Abstract
Background
The feasibility of remote visits following abdominal colorectal surgery has not been studied in relation to efficacy, patient satisfaction, and surgeon satisfaction. This study aims to assess reliability and satisfaction with a web-based questionnaire for post-operative visits following abdominal colorectal surgery.
Methods
This was a prospective single-arm cohort study at single-tertiary care center during admission for abdominal colorectal surgery. Using a web-based patient portal, patients completed a questionnaire 48 h prior to their scheduled in-person follow-up visits and submitted photographs of their incisions. Surgeons reviewed patient-entered data and responded within 24 h. Following the subsequent in-person visit, surgeons completed questionnaires to compare the accuracy of the web-based vs. in-person evaluations. Lastly, patients and surgeons completed separate satisfaction surveys after the in-person visits.
Results
A total of 33 patients were enrolled, of which 30 (90.9%) successfully completed the web questionnaire. Providers reported the online questionnaire to be concordant with the in-person visit in 90% of cases. Of the patients who completed the study, only half found the survey alone to be acceptable for follow-up. Patients spent significantly less time completing the online questionnaire (≤ 10 min) than in-person visits, including travel time (75 min, IQR 50–100). Only 12 patients (40%) uploaded photographs of their incisions. During in-person visits, management changes were employed in four patients (13.3%), of which 3 required treatment of superficial surgical site infections (10%).
Conclusion
This asynchronous web-based visit format was acceptable to colorectal surgeons but was only embraced by half of patients, despite considerable time savings. While patients preferred in-person visits, there may be opportunities to expand TeleHealth acceptance that focus on patient selection and education.
ClinicalTrials.gov: NCT05084131.
Graphical abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s00464-022-09383-8.
Keywords: Online patient portal, Telehealth, Colorectal surgery, Post-operative, Patient satisfaction, Surgeon satisfaction
Virtual health platforms are increasingly used in medicine and surgery, given recent improvements in health technology and informatics [1, 2]. Such platforms are thought to increase patient access to care and clinic efficiency, while maintaining standard of care and patient satisfaction [1, 3, 4]. It has been suggested that surgeons may be more reluctant to utilize virtual health platforms compared to non-surgical providers, due to fear of missing or misdiagnosing post-operative complications [2]. However, recent studies have highlighted benefits of remote post-operative care, including increased availability for new patient visits, reduced waiting times for operative scheduling, as well as decreased utilization of the emergency room (ER) for post-operative issues [4]. Furthermore, virtual health platforms may alleviate logistical and economic constraints patients may face with in-person visits. These include childcare, transportation, and parking costs, as well as time away from work [4]. Lastly, since the onset of the COVID pandemic, the use of remote health visits has been widely adopted by surgeons in order to continue providing care while minimizing the risk of exposure.
The use of virtual health platforms for colorectal surgery (CRS) patients and providers remains understudied. Colorectal surgery involves a broad range of disease indications (i.e., colorectal cancer, diverticulitis) which may entail complex reconstruction of the gastrointestinal tract and/or creation of stomas [5]. Furthermore, CRS patients are often considered high risk due to malignancy, immunosuppression, frailty, and malnutrition [5]. The primary aim of this study is to assess the feasibility of a web-based survey to replace in-person post-operative follow-up after elective colorectal surgery. We also aim to assess patient and provider satisfaction utilizing the web-based survey, as well as differences in patient management when comparing the two visit types.
Materials and methods
Institutional review board
This study was approved by the Institutional Review Board. All subjects provided informed consent prior to participating in study procedures.
Inclusion and exclusion criteria
Adult patients were identified prospectively at a single, tertiary care academic institution. Enrollment occurred between November 2019 and September 2020. Patients were included if they (1) were scheduled for elective abdominal colon or rectal resection, (2) had a smart mobile device or computer to access the patient portal (Epic MyChart), and (3) had the ability to take a photograph of their surgical incisions. Potential subjects were excluded if they required visiting nurse services upon discharge, had a prolonged hospital stay, were unable to use the web, were primarily non-English speaking, prisoners or pregnant. Four board-certified colorectal surgeons participated in this study. Of note, the study was halted from March to July 2020 due to the coronavirus pandemic. During this period, all elective procedures were canceled at our institution to accommodate the surge of inpatients affected by the COVID-19 virus. This led to a pause in our research activities, as this study was designed and approved for patients undergoing elective colorectal resections only.
