Abstract
Objective:
The present study aimed to: (1) identify recent temporal changes in the prevalence of different cognitive and behavioral eating disorder (ED) symptoms, current probable EDs, lifetime ED diagnoses, and mental healthcare use among college students across the United States; (2) determine whether established disparities in ED prevalence and receiving mental healthcare have widened or narrowed over time for marginalized groups within this population.
Method:
Participants included a large national sample of U.S. college students (N = 286,720) who completed the repeated cross-sectional Healthy Minds Study from 2013 to 2020. Descriptive statistics and polynomial regressions quantified time-trends in participants’ ED symptoms and past 12-month mental healthcare. Moderated regressions examined temporal changes in ED symptoms and mental healthcare based on sociodemographic characteristics.
Results:
Individuals’ engagement in different cognitive and behavioral ED symptoms, and likelihoods of exhibiting current probable EDs, reporting lifetime ED diagnoses, and (for individuals with current probable EDs) receiving therapy or counseling in the past 12-months exhibited nonlinear increases from 2013 to 2020. Further, the prevalence of current and lifetime ED symptoms and (for symptomatic individuals) past 12-month mental healthcare differed over time for individuals with different BMIs and gender, sexual, and racial/ethnic identities (but not ages). In particular, individuals with higher BMIs and those who identified as male, bisexual, and gay, lesbian, or queer exhibited increasing ED pathology over time.
Discussion:
These findings provide important information on groups of U.S. college students that have experienced increasing burden of ED symptoms and may help guide ED prevention, treatment, and research priorities.
Public Significance:
Recent temporal changes in the prevalence of eating disorder (ED) symptoms and mental healthcare were examined in a national sample of U.S. young adults.
Non-linear increases in ED symptoms and mental healthcare were identified among U.S. young adults overall from 2013 to 2020.
U.S. young adults with higher BMIs, males, bisexual, and gay, lesbian, or queer individuals exhibited increasing ED burden over time.
Keywords: disordered eating, eating disorders, mental health, young adults
1 |. INTRODUCTION
Eating disorder (ED) symptoms are associated with multiple adverse physical and mental health concerns (Udo & Grilo, 2019), commonly persist long-term (Romano et al., 2020), and are prevalent among clinical ED and nonclinical samples of adults (Galmiche et al., 2019; Lipson & Sonneville, 2017). Although rates of lifetime ED diagnoses are relatively low among U.S. adults (0.2%–3.5%; Hudson et al., 2007; Udo & Grilo, 2018), prevalence estimates suggest that approximately 19% of women and 14% of men exhibit ED symptoms of at least subclinical severity, and these rates have increased over the past decade (Galmiche et al., 2019). Given this, efforts to improve the understanding of how the prevalence of different ED symptoms has changed in recent years among large national samples are warranted.
1.1 |. Changes in ED symptoms
Whereas recent temporal changes in the prevalence of clinical ED diagnoses are well-documented (Galmiche et al., 2019; Qian et al., 2021), less is known about changes in specific ED symptoms (e.g., purging) among national nonclinical samples with elevated ED risk such as young adults and college students (Lipson & Sonneville, 2017; Udo & Grilo, 2018). The limited evidence-base that has examined recent changes in ED symptoms among national nonclinical samples is largely limited to population-based data in Australia. This research has generally shown that dietary restriction (e.g., fasting) and disinhibited eating behaviors (e.g., binge eating) have increased from the mid-1990s (fasting: 1%; binge eating: 2%) to approximately 2015 (fasting: 5%; binge eating: 13%) among Australian adolescents and adults (Da Luz et al., 2017; Mitchison et al., 2012, 2017). In contrast, changes in prevalence estimates for Australian individuals’ purging behaviors (e.g., self-induced vomiting; 0.5%–2%) were nonsignificant during this timeframe (Da Luz et al., 2017; Mitchison et al., 2012, 2017). To our knowledge, only one study has examined recent changes in specific ED symptoms within a national U.S. sample and these data suggest that the magnitude of increases in certain ED symptoms may differ from those identified for national samples in Australia. Specifically, comparably larger increases in fasting prevalence were identified between 2016 (men = 10%, women = 17%) and 2020 (men = 20%, women = 27%) among college students throughout the United States (Ganson et al., 2021) when compared to population-based prevalence estimates for fasting/strict dieting between 1995 (1%) and 2015 (5%) among Australian adolescents and adults (Da Luz et al., 2017).
To our knowledge, no existing research has examined time-trends in the prevalence of disinhibited disordered eating behaviors, purging behaviors, or cognitive ED symptoms (e.g., body dissatisfaction, food preoccupation) over the past decade among national U.S. samples. However, as a proxy, prevalence estimates from separate national studies in the United States have reported that past-week binge eating was endorsed by 5%–7% of young adults in the Add Health Study in 2002 (Liechty & Lee, 2013). This is relatively consistent with the 2% of adults in the National Comorbidity Survey Replication Study who reported binge eating at least twice per week between 2001 and 2003 (Hudson et al., 2007) and the 4% of young adults in the Growing Up Today Study (GUTS) who reported past-month binge eating in 2013 (Hart et al., 2020). In contrast, between 2013 and 2015, a markedly higher estimate for past-month binge eating was reported for 40% of U.S. college students in the multi-institute Healthy Bodies Study (Lipson & Sonneville, 2017). Compared to recent temporal changes in binge eating, purging behavior rates appear to have remained stable among U.S. young adults, with estimates of 1%–6% for past-week purging in 2002 among young adults in the Add Health Study (Liechty & Lee, 2013) and 2%–5% for past-year purging in 2013 among young adults in the GUTS (Hart et al., 2020). Although these prevalence estimates from separate national studies in the United States collectively provide some insight into the direction and magnitude of ED symptom changes, these data are confounded by different sample and methodological characteristics that may contribute to variability in estimates derived from multiple studies. Repeated crosssectional studies can complement these data by uncovering additional important information, such as how ED symptom prevalence estimates have varied among more recent (vs. earlier) representative samples of individuals throughout the United States, and warrant consideration.
1.2 |. Eating disorder symptom disparities
In addition to changes in ED symptoms that have may have emerged in the United States in general, the direction and magnitude of these time-trends have likely varied for different sociodemographic groups. Younger age groups, girls and women, transgender and gender diverse populations, sexual minority populations, and individuals living in larger bodies have historically experienced a disproportionate risk of exhibiting elevated ED symptoms and receiving clinical ED diagnoses relative to older populations, boys and men, cisgender populations, heterosexual populations, and individuals living in smaller bodies, respectively (Ganson et al., 2021; Kessler et al., 2013; Lipson & Sonneville, 2017; Qian et al., 2021; Romano & Lipson, 2021; Udo & Grilo, 2018). In contrast, findings of ED prevalence across diverse racial and ethnic groups have been more variable, with some studies suggesting that prevalence estimates for ED symptoms are comparable across racial and ethnic groups (Marques et al., 2011; Perez et al., 2016) whereas others have identified notable yet inconsistent disparities (Ganson et al., 2021; Lipson & Sonneville, 2017; Solmi et al., 2014; Udo & Grilo, 2018). Although it is unknown whether these documented disparities in ED symptom prevalence have widened or narrowed over the past decade among large national samples in the United States, earlier repeated cross-sectional data from representative samples of Australian adolescents and adults indicated that the magnitudes of increases in fasting/strict dieting and purging behaviors (but not binge eating) from 1998 to 2008 were larger among males versus females (Mitchison et al., 2014). Expanding upon these population-based findings in Australia by determining whether individuals throughout the United States who belong to socially marginalized groups that have been historically excluded from EDs research have exhibited recent changes in their ED symptoms can provide important information for use in contemporary targeted prevention and treatment efforts.
1.3 |. Mental healthcare
Further, treatment-seeking among individuals with ED symptoms is uncommon (<50%; Kessler et al., 2013; Solmi et al., 2014) and has varied for different cultural groups. For example, cross-sectional data have shown that individuals with elevated ED symptoms and who identify with various racial/ethnic minority identities (e.g., Hispanic/Latinx), identify as male, and who are younger are less likely to seek and receive ED treatment than individuals who identify as White, female, and who are older (Bohrer et al., 2017; Cachelin & Striegel-Moore, 2006; Grillot & Keel, 2018; Sonneville & Lipson, 2018; Thapliyal et al., 2018). In contrast, comparisons of individuals living in larger versus smaller bodies have yielded mixed results, with some studies suggesting that individuals with lower weights are less likely (Mond et al., 2009; Thapliyal et al., 2018) or more likely (Sonneville & Lipson, 2018) to receive ED treatment, whereas others have found null differences (Bohrer et al., 2017; Grillot & Keel, 2018). To our knowledge, no research has examined recent changes in the prevalence of help-seeking for ED concerns in the United States among individuals with a variety of diverse cultural identities. Improving the understanding of help-seeking in underserved groups may inform whether targeted outreach is needed to decrease barriers to care.
