Abstract
Circadian misalignment caused by differences in sleep duration between weekends and weekdays may be associated with adolescent mental health and sleep quality may be able to compensate for this problem. This study aimed to investigate the association between weekend catch-up sleep (CUS) ratio and sleep quality with depressive symptoms and suicidal ideation among South Korean adolescents. We used data from the Korea Youth Risk Behavior Web-based Survey 2015–2019 involving 270,619 adolescents. The weekend CUS ratio was calculated by dividing the average weekend sleep duration by the average weekday sleep duration (< 1.00, 1.00 ≤ CUS < 1.50, or ≥ 1.50). Subjective sleep quality was categorized as poor, moderate, or good. Multiple logistic regression analyses were performed. A weekend CUS ratio of < 1.00 and poor sleep quality was significantly associated with mental health. Absolutely short sleep duration (CUS < 1.00 and weekday sleep duration < 5 h) was most associated with depressive symptoms and suicidal ideation. Furthermore, adolescents with a CUS ratio of ≥ 1.50 showed increased odds of depressive symptoms despite having good sleep quality. Appropriate weekend CUS may benefit adolescents’ mental health. When investigating the relationship between adolescents’ sleep and mental health, a weekend CUS ratio should be considered in addition to sleep quality and duration.
Subject terms: Circadian rhythms and sleep, Public health
Introduction
Sleep related problems including short sleep duration and poor sleep quality are one of the most common health issues among adolescents worldwide1,2. Particularly, approximately 20% of adolescents may experience a depressive episode by the time they are 18 years old3, and the compelling evidence for association between regulation of sleep and emotion is continuously being reported4. Furthermore, the link between sleep disturbance and suicidal behaviors, a serious social and public health problem worldwide, has been highlighted5. However, exposures related to sleep timing, including chronotypes and social jet lag, have been less studied in adolescents6. Therefore, elucidating the relationship between sleep timing and poor-quality sleep in adolescents with depression and suicidal behavior is important for adolescent mental health.
Sleep problems, such as lack of sleep, low sleep quality, or irregular sleep habits, are believed to be causes of depression7–9. A previous study of adolescents in the United States reported that a longer weekday sleep duration is inversely associated with depressive symptoms10. Furthermore, recent studies have examined the associations between weekday–weekend sleep differences and mental health problems, such as depressive symptoms, suicide attempts, and self-injury, in adolescents11,12.
The National Sleep Foundation has recommended a sleep duration of 8–10 h for teenagers13. However, with environmental and psychological factors, such as early school hours and competitive academics, leading to a higher prevalence of insufficient sleep, many South Korean adolescents sleep for < 8 h, especially on weekdays14,15. The academic stress experienced by South Korean teenagers, where learning is considered a major indicator of success, causes stress not only in relation to school but also in life as a whole and has a significant impact on adolescents’ mental strength and overall adaptation16. Adolescents reduce sleep time and increase their academic time to escape or cope with this stress17. Therefore, improved sleep duration and quality may be critical for the mental health of South Korean adolescents.
Adolescents who live in an environment with a lack of sufficient sleep on weekdays due to schoolwork and other causes often sleep more on weekends, which is known as weekend catch-up sleep (CUS), than on weekdays. Weekend CUS calculated as the absolute difference between the weekday and weekend sleep durations18 is a compensatory phenomenon for weekday sleep deficit19. According to previous research, the average weekend sleep extension of high school students in Korea is reported to be up to 3 h14, whereas 35–40% of US secondary school students report that they extend their sleep time by more than 2 h on weekends20. By making up for the lack of sleep through weekend CUS, adolescents can resolve any sleep imbalance, reducing sleep-related problems21. However, adolescents with no difference in sleep duration between weekends and weekdays, or with a difference of more than 2 h (weekend oversleep), are more likely to experience mood, anxiety, substance use, and behavioral disorders, as well as suicidality21. That is, both too short and too long weekend oversleeps may be related to mental health among adolescents. Moreover, the social jet lag that accounts for the gap between ‘time zone’ on workdays/schooldays and free days can lead to chronic and ongoing circadian misalignment, which affects health through multiple mechanisms22,23.
Previous studies of weekend oversleep and social jet lag comparing the midpoint of sleep time on weekdays and weekends only considered the absolute time difference. However, since individuals have a different absolute sleep time stemming from biological and socio-environmental factors24,25, it would be meaningful to examine the ratio between the weekday and weekend sleep duration rather than investigating the absolute difference between the two. Additionally, sleep quality may affect the mental health of adolescents by mechanisms different from those of sleep duration. Considering that circadian rhythm disturbances are related to the pathophysiology of mood disorders25, we hypothesized that CUS that would impair the circadian rhythm would not be beneficial to adolescents’ mental health. In addition, it has been assumed that sleep quality could compensate for the difference in sleep duration even if the CUS ratio was out of a certain range. Thus, we investigated the association of weekend CUS ratio and subjective sleep quality with depressive symptoms and suicidal ideation among South Korean adolescents.
Methods
Study population and data
We used data obtained from the Korea Youth Risk Behavior Web-based Survey (KYRBS) during 2015–2019 for this cross-sectional study, which included a nationally representative sample of South Korean adolescents attending middle and high school (grades 7–12, age 12–18). All participants voluntarily log in using their certificate number and check the online informed consent themselves26. The KYRBS is a kind of Korean government-approved statistics (Approval number: 117058), and an anonymous self-administered structured questionnaire that does not involve any intervention on adolescents. Thus, ethics approval and informed consent of parents or legal guardians for the KYRBS was waived by the Korea Disease Control and Prevention Agency Institutional Review Board in accordance with the Bioethics and Safety Act, 201527. The KYRBS complied with the Declaration of Helsinki’s ethical standards and used a complex research design, which included multistage sampling, stratification, and clustering. The KYRBS was conducted through an online survey system, and the questionnaire comprised approximately 120 items in 15 sections. Respondents could not move on to the next section unless all the questions were answered in the current section, although responses with logical errors and responses that were outliers were treated as missing data. A total of 270,619 participants (male, 136,316 [50.4%]; female, 134,303 [49.6%]) were included in the study, excluding those who were treated as missing data due to logical errors or outliers in sleeping and waking times.
Variables
The main dependent variables were depressive symptoms and suicidal ideation. Depressive symptoms were assessed by the question “In the last 12 months, have you felt sad or hopeless enough to stop your daily activities for 2 weeks?.” Suicidal ideation was assessed by the question “Have you seriously considered suicide in the past 12 months?.” These variables were both dichotomized into a “yes” or “no” response.
The main independent variables were the weekend CUS ratio and subjective sleep quality. First, to determine the weekend CUS, the average sleep duration on weekdays and weekends was calculated using the question "During the past 7 days, what time did you usually go to bed and wake up?" In response to this question, the participants recorded the time they went to bed and the time they woke up on weekdays and weekends, respectively. Based on the recorded times, the average sleep time on weekdays and weekends was calculated.
The weekend CUS ratio was calculated by dividing the average weekend sleep duration by the average weekday sleep duration, according to the responses of the survey.
According to this formula, the weekend CUS ratio was classified as “CUS < 1.00,” “1.00 ≤ CUS < 1.50,” and “CUS ≥ 1.50.” For example, a teenager who slept 6 h during the weekday and 3 more hours on the weekend would be in the “CUS ≥ 1.50 (6 × 1.5 = 9 h)” group. However, a teenager who slept 7 h during the weekday and 3 more hours on the weekend would be included in the group with a “1.00 (7 h) ≤ CUS < 1.50 (10.5 h)”.
