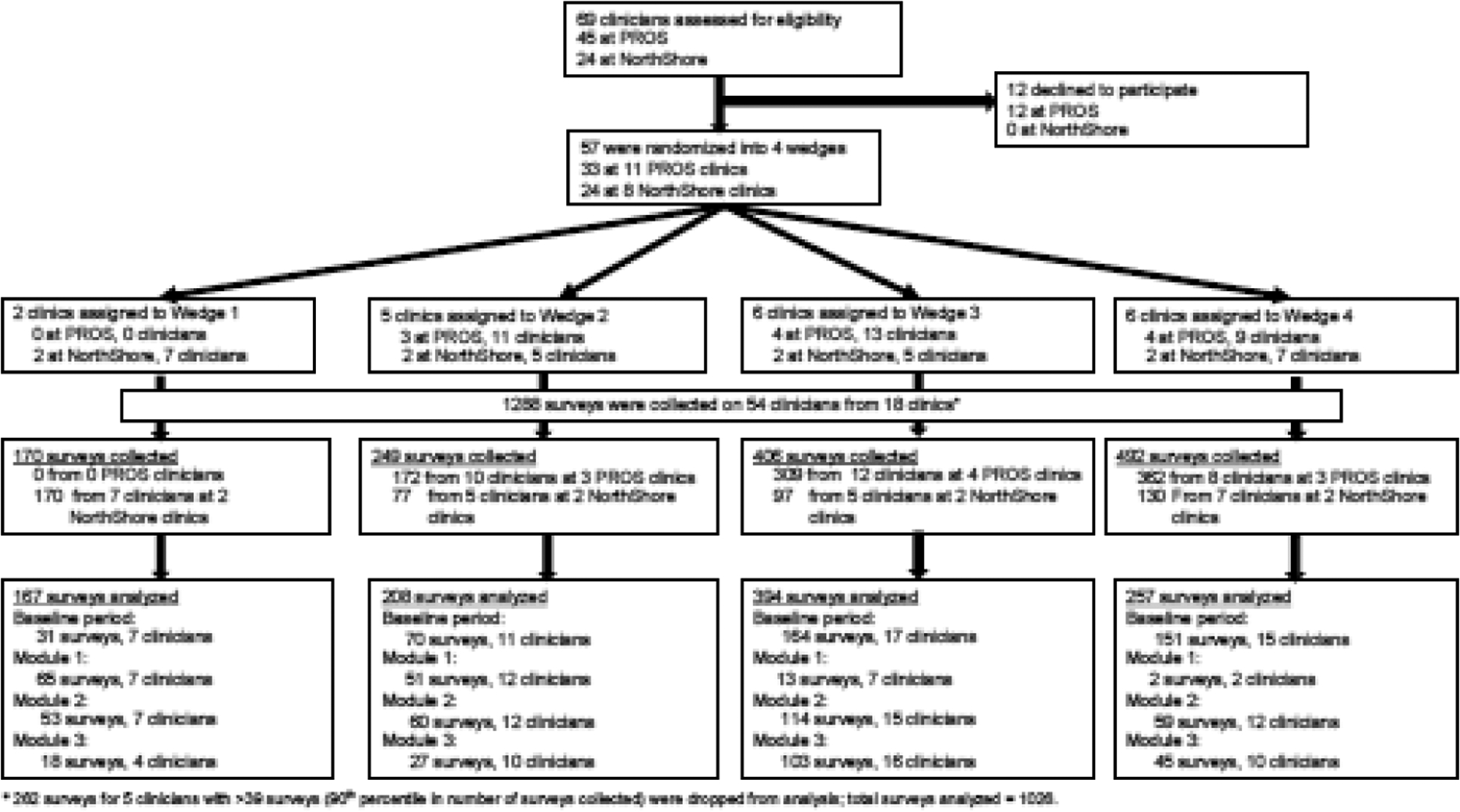
Study flow diagram
The main study outcome was the frequency with which clinicians gave a two-part treatment recommendation and/or a contingency plan during the treatment phase of ARTI visits as captured from parent post-visit surveys (Table1). From survey data, we constructed three, mutually exclusive communication-outcome categories: (A) clinician provided both a combined (positive + negative) treatment recommendation and a contingency plan (full implementation of communication behavior changes); (B) clinician provided either a combined treatment recommendation or a contingency plan (partial implementation); or (C) clinician provided neither a combined treatment recommendation nor a contingency plan (no implementation).
