Abstract
Background:
Single-incision laparoscopic cholecystectomy, first introduced in 1995, features acceptable cosmetic outcomes and postoperative pain control. The outcomes of single-port cholecystectomy by laparoscopy and robots were recently examined in many studies owing to surgeon and patient preference for minimally invasive surgery. A next-level da Vinci robotic platform was recently released. This study aimed to evaluate the feasibility and efficacy of robotic cholecystectomy (RC) using the da Vinci SP® system.
Methods:
In this retrospective observational single-center study, we analyzed the medical records of 304 patients who underwent RC between March 1, 2017 and May 31, 2021.
Results:
Of the 304 patients, the da Vinci Xi® (Xi) was used in 159 and the da Vinci SP® (SP) was used in 145. The mean operation time was 45.7 mins in the SP group versus 49.8 mins in the Xi group. The mean docking time of the SP group was shorter than that of the Xi group (5.7 min vs 8.8 min; p = 0.024). The mean immediate postoperative numerical rating scale (NRS) score was 4.0 in the SP group and 4.3 in the Xi group, showing a significant difference (p = 0.003). A separate analysis of only patients with acute cholecystitis treated with the da Vinci SP® showed that the immediate postoperative NRS score in the acute group was higher than that in the nonacute group.
Conclusions:
This study demonstrated acceptable results of single-site cholecystectomy using da Vinci SP®. Thus, pure single-port RC using the da Vinci SP® for various benign gallbladder diseases may be an excellent treatment option.
Keywords: Robotic surgery, Robotic cholecystectomy, Da Vinci SP
INTRODUCTION
Minimally invasive surgery (MIS) has revolutionized our surgical practice over the past few decades.1–3 MIS is safe and effective for the surgical management of several diseases, especially gallbladder disease.4–6 Multiport laparoscopic cholecystectomy is the well-known standard surgical procedure for benign gallbladder (GB) diseases. Single-incision laparoscopic cholecystectomy, which was first introduced in 1995, is considered an effective modality in terms of patient satisfaction, including cosmetic outcomes and postoperative pain control. Historically, however, it was seldom used because it was not ergonomic owing to behavioral restrictions caused by the narrow working spaces.
Since then, robotic systems, which first became capable of ergonomic and more detailed surgery in the early 2000s, have continued to overcome these limitations. The outcomes of single-port cholecystectomy by laparoscopy and robots were recently examined in many studies owing to surgeon and patient preference for MIS.7–9
The da Vinci Xi® system, among the most widely used robotic machines for single-site robotic cholecystectomy (RC), features unprecedented excellent ergonomics and preserves proper triangulation. However, the frustration caused by surgery performed using a nonwrist robot arm with a single port remained a problem. Intuitive Surgical (Sunnyvale, CA, USA) recently released a next-level single-port platform, the da Vinci SP® system, that features three fully wristed and elbowed instruments and a flexible camera within a single 2.5-cm cannula.
This study aimed to evaluate the feasibility and efficacy of RC using the da Vinci SP® system.
MATERIALS AND METHODS
Patient Selection
This retrospective observational single-center study was conducted after informed consent was provided by each patient and approval was granted by the ethics committee. We analyzed the medical records of 304 patients who underwent RC between March 1, 2017 and May 31, 2021. The da Vinci Xi® (Xi) was used to treat 159 and the da Vinci SP® (SP) was used to treat 145 patients.
Surgery using the SP was first performed in May 2020. The indication for RC were patients with presently symptomatic cholelithiasis or those who experienced symptoms in the past, including GB polyp and adenomyomatosis.
The exclusion criteria, applied equally to both platforms, were as follows: 1) severe acute cholecystitis; 2) suspected malignancy; and 3) history of major upper abdominal surgery such as stomach surgery.
The demographic, pre-, and postoperative data were retrospectively collected, as were the postoperative NRS scores for pain (immediately and 24 hours later).
OPERATIVE PROCEDURES
Single-Site RC Using the da Vinci Xi®
The patients were placed in the supine and reverse Trendelenburg position with the arms secured at the sides of the body. An approximately 3-cm vertical transumbilical incision was made. Through this incision, a single-site port (Intuitive Surgical) was inserted. When the pneumoperitoneum was established, the DaVinci Xi® system (Intuitive Surgical) was docked at the right upper section. We inserted an 8-mm camera cannula into the blue channel and targeted the GB. Next, on the right side, a curved cannula was inserted in the white channel for a permanent cautery hook. The same cannula was inserted under the hook on the left side of the Crocodile grasper. Finally, the first assistant retracted the GB cranially using the laparoscopic grasper, if necessary. Once all ports were in, the cystic duct and artery were ligated using robotic Hem-o-lok® clips (Weck Closure System, Research Triangle Park, NC, USA). Finally, the gallbladder was dissected from the GB fossa and retrieved using a multiport. The fascia was closed with interrupted sutures, and the subcutaneous tissue was closed with 4-0 Vicryl sutures.
Single-Site RC Using the da Vinci SP®
The patient was placed in a supine position and draped. A 30.0-cm vertical incision was made at the umbilicus, a uniport device (Uni-port, Dalim-medical, Seoul, Korea) was applied, and the da Vinci single 2.5-cm trocar was inserted into the uniport and connected to provide insufflation. After changing the position of the head and right side up, the single port was docked to the robot bearing the robotic arms. The camera was inserted into the middle hole, a fenestrated bipolar forceps was placed in the left hole (arm 1), a Cadiere forceps was placed in the upper-middle hole (arm 2), and the hook forceps was placed in the right hole (arm 3).
Superolateral traction of the gallbladder fundus was accomplished using arm 2. The dissection was started at the cystic plate with the left-handed grasper (bipolar) holding Hartmann’s pouch and the right-handed hook performing the diathermy. A critical view of safety was attained, and the cystic duct and artery were clipped and divided separately using a Hem-o-lok®. The gallbladder was dissected off its bed, and the first assistant placed the gasper device through the other opening of the uniport and grabbed it to ensure that the GB did not fall out. After checking for hemostasis and bile leakage, the instruments were withdrawn, the patient cart arm was undocked, and the specimen was pulled out using a single-site trocar and uniport device (Figure 1).
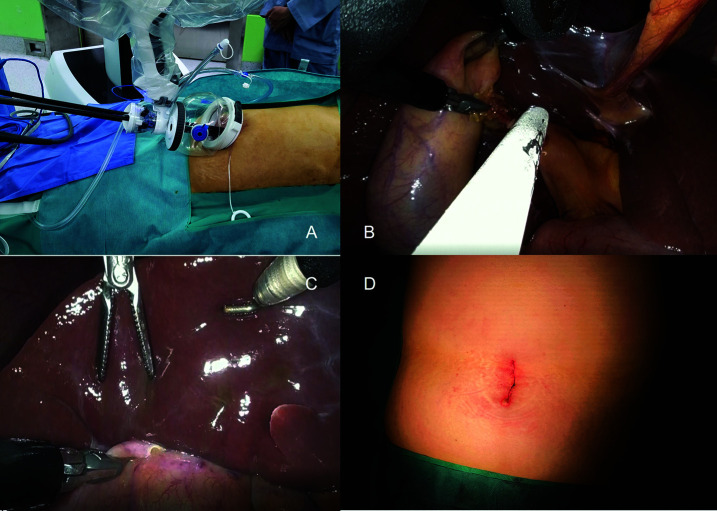
Figure 1.
Intraoperative procedure of the robotic da Vinci SP® cholecystectomy. (A) External view of the docked da Vinci SP® system with uniport. (B) View of the use suction device using accessory opening of the uniport device. (C) View of retraction of liver using endo-wristed robot arm when performing gall bladder dissection. (D) 3 centimeter skin incision at the umbilicus.
STATISTICAL ANALYSIS
Normally distributed data are reported as mean (standard deviation), while nonnormally distributed data are presented as medians (range). Continuous variables were compared using Student’s t test if normally distributed; otherwise, the Mann–Whitney U test was used.
Categorical variables were compared using the χ2 test. Data were considered statistically significant at P < .05. Statistical analyses were conducted using SPSS® version 220.0 for Windows (IBM, Chicago, IL, USA).
RESULTS
Clinicopathological Features and Surgical Outcomes of the Xi versus SP Groups
The mean patient age was 44.9 years in the SP group versus 39.8 years in the Xi group, showing a statistically significant intergroup difference (P = .017). In both groups, the dominant sex was female. Most patients in both groups were asymptomatic, while abdominal pain was otherwise the most common symptom.
In the SP group, an American Society of Anesthesiologists (ASA) score of 1 was observed in 87 cases, score 2 in 57 cases, and score 3 in 1 case. In the Xi group, an ASA score of 1 was observed in 96 cases, score 2 in 62 cases, and score 3 in 1 case, with no statistically significant intergroup difference. In both groups, GB stones was the most common pre-operative diagnosis. Acute cholecystitis was observed in 17 patients in the SP group versus eight patients in the Xi group. The detailed clinicopathological features of both groups are shown in Table 1.
Table 1.
Clinicopathological Features and Surgical Outcomes
| da Vinci SP® | da Vinci Xi® | p-Value | |
|---|---|---|---|
| (N = 145) | (N = 159) | ||
| Sex , n (%) | 0.017 | ||
| Female | 83 (57.2) | 113 (71.1) | |
| Male | 62 (42.8) | 46 (28.9) | |
| Age, years | 44.9 ± 10.9 | 39.8 ± 8.3 | < 0.001 |
| Body mass index, kg/m2 | 25.4 (23.2 – 28.4) | 23.7 (21.5 – 26.7) | < 0.001 |
| American Society of Anesthesiologists status, n (%) | 0.882 | ||
| 1 | 87 (60.0) | 96 (60.3) | |
| 2 | 57 (39.3) | 62 (39.0) | |
| 3 | 1 (0.7) | 1 (0.6) | |
| Pre-operative symptom | 0.533 | ||
| Asymptomatic | 70 (48.3) | 69 (43.4) | |
| Abdominal pain | 61 (42.1) | 69 (43.4) | |
| Dyspepsia | 12 (8.3) | 20 (12.6) | |
| Other | 2 (1.4) | 1 (0.6) | |
| Pre-operative diagnosis (1), n (%) | 0.097 | ||
| Gallbladder Stone | 85 (58.6) | 92 (57.9) | |
| Gallbladder polyp | 24 (16.6) | 25 (15.7) | |
| Combined | 31 (21.4) | 40 (25.2) | |
| Adenomyomatosis | 5 (3.4) | 2 (1.2) | |
| Pre-operative diagnosis (2), n (%) | 0.056 | ||
| Nonacute cholecystitis | 128 (88.3) | 151 (95.0) | |
| Acute cholecystitis | 17 (11.7) | 8 (5.0) | |
| Previous abdominal operation history | 0.644 | ||
| No | 125 (86.2) | 133 (83.6) | |
| Yes | 20 (13.8) | 26 (16.4) | |
| Bilirubin, mg/dL | 0.6 ± 0.3 | 0.5 ± 0.2 | 0.378 |
| White blood cell count, 103/uL | 5.7 ± 1.9 | 5.2 ± 1.3 | 0.015 |
| Operation time, min | 45.0 (38.0 – 55.0) | 47.0 (40.0 – 56.5) | 0.012 |
| Conversion, n (%) | 0 (0) | 0 (0) | |
| Docking time, min | 6.0 (5.0 – 8.0) | 8.0 (7.0 – 10.0) | 0.024 |
| Pain, Numerical Rating Scale | |||
| Immediate | 4.0 ± 0.9 | 4.3 ± 1.1 | 0.003 |
| After 24 hours | 2.1 ± 0.9 | 2.3 ± 1.2 | 0.136 |
| Hospital stay, day | 2.1 ± 0.8 | 2.2 ± 1.1 | 0.574 |
| Morbidity, Clavien-Dindo classification, n (%) | 0.607 | ||
| I | 6 (4.1) | 5 (3.1) | |
| II | 2 (1.4) | 4 (2.5) | |
| IIIa | 0 (0.0) | 1 (0.6) | |
| IIIb | 1 (0.7) | 0 (0.0) | |
No conversion from robotic surgery to open surgery occurred in either group.
The median operation time was 45 mins in the SP group versus 47 mins in the Xi group. The median docking time of the SP group was shorter than that of the Xi group (6.0 min vs 8.0 min; P = .024). The mean immediate postoperative NRS was 4.0 in the SP group and 4.3 in the Xi group, with a significant difference (P = .003). Postoperative morbidity of Clavien-Dindo grade ≥ 3 was observed in 1 case in each group, all of which were surgically performed for incisional hernia. The mean hospital stay was 2.1 days in the SP group versus 2.2 days in the Xi group. The detailed clinicopathological features and surgical outcomes of both groups are shown in Table 1.
OUTCOMES OF PATIENTS WITH ACUTE CHOLECYSTITIS USING THE DA VINCI SP®
A separate analysis of only patients with acute cholecystitis using the da Vinci SP® showed a higher bilirubin level, higher white blood cell count, and longer operation time compared with nonacute cholecystitis patients. However, the length of hospital stay and morbidity rate were not significantly different between the two groups. The immediate postoperative numerical rating scale score in the acute group was higher than that in the nonacute group, but there was no significant intergroup difference in NRS scores in the following 24 hours (Table 2).
Table 2.
Outcomes of Patients with Acute Cholecystitis Using da Vinci SP®
| Acute | Nonacute | p-Value | |
|---|---|---|---|
| (n = 17) | (n = 128) | ||
| Bilirubin , mg/dL | 0.9 ± 0.5 | 0.5 ± 0.1 | 0.003 |
| White blood cell count, 103/uL | 8.8 ± 3.7 | 5.3 ± 0.9 | 0.001 |
| Pre-operative symptom, n (%) | 0.001 | ||
| No symptom | 0 (0.0%) | 70 (54.7%) | |
| Abdominal pain | 15 (88.2%) | 46 (35.9%) | |
| Dyspepsia | 2 (11.8%) | 10 (7.8%) | |
| Other | 0 (0.0%) | 2 (1.6%) | |
| Pain, Numerical Rating Scale | |||
| Immediate | 4.9 ± 1.2 | 4.2 ± 1.0 | 0.014 |
| After 24 hours | 2.3 ± 1.0 | 2.3 ± 1.2 | 0.924 |
| Hospital stay, day | 2.6 ± 2.2 | 2.1 ± 0.3 | 0.304 |
| Morbidity, Clavien-Dindo classification, n (%) | 0.993 | ||
| I | 1 (5.9%) | 5 (3.9%) | |
| II | 1 (5.9%) | 1 (0.8%) | |
| IIIa | 0 (0.0%) | 0 (0.0%) | |
| IIIb | 1 (5.9%) | 0 (0.0%) | |
| Operation time, min | 62.0 (42.0 – 70.0) | 44.0 (36.5 – 53.0) | 0.017 |
DISCUSSION
To date, robotic surgery using a single-port platform has been used for hysterectomy, prostatectomy, and cholecystectomy. Robotic surgical systems have several advantages over laparoscopic surgery, and their applications have been gradually expanded to various fields and more complicated procedures.3, 10–12
Jang et al. reported an experience with single-site laparoscopic cholecystectomy using the da Vinci Xi® in 2021 and showed that it features better pain control or lower cost compared to conventional laparoscopic cholecystectomy.13 Many studies have been published in which the early single-site surgical platform, represented by da Vinci Si® and da Vinci Xi®, has a composite effect and better pain control compared to conventional laparoscopic surgery.14–17 Since then, the surgical platform has been gradually developed and several excellent surgical outcomes have been identified along with operator convenience.16,18–20 To the best of our knowledge, the current large study was the first to validate the feasibility of the da Vinci SP® system in benign GB disease. The da Vinci SP® system enables surgeons to perform delicate and complex operations through a small incision. The da Vinci SP® system consists of several key components, including an ergonomically designed console where the surgeon sits while operating, a patient-side cart on which the patient is positioned during surgery, interactive robotic arms, a three-dimensional high-definition vision system, and a proprietary endowrist arm. The distal triangulation of the SP robot arm provides a greater degree of freedom of movement, particularly in narrow and deep areas.
According to the present results comparing the Xi and SP, the complication rate based on the Clavien–Dindo classification, conversion rate, postoperative pain, and hospital stay were acceptable, suggesting that the da Vinci SP® platform is as safe as the da Vinci Xi® system.
In addition, in this study, compared to the da Vinci Xi®, the further reduced operation time, faster docking time, and low immediate NRS score were investigated. Docking in da Vinci SP® is significantly faster, as only one trocar requires docking compared to the three trocars in the da Vinci Xi®. Despite having the same incision size at the same location, the lower immediate postoperative NRS in patients with da Vinci SP® use was due to a more ergonomically designed wrist arm and vision card showing real-time instrument position relative to electronic treatment compared to the da Vinci Xi®.
In the study of single-site cholecystectomy using the SP platform prior to our study, there have been some issues in that it cannot respond suitably to bleeding accidents or bile spillage due to the absence of an accessory port for the assistant.20–22 This fact acted as a hurdle to the application of single-site cholecystectomy to acute cholecystitis for beginners who started robotic surgery and tried to perform single-site RC.
The authors validated that this hurdle could be overcome to some extent with the use of a multiport device in addition to the da Vinci SP®, which enables the application of the suction device and vascular stapler. The authors operated on a total of 17 patients with acute cholecystitis using the da Vinci SP® during the study period and recorded an operation time that was longer than the operation time of those who did not use the system, but no conversions to open surgery occurred.
In addition, except for one incisional hernia, no serious surgical complications were identified, and the mean hospital stay did not differ from that of the nonacute cholecystitis patient group. This result shows that the application of robotic surgery for acute cholecystitis can be expanded through additional large-scale and multicenter studies in the future. As such, the advantages of SP have been identified, but limitations also exist. However, energy devices, staplers, and surgical metal clips compatible with the SP system have not been developed to date. The development of instruments is absolutely necessary for application of the SP system to more hepatobiliary and pancreatic surgeries.
Also, there may be limitation on the application for other country or races with different demographic features, such as body mass index (BMI). In western countries, it is well known that the average BMI is relatively high, and many research studies shows that there is a positive correlation between high BMI and the incidence of incisional hernia. Lastly, the cost aspect of medical expenses was not considered in this study. For the establishment of robotic surgery as an effective technology, not only the medical aspect represented by the surgical outcome, but also the sociological aspect represented by the distribution of medical resources must be considered together.
In summary, this study demonstrated acceptable results of single-site cholecystectomy using the da Vinci SP®. In addition, analysis of the use of the SP in patients with acute cholecystitis confirmed its possible application in severe cholecystitis cases. Further studies of accumulated cases of various GB diseases are required to expand the usefulness of the da Vinci SP®.
Footnotes
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Informed consent: Dr. Wan-Bae Kim declares that written informed consent was obtained from the patient/s for publication of this study/report and any accompanying images.
Contributor Information
Wan-Joon Kim, Division of Hepatobiliary Pancreas Surgery, Department of Surgery, Korea University Guro Hospital, Korea University Medical College, Seoul, Korea..
Sae-Byeol Choi, Division of Hepatobiliary Pancreas Surgery, Department of Surgery, Korea University Guro Hospital, Korea University Medical College, Seoul, Korea..
Wan-Bae Kim, Division of Hepatobiliary Pancreas Surgery, Department of Surgery, Korea University Guro Hospital, Korea University Medical College, Seoul, Korea..
References:
- 1.Ruurda JP, Visser PL, Broeders IA. Analysis of procedure time in robot-assisted surgery: comparative study in laparoscopic cholecystectomy. Comput Aided Surg. 2003;8(1):24–29. [DOI] [PubMed] [Google Scholar]
- 2.Bodner J, Hoeller E, Wykypiel H, Klingler P, Schmid T. Long-term follow-up after robotic cholecystectomy. Am Surg. 2005;71(4):281–285. [DOI] [PubMed] [Google Scholar]
- 3.Corcione F, Esposito C, Cuccurullo D, et al. Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc. 2005;19(1):117–119. [DOI] [PubMed] [Google Scholar]
- 4.Yoshida T, Matsumoto T, Sasaki A, et al. Laparoscopic cholecystectomy in the treatment of patients with gall bladder cancer. J Am Coll Surg. 2000;191(2):158–163. [DOI] [PubMed] [Google Scholar]
- 5.Ruurda JP, Broeders IA, Simmermacher RP, Rinkes IH, Vroonhoven TJ. Feasibility of robot-assisted laparoscopic surgery: an evaluation of 35 robot-assisted laparoscopic cholecystectomies. Surg Laparosc Endosc Percutan Tech. 2002;12(1):41–45. [DOI] [PubMed] [Google Scholar]
- 6.Akatsu T, Ueda M, Shimazu M, et al. Long-term survival of patients with gallbladder cancer detected during or after laparoscopic cholecystectomy. World J Surg. 2005;29(9):1106–1109, discussion 1110. [DOI] [PubMed] [Google Scholar]
- 7.Heemskerk J, van Dam R, van Gemert WG, et al. First results after introduction of the four-armed da Vinci Surgical System in fully robotic laparoscopic cholecystectomy. Dig Surg. 2005;22(6):426–431. [DOI] [PubMed] [Google Scholar]
- 8.Vidovszky TJ, Smith W, Ghosh J, Ali MR. Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res. 2006;136(2):172–178. [DOI] [PubMed] [Google Scholar]
- 9.Breitenstein S, Nocito A, Puhan M, Held U, Weber M, Clavien PA. Robotic-assisted versus laparoscopic cholecystectomy: outcome and cost analyses of a case-matched control study. Ann Surg. 2008;247(6):987–993. [DOI] [PubMed] [Google Scholar]
- 10.Maeso S, Reza M, Mayol JA, et al. Efficacy of the da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis. Ann Surg. 2010;252(2):254–262. [DOI] [PubMed] [Google Scholar]
- 11.Kroh M, El-Hayek K, Rosenblatt S, et al. First human surgery with a novel single-port robotic system: cholecystectomy using the da Vinci Single-Site platform. Surg Endosc. 2011;25(11):3566–3573. [DOI] [PubMed] [Google Scholar]
- 12.Wren SM, Curet MJ. Single-port robotic cholecystectomy: results from a first human use clinical study of the new da Vinci single-site surgical platform. Arch Surg. 2011;146(10):1122–1127. [DOI] [PubMed] [Google Scholar]
- 13.Jeong Jang E, Kang SH, Kim KW. Early outcomes of robotic single site cholecystectomy using the daVinci Xi® System. JSLS. 2021;25(1):e2020.00082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han C, Shan X, Yao L, et al. Robotic-assisted versus laparoscopic cholecystectomy for benign gallbladder diseases: a systematic review and meta-analysis. Surg Endosc. 2018;32(11):4377–4392. [DOI] [PubMed] [Google Scholar]
- 15.Hagen ME, Balaphas A, Podetta M, et al. Robotic single-site versus multiport laparoscopic cholecystectomy: a case-matched analysis of short- and long-term costs. Surg Endosc. 2018;32(3):1550–1555. [DOI] [PubMed] [Google Scholar]
- 16.Migliore M, Arezzo A, Arolfo S, Passera R, Morino M. Safety of single-incision robotic cholecystectomy for benign gallbladder disease: a systematic review. Surg Endosc. 2018;32(12):4716–4727. [DOI] [PubMed] [Google Scholar]
- 17.Grochola LF, Soll C, Zehnder A, Wyss R, Herzog P, Breitenstein S. Robot-assisted single-site compared with laparoscopic single-incision cholecystectomy for benign gallbladder disease: protocol for a randomized controlled trial. BMC Surg. 2017;17(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cruz CJ, Huynh F, Kang IC, Lee WJ, Kang CM. Initial experiences of robotic SP cholecystectomy: a comparative analysis with robotic Si single-site cholecystectomy. Ann Surg Treat Res. 2021;100(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cianci S, Rosati A, Rumolo V, et al. Robotic single-port platform in general, urologic, and gynecologic surgeries: a systematic review of the literature and meta-analysis. World J Surg. 2019;43(10):2401–2419. [DOI] [PubMed] [Google Scholar]
- 20.Milone M, Vertaldi S, Bracale U, et al. Robotic cholecystectomy for acute cholecystitis: three case reports. Medicine (Baltimore). 2019;98(30):e16010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abel SA, Dy BM, Al-Lami H, et al. Comparison of short- and long-term postoperative occurrences after robotic single-incision cholecystectomy versus multiport laparoscopic cholecystectomy. Surg Endosc. 2021;10. [DOI] [PubMed] [Google Scholar]
- 22.Grochola LF, Soll C, Zehnder A, Wyss R, Herzog P, Breitenstein S. Robot-assisted versus laparoscopic single-incision cholecystectomy: results of a randomized controlled trial. Surg Endosc. 2019;33(5):1482–1490. [DOI] [PubMed] [Google Scholar]