Abstract
Context
Nerves or fascia may limit motion in young soccer players, thereby contributing to frequent hamstrings injuries. Nerve-gliding exercises and self-myofascial release techniques may enhance range of motion (ROM).
Objective
To compare the immediate effect of foam rolling (FR) and neurodynamic nerve gliding (NDNG) on hamstrings passive stiffness, viscoelasticity, flexibility, and proprioception during the warm-up of soccer players.
Design
Crossover study.
Setting
Research laboratory.
Patients or Other Participants
A total of 15 male soccer players (age = 18.0 ± 1.4 years, height = 183.1 ± 6.0 cm, mass = 76.9 ± 7.8 kg) on the same team.
Intervention(s)
The FR and NDNG consisted of 6 sets of 45 seconds with a 15-second rest between sets. Over a 2-week period, participants performed FR and NDNG on 2 separate occasions.
Main Outcome Measure(s)
Stiffness (between 50% and 80%, and 85% and 95% [STFmax] of maximal knee-extension ROM), viscoelasticity (stress-relaxation test), knee-extension ROM, hamstrings passive-resistance torque (PRT), hip-flexion angle (straight-leg raise test), and active knee-joint position sense.
Results
We observed an interaction between time and intervention for STFmax (F1,17 = 5.024, P = .042), knee-extension ROM (F1,17 = 7.371, P = .02), and PRT (F1,17 = 4.876, P = .044). The NDNG technique induced increases in STFmax (t17 = 2.374, P = .03), ROM (t17 = 2.843, P = .01), and PRT (t17 = 2.982, P = .008). Both NDNG and FR led to improved performance on the straight-leg raise test (F1,17 = 87.514, P < .001). No interaction or main effect was found for the stress-relaxation test or active knee-joint position sense.
Conclusions
Adding NDNG to the warm-up routine increased ROM more than FR and may benefit soccer players.
Keywords: self-myofascial release, neural gliding, viscoelasticity, mobility
Key Points
Foam rolling and neurodynamic nerve gliding both had immediate positive effects on hamstrings flexibility in young soccer players.
The neurodynamic nerve-gliding technique was more effective than foam rolling for movements involving increased pressure on neural tissue in young soccer players.
The risk factors and mechanisms of hamstrings injuries in soccer players remain elusive despite considerable research efforts. However, investigators1 have shown that greater flexibility reduced the risk of hamstrings strain injury during kicking in the follow-through phase, which is associated with perhaps the greatest muscle-tendon unit lengths and sciatic nerve overstretch in soccer. Because hamstrings flexibility is related to neurodynamic functions and affects the physiological properties of neural tissue, adequate warm-up techniques are critical. Athletes commonly warm up before workouts and competitions to reduce their injury risk by increasing flexibility and improve performance by elevating the intramuscular temperature and activating skeletal muscles and the central nervous system. Warm-up usually encompasses different dynamic drills (eg, jogging, sprinting, leg press, squats, small-sided games) along with stretching routines (eg, static, dynamic, ballistic, or proprioceptive neuromuscular facilitation stretching). In training, various semidynamic intermediate or passive forms of warm-up, such as foam rolling (FR), neural mobilization (neurodynamic nerve gliding [NDNG]), massage, and passive heating, are used to increase warm-up efficiency, but evidence for their effectiveness is insufficient. Sensitivity of the hamstrings muscles to stretch and pain can reduce flexibility, and one purpose of the warm-up is to enhance neural function.
Researchers reported that stretching exercises increased range of motion (ROM) and stretch tolerance.2–4 Stretch tolerance refers to the length of the myotendon unit at which the participant experiences pain or discomfort.2,4 The sensation of discomfort during stretch to or beyond the stretch-tolerance length may originate from the stretching of nerve and fascia5; supraphysiological strain of the peripheral nerve can ultimately impair signal conduction, disrupt nerve anatomy, and cause injury.6 Joint motion indeed causes mechanical stress of the peripheral nerves as they are elongated and glided relative to adjacent tissues7,8 because of adhesions between the epineurium and the surrounding tissue that restrict the nerves from gliding freely. The excessive stress or friction of the peripheral nerves may therefore limit ROM via pain provocation.9
The fascia has a dense sensory innervation, making it highly sensitive to stress and strain. Given that fascia is a continuous structure and crosses several joints, it can sustain exceptional stress levels during stretching maneuvers that involve polyarticular motion, such as the slump position or straight-leg raising.10 Because the stresses and strains on nerves and fascia during movement may limit motion, the effect of nerve-gliding exercises and self-myofascial release techniques on hamstrings flexibility could facilitate the free movement of nerves and fascia and thereby increase the threshold of stretch tolerance.
Foam rolling is an intensive self-treatment technique that applies compressive force to muscles and soft tissue to improve the function of skeletal muscle and connective tissue.11 It increases ROM, decreases myofascial pain, improves recovery from exercise-induced muscle damage, and enhances performance.12 It is more effective than static and dynamic stretching in immediately increasing quadriceps and hamstrings flexibility without hampering muscle strength13 or altering passive stiffness.14 However, these results were not unequivocal, as in experienced athletes15 and physically active injury-free males,16 FR produced a short-term decrease in connective tissue stiffness. The effects of FR on tissue stiffness depend on the athlete's experience with FR,15 rolling velocity,14 rolling duration,12,17 and their use in combination with other stretching techniques or warm-up routines.16,18
In theory, NDNG restores the dynamic balance between the relative movement of neural tissues and the surrounding mechanical interfaces by reducing pressure on the neural tissue and promoting optimal physiological function.19 It changes the nervous system's mobility via movement and gliding of the neural tissue when one end of the neural system is moved as the other end is slackened.20 The NDNG technique can modify tissue texture or sensation21 and induce greater muscle extensibility.22
Despite substantial evidence supporting the use of FR and NDNG for improving flexibility, the effects of these procedures on muscle stiffness, which can increase the muscle-tendon unit injury risk,17 are unknown. Each technique can affect the muscle spindles, which are the primary sensory organs in the muscle, and changes in the muscle spindles may alter proprioception. Given that hamstrings injuries are a frequent problem, particularly in young soccer players, we chose to focus on young players and use a specific warm-up that included either FR or NDNG to compare the immediate effects on muscle extensibility that may translate into hamstrings injury prevention. Our purpose was to compare the immediate effects of FR and NDNG on hamstrings passive stiffness, viscoelasticity, flexibility, and proprioception during the warm-up of soccer players. We used a randomized crossover study design to reduce the effects of individual structural features and the participants' perceived sensation associated with maximal ROM limitations.
