Abstract
Objective:
To determine the feasibility, acceptability, and implementation of a HIV self-test (HIVST) program through PrEP clients’ social and sexual networks.
Background:
HIV testing is critical for treatment and prevention engagement. HIVST kits can overcome barriers to testing. A negative result is an opportunity to provide PrEP information. We describe implementation factors associated with engaging current Mobile PrEP (MP) clients to distribute HIVST kits and PrEP information through their networks.
Setting:
Community venues in Miami-Dade County, Florida.
Methods:
A baseline survey collected network information and explored distribution plans for offering HIVST kits. A follow-up survey evaluated use and distribution. A logic model describes the process of implementation and evaluation. Up to 4 Ora-Quick HIV ST kits were offered to 81 MP clients. A brief training included resources for post-test engagement.
Results:
Forty-four percent of the kits were reported as distributed. Of 81 MP clients offered kits, 50 (62%) accepted. In a follow-up survey, 77% of MP clients distributed at least one kit. 56 (86%) social network (SN) members were Latino and 9 (14%) were Black. Three out of four MP clients engaged in PrEP discussions (77%) with SN members. Reported reasons for HIVST kit use included convenience, confidentiality, privacy concerns, and discomfort with going to a testing site. MP clients reported that kit distribution was impacted by the COVID-19 pandemic.
Conclusion:
HIV ST kits allowed PrEP users to engage others in their social and sexual networks for HIV testing and information regarding PrEP. Work to scale-up this intervention is underway.
Keywords: HIV testing, HIV self-test kit, implementation science, social network, PrEP, men who have sex with men, peer educators, HIV prevention
Introduction
HIV testing is a pillar of the Ending the HIV Epidemic (EHE) initiative and is critical for treatment and prevention engagement [1]. The Centers for Disease Control and Prevention (CDC) estimate that there are currently 1.2 million people living with HIV in the United States (US) and approximately 161,800 do not know their HIV status [2]. Gay, bisexual, and other men who have sex with men (MSM) are the populations most affected by HIV in the US, with Black and Latino MSM accounting for approximately 69% of new HIV diagnoses [3]. Young MSM of color and immigrants, particularly those who are undocumented, are less likely to be tested and become aware of their HIV status [3, 4]. Miami-Dade County (Miami) has one of the highest rates of newly diagnosed HIV infections in the US—four times the national average [5]. Preexposure prophylaxis (PrEP), an antiretroviral medication used to prevent the acquisition of HIV, can reduce HIV transmission by up to 99% among MSM when taken as directed [6–8]. However, the rate of PrEP use, relative to need, remains low in Miami-Dade County, in the US South generally, and among populations highly impacted by HIV including Black and Latino MSM [9–11].
Although the CDC recommends HIV testing at least annually for sexually active MSM [12], barriers to HIV testing include stigma, privacy, comfort, affordability, transportation, confidentiality, cost, and medical mistrust [12–14]. Peer education and HIV self-test (HIVST) kits can overcome barriers to testing to reach individuals who would otherwise not get tested [5]. HIVST kits can increase testing frequency, decrease time to HIV diagnosis, and are highly acceptable to most potential users [15–18]. In most models, however, HIVST kits must be requested by the individual desiring testing from a provider, website, or mobile health application, and many individuals in priority populations for HIV prevention may not have ready access to these tools [19]. Secondary distribution, in which HIVST kits are provided to social network (SN) contacts, has the potential to reach additional people who may have barriers to traditional testing engagement [18–20]. SN members are likely to have similar HIV risk profiles, and network interventions to increase HIV testing have been successful in identifying individuals with previously undiagnosed HIV infection [21, 22]. Distribution of HIVST kits to friends and sexual partners was found to be theoretically acceptable to US MSM, with 78% expressing willingness to distribute HIVST kits, including 73% willing to distribute to sexual partners and 72% to friends [20]. HIVST kit distribution by US MSM to potential sexual partners (with the suggestion that the HIVST kit be used prior to sex) has also been evaluated, with high acceptability and few adverse events [23, 24]. Peer recruiters have effectively distributed HIVST kits to Latino and Black MSM in the US, with recruiters also indicating that the HIVST kit distribution process was a positive experience [16]. In a large randomized controlled trial of HIVST kit distribution to US MSM, more new HIV diagnoses were identified through secondary use by SN members than among the direct study participants [18].
Peer navigation and the use of peers to increase knowledge and use of PrEP has been suggested as an implementation strategy to increase PrEP use [25]. Peer navigation was found to be acceptable to minority MSM, particularly when peers were matched on characteristics such as sexual orientation, race, age, and culture [26]. Peer navigation and SN interventions increased HIV testing among Spanish-speaking MSM and transgender women in a randomized controlled trial and could be adapted for PrEP information dissemination [27]. Among Latina farmworkers in South Florida, a SN intervention was successful in increasing HIV knowledge and testing as well as condom use and is being adapted for PrEP use and HIV testing among Latino MSM [28]. Previous studies have found that hearing about PrEP from a friend or sex partner often leads to a self-referral for PrEP [29–31]. This suggests that SN-based interventions could improve willingness to initiate PrEP and promote HIV testing among MSM.
