Abstract
Background:
Strengthening HIV prevention services is a key priority of the Ending the HIV Epidemic plan. Informed by the Consolidated Framework for Implementation Research, we examined HIV Testers’ perceived barriers and facilitators to implementing HIV prevention services, including Testers’ strengths and weaknesses, enabling factors within the inner and outer settings, and willingness to adopt potential implementation strategies.
Methods:
In 2019, the Penn Center for AIDS Research (CFAR) partnered with the Philadelphia Department of Public Health (PDPH) to examine systems-level challenges and opportunities experienced by PDPH-funded HIV Testers (individuals conducting HIV testing) in Philadelphia. We recruited HIV Testers to complete two web-surveys (n≈40 each) and in-depth interviews (n=11).
Results:
Testers self-reported high HIV testing self-efficacy and competence, despite identifying gaps in their knowledge of STI testing, reporting moderate willingness to recommend PrEP, and having insufficient cultural competency when working with priority populations. Testers indicated that educational materials and policies within their agencies might require re-alignment to affirm sexual and gender minority clients. In qualitative interviews, Testers noted challenges to implementing PDPH priorities as limited funding fueled competition between local agencies, deterred inter-agency partnerships, and limited their ability to serve key populations locally.
Discussion:
HIV Testers are critical partners in addressing agency-level barriers to HIV prevention service provision through multilevel implementation strategies. In partnership with PDPH, we will create and implement a train-the-trainers program consisting of skill building activities, technical assistance, and capacity-building for all agency personnel to address missed opportunities in HIV prevention. These activities will reinforce scalability and sustainability of PDPH-supported HIV prevention programs.
Keywords: Implementation science, Service delivery, PrEP
INTRODUCTION
Increasing HIV testing and pre-exposure prophylaxis (PrEP) in high HIV prevalence jurisdictions is a priority of the federal Ending the HIV Epidemic (EHE) in the U.S. initiative, which aims to reduce HIV incidence by 90% by 2030.1 As an EHE jurisdiction, Philadelphia County has prioritized increasing HIV testing and PrEP uptake among behaviorally at-risk populations with a plan to ensure that 97% of people living with HIV know their status and that 50% of individuals indicated for PrEP are prescribed the medication by 2025.2
While increasing individual-level PrEP awareness is essential, PrEP can only lead to population-level HIV reductions if health systems have the knowledge, capacity, and infrastructure for successful and inclusive HIV testing and PrEP implementation.3 However, HIV testing expansion and PrEP implementation efforts across the U.S. have been inequitably distributed.4, 5 Consistent with national trends,6, 7 HIV testing and PrEP initiation rates among non-Latinx Black and Latinx individuals have been lower than their White counterparts. Similarly, young cisgender men and transgender women who have sex with men (YMSM/TW) have lower HIV testing and PrEP uptake rates than adults aged ≥25 years.8, 9 Health department data regarding the uptake of community-based HIV testing in 2019 indicate that MSM accounted for 21% of all Philadelphia community-based HIV tests, even though estimates based on HIV incidence suggest that approximately 60% of the tests should have been performed in this key population. In contrast, 52.6% of HIV tests in 2019 were among heterosexuals, even though only 22% of the tests would be expected to be in this group based on HIV incidence estimates.10
The Philadelphia EHE plan also provides guidance to strengthen the HIV health workforce. HIV prevention staff must be well-equipped to address the unique needs of key populations, including providing care aligned with anti-racist and equity centered principles, co-locating gender-affirming and sexual health services within HIV prevention care, and offering youth-friendly services that attend to the developmental needs of adolescents and young adults.1, 2 Therefore, it is critical for research efforts to prioritize identifying and addressing the barriers impeding the evidence-based delivery of comprehensive, sexuality- and gender-affirming HIV prevention services across a broad range of HIV prevention settings.11 To be scalable across health department-funded agencies and reach intended service users, research is needed to identify implementation strategies that are standardized to Centers for Disease Control and Prevention (CDC) guidelines,12 grounded in a model of care that affirms the lived experiences of clients, and flexible enough to allow tailoring to each agency’s needs and resources.13
The Consolidated Framework for Implementation Research (CFIR) provides tools to systematically identify the necessary, multilevel factors across five domains pertinent to health care systems that facilitate effective adaptation, adoption, evaluation, and implementation of evidence-based interventions.14 With respect to HIV testing and PrEP scale up, the five CFIR domains (www.cfirguide.org) are: 1) Intervention Characteristics, including features of these evidence-based practices (e.g., cost, availability, and complexity) that may impact implementation; 2) Outer Setting, capturing influential implementation factors external to agencies (e.g., patient needs, public health policies, funding, and inter-agency collaboration); 3) Inner Setting, encompassing the culture, workflow, and environment within agencies; 4) Individual Characteristics, including the beliefs, knowledge, attitudes, and readiness for change within agency Testers and Agency Directors; and 5) Process, the strategies used to realize testing and PrEP goals within agencies.