The weekend CUS ratio of 1.00 was used to confirm the association between shorter sleep duration on weekends than on weekdays and mental health of adolescents. The upper cut point for CUS of 1.50 means that the average sleep duration on weekends is 1.50 times higher compared to the average sleep duration on weekdays. The upper cut point for CUS was selected using the following rationale: First, the appropriate amount of sleep for adolescents is 8–10 h13, which is 1.50 times greater than the average sleep duration for South Korean adolescents (i.e., 6–7 h15) on weekdays. Next, considering the previous studies that defined extremes when the absolute difference in sleep duration between weekdays and weekends was more than 2 h21, and that students in South Korea additionally slept for about 3 h more on weekends14, weekend sleep duration within 1.50 times of weekday sleep duration was set as normal.
Subjective sleep quality was measured by asking the participants whether their sleep was sufficient to recover from fatigue during the last 7 days. The five possible responses were: very good, good, moderate, poor, and very poor. Finally, we grouped subjective sleep quality into three categories: “good (very good and good),” “moderate,” or “poor (poor and very poor)”.
Other independent variables affecting depressive symptoms and suicidal ideation were also considered covariates. They included grade (7–12), average weekday and weekend sleep durations (< 5 h, 5 h ≤ duration < 7 h, 7 h ≤ duration < 9 h, or ≥ 9 h), economic status (low, medium–low, medium, medium–high, or high), residence type (live with family, live with relative, or live without family or relative), academic achievement (low, medium–low, medium, or medium–high, high), alcohol status (ever or never), smoking status (everyday, someday, or never), physical activity (low or high), self-reported health status (low, medium, or high), and perception of stress (low, medium, or high).
Statistical analyses
The analyses were performed separately by sex, considering gender differences in depressive symptoms and suicidal behaviors28. We performed chi-squared tests to assess differences between frequencies and proportions of categorical variables. To analyze the association of the weekend CUS ratio and subjective sleep quality with depressive symptoms and suicidal ideation, we used a multiple logistic regression analysis after adjusting for covariates. For evaluating the interaction between the weekend CUS ratio and weekday sleep duration and the interaction between the weekend CUS ratio and subjective sleep quality, additional multiple logistic regression analyses were performed. Finally, we performed sub-group analyses for the association of the weekend CUS ratio with depressive symptoms and suicidal ideation, stratified by residence type and perception of stress, as two covariates are closely related to sleep and mental health in adolescents29–31. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA), and a weighted logistic regression procedure was conducted to account for the complex and stratified sampling design of the KYRBS. P-values < 0.05 were considered statistically significant.
Results
Of the 270,619 participants, 136,316 (50.4%) were male and 134,303 (49.6%) were female. Among the male and female participants, 27,448 (20.1%) vs. 41,292 (30.7%) had experienced depressive symptoms, respectively, while 12,279 (9.0%) vs. 20,535 (15.3%) had had suicidal ideation, respectively. In male participants, the rates of depressive symptoms (18.8%) and suicidal ideation (8.3%) were lower among those who had 1.00 ≤ CUS ratio < 1.50 compared with those who had CUS ratio < 1.00 (depressive symptoms, 20.5%; suicidal ideation, 10.2%) and those who had CUS ratio ≥ 1.50 (depressive symptoms, 24.0%; suicidal ideation, 10.4%). Among female participants, the rates of depressive symptoms and suicidal ideation were lower when the CUS ratio was 1.00 or more and 1.50 or less (depressive symptoms, 28.6%; suicidal ideation, 14.0%) than when the CUS ratio was less than 1.00 (depressive symptoms, 33.6%; suicidal ideation, 19.0%) or more than 1.50 (depressive symptoms, 34.1%; suicidal ideation, 16.8%). The rates of depressive symptoms and suicidal ideation were the lowest in male and female participants with good sleep quality (male: depressive symptoms, 12.2%; suicidal ideation, 5.2%; female: depressive symptoms, 18.9%; suicidal ideation, 8.6%). Further details about the participants after excluding those with missing values are presented in Table 1.
Table 1.
General characteristics of the participants.
| Depressive symptoms | Suicidal ideation | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (n = 136,316) | Female (n = 134,303) | Male (n = 136,316) | Female (n = 134,303) | |||||||||||||
| Total | Yes | P-value | Total | Yes | P-value | Total | Yes | P-value | Total | Yes | P-value | |||||
| N | N | % | N | N | % | N | N | % | N | N | % | |||||
| Total (n = 270,619) | 136,316 | 27,448 | 20.1 | 134,303 | 41,292 | 30.7 | 136,316 | 12,279 | 9.0 | 134,303 | 20,535 | 15.3 | ||||
| Weekend catch-up sleep ratioa | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| CUS < 1.00 | 19,551 | 4005 | 20.5 | 11,123 | 3740 | 33.6 | 19,551 | 1993 | 10.2 | 11,123 | 2115 | 19.0 | ||||
| 1.00 ≤ CUS < 1.50 | 87,682 | 16,471 | 18.8 | 81,045 | 23,202 | 28.6 | 87,682 | 7263 | 8.3 | 81,045 | 11,339 | 14.0 | ||||
| CUS ≥ 1.50 | 29,083 | 6972 | 24.0 | 42,135 | 14,350 | 34.1 | 29,083 | 3023 | 10.4 | 42,135 | 7081 | 16.8 | ||||
| Subjective sleep quality | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Poor | 48,455 | 13,884 | 28.7 | 66,880 | 25,483 | 38.1 | 48,455 | 6576 | 13.6 | 66,880 | 13,114 | 19.6 | ||||
| Moderate | 46,204 | 8487 | 18.4 | 42,536 | 11,093 | 26.1 | 46,204 | 3550 | 7.7 | 42,536 | 5281 | 12.4 | ||||
| Good | 41,657 | 5077 | 12.2 | 24,887 | 4716 | 18.9 | 41,657 | 2153 | 5.2 | 24,887 | 2140 | 8.6 | ||||
| Sleep duration (h)b | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Duration < 5 | 7650 | 2440 | 31.9 | 12,817 | 5474 | 42.7 | 7650 | 1262 | 16.5 | 12,817 | 2930 | 22.9 | ||||
