Abstract
We investigated the effect of hydroxychloroquine (HCQ) as an add-on treatment to immunosuppressants on the expression of proinflammatory cytokines in patients with systemic lupus erythematosus. Serum levels of tumor necrosis factor (TNF)-α, interleukin (IL)-2, IL-6, IL-8, vascular endothelial growth factor (VEGF)-A, monocyte chemotactic protein-1 (MCP-1), macrophage inflammatory protein-1α (MIP-1α), and interleukin 1 receptor antagonist (IL-1ra) were measured immediately before and 3 months after treatment with oral HCQ. Among the 51 patients enrolled in the study, HCQ treatment led to significantly reduced serum levels of TNF-α, IL-6, IL-8, VEGF-A, IL-1ra, and IL-2 (p < 0.0001; p = 0.0006; p = 0.0460, p = 0.0177; p < 0.0001; p = 0.0282, respectively) and to decreased (but not significantly) levels of MIP-1α (p = 0.0746). No significant changes were observed in the serum MCP-1 levels before and after HCQ administration (p = 0.1402). Our results suggest that an add-on HCQ treatment modulates the expression of proinflammatory cytokines even in systemic lupus erythematosus patients with low disease activity.
Subject terms: Systemic lupus erythematosus, Cytokines, Interleukins, Tumour-necrosis factors
Introduction
Systemic lupus erythematosus (SLE) is a chronic systemic autoimmune disease in which multiple organ systems can be damaged by autoantibodies, immune complexes, and inflammation1. The pathogenesis of SLE involves a complex interplay of immunological, genetic, and environmental factors2. Several studies have identified associations between levels of several proinflammatory cytokines and SLE disease activity with specific clinical manifestations3–7. The levels of interferon (IFN) and IFN-inducible chemokines, such as macrophage inflammatory protein-1 (MIP-1), monocyte chemotactic protein-1 (MCP-1), and interferon-inducible protein-10, are reported to correlate with disease activity as measured by disease activity indices such as the erythrocyte sedimentation rate and anti-dsDNA antibody titer3. Other proinflammatory cytokines shown to correlate with SLE disease activity include tumor necrosis factor-α (TNF-α), interleukin (IL)-6, IL-8, IL-10, and vascular endothelial growth factor (VEGF)4–7.
The European League Against Rheumatism recommended hydroxychloroquine (HCQ) treatment for all patients with SLE in 20198. HCQ was approved for the treatment of SLE in Japan in July 2015; since then, it has been prescribed as an add-on treatment for many SLE patients on immunosuppressants, particularly for women of child-bearing age or patients with refractory rash. Because multiple beneficial effects of HCQ for SLE are reported9, additional HCQ treatment may be given to SLE patients with low disease activity (LDA) despite the lack of information regarding the mechanism of action of HCQ.
HCQ therapy has been reported to have a modulatory effect on interferon in patients with SLE10–13. However, there are few reports on the effects of HCQ on inflammatory cytokines, and little is known about the effects on biomarkers when HCQ is additionally administered to patients with SLE who are maintaining LDA with conventional therapy. In the present study, we investigated the effect of add-on HCQ on the levels of proinflammatory cytokines in SLE patients with LDA who were receiving immunosuppressants.
Results
Baseline characteristics and serum levels of proinflammatory factors
Patients who added immunosuppressant therapy after starting HCQ administration and patients who discontinued HCQ administration within 3 months were excluded from this study. Fifty-one SLE patients (47 women and 4 men) with sustained LDA of at least 3 months duration were enrolled in this study. The cohort baseline characteristics are shown in Table 1. The mean age [± standard deviation (SD)] was 42.1 ± 13.0 years. The mean disease duration was 15.4 ± 11.4 years, and the median Safety of Estrogens in Lupus Erythematosus National Assessment SLE Disease Activity Index (SELENA-SLEDAI) score was 4. Of the 51 patients, 30 had active skin involvement, and the median Cutaneous Lupus Erythematous Disease Area and Severity Index (CLASI) activity score was 3.
Table 1.