Informed by CFIR, our research sought to enumerate barriers and facilitators to comprehensive HIV prevention service scale-up within the Philadelphia Department of Public Health (PDPH)-funded HIV agencies and leverage these findings to guide intervention development/adaptation, implementation strategies, and project evaluation for a multilevel intervention to strengthen HIV prevention services for YMSM/TW.
METHODS
We conducted a mixed methods EHE implementation research collaboration between the University of Pennsylvania Center for AIDS Research (Penn CFAR) and the PDPH. The study’s primary aim was to identify systems-level HIV prevention challenges and opportunities experienced by PDPH-funded HIV Testers in Philadelphia. The University of Pennsylvania and PDPH Institutional Review Boards approved all procedures.
Sample
In the Fall of 2019, PDPH-funded HIV Testers were invited to complete a 15-minute, confidential, voluntary web-survey about their experiences and challenges with HIV prevention service provision at their agencies. Testers were identified via a list provided by the PDPH and were eligible to participate if they were a state-certified HIV Tester at a city-funded testing agency. In Fall 2020, we invited a second round of eligible Testers to complete a subsequent survey. For each survey, eligible participants were sent up to four weekly reminders to complete the surveys. The first and second surveys had a 62% (n=31/50 Testers) and 53% response rate (n =42/80 Testers), respectively, with a final total sample size of 73 Testers (56.2% response rate). To capture the voices of Testers who did not respond to either survey invitation as well as Agency Directors (n=27), we purposively sampled survey non-responders and Agency Directors to participate in semi-structured qualitative interviews. Participants who consented and completed research activities received a $20 Amazon e-gift card.
Data Collection
Both surveys were based on the PDPH AIDS Activities Coordinating Office HIV Testing Survey and measured similar constructs, including respondent demographics and service provision, encompassing typical Tester duties (HIV test counseling, condom provision, linkage to HIV care, PrEP counseling and navigation) and duties not standardly provided by all agencies (medication assisted therapy for opioid addiction, HIV post-exposure prophylaxis (PEP), syringe exchange, STI testing and treatment). Items regarding Testers’ knowledge, attitudes, and practices were developed by PDPH and had a 7th grade literacy level. Both surveys assessed CFIR-related domains with the exception of “Process” as our research was to assess pre-intervention implementation barriers and facilitators and generate implementation strategies. For the Individual Characteristics domain, items assessed participants’ perceived ability to engage clients in HIV test counseling; comfort with screening, discussing, and linking their clients to PrEP; and perceived training needs. For Inner Setting, items assessed perceived work support and climate, including the presence of cues signaling their agency as a safe space for LGBTQ+ communities. The semi-structured interview guides included open-ended questions about daily responsibilities, perceived barriers to high-quality prevention service delivery, and external factors affecting service delivery (e.g., funding, policies, community factors). Interviews were conducted via teleconference, audio-recorded and lasted 45–60 minutes. We achieved saturation across our thematic domains with the completion of 11 interviews, which included eight HIV Testers and three Agency Directors.
Data Analysis
Given our study’s exploratory nature and small sample size, we include univariate findings from both surveys. Qualitative interviews were professionally transcribed verbatim for analysis. Two study team members developed a codebook based on CFIR constructs and used thematic analysis to analyze the transcripts deductively. We revised the codebook iteratively to capture emerging additional themes from the data. Both team members independently coded all transcripts, meeting to discuss coding discrepancies and reach consensus across codes (100% inter-rater agreement).
RESULTS
CFIR Domain #1: Characteristics of the Individuals
Participant sociodemographic characteristics are provided in Table 1, with no differences observed between those who completed the first and second web-surveys. Participants’ mean age was 36.4 years (standard deviation [sd]=11.6) in the first and 39.9 years (sd=12.6) in the second survey. Both surveys included a majority non-Latinx Black sample, had a near-even split between cisgender males and cisgender females with a small number of transgender and non-binary participants, and a near-even split between heterosexual and sexual minority (LGBQ+) participants. Most participants were salaried employees, had been at their agency for ≥6 months, and had been an HIV Tester for ≥3 years.
Table 1.
