Abstract
Objectives
Poor control of asthma in the majority of patients could be partly due to their lack of knowledge concerning disease management, its triggering agents and when to seek advice from the healthcare provider. This study aims to assess the impact of pharmacist-led educational intervention on knowledge of self-management among asthmatic patients.
Design
A pre–post cohort study.
Setting
Outpatient department of a tertiary care hospital affiliated with Quaid-i-Azam University, Pakistan.
Participants
Approximately 265 adult asthmatic patients selected through a spirometry process, aged ≥18 years, were approached. 240 patients gave consent to participate in the study and were divided into control and treatment groups.
Interventions
The educational intervention consisted of individual patient counselling using educational material with time varied according to each patient’s comprehension and previous knowledge.
Primary and secondary outcome measures
Assessment consisted of a 14-item Asthma Self-Management Knowledge Questionnaire (ASMQ) quantifying a patient’s self-management knowledge through an ASMQ score and its change following an educational intervention.
Results
Disease self-management knowledge was low with an average raw ASMQ score of 4.1 (max 14); which equates to a transformed score of 29.34 (max 100) and the proportion of patients who correctly answered more than 50% of questions were 16.7% preintervention. More than half of the participants (55%) did not know that asthma cannot be cured. The administration of educational intervention protocols resulted in significantly improved level of knowledge of asthma self-management (<0.001) in the treatment group (mean ASMQ score improved from 4.20 to 9.77).
Conclusion
On baseline visit, patients possessed a poor knowledge about asthma self-management. Educational intervention protocols had a positive impact on improving patients’ knowledge about disease self-management. This would suggest that education and self-management skills should be seen as an integral component of asthma management and should be incorporated in structured patient care to achieve optimal asthma control.
Keywords: health informatics, public health, respiratory medicine (see thoracic medicine)
Strengths and limitations of this study.
Adherence to clearly defined inclusion and exclusion criteria.
A cohort study using a parallel control group for comparison.
An appropriate sample size consisting of representative asthmatic patients.
Participants were recruited only from a single centre.
Scarcity of tools to measure the asthma self-management knowledge.
Introduction
Asthma has over many years become one of the major health concerns affecting millions of people1 and is defined as a chronic, non-communicable inflammatory disorder of the airways, which affects 334 million people worldwide with an alarming prediction of an increase in 100 million more by the year 2025.1 2 Considering the most leading causes of disease which burdens society, asthma ranks 28th, causing approximately 1000 people to die every day around the globe. In addition, it ranks 16th among the leading causes of years of life lived with a disability and its prevalence is still rising in underdeveloped countries.3
Globally, asthma is becoming a growing contributor of increased morbidity and mortality and, thus, imposing a significant burden in terms of reducing productivity, not only on the patients but also on their families and healthcare systems.2 Genetic predisposition and exposure to numerous environmental substances including dust mites, pet dander, pollens as well as stress or sedentary lifestyle collectively accounts as contributing factors for developing and high prevalence of poorly controlled asthma.4
Despite the availability of effective diagnostic and treatment strategies, asthma is still poorly controlled in the majority of patients and its incidence is on the rise.5 6 Various reasons for such a low asthma control includes either healthcare system-related issues (unaffordability or unavailability of medications) or physician-related issues (incorrect or misdiagnosis, lack of proper diagnostic facilities, insufficient time to discuss matters with the patients, absence of reassessment of inhaler technique or lack of proper follow-up measures) or patient-related issues (non-compliant behaviours due to lack of knowledge about their disease and its management).5 In addition to non-adherence to the proper medication regimen, lack of proper education or routine follow-up, incorrect use of inhaler and lack of inhaler technique assessment during the patient visit also play a significant role in the suboptimal control of asthma.6 Being a controllable disease, asthma requires a prolonged guidelines compliant therapy along with patient education about the correct use of the prescribed medications and disease self-management.5 7