| 5 ≤ Duration < 7 | 54,582 | 12,814 | 23.5 | 63,715 | 20,953 | 32.9 | 54,582 | 5673 | 10.4 | 63,715 | 10,258 | 16.1 | ||||
| 7 ≤ Duration < 9 | 61,075 | 10,170 | 16.7 | 49,718 | 12,786 | 25.7 | 61,075 | 4450 | 7.3 | 49,718 | 6319 | 12.7 | ||||
| Duration ≥ 9 | 11,011 | 1631 | 14.8 | 6738 | 1654 | 24.5 | 11,011 | 749 | 6.8 | 6738 | 824 | 12.2 | ||||
| School year | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Mid1 (Grade 7) | 21,065 | 3356 | 15.9 | 21,090 | 5398 | 25.6 | 21,065 | 1659 | 7.9 | 21,090 | 3117 | 14.8 | ||||
| Mid2 (Grade 8) | 21,814 | 3904 | 17.9 | 21,672 | 6545 | 30.2 | 21,814 | 2018 | 9.3 | 21,672 | 3711 | 17.1 | ||||
| Mid3 (Grade 9) | 22,950 | 4573 | 19.9 | 22,956 | 7179 | 31.3 | 22,950 | 2200 | 9.6 | 22,956 | 3861 | 16.8 | ||||
| High1 (Grade 10) | 22,845 | 4672 | 20.5 | 22,242 | 6664 | 30.0 | 22,845 | 1941 | 8.5 | 22,242 | 3116 | 14.0 | ||||
| High2 (Grade 11) | 23,735 | 5322 | 22.4 | 22,638 | 7527 | 33.2 | 23,735 | 2258 | 9.5 | 22,638 | 3459 | 15.3 | ||||
| High3 (Grade 12) | 23,907 | 5621 | 23.5 | 23,705 | 7979 | 33.7 | 23,907 | 2203 | 9.2 | 23,705 | 3271 | 13.8 | ||||
| Economic status | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Low | 3757 | 1322 | 35.2 | 3164 | 1529 | 48.3 | 3757 | 786 | 20.9 | 3164 | 969 | 30.6 | ||||
| Medium–low | 15,745 | 4071 | 25.9 | 16,797 | 6587 | 39.2 | 15,745 | 2091 | 13.3 | 16,797 | 3817 | 22.7 | ||||
| Medium | 61,109 | 11,378 | 18.6 | 66,691 | 19,359 | 29.0 | 61,109 | 4862 | 8.0 | 66,691 | 9202 | 13.8 | ||||
| Medium–high | 39,427 | 7495 | 19.0 | 37,207 | 10,840 | 29.1 | 39,427 | 3143 | 8.0 | 37,207 | 5122 | 13.8 | ||||
| High | 16,278 | 3182 | 19.5 | 10,444 | 2977 | 28.5 | 16,278 | 1397 | 8.6 | 10,444 | 1425 | 13.6 | ||||
| Residence type | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Live w/o family or relative | 6302 | 1557 | 24.7 | 5503 | 1822 | 33.1 | 6302 | 676 | 10.7 | 5503 | 857 | 15.6 | ||||
| Live with relative | 948 | 301 | 31.8 | 786 | 370 | 47.1 | 948 | 172 | 18.1 | 786 | 222 | 28.2 | ||||
| Live with family | 129,066 | 25,590 | 19.8 | 128,014 | 39,100 | 30.5 | 129,066 | 11,431 | 8.9 | 128,014 | 19,456 | 15.2 | ||||
| Academic achievement | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Low | 14,205 | 3876 | 27.3 | 12,009 | 5121 | 42.6 | 14,205 | 1847 | 13.0 | 12,009 | 2873 | 23.9 | ||||
| Medium–low | 29,622 | 6632 | 22.4 | 31,125 | 10,888 | 35.0 | 29,622 | 2998 | 10.1 | 31,125 | 5461 | 17.5 | ||||
| Medium | 37,937 | 7168 | 18.9 | 40,336 | 11,847 | 29.4 | 37,937 | 3112 | 8.2 | 40,336 | 5467 | 13.6 | ||||
| Medium–high | 33,967 | 6234 | 18.4 | 35,528 | 9604 | 27.0 | 33,967 | 2699 | 7.9 | 35,528 | 4719 | 13.3 | ||||
| High | 20,585 | 3538 | 17.2 | 15,305 | 3832 | 25.0 | 20,585 | 1623 | 7.9 | 15,305 | 2015 | 13.2 | ||||
| Alcohol status | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Ever | 60,149 | 15,470 | 25.7 | 47,097 | 18,841 | 40.0 | 60,149 | 6906 | 11.5 | 47,097 | 9791 | 20.8 | ||||
| Never | 76,167 | 11,978 | 15.7 | 87,206 | 22,451 | 25.7 | 76,167 | 5373 | 7.1 | 87,206 | 10,744 | 12.3 | ||||
| Smoking status | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Everyday | 9024 | 3107 | 34.4 | 2360 | 1342 | 56.9 | 9024 | 1362 | 15.1 | 2360 | 740 | 31.4 | ||||
| Some day | 19,173 | 5106 | 26.6 | 7629 | 3709 | 48.6 | 19,173 | 2336 | 12.2 | 7629 | 2165 | 28.4 | ||||
| Never | 108,119 | 19,235 | 17.8 | 124,314 | 36,241 | 29.2 | 108,119 | 8581 | 7.9 | 124,314 | 17,630 | 14.2 | ||||
| Physical activity | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Low | 56,134 | 10,764 | 19.2 | 92,236 | 27,728 | 30.1 | 56,134 | 5246 | 9.3 | 92,236 | 13,514 | 14.7 | ||||
| High | 80,182 | 16,684 | 20.8 | 42,067 | 13,564 | 32.2 | 80,182 | 7033 | 8.8 | 42,067 | 7021 | 16.7 | ||||
| Self-reported health status | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Low | 6915 | 2622 | 37.9 | 10,402 | 5644 | 54.3 | 6915 | 1699 | 24.6 | 10,402 | 3659 | 35.2 | ||||
| Medium | 24,503 | 6374 | 26.0 | 34,433 | 13,152 | 38.2 | 24,503 | 3290 | 13.4 | 34,433 | 6974 | 20.3 | ||||
| High | 104,898 | 18,452 | 17.6 | 89,468 | 22,496 | 25.1 | 104,898 | 7290 | 6.9 | 89,468 | 9902 | 11.1 | ||||
| Perception of stress | < 0.001 | < 0.001 | < 0.001 | < 0.001 | ||||||||||||
| Low | 34,481 | 1956 | 5.7 | 18,385 | 1272 | 6.9 | 34,481 | 596 | 1.7 | 18,385 | 443 | 2.4 | ||||
| Medium | 60,140 | 8961 | 14.9 | 54,611 | 10,555 | 19.3 | 60,140 | 2798 | 4.7 | 54,611 | 3558 | 6.5 | ||||
| High | 41,695 | 16,531 | 39.6 | 61,307 | 29,465 | 48.1 | 41,695 | 8885 | 21.3 | 61,307 | 16,534 | 27.0 | ||||
aWeekend sleep duration/weekday sleep duration.
bAverage sleep duration of weekday and weekend.
Table 2 presents the adjusted odds ratio (aOR) of factors associated with depressive symptoms and suicidal behaviors. For both male and female participants, a weekend CUS ratio of < 1.00 was significantly associated with depressive symptoms (male: aOR, 1.05; 95% confidence interval [CI] 1.00–1.11; female: aOR, 1.10; 95% CI 1.04–1.16) and suicidal ideation (male: aOR, 1.11; 95% CI 1.08–1.22; female: aOR, 1.15; 95% CI 1.08–1.23). However, when the weekend CUS ratio was ≥ 1.50, the odds of having depressive symptoms was significantly higher in female participants (aOR, 1.04; 95% CI 1.01–1.08) than in male participants. Both male and female participants with poor subjective sleep quality were more likely to experience depressive symptoms (male: aOR, 1.48; 95% CI 1.41–1.55; female: aOR, 1.35; 95% CI 1.29–1.41) and suicidal ideation (male: aOR, 1.39; 95% CI 1.30–1.48; female: aOR, 1.25; 95% CI 1.18–1.33), respectively, than those with good sleep quality. Additionally, the odds of depressive symptoms (male: aOR, 1.40; 95% CI 1.31–1.50; female: aOR, 1.38; 95% CI 1.31–1.45) and suicidal ideation (male: aOR, 1.65; 95% CI 1.51–1.80; female: aOR, 1.58; 95% CI 1.49–1.69) increased as the average weekday and weekend sleep duration decreased to < 5 h in male and female participants, respectively, compared with that of participants with more than 7 h and less than 9 h of sleep on average. Other factors related to depressive symptoms or suicidal ideation are also described in Table 1.