The primary intention-to-treat analysis included all study clinicians who had any surveys completed (53/57, 93%). Eligible surveyed visits were the unit of analysis. We conducted mixed effects multinomial logistic regression with robust standard errors to account for clustering within practices. We examined how each clinician’s probability of using specific communication behaviors (outcome categories A, B, or C, above) varied from the baseline period (pre-intervention) to three post-intervention periods corresponding to when clinicians completed each of three intervention modules. For ease of interpretation, we report average marginal effects (AMEs) for all the predictors. An AME captures the average difference in the probability of using specific communication behaviors (outcome categories A, B, or C) when a predictor variable changes from the reference level to a different level, e.g., from the baseline period to the post-module 1 period[23, 24].
3. Results
Overall, 53 clinicians (47 pediatricians, 6 nurse practitioners) from 18 practices had eligible surveys during at least one of the four study time-periods and were included in the analysis. A total of 1,026 eligible ARTI visits were included in analyses (Figure 2). Across the study time-periods, demographic characteristics of the sampled children and their parents were similar except for annual household income (Table 2).
Table 2.
Sample demographics and parent reports of clinician communication behavior outcomes during pediatric visits for acute respiratory tract infections (ARTI), by study time period
| Demographics | Baseline | Module 1c | Module 2c | Module 3c | P-valueb |
|---|---|---|---|---|---|
| Number of children/parents | 416 | 131 | 286 | 193 | |
| Child Age | N(%)a | N(%) | N(%) | N(%) | |
| 6–12 months | 53 (12.7) | 14 (10.7) | 41 (14.3) | 22 (11.4) | 0.64 |
| 13–23 months | 58 (13.9) | 17 (13.0) | 39 (13.6) | 24 (12.4) | |
| 2–5 years | 172 (41.3) | 58 (44.3) | 135 (47.2) | 93 (48.2) | |
| 6–10 years | 133 (32.0) | 42 (32.1) | 71 (24.8) | 54 (28.0) | |
| Child Sex | |||||
| Male | 211 (50.7) | 74 (56.5) | 139 (48.6) | 82 (42.5) | 0.08 |
| Child Health Status | |||||
| Excellent | 180 (43.3) | 58 (44.3) | 116 (40.6) | 80 (41.5) | 0.24 |
| Very good | 150 (36.1) | 46 (35.1) | 107 (37.4) | 56 (29.0) | |
| Good | 46 (11.1) | 17 (13.0) | 31 (10.8) | 20 (10.4) | |
| Fair/Poor | 7 (1.7) | 3 (2.3) | 8 (2.7) | 8 (4.1) | |
| Missing | 33 (7.9) | 7 (5.3) | 24 (8.4) | 29 (15.0) | |
| Parent Age | |||||
| <25 years | 28 (6.7) | 6 (4.6) | 23 (8.0) | 17 (8.8) | 0.09 |
| 25–34 years | 136 (32.7) | 40 (30.5) | 111 (38.8) | 67 (34.7) | |
| 35–44 years | 201 (48.3) | 72 (55.0) | 103 (36.0) | 85 (44.0) | |
| ≥45 years | 47 (11.3) | 12 (9.2) | 46 (16.1) | 22 (11.4) | |
| Missing | 4 (1.0) | 1 (0.8) | 3 (1.0) | 2 (1.0) | |
| Parent Race | |||||
| White | 316 (76.0) | 104 (79.4) | 221 (77.3) | 149 (77.2) | 0.64 |
| Black / African American | 21 (5.0) | 9 (6.9) | 13 (4.5) | 6 (3.1) | |
| Asian | 25 (6.0) | 5 (3.8) | 17 (5.9) | 6 (3.1) | |
| American Indian or Alaska Native | 1 (0.2) | 0 | 4 (1.4) | 3 (1.6) | |
| Native Hawaiian and Pacific Islander | 1 (0.2) | 0 | 1 (0.4) | 0 | |