1.4 |. Study purpose
Given the clinical and theoretical importance of documenting recent changes in the prevalence of ED symptoms among large national samples, the present study used repeated cross-sectional data from a large study of college students across the United States to address the following aims: (1) examine recent changes in U.S. college students’ reporting of different cognitive and behavioral ED symptoms, the prevalence of exhibiting current probable EDs, reporting lifetime ED diagnoses, and—for participants with current probable EDs—receiving mental healthcare in the past 12-months; (2) determine whether disparities in experiencing current probable EDs, lifetime ED diagnoses, and mental healthcare use have widened or narrowed over time for marginalized groups.
2 |. METHOD
2.1 |. Participants and procedures
Participants included a national sample of college students across the United States who completed the standard module of the repeated cross-sectional multi-institute Healthy Minds Study (Healthy Minds Study [HMS] Network, 2022; https://healthymindsnetwork.org/research/data-for-researchers/) from 2013 through 2020. Institutional Review Board approval was obtained from all institutions and all procedures were performed in accordance with the ethical standards in the 1964 Declaration of Helsinki and its amendments. Random samples of 4000 degree-seeking students were obtained from the full populations at institutions with at least 4000 students. At smaller institutions, all students were recruited. After providing informed consent, participants completed an online survey.
2.2 |. Measures
2.2.1 |. Demographic characteristics
Participants reported their ages and gender, sexual, and racial/ethnic identities. There were differences in the demographic characteristic response options that were presented to participants across the 7 years of assessment. To facilitate the present statistical analyses, consistent categories (represented as dummy coded variable sets) were created to maximally capture the diversity present in participants’ responses. For gender identity, recoded response options included: (1) female (referent); (2) male; (3) transgender and gender diverse (individuals who identified as trans men, trans women, genderqueer, gender nonconforming, or with an unlisted/self-identified gender identity). For sexual identity, response options included: (1) heterosexual (referent); (2) bisexual; (3) gay, lesbian, or queer; (4) questioning; (5) unlisted/self-identified sexual identity. For racial/ethnic identity, response options included: (1) African American or Black; (2) American Indian or Alaskan Native; (3) Asian American or Asian; (4) Hispanic or Latinx; (5) Native Hawaiian or Pacific Islander; (6) Middle Eastern, Arab, or Arab American; (7) White (referent); (8) unlisted/self-identified racial/ethnic identity. Finally, self-reported height and weight data were used to compute participants’ BMIs.
2.2.2 |. Eating disorder symptoms
The 5-item SCOFF (Morgan et al., 1999) was used to assess participants’ ED symptoms. Items were rated as present (1) or absent (0). Descriptive data reflecting changes in endorsement rates for each item were examined. In addition, a binary variable representing whether participants exhibited current probable EDs via summed scores ≥2 (1) or exhibited lower levels of ED severity (0) was computed for use in the statistical models described below (Morgan et al., 1999). The SCOFF has exhibited good sensitivity and specificity as a screening tool for identifying clinical EDs among young adults (Morgan et al., 1999).
Participants also responded to the question, “Have you ever been diagnosed with any of the following conditions by a health professional (e.g., primary care doctor, psychiatrist, psychologist, etc.)?” Those who endorsed “Eating disorder (e.g., anorexia nervosa, bulimia nervosa)” were considered to report a Lifetime ED Diagnosis.
2.2.3 |. Past year therapy or counseling
Participants endorsed whether they received counseling or therapy for mental health concerns in the past 12-months (1 = yes, 0 = no). Analyses using this variable only included participants who endorsed current probable EDs (via SCOFF≥2).
2.3 |. Statistical analyses
Data analyses were weighted using nonresponse weights that adjust for differential probabilities of response (response rates = 13%–29%) between participants and nonresponders. Specifically, administrative data on the full student populations at institutions that participated in the HMS were used to estimate students’ likelihoods of responding to the HMS survey as a function of their gender, racial, and ethnic identities, academic levels, and grade point averages. These nonresponse weights were then applied to each respondent’s data, wherein students who were less likely to respond to the survey (as a function of the participant characteristics listed above) were assigned larger weights. Use of these weights results in parameter estimates that are reflective of the full populations at each institution that participated in the HMS over the assessed waves.
The temporal trajectory of participants’ ED symptoms between 2013 and 2020 was assessed in two ways. First, descriptive statistics characterizing the proportion of participants in each year who endorsed different cognitive and behavioral ED symptoms were examined. Second, to quantify these descriptive trends, polynomial regressions were run. In these models, study year was modeled as a predictor of three separate outcomes that captured whether participants: (1) exhibited current probable EDs (SCOFF≥2); (2) reported lifetime ED diagnoses; and (3) whether participants with current probable EDs received counseling or therapy in the past 12-months. Linear, quadratic, and cubic time trends for the study year variable were examined to identify the best fitting temporal trajectory. Prior to running these models, evidence of possible cohort effects was examined by assessing the configural, metric, and scalar measurement invariance of an ED symptoms latent factor, with the SCOFF items as indicators. Results did not suggest cohort effects were present, as evidenced by metric invariance (equivalent factor loadings; Fischer et al., 2019) for participants comprising each of the seven study years, via recommended criteria (CFI Δ = −0.012, RMSEA Δ = +0.001, SRMR Δ = +0.007; Chen, 2007).
Whether participants’ likelihoods of exhibiting current probable EDs, reporting lifetime ED diagnoses, and—for individuals with current probable EDs—using mental health services in the past 12-months differed over time for marginalized groups was subsequently examined via separate moderated regressions. Each model included the demographic correlate of interest (predictor), year (moderator), and a correlate * year interaction. Year of assessment and continuous correlates were centered prior to creating the interaction terms. Significant interactions were followed by simple slopes analyses to determine the nature of the associations for participants across the assessed years. Data missingness was managed using maximum likelihood estimation with robust standard errors.
3 |. RESULTS
The present sample includes 286,720 college students, overall (Mage = 23.23, SD = 6.52; MBMI = 24.93, SD = 5.98). Most respondents identified as female (n = 190,488; 66.50%), heterosexual (n = 233,878; 82.02%), and White (n = 182,991; 63.92%). Overall, 23.87% of participants exhibited current probable EDs (SCOFF ≥2) and 3.44% reported lifetime ED diagnoses. Among participants with current probable EDs, only 35.75% received counseling or therapy in the past 12-months. There was a small to moderate-sized association between participants’ current probable ED statuses and self-reported lifetime ED diagnoses (rtc = 0.210, p <.001) and, among participants with current probable EDs, a moderate to large association between lifetime ED diagnoses and past 12-month receipt of counseling or therapy (rtc = 0.356, p <.001). See Table 1.
TABLE 1.
