Since March 28, 2022, Shanghai has become the new COVID-19 epicenter in China, with more than 500,000 COVID-19 cases until May 5th, 2022, of which more than 90% are asymptomatic. More than 12,000 children in Shanghai were infected with COVID-19 during the current Omicron wave, which was characterized by family clustering. Because an increasing number of symptomatic children are required to be hospitalized, four major pediatric medical centers in Shanghai and other general hospitals were designated for admitting symptomatic pediatric COVID-19 cases in the early April. There were approximately 3,500 pediatric cases admitted from April 1st until May 5th, 2022.
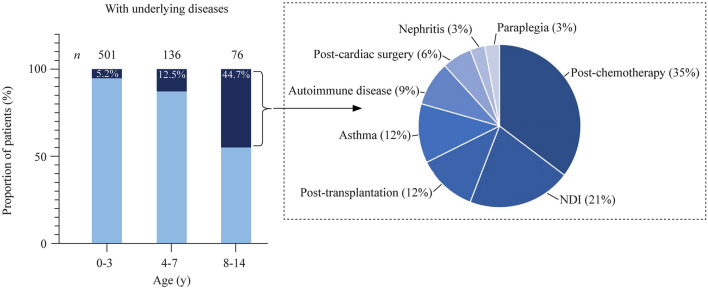
Our hospital is a designated general hospital with 890 beds (235 for children) for admitting COVID-19 patients and admitted approximately one-fifth of all symptomatic pediatric cases in Shanghai. In total, there were 713 cases admitted from April 7th to May 5th, with males accounting for 54.6% (389/713). For the age distribution, 70.3% (501/713), 19.1% (136/713), and 10.7% (76/713) were 0–3, 4–7, and 8–14 years, respectively. Among the 76 children aged 8–14 years, 44.7% (34/77) had underlying diseases, including 12 postchemotherapy patients with cancer or leukemia, 7 with neurodevelopmental impairments, 4 posttransplantation patients (liver 2, bone marrow 2), 4 with asthma, 3 with autoimmune disease, 2 postcardiac operations, 1 with nephritis, and 1 with paraplegia. Among the 501 cases aged 0–3 years and the 136 cases at 4–7 years, 5.2% (26/501) and 12.5% (17/136) had underlying conditions, respectively (Fig. 1). Except for one patient who was in a severe condition coinfected with mycoplasma pneumonia, all the other cases were under mild or moderate conditions.
Fig. 1.
Age distributions of infected pediatric cases and those with underlying diseases aged 8–14 years. NDI neurodevelopmental impairments
Based on the data analysis, we found two features of pediatric COVID-19 cases admitted during this Omicron wave in Shanghai. First, the percentage of younger hospitalized patients was much higher than before. This can be seen by comparing the percentage of patients aged 0–3 years in our data with that of the reported symptomatic patients aged 0–5 years in China from January 16, 2020 to February 8, 2020 [70.3% aged 0–3 vs. 41.4% (845/2039) aged 0–5 years] [1]. This finding is consistent with the latest published paper demonstrating that the average age of hospitalized pediatric cases during the Omicron period was much lower than that in the pre-Omicron period (2.2 ± 2.1 vs. 4.4 ± 4.5 years, P < 0.001) [2]. The potential reasons for such a situation are that vaccination of children aged 3–17 years was initiated on Nov. 2021 and that students aged 3–17 years had shifted to online learning since March 12, 2022 in Shanghai prevented COVID-19 transmission among them in schools. Second, admitted older children and young adolescents were more likely to have underlying conditions. Since most of their conditions were considered contraindications for vaccination, the rate of COVID-19 vaccination in children with underlying conditions is extremely low. However, paradoxically, compared with other healthy and vaccinated children, they are more predisposed to symptomatic COVID-19 infection [3, 4]. In addition, if pediatric cases with underlying conditions progressed to severe conditions, they would be more likely to require critical care or multidisciplinary care. Thus, even though no critical COVID-19 pediatric cases have been reported until May 5th, 2022. During this epidemic in Shanghai, we should still pay attention to pediatric patients with underlying diseases.