Participant Characteristics
| Survey 1 N = 31 |
Survey 2 N = 42 |
|||
|---|---|---|---|---|
| Variable | m (sd) | n (%) | m (sd) | n (%) |
| Age | 36.4 (11.6) | 39.9 (12.6) | ||
| Race/Ethnicity | ||||
| Non-Latinx Black | 20 (64.5) | 23 (54.8) | ||
| Latinx | 2 (6.5) | 9 (21.4) | ||
| Other | 9 (29.0) | 8 (19.0) | ||
| No Response | 0 (0.0) | 2 (4.8) | ||
| Current Gender Identity | ||||
| Cisgender Male | 16 (51.6) | 19 (45.2) | ||
| Cisgender Female | 12 (41.9) | 22 (52.4) | ||
| Transgender Female | 1 (3.2) | 0 (0.0) | ||
| Nonbinary | 1 (3.2) | 1 (2.4) | ||
| Sexual Orientation | ||||
| Heterosexual | 14 (45.2) | 23 (54.8) | ||
| LGBQ+ | 17 (54.8) | 19 (45.2) | ||
| Income Type | ||||
| Salaried | 20 (64.5) | 32 (76.2) | ||
| Non-Salaried/Hourly | 11 (35.5) | 10 (23.8) | ||
| Length of Time at Agency | ||||
| 0 – 2 Months | 1 (3.2) | 0 (0.0) | ||
| 3 – 5 Months | 2 (6.5) | 1 (2.4) | ||
| 6 – 11 Months | 8 (25.8) | 5 (11.9) | ||
| 12 Months or More | 20 (64.5) | 36 (85.7) | ||
| HIV Tester History | ||||
| Less than 1 Year | 4 (12.9) | 4 (9.5) | ||
| 1 – 2 Years | 7 (22.6) | 4 (9.5) | ||
| 3 – 4 Years | 9 (29.0) | 9 (21.4) | ||
| 5 – 7 Years | 3 (9.7) | 8 (19.0) | ||
| 8 – 10 Years | 4 (12.9) | 6 (14.3) | ||
| 11 – 15 Years | 2 (6.5) | 5 (11.9) | ||
| 15+ Years | 2 (6.5) | 6 (14.3) | ||
Most Testers were knowledgeable about HIV treatment and prevention concepts including PrEP, PEP, and viral suppression (Table 2). However, Testers were more likely to have gaps in knowledge related to HIV testing technologies and STIs, and best practices associated with comprehensive sexual health care competencies. For example, only 36% of Testers believed that PrEP effectively prevents HIV transmission when having condomless sex.
Table 2.
HIV Prevention and Care Knowledge
| Item | % Correct |
|---|---|
| A 4th generation HIV test (like Determine™) detects antibodies and antigens. | 64.5% |
| The window period for detecting a new HIV case in a 4th generation HIV test is 30 days. | 41.9% |
| The INSTI™ rapid test detects antibodies only. | 83.9% |
| The window period for detecting a new HIV case using the INSTI™ rapid test is 21 days. | 41.9% |
| HIV treatment (antiretroviral medication) works to decrease viral load and increase CD4 cells. | 87.1% |
| A person living with HIV does not need insurance to access HIV care in the City of Philadelphia and surrounding counties. | 93.5% |
| PrEP is a pill that can be taken daily before a person is exposed to HIV to prevent HIV | 93.5% |
| Someone under the daily oral PrEP regimen should take one pill by mouth every day. | 96.8% |
| The current recommended dose for PrEP to effectively prevent HIV infection is once every day. | 100.0% |
| A person must start PEP within 72 hours after potential HIV exposure. | 90.3% |
| Post-exposure prophylaxis (PEP) is a pill that can be taken daily to prevent HIV after a person is exposed to HIV. | 96.8% |
| Bacterial STIs (Chlamydia, Gonorrhea, and Syphilis) are curable. | 80.6% |
Testers reported high perceived ability to perform HIV testing job responsibilities (Table 3) and willingness to strengthen their knowledge and skills. In qualitative interviews, HIV Testers affirmed high levels of self-efficacy around HIV testing and PrEP counseling, but also noted that continued training was critical to maintaining skills and staying current with the latest science:
“As far as providing HIV testing, I feel like everyone is really proficient in that…I do think that training should occur…throughout the year just to make sure that we’re on the same page, like, as far as…terminology or instructions or new tests or just new…information.”
Table 3.