To achieve the EHE goals for HIV testing and PrEP scale-out, innovative interventions that are effective in geographic hotspots such as Miami and the US South, and among key populations disproportionately impacted by HIV, such as Black and Latino MSM, are needed [1, 25]. The University of Miami Mobile PrEP Program delivers full PrEP services including all laboratory testing, same-day prescription, sexually transmitted infection (STI) testing and treatment, and post-visit navigation through a fully equipped clinic vehicle to six highly impacted areas of Miami-Dade County including five neighborhood sites and a syringe exchange program. While the demographics of Mobile PrEP (MP) clients vary by neighborhood most MP clients are immigrant Latino MSM. In this study, we engaged current MP clients to distribute HIVST kits through their SN. MP clients were recruited to act as peer educators to use the knowledge and education that they have accrued about HIV testing and PrEP to engage their peers in conversations about sexual health and expand the reach of HIV testing through their SN. Our intervention is based on Social Contagion Theory [32], which emphasizes that preferences regarding HIV-related behaviors are potentially affected by the opinions and attitudes that prevail in an individual’s social environment [33]. Social Contagion Theory has been previously used to study contextual factors and race differences in adolescent sexual behaviors [34], and treatment-as-prevention strategies [35]. As current PrEP users have personal experience with HIV prevention engagement, we explore whether MP clients may be ideal distributors of HIVST kits and information regarding PrEP to their SN. This pilot study sought to identify specific implementation factors associated with implementing this intervention. In this manuscript, we describe the determinants, approach, and initial outcomes associated with this novel intervention for HIVST kit distribution using the Implementation Research Logic Model (IRLM)[36]. The goal of this pilot study is to understand the acceptability and feasibility of expanding the reach of HIV testing and PrEP information through MP clients’ SN through scale-up of this HIVST kit distribution intervention.
Methods
Setting
The University of Miami Mobile PrEP Program offers low barrier access to PrEP, sexually transmitted infection (STI) testing and treatment, and HIV prevention services through a mobile clinic vehicle in six highly impacted areas of Miami-Dade County including five neighborhood sites and a syringe exchange program (Figure 1). Mobile PrEP services were offered weekly or biweekly at each location on a rotating basis. HIVST kit distribution occurred from December 2019 to February 2020.
Figure 1.
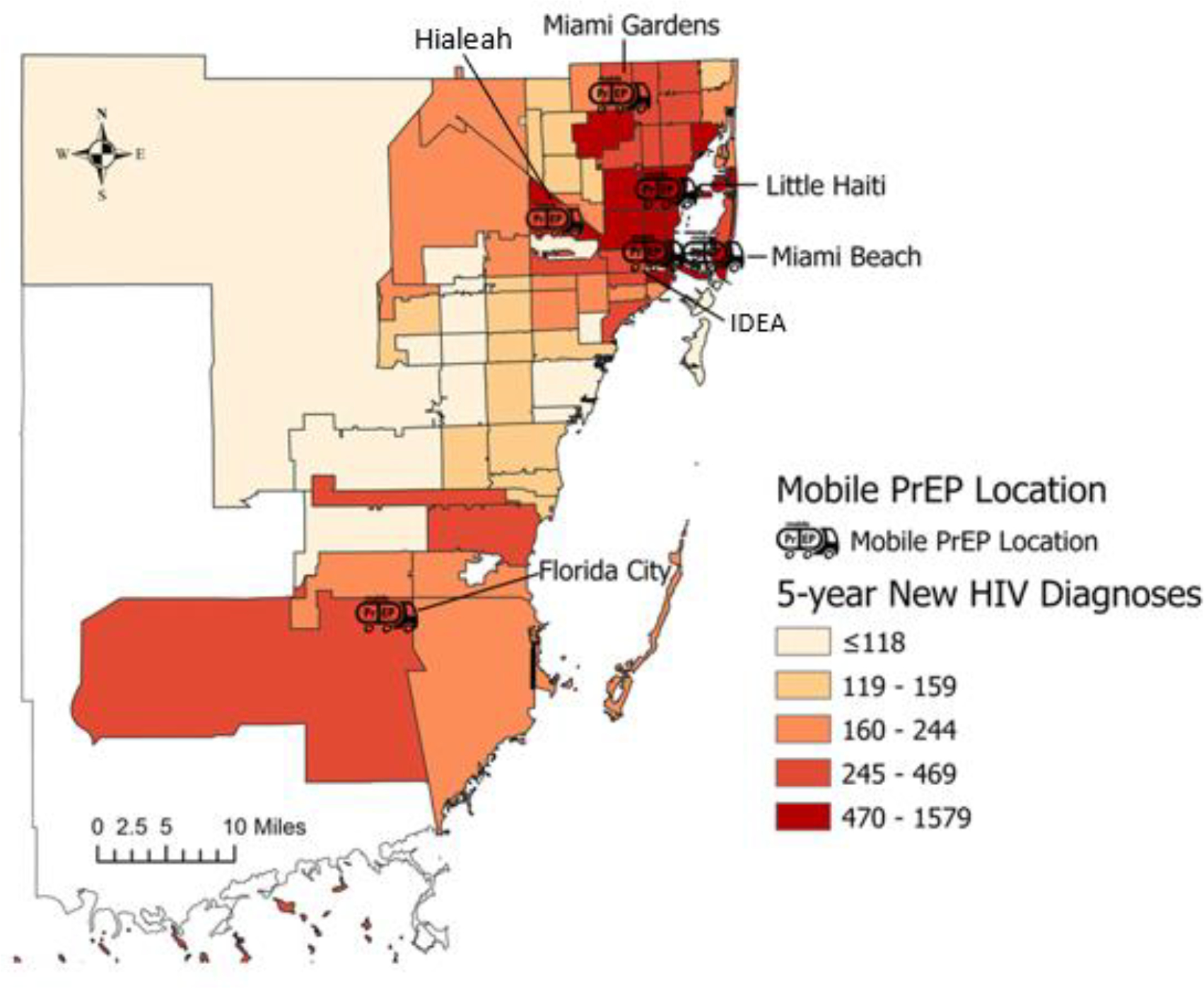
Sites for Mobile PrEP services and HIVST kit distribution. Color represents rates of persons living with HIV, 2018, for each zip code, base map from www.aidsvu.org.
Description of Intervention
During scheduled PrEP quarterly follow-up clinic visits, MP clients were offered up to four OraQuick In-Home (OraSure Technologies, Inc, Bethlehem, PA) oral fluid HIVST kits, free of cost, for distribution to their social and sexual network members. In addition to the information available in the testing kit, brief training regarding the test and resources for post-test engagement were provided. Training included a review of the window period for the HIVST kit and a recommendation that MP clients continue with other testing formats rather than using the HIVST kit, other than in the context of co-testing with a SN member as a form of support. Additionally, MP clients were encouraged to share information about PrEP, including brochures with contact information for accessing PrEP, and to share their own experiences with PrEP, if appropriate. Offer of kit and training was performed by the MP staff, at the end of the PrEP visit. MP clients were asked to distribute the kits to those SN members that they felt could benefit from testing, without further direction regarding recipients.