The patients’ general knowledge about asthma includes the pathophysiology of the disease, the purpose of the specific treatment regimen, recognition and management of exacerbations/disease triggers and especially, correct use of the inhaler.5 Self-management is defined as the ability of an individual to apply the appropriate guidelines or make informed decisions for managing their chronic conditions. This requires the efficient communication about patients’ condition with their family members, companions and healthcare professionals.8 Asthma self-management furthermore involves actions undertaken by the patients to monitor their disease symptoms and avoid exacerbations.9 The existing published literature signifies that asthma self-management is conditional on the education received by the patients since this improves their understanding of their treatment rationale and monitoring thereof and when made a part of their regular and planned care, not only improves asthma control and their quality of life but also reduces the healthcare costs by decreasing the frequency of hospital and emergency room visits and absenteeism from the work places.2 Variability of asthma disease (change in asthma over time) implies that exacerbations can possibly occur even if a patient’s asthma is well controlled. Therefore, patients should have the knowledge about their disease management and recognition of factors to indicate when to seek help from health professionals when confronted with such exacerbations.5
Despite well-documented evidence of the positive impact of asthma self-management programmes in achieving the desired patient outcomes and reducing healthcare costs, it is unfortunately rarely implemented in routine clinical practice.1 2 5
Despite being the sixth most populous country in the world and harbouring a high burden of asthma patients, there remains a scarcity of published information regarding the patients’ knowledge and impact of the educational intervention about asthma self-management in Pakistan. Therefore, the current study was conducted with the objective to evaluate the knowledge of disease self-management among established asthmatic patients and the impact of an educational intervention might illustrate to address this finding.
Methodology
Study setting and design
The cohort study was carried out at the pulmonology outpatient department of the Pakistan Institute of Medical Sciences, a tertiary care hospital located in the capital territory of Islamabad Pakistan. All asthmatic patients were selected through a spirometry process and were at least 18 years old. These patients visited the study site from May to September 2019 and were willing participants by giving their written consent. Those patients who were unable to communicate adequately, had a cognitive abnormality or any other disease with asthma-related symptoms such as chronic obstructive pulmonary disease, tuberculosis or a weak heart, were excluded. The Quasi experimental design was used. Participants in the study group were arbitrarily assigned to control and treatment groups. Both groups were roughly similar in terms of sociodemographic characteristics and asthma self-management knowledge resulting from a baseline visit. The educational intervention was provided to the treatment group. The baseline patients’ sociodemographic characteristics as well as knowledge of asthma self-management were assessed via a face-to-face interview. Educational material included specifically designed pamphlets. The principal author (SSS) provided educational counselling and evaluated the inhaler technique of each patient in the treatment group at baseline and follow-up visits. All educational counselling was provided to the control group patients on follow-up visits only along with evaluating their inhaler technique. Time allocated for counselling varied according to each patients’ comprehension and previous knowledge of their condition.
Data collection tools
A purpose developed data collection form was used to obtain the patients’ sociodemographic characteristics from their medical records and in one-on-one interviews with the patient. In order to evaluate a patients’ knowledge about what self-management of asthma meant, the principal investigator administered ASMQ forms to the patients.
The ASMQ contained 16 multiple-choice questions about preventive measures, use of inhalers, medications and peak flow metres.10 Tool scores were calculated by giving one point to each preferred response. For generating raw ASMQ scores, all answers were summed up and transformed to a score ranging between 0 and 100. Higher transformed scores on ASMQ signified a higher knowledge about self-management of asthma.5 Two questions related to the peak flow metres were omitted due to their minimum use in developing countries. This process generated an ASMQ raw score, which ranged from 0 to 14.11
Data compilation and statistical analysis
IBM SPSS Statistic V.21 was employed for data analysis. Descriptive statistics was used to summarise the mean and SD of the demographic variables of both groups, viz., treatment and control. Categorical variables were analysed using the χ2 test. For intragroup comparisons, the Wilcoxon matched pair test was used. A p value of ≤0.05 was labelled statistically significant.