Baseline characteristics of SLE patients enrolled in the study (n = 51).
| Characteristics | n = 51 |
|---|---|
| Female, n (%) | 47 (92) |
| Age, years, mean ± SD | 42.1 ± 13.0 |
| Disease duration, years, mean ± SD | 15.4 ± 11.4 |
| Past involvement | |
| Renal involvement | 22 (43) |
| Duration of CR free, years | 6.1 ± 5.2 |
| Complication of APS | 9 (18) |
| Disease activity | |
| SELENA-SLEDAI score, Median (range) | 4 (0–8) |
| Current skin involvement, % | 30 (59) |
| CLASI activity score | 3 (0–14) (n = 30) |
| CLASI damage score | 0 (0–5) (n = 30) |
| Anti-dsDNA positive, n (%)*1 | 18 (36) |
| Anti-dsDNA (IU/mL) | 5.4 (5–82.8) |
| C3 (mg/dL) | 76 (40–150) |
| C4 (mg/dL) | 13 (2–33) |
| CH50 (U/mL) | 34.1 (14–57.5) |
| Low complement, n (%)*2 | 27 (53) |
| White blood cells (/μL) | 5000 (1460–10,000) |
| Lymphocytes (/μL) | 1171 (349–3786) |
| Platelet (× 104/μL) | 21.8 (6.7–40.2) |
| Concomitant immunosuppressive treatments | |
| Prednisone | |
| n (%) | 44 (86) |
| Median dosage, mg/day (range) | 5.0 (1–10) |
| Other immunosuppressants*3 | 27 (53) |
| Tacrolimus | 15 (29) |
| Mycophenolate mofetil | 8 (16) |
| Cyclosporine A | 2 (4) |
| Azathioprine | 2 (4) |
| Mizoribine | 2 (4) |
| Methotrexate | 1 (2) |
*1Anti-dsDNA positive is defined as anti-dsDNA titer over 12 IU/mL.
*2Low complement is defined as C3, C4, and CH50 concentrations less than 68 mg/dL, less 12 mg/dL, and 30 U/mL, respectively.
*3Three patients received multiple immunosuppressants.
APS anti-phospholipid antibody syndrome, NPSLE neuropsychiatric systemic lupus erythematosus.
Serum levels of TNF-α, IL-6, IL-8, MCP-1, VEGF-A, and IL-1ra at baseline were significantly higher in SLE patients without skin involvement than in those with skin involvement (Table 2). Serum MCP-1 levels correlated with the SLEDAI score (r = 0.30; p = 0.0339). Serum MCP-1 and IL-1ra levels tended to be higher in SLE patients with anti-dsDNA antibody positive than in those with DNA antibody negative. However, no significant differences were observed between serum levels of complement factors or dsDNA antibodies in the baseline levels of all proinflammatory cytokines measured in this study. Serum IFN-α was detected in only 6 of the 51 patients (date not shown).
Table 2.
Association between clinical parameters and proinflammatory cytokines at baseline.
| Anti-dsDNA positive | Low complement | Skin involvement | |||||||
|---|---|---|---|---|---|---|---|---|---|
| + (n = 18) | − (n = 33) | P | + (n = 27) | − (n = 24) | P | + (n = 30) | − (n = 21) | P | |