Table 2.
Factors associated with depressive symptoms and suicidal behaviors.
| Variables | Depressive symptoms | Suicidal ideation | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||||
| aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | aOR | 95% CI | |
| Weekend catch-up sleep ratioa | ||||||||
| CUS < 1.00 | 1.05 | (1.00–1.11) | 1.10 | (1.04–1.16) | 1.11 | (1.08–1.22) | 1.15 | (1.08–1.23) |
| 1.00 ≤ CUS < 1.50 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| CUS ≥ 1.50 | 1.02 | (0.98–1.06) | 1.04 | (1.01–1.08) | 0.97 | (0.91–1.02) | 1.02 | (0.98–1.06) |
| Subjective sleep quality | ||||||||
| Poor | 1.48 | (1.41–1.55) | 1.35 | (1.29–1.41) | 1.39 | (1.30–1.48) | 1.25 | (1.18–1.33) |
| Moderate | 1.22 | (1.17–1.28) | 1.10 | (1.05–1.15) | 1.15 | (1.08–1.22) | 1.07 | (1.01–1.14) |
| Good | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Sleep duration (h)b | ||||||||
| Duration < 5 | 1.40 | (1.31–1.50) | 1.38 | (1.31–1.45) | 1.65 | (1.51–1.80) | 1.58 | (1.49–1.69) |
| 5 ≤ Duration < 7 | 1.17 | (1.13–1.22) | 1.13 | (1.10–1.18) | 1.23 | (1.16–1.30) | 1.20 | (1.15–1.26) |
| 7 ≤ Duration < 9 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Duration ≥ 9 | 0.96 | (0.90–1.03) | 1.01 | (0.94–1.08) | 1.04 | (0.94–1.14) | 0.96 | (0.87–1.05) |
| School year | ||||||||
| Mid1 (Grade 7) | 1.12 | (1.04–1.19) | 1.30 | (1.23–1.38) | 1.76 | (1.60–1.94) | 2.52 | (2.34–2.72) |
| Mid2 (Grade 8) | 1.12 | (1.05–1.19) | 1.39 | (1.31–1.46) | 1.85 | (1.69–2.02) | 2.45 | (2.28–2.63) |
| Mid3 (Grade 9) | 1.22 | (1.15–1.29) | 1.38 | (1.31–1.46) | 1.78 | (1.64–1.94) | 2.17 | (2.02–2.33) |
| High1 (Grade 10) | 1.01 | (0.96–1.07) | 1.04 | (0.99–1.09) | 1.21 | (1.12–1.32) | 1.37 | (1.28–1.47) |
| High2 (Grade 11) | 1.00 | (0.95–1.05) | 1.06 | (1.01–1.12) | 1.18 | (1.09–1.27) | 1.28 | (1.20–1.36) |
| High3 (Grade 12) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Economic status | ||||||||
| Low | 1.24 | (1.13–1.36) | 1.16 | (1.05–1.28) | 1.58 | (1.41–1.78) | 1.57 | (1.39–1.77) |
| Medium–low | 0.94 | (0.88–1.00) | 0.95 | (0.89–1.02) | 1.07 | (0.98–1.17) | 1.27 | (1.17–1.38) |
| Medium | 0.81 | (0.77–0.86) | 0.81 | (0.76–0.85) | 0.81 | (0.75–0.88) | 0.88 | (0.82–0.94) |
| Medium–high | 0.91 | (0.86–0.96) | 0.91 | (0.86–0.96) | 0.87 | (0.81–0.95) | 0.95 | (0.88–1.02) |
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Residence type | ||||||||
| Live w/o family or relative | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Live with relative | 1.39 | (1.15–1.68) | 1.57 | (1.28–1.92) | 1.53 | (1.20–1.94) | 1.52 | (1.22–1.88) |
| Live with family | 0.88 | (0.82–0.96) | 0.97 | (0.90–1.05) | 0.85 | (0.77–0.94) | 0.93 | (0.85–1.03) |
| Academic achievement | ||||||||
| Low | 1.36 | (1.27–1.46) | 1.60 | (1.50–1.70) | 1.17 | (1.07–1.28) | 1.31 | (1.21–1.43) |
| Medium–low | 1.29 | (1.22–1.37) | 1.43 | (1.36–1.51) | 1.19 | (1.10–1.28) | 1.19 | (1.11–1.28) |
| Medium | 1.17 | (1.10–1.24) | 1.26 | (1.20–1.33) | 1.11 | (1.03–1.20) | 1.03 | (0.96–1.10) |
| Medium–high | 1.11 | (1.05–1.17) | 1.11 | (1.06–1.17) | 1.04 | (0.97–1.12) | 1.02 | (0.95–1.09) |
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Alcohol status | ||||||||
| Ever | 1.41 | (1.36–1.46) | 1.51 | (1.46–1.56) | 1.37 | (1.30–1.43) | 1.54 | (1.48–1.61) |
| Never | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Smoking status | ||||||||
| Everyday | 1.62 | (1.52–1.73) | 1.88 | (1.69–2.11) | 1.46 | (1.34–1.58) | 1.63 | (1.45–1.83) |
| Some day | 1.27 | (1.21–1.33) | 1.48 | (1.39–1.58) | 1.28 | (1.21–1.36) | 1.53 | (1.43–1.64) |
| Never | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Physical activity | ||||||||
| Low | 0.77 | (0.75–0.80) | 0.83 | (0.80–0.85) | 0.93 | (0.89–0.97) | 0.84 | (0.80–0.87) |
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Self-reported health status | ||||||||
| Low | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Medium | 0.75 | (0.70–0.81) | 0.69 | (0.65–0.73) | 0.62 | (0.57–0.67) | 0.59 | (0.56–0.63) |
| High | 0.63 | (0.59–0.67) | 0.51 | (0.48–0.53) | 0.42 | (0.39–0.46) | 0.40 | (0.37–0.42) |
| Perception of stress | ||||||||
| Low | 0.12 | (0.11–0.13) | 0.11 | (0.10–0.12) | 0.09 | (0.08–0.10) | 0.09 | (0.08–0.10) |
| Medium | 0.31 | (0.30–0.32) | 0.32 | (0.31–0.33) | 0.22 | (0.21–0.24) | 0.24 | (0.23–0.25) |
| High | 1.00 | 1.00 | 1.00 | 1.00 | ||||
aWeekend sleep duration/weekday sleep duration.
bAverage sleep duration of weekday and weekend.
aOR adjusted odds ratio, CI Confidence Interval.
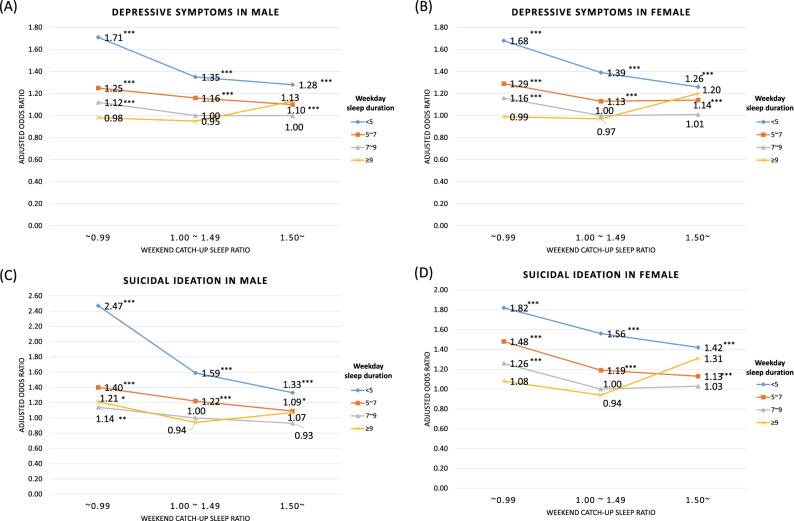
Figure 1 shows the multiple logistic regression results for the interaction between the weekend CUS ratio and weekday sleep duration. After adjusting for covariates, both male and female participants with a weekday sleep duration of < 5 h and weekend CUS ratio of < 1.00 had the highest odds of experiencing depressive symptoms (male: aOR, 1.71; 95% CI 1.43–2.05; female: aOR, 1.68; 95% CI 1.45–1.95) and suicidal ideation (male: aOR, 2.47; 95% CI 1.99–3.06; female: aOR, 1.82; 95% CI 1.55–2.14). In contrast, participants with a weekday sleep duration of ≥ 9 h and weekend CUS ratio of > 1.50 showed slightly higher odds of having depressive symptoms and suicidal ideation, although the results were not significant.
Figure 1.
Results of the multiple logistic regression analysis, including interaction between weekend CUS ratio and weekday sleep duration. *P value < 0.05; ** < 0.01; *** < 0.001. CUS catch-up sleep.
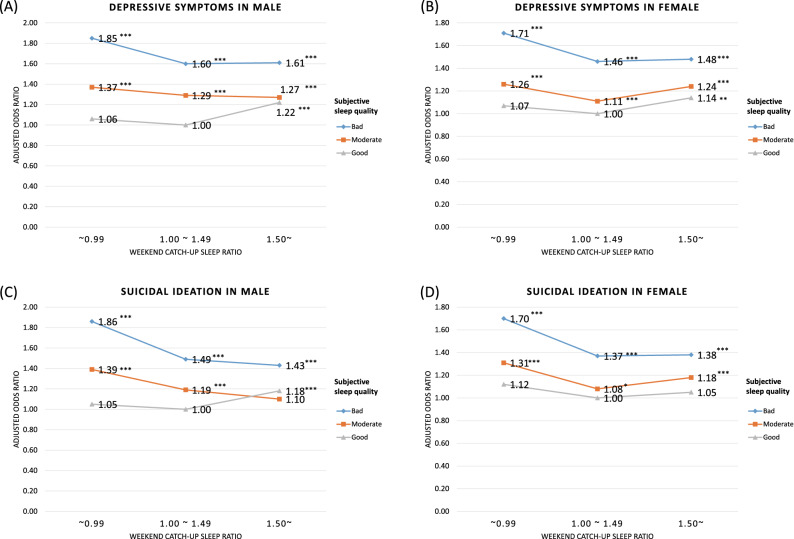
Figure 2 shows the multiple logistic regression results for the interaction between the weekend CUS ratio and subjective sleep quality. After adjusting for covariates, male and female adolescents with poor subjective sleep quality and a weekend CUS ratio of < 1.00 had increased odds of having depressive symptoms (male: aOR, 1.85; 95% CI 1.70–2.01; female: aOR, 1.71; 95% CI 1.57–1.86) and suicidal ideation (male: aOR, 1.86; 95% CI 1.67–2.08; female: aOR, 1.70; 95% CI 1.53–1.87). Even male and female participants with good subjective sleep quality showed slightly higher odds of depressive symptoms (male: aOR, 1.22; 95% CI 1.12–1.34; female: aOR, 1.14; 95% CI 1.03–1.25) and suicidal ideation (male: aOR, 1.18; 95% CI 1.03–1.36; female: aOR, 1.05; 95% CI 0.91–1.21) when the weekend CUS ratio was ≥ 1.50.
Figure 2.
Results of the multiple logistic regression analysis, including interaction between weekend CUS ratio and subjective sleep quality. *P value < 0.05; ** < 0.01; *** < 0.001. CUS catch-up sleep.
Table 3 presents the sub-group analyses of the association of the weekend CUS ratio with depressive symptoms and suicidal ideation stratified by independent variables. Male and female participants with a weekend CUS ratio of < 1.00 who lived with relatives showed higher depressive symptoms (male: aOR, 2.08; 95% CI 1.29–3.35; female: aOR, 1.85; 95% CI 1.02–3.37) and suicidal ideation (male: aOR, 2.67; 95% CI 1.53–4.67; female: aOR, 1.89; 95% CI 1.03–3.48) than those who did not live with family or relatives. Male and female adolescents with low perceived stress levels and a weekend CUS ratio of < 1.00 also showed higher depressive symptoms (male: aOR, 1.37; 95% CI 1.20–1.57; female: aOR, 1.37; 95% CI 1.10–1.71), although the association with suicidal ideation was observed in male participants only (aOR, 2.13; 95% CI 1.70–2.67).
Table 3.
Results of analyses of association of weekend catch-up sleep ratio with depressive symptoms and suicidal ideation stratified by independent variables after adjusting for all covariates.
| Variables | Depressive symptoms | Suicidal ideation | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Weekend catch-up sleep ratio | Weekend catch-up sleep ratio | |||||||||
| CUS < 1.00 | 1.00 ≤ CUS < 1.50 | CUS ≥ 1.50 | CUS < 1.00 | 1.00 ≤ CUS < 1.50 | CUS ≥ 1.50 | |||||
| aOR | 95% CI | aOR | aOR | 95% CI | aOR | 95% CI | aOR | aOR | 95% CI | |
| Male | ||||||||||
| Residence type | ||||||||||
| Live w/o family or relative | 1.23 | (0.98–1.53) | 1.00 | 1.01 | (0.86–1.19) | 1.38 | (1.03–1.85) | 1.00 | 0.95 | (0.75–1.21) |
| Live with relative | 2.08 | (1.29–3.35) | 1.00 | 0.72 | (0.48–1.07) | 2.67 | (1.53–4.67) | 1.00 | 0.67 | (0.40–1.12) |
| Live with family | 1.08 | (1.02–1.13) | 1.00 | 1.02 | (0.98–1.06) | 1.14 | (1.07–1.22) | 1.00 | 0.98 | (0.93–1.03) |
| Perception of stress | ||||||||||
| Low | 1.37 | (1.20–1.57) | 1.00 | 0.96 | (0.84–1.10) | 2.13 | (1.70–2.67) | 1.00 | 1.08 | (0.84–1.37) |
| Medium | 1.12 | (1.04–1.21) | 1.00 | 1.04 | (0.97–1.10) | 1.17 | (1.04–1.32) | 1.00 | 0.96 | (0.86–1.06) |
| High | 1.01 | (0.95–1.08) | 1.00 | 1.01 | (0.96–1.07) | 1.09 | (1.01–1.17) | 1.00 | 0.97 | (0.92–1.03) |
| Female | ||||||||||
| Residence type | ||||||||||
| Live w/o family or relative | 1.33 | (1.03–1.72) | 1.00 | 1.04 | (0.89–1.21) | 1.51 | (1.09–2.08) | 1.00 | 1.07 | (0.88–1.31) |
| Live with relative | 1.85 | (1.02–3.37) | 1.00 | 1.06 | (0.73–1.54) | 1.89 | (1.03–3.48) | 1.00 | 1.19 | (0.77–1.83) |
| Live with family | 1.12 | (1.06–1.18) | 1.00 | 1.03 | (1.00–1.07) | 1.19 | (1.12–1.27) | 1.00 | 1.03 | (0.99–1.08) |
| Perception of stress | ||||||||||
| Low | 1.37 | (1.10–1.71) | 1.00 | 1.01 | (0.87–1.18) | 1.39 | (0.99–1.95) | 1.00 | 1.21 | (0.93–1.57) |
| Medium | 1.10 | (1.01–1.20) | 1.00 | 1.04 | (0.99–1.10) | 1.19 | (1.04–1.35) | 1.00 | 1.01 | (0.93–1.10) |
| High | 1.12 | (1.05–1.20) | 1.00 | 1.03 | (0.99–1.07) | 1.21 | (1.13–1.30) | 1.00 | 1.04 | (0.99–1.09) |
CUS catch-up sleep, w/o without, aOR adjusted odds ratio, CI Confidence interval.
Discussion
In this study, both male and female adolescents whose weekend CUS ratio was 1.00–1.49 had fewer depressive symptoms and less suicidal ideation. Further, fewer depressive symptoms and less suicidal ideation were observed in participants with better subjective sleep quality. This demonstrates that the imbalance between weekday and weekend sleep was associated with experiencing depressive symptoms and suicidal ideation in adolescents.
To cope with weekday sleep debt, weekend CUS is associated with a lower prevalence of obesity, hypertension, anxiety, and depression32,33. Moreover, a recent study of South Korean high school students reported that adolescents’ weekend CUS duration of > 2 h is associated with a lower risk of depression19. However, no studies have confirmed whether longer weekend CUS is associated with depression and suicidal ideation, which are important mental health conditions in adolescents, although a long sleep duration may have adverse health effects34,35. To the best of our knowledge, this is the first study to confirm, using the weekend CUS ratio, that an imbalance between weekday and weekend hours is associated with increased odds of depressive symptoms and suicidal ideation in adolescents.
In our study, adolescents with a weekday sleep duration of < 5 h and weekend CUS ratio of < 1.00 showed particularly high levels of depressive symptoms and suicidal ideation. It is estimated that such results are due to an absolute lack of sleep. It has been reported that irritation, anxiety, and feelings of worthlessness are found in adolescents with a short sleep duration36. Shorter-duration sleepers are also less motivated and more likely to have trouble focusing36. Our findings support previous research showing that short sleep duration, including during weekends, can be associated with depressive symptoms or suicidal feeling in adolescents18,36,37.
When the quality of sleep and the CUS ratio were considered concurrently in adolescents with good sleep quality, no association between depressive symptoms and suicidal ideation was observed even if the CUS ratio was < 1.00. However, contrary to our expectation, if adolescents with good subjective sleep quality have a ≥ 1.50 times longer sleep duration on weekends than on weekdays, the odds of having depressive symptoms increases. One of the causes of reward-related problems, such as depression, may be circadian misalignment, which implies greater weekend–weekday advances in mid-sleep38. Circadian misalignment is associated with a decrease in the medial prefrontal cortex and striatal reactivity to reward, which may reflect a decreased reward sensitivity38. Sleep–wake homeostatic dynamics might also have influenced these results39,40. Moreover, while insufficient sleep is obviously associated with negative health effects, habitual excessive sleep can also increase mortality risks. In contrast, long sleep may lead to sleep fragmentation, fatigue, depression, photoperiodic abnormalities, or lack of challenge, which establishes a mortality link41. These results also suggest that the circadian misalignment can be compensated to some extent by the subjectively perceived quality of sleep, but if the degree of misalignment is severe, the compensatory effect disappears. Further biological studies are needed to clarify the causes of long sleep duration or how circadian misalignment adversely affects the mental health of adolescents.
We performed sub-group analyses considering the effect of family environment on sleep disorders29, the relationship between family environment and mental health30, and the relationship between perceived stress and sleep duration with metal health31. In the stratified analysis, the trend of association was significant, depending on residence type and perception of stress. When the weekend CUS ratio was < 1.00, male and female adolescents living with relatives or with low perceived stress levels were more likely to experience depressive symptoms and suicidal ideation. Previous studies reported that adolescents living apart from one or both biological parents showed association with suicidality30,42. However, to the best of our knowledge, no study has investigated the association between mental health and sleep duration, especially weekend CUS, among adolescents living with relatives. Our results imply that both the living environment and sleep-related factors should be considered to safeguard the mental health of adolescents who do not live with their parents. Furthermore, since the absolute lack or imbalance between weekday and weekend sleep durations had a greater effect on adolescents with low stress levels, an approach that considers the weekend CUS ratio is necessary in diagnosing and treating adolescent mental health disorders, in addition to the stress level.
Although the absolute amount of sleep is supposed to have more influence on the level of depressive symptoms and suicidal ideation than the weekend CUS ratio, the balance of sleep duration between weekdays and weekends also showed a meaningful association with the level of depressive symptoms and suicidal ideation after adjusting for average weekday and weekend sleep durations. In fact, previous findings also indicated that adolescents experience longer sleep duration on weekends than on weekdays14,20. This is the consequence of delayed circadian phase and compensation of the sleep debt from the weekdays’ lack of sleep in the form of weekend CUS43. Hence, to protect adolescents from depressive symptoms and suicidal ideation, we should identify ways to achieve balance of sleep duration between weekdays and weekends, as well as a sufficient amount of sleep. With sufficient amounts of sleep, good balance of sleep duration between weekdays and weekends and subjectively good quality of sleep can lower the level of adolescents’ depressive symptoms and suicidal ideation.
Therefore, we should recognize the importance of sleep hygiene education and sleep intervention to prevent depression or suicide in adolescents. Furthermore, personal and institutional efforts must be undertaken, which should include the provision of social systems and campaigns for sufficient sleep with good balance and quality44. Additionally, personal efforts are needed to maintain enough sleep with good balance and quality. Further research is needed to investigate the psychosocial and neurobiological mechanisms to explain the association of inadequate balance of sleep duration between weekdays and weekends with adolescents’ mental health.
Previous studies using the KYRBS suggested that sleep duration and sleeping time are associated with mental health concerns such as suicidal behaviors27,45–48. That is, a sleep duration of less than 4 h was associated with suicidal ideation45–47, and a prolonged time to fall asleep and wake up was also associated with suicidal ideation and suicidal ideation27,48. Our research is meaningful because we additionally analyzed the balance of sleep duration between weekdays and weekends using a “weekend CUS ratio.” Overall, our findings serve as a warning regarding the risk of depression or suicidal behaviors in adolescents with an imbalance of sleep duration between weekdays and weekends, and this is an important hypothesis to be confirmed in future neurobiological studies. Furthermore, because this cross-sectional study used multiyear national survey data (2015–2019) with 270,619 respondents based on random cluster sampling, our results were sufficiently representative of South Korean adolescents30,49. Additionally, we considered many covariates to increase the credibility and accuracy of our study.