Surveys
Enrolled subjects were scheduled for a routine in-person follow-up visit within 2 weeks of hospital discharge. They received an online questionnaire via the institutional patient portal (Epic MyChart) 48 h prior to their in-person visit. The survey inquired as to their level of post-operative pain, incision abnormalities (e.g., redness, drainage), and urinary and bowel habits (See Supplemental 1). Participants were given a brief tutorial of MyChart prior to hospital discharge and were also asked to upload a photograph of their incisions as part of the survey. An attending physician reviewed responses within 24 h of submission and responded to the patient using the same MyChart portal.
At the time of the in-person visit, patients filled out a satisfaction questionnaire tailored toward their in-clinic experience, travel time, and other logistics (See Supplemental 2). At the end of the in-clinic visit, providers completed a questionnaire to report potential changes in management from their original recommendations, as well as patient appropriateness for a survey visit alone (See Supplemental 3). Survey questions were chosen to reflect provider and patient satisfaction, as well as comparison of the two visit types, similar to other studies [3].
Study variables
Pre-operative demographic variables collected were age, gender, ethnicity, race, and past medical and surgical history. Perioperative data included type of surgical procedure, surgical approach, indication for surgery, American Society of Anesthesiologists (ASA) class, length of stay, and development of post-operative complications (up to 30 days). Continuous variables were summarized as median and interquartile range (IQR) and were compared using the Wilcoxon Rank Sum test. Categorical variables and survey responses were summarized using X2 tables. Analyses were performed in STATA v. 16.1 (Stata Corp, College Station, TX). Significance was defined as p < 0.05.
Results
Demographics
A total of 33 patients were enrolled in this study. Of the 70 patients screened, 13 (18.5%) declined and 16 (22.9%) were not enrolled due to logistical reasons (e.g., discharge from the hospital prior to being approached). Screening and other study procedures were put on hold due to the COVID-19 pandemic. Other reasons for non-enrollment are summarized in Fig. 1. Three patients were removed from the study, as they did not sign up for Epic MyChart after enrollment. Our final sample size thus consisted of 30 patients.
Fig. 1.
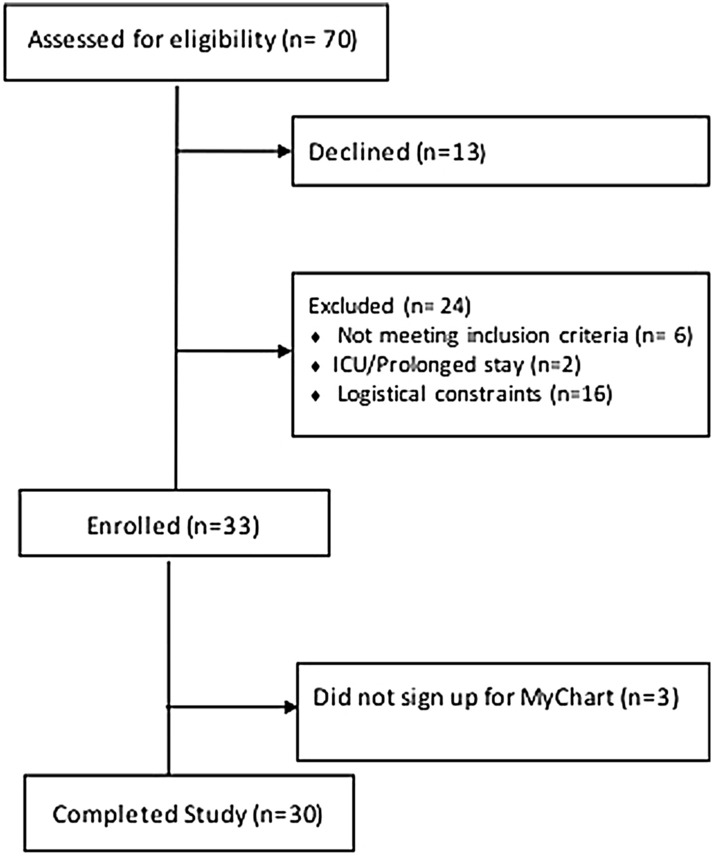
Flowchart of included patients
The majority of the sample was non-Hispanic White (n = 29, 96.7%) and female (n = 18, 60%) with a median age 61.5 years (IQR 51.6–67.2). Most underwent laparoscopic surgery (n = 23, 76.7%) with a median length of stay of 3 days (IQR 2–3). Types of resections and indications for surgery are summarized in Table 1. Four (13.3%) subjects experienced post-operative complications, which included urinary retention (n = 1) and SSI (n = 3).