Theoretical Framework and Implementation Research Logic Model
An implementation research logic model (IRLM; Figure 2) was developed (https://www.lucidchart.com) to make explicit the determinants, approach, and outcome measures assessed in this intervention [37]. Hypothesized determinants, facilitators of, and barriers to engagement in social and sexual network-based HIVST kit distribution, were elicited by an investigator and MP staff discussion and positioned within the five Consolidated Framework for Implementation Research (CFIR) domains (intervention characteristics, outer setting, inner setting, and characteristics of individuals) [38]. Implementation strategies were coded according to the taxonomy described in the Expert Recommendations for Implementing Change (ERIC) project[39]. Outcomes to be measured in this pilot project, and those planned for future assessments (grey box in IRLM; Figure 2), were categorized using the RE-AIM framework [40].
Figure 2.
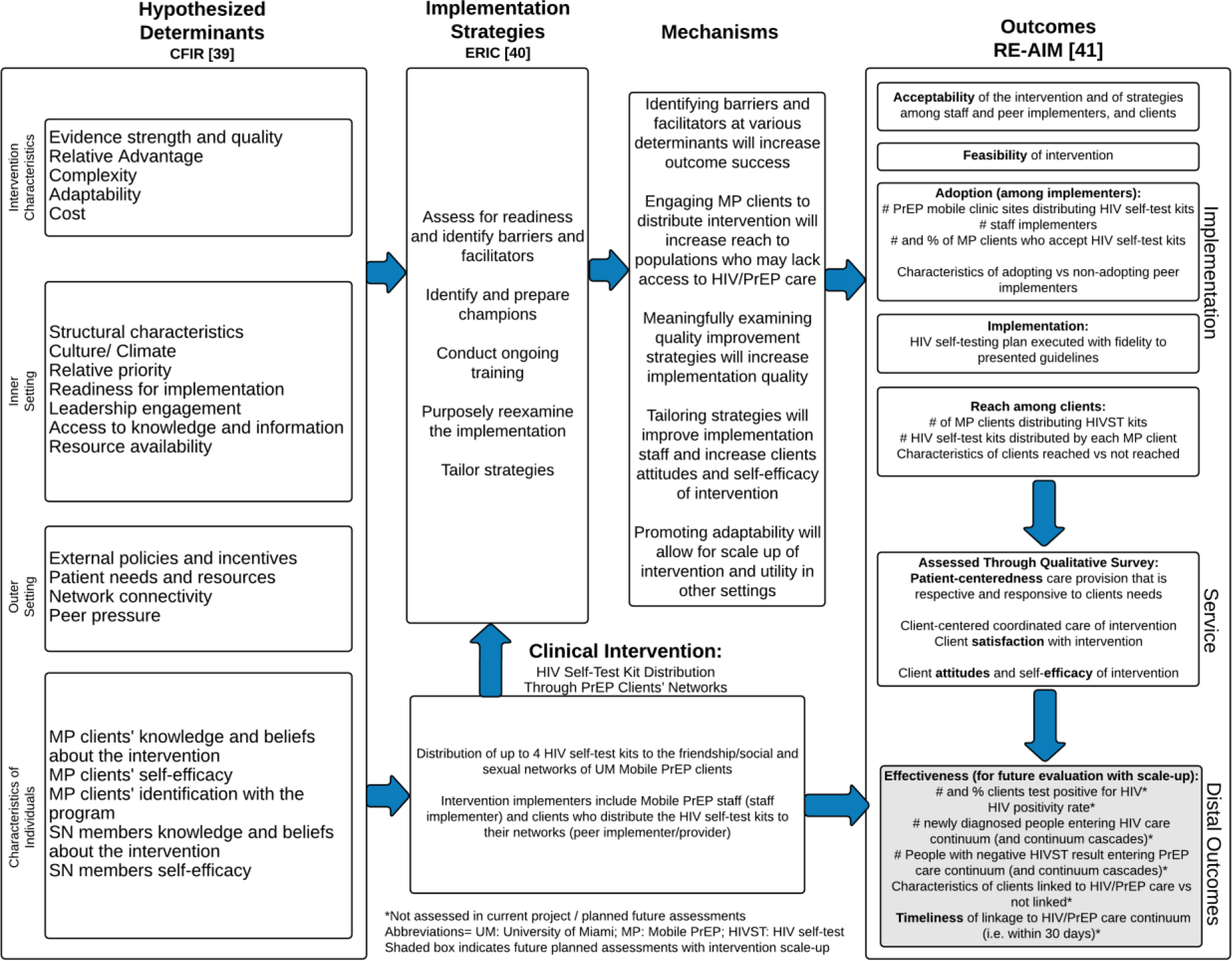
Implementation Research Logic Model
Assessments
As described by Palinkas, et al., mixed-methods assessments were employed in this study to measure pilot intervention outcomes while simultaneously understanding the process from the perspectives of both MP staff and MP client implementers [41]. The number of MP clients who were approached and did not wish to participate in HIVST kit distribution was recorded. For each MP client accepting HIVST kits for distribution, the number of kits accepted was recorded. A survey at the time of provision of HIVST evaluated MP client’s distribution plan, comfort level, and concerns in offering the test kits to friends/sexual partners. A post-survey consisting of quantitative and brief open-ended questions evaluated MP client’s post-distribution experience, SN member demographics, test results, PrEP use, comfort level, concerns in offering the kits, and suggestions for future implementation. All survey responses were anonymous, and no identifiers were collected.