Perceived Ability in HIV Testing, N = 42
| Thinking about your experiences as an HIV Tester, please reflect on your ability to do the following activities during an HIV testing visit (1=Poor; 4=Excellent): | m (sd) |
|---|---|
| Explain client confidentiality before HIV testing | 3.6 (0.7) |
| Help a client cope with their HIV diagnosis if their HIV test is positive | 3.5 (0.6) |
| Immediately link a client to HIV care if their HIV test is positive | 3.6 (0.7) |
| Explore whether HIV pre-exposure prophylaxis (PrEP) is right for a client | 3.5 (0.6) |
| Discuss benefits and risks of HIV post-exposure prophylaxis (PEP) with a client | 3.5 (0.6) |
| Offer condoms and lubricant (as appropriate) to a client | 3.7 (0.5) |
| Refer people who are using drugs (e.g., opioids, injection drug use) to naloxone and syringe access programs | 3.1 (0.7) |
| Refer a client to test for other STI services, including STI testing and treatment | 3.5 (0.6) |
| Explore clients’ reasons for testing if they identify as cisgender women | 3.4 (0.6) |
| Explore clients’ reasons for testing if they are people who inject drugs | 3.6 (0.5) |
| Explore clients’ reasons for testing if they identify as transgender or non-binary | 3.5 (0.6) |
| Explore clients’ reasons for testing if they identify as men who have sex with men | 3.6 (0.5) |
Across the surveys, the most endorsed HIV testing challenges were explaining client confidentiality before testing (9.5%) and immediately linking a client to HIV care if their test was reactive (9.5%). Overall, participants reported high levels of comfort with PrEP counseling. The primary challenge to participants’ PrEP service provision was assisting clients in setting up appointments with a PrEP provider (9.5% rated this task from neutral to completely uncomfortable). Testers noted lacking confidence in their behavioral skills to provide ancillary HIV prevention services, including overdose prevention counseling to people who inject drugs (PWID) (19.4%), referring PWID to naloxone and syringe access programs (29.0%), and exploring transgender and non-binary clients’ reasons for testing (19.4%). When asked to rank among topic areas for skill building, the top topics selected based on the proportion of participants who endorsed a need for training were Opioids 101 (75%), cultural competency when working with transgender populations (50%) and PWID (29%), PEP (29%), and STIs and HIV prevention (29%).
CFIR Domain #2: Intervention Characteristics
Participants endorsed HIV testing as effective and necessary. However, Testers had differing views on PrEP as a public health strategy. Many Testers suggested that PrEP counseling was well-integrated into the HIV testing workflow, stating that they talk about PrEP with nearly every client. Testers’ narratives regarding PrEP counseling discussions, however, highlighted a need for additional training to avoid stigmatizing language and assumptions based on perceived behavioral risk. As one Tester mentioned:
“Depending on how you answer the forms, like, ‘cause there’s a whole PrEP section on the form… So, yeah, it depends on those lifestyle questions, then would be like, “Yo, you should get PrEP.” Or “yeah, [LAUGH] you should definitely get PrEP.”
Staff often identified the complexity of PrEP services as a major barrier to implementation. Testers spoke about the multitude of steps required of clients to successfully link to PrEP care, including scheduling appointments, navigating insurance, and maintaining motivation to engage with PrEP.
“But then, it became the point of, ‘Okay, well, how do I get it? Oh, I have to go through all these steps.’… Now you got to fill out this form, and then someone will be in contact with you in a couple days. And then…they might not be in a space to answer the phone…And then from there, well then, okay, let’s handle insurance. So there’s…too many steps…before you actually get the product.”
Taken together, the series of complex steps needed to link clients to PrEP successfully often prevented all but the most well-resourced and highly motivated individuals from accessing PrEP and risked leaving YMSM/TW behind, as one Tester noted:
“I want to be able to give you PrEP. I want to have it available say ‘hey this is what you need.’ But in that process to get there [are] also obstacles in the way of making sure young people get the pill that they desperately need…”
Nearly half of Testers reported concerns about PrEP leading to risk compensation (i.e., intentionally avoiding condom use motivated by lower perceived HIV risk) and highlighted the belief that using PrEP might facilitate sexual behaviors that increase STI risk. As one Agency Director noted:
“…I also think that it has led to an increase in STIs. You know, I think there is a lot more unprotected sex; I think people’s guards are down with PrEP, it’s not 100% effective as we know… there have been a few breakthrough infections, but you know we’ve seen a lot more STIs.”
With respect to YMSM/TW, one Tester noted that some Testers or providers were reluctant to provide PrEP to youth, because they felt that youth shouldn’t be sexually active. Aligned with these sentiments, our first web-survey indicated that 41.6% of Testers agreed that “PrEP causes people to make unsafe choices”, and 45.2 % agreed that “People who take PrEP are likely to have more unsafe sex which will take away the benefit of PrEP.”
CFIR Domain #3: Inner Setting
In general, Testers reported high levels of work support, as measured by work autonomy (i.e., ability to make an important decision about their clients, m=4.1, range: 1–5, sd=1) and safety (m=4.4, range: 1–5, sd=0.7). Interpersonally, participants reported high levels of support from co-workers (m=3.9, range: 1–5, sd=1.0) and supervisors (m=4.0, range: 1–5, sd=1.1).
The availability of resources emerged as an essential factor shaping PrEP implementation across agencies. Specifically, staff suggested that lacking on-site PrEP services was a major barrier to successfully linking clients to PrEP, and that referrals to an outside organization for PrEP services opened more opportunities for linkage to fail. One Agency Director said:
“We may build that trust and now we gonna try to hand you off to somebody else. And that could be how we lose that person. It would be easier if we were able to give PrEP… Then it becomes easier that we become that connection.”
Even at agencies with robust clinical programs capable of providing on-site PrEP, Testers reported that clients struggled to get timely appointments with medical providers:
“I just see that sometimes it’s not immediately the service for the clients, sometimes it takes two to three months, … I hear from some of the clients say, ‘Oh, it takes forever with you guys to get referral to PrEP.’ …so we’re kind of tied up in the bureaucracy as well… And the resources are not as abundant as we would like to have it.”
Finally, it was noted that tailoring for youth that accounts for their health literacy and culture was needed to improve care delivery in the Inner Setting:
“[Some agencies], they service… young queer youth that can be candidate for PrEP, um, but they’re very sterile…. the language they use is very academic, and not everybody has access to that language, and that can be intimidating for someone who is queer, who is Black or Brown and is homeless and hasn’t finished high school…I think these organizations focus on being culturally competent, um, but they aren’t culturally affirmative.”
CFIR Domain #4: Outer Setting Characteristics Affecting Testing and PrEP
Limited funding, a focus on outcome metrics, and the transition into a biomedical HIV prevention system fueled competition between local agencies, deterred inter-agency partnerships, and were perceived to create additional workplace stress without improving the quality of services. One Tester described these pressures:
“You have to do this many tests a-month and you have to refer this many clients to PrEP per month. It’s too much focus on the numbers and when you do that you’re putting everybody else in competition with one another. We’re not in the financial banking field…This is helping people, saving people’s lives. Let’s break this barrier.”
An Agency Director echoed this sentiment, highlighting how funding competition disincentivizes inter-agency collaborations, not just in Philly but throughout the country:
“Because the problem with Philly and as every conference I ever go to… in other jurisdictions is that we are all pinned up against each other because we’re competing for funding.”
Staff also discussed how a lack of cosmopolitanism, or networking with other external organizations, hindered achievement of common goals across agencies. When asked about whether their agency promoted networking with other organizations, one Tester explained that there was little institutional support and that they instead had to seek networking opportunities independently.
Finally, with respect to better addressing the patient needs in the Outer Setting, both Testers and Agency Directors discussed the need for welcoming and stigma-reducing environments for Black and Latinx YMSM/TW that reflect their communities:
“[Testing site] is right in the middle of Center City, right by the Gayborhood, but it’s also by [universities]… and all of the-people that probably already have coverage and can get [HIV testing] done at their health centers at their schools or their physician or PCP. But when we have… people that are outside of our primary population in such large numbers coming, guess who’s the first people to walk out when there’s a line of people waiting to be seen? Trans and MSM, that are …people of color. They’re like, ‘I’m not gonna wait.’…People are already having anxiety, and then they see a room full of like, people outside of their community.”
Staff also noted the importance of addressing competing priorities around housing, food, jobs, and other social needs in the providing HIV testing and PrEP services to YMSM/TW:
“…It really does come down to people that are under resourced, in all… all the ways. We’re talking about like, yes, insurance. Yes, employment. Yes, education. …But we’re also talking about social systems and social support, um, and so there’s this…whole group of unsupported individuals that …it doesn’t seem that to be as HIV is the top priority.”
DISCUSSION
Engaging HIV Testers and Agency Directors as partners in addressing barriers to HIV prevention service provision is critical for implementing PDPH’s EHE strategic planning activities in Philadelphia County. The high self-reported HIV testing self-efficacy, competence, and collegial support evidenced among Testers will be leveraged to improve agency-level HIV prevention knowledge gaps and culturally competent service provision within local priority populations, including YMSM/TW. Specifically, PDPH is recalibrating their HIV Testing and PrEP programs through several implementation strategies, including strengthening the HIV healthcare workforce’s training on health equity and inclusive service delivery; reshaping prevention services delivery through new low-threshold sexual wellness centers aiming to reduce barriers to PEP, HIV/STI testing, and PrEP uptake; and refining investments in HIV community-based testing.
Our ongoing CFAR-PDPH EHE partnership has used these planning data to inform the technical assistance and capacity building detailed in the data-informed implementation science logic model15 (Figure 1) guiding this ongoing work. Our model highlights how key factors (in bold) identified in our survey and interview data across CFIR domains can support or hinder the effective implementation of PrEP for YMSM/TW in Philadelphia. The gray boxes describe the implementation strategies and mechanisms by which we will leverage and extend PDPH’s ongoing quality improvement work with agencies to develop and implement trainings to ameliorate gaps in prevention knowledge, self-efficacy, and cultural humility and facilitate environmental changes to make services more inclusive of YMSM/TW clients. These include trainings to address biased perceptions about PrEP and risk compensation identified in our surveys and interviews and in previous HIV testing literature.16, 17 Finally, consistent with our Type II hybrid implementation effectiveness design, we will collect Implementation and Pragmatic Effectiveness (Service and Clinical) Outcomes (with areas emphasized in our survey data in bold) to ensure we are meeting the context-specific goals of PDPH’s Philadelphia EHE plan.
Figure 1. Conceptual Implementation Research Logic Model.
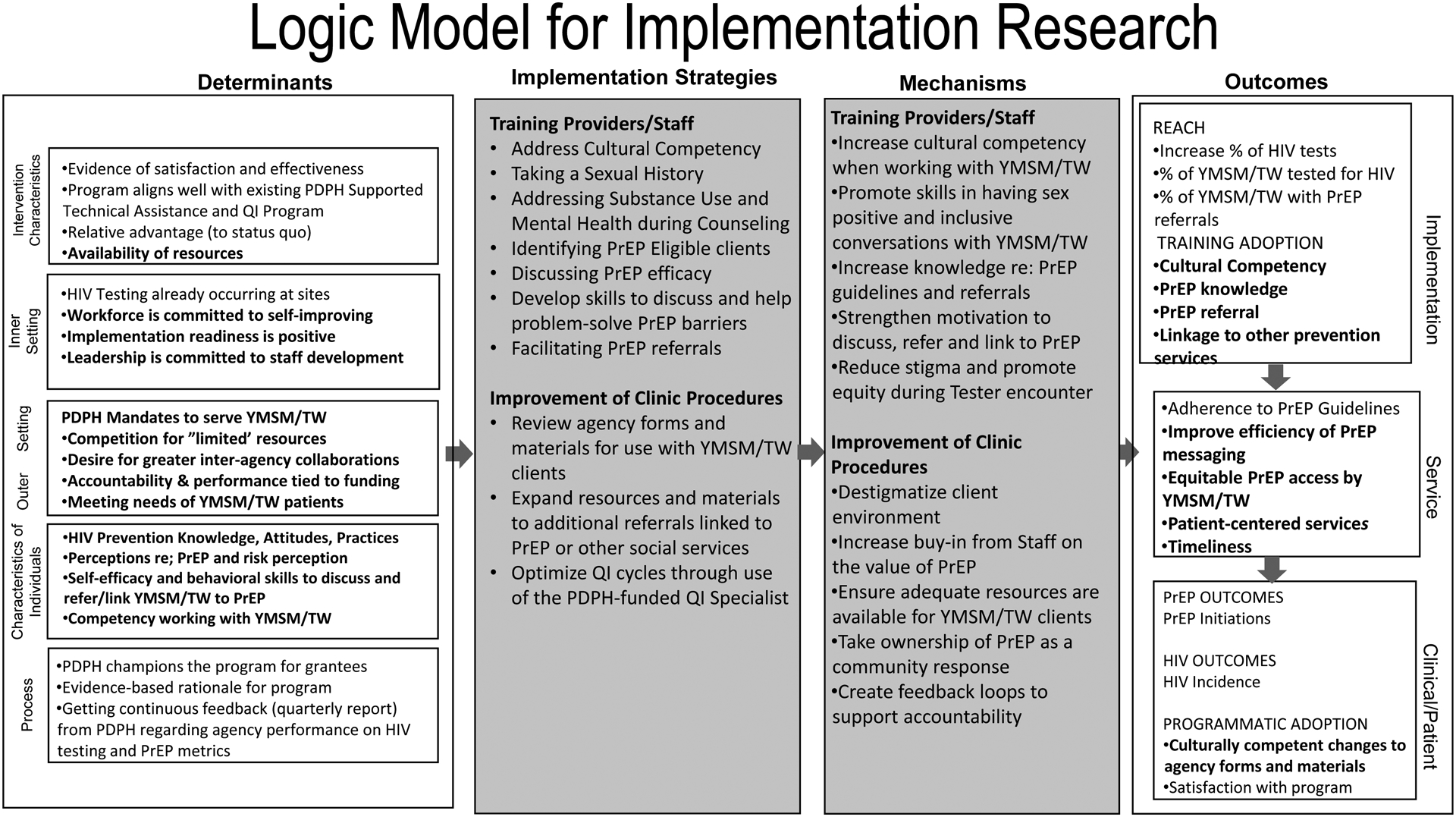
Our implementation logic model aligns with the ISC3I logic model recommended for EHE grantees. Within this model our CFAR EHE planning supplement has highlighted how key factors across CFIR domains hinder the effective implementation of PrEP for YMSM/TW in Philadelphia. The Gray boxes denote Implementation Mechanisms and Strategies for addressing these barriers and facilitators. The Outcomes boxes to the right denote the outcome measurements for ensuring our work aligns with key EHE priorities. Bolded items reflect concepts identified within this foundational EHE research.
Attending to agency Inner Settings, limited funding and/or personnel was widely cited as a major barrier to implementing services. As the need for affirming and equitable service provision for YMSM/TW from multiple marginalized backgrounds is increasingly prioritized, so too is the need for collaboration across the Outer Setting to facilitate the consolidation of local resources (e.g., PrEP prescribers, syringe access programs). Future implementation strategies should focus on alleviating the competitive pressure engendered by limited funding. For example, funding opportunities that incentivize innovative collaborations among agencies may expand HIV prevention service provision across priority populations and reduce the extent to which individual agencies feel siloed within a single priority population. These inter-agency linkages could provide ideal spaces to address potential biases and stigmatizing beliefs toward PrEP and reduce hesitancy toward integrating PrEP-supportive services within priority populations, including PWID and YMSM/TW. Lastly, increasing collaborations between agencies, including those with on-site PrEP availability, may empower less-resourced agencies to successfully navigate PrEP linkage for their clients.
Finally, PrEP navigation is one of the most challenging Outer Setting barriers to address. The need to adapt existing PrEP programs during the COVID-19 pandemic exacerbated barriers in linkage to PrEP. Reducing the complexity of PrEP delivery will be critical to ensuring equitable provision to YMSM/TW who also bear disproportionately greater burdens of systemic barriers to care. Our capacity building efforts will focus on developing trainings that can standardize education across agencies to help reduce complexity and will be updated as needed when new innovations are introduced to help ameliorate structural burdens to care. It is unclear the degree to which the recently revised Affordable Care Act patient protections requiring qualified health plans, including Medicaid expansion programs and commercial health plans, to cover PrEP at no cost to the client will ameliorate implementation complexity. The PDPH is working actively with HIV testing agencies to raise awareness and support the expansion of this new protection.
Our data have limitations. Testers who completed our surveys and interviews may have been more willing to share their experiences and offer insights regarding implementation barriers and facilitators than those who did not. As our research was intended to be foundational and hypothesis-generating, we could not assess the impact of agency characteristics on implementation attitudes. Our sample size of Agency Directors was small and precluded us making inferences about differences in perspective between Agency Directors and Testers. An important next step in implementation research across EHE settings will be to identify if there are Tester or Agency Director characteristics that are strongly associated with, for example, beliefs about PrEP and risk perception. These data could be used to identify specific program staff who may most benefit from targeted implementation strategies. Our participants reported strong perceptions that competition for funding has hindered local EHE efforts. Future research should quantitatively assess whether this belief is borne out in program outcomes. Finally, our goal was to assess implementation barriers and facilitators from the perspective of agency staff. Future research should also include the perspective of YMSM/TW Testing clients.
Next Steps
Our partnership will evaluate several implementation strategies18, 19 starting in Summer 2021, to achieve optimal HIV prevention service delivery at PDPH-funded agencies. These strategies will leverage existing PDPH programs and align with PDPH’s EHE priorities. For example, building on the PDPH’s remapping of services through a service restructuring strategy, we will employ educational and quality management implementation strategies for Testers. Trainings will focus on key areas identified in our data where additional capacity building is needed to fulfill our joint aim of improving provision of culturally competent and evidenced-based HIV prevention services to YMSM/TW in Philadelphia. These key areas include PrEP and PEP, STIs, cultural humility and motivational interviewing, community engagement, and LGBTQ competency. These efforts will support and reinforce implementation scalability and sustainability by training PDPH staff to deliver these trainings in the future.
Evidence-based innovations: HIV Testing and Pre-exposure prophylaxis (PrEP)
Innovation recipients: HIV Testers
Setting: Philadelphia Department of Public Health-funded agencies.
Implementation gap: While HIV testing is a key opportunity for linkage to PrEP, HIV Testers face individual, agency, and health system-level barriers to successfully linking priority populations, in particular young cisgender men and transgender women who have sex with men, to PrEP at the time of HIV testing.
Primary research goal: Identify determinants of implementation to inform strategies to increase linkage to prevention services by HIV Testers at PDPH-funded agencies.
Funding Support:
This research was supported by a grant from the Penn Center for AIDS Research (CFAR), an NIH-funded program (P30 AI 045008). This research was also funded through NIMH 1K23MH119976-01A1 (Wood). The content is solely the responsibility of the author and does not necessarily represent the official views of the funding agency.
Contributor Information
Sarah M. Wood, Craig Dalsimer Division of Adolescent Medicine, Children’s Hospital of Philadelphia; Department of Pediatrics, Perelman School of Medicine, University of Pennsylvania.
Steven Meanley, School of Nursing, University of Pennsylvania.
Stephen Bonett, School of Nursing, University of Pennsylvania,.
Mary Evelyn Torres, Philadelphia Department of Public Health.