| Concentration | |||||||||
| TNF-α, pg/mL | 4.2 (2.4, 13.3) | 3.7 (2.1, 7.1) | 0.3567 | 4.2 (3.0, 6.8) | 2.9 (1.6, 8.7) | 0.3443 | 3.4 (1.6, 5.3) | 4.6 (2.9, 13.3) | 0.0459* |
| IL-6, pg/mL | 2.1 (1.4, 6.0) | 1.6 (1.2, 3.3) | 0.2739 | 1.8 (1.4, 4.7) | 1.6 (1.1, 2.9) | 0.2948 | 1.4 (1.0, 3.2) | 2.0 (1.5, 38.9) | 0.0200* |
| IL-8, pg/mL | 9.9 (1.8, 49.5) | 3.7 (1.9, 9.3) | 0.2038 | 4.7 (1.9, 11.3) | 7.6 (1.8, 61.9) | 0.4593 | 2.6 (1.5, 5.7) | 10.8 (6.4, 80.8) | 0.0003* |
| MCP-1, pg/mL | 267.9 (179.4. 493.2) | 193.8 (149.7, 293.2) | 0.0653 | 216.5 169.6, 354.0) | 227.1 (144.5, 317.2) | 0.1713 | 167.2 (147.5, 260.2) | 277.0 (233.6, 355.1) | 0.0029* |
| VEGF-A, pg/mL | 63.3 (48.7, 84.8) | 42.6 (29.2, 73.8) | 0.1104 | 51.0 (34.5, 92.8) | 54.1 (30.9, 67.2) | 0.7699 | 41.8 (26.8, 60.4) | 78.8 (51.1, 99.2) | 0.0015* |
| IL-1ra, pg/mL | 1124.0 (557.6, 2241.5) | 653.2 (463.6, 1041.5) | 0.0713 | 688.7 (534.5, 1205.3) | 694.4 (420.9, 1509.8) | 0.6438 | 636.5 (466.8, 983.5) | 1092.4 (649.3, 2091.3) | 0.0594* |
| MIP-1a, pg/mL | 128.2 (104.6, 228.2) | 124.5 (116.7, 163.2) | 0.5292 | 120.6 (95.2, 164.6) | 137.9 (120.6, 176.1) | 0.1959 | 124.5 (120.6, 137.3) | 152.1 (95.0, 1093.8) | 0.6004 |
| IL-2, pg/mL | 8.3 (4.8, 13.2) | 9.7 (4.3, 10.5) | 0.6951 | 9.7 (4.5, 10.2) | 9.0 (4.5, 10.7) | 0.8551 | 10.0 (6.8, 10.4) | 4.9 (4.4, 27.7) | 0.2434 |
Median (25% quantile, 75% quantile).
*p < 0.05, Wilcoxon rank sum test.
Serum levels of proinflammatory factor after HCQ treatment
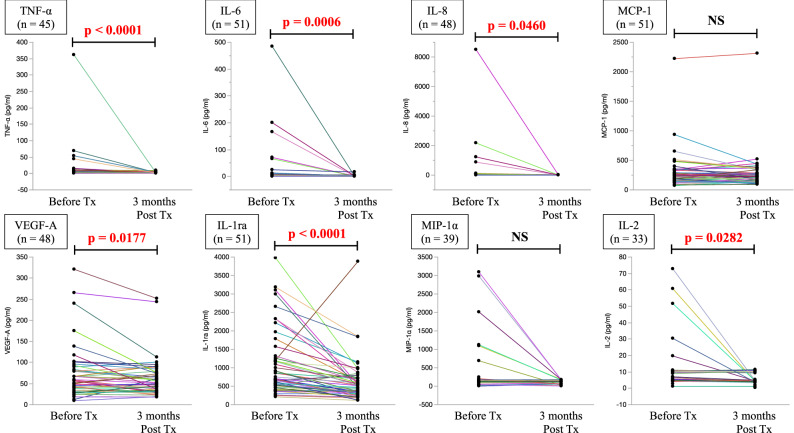
We analyzed serum levels of proinflammatory cytokines at 3 months after initiation of HCQ treatment. As shown in Fig. 1, TNF-α, IL-6, IL-8, VEGF-A, IL-1ra, and IL-2 decreased significantly after HCQ treatment. Although MIP-1α also decreased, the difference from baseline was not significant. In the patients with MCP-1 expression at baseline (n = 51), no change was observed after the addition of HCQ treatment (Fig. 1). No associations were observed between changes in serum proinflammatory cytokine levels and improvements in immunological biomarkers or disease activity scores (Table 3).
Figure 1.
Serum cytokine levels before and after hydroxychloroquine treatment. Serum levels of the indicated cytokines and factors were measured before and after 3 months (3 M Post) of treatment (Tx) with hydroxychloroquine. Colored lines represent individual patients. p values were determined using the Wilcoxon signed-rank test. NS not significant.
Table 3.