Following completion of the project, a brief web-based survey was distributed to the MP staff involved in the intervention (Qualtrics, Provo, UT) to assess perceived implementation determinants. Survey items were selected from the CFIR web interview guide tool (www.cfirguide.org) to reflect hypothesized determinants as presented in the IRLM [45]. Each statement requested a 5-point scale response (strongly disagree to strongly agree) except for a single item assessing MP staff’s impression of the stage of change/ readiness of PrEP clients to adopt the HIVST distribution intervention (precontemplation, contemplation, preparation, action, or maintenance) using the transtheoretical model [46]. An opportunity for a brief open-ended response was also provided for each category. A 30-minute group discussion also provided an opportunity for MP staff input and reflection on the intervention.
Analysis
Descriptive statistics included frequencies for categorical variables, and means, and ranges for continuous variables. Network visualizations were developed using Cytoscape [42] and Inkscape [43] software. Qualitative brief responses from MP client and MP staff surveys along with staff group discussion were coded according to best match with the CFIR taxonomy [44]. Constructs within each category were scored according to strength and valence of the determinant from −2 to +2 as previously described by Damschroder and Lowery, [47] based on a combination of the quantitative responses from MP staff surveys and qualitative short answer responses from MP clients and staff assessments as coded by two investigators (KK and SDL); differences in coding were discussed, and consensus reached.
Human Subjects Considerations
This study was categorized by non-human-subjects research by the University of Miami Institutional Review Board.
Results
MP Client HIVST Distribution
HIVST kits were offered to 81 MP clients from December 2019- February 2020. A total of 148 OraQuick HIVST kits were distributed to 50 MP clients (61.7% uptake) at six Mobile PrEP service locations across Miami-Dade (Figure 1). The social network visualization (Figure 3) demonstrates the distribution of kits from each site. The median number of kits accepted by participating MP clients was three (range 1–4). Table 1 describes the demographic characteristics of the 35 of 50 MP clients who were provided kits and responded to the post-distribution survey; 94.3% were male, 77.1% identified as Hispanic/Latino, and 68.6% were MSM.
Figure 3.
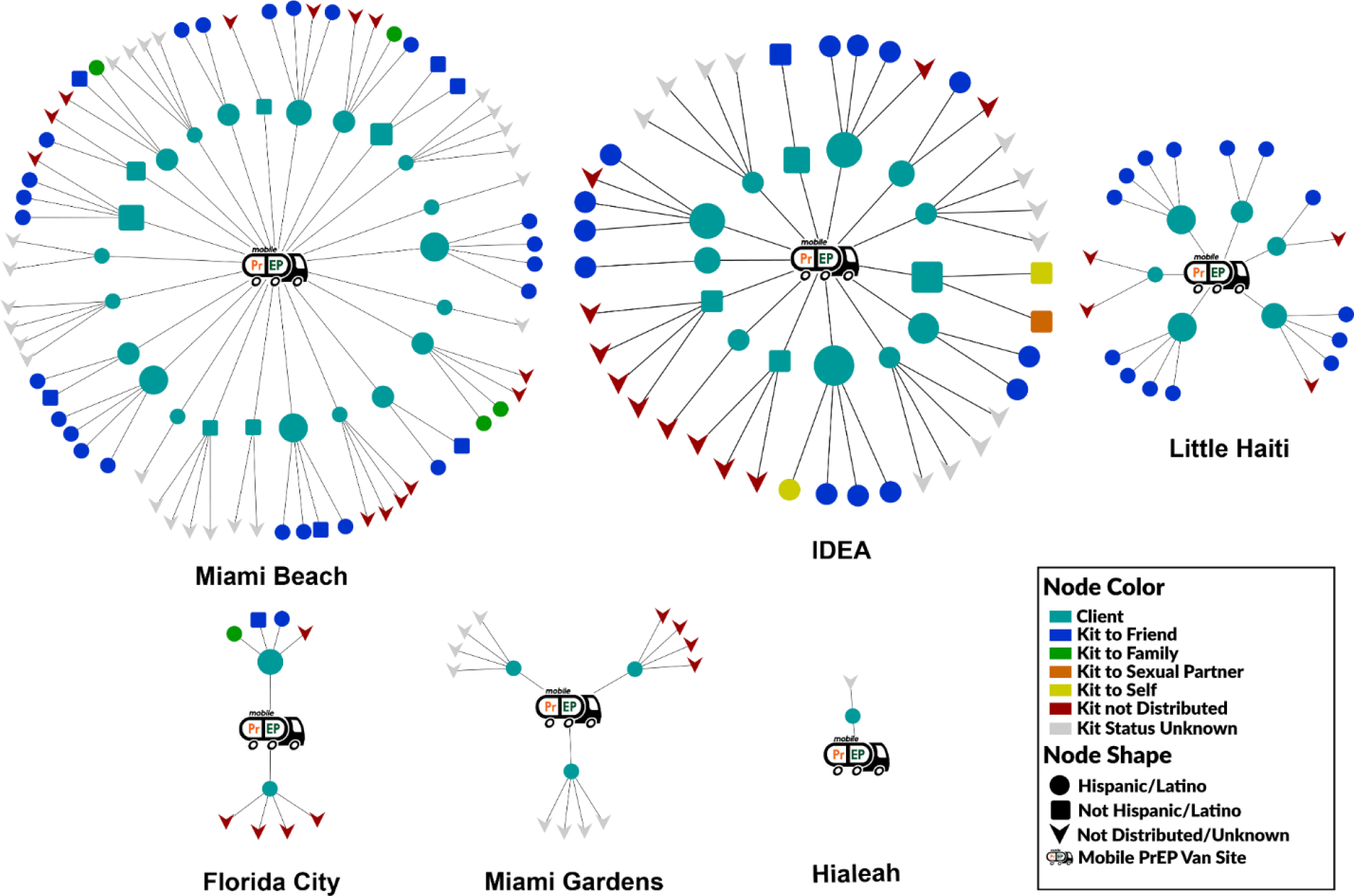
Post-Survey Social Network Visualization with Potential Reach of Self-testing Kits in Six Miami-Dade Communities Served by the Mobile PrEP Program
Table 1.
Post Survey Demographics of Mobile PrEP Clients and SN Members
| Demographics | MP Clients (N = 35) | SN Members (N = 65) |
|---|---|---|
|
|
|
|
| n (%) | n (%) | |
|
| ||
| Age | ||
| 24 and under | 1 (2.86%) | 3 (5%) |
| 25–34 | 17 (48.57%) | 29 (44%) |
| 35 and above | 17 (48.57%) | 30 (46%) |
| Preferred not to answer | 0 (0%) | 3 (5%) |
| Gender | ||
| Male | 33 (94.29%) | 57 (88%) |
| Female | 2 (5.71%) | 8 (12%) |
| Ethnicity | ||
| Non-Hispanic | 8 (22.86%) | 9 (14%) |
| Latino/Hispanic | 27 (77.14%) | 56 (86%) |
| Race | ||
| White | 28 (80%) | 55 (85%) |
| Black/African American | 5 (14.29%) | 9 (14%) |
| Asian | 0 (0%) | 1 (1%) |
| Other | 2 (5.71%) | 0 (0%) |
| Sexual Behavior * | ||
| MSM | 24 (68.57%) | - |
| MSM&W | 8 (22.86%) | - |
| MSW | 1 (2.86%) | - |
| WSM | 2 (5.71%) | - |
Data not collected for SN members.
men who have sex with men (MSM), men who have had sex with men and women (MSM&W), men who have sex with women (MSW), women who have sex with men (WSM)
MP Client Pre-Distribution Survey
All MP clients receiving HIVST kits for distribution completed a brief survey. After receiving instruction on the HIVST kit, 37 (74%) MP clients indicated that they thought the HIVST kit would be very easy to use and 42 (87.5%) reported that they were completely comfortable offering the HIVST kits to an SN member. No MP clients indicated any concerns about offering the HIVST kits to an SN member; 81% indicated that they had a SN member in mind for HIVST kit distribution.
MP Client Post-Distribution Survey
MP client in-person follow-up was significantly impacted by the COVID-19 pandemic beginning in March 2020. Due to COVID-19 distancing mandates, MP clients were contacted by telephone for follow-up, and information regarding the HIVST kit distribution was solicited during this interaction. Many MP clients indicated that their usual social network contacts were substantially decreased due to COVID-19-related shutdowns and shelter-in-place orders. Of the 50 MP clients who accepted HIVST kits for distribution, 35 were reached for follow-up and completed the post-distribution survey. Of those surveyed, 27 MP clients (77.1% of those reached for follow-up) distributed at least one kit to a SN member, and the median number reported as distributed was 2 (range 1–4). Of the 148 HIVST kits initially accepted by MP clients for distribution, 65 (44%) HIVST kits were known to be distributed to an SN member, 2 (1%) were used by the MP client to support the SN member, 41 (27.7%) HIVST kits were not distributed, and 40 (27%) kits were unaccounted for due to inability to contact the MP client for follow-up. Figure 3 depicts a social network visualization of the post-distribution survey data that highlights the potential reach of the HIVST kits among SN members.
Primary reasons for not distributing the HIVST kits included: not encountering anyone who would benefit from the HIVST kit (63.2%), losing the HIVST kit (10.5%), HIVST kit expiring before use (15.8%), and SN member refusing the HIVST kit (10.5%). Of the 67 HIVST kits distributed, 59 (88%) were distributed to friends of the MP clients, 5 (8%) were distributed to family members, 1 (1%) was distributed to a sexual partner, and 2 (3%) kits were used for self-testing alongside a SN member to provide moral support. Gender, perceived race/ethnicity, and perceived age of the SN member receiving the kits as reported by the MP clients who responded to the post-distribution survey is presented in Table 1. Most SN members (88%) were perceived to identify as cisgender men and 86% as Latino. 38 (58%) MP clients reported convenience as the main perceived reason that an SN member used a HIVST kit. Additionally, five MP clients (7%) reported that their SN member did not have an alternate venue for testing, 5 (7%) reported wanting to receive the test result privately, 3 (4%) indicated insurance concerns, 2 (3%) reported discomfort with accessing a traditional testing site, 2 (3%) had confidentiality concerns, 2 (3%) wanted to test with a partner, and 10 (15%) did not report a specific reason that the HIVST kit was used.
Of the 65 SN members who reported using an HIVST kit, 48 (74%) received a non-reactive result confirmed by a MP client. 17 (26%) MP clients were unaware of their SN members’ results. One SN member received a false positive HIVST result due to an expired kit, which was then followed by a negative confirmatory test (4th generation HIV Antigen/Antibody laboratory confirmatory test, as well as negative HIV nucleic acid amplification test). This SN member, after receiving the confirmed non-reactive result, began PrEP.
MP clients indicated that they discussed PrEP with 50 (77%) SN members who received HIVST kits. MP clients were instructed at the time of kit distribution to use the knowledge and education that they have accrued about HIV testing and PrEP to engage their peers and expand the reach of HIV testing and PrEP information. Detailed information from MP clients regarding the nature of the PrEP discussion following HIVST was not elicited as part of this study. After distributing the HIVST kits, 83% of MP clients reported that they felt completely comfortable (5 on a 5-point scale) with the process and expressed no concerns about offering the test. No MP clients indicated that they felt uncomfortable (3 or less on a 5-point scale). Interest in receiving additional HIVST kits for future distribution was expressed by 70.6% of MP clients responding to the follow-up survey.
Brief qualitative feedback from MP clients (Table 2) indicated that the intervention fit with community needs and priorities, and two clients expressed that they felt empowered to promote testing and HIV prevention within their networks. Three MP clients indicated that they would like additional materials regarding PrEP and post-exposure prophylaxis (PEP) as part of the distribution package. One client requested materials adapted for cisgender women and men who have sex with women as the materials provided were perceived to be focused on MSM. Four clients indicated that their distribution plans were altered due to COVID-19 restrictions. Three MP clients expressed frustration that the kits expired before they could be distributed.
Table 2.