Despite these strengths, our study had some limitations. First, the study’s cross-sectional design did not allow us to clearly identify the direction of the association of weekend CUS and subjective sleep quality with depressive symptoms and suicidal ideation. Second, the results of this study were based on anonymous self-reported data. Thus, the weekend CUS ratio and subjective sleep quality might have been underestimated or overestimated, and some survey questions might be subject to recall bias30. Third, as the dependent variables, depressive symptoms and suicidal ideation, consist of single-item questions like other population-based studies such as YRBS50,51, it may have caused measurement problems and misclassification52. However, according to the results of one study, the reliability of the questionnaire for depressive symptoms and suicidal ideation in YRBS, was “moderate” or higher53. Since KYRBS uses a questionnaire similar to YRBS, reliability can be guaranteed to a certain extent, but additional studies are needed. Moreover, the previous study that shorter of longer sleep duration was associated with the depressive symptoms measured by Patient Health Questionnaire helps to give meaning to this study that suggested the relationship between the CUS ratio, one of the characteristics of sleep, and depressive symptoms54–56. Finally, despite our efforts to control for confounding factors, not all covariates affecting depressive symptoms and suicidal ideation were considered. Therefore, the possibility of residual confounding cannot be eliminated.
In conclusion, our study demonstrated that both male and female adolescents with a weekend CUS ratio of < 1.00 were significantly more likely to have depressive symptoms and suicidal ideation. Furthermore, poor sleep quality was associated with increased odds of having depressive symptoms and suicidal ideation. Male and female adolescents with a weekday sleep duration of < 5 h and weekend CUS ratio of < 1.00 showed the highest increased odds of depressive symptoms and suicidal ideation. In contrast, adolescents with good subjective sleep quality and a weekend CUS ratio of ≥ 1.50 showed a higher prevalence of depressive symptoms. Further study is needed to examine the neurobiological mechanisms underlying the association of the balance of sleep duration with adolescents’ mental health. At the same time, policy makers need to consider appropriate education and interventions that can balance sleep duration on weekdays and weekends, as well as adequate sleep duration during weekdays, to improve adolescents’ mental health.
Acknowledgements
We would like to thank the Korea Disease Control and Prevention Agency, which provided the data based on a nationwide survey.
Author contributions
Contribution to the study design: H.L., Y.-J.K., Y.-H.J., S.H.K., and E.-C.P. Collection of data: H.L., Y.-J.K., and Y.-H.J. Analysis and interpretation of data: H.L., Y.-J.K., Y.-H.J., S.H.K., and E.-C.P. Drafting the manuscript: H.L., Y.-J.K., Y.-H.J., and S.H.K. Critical revision for intellectual content: S.H.K. and E.-C.P. Approval of the final version of manuscript: H.L., Y.-J.K., Y.-H.J., S.H.K., and E.-C.P.
Data availability
All the KYRBS data used this study are available to the public and can be seen in the KYRBS official website (http://www.kdca.go.kr/yhs/).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Hyunseo Lee, Yeon-Jeong Kim and Yong-Hyun Jeon.
Contributor Information
Seung Hoon Kim, Email: shoonkim@yuhs.ac.
Eun-Cheol Park, Email: ecpark@yuhs.ac.
References
- 1.Fallone G, Seifer R, Acebo C, Carskadon MA. How well do school-aged children comply with imposed sleep schedules at home? Sleep. 2002;25:739–745. doi: 10.1093/sleep/25.7.739. [DOI] [PubMed] [Google Scholar]
- 2.Kolomeichuk SN, Randler C, Morozov AV, Gubin DG, Drake CL. Social Jetlag and excessive daytime sleepiness from a sample of Russian children and adolescents. Nat. Sci. Sleep. 2021;13:729–737. doi: 10.2147/NSS.S290895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J. Abnorm. Psychol. 1993;102:133–144. doi: 10.1037/0021-843X.102.1.133. [DOI] [PubMed] [Google Scholar]
- 4.Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress. Anxiety. 2009;26:503–512. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- 5.Liu JW, et al. Associations between sleep disturbances and suicidal ideation, plans, and attempts in adolescents: A systematic review and meta-analysis. Sleep. 2019;42:66. doi: 10.1093/sleep/zsz054. [DOI] [PubMed] [Google Scholar]
- 6.Cespedes Feliciano EM, et al. Chronotype, Social Jet Lag, and cardiometabolic risk factors in early adolescence. JAMA Pediatr. 2019;173:1049–1057. doi: 10.1001/jamapediatrics.2019.3089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang SC, et al. Association of health literacy and sleep problems with mental health of Chinese students in combined junior and senior high school. PLoS ONE. 2019;14:e0217685. doi: 10.1371/journal.pone.0217685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raniti MB, et al. Sleep duration and sleep quality: Associations with depressive symptoms across adolescence. Behav. Sleep Med. 2017;15:198–215. doi: 10.1080/15402002.2015.1120198. [DOI] [PubMed] [Google Scholar]
- 9.Augner C. Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in students. Cent. Eur. J. Public Health. 2011;19:115–117. doi: 10.21101/cejph.a3647. [DOI] [PubMed] [Google Scholar]
- 10.Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? Am. J. Health Behav. 2010;34:237–248. doi: 10.5993/AJHB.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun W, Ling J, Zhu X, Lee TM, Li SX. Associations of weekday-to-weekend sleep differences with academic performance and health-related outcomes in school-age children and youths. Sleep Med. Rev. 2019;46:27–53. doi: 10.1016/j.smrv.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–1358. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 13.Liu BP, et al. Depressive symptoms are associated with short and long sleep duration: A longitudinal study of Chinese adolescents. J. Affect. Disord. 2020;263:267–273. doi: 10.1016/j.jad.2019.11.113. [DOI] [PubMed] [Google Scholar]
- 14.Yang CK, Kim JK, Patel SR, Lee JH. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics. 2005;115:250–256. doi: 10.1542/peds.2004-0815G. [DOI] [PubMed] [Google Scholar]
- 15.Sunwoo JS, et al. Sleep duration rather than sleep timing is associated with obesity in adolescents. Sleep Med. 2020;68:184–189. doi: 10.1016/j.sleep.2019.12.014. [DOI] [PubMed] [Google Scholar]
- 16.Kwak CW, Ickovics JR. Adolescent suicide in South Korea: Risk factors and proposed multi-dimensional solution. Asian J. Psychiatr. 2019;43:150–153. doi: 10.1016/j.ajp.2019.05.027. [DOI] [PubMed] [Google Scholar]
- 17.Lee YJ, Park J, Kim S, Cho SJ, Kim SJ. Academic performance among adolescents with behaviorally induced insufficient sleep syndrome. J. Clin. Sleep Med. 2015;11:61–68. doi: 10.5664/jcsm.4368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kang SG, et al. Weekend catch-up sleep is independently associated with suicide attempts and self-injury in Korean adolescents. Compr. Psychiatry. 2014;55:319–325. doi: 10.1016/j.comppsych.2013.08.023. [DOI] [PubMed] [Google Scholar]
- 19.Koo DL, et al. Association between morningness-eveningness, sleep duration, weekend catch-up sleep and depression among Korean high-school students. J. Sleep Res. 2021;30:e13063. doi: 10.1111/jsr.13063. [DOI] [PubMed] [Google Scholar]
