Abstract
Individuals with Methicillin-Resistant Staphylococcus aureus (MRSA) colonized nasal cavities were at greater risk of developing the infection and can serve as potential reservoirs of transmission. Aim of this study is to determine the extent of nasal carriage and associated factors linked to MRSA in medical and health science students of Arba Minch University (AMU), Ethiopia, who are much prone. An institution based cross-sectional study was conducted at AMU from 01st August through 30th November, 2020 by means of a systematic sampling technique using a structured questionnaire. Nasal swabs samples were collected and S. aureus were identified following standard microbiological methods. Methicillin resistance was tested using cefoxitin disk and antimicrobial susceptibility tests were performed by Kirby-Bauer disk diffusion. Biofilm forming ability was phenotypically detected by micro-titer plate assay. Descriptive statistics and multivariable logistic regression analysis were done by Statistical Package for Social Service (SPSS) version 25. The overall prevalence of Staphylococcus aureus and MRSA were 27.1% (70/258) and 7.4% (19/258) respectively. Methicillin-Resistant S. aureus carriage were higher among medical interns, 16.9% (11/65). Isolates in general were co-resistant to antibiotics, such as trimethoprim-sulfamethoxazole (63.2%) and tetracycline (48.4%). Multidrug resistance (MDR) were observed among 52.6% (10/19) of the isolates. Besides, 31.4% (6/19) of MRSA were biofilm producers and all of them were MDR. Multivariable analysis showed that mean exposure for > 2 years to hospital settings [p = 0.048, AOR: 4.99, 95% CI 1.01–24.66] and the habit of sharing clothing and sports equipment [p = 0.017, AOR: 5.43, 95% CI 1.35–21.83] were statistically significant. The overall prevalence of nasal colonized MRSA among students were comparatively lower than that observed in other studies done in Ethiopia itself. An alarming factor is that, 60% of MDR-MRSA were biofilm producers.
Subject terms: Microbiology, Antimicrobials, Bacteriology
Introduction
Methicillin-resistant Staphylococcus aureus includes any strain of S. aureus that has developed resistance to β-lactam antibiotics. The organism acquires resistance via the incorporation of a mecA gene into its chromosome at a specific site; mecA encodes an alternative penicillin-binding protein that has low affinity towards semisynthetic penicillins, including methicillin, nafcillin, and oxacillin agents1.
Now a days MRSA is a major threat to the public health, in countries where HIV/AIDS, malaria, tuberculosis, malnutrition, crowded living, change in climate contribute to an increased risk of Staphylococcal infections2. Methicillin-resistant S. aureus has been categorized into three main types, namely healthcare-acquired, community and livestock-associated based on its involvement, and can result in nosocomial, community and livestock-associated infections respectively3.
Colonization by MRSA is a well-known risk factor in developing infections both in adults and children. This is especially true in the case of patients who acquire MRSA from hospital settings where the risk of developing an infection is around 30%4. Strains of MRSA are usually spread by direct skin-to-skin contacts and may occur during hospital admissions, transfer, or other healthcare-related contacts; however, the roles of shared public spaces (e.g., dormitories, gym, barracks, etc.) were also noted5. It is reported that close contacts with a person already colonized or infected with MRSA can result in a 7.5-fold greater risk of becoming colonized. Persons colonized with MRSA are an increased risk of developing the infection and can serve as a source of transmission6.
The nose (anterior nasal mucosa) is known to be the primary ecological reservoir of MRSA in humans and is a main risk factor causing infections in various clinical settings. Several surfaces in hospital environments, gowns of healthcare workers, and patient-care items contaminated or colonized with MRSA have been shown to contribute to the risk of transmission7. Since medical students have long period of hospital stay, it is envisaged that they are also at greater risk of nasal colonization by MRSA, as in the case of health care workers.
Biofilm formation is an important virulence factors. Large biofilm-like bacterial aggregates including S. aureus and other species were found in the mucosal samples taken from patients with chronic rhino-sinusitis8. In addition, a recent study done in Arba Minch reported that biofilm forming nasal isolates of MRSA were more resistant than their non-biofilm-forming counterparts9.
As healthcare workers are commonly exposed to patients in their work set-up, it is important to assess the rate of prevalence of MRSA carriage to evaluate the extent of preventive and control measures to be taken, which can limit the spread. Accurate susceptibility testing is essential to be formulated much in advance of selecting empirical treatment strategies in the case of an unexpected outbreak. Different surveillance policies for detection of carriage and/or decolonization have been proven to be effective in minimizing the rate of infections. Elucidation of the prevalence of MRSA carriage and studies on the profiles of antibiotic susceptibility are pivotal. However, all over Africa, there exists no strict surveillance system or an effective control program to deal MRSA, which further worsen the menace.
As of now, only limited number of studies are carried out in the national level regarding the nasal carriage of MRSA, especially among medical and health science students. Furthermore, research on the ability of MRSA to form biofilm is not done extensively. Therefore, the present study is aimed at determining the extent of nasal carriage of MRSA, its antibiotics susceptibility, ability to form biofilm and associated factors, among the medical and health science students of AMU.
Results
Socio-demographic characteristics
A total of 258 participants were enrolled with a response rate of 100%. Of these, 72.9% (n = 188) were males. The age of study participants ranged from 21 to 27, with a mean value of 23 ± 1.13. With regard to the proportion of health science students among the total participants, 10.8% (n = 28) were from the department of nursing, 10.5% (n = 27) from health officers, 8.9% (n = 23) from midwifery, 8.5% (n = 22) from medical laboratory, 4.7% (n = 12) from anesthetic, and 4.3% (n = 11) from radiology. The study population is re-grouped into three categories such as medical interns, clinical and health science students for the convenience of statistical analysis (Table1).
Table 1.