Association between clinical parameters and changes in proinflammatory cytokines.
| Change in anti-dsDNA antibody titer, IU/mL | Change in C3 level, mg/dL | Change in C4 level, mg/dL | Change in CH50 level, U/mL | CLASI responder¶ (n = 21) | CLASI nonresponder¶ (n = 9) | P*2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ρ | P*1 | ρ | P*1 | ρ | P*1 | ρ | P*1 | ||||
| TNF-α, pg/mL | 0.088 | 0.5658 | − 0.17 | 0.2609 | 0.011 | 0.9440 | 0.042 | 0.7866 | − 0.7 (− 1.4, − 0.5) | − 0.01 (− 1.4, 0.2) | 0.1357 |
| IL-6, pg/mL | 0.059 | 0.6800 | − 0.10 | 0.4719 | 0.044 | 0.7570 | 0.074 | 0.6037 | − 0.2 (− 0.9, 0.2) | − 0.1 (− 1.4, 0. 5) | 0.5563 |
| IL-8, pg/mL | 0.19 | 0.1966 | 0.035 | 0.8119 | 0.093 | 0.5279 | 0.033 | 0.8255 | 0.08 (− 0.9, 1.4) | − 0.2 (− 1.4, 1.6) | 0.7306 |
| MCP-1, pg/mL | − 0.068 | 0.6332 | 0.068 | 0.6350 | − 0.12 | 0.4034 | 0.050 | 0.7303 | − 16.2 (− 31.1, 64.9) | − 18.1 (− 84.8, 16.5) | 0.2579 |
| VEGF-A, pg/mL | 0.22 | 0.1248 | − 0.037 | 0.8024 | 0.12 | 0.4041 | 0.15 | 0.3073 | − 0.6 (− 14.3, 9.1) | − 1.3 (− 18.0, 12.5) | 0.8262 |
| IL-1ra, pg/mL | − 0.0078 | 0.9567 | − 0.058 | 0.6859 | 0.0097 | 0.9460 | 0.13 | 0.3592 | − 150.9 (− 517.5, − 40.7) | − 289.9 (− 563.6, − 195.4) | 0.2393 |
| MIP-1a, pg/mL | 0.19 | 0.2532 | − 0.044 | 0.7904 | 0.16 | 0.3189 | 0.076 | 0.6444 | − 1.8 (− 3.9, 3.9) | − 64.5 (− 144.6, 15.7) | 0.9495 |
| IL-2, pg/mL | 0.29 | 0.1063 | 0.096 | 0.5954 | 0.29 | 0.1074 | − 0.0029 | 0.9871 | 0.3 (− 0.6, 0.8) | − 0.8 (− 2.3, 1.2) | 0.5383 |
The association between the changes in proinflammatory cytokines and changes in anti-dsDNA titer levels and complement levels was analyzed using univariate analysis. ρ indicates Spearman’s correlation coefficient. *1p < 0.05, Spearman’s correlation.
¶ Of the patients with skin lesion, 21 cases met the criteria for CLASI responder ( +) and 9 cases did not ( −). The median (25% quantile–75% quantile) of change in each proinflammatory cytokine is shown. *2 p < 0.05, Wilcoxon rank sum test.
Safety
The major adverse events observed during the 3-month period were diarrhea in 12 patients (23.5%) and rash in 4 patients (7.8%). Other adverse events included fatigue, fever, and eye symptoms in two patients each. Regarding ocular symptoms, color blindness and blurred vision were observed in one patient each; however, no ophthalmologic abnormality was noted in either case, and the symptoms improved within a few days. For four patients who had diarrhea and two patients who had rashes, the HCQ dose was reduced; however, it was noted that the adverse events improved spontaneously in other cases as well without HCQ dose reduction.
Discussion
Previous studies have demonstrated significant associations between proinflammatory cytokines, especially IL-1, IL-6, TNF-α, and IFNs, and SLE severity14–21. However, the serum levels of most of the proinflammatory cytokines measured in this study did not correlate with disease activity indices (SLEDAI and CLASI) or with serum immunological biomarkers, most likely because our study included only SLE patients with LDA. However, it is possible that patients considered to have LDA may express elevated levels of proinflammatory cytokines.