Patient and public involvement
Patients were not involved in the design and conduction of this study.
Results
Approximately 265 adult asthmatic patients aged ≥18 years were initially approached. Among them, a total of 240 patients gave their consent to participate in the study. The majority of participants (47.5%) belonged to the age group of 36–55 years, of which 56.7% were men, and 15.4% had a history of an allergy while 25.4% had a positive family history of asthma (table 1). 47.5% of the study group were categorised as not working and 32.9% as white collar workers according to the International Standard Classification of Occupations categories for occupational status.12
Table 1.
Sociodemographics of study participants
| Characteristics | Categories | CG | TG | P value |
| Age | 39.46±13.5 | 39.70±13.99 | 0.892 | |
| Age categories | 18–35 | 27 | 32 | 0.881 |
| 36–55 | 54 | 60 | ||
| >56 | 39 | 28 | ||
| Gender | Male | 61 | 75 | 0.068 |
| Female | 59 | 45 | ||
| Residence | Rural | 75 | 66 | 0.597 |
| Urban | 45 | 54 | ||
| Occupation | Not working | 61 | 53 | 0.827 |
| (ISO categories) | Blue collar worker | 25 | 22 | |
| White collar worker | 34 | 45 | ||
| Educational | Illiterate | 20 | 24 | 0.870 |
| Status | Primary | 36 | 40 | |
| Secondary | 37 | 27 | ||
| Graduate | 27 | 29 | ||
| Family history | Asthma | 30 | 26 | 0.846 |
| Allergy | 22 | 15 | ||
| Both | 30 | 35 | ||
| None | 38 | 44 | ||
| Smoking status | Ex-smokers | 22 | 27 | 0.927 |
| Current-smokers | 33 | 38 | ||
| Never-smoke | 65 | 55 | ||
| Disease duration | ≤2 | 47 | 51 | 0.978 |
| Categories (years.) | 2–5 | 45 | 34 | |
| >5 | 28 | 35 |
CG, Control Group; ISO, International Standard Classification of Occupations; TG, Treatment Group.
Pre and postintervention ASMQ raw and transformed scores are presented in table 2. No statistically significant difference in the ASMQ raw and transformed scores was observed in control group (p value=0.487). However, as a result of educational intervention, there was a statistically significant change in these scores in the treatment group (p value <0.001).
Table 2.
Pre and post ASMQ categories, ASMQ raw and transformed scores in control and treatment group
| Pre | Post | P value | |
| ASMQ raw score | |||
| Control group | 4.01±3.32 | 3.89±2.92 | 0.487 |
| Treatment group | 4.20±3.03 | 9.77±2.58 | <0.001 |
| ASMQ transformed score | |||
| Control group | 28.69±23.75 | 27.76±20.86 | 0.487 |
| Treatment group | 30±21.64 | 69.83±18.42 | <0.001 |
ASMQ, Asthma Self-Management Knowledge Questionnaire.
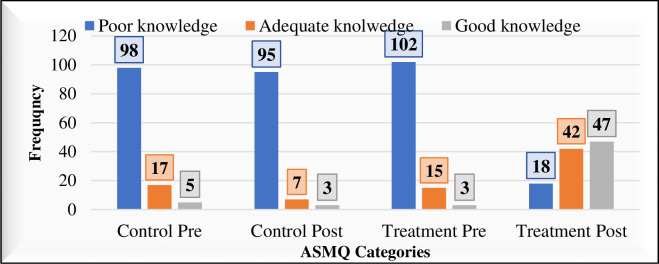
Figure 1 illustrates that as a result of the educational intervention, the number of patients possessing a good knowledge improved from 3 to 47 and those possessing adequate knowledge improved from 15 to 42 in the treatment group. Patients’ knowledge was categorised on the basis of a transformed score as: good (>75), adequate (50–75) and poor (<50).