Table 1.
Demographics and perioperative details
| Age, median (IQR) | 61.5 (51.6–67.2) |
| White race | 30 (100) |
| Female sex | 18 (60.0) |
| Hispanic ethnicity | 1 (3.3) |
| ASA class | |
| Class 1—no disturbance | 1 (3.3) |
| Class 2—mild to moderate disturbance | 22 (73.3) |
| Class 3—severe disturbance | 7 (23.3) |
| Surgical approach | |
| Open | 2 (6.7) |
| Laparoscopic | 23 (76.7) |
| Robotic | 5 (16.7) |
| Surgery type | |
| Sigmoid colectomy | 14 (46.7) |
| Right colectomy | 6 (20.0) |
| Left colectomy | 3 (10.0) |
| LAR | 2 (6.7) |
| Other | 5 (16.7) |
| Surgical indication | |
| Diverticulitis | 17 (56.7) |
| IBD | 4 (13.3) |
| Colon cancer | 4 (13.3) |
| Other benign | 5 (16.7) |
| Length of stay (days), median (IQR) | 3 (2–3) |
| Perioperative complications | 4 (13.3) |
All values listed are n (%) unless otherwise stated
LAR low anterior resection, IBD inflammatory bowel disease
Survey responses: patients
Eleven (36.7%) subjects completed the online survey in less than 5 min and 13 (43.3%) in 6–10 min (Fig. 2). Thus, 80% of the sample completed the survey within 10 min. By comparison, the median time for in-person clinic visits was 75 (IQR 50–100) minutes, including travel time (Table 2). When asked whether they would be comfortable with the web visit replacing the in-clinic visit, 15 (50%) patients answered affirmatively. Twelve (40%) patients uploaded a photo of their incisions at the time of the survey; the remainder was not able to do so due to technical difficulties (i.e., files too large to upload). Although patients who submitted photographs of their incisions were overall older than those who did not (median age 65, IQR 51.6–67.7 vs. 61.4, IQR 50.1–67.1 years), this result was not statistically significant (p = 0.3).
Fig. 2.
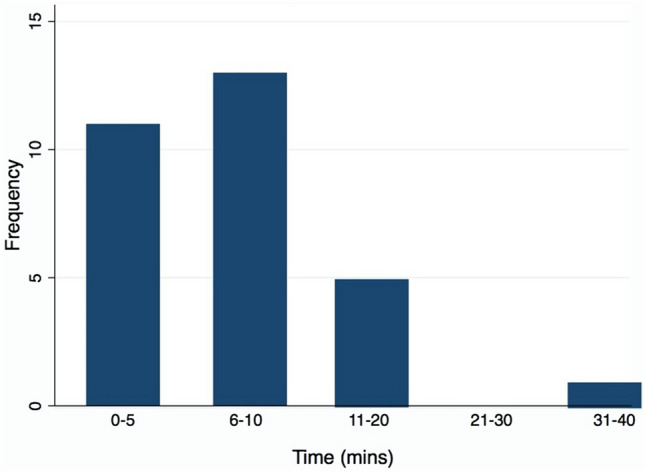
Time to survey completion
Table 2.
Patient responses to online survey
| Did you like online questionnaire format | |
| Very unhappy | 1 (3.3) |
| Somewhat unhappy | 0 (0) |
| Neutral | 9 (30.0) |
| Somewhat happy | 8 (26.7) |
| Very happy | 12 (40.0) |
| Likelihood of recommending online questionnaire to other patients | |
| Very unlikely | 1 (3.3) |
| Somewhat unlikely | 2 (6.7) |
| Neutral | 6 (20.0) |
| Somewhat likely | 11 (36.7) |
| Very likely | 10 (33.3) |
| Rating of office care (out of 5), mean, SD | 4.6 (1.2) |
| Total visit time (mins), mean, SD | 73.3 (30.1) |
| Would you be comfortable with the online visit replacing the first follow-up visit? | |
| Yes | 15 (50) |
| No | 15 (50) |
All values listed are n (%) unless otherwise stated
As shown in Table 3, reasons in favor of the web-based survey as sole means of follow-up included: visit efficiency and lack of traveling (n = 11, 73.3%), no parking fees (n = 9, 60%), and elimination of travel logistics, such as finding a ride, time from work and childcare (n = 5, 33%). Reasons for preferring in-person visits included ease of asking questions (n = 10, 66.7%), need for reassurance and overall preference for in-person visits (n = 9, 60%), as well as better physical exam (n = 7, 46.7%). There were no statistically significant differences in age, gender, or ASA class among patients who were in favor vs. those who were against the web-based visit alone.