We observed decreases in serum levels of TNF-α, IL-6, VEGF-A, IL-1ra, IL-2, MIP-1α, and IL-8 after add-on HCQ treatment. Our results differ from those of Monzavi et al., who reported no change in serum IL-8 levels after HCQ treatment of newly diagnosed SLE patients22. This difference and the observed lack of change in MCP-1 upon HCQ treatment are likely due to the inclusion of only patients with LDA. Blood and urine MCP-1 levels have been reported to be associated with active SLE, particularly lupus nephritis, with urine MCP-1 levels of patients with SLE being significantly higher than those of patients with inactive lupus nephritis and controls23–25. In the present study, there was no significant difference in the serum MCP-1 levels before HCQ treatment between patients with and without a history of lupus nephritis. Since the patients included in this study had SLE without any active major organ involvement, it is possible that the serum MCP-1 levels did not significantly decrease after the add-on HCQ treatment. Serum IL-6, IL-8, IL-18, and IFN-α levels have been proposed to be useful predictors of SLE relapse18,19,26. We found that HCQ was effective in reducing serum proinflammatory cytokine levels even in patients with LDA, suggesting that HCQ may help prevent relapse of SLE.
Despite its common use, the mechanism of action of HCQ in autoimmune diseases is unclear. HCQ is a weak base known to raise the pH of acidic intracellular vesicles and interfere with their physiological functions, including autophagy and antigen processing13. HCQ also interferes with intracellular signaling, which may suppress the response to engagement of the innate Toll-like receptors (TLRs), thereby inhibiting the production and release of cytokines and promoting apoptosis in lymphocytes and endothelial cells27,28. Both of these HCQ-induced processes may contribute to the decreased production of proinflammatory cytokines. In addition, HCQ-mediated inhibition of TLR activation suppresses the activity of plasmacytoid dendritic cells and autoreactive B cells in SLE patients28,29, leading to a reduction in inflammation. Indeed, Sacre et al. demonstrated that HCQ treatment of SLE patients reduced the ability of plasmacytoid dendritic cells to produce IFN-α and TNF-α in response to TLR-9 and TLR-7 stimulation in vivo11. We believe that the HCQ-induced decrease in cytokine observed in the present study may be mediated by these effects.
We previously reported that HCQ modulates the serum levels of S100A8 and S100A9, which are associated with disease activity in SLE patients with LDA30. S100 proteins are components of neutrophil extracellular traps (NETs)31, which play an important role in the pathogenesis of SLE32–34. In addition, chloroquine and HCQ are reported to inhibit NETs in vivo and in vitro35–37, suggesting the involvement of S100 protein regulation in their underlying mechanism of action. S100A8 and S100A9 proteins upregulate the expression of proinflammatory cytokines such as IL-6 and IL-838–41; therefore, the HCQ-mediated modulation of S100 proteins may also be involved in the suppression of proinflammatory cytokine expression in SLE patients.
This study has several limitations. First, we did not monitor HCQ adherence by measuring blood HCQ levels. Second, whether the change in proinflammatory cytokine levels were a direct result of add-on HCQ treatment is difficult to determine unequivocally because some patients were receiving other immunosuppressants. Third, the sample size was small due to the strict inclusion and exclusion criteria. This study was an exploratory study and the sample size was not strictly adjusted due to exclusion criteria. We believe that a prospective study with a calculated sample size and a control group is needed to support the results of the present study. Finally, the serum level of IFN-α was undetectable in most patients due to sub-sensitivity. Nevertheless, our study has merit because it is the first to demonstrate the effect of add-on HCQ treatment on proinflammatory cytokines in SLE patients with LDA.
In conclusion, we found that add-on HCQ treatment decreased the serum levels of several proinflammatory cytokines in SLE patients with LDA. Our results suggest that add-on HCQ treatment may reduce proinflammatory cytokine expression in SLE patients. Long-term prospective studies are needed to clarify whether proinflammatory cytokine modulation caused by an add-on HCQ treatment is associated with improved prognosis or prevention of relapse in SLE.
Patients and methods
Patients
This single-center exploratory study prospectively enrolled subjects diagnosed with SLE according to the American College of Rheumatology criteria42 or the Systemic Lupus Collaborating Clinics criteria43. All enrolled patients began HCQ treatment for the first time between September 2015 and March 2019. All patients had a ≥ 3-month history of LDA before enrollment, defined as (i) a SELENA-SLEDAI score ≤ 8 with no activity in major organ systems (renal involvement, neuropsychiatric SLE, cardiopulmonary involvement, or vasculitis); (ii) current prednisolone or equivalent dose of ≤ 10 mg per day; and (iii) well-tolerated maintenance doses of other immunosuppressant. