Abstract
Fragility fractures of the pelvis (FFP) and fragility fractures of the sacrum (FFS), which are emerging in the geriatric population, exhibit characteristics that differ from those of pelvic ring disruptions occurring in the younger population. Treatment of FFP/FFS by a multidisciplinary team can be helpful in reducing morbidity and mortality with the goal of reducing pain, regaining early mobility, and restoring independence for activities of daily living. Conservative treatment, including bed rest, pain therapy, and mobilization as tolerated, is indicated for treatment of FFP type I and type II as loss of stability is limited with these fractures. Operative treatment is indicated for FFP type II when conservative treatment has failed and for FFP type III and type IV, which are displaced fractures associated with intense pain and increased instability. Minimally invasive stabilization techniques, such as percutaneous fixation, are favored over open reduction internal fixation. There is little evidence regarding outcomes of patients with FFP/FFS and more literature is needed for determination of optimal management. The aim of this article is to provide a concise review of the current literature and a discussion of the latest recommendations for orthopedic treatment and management of FFP/FFS.
Keywords: Osteoporosis, Fractures, Pelvis, Sacrum, Fracture fixation
INTRODUCTION
Fragility fractures of the pelvis (FFP) and fragility fractures of the sacrum (FFS) occur primarily in the geriatric population. The frequency of these injuries is increasing secondary to an aging population and improved diagnostic modalities1). Fragility fractures differ from their high energy counterparts due to osteoporotic bone in the elderly. Because of the vast differences in the two populations, a separate classification system and treatment algorithm are needed for FFP/FFS2,3).
Osteoporosis is defined as an age-related decrease in bone mass leading to a disruption of the microarchitecture of bone. The effects of this pathologic breakdown are potentially devasting, resulting in up to 1.5 million osteoporotic fractures each year4). In evaluation of patients for osteoporosis, a dual energy X-ray absorptiometry t-score of <–2.5 is diagnostic. The fracture risk assessment score (FRAX) is another tool used for calculation of the 10-year risk for major osteoporosis related fractures. Hip fractures commonly seen in individuals 70 to 80 years old are one type of classic osteoporotic fracture predicted by the FRAX score5).
A study conducted by Sullivan et al.6) between 1993 and 2010 demonstrated that the annual incidence of traditional hip fractures peaked in 1996. Of particular interest, the incidence of hip fractures declined by 25.7% over the next 18 years, while the incidence of geriatric pelvic ring fractures increased by 24%6). This trend was also documented in several European countries during the same time period7,8,9,10). According to the hypothesis presented by Kannus et al.7), the increase in FFP is related to the longer life expectancy and improved diagnostic imaging. With the increase in FFP/FFS, understanding the differences in assessment and treatment from the traditional high-energy pelvic fracture is important.
FFP/FFS VERSUS HIGH ENERGY TRAUMA
Pelvic ring injuries typically occur in young patients as a result of trauma. The likelihood of life-threatening hemorrhage and visceral injury due to displacement of fracture fragments causing major soft tissue damage and physiologically important blood loss is high in these patients11). In contrast, FFP/FFS are observed in the geriatric population with low-energy mechanisms of injury. Falls from standing or sitting height are common. Patients may describe a subacute onset of pelvic or low back pain as they either do not recall the injury or there was an accumulation of multiple small events over time12). On evaluation, patients are typically on bed rest with pain in the pelvic region and no life-threatening injuries. However, because slow bleeding can occur, monitoring patients with FFP/FFS is important. There are similarities as increased morbidity and mortality are observed in low and high energy pelvic fractures. Death due to injury is more likely to occur in patients who experience high energy pelvic trauma. However, for low energy pelvic fragility fractures, increased risk of mortality is associated with lack of mobility secondary to pre-existing comorbidities. Andrich et al.13) reported a significant increase in mortality within eight months in patients with low energy pelvic ring injuries. In a study reported by van Dijk et al.14), the one-, five-, and ten-year mortality in patients over 60 years old with isolated pubic ramus fracture was 24.7%, 64.4%, and 93.8%, respectively. Up to one-third of the deaths were the result of cardiovascular events, a 25 times increased risk over matched controls. Findings of these studies highlight the significance of FFP and the effect of comorbidities on morbidity and mortality14).
PATHOPHYSIOLOGY OF FFP/FFS
Although bone loss does not occur uniformly in an osteoporotic pelvis, it occurs with a consistent pattern. Wagner et al.15) reported that excessive bone loss is typically observed at both sacral ala lateral to the foramina and in the sacral bodies at the transition from S1 to S2 and from S2 to S3. Complete loss of bone mass in the sacral ala, described as a sacral void, was demonstrated in a subset of patients15). The most common fracture pattern for FFS is the H-type (bilateral vertical components with a horizontal component), followed by unilateral vertical, and then bilateral vertical fractures. In these injuries the vertical component occurs along the lateral sacral ala, sparing the neural foramina16).
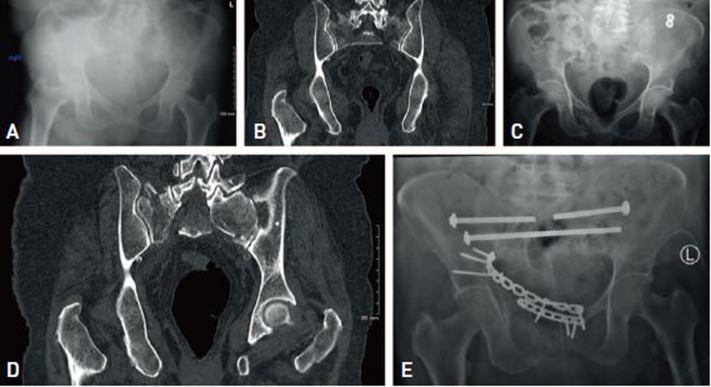
As opposed to low-energy FFP/FFS caused by gradual collapse or “implosion” with progressive loss of stability, high energy pelvic fractures typically present as an eruption of energy within the pelvis, causing significant instability. The history of FFP/FFS typically involves a low energy fall resulting in a pubic ramus fracture, which is treated conservatively. Over time, with recurrent falls or increased mobilization, development of new fractures can occur in the anterior or posterior pelvis leading to progressive instability (Fig. 1). Continual micro-motion of the fragments is created by the combination of increasing rigidity of the ligamentous complex around the osteoporotic bone and unstable bony structure. With this unique pathology bone resorption is promoted, leading to complete destruction of the sacroiliac (SI) joints or pubic symphysis and eventual pelvic collapse17).
Fig. 1. Patient is an 87-year-old female who presented to the emergency department after a ground level fall. She was diagnosed with right minimally displaced superior and inferior pubic ramus fractures (A), and a nondisplaced right Zone 1 sacral ala fracture (B) representing a type IIc fracture. Patient was able to ambulate with assistive device and was discharged home the same day. Patient presented seven weeks after the injury with worsening pain and inability to ambulate. Radiographs demonstrate further displacement of right superior and inferior pubic rami fractures with delayed union and right sacral ala fracture (C); computed tomography scan demonstrates displaced bilateral Zone 1 sacral alar fractures (D) representing a type IVc fracture. Patient was subsequently taken to the operating room for percutaneous bilateral S1 iliosacral screws, S2 trans-sacral-trans-iliac screws, and superior pubic ramus open reduction internal fixation (E).
DIAGNOSIS AND CLASSIFICATION OF FFP/FFS
A comprehensive classification for FFP/FFS based on 245 patients aged >65 years was described by Rommens and Hofmann2). The system is based on standard anterior-posterior, inlet, and outlet radiographs, as well as a computed tomography (CT) scan of the pelvis3). Two major criteria are utilized for the classification: stability of the pelvic ring broken down into four categories and the location of the instability.
FFP type I fractures, indicated by slight instability in the anterior pelvis, account for 17.5% of fractures. Type Ia includes unilateral pubic ramus fractures and type Ib bilateral pubic rami fractures. With involvement of the posterior pelvic ring in over 80% of cases of FFP/FFS, evaluation using CT is crucial for appropriate classification of fractures. Detection of occult fractures of the posterior pelvis may require use of magnetic resonance imaging (MRI)3). MRI is highly sensitive to marrow abnormalities surrounding the fracture line and is useful for identification of occult, nondisplaced fractures of the posterior pelvis, especially in patients with osteoporotic bone18,19,20).
FFP type II fractures, classified as moderate instability, are characterized by nondisplaced posterior pelvic ring fractures and account for 50% of cases of FFP. Type IIa fractures are nondisplaced fractures of the posterior pelvis without an anterior pelvic ring fracture, type IIb fractures involve a crush zone in the sacral ala with anterior pelvic ring fracture, and type IIc involve a nondisplaced sacral, SI, or iliac fractures with associated anterior pelvic ring fracture. Of particular importance, the behavior of FFP/FFS is different from that of high energy pelvic ring fracture, and the ring is not always disrupted in two places.
FFP type III fractures which account for 10% of these injuries, are characterized by unilateral displacement of the posterior pelvis with associated anterior pelvic ring fracture. Despite subtle displacement of the fracture, FFP type III are associated with a high level of instability. Type IIIa is a fracture that occurs through the ilium, type IIIb is a fracture that occurs through the SI joint, and type IIIc is a fracture that occurs through the sacrum, all with associated anterior pelvic ring fractures. Although nondisplaced fractures of the posterior pelvis without anterior pelvic ring fracture have been reported (type IIa), unilateral posterior pelvic displacement without an associated anterior pelvic ring fracture has rarely been reported in the literature and is extremely uncommon21,22).
The highest level of instability is associated with FFP type IV fractures, which account for 20% of these injuries. Type IV fractures are described as bilateral displaced posterior pelvic ring fractures with or without associated anterior pelvic ring fractures. Type IVa are bilateral ilium fractures, type IVb are H-type sacral fractures (with spinopelvic dissociation), and type IVc are described as any combination of injuries not described by type IVa or IVb. With all cases of FFP, progression of stable fracture patterns to more unstable injuries can occur23). In an assessment of the reliability of the classification system proposed by Rommens and Hofmann2), Krappinger et al.24) found that overall reliability was acceptable. However, relatively poor reliability was reported for classification of FFP involving complete nondisplaced or displaced sacral fractures and conduct of future studies to address this issue will be needed24).
TREATMENT OPTIONS
Treatment of patients with FFP/FFS by a team of orthopedic surgeons, geriatricians, internists, pain management specialists, and physical therapists ensures the best opportunity for recovery and results in decreased length of stay and lower mortality rates25). Mitigating potential negative effects of comorbidities is invaluable in the effort to optimize these patients for mobilization. A study reported by van Dijk et al.14) demonstrated that long-term immobilization (median 10 days) of patients with FFP resulted in a complication rate of 20.2%.