- 20.Matthews KA, Hall M, Dahl RE. Sleep in healthy black and white adolescents. Pediatrics. 2014;133:e1189–1196. doi: 10.1542/peds.2013-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang J, et al. Sleep patterns and mental health correlates in US adolescents. J. Pediatr. 2017;182:137–143. doi: 10.1016/j.jpeds.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006;23:497–509. doi: 10.1080/07420520500545979. [DOI] [PubMed] [Google Scholar]
- 23.Knapen SE, et al. Social jetlag and depression status: Results obtained from the Netherlands study of depression and anxiety. Chronobiol. Int. 2018;35:1–7. doi: 10.1080/07420528.2017.1374966. [DOI] [PubMed] [Google Scholar]
- 24.Han CH, Chung JH. Association of asthma and sleep insufficiency among South Korean adolescents: Analysis of web-based self-reported data from the Korean youth risk behavior web-based survey. J. Asthma. 2020;57:253–261. doi: 10.1080/02770903.2019.1565827. [DOI] [PubMed] [Google Scholar]
- 25.Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum. Psychopharmacol. 2008;23:571–585. doi: 10.1002/hup.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim Y, et al. Data resource profile: The Korea Youth Risk Behavior Web-based Survey (KYRBS) Int. J. Epidemiol. 2016;45:1076–1076e. doi: 10.1093/ije/dyw172. [DOI] [PubMed] [Google Scholar]
- 27.Jeong W, et al. Association of bedtime with both suicidal ideation and suicide planning among Korean adolescents. Int. J. Environ. Res. Public Health. 2019;16:66. doi: 10.3390/ijerph16203817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hankin BL, Mermelstein R, Roesch L. Sex differences in adolescent depression: Stress exposure and reactivity models. Child Dev. 2007;78:279–295. doi: 10.1111/j.1467-8624.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- 29.Billows M, et al. Family disorganization, sleep hygiene, and adolescent sleep disturbance. J. Clin. Child Adoles. Psychol. 2009;53(38):745–752. doi: 10.1080/15374410903103635. [DOI] [PubMed] [Google Scholar]
- 30.Kim SH, Jeong SH, Park EC, Jang SI. Association of cigarette type initially smoked with suicidal behaviors among adolescents in Korea from 2015 to 2018. JAMA Netw. Open. 2021;4:e218803. doi: 10.1001/jamanetworkopen.2021.8803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Y, et al. The mediating role of sleep quality on the relationship between perceived stress and depression among the elderly in urban communities: A cross-sectional study. Public Health. 2017;149:21–27. doi: 10.1016/j.puhe.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 32.Hwangbo Y, Kim WJ, Chu MK, Yun CH, Yang KI. Association between weekend catch-up sleep duration and hypertension in Korean adults. Sleep Med. 2013;14:549–554. doi: 10.1016/j.sleep.2013.02.009. [DOI] [PubMed] [Google Scholar]
- 33.Im HJ, et al. Association between weekend catch-up sleep and lower body mass: Population-based study. Sleep. 2017;40:66. doi: 10.1093/sleep/zsx089. [DOI] [PubMed] [Google Scholar]
- 34.Park S, et al. Short or long sleep duration and CKD: A Mendelian randomization study. J Am Soc Nephrol. 2020;31:2937–2947. doi: 10.1681/ASN.2020050666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Millman RP. Excessive sleepiness in adolescents and young adults: Causes, consequences, and treatment strategies. Pediatrics. 2005;115:1774–1786. doi: 10.1542/peds.2005-0772. [DOI] [PubMed] [Google Scholar]
- 36.Yeo SC, et al. Associations of sleep duration on school nights with self-rated health, overweight, and depression symptoms in adolescents: Problems and possible solutions. Sleep Med. 2019;60:96–108. doi: 10.1016/j.sleep.2018.10.041. [DOI] [PubMed] [Google Scholar]
- 37.Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35:455–460. doi: 10.5665/sleep.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hasler BP, et al. Weekend-weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biol. Psychol. 2012;91:334–341. doi: 10.1016/j.biopsycho.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jenni OG, van Reen E, Carskadon MA. Regional differences of the sleep electroencephalogram in adolescents. J. Sleep Res. 2005;14:141–147. doi: 10.1111/j.1365-2869.2005.00449.x. [DOI] [PubMed] [Google Scholar]
- 40.Duffy JF, et al. Workshop report. Circadian rhythm sleep–wake disorders: Gaps and opportunities. Sleep. 2021;44:66. doi: 10.1093/sleep/zsaa281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Med. Rev. 2007;11:341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J. Child Psychol. Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 43.Crowley SJ, Acebo C, Carskadon MA. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8:602–612. doi: 10.1016/j.sleep.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 44.Meltzer LJ, Wahlstrom KL, Plog AE, Strand MJ. Changing school start times: Impact on sleep in primary and secondary school students. Sleep. 2021;6:66. doi: 10.1093/sleep/zsab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim Y, Kim K, Kwon H-J, Kim J-S. Associations between adolescents' sleep duration, sleep satisfaction, and suicidal ideation. Salud Ment. 2016;39:213–219. doi: 10.17711/SM.0185-3325.2016.025. [DOI] [Google Scholar]
- 46.Park T-J, Kim J. Is insufficient sleep duration associated with suicidal behavior in Korean adolescents? Sleep Biol. Rhythms. 2017;15:117–125. doi: 10.1007/s41105-016-0087-1. [DOI] [Google Scholar]
- 47.Park WS, Yang KI, Kim H. Insufficient sleep and suicidal ideation: A survey of 12,046 female adolescents. Sleep Med. 2019;53:65–69. doi: 10.1016/j.sleep.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 48.Kim JH, Park EC, Lee SG, Yoo KB. Associations between time in bed and suicidal thoughts, plans and attempts in Korean adolescents. BMJ Open. 2015;5:e008766. doi: 10.1136/bmjopen-2015-008766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kim HJ, Oh SY, Lee DW, Kwon J, Park E-C. The effects of intense physical activity on stress in adolescents: Findings from Korea Youth Risk Behavior Web-Based Survey (2015–2017) BMJ Open. 2019;16:1870. doi: 10.3390/ijerph16101870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lowry R, Crosby AE, Brener ND, Kann L. Suicidal thoughts and attempts among U.S. High school students: Trends and associated health-risk behaviors, 1991–2011. J. Adoles. Health. 2014;54:100–108. doi: 10.1016/j.jadohealth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 51.Nock MK, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6:e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Millner AJ, Lee MD, Nock MK. Single-item measurement of suicidal behaviors: Validity and consequences of misclassification. PLoS ONE. 2015;10:e0141606. doi: 10.1371/journal.pone.0141606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brener ND, et al. Reliability of the 1999 youth risk behavior survey questionnaire. J. Adoles. Health. 2002;31:336–342. doi: 10.1016/S1054-139X(02)00339-7. [DOI] [PubMed] [Google Scholar]
- 54.Moitra P, Madan J, Shaikh NI. Eating habits and sleep patterns of adolescents with depression symptoms in Mumbai, India. Maternal Child Nutr. 2020;16(Suppl 3):e12998. doi: 10.1111/mcn.12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim HM, Lee SW. Beneficial effects of appropriate sleep duration on depressive symptoms and perceived stress severity in a healthy population in Korea. Korean J. Fam. medicine. 2018;39:57–61. doi: 10.4082/kjfm.2018.39.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiang J, et al. Abnormal night sleep duration and poor sleep quality are independently and combinedly associated with elevated depressive symptoms in Chinese rural adults: Henan Rural Cohort. Sleep Med. 2020;70:71–78. doi: 10.1016/j.sleep.2019.10.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the KYRBS data used this study are available to the public and can be seen in the KYRBS official website (http://www.kdca.go.kr/yhs/).