Figure 1.
Pre and post ASMQ categories in the control and treatment group. ASMQ, Asthma Self-Management Knowledge Questionnaire.
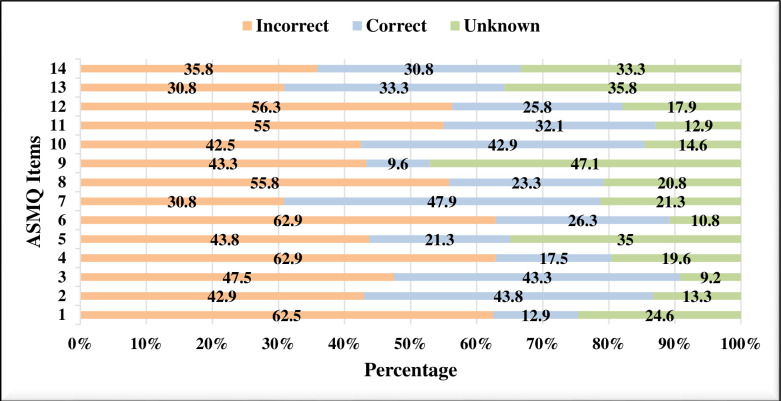
Figure 2 illustrates that question 7 (the holding of breath after use of an inhaler for several seconds) has the highest percentage of correct answers, that is, 47.9%. Only 32.1% of the participants knew that asthma is an incurable disease, which emphasises the need for a comprehensive patients’ education about the regular uptake of medications to achieve disease control. Item 9 (patients’ increased need for maintenance medicines in case he/she is using more rescue medications than are prescribed) was frequently answered to be unknown (47.1%).
Figure 2.
Responses to 14 items of ASMQ at baseline. ASMQ, Asthma Self-Management Knowledge Questionnaire.
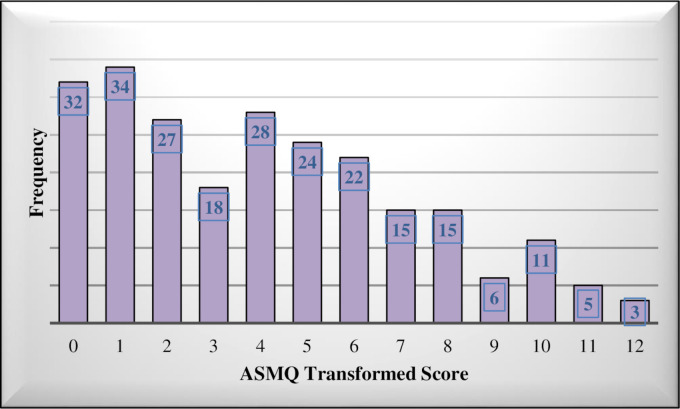
Figure 3 illustrates the distribution of the raw ASMQ score at baseline. 0–14 is the total possible range with higher scores resulting in higher ASMQ transformed scores and, thus, indicating a better asthma self-management knowledge. This underlying distribution of ASMQ raw scores indicates a poor disease management knowledge among the study participants.
Figure 3.
Distribution of raw ASMQ score at baseline. 0–14 is total possible range with higher scores resulting in higher ASMQ transformed score and thus good asthma self-management knowledge. ASMQ, Asthma Self-Management Knowledge Questionnaire.