METHODS
Study Design
During a 2-week period, participants performed FR and NDNG on 2 separate occasions. The order of these 2 intervention sessions was randomized and counterbalanced among participants. The dependent variables in the study were changes in stiffness, viscoelasticity, flexibility, and proprioception of the knee flexors as assessed using the straight-leg raise test (SLR), stress-relaxation test (SRT), passive-stretching test (PST), and active knee-joint position sense test (AKJPS). The independent variables were time and type of stretching intervention (FR or NDNG).
Participants
Fifteen male soccer players (age = 18.0 ± 1.4 years [range = 17–21 years], height = 183.1 ± 6.0 cm, mass = 76.9 ± 7.8 kg, body mass index = 23.0 ± 1.3) who trained with the same team participated in the study. Based on previous data,2 a power calculation indicated that at least 14 participants were required to detect a 10% difference in passive hamstrings stiffness between interventions with an α level of .05 and the desired power of 80%. Volunteers were included if they were healthy and had trained with the team for at least 6 months before the study. The exclusion criteria were a hamstrings injury within the year before the study, regular performance of lower extremity muscle-stretching exercises, a history of neck trauma (whiplash) or neck symptoms, fracture in any part of the body, growth disorder, neurologic or orthopaedic disorder, diagnosed herniated disk, low back and hip pain in the 6 months before the study, or regular use of analgesic or nonsteroidal anti-inflammatory drugs. All participants provided written informed consent or assent, and a parent or guardian provided written informed consent for participants aged <18 years. The Lithuanian Sports University Biomedical Research Ethics Committee approved the study protocol.
Procedures
All participants attended a familiarization session to become accustomed to the equipment and procedures a few days before the start of the study. The familiarization session and testing were carried out by the same team of investigators (M.M.Z.A., R.M.K., G.K., K.V., A.S.). Testing was performed at the same time of the day with room temperature maintained at 22°C.
Pretesting
Before the warm-up on the test day, body composition analysis was conducted using a body fat analyzer (model 305; Tanita Corp). Surface electrodes (model EL254S; Biopac Systems, Inc) were attached to shaved and cleaned skin over the upper third of the right biceps femoris and semitendinosus muscles, and a ground electrode was fixed over the medial side of the patella. The interelectrode distance was 30 mm. Participants completed a warm-up exercise of 8 minutes of stationary cycling at 50 W.
Preintervention
After the warm-up, participants were seated on a Biodex System 3 isokinetic dynamometer with their hips and knees flexed to 90° (0° corresponded to full extension of the knee) and trunk strapped securely. They performed 3 passive maximal right knee extensions so that we could determine the ROM and passive-resistance torque (PRT). Then 2 maximal voluntary isometric contractions (MVICs) of the right knee flexors and extensors were performed. Each MVIC of the knee flexors and extensors lasted 5 seconds, with a 2-minute rest between contractions. The recordings of passive knee extension and MVICs of the knee flexors and extensors were synchronized with the recording of electromyography (EMG) signals sampled at 1000 Hz. The SLR and AKJPS tests were conducted before the FR or NDNG intervention.
Postintervention
The SLR, passive-stretching, and AKJPS tests were repeated immediately after the intervention. Measurements were obtained in the same order as at preintervention.
Straight-Leg Raise
Participants performed the passive SLR test while wearing shorts and lying in the supine position. They were instructed to relax the right lower limb. One examiner (M.M.Z.A.) grasped the ankle and raised the limb slowly while keeping the knee in full extension and the ankle in neutral position until the individual expressed discomfort in the thigh or exhibited posterior pelvic tilt (noted as movement of the anterior-superior iliac spine). The second investigator (K.V.) measured the hip-flexion angle using a universal goniometer with the axis over the greater trochanter of the femur. The stationary arm of the goniometer was placed parallel to the table (checked using a level), the moving arm was placed along the line between the head of the fibula and the fibular malleolus, and then the angle was recorded.22 At least 3 trials, with a 15-second rest between trials, were performed. If the values from any 2 trials differed by >2°, the test was repeated. The average of the 2 closest results was recorded as the passive SLR angle. The measurements were reliable throughout the trials: the intraclass correlation coefficient (ICC) of the SLR measurements was 0.868 (95% CI = 0.520, 0.964).
Passive-Stretching Test
For the PST, the participant was seated on the isokinetic dynamometer without shoes, with the hip flexed to about 120° and the knee flexed to 80°; the shank was placed at 50° below the horizontal, and the knee was fully extended to 180°.2 The pelvis and both thighs were stabilized using hook-and-loop straps. The rotational axis of the dynamometer was aligned with the transverse knee-joint axis and connected to the point of force application at the distal end of the tibia 5 cm above the lateral malleolus using a length-adjustable rigid lever arm. In this position, the dynamometer passively extended the knee at 5°/s to the endpoint of maximal discomfort without pain. The PRT result and knee ROM were recorded for further passive-stiffness calculation. Range of motion was defined as the maximal knee-extension angle from the initial position (0°) and PRT at maximal discomfort. The procedure was repeated 3 times, with 1 minute of rest after each passive knee extension. After the second knee extension, the end position was held for 60 seconds, and the torque decline was recorded as the SRT result. The measurements were reliable throughout the trials: the ICC for the knee ROM was 0.993 (95% CI = 0.965, 0.997) and for PRT was 0.985 (95% CI = 0.967, 0.993).