Participant characteristics
| All participants |
2013–2014 n = 18,091 |
2014–2015 n = 16,188 |
2015–2016 n = 30,130 |
2016–2017 n = 43,179 |
2017–2018 n = 51,683 |
2018–2019 n = 45,101 |
2019–2020 n = 82,336 |
|
|---|---|---|---|---|---|---|---|---|
| M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | M (SD) or n (%) | |
| Age | 23.23 (6.52) | 23.24 (5.66) | 23.12 (5.63) | 22.66 (5.75) | 23.83 (7.13) | 23.23 (6.40) | 23.21 (6.95) | 23.16 (6.60) |
|
| ||||||||
| Gender identity | ||||||||
| Female | 190,488 (66.50%) | 11,512 (63.63%) | 9940 (61.41%) | 19,184 (63.73%) | 29,201 (67.72%) | 34,801 (67.39%) | 30,120 (66.84%) | 55,730 (67.75%) |
| Male | 90,340 (31.54%) | 6535 (36.12%) | 6164 (38.08%) | 10,545 (35.03%) | 13,102 (30.38%) | 15,289 (29.61%) | 13,977 (31.02%) | 24,728 (30.06%) |
| Transgender or gender diverse | 5633 (1.97%) | 44 (0.24%) | 82 (0.51%) | 371 (1.23%) | 818 (1.90%) | 1550 (3.00%) | 966 (2.14%) | 1802 (2.19%) |
|
| ||||||||
| Sexual identity | ||||||||
| Heterosexual | 233,878 (82.02%) | 16,297 (90.24%) | 13,930 (86.16%) | 26,195 (87.16%) | 36,009 (83.73%) | 40,367 (78.52%) | 36,064 (80.65%) | 65,016 (79.53%) |
| Bisexual | 21,175 (7.43%) | 687 (3.80%) | 806 (4.99%) | 1677 (5.58%) | 3235 (7.52%) | 3932 (7.65%) | 3467 (7.75%) | 7371 (9.02%) |
| Gay, lesbian, or queer | 13,224 (4.64%) | 592 (3.28%) | 728 (4.50%) | 1003 (3.34%) | 1553 (3.61%) | 3234 (6.29%) | 2206 (4.93%) | 3908 (4.78%) |
| Questioning | 4496 (1.58%) | 244 (1.35%) | 334 (2.07%) | 500 (1.66%) | 841 (1.96%) | 782 (1.52%) | 603 (1.35%) | 1192 (1.46%) |
| Unlisted/self-identified sexual identity | 12,389 (4.34%) | 240 (1.33%) | 370 (2.29%) | 680 (2.26%) | 1368 (3.18%) | 3096 (6.02%) | 2374 (5.31%) | 4261 (5.21%) |
|
| ||||||||
| Racial/ethnic identity | ||||||||
| White | 182,991 (63.92%) | 10,847 (59.98%) | 11,093 (68.50%) | 20,687 (68.66%) | 28,798 (66.81%) | 30,102 (58.34%) | 28,882 (64.16%) | 52,582 (63.99%) |
| Black or African American | 14,796 (5.17%) | 936 (5.18%) | 555 (3.43%) | 905 (3.00%) | 2422 (5.62%) | 2723 (5.28%) | 2462 (5.47%) | 4793 (5.83%) |
| American Indian or Alaskan Native | 816 (0.29%) | 24 (0.13%) | 32 (0.20%) | 50 (0.17%) | 171 (0.40%) | 158 (0.31%) | 126 (0.28%) | 255 (0.31%) |
| Asian or Asian American | 35,063 (12.25%) | 2985 (16.51%) | 1985 (12.26%) | 3799 (12.61%) | 4792 (11.12%) | 7596 (14.72%) | 5325 (11.83%) | 8581 (10.44%) |
| Hispanic or Latinx | 17,554 (6.13%) | 1448 (8.01%) | 874 (5.40%) | 216 (0.72%) | 1751 (4.06%) | 3982 (7.72%) | 3141 (6.98%) | 6142 (7.47%) |
| Native Hawaiian or Pacific Islander | 392 (0.14%) | 39 (0.22%) | 21 (0.13%) | 32 (0.11%) | 74 (0.17%) | 68 (0.13%) | 52 (0.12%) | 106 (0.13%) |
| Middle Eastern, Arab, or Arab American | 3734 (1.30%) | 209 (1.16%) | 117 (0.72%) | 239 (0.79%) | 504 (1.17%) | 835 (1.62%) | 671 (1.49%) | 1159 (1.41%) |
| Unlisted/self-identified race | 30,954 (10.81%) | 1596 (8.83%) | 1517 (9.37%) | 4202 (13.95%) | 4590 (10.65%) | 6136 (11.89%) | 4359 (9.68%) | 8554 (10.41%) |
|
| ||||||||
| Body mass index | 24.93 (5.98) | 24.04 (4.83) | 24.18 (5.25) | 23.64 (8.76) | 25.21 (5.95) | 24.71 (5.62) | 25.21 (5.87) | 25.33 (5.95) |
|
| ||||||||
| Probable current eating disorder (SCOFF≥2)a | 68,433 (23.87%) | 2929 (16.19%) | 2860 (17.66%) | 6214 (20.62%) | 9919 (22.97%) | 12,688 (24.55%) | 11,652 (25.84%) | 22,171 (26.93%) |
|
| ||||||||
| Lifetime eating disorder diagnosis | 9609 (3.44%) | 443 (2.60%) | 475 (3.09%) | 965 (3.26%) | 1385 (3.27%) | 1791 (3.53%) | 1620 (3.68%) | 2930 (3.63%) |
|
| ||||||||
| Past 12-month counseling or therapyb | 23,914 (35.75%) | 730 (25.20%) | 843 (30.48%) | 1948 (31.98%) | 3230 (33.20%) | 4540 (36.57%) | 4385 (38.72%) | 8238 (38.03%) |
Note: N = 286,720; gender diverse includes individuals who identified as genderqueer, gender nonconforming, or with an unlisted/self-identified gender identity.
Based on SCOFF scores ≥2 (Morgan et al., 1999).
Among participants who exhibited probable current eating disorders (via SCOFF≥2).
Descriptive statistics characterizing the percentage of participants who endorsed various ED symptoms in each year are reported in Figure 1. Across years, the most frequently endorsed symptom was participants’ fears that they experienced a loss of control over their eating (21%–32%). There was a significant increase in the percentage of participants who reported this symptom over time (Wald χ22013 vs. 2020 (1) = 428.97, p <.001). There were steady increases in the proportions of participants who believed that they were “fat” despite others telling them that they are too thin (13%–18%; Wald χ22013 vs. 2020 (1) = 158.91, p <.001) and that food dominates their lives (11%–17%; Wald χ2 2013 vs. 2020 (1) = 145.78, p <.001). There was a large increase in the percentage of participants who engaged in self-induced vomiting between 2013–2014 (6%) and 2014–2015 (15%), followed by a consistent endorsement rate (~13%–14%; Wald χ2 2013 vs. 2020 (1) = 594.63, p <.001). Finally, there was a steady increase in the number of participants who indicated that they recently lost over 15 pounds in a 3-month period (6%–11%; Wald χ2 2013 vs. 2020 (1) = 209.24, p <.001).
FIGURE 1.
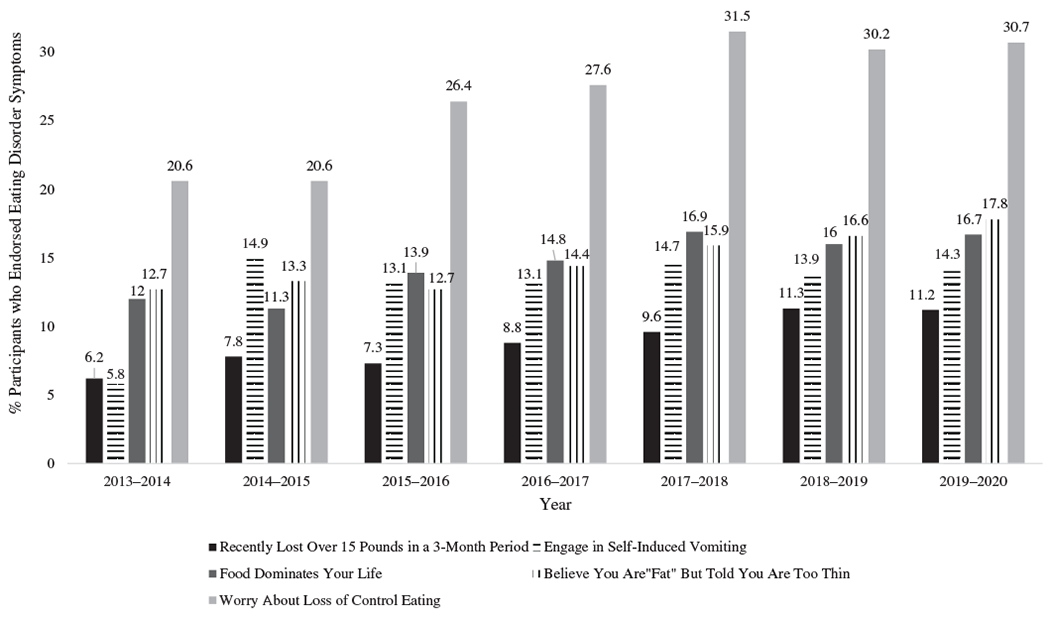
Cognitive and behavioral eating disorder symptoms endorsed by U.S. college students between 2013 and 2020
To quantify these descriptive trends, polynomial regressions were run to identify the best-fitting trajectories for the ED symptoms and mental healthcare covariates from 2013 to 2020. A quadratic association between study year and individuals’ likelihood of exhibiting current probable EDs was significant (quadratic model; year: b = 0.257, SE = 0.018, p <.001; year2: b = −0.018, SE = 0.002, p <.001) and consequently served as the best-fitting model (cubic model; year3: p = .798). In contrast, cubic associations between study year and individuals’ likelihoods of reporting lifetime ED diagnoses (cubic model; year: b = −0.192, SE = 0.130, p = .141; year2: b = 0.080, SE = 0.035, p = .023; year3: b = −0.007, SE = 0.003, p = .009) and, among individuals with current probable EDs, receiving therapy or counseling in the past 12-months (cubic model; year: b = −0.295, SE = 0.116, p = .011; year2: b = 0.115, SE = 0.030, p <.001; year3: b = −0.010, SE = 0.002, p <.001) served as the best-fitting temporal trajectories for these covariates. As shown in Figure 2, there was a shallow nonlinear increase in individuals’ current likelihood of exhibiting probable EDs from 2013 to 2014 through 2019–2020. In addition, individuals’ probabilities of self-reporting lifetime ED diagnoses and receiving therapy or counseling were highest in more recent years. There was more variability in rates of mental healthcare use versus diagnostic statuses over time and a slight decrease in mental healthcare between 2018–2019 and 2019–2020.
FIGURE 2.
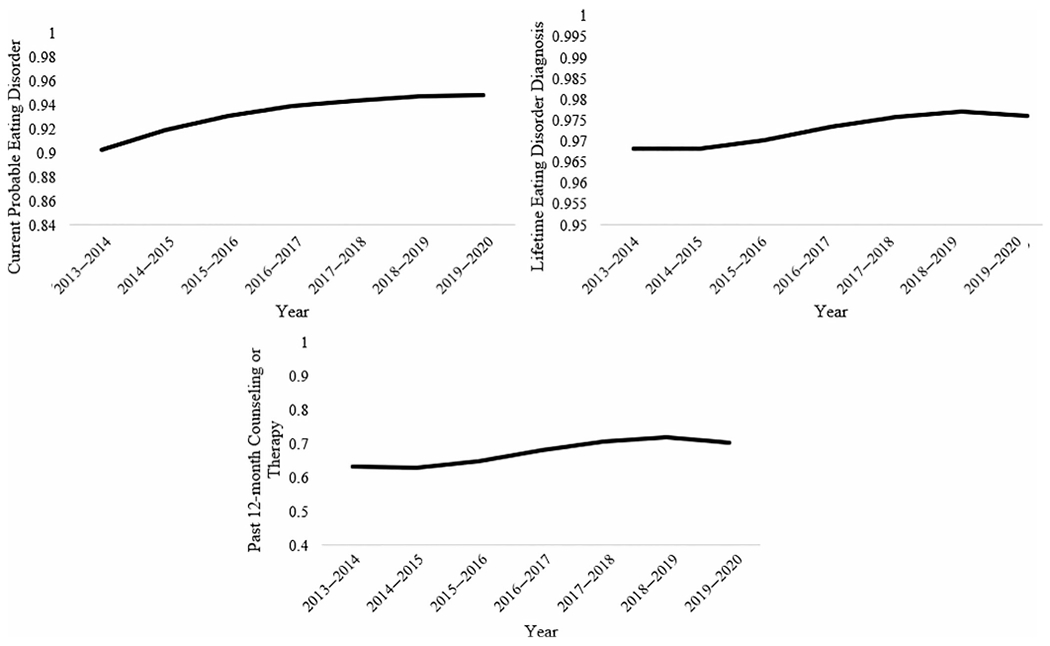
Trajectories of individuals’ eating disorder symptoms and mental health treatment from 2013 to 2020. The model for past 12-month therapy or counseling was run using data from participants who exhibited current probable EDs only (i.e., SCOFF ≥2)
3.1 |. Eating disorder symptom disparities
Table 2 displays results of regressions that examined temporal variations in marginalized groups’ likelihoods of exhibiting current probable EDs, reporting lifetime ED diagnoses, and—among individuals with current probable EDs—receiving counseling or therapy in the past 12-months. Table 3 displays simple slopes analyses for models with significant moderation effects; these analyses are graphically presented in the Supplement.
TABLE 2.
Temporal differences in associations between demographic correlates and eating disorder symptoms from 2013–2014 to 2019–2020
| Probable current eating disordera |
Past 12 month therapy or counselingb |
|||||||
|---|---|---|---|---|---|---|---|---|
| b (SE) | p | OR | Model R2 | b (SE) | p | OR | Model R2 | |
|
| ||||||||
| Age | −0.02 (0.001) | <.001 | 0.982 | 0.01 | 0.001 (0.002) | .707 | 1.001 | 0.01 |
|
| ||||||||
| Year | 0.10 (0.003) | <.001 | 1.106 | 0.08 (0.01) | <.001 | 1.085 | ||
|
| ||||||||
| Age * year | −0.001 (0.001) | .421 | 0.999 | 0.001 (0.001) | .429 | 1.001 | ||
|
| ||||||||
| Gender identity (Ref = female) | 0.06 | 0.03 | ||||||
| Male | −0.79 (0.02) | <.001 | 0.455 | −0.47 (0.03) | <.001 | 0.622 | ||
| Transgender or gender diversec | 0.26 (0.04) | <.001 | 1.300 | 1.11 (0.07) | <.001 | 3.020 | ||
|
| ||||||||
| Year | 0.09 (0.004) | <.001 | 1.092 | 0.08 (0.01) | <.001 | 1.087 | ||
|
| ||||||||
| Male * year | 0.04 (0.01) | <.001 | 1.038 | 0.01 (0.02) | .642 | 1.008 | ||
|
| ||||||||
| Transgender or gender diverse * year | −0.03 (0.03) | .285 | 0.971 | −0.10 (0.05) | .038 | 0.901 | ||
|
| ||||||||
| Sexual orientation identity (Ref = heterosexual) | 0.03 | 0.04 | ||||||
| Bisexual | 0.65 (0.02) | <.001 | 1.919 | 0.80 (0.04) | <.001 | 2.232 | ||
| Gay, lesbian, or queer | 0.49 (0.03) | <.001 | 1.638 | 0.77 (0.05) | <.001 | 2.159 | ||
| Questioning | 0.64 (0.05) | <.001 | 1.891 | 0.72 (0.08) | <.001 | 2.046 | ||
| Unlisted/self-identified sexual identity | 0.55 (0.03) | <.001 | 1.733 | 0.86 (0.05) | <.001 | 2.357 | ||
|
| ||||||||
| Year | 0.09 (0.004) | <.001 | 1.099 | 0.06 (0.01) | <.001 | 1.063 | ||
|
| ||||||||
| Bisexual * year | −0.01 (0.01) | .597 | 0.993 | 0.06 (0.02) | .010 | 1.059 | ||
|
| ||||||||
| Gay, lesbian, or queer * year | −0.01 (0.02) | .701 | 0.994 | 0.09 (0.03) | .002 | 1.093 | ||
|
| ||||||||
| Questioning * year | −0.002 (0.02) | .942 | 0.998 | 0.07 (0.04) | .125 | 1.067 | ||
|
| ||||||||
| Unlisted/self-identified sexual identity * year | −0.03 (0.02) | .124 | 0.970 | −0.07 (0.03) | .050 | 0.936 | ||
|
| ||||||||
| Racial/ethnic identity (Ref = White) | 0.02 | 0.03 | ||||||
| Black or African American | −0.26 (0.04) | <.001 | 0.773 | −0.44 (0.07) | <.001 | 0.647 | ||
| American Indian or Alaskan Native | 0.18 (0.12) | .116 | 1.199 | −0.14 (0.20) | .485 | 0.872 | ||
| Asian or Asian American | 0.28 (0.02) | <.001 | 1.321 | −0.83 (0.04) | <.001 | 0.434 | ||
| Hispanic or Latinx | 0.25 (0.03) | <.001 | 1.282 | −0.49 (0.05) | <.001 | 0.611 | ||
| Native Hawaiian or Pacific Islander | 0.73 (0.15) | <.001 | 2.084 | −0.78 (0.26) | .002 | 0.460 | ||
| Middle Eastern, Arab, or Arab American | 0.40 (0.05) | <.001 | 1.493 | −0.70 (0.10) | <.001 | 0.496 | ||
| Unlisted/self-identified race/ethnicity | 0.18 (0.02) | <.001 | 1.194 | −0.02 (0.04) | .639 | 0.983 | ||
|
| ||||||||
| Year | 0.11 (0.004) | <.001 | 1.114 | 0.09 (0.01) | <.001 | 1.092 | ||
|
| ||||||||
| Black or African American * year | −0.001 (0.02) | .962 | 0.999 | 0.000 (0.04) | .991 | 1.000 | ||
|
| ||||||||
| American Indian or Alaskan Native * year | −0.02 (0.08) | .796 | 0.979 | −0.05 (0.13) | .719 | 0.955 | ||
|
| ||||||||
| Asian or Asian American * year | −0.04 (0.01) | <.001 | 0.958 | 0.02 (0.02) | .507 | 1.015 | ||
|
| ||||||||
| Hispanic or Latinx * year | −0.02 (0.01) | .245 | 0.984 | −0.02 (0.03) | .418 | 0.978 | ||
|
| ||||||||
| Native Hawaiian or Pacific Islander * year | 0.05 (0.08) | .539 | 1.050 | −0.19 (0.12) | .102 | 0.829 | ||
|
| ||||||||
| Middle Eastern, Arab, or Arab American * year | 0.02 (0.03) | .564 | 1.017 | −0.03 (0.07) | .717 | 0.975 | ||
|
| ||||||||
| Unlisted/self-identified race/ethnicity * year | −0.01 (0.01) | .559 | 0.993 | −0.03 (0.02) | .263 | 0.976 | ||
|
| ||||||||
| Body mass index | 0.05 (0.001) | <.001 | 1.052 | 0.04 | −0.004 (0.002) | .047 | 0.996 | 0.01 |
|
| ||||||||
| Year | 0.09 (0.004) | <.001 | 1.089 | 0.08 (0.01) | <.001 | 1.085 | ||
|
| ||||||||
| Body mass index * year | 0.002 (0.001) | .001 | 1.002 | −0.001 (0.001) | .496 | 0.999 | ||
|
| ||||||||
| Lifetime eating disorder diagnosis |
||||||||
| b (SE) | p | OR | Model R2 | |||||
|
| ||||||||
| Age | −0.02 (0.003) | <.001 | 0.983 | 0.01 | ||||
|
| ||||||||
| Year | 0.04 (0.01) | <.001 | 1.036 | |||||
|
| ||||||||
| Age * year | −0.001 (0.001) | .500 | 0.999 | |||||
|
| ||||||||
| Gender identity (Ref = female) | 0.23 | |||||||
| Male | −1.95 (0.07) | <.001 | 0.142 | |||||
| Transgender or gender diversec | 0.67 (0.07) | <.001 | 1.946 | |||||
| Year | 0.03 (0.01) | .001 | 1.027 | |||||
| male * year | −0.003 (0.03) | .928 | 0.997 | |||||
| Transgender or gender diverse * year | 0.07 (0.04) | .137 | 1.068 | |||||
|
| ||||||||
| Sexual orientation identity (Ref = heterosexual) | 0.05 | |||||||
| Bisexual | 1.18 (0.04) | <.001 | 3.259 | |||||
| Gay, lesbian, or queer | 0.90 (0.06) | <.001 | 2.468 | |||||
| Questioning | 0.69 (0.10) | <.001 | 1.988 | |||||
| Unlisted/self-identified sexual identity | 1.00 (0.06) | <.001 | 2.729 | |||||
| Year | −0.02 (0.01) | .078 | 0.984 | |||||
| Bisexual * year | 0.08 (0.02) | .001 | 1.084 | |||||
| Gay, lesbian, or queer * year | 0.16 (0.03) | <.001 | 1.174 | |||||
| Questioning * year | 0.08 (0.05) | .115 | 1.086 | |||||
| Unlisted/self-identified sexual identity * year | 0.04 (0.03) | .194 | 1.045 | |||||
|
| ||||||||
| Racial/ethnic identity (Ref = White) | 0.07 | |||||||
| Black or African American | −1.66 (0.12) | <.001 | 0.189 | |||||
| American Indian or Alaskan Native | −0.48 (0.26) | .070 | 0.621 | |||||
| Asian or Asian American | −0.85 (0.06) | <.001 | 0.429 | |||||
| Hispanic or Latinx | −0.65 (0.08) | <.001 | 0.523 | |||||
| Native Hawaiian or Pacific Islander | −0.07 (0.42) | .864 | 0.931 | |||||
| Middle Eastern, Arab, or Arab American | −0.42 (0.15) | .005 | 0.654 | |||||
| Unlisted/self-identified race/ethnicity | −0.08 (0.05) | .061 | 0.920 | |||||
| Year | 0.05 (0.01) | <.001 | 1.053 | |||||
| Black or African American * year | −0.09 (0.07) | .175 | 0.912 | |||||
| American Indian or Alaskan Native * year | −0.08 (0.17) | .651 | 0.928 | |||||
| Asian or Asian American * year | −0.06 (0.03) | .061 | 0.945 | |||||
| Hispanic or Latinx * year | −0.03 (0.04) | .479 | 0.975 | |||||
| Native Hawaiian or Pacific Islander * year | 0.05 (0.14) | .726 | 1.051 | |||||
| Middle Eastern, Arab, or Arab American * year | −0.10 (0.09) | .291 | 0.906 | |||||
| Unlisted/self-identified race/ethnicity * year | 0.001 (0.03) | .952 | 1.001 | |||||
|
| ||||||||
| Body mass index | −0.02 (0.003) | <.001 | 0.978 | 0.01 | ||||
|
| ||||||||
| Year | 0.04 (0.01) | <.001 | 1.045 | |||||
|
| ||||||||
| Body mass index * year | 0.01 (0.002) | .008 | 1.005 | |||||
Note: All models used maximum likelihood estimation with robust standard errors; year of assessment and continuous covariates were centered prior to creating the interaction terms. All the significant effects are marked in bold.
Abbreviation: ED, eating disorder.
Based on SCOFF scores ≥2 (Morgan et al., 1999).
Models were run using data from participants who exhibited current probable EDs only (i.e., SCOFF ≥2).
The transgender or gender diverse category included participants who identified as trans men, trans women, genderqueer, gender nonconforming, or with an unlisted/self-identified gender identity.
TABLE 3.
Simple slopes for significant interaction terms
| Year | Current probable eating disordera |
Year | Past 12 month therapy or counselingb |
||
|---|---|---|---|---|---|
| b (SE) | p | b (SE) | p | ||
|
| |||||
| Female (0) versus male (1) | Female (0) versus transgender or gender diverse (1) | ||||
|
| |||||
| 2013–2014 | −0.935 (0.035) | <.001 | 2013–2014 | 1.540 (0.231) | <.001 |
|
| |||||
| 2014–2015 | −0.898 (0.028) | <.001 | 2014–2015 | 1.435 (0.183) | <.001 |
|
| |||||
| 2015–2016 | −0.861 (0.022) | <.001 | 2015–2016 | 1.331 (0.138) | <.001 |
|
| |||||
| 2016–2017 | −0.823 (0.017) | <.001 | 2016–2017 | 1.227 (0.097) | <.001 |
|
| |||||
| 2017–2018 | −0.786 (0.016) | <.001 | 2017–2018 | 1.123 (0.070) | <.001 |
|
| |||||
| 2018–2019 | −0.749 (0.018) | <.001 | 2018–2019 | 1.019 (0.073) | <.001 |
|
| |||||
| 2019–2020 | −0.711 (0.023) | <.001 | 2019–2020 | 0.915 (0.105) | <.001 |
|
| |||||
| White (0) versus Asian (1) | Heterosexual (0) versus bisexual (1) | ||||
|
| |||||
| 2013–2014 | 0.449 (0.040) | <.001 | 2013–2014 | 0.564 (0.101) | <.001 |
|
| |||||
| 2014–2015 | 0.406 (0.031) | <.001 | 2014–2015 | 0.621 (0.081) | <.001 |
|
| |||||
| 2015–2016 | 0.363 (0.024) | <.001 | 2015–2016 | 0.679 (0.062) | <.001 |
|
| |||||
| 2016–2017 | 0.319 (0.020) | <.001 | 2016–2017 | 0.736 (0.047) | <.001 |
|
| |||||
| 2017–2018 | 0.276 (0.020) | <.001 | 2017–2018 | 0.794 (0.038) | <.001 |
|
| |||||
| 2018–2019 | 0.232 (0.025) | <.001 | 2018–2019 | 0.851 (0.041) | <.001 |
|
| |||||
| 2019–2020 | 0.189 (0.032) | <.001 | 2019–2020 | 0.908 (0.054) | <.001 |
|
| |||||
| Body mass index | Heterosexual (0) versus gay, lesbian, or queer (1) | ||||
|
| |||||
| 2013–2014 | 0.042 (0.003) | <.001 | 2013–2014 | 0.400 (0.128) | .002 |
|
| |||||
| 2014–2015 | 0.044 (0.002) | <.001 | 2014–2015 | 0.489 (0.102) | <.001 |
|
| |||||
| 2015–2016 | 0.046 (0.002) | <.001 | 2015–2016 | 0.578 (0.078) | <.001 |
|
| |||||
| 2016–2017 | 0.049 (0.001) | <.001 | 2016–2017 | 0.666 (0.058) | <.001 |
|
| |||||
| 2017–2018 | 0.051 (0.001) | <.001 | 2017–2018 | 0.755 (0.048) | <.001 |
|
| |||||
| 2018–2019 | 0.053 (0.001) | <.001 | 2018–2019 | 0.844 (0.054) | <.001 |
|
| |||||
| 2019–2020 | 0.055 (0.002) | <.001 | 2019–2020 | 0.933 (0.072) | <.001 |
|
| |||||
| Lifetime eating disorder diagnosis | |||||
|
| |||||
| Heterosexual (0) versus bisexual (1) | |||||
|
| |||||
| 2013–2014 | 0.863 (0.108) | <.001 | 2013–2014 | ||
|
| |||||
| 2014–2015 | 0.943 (0.087) | <.001 | 2014–2015 | ||
|
| |||||
| 2015–2016 | 1.024 (0.067) | <.001 | 2015–2016 | ||
|
| |||||
| 2016–2017 | 1.105 (0.050) | <.001 | 2016–2017 | ||
|
| |||||
| 2017–2018 | 1.186 (0.041) | <.001 | 2017–2018 | ||
|
| |||||
| 2018–2019 | 1.267 (0.044) | <.001 | 2018–2019 | ||
|
| |||||
| 2019–2020 | 1.348 (0.058) | <.001 | 2019–2020 | ||
|
| |||||
| Heterosexual (0) versus gay, lesbian, or queer (1) | |||||
|
| |||||
| 2013–2014 | 0.271 (0.146) | .064 | 2013–2014 | ||
|
| |||||
| 2014–2015 | 0.431 (0.118) | <.001 | 2014–2015 | ||
|
| |||||
| 2015–2016 | 0.591 (0.093) | <.001 | 2015–2016 | ||
|
| |||||
| 2016–2017 | 0.752 (0.071) | <.001 | 2016–2017 | ||
|
| |||||
| 2017–2018 | 0.912 (0.058) | <.001 | 2017–2018 | ||
|
| |||||
| 2018–2019 | 1.073 (0.059) | <.001 | 2018–2019 | ||
|
| |||||
| 2019–2020 | 1.233 (0.074) | <.001 | 2019–2020 | ||
|
| |||||
| Body mass index | |||||
|
| |||||
| 2013–2014 | −0.043 (0.008) | <.001 | 2013–2014 | ||
|
| |||||
| 2014–2015 | −0.038 (0.007) | <.001 | 2014–2015 | ||
|
| |||||
| 2015–2016 | −0.033 (0.005) | <.001 | 2015–2016 | ||
|
| |||||
| 2016–2017 | −0.028 (0.004) | <.001 | 2016–2017 | ||
|
| |||||
| 2017–2018 | −0.023 (0.003) | <.001 | 2017–2018 | ||
|
| |||||
| 2018–2019 | −0.018 (0.004) | <.001 | 2018–2019 | ||
|
| |||||
| 2019–2020 | −0.013 (0.005) | .013 | 2019–2020 | ||
Based on SCOFF scores ≥2 (Morgan et al., 1999).
Models were run using data from participants who exhibited current probable EDs only (i.e., SCOFF ≥2).
3.1.1 |. Eating disorder correlates
Moderation via study year was evident for models that assessed associations between: (1) participants’ gender and racial/ethnic identities relative to the likelihoods that they exhibited current probable EDs (but not lifetime ED diagnoses); (2) participants’ sexual identities and lifetime ED diagnoses (but not current probable EDs); and (3) participants’ BMIs and both ED outcomes. Specifically, individuals who identified as male were less likely to exhibit current probable EDs than females (OR = 0.455), yet the magnitude of this difference decreased across study years (OR = 1.038). Although transgender or gender diverse individuals were more likely to exhibit current probable EDs than females (OR = 1.300), the magnitude of this difference did not change over time. Additionally, Asian/Asian American individuals were more likely to exhibit current probable EDs than White individuals (OR = 1.321), and the magnitude of this difference decreased over time (OR = 0.958). Hispanic/Latinx, Native Hawaiian/Pacific Islander, and Middle Eastern/Arab/Arab American participants, and those with an unlisted/self-identified race/ethnicity also exhibited a greater (ORs = 1.194–2.084) likelihood of exhibiting current probable EDs than White participants, whereas Black/African American participants exhibited a lower (OR = 0.773) likelihood of exhibiting current probable EDs than White participants; however, these associations did not exhibit temporal changes. Further, bisexual (OR = 3.259) and gay, lesbian, or queer (OR = 2.468) participants were more likely to report lifetime ED diagnoses than heterosexual participants, and the magnitude of these differences increased across study years (ORs = 1.084 and 1.174, respectively). Participants who identified as questioning (OR = 1.988) and with an unlisted/self-identified sexual identity (OR = 2.729) were also more likely to report lifetime ED diagnoses than heterosexual participants; however, these associations did not change over time. Finally, higher BMI was associated with a greater likelihood of exhibiting current probable EDs (OR = 1.052), an association that increased in magnitude over time (OR = 1.002). In contrast, BMI was inversely associated with reporting lifetime EDs (OR = 0.978) and the strength of this inverse association decreased over time (OR = 1.005).
3.1.2 |. Mental healthcare
Among participants with current probable EDs, moderation via study year was evident for models that assessed associations between participants’ gender and sexual identities relative to the likelihood that they received therapy or counseling in the past 12-months. Specifically, transgender or gender diverse participants (OR = 3.020) were more likely to receive therapy or counseling in the past 12-months than female participants, yet the magnitude of this difference decreased in strength over time (OR = 0.901). Although males conversely exhibited a lower (OR = 0.622) likelihood of using mental health services in the past 12-months than females, this association did not differ over time. Further, bisexual (OR = 2.232) and gay, lesbian, or queer participants (OR = 2.159) were more likely to report past 12-month therapy or counseling than heterosexual individuals, and the magnitude of these differences increased over time (ORs = 1.059 and 1.093, respectively). Participants who identified as questioning (OR = 2.046) and with an unlisted/self-identified sexual identity (OR = 2.357) were also more likely to report past 12-month therapy or counseling than those who identified as heterosexual, but these associations did not change over time.
4 |. DISCUSSION
Little is known about whether the prevalence of ED symptoms has changed in recent years among national samples of U.S college students, or whether established ED symptom disparities have widened or narrowed for marginalized groups within this population. To address these research gaps, the present study used repeated crosssectional data from a large national sample of U.S. college students to: (1) identify changes in the prevalence of different cognitive and behavioral ED symptoms, current probable EDs, lifetime ED diagnoses, and mental healthcare use from 2013 to 2020; and (2) determine whether disparities in these ED symptoms and mental healthcare have widened or narrowed over time for marginalized groups. Results indicated that individuals’ reported ED symptoms and past 12-month mental healthcare use significantly increased from 2013 to 2020. Further, associations between individuals’ gender, sexual, and racial/ethnic identities, and BMIs (but not ages) relative to their current and lifetime ED symptoms and mental healthcare use differed over time. Important variations were identified in these time-trends based on the ED status or mental healthcare outcome, and specific sociodemographic group under investigation. These findings provide insight into potential prevention, treatment, and research priorities that may warrant consideration moving forward.
4.1 |. Changes in eating disorder symptoms
In the present study, U.S. college students’ likelihoods of exhibiting current probable EDs, reporting lifetime ED diagnoses, and (among individuals with current probable EDs) receiving therapy or counseling exhibited nonlinear increases from 2013 to 2020. These findings align with and extend trends identified by population-based studies in Australia (Da Luz et al., 2017; Mitchison et al., 2012, 2017) and point-prevalence estimates from separate national U.S. samples in recent decades (Ganson et al., 2021; Hart et al., 2020; Hudson et al., 2007; Liechty & Lee, 2013; Lipson & Sonneville, 2017). Notably, although both ED symptoms and mental healthcare prevalence estimates increased over time, very few participants with current probable EDs received mental healthcare from 2013 (25.20%) to 2020 (38.03%). This is concerning, as the relative increase in treatment-seeking did not seem to outpace the relative increase in the proportion of U.S. college students who exhibited heightened ED symptoms over time. The present findings consequently underscore the need to increase prevention efforts in settings such as college and university campuses, and to ensure equitable access to evidence-based treatments for those with clinical symptomology (Streatfeild et al., 2021).
The present findings also extend existing EDs time-trend research by identifying significant increases in all assessed cognitive and behavioral ED symptoms (via the SCOFF) among U.S. college students. Of particular importance, approximately one-fifth to one-third of U.S. college students in this sample reported worrying that they experienced a loss of control over their eating between 2013 and 2020. This is noteworthy, as loss of control eating is a central symptom of binge eating disorder (American Psychological Association, 2013) and has exhibited particularly adverse patterns of association with various physical and mental health concerns when compared to other disinhibited eating behaviors (e.g., overeating; Goldschmidt, 2017; Thompson et al., 2021). As an extension of this study, it will prove useful for future large-scale repeated cross-sectional studies to determine whether these prevalence estimates for worrying about loss of control eating align with time-trends for individuals’ engagement in this disordered eating behavior.
In addition, whereas approximately 6% of U.S. college students reported purging via self-induced vomiting in 2013–2014, this prevalence estimate increased to 14% by 2019–2020. This marked increase is considerably higher than purging prevalence estimates identified among community-based national samples in Australia (0.5%–2%; Da Luz et al., 2017; Mitchison et al., 2012, 2017) and the United States (0.5%–4%; Hart et al., 2020) in recent decades. It is possible that differences in prevalence estimates for self-induced vomiting in the present study versus prior large-scale national research may be due to differences in sample type (college, community) or the wording of purging behavior survey items. Future research that directly assesses these potential sources of variation is needed to better contextualize this result.
4.2 |. Eating disorder symptom disparities
In addition to increases in ED symptoms identified among U.S. college students overall, the direction and magnitude of these time-trends varied for different marginalized groups. Specifically, individuals with younger ages, sexual and gender minority identities, most racial/ethnic minority identities, and higher BMIs were more likely to: (1) meet criteria for current probable EDs; and (2) (with exceptions for individuals with most racial/ethnic minority identities and higher BMIs) self-report lifetime ED diagnoses. These findings are generally consistent with results from well-established ED symptom disparities research (Ganson et al., 2021; Kessler et al., 2013; Lipson & Sonneville, 2017).
Further, the present study is the first to show that identifying as bisexual and gay, lesbian, or queer (vs. heterosexual) and exhibiting higher (vs. lower) BMIs became increasingly robust predictors of elevated ED pathology in more recent cohorts of U.S. college students. Similarly, although individuals who identified as male were less likely to exhibit current probable EDs than females, the magnitude of this difference decreased (i.e., began to equalize) across study years. This gender difference finding aligns with initial time-trend research among Australian adults (Mitchison et al., 2014) and growing recognition of understudied ED symptoms (e.g., musculature-enhancing behaviors, drive for muscularity) that present at elevated rates among boys and men (Nagata et al., 2020). Collectively, these ED symptom disparities findings suggest that individuals who identify as male, bisexual, and gay, lesbian, or queer, and those with higher BMIs have become increasingly at-risk groups that will warrant continued attention in the coming years.
Reports of receiving mental healthcare also differed over time for participants with elevated ED symptoms who comprised certain marginalized groups. Specifically, individuals who exhibited current probable EDs and identified as bisexual and gay, lesbian, or queer were more likely to receive therapy or counseling in the 12-months prior to assessment than those who identified as heterosexual, and the magnitude of these differences increased (i.e., widened) across study years. In contrast, although symptomatic individuals who identified as transgender or gender diverse were more likely to receive therapy or counseling in the past 12-months than those who identified as female, the magnitude of this difference decreased (i.e., narrowed) in strength between 2013 and 2020. More targeted outreach efforts may consequently be needed to engage individuals with transgender or gender diverse identities in mental healthcare, in particular. Further, given that the present study was (to our knowledge) the first to examine how mental healthcare use has changed in recent years for individuals with at-risk ED symptoms who comprise these marginalized groups at the national level, it will be important for future national studies to examine mental healthcare use among individuals with a variety of diverse identities, beyond the historic “binaries” (e.g., males vs. females, heterosexual vs. sexual minority, White race/ethnicity vs. non-White, etc.) that have generally only been accounted for in research in this area.
4.3 |. Strengths and limitations
The present study has multiple strengths, including the empirical and clinical importance of these findings, and the use of a large national sample of U.S. college students that was weighted to make the results generalizable to the full populations at institutes that participated in the HMS from 2013 to 2020. It also serves as the largest study of this nature to account for multiple aspects of diversity that individuals identify with that are not often assessed in national studies, such as multiple understudied sexual, gender, and racial/ethnic identities. However, the present study also possesses various limitations, such as the low response rates across study years (13%–29%). However, these rates are comparable to those in other national studies (American College Health Association, 2022) and were adjusted for using participant nonresponse weights that were computed to account for known differences between responders and nonresponders, such that the impact of this limitation on the present findings is minimal. Second, many of the moderation effects attesting to temporal changes in ED statuses and mental healthcare for marginalized groups were small in magnitude. Whether these statistically significant effects are clinically meaningful warrants assessment in real-world care settings (e.g., college/university counseling centers). Third, although repeated cross-sectional designs can limit longitudinal inferences (Kraemer et al., 2000), we did not identify cohort effects in our data (a primary concern for repeated cross-sectional studies) and made analytic choices to adjust for other potential biases of this nature; consequently, concerns associated with this study design are likely minimal. Fourth, although the SCOFF is a widely-used ED screening measure (Botella et al., 2013; Kutz et al., 2020), it mainly assesses cognitive ED symptoms and is not a diagnostic assessment. Future research is needed to examine how the identified prevalence estimates align with estimates for behavioral ED symptoms and confirmed ED diagnoses. Finally, the COVID-19 pandemic has negatively impacted individuals’ ED symptoms (Linardon et al., 2022). Although this impact is likely minimal among the present sample, as few participants (7.27%) completed the HMS post-COVID onset, the role of COVID-19 in relation to college students’ ED symptoms should be assessed in future studies.
4.4 |. Implications
The present study also has several implications that may warrant consideration in prevention and intervention efforts designed to address ED concerns among U.S. college students. For example, individuals living in larger bodies and those who identified as male (vs. female), bisexual, and gay, lesbian, or queer (vs. heterosexual) exhibited increasing ED pathology over time. This evidence of growing ED symptom disparities for these groups stresses the necessity of applying a health equity lens to ED prevention and treatment, the urgent need to identify social and structural/systemic determinants of these disparities (e.g., sizeism/fatphobia, heterosexism), and the need for system-level policies designed to increase culturally-competent healthcare for marginalized groups. Further, screening efforts to identify prodromal ED symptoms among individuals comprising these at-risk groups appears increasingly warranted, alongside those with the additional diverse sexual, gender, and racial/ethnic identities that were found to have consistently elevated burden of ED symptoms over time.
Supplementary Material
Funding information
National Institute of Mental Health, Grant/Award Numbers: F31MH120982, K01MH121515; National Institute on Drug Abuse, Grant/Award Number: K01DA054357; National Institute on Minority Health and Health Disparities, Grant/Award Number: F31MD015203; William T. Grant Foundation
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of the article at the publisher’s website.
DATA AVAILABILITY STATEMENT
The present data is available from https://healthymindsnetwork.org/research/data-for-researchers/ and code will be made available upon reasonable request.
REFERENCES
- American College Health Association. (2022). American college health association-National College Health Assessment III: Reference group executive summary fall 2021. American College Health Association. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Bohrer BK, Carroll IA, Forbush KT, & Chen PY (2017). Treatment seeking for eating disorders: Results from a nationally representative study. International Journal of Eating Disorders, 50(12), 1341–1349. [DOI] [PubMed] [Google Scholar]
- Botella J, Sepúlveda AR, Huang H, & Gambara H (2013). A metaanalysis of the diagnostic accuracy of the SCOFF. The Spanish Journal of Psychology, 16, 1–8. 10.1017/sjp.2013.92 [DOI] [PubMed] [Google Scholar]
- Cachelin FM, & Striegel-Moore RH (2006). Help seeking and barriers to treatment in a community sample of Mexican American and European American women with eating disorders. International Journal of Eating Disorders, 39(2), 154–161. 10.1002/eat.20213 [DOI] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. 10.1080/10705510701301834 [DOI] [Google Scholar]
- Da Luz FQ, Sainsbury A, Mannan H, Touyz S, Mitchison D, & Hay P (2017). Prevalence of obesity and comorbid eating disorder behaviors in South Australia from 1995 to 2015. International Journal of Obesity, 41(7), 1148–1153. 10.1038/ijo.2017.79 [DOI] [PubMed] [Google Scholar]
- Fischer KA, Klein AG, & Reinecke J (2019). Nonlongitudinal estimation of growth curve parameters: The cohort growth model. Structural Equation Modeling: A Multidisciplinary Journal, 26(3), 402–417. [Google Scholar]
- Galmiche M, Déhelotte P, Lambert G, & Tavolacci MP (2019). Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. The American Journal of Clinical Nutrition, 109(5), 1402–1413. 10.1093/ajcn/nqy342 [DOI] [PubMed] [Google Scholar]
- Ganson KT, Rodgers RF, Murray SB, & Nagata JM (2021). Prevalence and demographic, substance use, and mental health correlates of fasting among US college students. Journal of Eating Disorders, 9(1), 1–12. 10.1186/s40337-021-00443-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB (2017). Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obesity Reviews, 18(4), 412–449. 10.1111%2Fobr.12491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grillot CL, & Keel PK (2018). Barriers to seeking treatment for eating disorders: The role of self-recognition in understanding gender disparities in who seeks help. International Journal of Eating Disorders, 51(11), 1285–1289. [DOI] [PubMed] [Google Scholar]
- Hart LM, Gordon AR, Sarda V, Calzo JP, Sonneville KR, Samnaliev M, & Austin SB (2020). The association of disordered eating with health-related quality of life in US young adults and effect modification by gender. Quality of Life Research, 29, 1203–1215. 10.1007/s11136-019-02396-2 [DOI] [PubMed] [Google Scholar]
- Healthy Minds Study Network (2022). Healthy minds study annual reports [Dataset]. https://healthymindsnetwork.org/research/data-for-researchers/ [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348–358. 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Chiu WT, Deitz AC, Hudson JI, Shahly V, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, de Graaf R, Maria Haro J, Kovess-Masfety V, O’Neill S, Posada-Villa J, Sasu C, Scott K, Viana MC, … Xavier M (2013). The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biological Psychiatry, 73(9), 904–914. 10.1016/j.biopsych.2012.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Yesavage JA, Taylor JL, & Kupfer D (2000). How can we learn about developmental processes from cross-sectional studies, or can we? American Journal of Psychiatry, 157(2), 163–171. [DOI] [PubMed] [Google Scholar]
- Kutz AM, Marsh AG, Gunderson CG, Maguen S, & Masheb RM (2020). Eating disorder screening: A systematic review and metaanalysis of diagnostic test characteristics of the SCOFF. Journal of General Internal Medicine, 35(3), 885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liechty JM, & Lee M (2013). Longitudinal predictors of dieting and disordered eating among young adults in the US. International Journal of Eating Disorders, 46(8), 790–800. 10.1002/eat.22174 [DOI] [PubMed] [Google Scholar]
- Linardon J, Messer M, Rodgers RF, & Fuller-Tyszkiewicz M (2022). A systematic scoping review of research on COVID-19 impacts on eating disorders: A critical appraisal of the evidence and recommendations for the field. International Journal of Eating Disorders, 55(1), 3–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipson SK, & Sonneville KR (2017). Eating disorder symptoms among undergraduate and graduate students at 12 US colleges and universities. Eating Behaviors, 24, 81–88. 10.1016/j.eatbeh.2016.12.003 [DOI] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, & Diniz JB (2011). Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders, 44(5), 412–420. 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Slewa-Younan S, & Mond J (2012). Time trends in population prevalence of eating disorder behaviors and their relationship to quality of life. PLoS One, 7(11), e48450. 10.1371/journal.pone.0048450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Slewa-Younan S, & Mond J (2014). The changing demographic profile of eating disorder behaviors in the community. BMC Public Health, 14(1), 1–9. 10.1186/1471-2458-14-943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, Touyz S, González-Chica DA, Stocks N, & Hay P (2017). How abnormal is binge eating? 18-year time trends in population prevalence and burden. Acta Psychiatrica Scandinavica, 136(2), 147–155. 10.1111/acps.12735 [DOI] [PubMed] [Google Scholar]
- Mond JM, Hay PJ, Darby A, Paxton SJ, Quirk F, Buttner P, Owen C, & Rodgers B (2009). Women with bulimic eating disorders: When do they receive treatment for an eating problem? Journal of Consulting and Clinical Psychology, 77(5), 835. [DOI] [PubMed] [Google Scholar]
- Morgan JF, Reid F, & Lacey JH (1999). The SCOFF questionnaire: Assessment of a new screening tool for eating disorders. British Medical Journal, 319(7223), 1467–1468. 10.1136/bmj.319.7223.1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagata JM, Ganson KT, & Murray SB (2020). Eating disorders in adolescent boys and young men: An update. Current Opinion in Pediatrics, 32(4), 476–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez M, Ohrt TK, & Hoek HW (2016). Prevalence and treatment of eating disorders among Hispanics/Latino Americans in the United States. Current Opinion in Psychiatry, 29(6), 378–382. 10.1097/YCO.0000000000000277 [DOI] [PubMed] [Google Scholar]
- Qian J, Wu Y, Liu F, Zhu Y, Jin H, Zhang H, Wan Y, Li C, & Yu D (2021). An update on the prevalence of eating disorders in the general population: A systematic review and meta-analysis. Eating and Weight Disorders, 27(2), 415–428. 10.1007/s40519-021-01162-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano KA, Heron KE, Amerson R, Howard LM, MacIntyre RI, & Mason TB (2020). Changes in disordered eating behaviors over 10 or more years: A meta-analysis. International Journal of Eating Disorders, 53(7), 1034–1055. 10.1002/eat.23288 [DOI] [PubMed] [Google Scholar]
- Romano KA, & Lipson SK (2021). Weight misperception and thin-ideal overvaluation relative to the positive functioning and eating disorder pathology of transgender and nonbinary young adults. Psychology of Sexual Orientation and Gender Diversity, 1–8. 10.1037/sgd0000524 [DOI] [Google Scholar]
- Solmi F, Hatch SL, Hotopf M, Treasure J, & Micali N (2014). Prevalence and correlates of disordered eating in a general population sample: The South East London Community Health (SELCoH) study. Social Psychiatry and Psychiatric Epidemiology, 49(8), 1335–1346. 10.1007/s00127-014-0822-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonneville KR, & Lipson SK (2018). Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. International Journal of Eating Disorders, 51(6), 518–526. [DOI] [PubMed] [Google Scholar]
- Streatfeild J, Hickson J, Austin SB, Hutcheson R, Kandel JS, Lampert JG, Myers EM, Richmond TK, Samnaliev M, Velasquez K, Weissman RS, & Pezzullo L (2021). Social and economic cost of eating disorders in the United States: Evidence to inform policy action. International Journal of Eating Disorders, 54(5), 851–868. 10.1002/eat.23486 [DOI] [PubMed] [Google Scholar]
- Thapliyal P, Mitchison D, Mond J, & Hay P (2018). Gender and help-seeking for an eating disorder: Findings from a general population sample. Eating and Weight Disorders, 25(1), 215–220. [DOI] [PubMed] [Google Scholar]
- Thompson KA, DeVinney AA, Goy CN, Kuang J, & Bardone-Cone AM (2021). Subjective and objective binge episodes in relation to eating disorder and depressive symptoms among middle-aged women. Eating and Weight Disorders, 1–8. 10.1007/s40519-021-01305-2 [DOI] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and correlates of DSM-5–defined eating disorders in a nationally representative sample of US adults. Biological Psychiatry, 84(5), 345–354. 10.1016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2019). Psychiatric and medical correlates of DSM-5 eating disorders in a nationally representative sample of adults in the United States. International Journal of Eating Disorders, 52(1), 42–50. 10.1002/eat.23004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The present data is available from https://healthymindsnetwork.org/research/data-for-researchers/ and code will be made available upon reasonable request.