The treatment algorithm proposed by Rommens et al.26), which ranges from non-operative to operative, focuses on preserving stability. Conservative management including pain control and early mobilization should be attempted first for FFP type I and type II. Percutaneous fixation may be beneficial in cases where conservative management fails. The focus of operative fixation should be on minimally invasive stabilization, with less importance placed on anatomic reduction. Osterhoff et al.27) reported that early fixation of patients who were not able to mobilize within three to five days resulted in a higher complication rate and mortality at one year, but better long-term survival after two years, suggesting that a patient’s life expectancy may be an important consideration. Percutaneous fixation is favored for minimally displaced FFP type III fractures with open reduction and internal fixation (ORIF) reserved for displaced injuries. FFP type IV fractures should be stabilized in the same manner, but with bilateral fixation of the pelvic ring.
Although numerous strategies for treatment of FFP have been proposed, there is a lack of quality evidence comparing the outcomes of various fixation techniques for FFP22). In a recent systematic review by Wilson et al.22), 17 studies including 766 patients were analyzed; of these, 463 patients underwent operative management. Only one randomized control trial (RCT) and three retrospective studies with non-operative comparator groups were identified; all of these studies were hampered by significant bias. Nevertheless, the authors did report significant improvement in pain and mobility with percutaneous stabilization of the posterior pelvic ring; however, anterior fixation was often absent or performed using variable techniques when present. Wilson et al.22) also noted that operative stabilization of FFP should be considered after 48 hours of failed conservative management in order to avoid morbidity associated with immobility; however, conduct of more high-quality comparative studies is required before definitive conclusions and recommendations can be provided.
1. Conservative Treatment
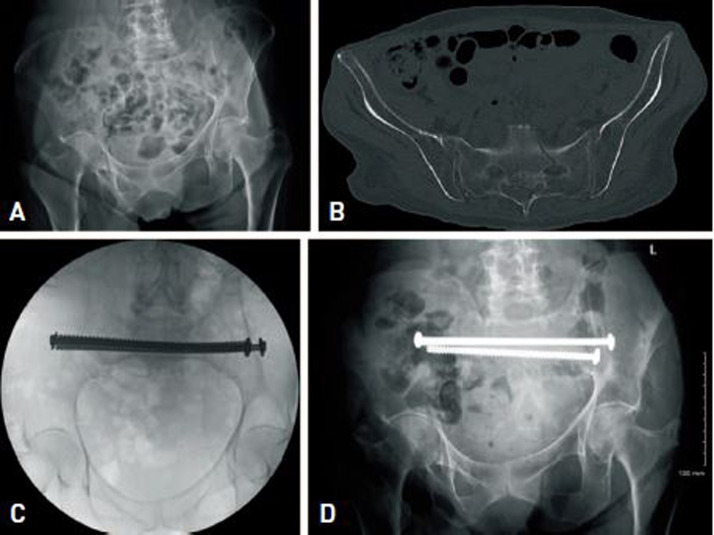
Non-operative treatment should consist of a short period of bed rest, pain control, and early mobilization as tolerated. Mobilization should begin with bed mobility and progress to ambulation28). Diagnostic testing should be repeated after mobilization in order to evaluate for further displacement and possible need for surgical stabilization. Conservative management is considered a failure if pain is unbearable upon attempts by the patient to ambulate (Fig. 2). Unfortunately, data for evaluation of the outcomes of conservative management is limited; however, new studies are emerging. In a recent study reported in 2021, Rommens et al.29) conducted a retrospective comparison of operative vs. conservative management for FFP types II, III, and IV in 238 patients; 100 of these patients received conservative treatment. The study concluded that operative treatment of FFP resulted in lower mortality rates (P<0.001), although longer length of stay (P<0.001) and more in hospital complications (P=0.006) were observed in the operative group29). Patients in the non-operative group had greater mobility and independence at discharge (P<0.001); however, comparable quality of life was observed between the groups29).
Fig. 2. Patient is an 80-year-old female who presented to the emergency department after a ground-level fall and inability to ambulate due to pain. Patient was discharged after negative radiographs (A). A computed tomography of the pelvis was ordered the following day by the patient’s primary care provider which demonstrated a right non-displaced Zone 2 sacrum fracture and a left minimally displaced Zone 2 sacral fracture (fragility fractures of the pelvis type IIA) (B). With continued inability to ambulate the patient was taken to the operating room for bilateral S1 trans-sacral-trans-iliac partially threaded percutaneous screw fixation with fully-threaded S2 trans-sacral-trans-iliac percutaneous screw fixation. Intraoperative pelvic inlet fluoroscopy (C) and postoperative radiograph (D) demonstrate well placed hardware stabilizing the posterior pelvic ring. Patient was able to ambulate with physical therapy postoperative day 1 and was subsequently discharged home. At first follow-up three weeks later, patient was ambulating without assistive device.
In addition, mixed results have been obtained with the use of anabolic agents such as parathyroid hormone (PTH) for conservative treatment of osteoporotic FFP30,31,32). A systematic review including five RCTs conducted by Moon et al.30) reported on the use of PTH on bone-healing in osteoporotic hip and pelvis fractures. The authors concluded that although the rate of treatment failure was lower in the PTH group than in the control group (placebo), the difference was not statistically significant, citing a lack of evidence to confirm the efficacy of PTH in treatment of FFP30). In addition, a RCT conducted by Nieves et al. comparing treatment of FFP with PTH versus placebo reported no evidence of improved healing by CT or pain reduction; however, a statistically significant improvement of physical performance with PTH, but not placebo, was noted31). Moreover, the use of PTH versus placebo for treatment of FFP was also assessed in a retrospective, case-controlled study of 41 patients conducted by Yoo et al.32). The authors concluded that there was a statistically significant improvement in mobilization time as well as fracture healing upon treatment with PTH versus placebo32). Thus, conduct of further studies investigating the use of PTH for conservative treatment of FFP in osteoporotic patients is needed in order to determine its efficacy.