Themes and illustrative quotes mapped to CFIR domains and constructs
| CFIR Domains | CFIR Constructs | Themes | Illustrative Quotes |
|---|---|---|---|
| Intervention Characteristics | Complexity: −2 | The complexity of intervention may lead to initial resistance to participation. Intervention logistics require streamlining. | “…Many patients thought it was too complex and complicated and did not accept it. Also, the logistics for tracking and keeping up with the box seemed to be complicated for the navigators as well. It could help if only one navigator oversaw the intervention….” MP Study Staff |
| Indirect response reporting may be a drawback to data collection and accuracy | “…disadvantage with this intervention …is that it relies on indirect information (the person who received the kit) to give information on the person that they gave the kit to.” MP Study Staff | ||
| Logistics regarding expiration and distribution timeframe need to be reassessed | “Don’t like that the kits expired… better if the kits were given out with more time. … would be happy to get more kits… have a lot of friends that would be interested!” MP Client | ||
| Evidence Strength and Quality: +1 | Positive perceptions of existing evidence supporting the need for intervention | “…a crucial part to the end of the HIV epidemic.” MP Study Staff | |
| Positive perceptions of the intervention’s efficacy and potential reach | “The intervention is effective …ability to have a large-scale reach within participants social networks.” MP Study Staff | ||
| Positive perceptions of interventions ability to provide awareness and education | “…helps to reduce stigma around testing.” MP Client | ||
| Adaptability: +2 | Initial positive perceptions of the intervention with room for future adaptations | “…great concept theoretically and in-person. … many variables that can be modified and adapted to actual needs.” MP Study Staff | |
| Future adaptations needed to address difficulties due to COVID-19 | “Consider delivery of the test kits because of COVID-19 to make it more convenient.” MP Client | ||
| Inner Setting | Relative Priority: +1 | Positive perceptions of the implementation environment and community buy-in | “I think it is the perfect environment to implement an intervention like this one. The community surrounding is very supportive, and I believe it was very well received.” MP Study Staff |
| Positive perceptions of the intervention within the community | “The community truly cares deeply…, so it aims to benefit our communities in Miami.” MP Study Staff | ||
| Culture: +2 | Community and MP clients appear well equipped to implement the intervention and have an adequate support network | “The system and the community surrounding are strong and cohesive as a network to implement the intervention. Mobile PrEP clients are knowledgeable about PrEP and testing and work as a strong peer support network.” MP Study Staff | |
| Outer Setting | Patient Needs and Resources: +2 | Tailored education needed for priority communities | “…people need more education on PrEP & HIV/STI, and more heterosexual people need education on HIV/STI and to think PrEP is an option.” MP Client |
| Expansion into different methods to deliver education surrounding topics described in the intervention is needed | “Promote it more, how-to videos or more instructions.” MP Client | ||
| Further promotion on effective prevention strategies and community resources will be extended | “…advertise more about PrEP and program services. Provide more education on HIV & PrEP.” MP Client | ||
| External Policies and Incentives: −1 | Negative impact on distribution due to COVID-19 | “COVID-19 impacted distribution would like to receive more kits…” MP Client | |
| Characteristics of Individuals | Individual Identification with the Program: +1 | MP clients appear supportive of intervention and organizational values | “Those (Mobile PrEP clients) that are distributing the kits are very committed and dedicated to our organization, values, and mission.” MP Study Staff |
| Self-Efficacy: +1 | MP clients appear knowledgeable and prepared to further the implementation of the intervention within the community | “The Mobile PrEP clients who are distributing test kits to their social network are well equipped and knowledgeable about HIV testing and self-test kits. They are aware of the importance of testing and PrEP and are interested in acting as peer educators for the intervention.” MP Study Staff | |
| Knowledge and Beliefs about the Intervention: +1 | MP clients appear willing to extend the intervention to SN members and identify populations in need of additional education | “…excited for the opportunity to help my friends because they had never been tested before. …more education for people that are not in the LGBTQI+ community about PrEP and HIV testing.” MP Client |
Mobile PrEP clients (MP clients), Social Network Member (SN member)
MP Staff Survey
Mobile PrEP staff directly responsible for HIVST kit instruction and distribution (n= 13) completed a brief assessment of implementation determinants for HIVST use and PrEP engagement. On a 5-point Likert scale, all assessed items had a mean response of greater than 3 (indicating a positive rating for the determinant), with the highest-ranking determinants being agreement that the intervention was a good match for the structural characteristics of the organization (i.e., the Mobile PrEP program) (mean= 4.7), implementation climate (mean= 4.7), and communication of goals and feedback with MP clients (mean= 4.6). The lowest ranking items were cost of the intervention (mean= 2.5), complexity of the intervention (mean= 2.5), and external policy and incentives (mean= 2.5). Short narrative responses and discussions provided additional support for the following facilitators: implementation climate, network complexity, communication of goals and feedback with MP clients. The following barriers were also identified: cost, complexity of intervention as well as logistics of tracking HIVST kits (mapped to “resource availability). MP staff’s impression of the stage of change/ readiness of MP clients to adopt the HIVST distribution intervention using the transtheoretical model indicated that MP clients are in the stage of “Action,” (Clients had begun to distribute HIV self-testing kits). A summary of the most relevant CFIR domains and constructs that emerged through the triangulation of themes from qualitative data, as well as from MP staff survey responses, are presented in Table 2 with illustrative quotes from MP staff and MP clients.
Discussion
To achieve EHE plan outcomes [1] there is an urgent need to develop and test innovative implementation interventions for equitable scale-up of HIV testing and PrEP engagement, particularly among populations underrepresented in testing and PrEP care. In this study, we assessed the implementation factors associated with the novel intervention of engaging current clients with personal PrEP experience to distribute HIVST kits through their social and sexual networks, with the goal of increasing the reach of HIV testing and PrEP information. Using an IRLM, and consistent with Proctor’s recommendations for reporting, we made explicit the steps involved in the development and preliminary assessment of this intervention.