Table 3.
Reasons for and against online visit
| Reasons for online visit | |
| More efficient | 11 (73.3) |
| Easy to use | 11 (73.3) |
| Saves traveling time | 11 (73.3) |
| Saves parking fees | 9 (60.0) |
| Saves from arranging a ride | 5 (33.3) |
| Saves from finding time off work or childcare | 5 (33.3) |
| Other | 1 (6.6) |
| Reasons against online visit | |
| Easier to ask questions | 10 (66.7) |
| More reassuring | 9 (60.0) |
| Prefer face-to-face visit | 9 (60.0) |
| In-person visit is better for exam | 7 (46.7) |
| Better overall care | 2 (13.3) |
| Other | 2 (13.3) |
All values listed are n (%) unless otherwise stated
Survey responses: providers
Providers responded that the web-based visit could replace the in-person visit in 27 instances (90.9%) and that they would prefer a web-based visit alone in 26 of the subjects enrolled (86.7%). The online questionnaire was deemed to reflect the in-person visit in 83.3% of cases. Changes in management were made on 4 occasions, only one of which a patient had uploaded a photograph (Table 4). Reasons for management changes included SSI (n = 3, 13.3%) and resumption of chronic anticoagulation (n = 1, 3.3%).
Table 4.
Provider responses
| Can the web-based visit replace the office visit? | |
| Yes | 27 (90.0) |
| No | 3 (10.0) |
| Reasons why office visit preferred | |
| Wound non-healing | 2 (66.7) |
| Patient had many questions | 1 (33.3) |
| Would you prefer a web based or in-person visit for this patient? | |
| Web based | 26 (86.7) |
| In-clinic | 4 (13.3) |
| How well did the online questionnaire reflect the in-person visit? | |
| Neutral | 2 (6.7) |
| Somewhat well | 3 (10.0) |
| Very well | 25 (83.3) |
| Any management changes during in-person visit? | |
| No | 26 (86.7) |
| Yes | 4 (13.3) |
| Description of management changes | |
| SSI | 3 (10) |
| Management of anticoagulation | 1 (3.3) |
| Photos uploaded for all pts with management changes (n = 4) | 1 (25.0) |
All values listed are n (%) unless otherwise stated
Discussion
Principal findings
The use of remote health care visits with patient portals, mobile apps, and telemedicine has been well established in non-surgical specialties [3, 6–9]. In recent years, there has been an increasing trend in utilizing such platforms in surgical divisions, including orthopedics [10, 11], general/acute care surgery [4, 12], and bariatrics [13]. This study investigates the feasibility of a web-based survey delivered via an institutional Epic-based patient portal for the first post-operative visit after elective colon or rectal resection, involving a wide range of diagnoses and surgical procedures. Our results demonstrate that a post-operative online visit platform is feasible and reflects the assessment and findings of an in-person exam in most patients. No major complications were discovered at the in-person visit that were missed with the web-based survey. Although this study was designed prior to the COVID-19 pandemic, it poses a novel alternative for post-operative follow-up care, particularly for patients who continue to require adherence to social distancing guidelines (i.e., immunocompromised). Furthermore, the asynchronous nature of this platform allows for surgeon flexibility while facilitating timely communication. The use of patient portal surveys may eliminate the need for live telephone or video visits, which are commonly used for Telehealth appointments.
Several studies demonstrate surgeon willingness to adopt remote post-operative visit platforms. A UK study aiming to assess whether the National Health Service could be used for post-operative monitoring after colorectal surgery concluded that the system was capable of detecting post-operative complications. However, the study involved a total of 17 patients and did not comment on patient and provider satisfaction [14]. Our participating colorectal surgeons similarly reported that the web-based survey could replace in-person follow-ups in 90% of cases and that survey responses reflected the in-person visit in 83% of cases. In a study assessing the use of wound photography for post-operative assessment, it was found that wound photographs increased surgeon confidence to diagnose SSIs [15]. Unfortunately, due to technical challenges, our ability to identify SSIs was limited, as only 40% of our patients uploaded incision photos. Another study assessing the use of a mobile app for post-operative monitoring in breast and orthopedic surgery patients found that surgeons were comfortable using the app to decrease the number of in-person post-operative visits and thus improve clinic efficiency [10].
In contrast, only 50% of our sample reported that a post-operative evaluation with the web-based survey alone was sufficient, despite the significant time savings and convenience. Primary reasons for preferring in-person visits were ease of asking questions, desire for a face-to-face interaction, and the perception that in-person visits provided more reassurance. Furthermore, the two groups (patients who preferred the idea of a web-based visit alone vs. those who rejected it) were similar in their demographics, ASA class, and disease process/surgical indication. These results provide new insights compared to previously reported findings in terms of patient satisfaction and acceptance of virtual post-operative visit platforms. In a study analyzing use of a patient portal for post-op visits, Broman et al. reported that 76% of their sample found the online format alone to be acceptable for follow-up [3]. The mean overall satisfaction score for a mobile app used for post-op monitoring for breast and orthopedic patients was 3.9 out of 4 [10]. Our findings demonstrate that although virtual visits may be better accepted by colorectal surgeons, a large proportion of CRS patients may prefer the in-person interaction and opportunity for discussion, despite the added travel inconvenience, cost, and time commitment.
Potential solutions to improve patient satisfaction scores with our online tool include more extensive education sessions with research staff at the time of enrollment. During these sessions, patients would become more familiar with the platform, which would help tailor their expectations at the time of survey completion post-discharge. Our survey also solely consisted of a sequential list of questions, which may have thus not provided as much reassurance as an in-person visit. Enlisting the help of our Information technology department (IT) to include voice prompts and visual cues to make the platform more interactive may improve patient satisfaction scores.
Limitations
This study presents several limitations. First, our sample was overwhelmingly Caucasian with a median age of 61.5 years. This limits our ability to assess whether a web-based visit would be acceptable to patients of different races, ethnicities, and age groups and reflects inherent bias related to the widespread applicability of this option across a diverse population. Second, over 50% of the sample were unable to upload a picture, most often due to file size limits. Similar technical difficulties are reported in other studies, who identified lack of technology education and familiarity with a Telehealth platform as a barrier to using that modality [16]. To circumvent this obstacle in future studies, subjects would likely benefit from the more extensive education sessions upon enrollment, mentioned above, to better navigate the involved technology. Third, we discovered some specific areas to focus the online questionnaire to better reflect patient needs which will enhance future communications. Lastly, this is a small feasibility study in a single institution and thus our findings may not be generalizable to other settings.
Conclusion
Our findings demonstrate that an asynchronous online patient post-operative follow-up visit is feasible following colorectal surgery. While less time consuming and a more efficient use of resources, patients in this study preferred the in-person visit for the opportunity to sit and communicate directly with their surgeon. Platforms with more reliable technology, better patient education, and inclusion of a wider patient demographic may improve utilization and satisfaction.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
CCB, SSH, and JAM were responsible for the conception, design, and redaction of this manuscript. CCB conducted the statistical analyses. JSD, PRS, KA, and JAM contributed to the design, data interpretation, and revisions for the final approval of this manuscript. All authors provided substantial contributions.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Disclosures
Catherine C. Beauharnais, Susanna S. Hill, Paul R. Sturrock, Jennifer S. Davids, Karim Alavi, and Justin A. Maykel have no conflict of interest or financial ties to disclose.
Footnotes
Prior Presentation Accepted as a poster presentation at the New England Surgical Society (NESS) Annual Meeting, Foxwoods, CT, September 2021.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kachare MD, Rossi AJ, Donohue KD, Davidov T. Telesurgical assessment: using smartphone messaging to efficiently manage postoperative wounds. Telemed e-Health. 2020;26:1540–1542. doi: 10.1089/tmj.2019.0270. [DOI] [PubMed] [Google Scholar]
- 2.Irarrázaval MJ, Inzunza M, Muñoz R, Quezada N, Brañes A, Gabrielli M, Soto P, Dib M, Urrejola G, Varas J, Valderrama S, Crovari F, Achurra P. Telemedicine for postoperative follow-up, virtual surgical clinics during COVID-19 pandemic. Surg Endosc. 2021;35:6300–6306. doi: 10.1007/s00464-020-08130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kummerow Broman K, Oyefule OO, Phillips SE, Baucom RB, Holzman MD, Sharp KW, Pierce RA, Nealon WH, Poulose BK. Postoperative care using a secure online patient portal: changing the (inter)face of general surgery. J Am Coll Surg. 2015;221:1057–1066. doi: 10.1016/j.jamcollsurg.2015.08.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parnell K, Kuhlenschmidt K, Madni D, Chernyakhovsky C, Donovan I, Garofalo K, Hambrick S, Scott DJ, Oltmann SC, Luk S. Using telemedicine an an acute care surgery service: improving clinic efficiency and access to care. Surg Endosc. 2021;35(10):5760–5765. doi: 10.1007/s00464-020-08055-9. [DOI] [PubMed] [Google Scholar]
- 5.Kirchhoff P, Clavien PA, Hahnloser D. Complications in colorectal surgery: risk factors and preventive strategies. Patient Saf Surg. 2010;4(1):5. doi: 10.1186/1754-9493-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Nurs Times. 2001;97(35):35. [PubMed] [Google Scholar]
- 7.Cronin RM, Davis SE, Shenson JA, Chen Q, Rosenbloom ST, Jackson GP. Growth of secure messaging through a patient portal as a form of outpatient interaction across clinical specialties. Appl Clin Inform. 2015;6(2):288–304. doi: 10.4338/ACI-2014-12-RA-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross SE, Moore LA, Earnest MA, Wittevrongel L, Lin CT. Providing a web-based online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res. 2004;6(2):e12. doi: 10.2196/jmir.6.2.e12.May14,2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Basch E, Artz D, Iasonos A, Speakman J, Shannon K, Lin K, Pun C, Yong H, Fearn P, Barz A, Scher H, Mccabe M, Schrag D. Evaluation of an online platform for cancer patient self-reporting of chemotherapy toxicities. J Am Med Inform Assoc. 2007;14(3):264–268. doi: 10.1197/jamia.M2177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semple JL, Sharpe S, Murnaghan L, Theodoropoulos J, Metcalfe K. Using a mobile app for monitoring post-operative quality of recovery of patients at home: a feasibility study. JMIR mHealth uHealth. 2015;3(1):e18. doi: 10.2196/mhealth.3929.Feb12,2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang J, Dushaj K, Rasquinha VJ, Scuderi GR, Hepinstall MS. Monitoring surgical incision sites in orthopedic patients using an online physician-patient messaging platform. J Arthroplasty. 2019;34(9):1897–1900. doi: 10.1016/j.arth.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 12.Chen DW, Davis RW, Balentine CJ, Scott AR, Gao Y, Tapia NM, Berger DH, Suliburk JW. Utility of routine postoperative visit after appendectomy and cholecystectomy with evaluation of mobile technology access in an urban safety net population. J Surg Res. 2014;190(2):478–483. doi: 10.1016/j.jss.2014.04.028. [DOI] [PubMed] [Google Scholar]
- 13.Sada A, Asaad M, Reidt WS, Kellogg TA, Kendrick ML, McKenzie TJ, Habermann EB. Are in-person post-operative clinic visits necessary to detect complications among bariatric surgery patients? Obes Surg. 2020;30(5):2062–2065. doi: 10.1007/s11695-019-04329-x. [DOI] [PubMed] [Google Scholar]
- 14.Bragg DD, Edis H, Clark S, Parsons SL, Perumpalath B, Lobo DN, Maxwell-Armstrong CA. Development of a telehealth monitoring service after colorectal surgery: a feasibility study. World J Gastrointest Surg. 2017;9(9):193–199. doi: 10.4240/wjgs.v9.i9.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kummerow Broman K, Gaskill CE, Faqih A, Feng M, Phillips SE, Lober WB, Pierce RA, Holzman MD, Evans HL, Poulose BK. Evaluation of wound photography for remote postoperative assessment of surgical site infections. JAMA Surg. 2019;154(2):117–124. doi: 10.1001/jamasurg.2018.3861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kemp MT, Liesman DR, Williams AM, Brown CS, Iancu AM, Wakam GK, Biesterveld BE, Alam HS. Surgery provider perceptions on telehealth visits during the COVID-19 pandemic: room for improvement. J Surg Res. 2021;260:300–306. doi: 10.1016/j.jss.2020.11.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.