2. Operative Treatment
1) Posterior stabilization procedures
(1) Iliosacral screw osteosynthesis
Iliosacral (IS) screw osteosynthesis is the technique used most commonly in treatment of SI joint dislocations and sacral fractures in high-energy pelvic trauma; however, it is also used in treatment of FFP33,34). Percutaneous IS screw fixation, which is minimally invasive, is performed using cannulated 6.5- to 8-mm screws inserted from the outer cortex of the posterior ilium in the direction of the body of S1 or S2. IS screws have an orientation that is perpendicular to the SI joint for SI dislocations, and perpendicular to the fracture line in sacral ala fractures34). In a study reported in 2004, van Zwienen et al.35) demonstrated that insertion of two IS screws in the S1-S1 or S1-S2 configuration provides additional posterior stability when compared to use of one IS screw. Wagner et al.15) demonstrated that the highest bone mineral density was observed in sacral bodies, thus IS screws should pass through the midline of the sacrum. Long screws that reach the opposite sacral ala should be used in order to prevent screw loosening36). The presence of dysmorphic sacra and reduced size of the S2 corridor compared to S1 can complicate optimal positioning of IS screws34). Use of combined percutaneous IS screws with cement augmentation to increase screw pull out strength and decrease postoperative pain has been described in some studies; however, conduct of long-term follow-up studies is needed before the procedure can become standardized37,38,39,40). In a study conducted in 10 human cadavers, Suero et al.41) demonstrated that a single cement-augmented cannulated IS screw provides stability similar to that of non-cement-augmented double IS screws. A novel procedure using balloon guided cement augmentation of IS screws recently showed promising preliminary data in eight patients, with elimination of cement leakage into the sacrum after injection42). Although not tested in vivo, the use of screw-in-screw fixation, consisting of a 7.3-mm cannulated SI screw and a 2.7-mm locking-head screw at a 15° set angle, has been reported to provide greater stability than a SI screw and prevent screw cutout in nine artificial pelvises43).
(2) Sacroplasty
Sacroplasty involves percutaneous injection of polymethyl methacrylate (PMMA) cement into the sacral trabecular bone to augment FFS by reducing painful micromotion at the fracture site44). Indications for the procedure include bone bruising in the sacrum indicating the onset of trabecular bone fracture. In a meta-analysis conducted by Chandra et al.45) which included 664 patients who underwent sacroplasty for treatment of sacral insufficiency fractures secondary to osteoporosis, the authors concluded that sacroplasty is safe and effective for pain relief in patients with osteoporotic sacral fractures with statistically significant improvement in visual analogue scale scores for pain up to 12 months45). To guide the application of PMMA and minimize the risk of cement leakage through fracture lines with subsequent nerve impaction, a classification system for identification of cortical break and fracture morphology in the sacral bone associated with the greatest risk of cement leakage was proposed by Bakker et al.46). Due to the likelihood of cement leakage, sacroplasty should be avoided in complete sacral fractures. Balloon-assisted sacroplasty, an emerging technique, has been reported to alleviate pain and minimize cement leakage in sacral insufficiency fractures and may be of use in the future47,48).
(3) Transsacral bar osteosynthesis
Transsacral bar osteosynthesis is indicated for treatment of unilateral or bilateral sacral ala fractures. A 6-mm bar is inserted through the posterior ilium and SI joint and advanced through the center of the S1 vertebral body to the opposite posterior ilium49). Compression across the fracture is achieved by tightening of washers and nuts at both ends of the bar against the posterior ilium. CT-guided preoperative analysis of fracture morphology and transsacral corridor dimensions is crucial due to the high variation of sacral anatomy among individuals49). A few studies analyzing the use of transsacral bar osteosynthesis for treatment of FFS have been reported; favorable outcomes for patients were demonstrated in all of these studies50,51,52,53). In a recent study conducted by Wagner et al.54), the use of available space in the sacrum for virtual implants was evaluated; the results showed that S2 more consistently offers space for transsacral implants compared to S1; however, conduct of further studies is needed in order to validate these findings in vivo54).
(4) Transiliac bridging osteosynthesis
Transiliac bridging osteosynthesis, which connects the left and right posterior ilium posterior to the sacrum, is indicated in treatment of mono- or bilateral sacral insufficiency fractures55). The plate functions as a tension-band construct across the sacrum. Two vertical incisions are made at the posterosuperior iliac spine, and the plate is contoured to the anatomy of the posterior ilium. A sub-fascial tunnel is created towards the contralateral spine and the plate is slid through the tunnel. The plate is fixed with cortical screws in each iliac wing. Higher fixation stiffness in the posterior pelvic ring can be obtained with the use of angled plates compared with non-angled plates56,57). The risk of iatrogenic neurovascular lesions is low since the plate is tunneled posterior to the sacrum; however, limited reduction potential, difficulty contouring the plate, and higher rates of symptomatic hardware have been reported57).
(5) Transiliac internal fixation
Transiliac internal fixation is an alternative treatment for unilateral osteoporotic sacral fractures located in the central, transforaminal, or alar region of the sacrum58). Pedicle screws (maximum length 120 mm) are inserted in a craniocaudal direction in the posterior ilium 1-2 cm cranial to the posterior superior iliac spine (PSIS) or in a posterior-anterior direction from the PSIS to the anterior inferior iliac spine (AIIS) and connected with a transverse rod58). Cement augmentation is an option for improving the stability of the implant in osteoporotic bone59). Stability of this technique in treatment of high energy pelvic trauma has been reported; however, few studies regarding treatment of FFP have been reported in the literature60).
(6) Lumbopelvic fixation
Lumbopelvic fixation is indicated for treatment of displaced and unstable injuries such as U- or H-type fractures of the sacrum (type IVb) by connecting the lumbar spine to the posterior ilium61). A 6-mm pedicle screw is inserted into L4-L5 and another 6-mm pedicle screw is inserted into the PSIS directed toward the AIIS with a longitudinal rod connecting the pedicle screws62). The left and right longitudinal rods are connected using a transverse connecting rod. The procedure can be performed percutaneously with use of subcutaneous tunnels for the connecting bars; however, ORIF may be required for highly unstable fractures. Combination of lumbopelvic fixation with IS screws forms a “triangular osteosynthesis” to address multiplanar instabilities usually observed in high-energy pelvic trauma62). Unfortunately, literature evaluating the use of this technique for treatment of FFP is limited63,64).
2) Anterior stabilization procedures
Posterior pelvic ring fractures are normally accompanied by anterior pelvic ring fractures. Instability in the anterior fracture and strain on the posterior fixation can result from fixation of a posterior ring fracture without concurrent fixation of an anterior ring fracture.
(1) External fixation
External fixation is used for temporary stabilization of high energy pelvic ring fractures; however, it has been reported to result in higher rates of complication when used in treatment of FFP26,65). Fixation time is longer when used for FFP compared to pelvic ring fractures in younger adults, increasing the risk of infection. Overall range of motion is restricted and osteoporotic bone in FFP increases the risk of pin loosening. As a result, surgeons have trended away from external fixation for treatment of FFP.
(2) Internal fixation
Indications for internal fixation include unstable unilateral or bilateral pubic rami fractures isolated or combined with posterior pelvic fractures. Bilateral screws are inserted from the AIISs to the PSISs using a curved rod, connected to both screw heads, inserted subcutaneously over the anterior pelvis66). Complications including femoral nerve palsy and damage to the lateral femoral cutaneous nerve have been reported67,68,69).
(3) Retrograde transpubic screw
Superior pubic rami fractures or anterior column acetabular fractures are indications for retrograde transpubic screw fixation70). The corridor of the anterior column passes medially and superiorly to the acetabulum and runs from the anterior cortex near the pubic tubercle to the external cortex of the ilium above the acetabulum70). Solid or cannulated screws can be placed percutaneously in the corridor for stabilization of the fracture26,70,71). A biomechanical analysis of artificial pelvises conducted by Lodde et al.72) found that retrograde transpubic screw fixation is an adequate and minimally invasive technique for treatment of superior pubic ramus fractures.
(4) Plate osteosynthesis
Plate osteosynthesis, which provides the strongest mechanical fixation for pelvic bone, is best indicated for pure ligamentous disruptions of the pubic symphysis or parasymphyseal fractures66). The technique is performed using a transverse suprapubic Pfannenstiel incision or vertical midline incision. The modified Stoppa approach can be used for the majority of anterior pelvic ring fractures66). Small fragment curved plates are used with the longest-possible screw trajectories in order to obtain good purchase17,66). Double plate osteosynthesis is recommended for chronic instabilities or bone defects and is associated with a lower rate and later onset of screw loosening compared to single plate osteosynthesis26,73).
CONCLUSION
Incidence of FFP/FFS has increased significantly due to both an aging population and improved diagnostic modalities. Evaluation and treatment of these patients differ significantly from that of high-energy pelvic ring injuries typically seen in younger patients. Because stable injury patterns often progress to more unstable pelvic ring injuries, appropriate classification, monitoring, and treatment of these patients is important. Non-operative management is often considered first and should focus on early mobility. Operative fixation should focus on stabilization of the minimally invasive pelvic ring in order to facilitate early mobilization and avoid complications that can arise from comorbidities associated with immobility. Further high-quality comparative literature is needed before optimal treatment criteria can become standardized.
ACKNOWLEDGEMENTS
We would like to thank Dr. Donald Adams for his support and invaluable contributions to the final manuscript.
Footnotes
CONFLICT OF INTEREST: The authors declare that there is no potential conflict of interest relevant to this article.