Uptake of HIVST kit distribution among MP clients was moderate, and the distribution process and subsequent reporting were significantly disrupted by alterations to in-clinic follow-up and social network interactions due to the onset of the COVID-19 pandemic immediately after the completion of the kit distribution to MP clients. Nevertheless, among those MP clients participating in kit distribution, most expressed comfort and satisfaction with the process as well as enthusiasm for the intervention. An encouraging key finding was that the majority of those distributing HIVST kits reported having a conversation regarding PrEP with their SN member.
Our findings regarding the acceptability and safety of HIVST kit distribution are consistent with those of previous studies involving the secondary distribution of kits [15, 18, 24]. As has been suggested previously, HIVST kits are an important opportunity for engagement not only for the detection of new HIV infections but also for the introduction of prevention strategies including PrEP [44]. Additionally, we found that the HIVST kit distribution intervention initiated through a Mobile PrEP clinic was consistent with the culture and climate of the organization and perceived to be a high-priority intervention as reported by MP staff. The Mobile PrEP program is focused on the extension of care into communities that have barriers to access to services and therefore may have a climate more favorable to interventions focused on further extension of that reach. PrEP programs based on more traditional clinical settings may have different levels of enthusiasm and perception of priority for interventions such as this. The intervention was perceived to be relatively complex, with need for logistical, communication and packaging strategies to streamline its execution. The preparatory intervention for MP clients requires approximately 20 minutes of staff counseling time and tracking of HIVST kit outcomes and ensuring linkage to HIV or PrEP care was noted to be complex by some staff. Further improvements in the process of education, distribution, and tracking of HIVST kits may be useful to facilitate implementation in busy clinical settings. While there was no cost to the clients for the kits in this study, the HIVST kit available in the US has a retail cost of approximately $40, and these costs must be considered in plans for scale-up. While maintenance of the intervention was not assessed due to the planned short timeframe for the pilot study, the MP staff and MP client responses provide information that would be relevant to maintenance and sustainment of a future HIVST distribution intervention within organizations with similar context.
We found that distribution of home-based HIVST kits through current MP clients’ social networks had many perceived advantages among MP staff, with strong organizational support and belief in the strength of MP client’s social networks as a relative advantage to the intervention. Since most of the MP clients and SN members reached were Latino MSM, preferences for PrEP peer educators with similar/matching demographics observed in other studies [26] may have contributed to this perception.
Limitations of our pilot study include a small sample size and the significant impact of COVID-19 on HIVST kit distribution and follow-up. Despite these limitations, nearly half of the distributed kits were reported on follow-up as having been used. These results may represent an underestimate of the efficiency and feasibility of this approach due to these substantial unanticipated disruptions. Scale-up of this intervention under more stable circumstances may yield more promising results.
Additionally, all HIVST kit use data recorded as reported/perceived by MP clients is unconfirmed. There is a possibility that responses were impacted by social desirability bias as surveys were administered by clinic staff with a pre-existing counseling/navigation relationship with MP clients. The occurrence of PrEP conversations was assessed through the question: “If the test was negative, did you speak with the person being tested about PrEP?”; future evaluations will include more specific inquiries regarding the content and outcomes of these conversations and will include the perspective of the individual receiving the test kit. In our setting, most MP clients and SN members were Latino MSM. Our experience may not be generalizable to other populations with differences in SN strength or less concordance in sociodemographic factors. Other limitations include not collecting data on the sexual behaviors of SN members.
To our knowledge, this is the first description of an intervention to activate current PrEP clients as distributors of HIVST kits and initiators of PrEP conversations in their social networks. Our assessment, although limited by unanticipated COVID-19-related disruptions, supports the feasibility within our organization and the favorable response of MP clients to this approach. Future adaptations of the intervention will address complexity through process streamlining. Many MP clients reported participating in PrEP conversations as part of the HIVST process; an ongoing follow-up study includes more detailed assessments of this finding, as well as distal measures of PrEP engagement including impact on reach and adoption of PrEP and effectiveness in HIV prevention service engagement and maintenance.
Evidence-based innovation: HIV self-test kit (HIVST) distribution
Innovation recipients: People at risk for HIV
Setting: Mobile clinic vehicle in six highly impacted areas of Miami-Dade County, Florida
Implementation gap: Secondary distribution, in which HIVST kits are provided to social network contacts by those already engaged in PrEP care, has the potential to reach additional people who may have barriers to traditional testing engagement, but the feasibility is not established
Primary research goal: Identify determinants for future intervention implementation
Implementation strategies: Identification and preparation of champions, tailoring of intervention to unique strengths of current clients.
Acknowledgments
Sources of Support:
Miami Center for AIDS Research funded by a grant (P30A1073961) from the National Institutes of Health to the University of Miami (Ending the HIV Epidemic Administrative Supplement to SDL)
References
- 1.Fauci AS, et al. , Ending the HIV Epidemic: A Plan for the United States. JAMA, 2019. 321(9): p. 844–845. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. HIV Testing. 2020 May 2021]; Available from: https://www.cdc.gov/hiv/testing/index.html. [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV and Gay and Bisexual Men. 2020 May 2021]; Available from: https://www.cdc.gov/hiv/group/msm/. [Google Scholar]
- 4.Lee JJ and Yu G, HIV Testing, Risk Behaviors, and Fear: A Comparison of Documented and Undocumented Latino Immigrants. AIDS Behav, 2019. 23(2): p. 336–346. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention, Diagnoses of HIV infection among adults and adolescents in metropolitan statistical areas—United States and Puerto Rico, 2017 HIV Surveillance Supplemental Report 2019, 2019. 24. [Google Scholar]
- 6.Grant RM, et al. , Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med, 2010. 363(27): p. 2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson PL, et al. , Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med, 2012. 4(151): p. 151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCormack S, et al. , Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet, 2016. 387(10013): p. 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegler AJ, et al. , The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol, 2018. 28(12): p. 841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith DKVH, Grey J.A. M, By Race/Ethnicity, Blacks Have Highest Number Needing PrEP in the United States, 2015, in Conference on Retroviruses and Opportunistic Infections. 2018: Boston, Massachusetts. USA. [Google Scholar]
- 11.Centers for Disease Control and Prevention. HIV in the Southern United States. CDC Issue Brief; 2015; December, 2015:[Available from: http://www.cdc.gov/hiv/pdf/policies/cdc-hiv-in-the-south-issue-brief.pdf. [Google Scholar]
- 12.Centers for Disease Control and Prevention, HIV Screening in Clincial Settings. 2019.