| Mixed raced | 46 (11.1) | 12 (9.2) | 25 (8.7) | 25 (13.0) | |
| Missing | 6 (1.4) | 1 (0.8) | 5 (1.8) | 4 (2.1) | |
| Parent Hispanic Ethnicity | 78 (18.8) | 25 (19.1) | 51 (17.8) | 51 (26.4) | 0.28 |
| Parent Education | |||||
| High School or Less | 82 (19.7) | 30 (22.9) | 70 (24.5) | 59 (30.6) | 0.05 |
| Some College or Bachelor’s Degree | 191 (45.9) | 55 (42.0) | 121 (42.3) | 87 (45.1) | |
| > Bachelor’s Degree | 139 (33.4) | 45 (34.4) | 91 (31.8) | 42 (21.8) | |
| Missing | 4 (1.0) | 1 (0.8) | 4 (1.4) | 5 (2.6) | |
| Household Annual Income | |||||
| < $30,000 | 56 (13.5) | 7 (5.3) | 50 (17.5) | 39 (20.2) | <.01 |
| $30,000 – $60,000 | 61 (14.7) | 17 (13.0) | 40 (14.0) | 24 (12.4) | |
| > $60,000 | 216 (51.9) | 87 (66.4) | 133 (46.5) | 77 (39.9) | |
| Missing | 83 (20.0) | 20 (15.2) | 66 (22.0) | 53 (27.4) | |
| Communication Behavior Outcomese (Unadjusted) | |||||
| Category A | 64 (15.4) | 24 (18.5) | 58 (20.3) | 48 (25.0) | 0.04 |
| Category B | 220 (52.9) | 66 (50.8) | 147 (51.4) | 105 (54.7) | |
| Category C | 132 (31.7) | 40 (30.8) | 81 (28.3) | 39 (20.3) | |
| Missing | 0 (0.0) | 1 (0.8) | 0 (0.0) | 1 (0.5) |
N(%): Number (percent); Different populations of parents/children are represented for each cross-sectional time-period
P-value represents differences across the 4 time periods listed.
Module 1 content: Two 25-minute online tutorials about best practices for both clinician communication behaviors and antibiotic prescribing; live or recorded 40-minute webinars on those same topics; individualized feedback report presenting antibiotic prescribing rates during ARTI visits in the baseline control period.
Module 2 content: Two 5-minute online booster video vignettes recapping communication best practices followed by knowledge questions; a second antibiotic prescribing feedback report, presenting prescribing rates during module 1.
Module 3 content: One 5-minute communication booster video vignette followed by knowledge questions; a third and a fourth antibiotic prescribing feedback report, presenting prescribing rates during modules 2 and 3, respectively.
Mixed: More than one race
Outcome Category A = Clinician used both a negative-positive combined treatment recommendation and a contingency plan
Outcome Category B = Clinician used either a negative-positive combined treatment recommendation or a contingency plan, but not both
Outcome Category C = Clinician used neither preferred communication behavior
Intention-to-treat analyses indicated that, after completion of intervention module 3, the adjusted probability of using communication-outcome category ‘A’ (full implementation) increased by an absolute 8.1% compared to baseline (95% Confidence Interval [CI]: 2.4%, 13.8%, p=0.005; Table 3 and supplementary Figure 3), while the probability of using communication-outcome category ‘C’ (complete failure to implement) decreased by 9.9% (95% CI: −16.1%, −3.6%, p=.002). There was no change in the probability of using communication-outcome category ‘B’ (partial implementation). Using all eligible surveys in analyses did not change the reported results (not shown).
Table 3.