References
- 1.Rommens PM, Hofmann A. Focus on fragility fractures of the pelvis. Eur J Trauma Emerg Surg. 2021;47:1–2. doi: 10.1007/s00068-020-01550-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44:1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 3.Rommens PM, Wagner D, Hofmann A. Do we need a separate classification for fragility fractures of the pelvis? J Orthop Trauma. 2019;33 Suppl 2:S55–S60. doi: 10.1097/BOT.0000000000001402. [DOI] [PubMed] [Google Scholar]
- 4.Gass M, Dawson-Hughes B. Preventing osteoporosis-related fractures: an overview. Am J Med. 2006;119(4 Suppl 1):S3–S11. doi: 10.1016/j.amjmed.2005.12.017. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Scientific group on the assessment of osteoporosis at primary health care level [Internet] Geneva: World Health Organization; 2004. [2021 Jul 7]. Available from: https://www.sheffield.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf . [Google Scholar]
- 6.Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014;37:151–157. doi: 10.3928/01477447-20140225-50. [DOI] [PubMed] [Google Scholar]
- 7.Kannus P, Niemi S, Parkkari J, Sievänen H. Continuously declining incidence of hip fracture in Finland: analysis of nationwide database in 1970-2016. Arch Gerontol Geriatr. 2018;77:64–67. doi: 10.1016/j.archger.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Kannus P, Parkkari J, Niemi S, Sievänen H. Low-trauma pelvic fractures in elderly Finns in 1970-2013. Calcif Tissue Int. 2015;97:577–580. doi: 10.1007/s00223-015-0056-8. [DOI] [PubMed] [Google Scholar]
- 9.Nanninga GL, de Leur K, Panneman MJ, van der Elst M, Hartholt KA. Increasing rates of pelvic fractures among older adults: The Netherlands, 1986-2011. Age Ageing. 2014;43:648–653. doi: 10.1093/ageing/aft212. [DOI] [PubMed] [Google Scholar]
- 10.Andrich S, Haastert B, Neuhaus E, et al. Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS One. 2015;10:e0139078. doi: 10.1371/journal.pone.0139078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29:981–1000. discussion 1000-2. [PubMed] [Google Scholar]
- 12.Krappinger D, Kammerlander C, Hak DJ, Blauth M. Low-energy osteoporotic pelvic fractures. Arch Orthop Trauma Surg. 2010;130:1167–1175. doi: 10.1007/s00402-010-1108-1. [DOI] [PubMed] [Google Scholar]
- 13.Andrich S, Haastert B, Neuhaus E, et al. Excess mortality after pelvic fractures among older people. J Bone Miner Res. 2017;32:1789–1801. doi: 10.1002/jbmr.3116. [DOI] [PubMed] [Google Scholar]
- 14.van Dijk WA, Poeze M, van Helden SH, Brink PR, Verbruggen JP. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury. 2010;41:411–414. doi: 10.1016/j.injury.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Wagner D, Hofmann A, Kamer L, et al. Fragility fractures of the sacrum occur in elderly patients with severe loss of sacral bone mass. Arch Orthop Trauma Surg. 2018;138:971–977. doi: 10.1007/s00402-018-2938-5. [DOI] [PubMed] [Google Scholar]
- 16.Linstrom NJ, Heiserman JE, Kortman KE, et al. Anatomical and biomechanical analyses of the unique and consistent locations of sacral insufficiency fractures. Spine (Phila Pa 1976) 2009;34:309–315. doi: 10.1097/BRS.0b013e318191ea01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rommens PM, Wagner D, Hofmann A. Fragility fractures of the pelvis. JBJS Rev. 2017;5:e3. doi: 10.2106/JBJS.RVW.16.00057. [DOI] [PubMed] [Google Scholar]
- 18.Jarraya M, Hayashi D, Roemer FW, et al. Radiographically occult and subtle fractures: a pictorial review. Radiol Res Pract. 2013;2013:370169. doi: 10.1155/2013/370169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nüchtern JV, Hartel MJ, Henes FO, et al. Significance of clinical examination, CT and MRI scan in the diagnosis of posterior pelvic ring fractures. Injury. 2015;46:315–319. doi: 10.1016/j.injury.2014.10.050. [DOI] [PubMed] [Google Scholar]
- 20.Graul I, Marintschev I, Hackenbroch C, Palm HG, Friemert B, Lang P. Modified therapy concepts for fragility fractures of the pelvis after additional MRI. PLoS One. 2020;15:e0238773. doi: 10.1371/journal.pone.0238773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rommens PM, Hofmann A. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Classification of fragility fractures of the pelvis; pp. 69–80. [Google Scholar]
- 22.Wilson DGG, Kelly J, Rickman M. Operative management of fragility fractures of the pelvis - a systematic review. BMC Musculoskelet Disord. 2021;22:717. doi: 10.1186/s12891-021-04579-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rommens PM, Arand C, Hopf JC, Mehling I, Dietz SO, Wagner D. Progress of instability in fragility fractures of the pelvis: an observational study. Injury. 2019;50:1966–1973. doi: 10.1016/j.injury.2019.08.038. [DOI] [PubMed] [Google Scholar]
- 24.Krappinger D, Kaser V, Kammerlander C, Neuerburg C, Merkel A, Lindtner RA. Inter- and intraobserver reliability and critical analysis of the FFP classification of osteoporotic pelvic ring injuries. Injury. 2019;50:337–343. doi: 10.1016/j.injury.2018.11.027. [DOI] [PubMed] [Google Scholar]
- 25.Patel JN, Klein DS, Sreekumar S, Liporace FA, Yoon RS. Outcomes in multidisciplinary team-based approach in geriatric hip fracture care: a systematic review. J Am Acad Orthop Surg. 2020;28:128–133. doi: 10.5435/JAAOS-D-18-00425. [DOI] [PubMed] [Google Scholar]
- 26.Rommens PM, Arand C, Hofmann A, Wagner D. When and how to operate fragility fractures of the pelvis? Indian J Orthop. 2019;53:128–137. doi: 10.4103/ortho.IJOrtho_631_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osterhoff G, Noser J, Held U, Werner CML, Pape HC, Dietrich M. Early operative versus nonoperative treatment of fragility fractures of the pelvis: a propensity-matched multicenter study. J Orthop Trauma. 2019;33:e410–e415. doi: 10.1097/BOT.0000000000001584. [DOI] [PubMed] [Google Scholar]
- 28.Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2000;79:404–409. doi: 10.1097/00002060-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 29.Rommens PM, Boudissa M, Krämer S, Kisilak M, Hofmann A, Wagner D. Operative treatment of fragility fractures of the pelvis is connected with lower mortality. A single institution experience. PLoS One. 2021;16:e0253408. doi: 10.1371/journal.pone.0253408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moon NH, Jang JH, Shin WC, Jung SJ. Effects of teriparatide on treatment outcomes in osteoporotic hip and pelvic bone fractures: meta-analysis and systematic review of randomized controlled trials. Hip Pelvis. 2020;32:182–191. doi: 10.5371/hp.2020.32.4.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nieves JW, Cosman F, McMahon D, et al. Teriparatide and pelvic fracture healing: a phase 2 randomized controlled trial. Osteoporos Int. 2022;33:239–250. doi: 10.1007/s00198-021-06065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yoo JI, Ha YC, Ryu HJ, et al. Teriparatide treatment in elderly patients with sacral insufficiency fracture. J Clin Endocrinol Metab. 2017;102:560–565. doi: 10.1210/jc.2016-3582. [DOI] [PubMed] [Google Scholar]
- 33.Gänsslen A, Lindahl J, Kobbe P. In: Pelvic ring fractures. Gänsslen A, Lindahl J, Grechenig S, Füchtmeier B, editors. Cham: Springer Nature; 2021. Iliosacral screw fixation; pp. 393–435. [Google Scholar]
- 34.Rommens PM, Wagner D, Hofmann A. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Iliosacral screw osteosynthesis; pp. 121–137. [Google Scholar]
- 35.van Zwienen CM, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004;18:589–595. doi: 10.1097/00005131-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Zhao Y, Li J, Wang D, Liu Y, Tan J, Zhang S. Comparison of stability of two kinds of sacro-iliac screws in the fixation of bilateral sacral fractures in a finite element model. Injury. 2012;43:490–494. doi: 10.1016/j.injury.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 37.Collinge CA, Crist BD. Combined percutaneous iliosacral screw fixation with sacroplasty using resorbable calcium phosphate cement for osteoporotic pelvic fractures requiring surgery. J Orthop Trauma. 2016;30:e217–e222. doi: 10.1097/BOT.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 38.Wähnert D, Raschke MJ, Fuchs T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum: a new method using modified implants. Int Orthop. 2013;37:1147–1150. doi: 10.1007/s00264-013-1875-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.König MA, Hediger S, Schmitt JW, Jentzsch T, Sprengel K, Werner CML. In-screw cement augmentation for iliosacral screw fixation in posterior ring pathologies with insufficient bone stock. Eur J Trauma Emerg Surg. 2018;44:203–210. doi: 10.1007/s00068-016-0681-6. [DOI] [PubMed] [Google Scholar]
- 40.Hartensuer R, Lodde MF, Keller J, et al. Safety, effect and feasibility of percutaneous SI-screw with and without augmentation-a 15-year retrospective analysis on over 640 screws. J Clin Med. 2020;9:2660. doi: 10.3390/jcm9082660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suero EM, Greiner A, Becker CA, et al. Biomechanical stability of sacroiliac screw osteosynthesis with and without cement augmentation. Injury. 2021;52:2707–2711. doi: 10.1016/j.injury.2020.01.043. [DOI] [PubMed] [Google Scholar]
- 42.Sandmann GH, Stöckle U, Freude T, Stuby FM. Balloon guided cement augmentation of iliosacral screws in the treatment of insufficiency fractures of the sacrum-description of a new method and preliminary results. Acta Chir Orthop Traumatol Cech. 2018;85:85–88. [PubMed] [Google Scholar]
- 43.Zderic I, Wagner D, Schopper C, et al. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening-biomechanical evaluation of a new concept. J Orthop Res. 2021;39:761–770. doi: 10.1002/jor.24895. [DOI] [PubMed] [Google Scholar]
- 44.Bastian JD, Keel MJB. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Sacroplasty; pp. 105–117. [Google Scholar]
- 45.Chandra V, Wajswol E, Shukla P, Contractor S, Kumar A. Safety and efficacy of sacroplasty for sacral fractures: a systematic review and meta-analysis. J Vasc Interv Radiol. 2019;30:1845–1854. doi: 10.1016/j.jvir.2019.06.013. [DOI] [PubMed] [Google Scholar]
- 46.Bakker G, Hattingen J, Stuetzer H, Isenberg J. Sacral insufficiency fractures: how to classify? J Korean Neurosurg Soc. 2018;61:258–266. doi: 10.3340/jkns.2017.0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schwetje D, Wahd YESH, Bornemann R, Jansen TR, Pflugmacher R, Kasapovic A. Balloon-assisted sacroplasty as a successful procedure for osteoporotic sacral insufficiency fractures after failure of the conservative treatment. Sci Rep. 2020;10:18455. doi: 10.1038/s41598-020-75384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Urits I, Orhurhu V, Callan J, et al. Sacral insufficiency fractures: a review of risk factors, clinical presentation, and management. Curr Pain Headache Rep. 2020;24:10. doi: 10.1007/s11916-020-0848-z. [DOI] [PubMed] [Google Scholar]
- 49.Hofmann A, Rommens PM. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Transsacral bar osteosynthesis; pp. 145–156. [Google Scholar]
- 50.Sciubba DM, Wolinsky JP, Than KD, Gokaslan ZL, Witham TF, Murphy KP. CT fluoroscopically guided percutaneous placement of transiliosacral rod for sacral insufficiency fracture: case report and technique. AJNR Am J Neuroradiol. 2007;28:1451–1454. doi: 10.3174/ajnr.A0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vanderschot P, Kuppers M, Sermon A, Lateur L. Transiliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J Orthop. 2009;43:245–252. doi: 10.4103/0019-5413.53454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Operative technique and outcome. Injury. 2012;43:446–451. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 53.Wagner D, Kisilak M, Porcheron G, et al. Trans-sacral bar osteosynthesis provides low mortality and high mobility in patients with fragility fractures of the pelvis. Sci Rep. 2021;11:14201. doi: 10.1038/s41598-021-93559-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagner D, Kamer L, Sawaguchi T, et al. Space available for trans-sacral implants to treat fractures of the pelvis assessed by virtual implant positioning. Arch Orthop Trauma Surg. 2019;139:1385–1391. doi: 10.1007/s00402-019-03204-9. [DOI] [PubMed] [Google Scholar]
- 55.Hockertz T. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Bridging plate osteosynthesis; pp. 157–164. [Google Scholar]
- 56.Kobbe P, Hockertz I, Sellei RM, Reilmann H, Hockertz T. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop. 2012;36:159–164. doi: 10.1007/s00264-011-1279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Krappinger D, Larndorfer R, Struve P, Rosenberger R, Arora R, Blauth M. Minimally invasive transiliac plate osteosynthesis for type C injuries of the pelvic ring: a clinical and radiological follow-up. J Orthop Trauma. 2007;21:595–602. doi: 10.1097/BOT.0b013e318158abcf. [DOI] [PubMed] [Google Scholar]
- 58.Müller M, Schmitz P, Nerlich M. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Transiliac internal fixator; pp. 165–174. [Google Scholar]
- 59.Schmitz P, Baumann F, Grechenig S, Gaensslen A, Nerlich M, Müller MB. The cement-augmented transiliacal internal fixator (caTIFI): an innovative surgical technique for stabilization of fragility fractures of the pelvis. Injury. 2015;46 Suppl 4:S114–S120. doi: 10.1016/S0020-1383(15)30029-2. [DOI] [PubMed] [Google Scholar]
- 60.Dienstknecht T, Berner A, Lenich A, Nerlich M, Fuechtmeier B. A minimally invasive stabilizing system for dorsal pelvic ring injuries. Clin Orthop Relat Res. 2011;469:3209–3217. doi: 10.1007/s11999-011-1922-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lindahl J, Gänsslen A. In: Pelvic ring fractures. Gänsslen A, Lindahl J, Grechenig S, Füchtmeier B, editors. Cham: Springer Nature; 2021. Lumbopelvic fixation; pp. 473–500. [Google Scholar]
- 62.Schildhauer TA, Chapman JR. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Triangular osteosynthesis and lumbopelvic fixation; pp. 175–189. [Google Scholar]
- 63.Maki S, Nakamura K, Yamauchi T, et al. Lumbopelvic fixation for sacral insufficiency fracture presenting with sphincter dysfunction. Case Rep Orthop. 2019;2019:9097876. doi: 10.1155/2019/9097876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Roetman B, Schildhauer TA. Lumbopelvine Stabilisierung bei bilateraler lumbosakraler Instabilität. Unfallchirurg. 2013;116:991–999. doi: 10.1007/s00113-012-2338-1. [DOI] [PubMed] [Google Scholar]
- 65.Rommens PM, Arand C, Thomczyk S, Handrich K, Wagner D, Hofmann A. Fragility fractures of the pelvis. Unfallchirurg. 2019;122:469–482. doi: 10.1007/s00113-019-0643-7. [DOI] [PubMed] [Google Scholar]
- 66.Cole PA, Dyskin EA, Gilbertson JA, Mayr E. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Plate osteosynthesis, subcutaneous internal fixation and anterior pelvic bridge fixation; pp. 225–248. [Google Scholar]
- 67.Apivatthakakul T, Rujiwattanapong N. “Anterior subcutaneous pelvic internal fixator (INFIX), is it safe?” A cadaveric study. Injury. 2016;47:2077–2080. doi: 10.1016/j.injury.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 68.Fang C, Alabdulrahman H, Pape HC. Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop. 2017;41:1785–1790. doi: 10.1007/s00264-017-3415-4. [DOI] [PubMed] [Google Scholar]
- 69.Hesse D, Kandmir U, Solberg B, et al. Femoral nerve palsy after pelvic fracture treated with INFIX: a case series. J Orthop Trauma. 2015;29:138–143. doi: 10.1097/BOT.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 70.Rommens PM, Wagner D, Hofmann A. In: Fragility fractures of the pelvis. Rommens PM, Hofmann A, editors. Cham: Springer Nature; 2017. Retrograde transpubic screw fixation; pp. 211–223. [Google Scholar]
- 71.Rommens PM, Graafen M, Arand C, Mehling I, Hofmann A, Wagner D. Minimal-invasive stabilization of anterior pelvic ring fractures with retrograde transpubic screws. Injury. 2020;51:340–346. doi: 10.1016/j.injury.2019.12.018. [DOI] [PubMed] [Google Scholar]
- 72.Lodde MF, Katthagen JC, Schopper CO, et al. Biomechanical comparison of five fixation techniques for unstable fragility fractures of the pelvic ring. J Clin Med. 2021;10:2326. doi: 10.3390/jcm10112326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Herteleer M, Boudissa M, Hofmann A, Wagner D, Rommens PM. Plate fixation of the anterior pelvic ring in patients with fragility fractures of the pelvis. Eur J Trauma Emerg Surg. 2021 Mar 11; doi: 10.1007/s00068-021-01625-z. [DOI] [PMC free article] [PubMed] [Google Scholar]