- 13.Brooks RA, et al. , Preventing HIV among Latino and African American gay and bisexual men in a context of HIV-related stigma, discrimination, and homophobia: perspectives of providers. AIDS Patient Care STDS, 2005. 19(11): p. 737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Threats M, et al. , Deterrents and motivators of HIV testing among young Black men who have sex with men in North Carolina. AIDS Care, 2020: p. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson CC, et al. , Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc, 2017. 20(1): p. 21594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lightfoot MA, et al. , Using a Social Network Strategy to Distribute HIV Self-Test Kits to African American and Latino MSM. J Acquir Immune Defic Syndr, 2018. 79(1): p. 38–45. [DOI] [PubMed] [Google Scholar]
- 17.Katz DA, et al. , HIV Self-Testing Increases HIV Testing Frequency in High-Risk Men Who Have Sex With Men: A Randomized Controlled Trial. J Acquir Immune Defic Syndr, 2018. 78(5): p. 505–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacGowan RJ, et al. , Effect of Internet-Distributed HIV Self-tests on HIV Diagnosis and Behavioral Outcomes in Men Who Have Sex With Men: A Randomized Clinical Trial. JAMA Intern Med, 2020. 180(1): p. 117–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steehler K and Siegler AJ, Bringing HIV Self-Testing to Scale in the United States: a Review of Challenges, Potential Solutions, and Future Opportunities. J Clin Microbiol, 2019. 57(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma A, et al. , Willingness to distribute free rapid home HIV test kits and to test with social or sexual network associates among men who have sex with men in the United States. AIDS Care, 2017. 29(12): p. 1499–1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kimbrough LW, et al. , Accessing social networks with high rates of undiagnosed HIV infection: The social networks demonstration project. Am J Public Health, 2009. 99(6): p. 1093–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amirkhanian YA, Social networks, sexual networks and HIV risk in men who have sex with men. Curr HIV/AIDS Rep, 2014. 11(1): p. 81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carballo-Dieguez A, et al. , Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav, 2012. 16(7): p. 1753–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Witzel TC, et al. , Comparing the effects of HIV self-testing to standard HIV testing for key populations: a systematic review and meta-analysis. BMC Med, 2020. 18(1): p. 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sullivan PS, et al. , Implementation Strategies to Increase PrEP Uptake in the South. Curr HIV/AIDS Rep, 2019. 16(4): p. 259–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pagkas-Bather J, et al. , What’s PrEP?: peer navigator acceptability among minority MSM in Washington. BMC Public Health, 2020. 20(1): p. 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes SD, et al. , A peer navigation intervention to prevent HIV among mixed immigrant status Latinx GBMSM and transgender women in the United States: outcomes, perspectives and implications for PrEP uptake. Health Educ Res, 2020. 35(3): p. 165–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanamori M, et al. , Progreso en Salud: Findings from Two Adapted Social Network HIV Risk Reduction Interventions for Latina Seasonal Workers. Int J Environ Res Public Health, 2019. 16(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fuchs J, Lessons learned from the US PrEP Demonstration Project: Moving from the “real world” to the “real, real world.”. 2015: San Francisco, CA. [Google Scholar]
- 30.Ezennia O, Geter A, and Smith DK, The PrEP Care Continuum and Black Men Who Have Sex with Men: A Scoping Review of Published Data on Awareness, Uptake, Adherence, and Retention in PrEP Care. AIDS Behav, 2019. 23(10): p. 2654–2673. [DOI] [PubMed] [Google Scholar]
- 31.Algarin AB, et al. , The Pre-exposure Prophylaxis (PrEP) Continuum of Care and Correlates to Initiation Among HIV-Negative Men Recruited at Miami Gay Pride 2018. Journal of urban health : bulletin of the New York Academy of Medicine, 2019. 96(6): p. 835–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodgers JL and Rowe DC, Social contagion and adolescent sexual behavior: A developmental EMOSA model. Psychological Review, 1993. 100(3): p. 479. [DOI] [PubMed] [Google Scholar]
- 33.Kohler H-P, Behrman JR, and Watkins SC, Social networks and HIV/AIDS risk perceptions. Demography, 2007. 44(1): p. 1–33. [DOI] [PubMed] [Google Scholar]
- 34.Eitle D and Thorsen M, School contextual factors and race differences in adolescent sexual behaviors. International Journal of Sexual Health, 2018. 30(3): p. 309–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramadanovic B, et al. , Changing risk behaviours and the HIV epidemic: a mathematical analysis in the context of treatment as prevention. PLoS One, 2013. 8(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith JD, Li DH, and Rafferty MR, The Implementation Research Logic Model: a method for planning, executing, reporting, and synthesizing implementation projects. Implement Sci, 2020. 15(1): p. 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Proctor EK, Powell BJ, and McMillen JC, Implementation strategies: recommendations for specifying and reporting. Implement Sci, 2013. 8: p. 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Damschroder LJ, et al. , Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci, 2009. 4: p. 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Powell BJ, et al. , A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci, 2015. 10: p. 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glasgow RE, et al. , RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Frontiers in Public Health, 2019. 7(64). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Palinkas LA, et al. , Mixed method designs in implementation research. Adm Policy Ment Health, 2011. 38(1): p. 44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shannon P, et al. , Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res, 2003. 13(11): p. 2498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Harrington B. Inkscape. 2005 May, 2021]; Available from: http://www.inkscape.org/. [Google Scholar]
- 44.Ortblad KF and Stekler JD, HIV self-testing: finding its way in the prevention tool box. BMC Med, 2020. 18(1): p. 373. [DOI] [PMC free article] [PubMed] [Google Scholar]