Dovie L. Watson, Perelman School of Medicine, University of Pennsylvania.
Javontae L Williams, Philadelphia Department of Public Health.
Kathleen A. Brady, Philadelphia Department of Public Health.
José A. Bauermeister, School of Nursing, University of Pennsylvania.
REFERENCES
- 1.Department of Health and Human Services. Ending the HIV Epidemic: A Plan for America. 2020. Accessed June 11, 2021 https://files.hiv.gov/s3fs-public/EndingTheHIV-EpidemicPACHA.pdf
- 2.Philadelphia Department of Public Health. A Community Plan to End the HIV Epidemic in Philadelphia,2020 December 1, 2020. Accessed June 11, 2021 https://www.phila.gov/media/20201201165516/Ending-the-HIV-Epidemic-in-Philadelphia-A-Community-Plan.pdf
- 3.Bauermeister JA, Golinkoff JM, Lin WY, et al. Testing the Testers: Are Young Men Who Have Sex With Men Receiving Adequate HIV Testing and Counseling Services? J Acquir Immune Defic Syndr. Dec 1 2019;82 Suppl 2:S133–S141. doi: 10.1097/QAI.0000000000002173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calabrese SK. Understanding, Contextualizing, and Addressing PrEP Stigma to Enhance PrEP Implementation. Curr HIV/AIDS Rep. Sep 23 2020;doi: 10.1007/s11904-020-00533-y [DOI] [PubMed] [Google Scholar]
- 5.Pinto RM, Berringer KR, Melendez R, Mmeje O. Improving PrEP Implementation Through Multilevel Interventions: A Synthesis of the Literature. AIDS Behav. Nov 2018;22(11):3681–3691. doi: 10.1007/s10461-018-2184-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanny D, Jeffries WLt, Chapin-Bardales J, et al. Racial/Ethnic Disparities in HIV Preexposure Prophylaxis Among Men Who Have Sex with Men - 23 Urban Areas, 2017. MMWR Morb Mortal Wkly Rep. Sep 20 2019;68(37):801–806. doi: 10.15585/mmwr.mm6837a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goedel WC, King MRF, Lurie MN, Nunn AS, Chan PA, Marshall BDL. Effect of Racial Inequities in Pre-exposure Prophylaxis Use on Racial Disparities in HIV Incidence Among Men Who Have Sex With Men: A Modeling Study. J Acquir Immune Defic Syndr. Nov 1 2018;79(3):323–329. doi: 10.1097/QAI.0000000000001817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips G 2nd, Ybarra ML, Prescott TL, Parsons JT, Mustanski B. Low Rates of Human Immunodeficiency Virus Testing Among Adolescent Gay, Bisexual, and Queer Men. J Adolesc Health. Oct 2015;57(4):407–12. doi: 10.1016/j.jadohealth.2015.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. Dec 2018;28(12):841–849. doi: 10.1016/j.annepidem.2018.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Health PDoP. Unpublished data. 2021.
- 11.Hillis A, Germain J, Hope V, McVeigh J, Van Hout MC. Pre-exposure Prophylaxis (PrEP) for HIV Prevention Among Men Who Have Sex with Men (MSM): A Scoping Review on PrEP Service Delivery and Programming. AIDS Behav. Nov 2020;24(11):3056–3070. doi: 10.1007/s10461-020-02855-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. 2018;
- 13.Lambdin BH, Cheng B, Peter T, et al. Implementing Implementation Science: An Approach for HIV Prevention, Care and Treatment Programs. Curr HIV Res. 2015;13(3):244–9. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. Aug 7 2009;4:50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith JD, Li DH, Rafferty MR. The implementation research logic model: A method for planning, executing, reporting, and synthesizing implementation projects medRxiv. 2020;doi: 10.1101/2020.04.05.20054379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kundu I, Martinez-Donate A, Karkada N, et al. Attitudes and referral practices for pre-exposure prophylaxis (PrEP) among HIV rapid testers and case managers in Philadelphia: A mixed methods study. PLoS One. 2019;14(10):e0223486. doi: 10.1371/journal.pone.0223486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kutscha F, Gaskins M, Sammons M, Nast A, Werner RN. HIV Pre-Exposure Prophylaxis (PrEP) Counseling in Germany: Knowledge, Attitudes and Practice in Non-governmental and in Public HIV and STI Testing and Counseling Centers. Front Public Health. 2020;8:298. doi: 10.3389/fpubh.2020.00298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell BJ, Beidas RS, Lewis CC, et al. Methods to Improve the Selection and Tailoring of Implementation Strategies. J Behav Health Serv Res. Apr 2017;44(2):177–194. doi: 10.1007/s11414-015-9475-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. Feb 12 2015;10:21. doi: 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]