Socio-demographic, clinical and behavioral characteristics of medicine and health science students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
| Variables | Frequency | Percentage (%) | |
|---|---|---|---|
| Sex | Male | 188 | 72.9 |
| Female | 70 | 27.1 | |
| Age | Less than 24 | 172 | 66.6 |
| 24 and above | 86 | 33.3 | |
| Category of students | Clinical and OHS students | 193 | 74.8 |
| Medical intern | 65 | 25.2 | |
| Mean exposure to hospital | Less than 6 months | 98 | 38.0 |
| 6 months to 1 year | 60 | 23.3 | |
| 1 to 2 years | 35 | 13.6 | |
| Greater than 2 years | 65 | 25.1 | |
| Nose picking habit | Yes | 125 | 48.4 |
| No | 133 | 51.6 | |
| Use of gloves while handling patients | Always | 63 | 24.4 |
| Sometimes | 140 | 54.3 | |
| Rarely | 55 | 21.3 | |
| Antibiotic use (last three months) | Yes | 13 | 5.0 |
| No | 245 | 95.0 | |
| Ways of antibiotic usage | Full course | 257 | 99.6 |
| Incomplete course | 1 | 0.4 | |
| Visiting gymnasium | Yes | 64 | 24.8 |
| No | 194 | 75.2 | |
| Sharing of clothing | Yes | 65 | 25.2 |
| No | 193 | 74.8 | |
| Participate in invasive procedures | Yes | 150 | 58.1 |
| No | 108 | 41.9 | |
Clinical and behavioral characteristics
Out of 258 participants, 25.1% (n = 65) were medical interns and had exposure for more than 2 years in the hospital, 54.3% (n = 140) of them use gloves sometimes while handling patients; 51.6% (n = 133) are devoid of the habit of nose picking. On the other hand, 24.8% (n = 64) participate in sports or visit gymnasium. About 58% (n = 150) had indulged in invasive procedures and 58.9% (n = 152) of them were accommodated in a single dormitory type meant for a group of 6 members, and 69.8% (n = 180) clean their dormitory twice a week. Most of the participants, ie., 78.7% (n = 203) maintain only moderate level of hand sanitization practices (Table1).
Prevalence of nasal S. aureus carriage
During the study, totally 70 (27.1%) isolates of S. aureus were recovered from 258 participants. The rate of nasal carriage was relatively high among females in terms of percentage (32.9%). Nasal carriage of S. aureus was detected among 29 out of 86 (33.7%) members from the age group of 24 and above and also it was the highest among medical interns, ie., 26 (40%) followed by clinical students, 17 (24.3%) and other health science students, 27 (22%) (Table 2).
Table 2.
Prevalence of S. aureus and MRSA among medicine and health science students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
| Variables | S. aureus carriage | MRSA carriage | Total | |||
|---|---|---|---|---|---|---|
| Yes (n = 70) | No (n = 188) | Yes (n = 19) | No (n = 51) | |||
| n (%) | ||||||
| Sex | Male | 47 (25) | 141 (75) | 10 (5.3) | 178 (94.7) | 188 |
| Female | 23 (32.9) | 47 (67.1) | 9 (12.9) | 61 (87.1) | 70 | |
| Age | Less than 24 | 41 (23.8) | 131 (76.2) | 8 (4.7) | 164 (95.3) | 172 |
| 24 and above | 29 (33.7) | 57 (66.3) | 11 (12.8) | 75 (87.2) | 86 | |
| Category of students | Medical intern | 26 (40) | 39 (60) | 11 (16.9) | 54 (83.1) | 65 |
| Clinical student | 17 (24.3) | 53 (75.7) | 3 (4.3) | 67 (95.7) | 70 | |
| Other health science | 27 (22) | 96 (78) | 5 (4.0) | 118 (96.0) | 123 | |
Prevalence of nasal MRSA carriage
Among the 70 isolates of S. aureus, 19 were identified as MRSA, and hence, the prevalence among S. aureus positive participants was 27.1%. Overall prevalence of MRSA was 7.4% (n = 19); the carriage was found to be higher among medical interns, ie., 16.9% (n = 11) followed by clinical year students, 4.3% (n = 3) and health science students, 4.0% (n = 5). Of the total MRSA carriage, males account for the 53% (n = 10); carriage was found higher, ie., 12.8% (n = 11) among the age group of 24 and above (Table 2; Fig. 1).
Figure 1.
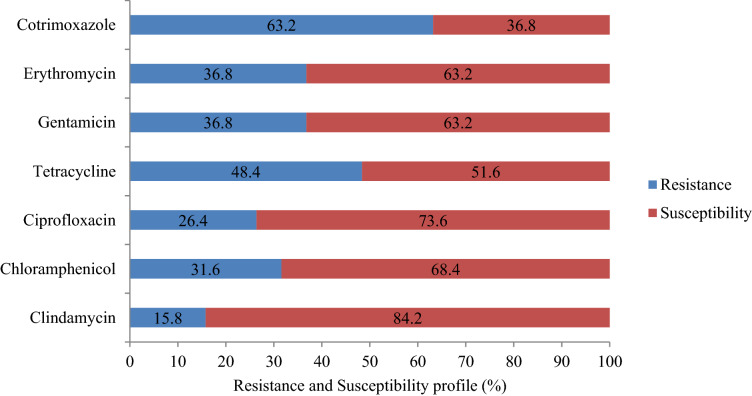
Antimicrobial susceptibility profiles of nasal MRSA isolates among Medicine and Health Science Students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
Antibiotic susceptibility tests
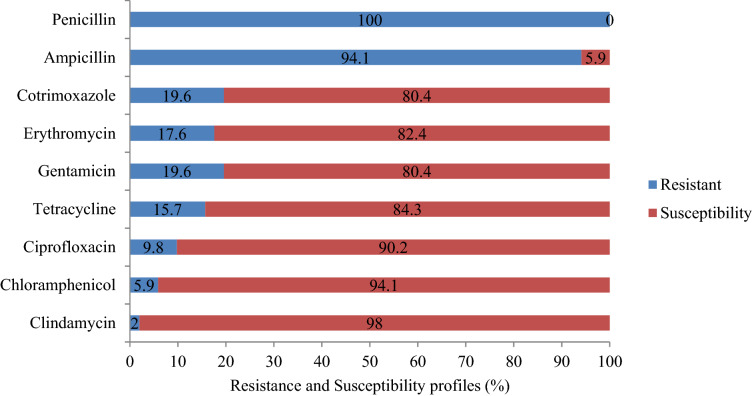
A total of 51 methicillin susceptible S. aureus (MSSA) isolates were subjected to tests against nine antibiotics. It was found that majority of these isolates were susceptible to seven antibiotics ie., to an extent of 80.4 to 98.0%. At the same time, they showed a very high level of resistance to two antibiotics such as penicillin (100%) and ampicillin (94.1%) (Fig. 2). Most of the isolates of MRSA were found susceptible to antibiotics such as clindamycin (84.2%), ciprofloxacin (73.6%) and chloramphenicol (68.4%). It was found that 63.2% of each of the isolates were susceptible to gentamicin and erythromycin whereas 52.6% showed susceptibility to tetracycline. On the other hand, 63.2% of the isolates were resistant to trimethoprim-sulfamethoxazole (Fig. 1). No intermediate category was observed in this study. Of the nine erythromycin resistant isolates of MSSA, erythromycin inducible clindamycin resistance (iMLSB) was detected in 55.6% (n = 5). Among the isolates of MRSA, iMLSB phenotype was observed in 57.1% (n = 4) of erythromycin resistant cases.
Figure 2.
Antimicrobial susceptibility profiles of nasal MSSA isolates among Medicine and Health Science Students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
Multi-drug resistance profiles of MSSA and MRSA
Among the isolates of MSSA, 39.2% (n = 20) were MDR; of them, 65% (n = 13) showed resistance to three different classes of antibiotics. About 35% (n = 7) isolates showed resistance to four classes of antibiotics in varying profiles. It was found that ten of the MRSA isolates are MDR (52.6%), and out of these, seven isolates (70%) showed resistance to three classes of antibiotics. Two isolates displayed resistance to four classes of antibiotics, ie., CLN/CHL/TET/GEN. Besides, one isolate of MRSA showed resistance to five classes of antibiotics (Table 3).
Table 3.
Multidrug resistance profile of nasal MRSA isolates among Medicine and Health Science Students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
| Resistance profile | MDR | Resistance profiles | Source of isolate | No. of isolates n (70) | ||
|---|---|---|---|---|---|---|
| MI | CS | OH | ||||
| MRSA | ||||||
| R3 | E/ SXT /TET | 2 | 1 | 1 | 4 | |
| R3 | E/CLN/TET | 2 | 1 | – | 3 | |
| R4 | CLN/ CHL/TET/GEN | 1 | – | 1 | 2 | |
| R5 | E/TET/CLN/GEN/CPR | 1 | – | – | 1 | |
| Total MRSA | 6 | 2 | 2 | 10/19(52.6) | ||
| MSSA | R3 | AMP/PEN/GEN | 2 | 1 | 1 | 4 |
| R3 | AMP/PEN/SXT | 3 | 1 | 1 | 5 | |
| R3 | AMP/PEN/TET | 2 | 1 | 1 | 4 | |
| R4 | AMP/PEN/E/SXT | 2 | 1 | 1 | 4 | |
| R4 | AMP/PEN/GEN/CLN | 2 | – | 1 | 3 | |
| Total | 11 | 4 | 5 | 20/51(39.2) | ||
PEN: penicillin, CPR: ciprofloxacin, CLN: clindamycin, GEN: gentamicin, E: erythromycin, CHL: chloramphenicol, AMP: ampicillin, TET: tetracycline and SXT: trimethoprim-sulfamethoxazole, MI: Medical intern, CS: clinical students, OH: other health students, R3: resistant to 3 antibiotics, R4: resistant to 4 antibiotics, R5: resistant to 5 antibiotics.
Biofilm forming potentials of MRSA
According to the OD reading from micro-titer plates, 2 (10.5%) isolates exhibited strong biofilm forming potency followed by another couple of isolates that displayed only a moderate level of activity. A third pair of isolates was found to be weak biofilm formers. On the other hand, 13 (68.5%) isolates were biofilm non-formers. In total, biofilm forming isolates were 31.6%, (6/19). All the six isolates of biofilm formers were obtained from medical interns and 60% of them were found to be MDR.
Factors associated with MRSA carriage
Participants in the age group of 24 and above were colonized with MRSA in a relatively higher proportion than others, however was not statistically significant. The carriage was found to be higher among females, 39.1% (n = 9) and is statistically significant (p = 0.04). Among the 19 participants tested positive for MRSA, 13 practiced sports or visited gymnasium, but this also was not statistically significant (p = 0.48). In bivariable analysis, MRSA colonization was found to be statistically significant with variables such as sex (p = 0.046), age (p = 0.023), category of students (p = 0.002), mean exposure to hospital (p = 0.002), habit of nose picking (p = 0.010), usage of gloves during the handling of patients (p = 0.000), sharing of clothing and sports equipment (p = 0.000), participation in invasive procedures (p = 0.162), strength of accommodation in a single dormitory (p = 0.010) and the hand sanitization level (p = 0.000) (Table 4). However, the results of multivariable analysis showed that odds of having a nasal MRSA are 4.9 times higher in students having > 2 years of mean exposure to hospital [p = 0.048, AOR: 4.99, 95% CI 1.01–24.66]. Besides, the odds of MRSA colonization are 5.13 times higher in participants having a habit of nose picking [p = 0.05, AOR: 5.13, 95% CI 0.94–27.74)]. Similarly, the odds of being colonized by MRSA was 5.4 times higher in students who share clothing and sports equipment [p = 0.017, AOR: 5.43, 95% CI 1.35–21.83].
Table 4.
Bivariable and multivariable logistic regression analysis of factors associated with nasal carriage of MRSA among Medicine and Health Science Students of Arba Minch University, Arba Minch, southern Ethiopia, 2020.
| Variables | Category | MRSA carriage | Analysis | ||||
|---|---|---|---|---|---|---|---|
| No | Yes | COR (95% CI) | p value | AOR (95% CI) | p value | ||
| Sex | Male | 188 | 10 | 1 | 1 | 1 | |
| Female | 70 | 9 | 2.62 (1.01–6.76) | 0.04* | 3.24(0.60–17.53) | 0.17 | |
| Age | Less than 24 | 172 | 8 | 1 | 1 | 1 | |
| 24 and above | 86 | 11 | 3.00(1.16–7.78) | 0.02* | 0.82(0.16–4.01) | 0.81 | |
| Category of students | Medical Interns | 65 | 11 | 4.71(1.80–12.30) | 0.002* | 4.78(0.65–34.69) | 0.12 |
| Clinical and OHS students | 193 | 8 | 1 | 1 | 1 | ||
| Mean exposure to hospital | ≤ 2 years | 193 | 8 | 1 | 1 | 1 | |
| > 2 years | 65 | 11 | 4.71(1.80–12.30) | 0.002* | 4.99(1.01–24.66) | 0.04** | |
| Habit of nose picking | Yes | 125 | 15 | 4.39(1.41–13.64) | 0.01* | 5.13(0.94–27.74) | 0.05** |
| No | 133 | 4 | 1 | 1 | 1 | ||
| Participation in sports | Yes | 64 | 6 | 1.44(0.52–3.96) | 0.48 | – | – |
| No | 194 | 13 | 1 | 1 | |||
| Sharing of clothing and sports equipment | Yes | 65 | 13 | 7.79(2.82–21.49) | 0.000* | 5.43(1.35–21.83) | 0.01** |
| No | 193 | 6 | 1 | 1 | 1 | ||
| Participation in invasive procedures | Yes | 150 | 14 | 2.12(0.74–6.07) | 0.16* | 1.61(0.21–11.97) | 0.64 |
| No | 108 | 5 | 1 | 1 | 1 | ||
| Use of glove while handling patients | Always | 197 | 8 | 1 | 1 | 1 | |
| Sometimes | 42 | 11 | 6.44 (2.44–17.01) | 0.00 | 2.45 (0.76–7.82) | 0.13 | |
*Statistically significant at p < 0.25 in bivariable analysis; **Statistically significant at p < 0.05 in multivariable analysis, AOR: Adjusted odds ratio, COR: Crude odds ratio, 1: reference group, CI: Confidence interval.
Discussions
During the last three decades, MRSA has evolved as one of the most important causes of hospital acquired infection worldwide. It is a well acknowledged fact that nasal colonized healthcare workers in hospitals can become reservoirs leading to the spread of MRSA to susceptible patients15. Its identification can help in the initiation of decolonization measures combined with other precautions such as taking care of hand hygiene aimed at the reduction of transmission and spread.
In Ethiopia, nasal colonization by MRSA among medical and health science students are not studied extensively, despite their increased exposure to nosocomial pathogens from risky patients16. This innovative study provides a baseline data pertaining to the prevalence, associated factors, antimicrobial susceptibility profiles, and biofilm-forming potentials of nasally colonized MRSA among such a group in the Arba Minch town of Ethiopia. According to the present study, the overall prevalence of nasal S. aureus among medical students is 27.1%. This value is more or less in parity with the results of studies done among students from other countries such as Poland (30%)17, China (23.1%)18, Thailand (29.7%)19 and Saudi Arabia (25.3%)20. However, it is lower than that reported from a study done in Nepal (35%)21, which could be due to variations in geographical locations, study settings, methodology used and also because of the inclusion of undergraduates other than medical/health science students who had less frequent exposure to hospitals. Our results are showing a relatively upward trend in comparison to those studies reported from Jimma, Ethiopia (21.1%)22, Tanzania (21.0%)23, Nigeria (14%)24, and Iran (19.6%)25. These inconsistencies might be attributed to differences in situations existing in various countries and hospital settings and also in infection control and prevention policies and standard precautions taken. Moreover, the overall prevalence of MRSA found in this study is 7.4% and is comparable to the studies conducted in Jimma, Ethiopia (8.4%)22, and China (9.4%)18. However, this percentage is lower than the extent reported from Nepal (19.5%)21, Iran (13.14%)25, and Nigeria (13.6%)26. The lower prevalence found in our study might be due to the inequalities in the nature of environmental exposures, spatial differences and types of methodologies used.
Also the prevalence found in the current study is relatively higher than that previously reported from Tanzania (1.5%)27, Democratic Republic of Congo (2.6%)28, and Saudi Arabia (6.7%)20. These fluctuations might be due to the variations in infection control and prevention policies existing across countries, differences in perceptions, awareness of students about the epidemiology of MRSA and the nature of geographical status, as already cited above.
Another interesting finding is that the wider extent of S. aureus colonization (27.3%) and lower MRSA carriage (7.4%) observed in Arba Minch are comparable to an earlier study reported from Jimma, Ethiopia22 and could be due to the similarity in methodologies used. However, as mentioned earlier, the prevalence of MRSA among students was 7.3%, indicating a rate of nasal colonization more or less equivalent to that existing among the general population and healthcare workers at the national level16. In that meta-analytical study, authors arrived at a pooled prevalence of 10.94%, in the case of nasal MRSA. In the present study, the prevalence of nasal MRSA is found to be higher in medical interns compared to other students, however, there was no notable statistically significant association. Our results are in line with a couple of the earlier studies conducted in Jimma, Ethiopia22 and Saudi Arabia20. The high prevalence of nasal MRSA in medical interns could be attributed to their long-term exposure to hospital environments and regular interactions with patients. In this context, it is envisaged that medical students carrying multidrug-resistant S. aureus can pose serious threats to patients as well as to other people in their immediate vicinity. It is not possible to draw any strong conclusions from this findings and therefore further in-depth study is required to examine the relationship between MRSA nasal colonization in medical students and the subsequent transmission to patients.
The rise of drug-resistant MRSA is a serious challenge in the treatment and control of staphylococcal infections. Therefore, the rapid detection of MRSA and elucidation of its susceptibility profile are crucial from a treatment point of view, especially in the context of limited therapeutic regimens existing. Literature related to the antimicrobial susceptibility profiles of MRSA in medical students in Ethiopia is scanty. In this study, totally seven commonly used antibiotics were selected to inspect the susceptibility profiles of MRSA. Antimicrobial susceptibility profiles were detected in the case of all the MRSA isolates, but to varied extents. Resistance were particularly exhibited against the antibiotics, viz., trimethoprim-sulfamethoxazole (63.2%) (95% CI 47.8%, 78.5%) followed by tetracycline (48.4) (95% CI 27.1%, 64.6%), however, lower extents of resistance only were displayed against gentamicin and erythromycin, each 36.2% (95% CI 19.1%–49.3%) and chloramphenicol, 31.6% (95% CI 17.1%–45.2%).
Resistance exhibited against trimethoprim-sulfamethoxazole (63.2%) was in line with a couple of studies conducted in different regions of Ethiopia, such as Adigrat (64.3%)29 and Dessie (66.7%)30. However, it is lower compared to the data obtained from studies conducted in Poland (100%)17 and Jimma, Ethiopia (83.9%)22. These differences in resistance might be due to the types of antimicrobials used and the variations in the characteristics of study populations included.
In our study, 48.4% of isolates showed resistance to tetracycline and this is in contrast to the results of other works reported from Kenya (35%)31 and Poland (37.5%)17; but less severe than the extent of resistance found in a study done in Jimma, Ethiopia (64.5%)22. The resistance profile of MRSA against gentamicin (36.8%), erythromycin (36.8%) and chloramphenicol (31.6%) observed currently are in line with the results of a study conducted in Kenya31; but is less pronounced than that found in Adigrat, Ethiopia29.
On the other hand, isolates of MRSA showed only nominal resistance to clindamycin (15.8%). A similar trend of resistance was observed in a study reported earlier from Jimma, Ethiopia (16.1%)22. In the case of ciprofloxacin, enhanced resistance was reported from Jimma (51.6%)22, Adigrat29 and Mekelle32, compared to our results (26.4%). These discrepancies might be due to the fact that there is a gradual increase in antibiotic resistance which in turn might be the result of overuse or misuse of antimicrobial agents and or due to probable mutations and horizontal gene transfer occurring among bacteria.
Results revealed that out of the 19 MRSA isolates tested for inducible clindamycin resistance, 57.1% were positive and this is much elevated than a couple of studies done in Tanzania (31.8%)6 and Egypt 5.3%33. These variations might be due to the deviation in the trends in usage of antibiotics, methodology adopted, and also the type of study participants involved.
Multidrug resistance shown by MRSA is currently considered as a global threat by WHO. In the present study, MDR was observed in the case of 52.6% MRSA. Literature linked to MDR among medical students is limited, but this result is matching with a couple of studies conducted in Mekelle (50%)32 and Jimma (48.4%)22, Ethiopia; however, not that severe compared to the extent of MDR revealed by earlier studies conducted in Arba Minch itself, (75%)34, Egypt (85.8%)33 and Tanzania (72.7%)6. Surprisingly, results of another study conducted in Arba Minch previously showed a very weak level of MDR ie., 18.7% only9. The emergence of high MDR-MRSA could be due to the unscrupulous usage of those antibiotics in the study area. The overall picture of antimicrobial susceptibility profile obtained could be helpful for judiciously choosing antibiotics in future for the effective management of MRSA.
In the present study, 31.6% of the isolates produced biofilm and among them almost 33.4% were very effective producers of biofilm whereas some of them were moderate and weak i.e., 33.3% each. Published literature related to biofilm forming ability of MRSA found in medical students is limited in an Ethiopian context. Earlier studies performed in Arba Minch among HIV patients reported that 34.3% isolates of MRSA were biofilm formers9. However, this is lower than that found among food handlers (80%) in the same town34.
It has been found that 60% of MDR isolates among MRSA were biofilm formers and all these are isolated from medical interns. Further statistical analysis of the process of biofilm-formation by MRSA and MDR isolates revealed that it is positively skewed towards MDR isolates. This trend is comparable to that found in some of the previous studies conducted in Nigeria35, and Brazil36.
Different socio-demographic and behavioral associated factors had been analyzed by taking into consideration the spread of nasal carriages of MRSA among medicine and health science students. Of those factors, mean exposure to hospital for > 2 years was one of the significantly associated factors (p = 0.04) related to the nasal carriage of MRSA. It is an important predisposing factor connected to colonization in the population analyzed in this study. Here, the odds of having MRSA isolate was 4.9 times higher among students who have mean exposure to hospital for > 2 years. Other vital factor which are intimately associated with the nasal carriage of MRSA was sharing of clothing and sports equipment (p = 0.01). In this study, the odds of being colonized by MRSA was 5.4 times higher among students who share clothing and sports equipment than their counter parts.
Conclusions
The prevalence of nasal carriage of S. aureus and MRSA in this study were found to be comparable to that reported earlier in Ethiopia itself. Higher MRSA carriage rate was noticed among medical interns in comparison to other health science and clinical students. Of the MRSA isolates, about 52.6% were considered as MDR and 60% of them were found to be biofilm formers. In addition, 84.2% of the MRSA isolates were susceptible to clindamycin. Students having > 2 years of mean exposure to hospital and those who share clothing and sports equipment were found to be significantly associated with the acquisition of nasal carriage of MRSA.
Materials and methods
Study area, design and period
An institution based cross sectional study was conducted in the College of Medicine and Health Sciences, AMU, southern Ethiopia from 01 August through 30th November 2020, located in Arba Minch town which enrolls 1598 students in total in the health sciences and medical programs (regular). In 2019/2020 academic year, among the new entrants, 1029(64.4%) were males. The campus consists of a number of departments such as medicine, nursing, pharmacy, anesthesia, midwifery, radiology, medical laboratory science, environmental health, health informatics and public health.
Study population and eligibility criteria
All undergraduate students belonging to clinical medicine and health sciences, who had a clinical exposure for eight hours per day for more than 3 months in any hospital setting during the study period, are considered. The inclusion criteria set for the study comprises; 1. all medical and health science graduating class students who have exposure for 8 h per day for the previous 3 months and who are available during the study period; 2. students without a history of hospitalization in the preceding six months (i.e., they are not exposed because of admission, rather exposed during care giving). The exclusion criteria include; (1) participants who had nasal infections during the study period, (2) those who received intranasal antibiotic ointment or other antibiotics within the previous two weeks of the commencement of the study or who underwent a nasal decolonization procedure. The study protocol was approved by the Institutional Research Ethics Review Board of the College of Medicine and Health Science of Arba Minch University (IRB/464/12). This study was conducted in accordance with the declaration of Helsinki. Besides, separate permission was procured from Arba Minch University, College of Medicine and Health Sciences. Formal written consent was obtained from each study participant. Confidentiality was strictly maintained from sample collection up to the final report writing.
Sample size determination and sampling technique
The sample size was calculated by using a single population proportion formula, where, p value of 50% was chosen due to the dearth of prior studies conducted among similar study population. Calculations were done using an open Epi version 3 by assuming 95% confidence level with 5% degree of precision, as followed in the case of sample size for frequency10.
| Population size (for finite population correction factor or fpc)(N): | 535 |
| Hypothesized % frequency of outcome factor in the population (p): | 50% ± 5 |
| Confidence limits as % , (absolute + /− %)(d): | 5% |
| Design effect (for cluster surveys-deff): | 1 |
Accordingly, the sample size determined was 224.
Then by assuming a non-response rate of 15%, the total subjects included in the study was 258 (n = 224; n + 15% of 224 = 258); and it is the final sample size.
Sampling technique
Clinical medical and other graduating health science students at the verge of completion of their courses during the study year and who were also attending clinical practices in different departments of AMGH or any other hospitals were stratified, based on academic years (for medicine students) and departments (for other graduating class students). A proportional allocation sampling technique was followed for each stratum; as clinical-I, clinical-II, medical intern, graduating class of anesthesia, medical laboratory, midwifery, nursing, radiology and health officer; also a systematic sampling technique was used to recruit the rest. Probability proportional to size /PPS (proportional allocation technique)11 was obtained by using the formula,
where: ni = Required sample size of students from each ith stratum; Ni = Number of medical students in the ith stratum; n = Over all sample size; N = Total number of students in the ith stratum.
Absolute proportions were found in anesthesia, 4.7% (n = 12), clinical – I medical students, 13.2% (n = 34), clinical—II medical students, 13.9% (n = 36), medical interns, 25.2% (n = 65), health officers, 10.5% (n = 27), medical laboratory science, 8.5% (n = 22), midwifery, 8.9% (n = 23), nursing, 10.8% (n = 28) and radiology, 4.3% (n = 11).
Collection methods
Data collection tool and procedure
A pre-tested structured questionnaire with three sections was used to collect the data; it is formulated after an extensive literature survey. The first section consisted of socio-demographic questions, the second part comprised clinical data and the third section corresponded questions linked to behavioral peculiarities. Informed consents were sought for all participants prior to study. Socio-demographic and other related information were accumulated by the data collector through a face-to-face interview.
Sample collection, transportation, processing and analysis
Nasal samples were collected by inserting a sterile cotton swab (moistened with sterile normal saline prior to sampling, to avoid discomfort) into both nostrils9. A single specimen was obtained from each participant from both anterior nares consecutively, using the same swab and it was then placed in a sterile normal saline, transported to the Microbiology and Parasitology Laboratory, Department of Medical Laboratory Sciences, using a cold chain within an hour of collection.
Isolation and identification of S. aureus
All the samples were processed immediately to avoid any possible contamination. Each sample was directly inoculated into mannitol salt agar (Oxoid, Hampshire, UK). The inoculated plates were then incubated for 24 h at 37 °C, and the yellowish colonies obtained were subsequently subjected to species identification and confirmation. Morphological, physiological and biochemical characteristics (positive catalase and coagulase tests), of bacteria were ascertained by adopting standard laboratory methods including Gram staining and examination of morphology on different media such as DNase and blood agar12. Corresponding American Type Culture Collection (ATCC) strains were utilized as references.
Detection of MRSA
Identification of MRSA was performed in accordance with the criteria set by Clinical Laboratory Standard Institute (CLSI), using cefoxitin disk diffusion assay. Bacterial suspension (5 ml) of 0.5 McFarland (1 × 108 CFU/ml) was prepared and swabbed into Mueller Hinton agar (MHA) (Hi-media, India), and cefoxitin disk were placed. After incubation for 24 h at 37 °C, the zone of inhibition was measured. Strains showing zone of inhibition ≤ 21 mm were extrapolated as MRSA13.
Antimicrobial susceptibility testing
Antibiotic susceptibility profiling of all isolates of MRSA were achieved by Kirby–Bauer disk diffusion technique according to the criteria set by CLSI13. Inoculums equivalent to the opacity of 0.5 McFarland standards were prepared and swabbed over MHA surface; exposed to a concentration gradient of antibiotic, and then incubated face up at 37 °C for 24 h. Diameter of zones of inhibition were measured to the nearest millimeter and categorized as sensitive, intermediate, and resistant according to the table described in CLSI. Following antibiotics were used to examine the susceptibility profiles of MRSA, viz., penicillin G (10 units), ciprofloxacin (5 μg), clindamycin (2 μg), gentamicin (10 μg), erythromycin (15 μg), chloramphenicol (30 μg), ampicillin (10 μg), ceftriaxone (30 μg), tetracycline (30 μg) and trimethoprim-sulfamethoxazole (1.25/25.75 μg) and cefoxitin (30 μg)13. In addition, inducible clindamycin resistance was also analyzed by disk diffusion using D-zone test. Erythromycin disk (15 μg) was placed at a distance of 15–26 mm (edge to edge) from a clindamycin disk (2 μg) on MHA. After overnight incubation, plates were examined for the formation of flattened zone of inhibition adjacent to the erythromycin disk. A truncated clindamycin zone of inhibition (D-shape) indicated inducible resistance; this method is applied only to organisms which were resistant to erythromycin and susceptible or intermediate to clindamycin13.
Detection of biofilm
Micro-titer plate assay was used for the detection of biofilm forming MRSA isolates in this study14. Well standardized bacterial suspensions were prepared in sterile normal saline from pure colonies and adjusted to a 0.5 McFarland turbidity standard. Standardized bacterial suspensions were diluted with tryptic soy broth (TSB), supplemented with 1% glucose to a final volume of 200 µl per well. This experiment was performed for each isolate in triplicate and incubated at 37 °C for 24 h in flat-bottomed polystyrene micro-titer plates, the contents of the wells were then removed and washed with 300 μl (0.3 ml) of phosphate buffered saline (PBS). Finally, the wells were fixed with 150 μl of 99% methanol for 30 min and stained with crystal violet (0.1% w/v) for 15 min. Excess stain was rinsed off with distilled water. After drying, the wells were treated with 150μL of 95% ethanol for 30 min at room temperature to solubilize the dried crystal violet stain adhered to the biofilm. Optical densities (OD) were then determined by an automated micro ELISA reader at a wavelength of 570 nm. These OD values were considered as an index of bacterial adhesion and biofilm formation. Six wells (A1 to A6) of micro-titer plates were used as negative controls which contained only TSB + 1% glucose without bacteria. Average of three wells used for each bacterial isolate is considered as the actual OD since each of them was added to three wells. The cut-off value of optical density (ODc) was calculated and defined as three standard deviations above the mean OD of the negative control.
Isolates were classified as follows: as described elsewhere14.
Bacterial OD ≤ ODc = non-biofilm former;
OD > ODc, but ≤ 2 ODc = weak biofilm former;
OD > 2 ODc, but ≤ 4 ODc = moderate biofilm former and
OD > 4ODc = strong biofilm former
Quality control
A pre-test was done on 5% of the total sample size before one week of the actual study in Wolita Sodo University to validate the variables and data collection tools were modified accordingly. Standard quality measures were implemented throughout the entire process of data collection and the laboratory works and also the completeness, accuracy, clarity, and consistency of data were checked. Standard Operating Procedures (in-house SOP manual) for each operation were strictly followed. All culture media were prepared following the instructions of manufacturers and sterility was tested by incubating 5% of each batch at 35–37 °C overnight, for the evaluation of any possible contamination. Moreover, positive control (standard) strains of S. aureus, (ATCC 25923) were used as the quality controls (reference) for biochemical tests and agar plates including MHA with vancomycin disk; this ensured the testing performance, i.e., the potency of the disk, as per CLSI 2019 guidelines.
Data analysis
Data were checked, cleaned and coded for its completeness and entered into the Epi data version 4.6.0.2 software, and analyzed by the Statistical Package for Social Sciences (SPSS) version 25. Descriptive statistics including frequency, mean and percentages were used. Binary logistic regression model was used to analyze the association among dependent and independent variables. Those variables with p value < 0.25 in bivariable analysis were considered as candidates for further multivariable analysis; p value ≤ 0.05 was considered as statistically significant. Adjusted odds ratio (AOR) and 95% confidence interval (CI) were used to determine the strength of association among variables.
Acknowledgements
We greatly acknowledge the continuous support and encouragement given by the Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, AMGH. Thanks are extended to Prof. Dr. K.R. Sabu for the English corrections.
Author contributions
E.M., A.M., A.A. and M.W. designed research; E.M. conduct the research; A.M., A.A., M.W. T.H. and B.W. guided the research; A.M., A.A., M.W., T.H. and B.W. conducted review and editing the original draft and A.M. and A.A. reviewed and wrote the paper. All authors reviewed the manuscript.
Funding
The authors received no specific funding for this work.
Data availability
All relevant data are within the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Al-haddad OH, Zorgani A, Ghenghesh KS. Nasal carriage of multi-drug resistant panton-valentine leucocidin-positive methicillin-resistant Staphylococcus aureus in children in Tripoli-Libya. Am. J. Trop. Med. Hyg. 2014;90:724–727. doi: 10.4269/ajtmh.13-0715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodrigues S, Conceição T, Silva IS, de Lencastre H, Aires-de-Sousa M. Frequent MRSA nasal colonization among hospitalized children and their parents in Angola and São Tomé and Príncipe. J. Hosp. Infect. 2018;100:344–349. doi: 10.1016/j.jhin.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 3.Bal AM. Genomic insights into the emergence and spread of international clones of healthcare-, community- and livestock-associated methicillin-resistant Staphylococcus aureus: blurring of the traditional definitions. J. Glob. Antimicrob. Resist. 2016;6:95–101. doi: 10.1016/j.jgar.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Gurieva, T. V., Bootsma, M. C., & Bonten, M. J. Decolonization of patients and health care workers to control nosocomial spread of methicillin-resistant Staphylococcus aureus: a simulation study. BMC Infect. Dis.12, 12–20. doi:10.1186/1471-2334-12-302 (2012) [DOI] [PMC free article] [PubMed]
- 5.Stevens AM, Hennessy T, Baggett HC, Bruden D, Parks D, Klejka J. Methicillin-Resistant Staphylococcus aureus carriage and risk factors for skin infections, Southwestern Alaska, USA. Emerg. Infect. Dis. 2010;16:797–803. doi: 10.3201/eid1605.091851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joachim A, et al. Prevalence of methicillin-resistant Staphylococcus aureus carriage on admission among patients attending regional hospitals in Dar es Salaam, Tanzania. BMC Res. Notes. 2017;10:417. doi: 10.1186/s13104-017-2668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turabelidze G, Lin M, Wolkoff B, Dodson D, Gladbach S, Zhu BP. Personal hygiene and methicillin-resistant Staphylococcus aureus infection. Emerg. Infect. Dis. 2006;12:422–427. doi: 10.3201/eid1205.060625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bekir K, et al. Molecular detection of adhesins genes and biofilm formation in methicillin resistant Staphylococcus aureus. Afr. J. Microbiol. Res. 2012;6:4908–4917. [Google Scholar]
- 9.Manilal A, et al. Methicillin-resistant Staphylococcus aureus colonization in HIV patients of Arba Minch Province, Ethiopia: Carriage rates, antibiotic resistance, and biofilm formation. Acta Microbiol. Immunol. Hung. 2019;66:69–83. doi: 10.1556/030.66.2019.014. [DOI] [PubMed] [Google Scholar]
- 10.XXX. https://www.openepi.com/SampleSize/SSPropor.htm.
- 11.Daniel WW, Cross CL. Biostatistics: a foundation for analysis in the health sciences. 7. Hoboken: Wiley; 2012. [Google Scholar]
- 12.Collee, J.G., Marmion, B.P., Fraser, A.G., Simmons, A., & Mackie T. Mackie and McCartney practical medical microbiology, 14th edn. A division of Reed Elsevier India Private Limited (Elsevier, Amsterdam, 2012).
- 13.CLSI. Performance standards for antimicrobial susceptibility testing, 29th edn., CLSI supplement M100 (2019).
- 14.Moori-Bakhtiari N, Moslemi M. Phenotypic evaluation of biofilm producing ability in Methicillin resistant Staphylococcus aureus. J. Kashan Univ. Med. Sci. Feyz. 2017;20:25–31. [Google Scholar]
- 15.den Heijer, C.D., et al. APRES Study Team. Prevalence and resistance of commensal Staphylococcus aureus, including meticillin-resistant S. aureus, in nine European countries: a cross-sectional study. Lancet Infect. Dis.13, 409–415. doi: 10.1016/S1473-3099(13)70036-7 (2013). [DOI] [PubMed]
- 16.Reta A, Mengist A, Tesfahun A. Nasal colonization of methicillin resistant Staphylococcus aureus in Ethiopia: a systematic review and meta-analysis. Ann. Clin. Microbiol. Antimicrob. 2019;18:25. doi: 10.1186/s12941-019-0324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piechowicz L, Garbacz K, Wiśniewska K, Dąbrowska-Szponar M. Screening of Staphylococcus aureus nasal strains isolated from medical students for toxin genes. Folia Microbiol. (Praha) 2011;56:5–9. doi: 10.1007/s12223-011-0041-1. [DOI] [PubMed] [Google Scholar]
- 18.Ma, X.X., et al. Nasal carriage of methicillin-resistant Staphylococcus aureus among preclinical medical students: epidemiologic and molecular characteristics of methicillin-resistant S. aureus clones. Diagn. Microbiol. Infect. Dis.70, 22–30, doi: 10.1016/j.diagmicrobio.2010.12.004 (2011). [DOI] [PubMed]
- 19.Treesirichod A, Hantagool S, Prommalikit O. Nasal carriage and antimicrobial susceptibility of Staphylococcus aureus among medical students at the HRH princess Maha Chakri Sirindhorn medical center, Thailand: a cross sectional study. J. Infect. Public Health. 2013;6:196–201. doi: 10.1016/j.jiph.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Zakai SA. Prevalence of methicillin-resistant Staphylococcus aureus nasal colonization among medical students in Jeddah, Saudi Arabia. Saudi Med. J. 2015;36:807–812. doi: 10.15537/smj.2015.7.11609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhatta DR, et al. Nasal and pharyngeal colonization by bacterial pathogens: a comparative study between preclinical and clinical sciences medical students. Can. J. Infect. Dis. Med. Micbiol. 2018 doi: 10.1155/2018/7258672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Efa F, Alemu Y, Beyene G, Gudina EK, Kebede W. Methicillin-resistant Staphylococcus aureus carriage among medical students of Jimma University, Southwest Ethiopia. Heliyon. 2019;5:e01191. doi: 10.1016/j.heliyon.2019.e01191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geofrey A, Abade A, Aboud S. Methicillin-resistant staphylococcus aureus (MRSA) colonization among Intensive Care Unit (ICU) patients and health care workers at Muhimbili national hospital, Dar Es Salaam, Tanzania, 2012. Pan. Afr. Med. J. 2015;21:211–220. doi: 10.11604/pamj.2015.21.211.4207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Adesida SA, et al. Associated risk factors and pulsed field gel electrophoresis of nasal isolates of Staphylococcus aureus from medical students in a tertiary hospital in Lagos, Nigeria. Braz. J. Infect. Dis. 2007;11:63–69. doi: 10.1590/s1413-86702007000100016. [DOI] [PubMed] [Google Scholar]
- 25.Abroo S, Hosseini Jazani N, Sharifi Y. Methicillin-resistant Staphylococcus aureus nasal carriage between healthy students of medical and nonmedical universities. Am. J. Infect. Control. 2017;45:709–712. doi: 10.1016/j.ajic.2017.02.034. [DOI] [PubMed] [Google Scholar]
- 26.Egwuatu CC, Ogunsola FT, Egwuatu TO, Oduyebo OO. Prevalence and risk factors for carriage of methicillin-resistant Staphylococcus aureus (MRSA) among healthcare workers in a tertiary institution in Nigeria. J. Med. Dent. Sci. 2013;8:9–13. doi: 10.1016/S1991-7902(13)00189-X. [DOI] [Google Scholar]
- 27.Okamo B, Moremi N, Seni J, Mirambo MM, Kidenya BR, Mshana SE. Prevalence and antimicrobial susceptibility profiles of Staphylococcus aureus nasal carriage among pre-clinical and clinical medical students in a Tanzanian University. BMC Res. Notes. 2016;9:47. doi: 10.1186/s13104-016-1858-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Boeck H, et al. Staphylococcus aureus nasal carriage among healthcare workers in Kisangani, the Democratic Republic of the Congo. Eur. J. Clin. Microbiol. Infect. Dis. 2015;34:1567–1572. doi: 10.1007/s10096-015-2387-9. [DOI] [PubMed] [Google Scholar]
- 29.Legese H, et al. Nasal carriage, risk factors and antimicrobial susceptibility pattern of methicillin resistant Staphylococcus aureus among healthcare workers in Adigrat and Wukro hospitals, Tigray, Northern Ethiopia. BMC Res. Notes. 2018;11:250. doi: 10.1186/s13104-018-3353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shibabaw A, Abebe T, Mihret A. Nasal carriage rate of methicillin resistant Staphylococcus aureus among Dessie Referral Hospital Health Care Workers; Dessie, Northeast Ethiopia. Antimicrob. Resist. Infect. Control. 2013;2:25. doi: 10.1186/2047-2994-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gitau W, Masika M, Musyoki M, Museve B, Mutwiri T. Antimicrobial susceptibility pattern of Staphylococcus aureus isolates from clinical specimens at Kenyatta National Hospital. BMC Res. Notes. 2018;11:226. doi: 10.1186/s13104-018-3337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gebremedhn G, Gebremariam TT, Wasihun AG, Dejene TA, Saravanan M. Prevalence and risk factors of methicillin-resistant Staphylococcus aureus colonization among HIV patients in Mekelle, Northern Ethiopia. Springerplus. 2016;5:877. doi: 10.1186/s40064-016-2613-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abdel-Maksoud M, et al. Methicillin-resistant Staphylococcus aureus recovered from healthcare- and community-associated infections in Egypt. Int. J. Bacterial. 2016 doi: 10.1155/2016/5751785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mama M, Alemu G, Manilal A, Seid M, Idhayadhulla A. Prevalence and biofilm forming potency of multi-drug resistant Staphylococcus aureus among food handlers in Arba Minch University, South Ethiopia. Acta Microbiol. Hellen. 2015;63:51–64. [Google Scholar]
- 35.Anie CO. Evaluation of biofilm and enterotoxin producing capacity of methicillin-resistant Staphylococcus aureus isolated from healthy persons. J. Appl. Sci. Environ. Manag. 2019;22:67–81. [Google Scholar]
- 36.de Araujo GL, et al. Commensal isolates of methicillin-resistant Staphylococcus epidermidis are also well equipped to produce biofilm on polystyrene surfaces. J. Antimicrob. Chemother. 2006;57:855–864. doi: 10.1093/jac/dkl071. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the manuscript.