Adjusted difference in probability of parents reporting clinician use of preferred communication behaviors during pediatric visits for acute respiratory tract infections (ARTI)
| Communication Behavior Outcome Category Aa | Communication Behavior Outcome Category Ba | Communication Behavior Outcome Category Ca | ||||
|---|---|---|---|---|---|---|
| Predictors | Adjusted Difference (95% CI)b | P-value | Adjusted Difference (95% CI) | P-value | Adjusted Difference (95% CI) | P-value |
| Post Module 3 | 8.1 (2.4, 13.8) | <.01 | 1.8 (−6.2, 9.7) | .43 | −9.9 (−16.1, −3.6) | <.01 |
| 6–10 Years | −10.7 (−21.1, −0.3) | .04 | −0.8 (−14.8, 13.3) | .92 | 11.5 (−1.4, 24.4) | .08 |
| Male | −1.9 (−5.5, 1.7) | .30 | 5.6 (0.3, 10.9) | .04 | −3.7 (−8.9, 1.5) | .16 |
| 45+ Years | 10.0 (−3.3, 23.3) | .14 | −4.7 (−16.9, 7.6) | .45 | −5.31 (−25.3, 14.7) | .60 |
| >Bachelor’s degree | −6.6 (−11.5, −1.7) | <.01 | −7.1 (−13.2, −1.0) | .02 | 13.7 (7.3, 20.1) | <.01 |
| Mixed/Other | −7.3 (−10.5, −4.0) | <.01 | 12.4 (3.3, 21.4) | <.01 | −5.1 (−15.2, 5.0) | .32 |
| Hispanic | 4.3 (−6.8, 15.5) | .44 | 2.4 (−5.5, 10.3) | .54 | −6.8 (−14.8, 1.3) | .10 |
Outcome Category A = Clinician used both a negative-positive combined treatment recommendation and a contingency plan
Outcome Category B = Clinician used either a negative-positive combined treatment recommendation or a contingency plan, but not both
Outcome Category C = Clinician used neither preferred communication behavior
Adjusted difference is the absolute change in the percent of visits where parents reported the specified communication behaviors were used by clinicians comparing each predictor to its respective referent; 95% CI = 95%
Confidence Interval
Module 1 content: Two 25-minute online tutorials about best practices for both clinician communication practices and antibiotic prescribing; live or recorded 40-minute webinars on those same topics; individualized feedback report presenting antibiotic prescribing rates during ARTI visits in the baseline control period.
Module 2 content: Two 5-minute online booster video vignettes recapping communication best practices followed by knowledge questions; a second antibiotic prescribing feedback report, presenting prescribing rates during module 1.
Module 3 content: One 5-minute communication booster video vignette followed by knowledge questions; a third and a fourth antibiotic prescribing feedback report, presenting prescribing rates during modules 2 and 3, respectively.
4. Discussion and Conclusions
4.1. Discussion
Previously, we demonstrated that the DART program significantly reduced both overall and inappropriate outpatient antibiotic prescribing for ARTIs experienced by children 6 months to < 11 years old [15]. While the DART program was multifaceted, it centrally involved an effort to change clinician communication behaviors. Specifically, we trained clinicians to deliver a two-part, negative plus positive treatment recommendation and to offer a contingency plan. Current findings support the receipt fidelity of the DART program’s communication content, with parent surveys recording that clinicians significantly increased their use of both behaviors during visits, and significantly decreased their use of none of these behaviors during visits. Clinicians’ use of one of the two behaviors increased marginally, but not significantly.
This study has several limitations. First, we were unable to audio/videotape visits and depended on parent reports of clinician communication behaviors. However, bias in over or under-reporting would be expected to occur non-differentially across the baseline and post-intervention periods. Second, parent reports of communication behaviors were only collected for a sub-sample of the ARTI visits included in the main DART intervention trial [15], and data on prescribing for the sampled visits could not be linked to parent reported communication behaviors due to the anonymity of the surveys. Thus, although observation of the DART communication behaviors increased, the sampled visits in this study may not have corresponded to visits where antibiotics were not prescribed. This sub-sample was also a convenience sample and may be biased and not representative of the entire study population.
4.2. Conclusion
Despite these limitations, our findings support the receipt fidelity of the DART program’s communication training content. Such content involved the ordered placement of specific wording during visits, as recommended by conversation analysis [22].
4.3. Practice Implications
Clinicians can be trained to implement and increase the frequency of two specific communication behaviors that, in past observational studies, were associated with decreased inappropriate antibiotic prescribing for ARTIs and increased visit satisfaction.[16, 17] Broad implementation of the DART program may support ongoing pediatric outpatient antibiotic stewardship.
Supplementary Material
Supplementary Figure 3. Adjusted probability of parents reporting clinician use of preferred communication behavior
Highlights.