Discussion
To the best of our knowledge, this is probably the first study conducted in Pakistan to assess the patient’s self-management knowledge of their asthma condition and the impact of an educational intervention might have to manage this condition. The findings of the current study signify that at the baseline visit, the majority of the study participants (83.3%) were poorly educated about the self-management of asthma, and their knowledge was significantly improved after an educational intervention. Likewise, findings regarding the patients’ poor knowledge about asthma self-management have been reported by studies conducted elsewhere. For example, a study conducted by Nguyen et al in Vietnam reported a poor knowledge with a mean raw ASMQ score of 4.3 which equates to the transformed score of 30.5 Similarly, another observational study conducted in the Kingdom of Saudi Arabia reported an average ASMQ score of 3.5 (3.5/14).13 The format of both of these studies was similar to that of the present study after the two items related to the peak flow metre were similarly removed.5 Likewise, a study conducted in Sri Lanka reported that only 34% of the patients were knowledgeable about their disease and medications.5
A multicentre study in China reported a low level of disease awareness among the parents of asthmatic children.14 Another study illustrated that 62.7% of asthmatics have poor, 12% have good and only 25.3% possess an adequate knowledge of their condition.15 Similar studies showed that although the patients have a positive attitude towards the disease, their specific disease knowledge was low.16 17 In our study, the proportion of patients (16.7%) who correctly answered more than 50% of the questions was greater than that reported by Al et al,13 (4%) but similar to that reported by Nguyen et al (16.5%).5
Despite the significance of the correct use of inhaler devices, including the metre dose inhaler in optimal control of asthma, there have been reports of its incorrect use.5 We found that only 47.9% of the participants in the current study had the correct knowledge about the holding of breath after inhaling for several seconds, and 23.8% agreed with the misconception about consecutively taking the second puff as soon as possible after the first. Only 26.3% knew that they should inhale slowly and 63% did not know about the correct use of the inhaler. This strongly suggests that there is a need for patient education through healthcare providers on the correct procedure of the inhalation technique. Lack of health education and regular follow-up visits has previously been reported as the predictors of incorrect inhaler use and poor asthma control.18 Significant improvement through education at follow-ups (p=0.000) in the inhalation technique through assessing and demonstrating the correct inhaler technique has been reported by another study.19 Therefore, healthcare providers should regularly demonstrate and re-evaluate the patients’ inhaler technique at each visit to prevent or reduce the chances for errors in the inhalation technique.5
Despite being an incurable disease, 55% of the current study group were of the opinion that it can be cured, thus equating control with cure. Similar findings regarding the patients’ misconception that asthma is curable have been reported by studies conducted in Vietnam and Saudi Arabia.5 20 Furthermore, there was a lack of knowledge about control and rescue medications: for example, 36.3% of the current study participants answered that breathing becomes better immediately after taking the maintenance medicines, and 30.8% thought that future flare-ups can be prevented by using rescue medicines. These misconceptions and lack of knowledge were also reported by Al et al, stating that only 22% and 16.6% of the participants had correct knowledge about controller and rescue medicines. Similar poor knowledge about the correct use of maintenance and rescue medicines has been reported from Vietnam.5 13 In the current study, a response regarding what to do when manifesting asthma symptoms and not knowing their cause, only 23.3% answered correctly to change one’s immediate environment.
The low level of patients’ knowledge of asthma self-management found in the current study and studies conducted elsewhere emphasise the importance of educational programmes among patients with asthma. In the current study, the pharmacist administered educational intervention in the treatment group significantly increased the mean ASMQ score from 4.20/14 to 9.77/14 (transformed score 69.83/100). On the other hand, no significant increase in these scores was observed in the control group. In the current study, educational intervention increased the number of patients with >50 ASMQ score up to 89 in the treatment group. This is in agreement with the results of an intervention study in which a full version of ASMQ (all 16 items) was used. The study reported a statistically significant increase in the ASMQ score for the group of patients who received an educational intervention.19 A similar positive impact of an educational intervention on patients’ self-management knowledge of asthma, medication adherence and asthma control (60% better control and 18% well controlled) has also been reported.21
Likewise, the positive impact of patient-tailored educational interventions on knowledge about disease self-management, better disease control, treatment outcomes and patients’ health-related quality of life has been reported by studies conducted elsewhere.18 21–25 This specifically applies to the shift of modern treatment goals to early detection and prevention of exacerbations, effective strategies including either broad commitments and interactive educational sessions at different healthcare levels and a cost-effective approach for underdeveloped countries.26 27
Conclusion
The low level of asthma self-management knowledge and positive impact of educational intervention in reducing current knowledge gaps emphasise the need for designing and implementation of educational programmes, ongoing monitoring and regular follow-ups in such a way to fit all patient needs especially including the less educated ones. Assessment of patient’s self-management knowledge provides room for designing specific programmes aimed at the areas where knowledge deficits are evident, thus providing a cost-effective approach, which otherwise is impossible because of resource and time limitations. Moreover, regular and repeated assessment of inhaler technique, if made necessary, will optimise the therapeutic benefits and help to achieve better disease control.