In combating this wave of COVID-19 in Shanghai, we have the following suggestions to share: (1) it is urgent to set up a hierarchical admission system for pediatric patients in China. Now, all the pediatric hospitals were designated to admit patients of various severities in Shanghai, making those large tertiary pediatric medical hospitals with well-equipped pediatric intensive care units and multidisciplinary teams overwhelmed with patients who had mild conditions. Doctors and nurses were working overtime for admitting mild cases, while the patients with underlying conditions potentially requiring close monitoring and multidisciplinary care received insufficient attention. Therefore, the major pediatric medical centers should only admit COVID-19 patients with high risk (e.g., patients with underlying conditions) to fully take advantage. Patient triage, referring and transport systems need to be improved and streamlined as soon as possible; (2) The contraindications of vaccination should be clarified in official guidelines based on sound scientific evidence so that children with underlying diseases can also be safely vaccinated. Voluntary COVID-19 vaccination for 3–11 year-old children was initiated in Nov. 2021 in China, but with a low rate of vaccination among children with underlying conditions. When contraindications for vaccination were not clarified, even though theoretically, the absolute contraindication for vaccination is rare [5], most primary doctors qualifying vaccination for a specific child may consider congenital heart disease, atopic diseases, asthma, cancer, and other mild underlying diseases as contraindications for COVID-19 vaccination. Of note, children with these underlying diseases are predisposed to COVID-19 infection and potentially benefit most from vaccination. Therefore, an official guideline for vaccinating children with underlying diseases must be introduced, so that some previously “Covid-19 vaccinating unsuitable” children can be vaccinated in the near future, and (3) Systematic studies on the epidemiology of COVID-19 among children are needed. Public fear and uncertainty about COVID-19 impede the control of the pandemic. We should perform scientific studies on the transmission, severity, and long-term complications of COVID-19 among children, the optimal isolation duration of pediatric cases, and the efficacy of vaccination in younger age groups, such as children aged 1–3 years. These studies are urgently needed to guide further anti-pandemic policies.
In conclusion, after 2 years of the COVID-19 pandemic, Shanghai reported a high number of pediatric cases driven by the Omicron variant (BA.2), characterized by high transmissibility and immune evasion. Children aged younger or with underlying conditions are two major concerns for potential severe cases. Improving patient triage, referring and transport systems, increasing the vaccination rate in children with underlying conditions, and systematically studying the characteristics of Omicron variant infection in children are strongly suggested.
Author contributions
Conceptualization and design: WZ; data collection, analysis: JZ; drafting of the manuscript: JZ; supervision: YL, LW, TZ, YC; writing—review and editing: WZ.
Funding
This study was funded by the National Key Research and Development Program of China (2021YFC2701800, 2021YFC2701801) and Shanghai Municipal Science and Technology Major Project (ZD2021CY001).
Data availability
Data are available by contacting the corresponding author.
Declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article. Author Wen-Hao Zhou is a member of the Editorial Board for the World Journal of Pediatrics. The paper was handled by the other Editor and has undergone a rigorous peer-review process. Author Wen-Hao Zhou was not involved in the journal’s review or decisions making, this manuscript.
Ethical approval
Data were analyzed as a whole, no individual inform consent was obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics. 2020;145:e20200702. doi: 10.1542/peds.2020-0702. [DOI] [PubMed] [Google Scholar]
- 2.Martin B, DeWitt PE, Russell S, Sanchez-Pinto LN, Haendel MA, Moffitt R, et al. Acute upper airway disease in children with the Omicron (B.1.1.529) variant of SARS-CoV-2-A report from the US National COVID Cohort Collaborative. JAMA Pediatr. 2022 doi: 10.1001/jamapediatrics.2022.1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsabouri S, Makis A, Kosmeri C, Siomou E. Risk factors for severity in children with Coronavirus disease 2019: a comprehensive literature review. Pediatr Clin North Am. 2021;68:321–338. doi: 10.1016/j.pcl.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mukkada S, Bhakta N, Chantada GL, Chen Y, Vedaraju Y, Faughnan L, et al. Global characteristics and outcomes of SARS-CoV-2 infection in children and adolescents with cancer (GRCCC): a cohort study. Lancet Oncol. 2021;22:1416–1426. doi: 10.1016/S1470-2045(21)00454-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luxi N, Giovanazzi A, Capuano A, Crisafulli S, Cutroneo PM, Fantini MP, et al. COVID-19 vaccination in pregnancy, paediatrics, immunocompromised patients, and persons with history of allergy or prior SARS-CoV-2 infection: overview of current recommendations and pre- and post-marketing evidence for vaccine efficacy and safety. Drug Saf. 2021;44:1247–1269. doi: 10.1007/s40264-021-01131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by contacting the corresponding author.