Pediatric antibiotic over-prescribing for acute respiratory illnesses is common
Clinician communication is associated with inappropriate antibiotic prescribing
Communication training can successfully change clinician communication behaviors
Acknowledgment:
We thank the practices, pediatricians, and nurse practitioners that participated in the DART study. The NorthShore practices were as follows (alphabetical order, listed with permission): Deerfield, Illinois; Evanston, Illinois (Central); Evanston, Illinois (Davis); Glenview, Illinois; Gurnee, Illinois; Lincolnwood, Niles, Old Orchard, Illinois; Plaza Del Lago, Illinois; Vernon Hills, Illinois. The PROS practices were as follows (alphabetical order, listed with permission): Advanced Preventive Care Pediatrics (Bradenton, FL); All Star Pediatrics (Countryside, IL); A to Z Pediatric and Youth Healthcare (Addison, IL); Cornerstone Pediatrics (Seguin, TX); East End Pediatrics, PC (East Hampton, NY); Eureka Pediatrics (Eureka, CA); Hampton Pediatrics, PLLC (Southampton, NY); Paragould Pediatrics, PLLC (Paragould, AR); Pediatric Medicine of Wallingford, LLP (Wallingford, CT); Pediatric Partners of the Southwest (Durango, CO); Plateau Pediatrics (Crossville, TN).
Funding:
Supported by the National Institutes of Health R01 HD084547-01 to Dr Mangione-Smith (principal investigator). Additional infrastructure funding was provided by the American Academy of Pediatrics and the Health Resources and Services Administration of the US Department of Health and Human Services under UA6MC15585, National Research Network to Improve Child Health. The information, content, and/or conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the Health Resources and Services Administration, Department of Health and Human Services, or US Government. Additionally, the funders and/or sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; or decision to submit the article for publication. Funded by the National Institutes of Health (NIH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Clinical Trial Registration:ClinicalTrials.gov Identifier: NCT02943551
Financial Disclosure Statement: The authors have no financial relationships relevant to this article to disclose.
Data Sharing Statement:
Deidentified data limited to anonymous survey data will be shared. No protected health information for study participants will be shared. Data will be provided as a CSV file with a data dictionary defining all variables included in the file and will be transferred using a secure file transfer protocol. Additional tools will not be made available. The data will be made available upon publication of the primary studies to researchers who provide a detailed methodologically sound proposal and data use agreement. Proposals should be submitted to Dr. Mangione-Smith (Rita.M.Mangione-Smith@kp.org).
References
- [1].Butler CC, Simpson SA, Dunstan F, Rollnick S, Cohen D, Gillespie D, et al. Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: practice based randomised controlled trial. BMJ 2012;344:d8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Little P, Stuart B, Francis N, Douglas E, Tonkin-Crine S, Anthierens S, et al. Effects of internet-based training on antibiotic prescribing rates for acute respiratory-tract infections: a multinational, cluster, randomised, factorial, controlled trial. Lancet 2013;382:1175–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Little P, Stuart B, Francis N, Douglas E, Tonkin-Crine S, Anthierens S, et al. Antibiotic Prescribing for Acute Respiratory Tract Infections 12 Months After Communication and CRP Training: A Randomized Trial. Ann Fam Med 2019;17:125–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gulliford MC, Juszczyk D, Prevost AT, Soames J, McDermott L, Sultana K, et al. Electronically delivered interventions to reduce antibiotic prescribing for respiratory infections in primary care: cluster RCT using electronic health records and cohort study. Health technology assessment (Winchester, England) 2019;23:1–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mortazhejri S, Hong PJ, Yu AM, Hong BY, Stacey D, Bhatia RS, et al. Systematic review of patient-oriented interventions to reduce unnecessary use of antibiotics for upper respiratory tract infections. Syst Rev 2020;9:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Stuart B, Hounkpatin H, Becque T, Yao G, Zhu S, Alonso-Coello P, et al. Delayed antibiotic prescribing for respiratory tract infections: individual patient data meta-analysis. Bmj 2021;373:n808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].McDonagh M, Peterson K, Winthrop K, Cantor A, Holzhammer B, Buckley DI. AHRQ Comparative Effectiveness Reviews. Improving Antibiotic Prescribing for Uncomplicated Acute Respiratory Tract Infections, Rockville (MD): Agency for Healthcare Research and Quality (US); 2016. [PubMed] [Google Scholar]
- [8].Wei X, Zhang Z, Hicks JP, Walley JD, King R, Newell JN, et al. Long-term outcomes of an educational intervention to reduce antibiotic prescribing for childhood upper respiratory tract infections in rural China: Follow-up of a cluster-randomised controlled trial. PLoS medicine 2019;16:e1002733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gerber JS, Prasad PA, Fiks AG, Localio AR, Bell LM, Keren R, et al. Durability of Benefits of an Outpatient Antimicrobial Stewardship Intervention After Discontinuation of Audit and Feedback. JAMA 2014;312:2569–70. [DOI] [PubMed] [Google Scholar]
- [10].Medical Research Council. Developing and evaluating complex interventions. https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/; 2019. accessed Access Day Access Month Access Year]|.
- [11].Bellg AJ, Borrelli B, Resnick B, Hecht J, Minicucci DS, Ory M, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health psychology : official journal of the Division of Health Psychology, American Psychological Association; 2004;23:443–51. [DOI] [PubMed] [Google Scholar]
- [12].Geraets JJ, Goossens ME, van Haastregt JC, de Groot IJ, de Bruijn CP, de Bie RA, et al. Implications of process evaluation for clinical effectiveness and clinical practice in a trial on chronic shoulder complaints. Patient Educ Couns 2006;61:117–25. [DOI] [PubMed] [Google Scholar]
- [13].van Haastregt JC, van Rossum E, Diederiks JP, de Witte LP, Voorhoeve PM, Crebolder HF. Process-evaluation of a home visit programme to prevent falls and mobility impairments among elderly people at risk. Patient Educ Couns 2002;47:301–9. [DOI] [PubMed] [Google Scholar]
- [14].Dialogue Around Respiratory Illness Treatment. https://www.uwimtr.org/dart/; 2016. accessed Access Day Access Month Access Year]|.
- [15].Kronman MP, Gerber JS, Grundmeier RW, Zhou C, Robinson JD, Heritage J, et al. Reducing Antibiotic Prescribing in Primary Care for Respiratory Illness. Pediatrics 2020;146:e20200038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Mangione-Smith R, Zhou C, Robinson JD, Taylor JA, Elliott MN, Heritage J Communication practices and antibiotic use for acute respiratory tract infections in children. Ann Fam Med 2015;13:221–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mangione-Smith R, McGlynn EA, Elliott MN, McDonald L, Franz CE, Kravitz RL. Parent expectations for antibiotics, doctor-parent communication, and satisfaction. Arch Pediatr Adolesc Med 2001;155:800–6. [DOI] [PubMed] [Google Scholar]
- [18].Fiks AG, Scheindlin B, Shone L 30th Anniversary of Pediatric Research in Office Settings (PROS): An Invitation to Become Engaged. Pediatrics 2016;138:e20161126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Stivers T Non-antibiotic treatment recommendations: delivery formats and implications for parent resistance. Soc Sci Med 2005;60 949–64. [DOI] [PubMed] [Google Scholar]
- [20].Stivers T Treatment decisions: negotiations between doctors and patients in acute care encounters. In: Heritage J, Maynard D (Eds.). Communication in medical care: interactions between primary care physicians and patients, Cambridge: Cambridge University Press; 2006, pp. 279–312. [Google Scholar]
- [21].Stivers T Parent resistance to physicians’ treatment recommendations: one resource for initiating a negotiation of the treatment decision. Health Commun 2005;18:71–4. [DOI] [PubMed] [Google Scholar]
- [22].Montiegel K, Robinson JD. Conversation analysis and health communication. In: Thompson TL, Harrington NG (Eds.). The Routledge Handbook of Health Communication New York: Routledge; 2022, pp. 539–57. [Google Scholar]
- [23].Haan P, Uhlendorff A Estimation of multinomial logit models with unobserved heterogeneity using maximum simulated likelihood. Stata Journal 2006;6:229–45. [Google Scholar]
- [24].Train K Discrete choice methods with simulation. Cambridge University Press; 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 3. Adjusted probability of parents reporting clinician use of preferred communication behavior
Data Availability Statement
Deidentified data limited to anonymous survey data will be shared. No protected health information for study participants will be shared. Data will be provided as a CSV file with a data dictionary defining all variables included in the file and will be transferred using a secure file transfer protocol. Additional tools will not be made available. The data will be made available upon publication of the primary studies to researchers who provide a detailed methodologically sound proposal and data use agreement. Proposals should be submitted to Dr. Mangione-Smith (Rita.M.Mangione-Smith@kp.org).