Supplementary Material
Acknowledgments
We would like to express our sincere gratitude to our colleagues from Department of Pharmacy, Quaid-i-Azam University along with doctors, pharmacists and nursing staff from Department of Pulmonology, Pakistan Institute of Medical Sciences (PIMS), Islamabad for their kind support throughout our research period.
Footnotes
Contributors: All authors (SSidraS, AmK, RA, SSadiaS, AB, NA, SMu, SMe, IRG, SAR, AhK, KUS) have conceptualised and designed the study. SSidraS, RA and SSadiaS collected the data. SSidraS, AmK, SMu and KUS have contributed to the data acquisition and analysis. SSidraS drafted the manuscript and AmK, NA, AB, SMe, SAR and AhK have reviewed the manuscript critically. IRG attended to the English language used in the manuscript. All authors read and have approved the final manuscript. The study is supervised by AmK and KUS and are guarantors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Bioethics Committee of Quaid-i-Azam University, Islamabad and Institutional review board of PIMS [F.1-1/2019 (EC) PIMS]. Participants gave informed consent to participate in the study before taking part.
References
- 1.Wireklint P, Hasselgren M, Montgomery S, et al. Factors associated with knowledge of self-management of worsening asthma in primary care patients: a cross-sectional study. J Asthma 2021;58:1087–93. 10.1080/02770903.2020.1753209 [DOI] [PubMed] [Google Scholar]
- 2.Farzandipour M, Nabovati E, Heidarzadeh Arani M, et al. Enhancing asthma patients' self-management through smartphone-based application: design, usability evaluation, and educational intervention. Appl Clin Inform 2019;10:870–8. 10.1055/s-0039-1700866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Global Asthma Network . Global asthma network. the global asthma report 2014. Auckland, New Zealand: Global Asthma Network, 2014. [Google Scholar]
- 4.Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ 2009;181:E181–90. 10.1503/cmaj.080612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen VN, Huynh TTH, Chavannes NH. Knowledge on self-management and levels of asthma control among adult patients in Ho Chi Minh City, Vietnam. Int J Gen Med 2018;11:81–9. 10.2147/IJGM.S157050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabar MF, Akram M, Awan FI. Awareness of asthma genetics in Pakistan: a review with some recommendations. Adv Life Sci 2018;6:1–10. [Google Scholar]
- 7.Irfan O, Irfan B, Khan ZA, et al. Knowledge about asthma: a cross-sectional survey in 4 major hospitals of Karachi, Pakistan. J Pak Med Assoc 2017;67:1787. [PubMed] [Google Scholar]
- 8.Holley S, Walker D, Knibb R, et al. Barriers and facilitators to self-management of asthma in adolescents: an interview study to inform development of a novel intervention. Clin Exp Allergy 2018;48:944–56. 10.1111/cea.13141 [DOI] [PubMed] [Google Scholar]
- 9.Mancuso CA, Sayles W, Allegrante JP. Knowledge, attitude, and self-efficacy in asthma self-management and quality of life. J Asthma 2010;47:883–8. 10.3109/02770903.2010.492540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mancuso CA, Sayles W, Allegrante JP. Development and testing of the asthma self-management questionnaire. Ann Allergy Asthma Immunol 2009;102:294–302. 10.1016/S1081-1206(10)60334-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotwani A, Shendge S. Asthma self-management: a study in an emergency room of a chest hospital in Delhi, India. South Med Rev 2012;5:20. [PMC free article] [PubMed] [Google Scholar]
- 12.Razzaq S, Nafees AA, Rabbani U, et al. Epidemiology of asthma and associated factors in an urban Pakistani population: adult asthma study-Karachi. BMC Pulm Med 2018;18:1–13. 10.1186/s12890-018-0753-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.AI E, Alharthi B, Alharthi S. Self-Management and control of asthma among adult patients in King Faisal medical complex Taif, KSA 2017.