Active Knee-Joint Position Sense
After the PST, we used the isokinetic dynamometer to measure AKJPS. To avoid visual input, the participant was blindfolded for the duration of the test. The starting position was 15° of knee flexion (0° corresponded to full knee extension). The leg was moved passively (flexed) at a speed of 10°/s to 45° of knee-joint flexion, and this position was held for 5 seconds. The participant was instructed to remember this position. Next, the lever on the dynamometer was released, and the investigator (A.S.) again lifted the limb to the starting position. The individual was instructed to actively reproduce the predetermined target angle using the same limb. After reaching this estimated angle, the participant stopped the dynamometer motion by pressing a button. The AKJPS test consisted of 3 trials, with a 15-second rest between trials. The AKJPS was calculated as the absolute error between the target and estimated position.23 The average of the 3 trials was used for statistical analysis. The measurements were reliable throughout the trials: the ICC of the AKJPS measurements was 0.801 (95% CI = 0.637, 0.899).
Interventions
Participants performed the FR and NDNG interventions using their right limb. The FR and NDNG procedures consisted of 6 sets of 45 seconds, with a 15-second rest between sets. The procedures were based on literature reviews of FR24 and NDNG.20,22
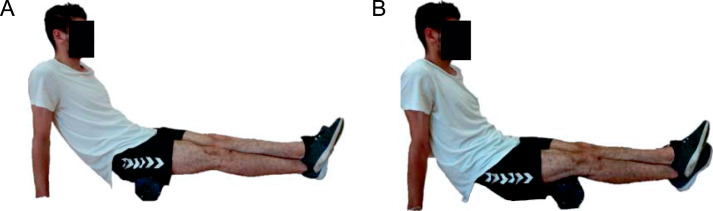
Foam Rolling
The FR intervention was performed using a smooth-surface, moderately firm foam roller (length = 45.15 cm; diameter = 15.24 cm; The Mad Group [HQ] Ltd). Participants rolled the right limb from the ischial tuberosity to the knee, moving the body backward and forward over the roller, with the left limb placed over the right limb. The hands were set on the floor and did not move during the rolling motion (Figure 1). The investigator (M.M.Z.A.) used a numeric rating scale (0 representing no discomfort and 10 representing maximal discomfort) to control participants' intensity of pressure during the intervention (discomfort was rated 5/10).25 Participants performed rolling at a frequency of 20 cycles per minute using 1.5 seconds for each rolling direction, resulting in 15 complete rolling cycles in 45 seconds. An investigator (G.K.) carefully controlled the movement execution and velocity using a chronometer.
Figure 1.
The foam-rolling technique. The participant was instructed to move his body backward and forward over the roller to apply pressure to the posterior aspect of the thigh. He set his hands on the floor and did not move them during the rolling motion. With the left limb placed over the right limb, the participant rolled the right limb, A, from the ischial tuberosity, B, to the back of the knee.
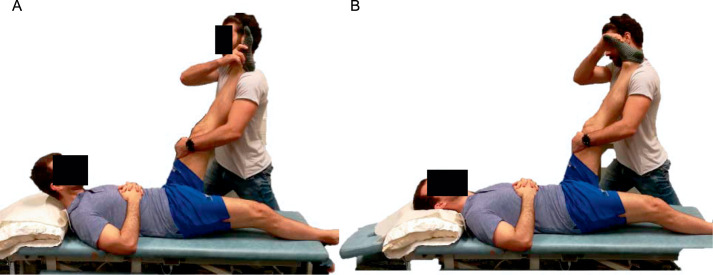
Neurodynamic Nerve Gliding
Neurodynamic nerve gliding is a neural mobilization method in which one end of the neural tissue is elongated while the other is relaxed, and then the sequence is reversed.22 It can be performed by the individual, but in this study, for standardization purposes, the same researcher (R.M.K.) applied NDNG to all participants.22 The individual was in the supine position with a slightly flexed cervical and thoracolumbar spine supported by a cushion (Figure 2). The investigator flexed the hip joint up to 90°, maintaining neutral position of the ankle, and pushed the knee joint into extension to reach the maximal tolerable stretch of the hamstrings. After the maximal stretch was achieved, the participant bent the head forward to increase cervical spine flexion as the investigator plantarflexed the foot. The individual then bent the head backward and extended the cervical spine while the investigator dorsiflexed the foot.
Figure 2.
The neurodynamic nerve-gliding technique. The participant was positioned supine with a slightly flexed cervical and thoracolumbar spine supported by a cushion. A, The participant bent his head forward to increase cervical spine flexion, and the investigator plantarflexed the foot. B, The participant then bent his head backward to extend the cervical spine, and the investigator dorsiflexed the foot.
Data Analysis
Angle and torque obtained using the dynamometer, as well as EMG signals, were synchronized and recorded using the Biopac MP100 acquisition system and AcqKnowledge software. Before calculating hamstrings passive stiffness, we estimated muscle activity during passive stretching. Measurements were accepted only if the activity of the knee flexors and extensors was <5% of the maximal EMG value.2
The EMG Analysis
The EMG signals were filtered with a bandpass of 10 to 500 Hz using a fourth-order Butterworth filter. The EMG amplitude was transformed into a root mean square value by integrating the moving average filter with a 0.03-second width. The maximal EMG value was quantified by calculating the root mean square over a 0.05-second period around the peak torque achieved during MVICs of the knee flexors and extensors.
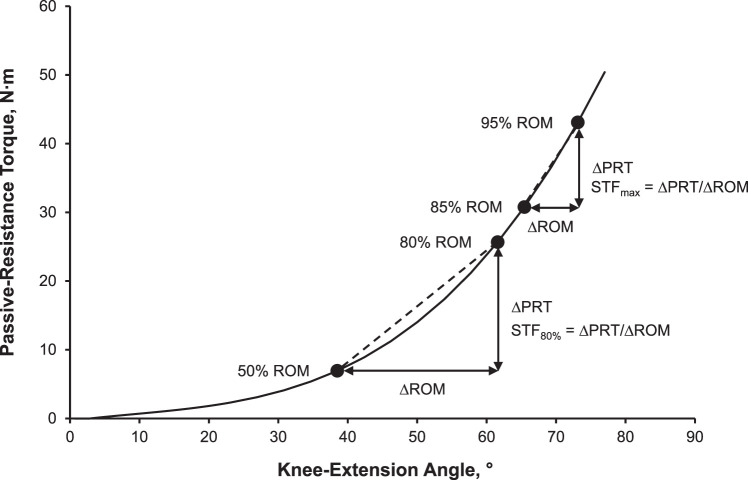
Passive Stiffness
The passive torque–angle relationship was fitted to a third-degree polynomial using the least-squares method, and the R2 value was used to evaluate the fit. Passive hamstrings stiffness (STF) was defined as the change in PRT (in newton meters), with gravity correction for the weight of the lower limb, divided by the change in ROM (in degrees; ΔPRT/ΔROM).4 Stiffness was calculated as the PRT-angle curve slope: from 85% to 95% (STFmax) and from 50% to 80% (STF80%) of maximal knee-extension ROM before and after FR and NDNG (Figure 3). Calculation of the ICCs showed that intraexaminer reliability was high for both measures assessed: 0.943 (95% CI = 0.66, 0.981) for STFmax and 0.956 (95% CI = 0.917, 0.978) for STF80%.
Figure 3.
An example of a passive-resistance torque-angle curve relationship during passive stretching. Passive stiffness was defined as the change in passive-resistance torque (ΔPRT) divided by the change in range of motion (ΔROM; ΔPRT/ΔROM) and was expressed as the slope of the torque-angle curve in the middle (STF80%) and end (STFmax) of joint ROM.
Stress-Relaxation Behavior
The decline in PRT was recorded during the SRT as a measure of hamstrings viscosity. The time course of stress relaxation was carefully fitted using a double exponential function of the form
 |
where T is the PRT (in newton meters); t is the stretch time (in seconds); and A, B, C,  1, and
1, and  2 are the constants obtained from the nonlinear regression (in newton meters for A, B, and C and in seconds for
2 are the constants obtained from the nonlinear regression (in newton meters for A, B, and C and in seconds for  1 and
1 and  2).26
2).26
We used a double exponential function to fit the stress-relaxation data to the equation with the nonlinear regression Solver facility in Excel (version 2016; Microsoft Corp). The constants in the double-exponential equation have the following physical meanings: A is the residual torque remaining after an infinite stretch duration, and B and C describe the decline in torque at an infinite stretch duration attributable to each of the 2 components of the decline in PRT. The time constant  1 describes how fast the stress is relaxed from its initial to equilibrium value (63% of the total change), and
1 describes how fast the stress is relaxed from its initial to equilibrium value (63% of the total change), and  2 describes the time taken for stress to decline to 1/e (or by 36.7% of its initial value).
2 describes the time taken for stress to decline to 1/e (or by 36.7% of its initial value).
Statistical Analysis
We analyzed all data using IBM SPSS (version 22; IBM Corp). The Shapiro-Wilk test was calculated to check for normal distribution, and all of the data were found to be normally distributed. Two-way analysis of variance with repeated measures was conducted to identify the effects of the intervention (FR or NDNG) and time (baseline, postintervention) on the dependent variables (STFmax, STF80%, SLR, knee-extension ROM, SRT, PRT, AKJPS). When appropriate, the follow-up test included paired-samples t tests to identify differences between means. We determined partial η2 as a measure of the effect sizes in repeated-measures statistics, by which interactions between the interventions (FR or NDNG) and time (baseline, postintervention) were estimated. The effect size for a paired-samples t test (assessment of the treatment's effectiveness) was estimated using the Cohen dz, calculated by dividing the mean paired difference by the SD of the difference. We identified the test-retest reliability of the selected variables using absolute-agreement ICC (2,1) with a 95% CI between baseline scores of the first and second sessions. The α level was set at .05 for all analyses.
RESULTS
Passive Stiffness and Flexibility
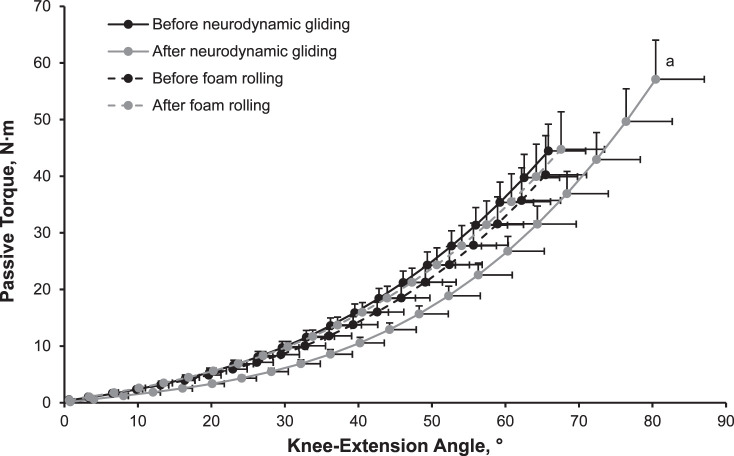
Interactions between time and intervention were found for STFmax (F1,17 = 5.024, P = .042, ηp2 = 0.264), passive knee-extension ROM (F1,17 = 7.371, P = .02, ηp2 = 0.345), and PRT (F1,17 = 4.876, P = .044, ηp2 = 0.258). The NDNG induced increases in STFmax (t17 = 2.374, P = .03, dz = 0.56), ROM (t17 = 2.843, P = .01, dz = 0.67; Figure 4), and PRT (t17 = 2.982, P = .008, dz = 0.70), but FR produced no changes (Table 1). For hip-flexion angle assessed using SLR, we observed no interaction between time and intervention (P > .05, ηp2 = 0.003). A time effect was present for both NDNG and FR (F1,17 = 87.415, P < .001, ηp2 = 0.862) as SLR measurements increased.
Figure 4.
The passive-resistance torque–angle (range-of-motion) relationship was determined at baseline and immediately after neurodynamic nerve gliding and foam rolling. Data are expressed as mean ± SE of the mean. a Statistical maximum range-of-motion difference from the baseline measure (P = .01).
Table 1.
Hamstrings Flexibility, Stiffness, and Active Knee-Joint Position Sense Before and After Foam Rolling and Neurodynamic Gliding, Mean ± SD
| Technique |
Passive Stiffness During Maximal Knee-Extension Range of Motion, N·m/° |
Hip-Flexion Angle During Passive-Resistance Straight-Leg Raise Test, ° |
Knee Range of Motion, ° |
Peak Passive-Resistance Torque, N·m |
Average Absolute Error for Active Knee-Joint Position Sense, ° |
|
| Between 50% and 80% |
Between 85% and 95% |
|||||
| Foam rolling | ||||||
| Baseline | 0.80 ± 0.22 | 1.31 ± 0.43 | 71 ± 6 | 63 ± 15 | 42 ± 15 | 4.7 ± 2.8 |
| Immediately after | 0.82 ± 0.25 | 1.36 ± 0.48 | 77 ± 6b | 63 ± 17 | 44 ± 18 | 5.3 ± 3.5 |
| Neurodynamic gliding | ||||||
| Baseline | 0.82 ± 0.16 | 1.32 ± 0.31 | 71 ± 5 | 64 ± 17 | 42 ± 13 | 5.5 ± 2.7 |
| Immediately after | 0.91 ± 0.21 | 1.59 ± 0.44a | 77 ± 6b | 73 ± 20a | 54 ± 20a | 5.7 ± 5.0 |
Different from baseline (P < .05).
Different from baseline (P < .01).
Stress-Relaxation Behavior
We noted no interaction between time and intervention (P > .05) for the stress-relaxation behavior (coefficient A, B, C, τ1, and τ2). No change in viscoelasticity was seen after FR or NDNG compared with baseline (P values > .05; Table 2).
Table 2.
Constants in the Viscoelastic Model of the Hamstrings Muscle During the Stress-Relaxation Test Before and After Foam Rolling and Neurodynamic Gliding, Mean ± SD
| Technique |
N·m |
τ1, s |
τ2, s |
||
|
A
|
B
|
C
|
|||
| Foam rolling | |||||
| Baseline | 28.6 ± 12.0 | 9.1 ± 4.4 | 3.0 ± 1.7 | 35.6 ± 20.1 | 2.9 ± 1.8 |
| Immediately after | 30.7 ± 15.9 | 8.2 ± 3.0 | 2.9 ± 1.6 | 34.7 ± 19.1 | 2.3 ± 1.2 |
| Neurodynamic gliding | |||||
| Baseline | 31.4 ± 11.6 | 7.5 ± 3.3 | 3.2 ± 2.2 | 28.5 ± 15.7 | 3.1 ± 1.8 |
| Immediately after | 34.4 ± 12.9 | 8.5 ± 2.2 | 4.1 ± 2.2 | 40.7 ± 13.1 | 2.8 ± 1.6 |
Abbreviations: A, the residual passive torque remaining after an infinite stretch duration; B and C, the decline in torque at the infinite stretch duration attributable to each of the 2 components of the decline in torque; τ1, the time constant describing how fast the stress relaxed from its initial to equilibrium value (63% of the total change); τ2, the time constant describing the time taken for stress decline to 1/e (or by 37% of its initial value).
Active Knee-Joint Position Sense
For AKJPS, we identified no interaction between time and intervention (P > .05). The average absolute error of AKJPS after FR and NDNG did not differ from baseline (P values > .05; Table 1).
DISCUSSION
We investigated the immediate effect of FR and NDNG on hamstrings passive stiffness, viscoelasticity, flexibility, and proprioception to inform the design of a warm-up routine for soccer players. Both FR and NDNG substantially increased straight-leg hip-flexion amplitude, but only NDNG increased knee ROM in unfavorable positions during knee extension when the pressure on neural tissues was high. This finding may be important for soccer players because NDNG affected passive stiffness and knee-extension ROM to a larger extent than FR and could be more advantageous than and preferable to FR as part of a warm-up in soccer players.
Passive Stiffness and Flexibility
Foam rolling has become increasingly popular in the last decade as part of warm-up in sport settings. Researchers27 suggested that FR in warm-up could increase performance among soccer players. These athletes typically start a warm-up routine using FR, followed by stretching and dynamic sport-specific work with the ball. The belief is that FR releases tension in their muscles, thus ensuring greater ROM. However, the findings have been contradictory, and whether FR improves hamstrings flexibility is unclear. Investigators who measured flexibility using the change in hip ROM during the SLR test28 or sit-and-reach test29 found that FR increased flexibility. Other authors16,18 evaluated flexibility using knee ROM and noted no effect of FR. We also obtained contradictory results, with increases in ROM but only for SLR, and we observed that the position of the hip and knee joints during the measurements must be considered when assessing the effects of FR. Clinical assessment has shown that active knee extension, one of the most common measures of apparent hamstrings tightness, correlates poorly with other measures such as passive SLR, sit-and-reach, and fingertip-to-floor tests.30
The most striking result of our study was that NDNG increased ROM in hip flexion (7.80% ± 5.78%) and knee extension (15.08% ± 15.03%). This technique is assumed to improve passive knee ROM and SLR angle by increasing nerve excursion and reducing nerve irritation.19 However, different stretching techniques demonstrated differences in longitudinal sciatic nerve excursion.31 The sliding technique and passive knee extension with a bent hip resulted in distal nerve excursion; hip flexion during the passive SLR resulted in proximal nerve excursion. These divergences may explain why both SLR angle and knee ROM increased after NDNG but ROM remained unchanged after FR.
In our research, FR increased the SLR angle without changing hamstrings stiffness, and this finding may be explained by increased stretch tolerance.17 Foam rolling is an intensive self-treatment that is thought to mimic the effects of manual therapy techniques. The pressure applied during the rolling motion stretches the soft tissues and induces myofascial relaxation. Fascia is populated by a dense network of mechanoreceptors, such as Meissner corpuscles, Ruffini cylinders, Pacinian corpuscles, and Merkel receptors.32 Stimulation of the Ruffini and Pacinian receptors via FR may induce muscle relaxation by inhibiting sympathetic activity, but an FR exercise session should last at least 15 minutes.33 Ischemic compression and passive stretching reduce pain perception34 and may increase stretch tolerance, pain tolerance, or both at the end ROM after FR, which should allow greater joint excursion. In addition, the pressure applied during the rolling motion stretches the soft tissues and induces myofascial relaxation, which improves myofascial mobility by increasing fascial sliding without a change in muscle stiffness.11
We found that the ROM–PRT curve after NDNG shifted to the right: stiffness decreased in the first part of stretching, slightly increased in the middle part of ROM, and increased substantially at the end of ROM (Figure 4). Such a pattern of increased PRT could be attributed to the peripheral nerve tissue's resistance to stretching.35 The primary theoretical objective of NDNG is to restore the dynamic balance between the relative movement of neural tissues and the surrounding mechanical interfaces by reducing pressure on the neural tissue and promoting optimal physiological function.19 Then, because of free sliding of the nerves, NDNG could decrease PRT at the beginning of the stretch and increase it at the end of the stretch. Yet we did not measure sliding of the peripheral nerves or fascial layers, so these assumptions are speculative.
Stress-Relaxation Behavior
We identified no interaction between time and intervention for stress-relaxation behavior, indicating that stress relaxation was affected similarly by FR and NDNG. In contrast to our findings, some researchers15,16 have reported a short-term decrease in the shear modulus after FR. These results could be based on tissue thixotropy,12 which occurs when viscous (thicker) fluids become less viscous or more fluidlike when agitated, sheared, or stressed. According to Fadnes et al,36 under intense stimulation, plasma may extrude from the blood vessels into the interstitial fluid matrix and increase the viscosity of the extracellular matrix. Given that FR increases blood flow37 and improves vascular function,38 it likely increases muscle viscosity, which should reduce shear-wave speed and cause a short-term decrease in the shear modulus (index of stiffness).15,16
Our work did not confirm the effect of FR or NDNG on muscle viscosity. A change in the mechanical properties of fascia occurs after application of a large force (causing a large deformation and tearing of tissue) or a smaller force for a long time.32 We found that the duration of FR and NDNG was relevant to the specific warm-up of athletes (6 sets of 45 seconds with a 15-second rest between sets). During FR, the compressive force was not greater than body weight, and no pain (overstretch) occurred during NDNG or passive stretching. These circumstances led us to assume that FR and NDNG can alter the mechanical properties of hamstrings during the warm-up only when the intervention lasts longer than in our study, reaches higher pressures, or results in overstretching of tissue. Again, the SRT performed via the passive-stretching muscle-tendon unit we used may be less sensitive to muscle-fluid changes compared with shear-wave elastography.15,16
Active Knee-Joint Position Sense
Mechanoreceptors are thought to mediate the sensation of joint motion.39 Therefore, we expected that their stimulation during FR would affect AKJPS. However, neither FR nor NDNG affected AKJPS. The single session of hamstrings FR with the moderately firm foam roller may have been insufficient to elicit a neurologic response at the knee. Our results are consistent with those of Romero-Franco et al18 but contradict those of Lee et al,40 who performed FR on both the hamstrings and quadriceps. These differences may thus reflect the importance of antagonist muscles for knee-joint position sense and suggest that FR affects knee-joint position sense only when it is performed on both knee flexors and extensors.
Clinical Implications
We demonstrated that NDNG may be preferable to FR as part of a warm-up for athletes seeking an immediate increase in hamstrings flexibility involving the proximal and distal parts of the muscle, increasing mobility during knee extension with a bent hip. The NDNG technique can reduce the substantial stress placed on the neural tissue and muscle fibers and increase joint mobility during specific actions, such as sprinting and kicking with a large limb swing.
Limitations
The lack of information about the effects of FR and NDNG on muscle strength and specific soccer performance can be viewed as a limitation. Adding more direct estimates of the changes in fascial sliding and peripheral nerve stress would have provided better interpretations of the effects of FR and NDNG. In addition, we studied only young, healthy male athletes who did not report muscle pain or joint-motion restrictions; we did not assess female soccer players.
CONCLUSIONS
Both FR and NDNG had immediate positive effects on hamstrings flexibility in young soccer players. The NDNG technique had advantages for movements involving increased pressure on the neural tissue. Our findings suggested that coaches should be encouraged to include NDNG in the warm-up routine.
REFERENCES
- 1.Zhang L, Li H, Garrett WE, Liu H, Yu B. Hamstring muscle-tendon unit lengthening and activation in instep and cut-off kicking. J Biomech . 2020;99:109482. doi: 10.1016/j.jbiomech.2019.109482. [DOI] [PubMed] [Google Scholar]
- 2.Muanjai P, Jones DA, Mickevicius M, et al. The acute benefits and risks of passive stretching to the point of pain. Eur J Appl Physiol . 2017;117(6):1217–1226. doi: 10.1007/s00421-017-3608-y. [DOI] [PubMed] [Google Scholar]
- 3.Weppler CH, Magnusson SP. Increasing muscle extensibility: a matter of increasing length or modifying sensation? Phys Ther . 2010;90(3):438–449. doi: 10.2522/ptj.20090012. [DOI] [PubMed] [Google Scholar]
- 4.Cabido CET, Bergamini JC, Andrade AGP, Lima FV, Menzel HJ, Chagas MH. Acute effect of constant torque and angle stretching on range of motion, muscle passive properties, and stretch discomfort perception. J Strength Cond Res . 2014;28(4):1050–1057. doi: 10.1519/JSC.0000000000000241. [DOI] [PubMed] [Google Scholar]
- 5.Nordez A, Gross R, Andrade R, et al. Non-muscular structures can limit the maximal joint range of motion during stretching. Sports Med . 2017;47(10):1925–1929. doi: 10.1007/s40279-017-0703-5. [DOI] [PubMed] [Google Scholar]
- 6.Rickett T, Connell S, Bastijanic J, Hegde S, Shi R. Functional and mechanical evaluation of nerve stretch injury. J Med Syst . 2011;35(5):787–793. doi: 10.1007/s10916-010-9468-1. [DOI] [PubMed] [Google Scholar]
- 7.Silva A, Manso A, Andrade R, Domingues V, Brandao MP, Silva AG. Quantitative in vivo longitudinal nerve excursion and strain in response to joint movement: a systematic literature review. Clin Biomech (Bristol Avon) . 2014;29(8):839–847. doi: 10.1016/j.clinbiomech.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 8.Topp KS, Boyd BS. Structure and biomechanics of peripheral nerves: nerve responses to physical stresses and implications for physical therapist practice. Phys Ther . 2006;86(1):92–109. doi: 10.1093/ptj/86.1.92. [DOI] [PubMed] [Google Scholar]
- 9.Rade M, Shacklock M, Könönen M, et al. Normal multiplanar movement of the spinal cord during unilateral and bilateral straight leg raise: quantification, mechanisms, and overview. J Orthop Res . 2017;35(6):1335–1342. doi: 10.1002/jor.23385. [DOI] [PubMed] [Google Scholar]
- 10.Andrade RJ, Freitas SR, Vaz JR, Bruno PM, Pezarat-Correia P. Provocative mechanical tests of the peripheral nervous system affect the joint torque-angle during passive knee motion. Scand J Med Sci Sports . 2015;25(3):338–345. doi: 10.1111/sms.12250. [DOI] [PubMed] [Google Scholar]
- 11.Krause F, Wilke J, Niederer D, Vogt L, Banzer W. Acute effects of foam rolling on passive stiffness, stretch sensation and fascial sliding: a randomized controlled trial. Hum Mov Sci . 2019;67:102514. doi: 10.1016/j.humov.2019.102514. [DOI] [PubMed] [Google Scholar]
- 12.Behm DG, Wilke J. Do self-myofascial release devices release myofascia? rolling mechanisms: a narrative review. Sports Med . 2019;49(8):1173–1181. doi: 10.1007/s40279-019-01149-y. [DOI] [PubMed] [Google Scholar]
- 13.Su H, Chang N-J, Wu W-L, Guo L-Y, Chu I-H. Acute effects of foam rolling, static stretching, and dynamic stretching during warm-ups on muscular flexibility and strength in young adults. J Sport Rehabil . 2017;26(6):469–477. doi: 10.1123/jsr.2016-0102. [DOI] [PubMed] [Google Scholar]
- 14.Wilke J, Niemeyer P, Niederer D, Schleip R, Banzer W. Influence of foam rolling velocity on knee range of motion and tissue stiffness: a randomized, controlled crossover trial. J Sport Rehabil . 2019;28(7):711–715. doi: 10.1123/jsr.2018-0041. [DOI] [PubMed] [Google Scholar]
- 15.Mayer I, Hoppe MW, Freiwald J, et al. Different effects of foam rolling on passive tissue stiffness in experienced and nonexperienced athletes. J Sport Rehabil . 2019;29(7):926–933. doi: 10.1123/jsr.2019-0172. [DOI] [PubMed] [Google Scholar]
- 16.Morales-Artacho AJ, Lacourpaille L, Guilhem G. Effects of warm-up on hamstring muscles stiffness: cycling vs foam rolling. Scand J Med Sci Sports . 2017;27(12):1959–1969. doi: 10.1111/sms.12832. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura M, Onuma R, Kiyono R, et al. The acute and prolonged effects of different durations of foam rolling on range of motion, muscle stiffness, and muscle strength. J Sports Sci Med . 2021;20(1):62–68. doi: 10.52082/jssm.2021.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romero-Franco N, Romero-Franco J, Jiménez-Reyes P. Jogging and practical-duration foam-rolling exercises and range of motion, proprioception, and vertical jump in athletes. J Athl Train . 2019;54(11):1171–1178. doi: 10.4085/1062-6050-474-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellis RF, Hing WA. Neural mobilization: a systematic review of randomized controlled trials with an analysis of therapeutic efficacy. J Man Manip Ther . 2008;16(1):8–22. doi: 10.1179/106698108790818594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nee RJ, Butler D. Management of peripheral neuropathic pain: integrating neurobiology, neurodynamics, and clinical evidence. Phys Ther Sport . 2006;7(1):36–49. doi: 10.1016/j.ptsp.2005.10.002. [DOI] [Google Scholar]
- 21.De-la-Llave-Rincon AI, Ortega-Santiago R, Ambite-Quesada S, et al. Response of pain intensity to soft tissue mobilization and neurodynamic technique: a series of 18 patients with chronic carpal tunnel syndrome. J Manipulative Physiol Ther . 2012;35(6):420–427. doi: 10.1016/j.jmpt.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Castellote-Caballero Y, Valenza MC, Martín-Martín L, Cabrera-Martos I, Puentedura EJ, Fernández-de-las-Peñas C. Effects of a neurodynamic sliding technique on hamstring flexibility in healthy male soccer players: a pilot study. Phys Ther Sport . 2013;14(3):156–162. doi: 10.1016/j.ptsp.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 23.Walsh GS. Effect of static and dynamic muscle stretching as part of warm up procedures on knee joint proprioception and strength. Hum Mov Sci . 2017;55:189–195. doi: 10.1016/j.humov.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 24.Hendricks S, Hayd'n H, den Hollander S, Lombard W, Parker R. Effects of foam rolling on performance and recovery: a systematic review of the literature to guide practitioners on the use of foam rolling. J Bodyw Mov Ther . 2020;24(2):151–174. doi: 10.1016/j.jbmt.2019.10.019. [DOI] [PubMed] [Google Scholar]
- 25.Krause F, Wilke J, Niederer D, Vogt L, Banzer W. Acute effects of foam rolling on passive tissue stiffness and fascial sliding: study protocol for a randomized controlled trial. Trials . 2017;18(1):114. doi: 10.1186/s13063-017-1866-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duong B, Low M, Moseley AM, Lee RY, Herbert RD. Time course of stress relaxation and recovery in human ankles. Clin Biomech (Bristol Avon) . 2001;16(7):601–607. doi: 10.1016/s0268-0033(01)00043-2. [DOI] [PubMed] [Google Scholar]
- 27.D'Andrea JD, Wicke J, Kleber F. Foam rolling as a warm-up technique for anaerobic power activities. Int J Sports Exerc Med . 2017;3(5):077. doi: 10.23937/2469-5718/1510077. [DOI] [Google Scholar]
- 28.Madoni SN, Costa PB, Coburn JW, Galpin AJ. Effects of foam rolling on range of motion, peak torque, muscle activation, and the hamstrings-to-quadriceps strength ratios. J Strength Cond Res . 2018;32(7):1821–1830. doi: 10.1519/JSC.0000000000002468. [DOI] [PubMed] [Google Scholar]
- 29.Sullivan KM, Silvey DBJ, Button DC, Behm DG. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther . 2013;8(3):228–236. [PMC free article] [PubMed] [Google Scholar]
- 30.Hansberger BL, Loutsch R, Hancock C, Bonser R, Zeigel A, Baker RT. Evaluating the relationship between clinical assessments of apparent hamstring tightness: a correlational analysis. Int J Sports Phys Ther . 2019;14(2):253–263. [PMC free article] [PubMed] [Google Scholar]
- 31.Coppieters MW, Andersen LS, Johansen R, et al. Excursion of the sciatic nerve during nerve mobilization exercises: an in vivo cross-sectional study using dynamic ultrasound imaging. J Orthop Sports Phys Ther . 2015;45(10):731–737. doi: 10.2519/jospt.2015.5743. [DOI] [PubMed] [Google Scholar]
- 32.Schleip R. Fascial plasticity—a new neurobiological explanation, part 1. J Bodyw Mov Ther . 2003;7(1):11–19. doi: 10.1016/S1360-8592(02)00067-0. [DOI] [Google Scholar]
- 33.Lastova K, Nordvall M, Walters-Edwards M, Allnutt A, Wong A. Cardiac autonomic and blood pressure responses to an acute foam rolling session. J Strength Cond Res . 2018;32(10):2825–2830. doi: 10.1519/JSC.0000000000002562. [DOI] [PubMed] [Google Scholar]
- 34.Kostopoulos D, Nelson AJ, Jr, Ingber RS, Larkin RW. Reduction of spontaneous electrical activity and pain perception of trigger points in the upper trapezius muscle through trigger point compression and passive stretching. J Musculoskelet Pain . 2008;16(4):266–278. doi: 10.1080/10582450802479594. [DOI] [Google Scholar]
- 35.McHugh MP, Johnson CD, Morrison RH. The role of neural tension in hamstring flexibility. Scand J Med Sci Sports . 2012;22(2):164–169. doi: 10.1111/j.1600-0838.2010.01180.x. [DOI] [PubMed] [Google Scholar]
- 36.Fadnes HO, Reed RK, Aukland K. Mechanisms regulating interstitial fluid volume. Lymphology . 1978;11(4):165–169. [PubMed] [Google Scholar]
- 37.Hotfiel T, Swoboda B, Krinner S, et al. Acute effects of lateral thigh foam rolling on arterial tissue perfusion determined by spectral doppler and power doppler ultrasound. J Strength Cond Res . 2017;31(4):893–900. doi: 10.1519/JSC.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 38.Okamoto T, Masuhara M, Ikuta K. Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res . 2014;28(1):69–73. doi: 10.1519/JSC.0b013e31829480f5. [DOI] [PubMed] [Google Scholar]
- 39.Ergen E, Ulkar B. Frontera WR, Herring SA, Micheli LJ, Silver JK, Young TP, editors. Proprioception and coordination. In. Clinical Sports Medicine: Medical Management and Rehabilitation. Elsevier Inc; 2007. pp. 237–255. eds. [DOI]
- 40.Lee C-L, Chu I-H, Lyu B-J, Chang W-D, Chang N-J. Comparison of vibration rolling, nonvibration rolling, and static stretching as a warm-up exercise on flexibility, joint proprioception, muscle strength, and balance in young adults. J Sports Sci . 2018;36(22):2575–2582. doi: 10.1080/02640414.2018.1469848. [DOI] [PubMed] [Google Scholar]