- 14.Zhao J, Shen K, Xiang L, et al. The knowledge, attitudes and practices of parents of children with asthma in 29 cities of China: a multi-center study. BMC Pediatr 2013;13:1–6. 10.1186/1471-2431-13-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbas N, Amen M. Knowledge on self-management and level of asthma control among adult asthmatic patients attending Kalar General Hospital. Journal of Garmian University 2019;6:310–9. 10.24271/garmian.196356 [DOI] [Google Scholar]
- 16.A. Shamkuwar C, Kumari N, H. Meshram S, et al. Evaluation of knowledge, attitude and medication adherence among asthmatics outpatients in tertiary care teaching hospital-A questionnaire based study. Journal of Young Pharmacists 2016;8:39–43. 10.5530/jyp.2016.1.9 [DOI] [Google Scholar]
- 17.Werthmann D, Rabito FA, Reed C. Knowledge, attitudes, and practices concerning cockroach exposure among caregivers of children with asthma. BMC Public Health 2021;21:1–10. 10.1186/s12889-021-11497-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Jahdali H, Ahmed A, Al-Harbi A, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol 2013;9:1–7. 10.1186/1710-1492-9-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hiral P, ShobhaRani R, Nalini P. Impact of patient education on quality of life of asthma patients in an Indian tertiary care hospital. Indian Journal of Pharmacy Practice 2013;6. [Google Scholar]
- 20.Donques A, Alaki E, Almazyad W, et al. Knowledge and perception of asthmatic patients and their family towards asthma disease and management in King Saud medical City, Riyadh, KSA. J Clin Respir Dis Care 2017;3:128. [Google Scholar]
- 21.Kovačević M, Ćulafić M, Jovanović M, et al. Impact of community pharmacists' interventions on asthma self-management care. Res Social Adm Pharm 2018;14:603–11. 10.1016/j.sapharm.2017.07.007 [DOI] [PubMed] [Google Scholar]
- 22.Beshah PS. The knowledge, attitudes and practices of caregivers of children with asthma attending the Raleigh Fitkin Memorial Hospital. Manzini, Swaziland: Stellenbosch: Stellenbosch University; 2018. [Google Scholar]
- 23.Chavannes NH, Grijsen M, van den Akker M, et al. Integrated disease management improves one-year quality of life in primary care COPD patients: a controlled clinical trial. Prim Care Respir J 2009;18:171–6. 10.3132/pcrj.2009.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Habib GMM, Rabinovich R, Divgi K, et al. Systematic review (protocol) of clinical effectiveness and models of care of low-resource pulmonary rehabilitation. NPJ Prim Care Respir Med 2019;29:1–4. 10.1038/s41533-019-0122-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ryan D, Angier E, Gomez M, et al. Results of an allergy educational needs questionnaire for primary care. Allergy 2017;72:1123–8. 10.1111/all.13134 [DOI] [PubMed] [Google Scholar]
- 26.Haahtela T, Tuomisto LE, Pietinalho A, et al. A 10 year asthma programme in Finland: major change for the better. Thorax 2006;61:663–70. 10.1136/thx.2005.055699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Franco R, Santos AC, do Nascimento HF, et al. Cost-Effectiveness analysis of a state funded programme for control of severe asthma. BMC Public Health 2007;7:1–8. 10.1186/1471-2458-7-82 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article.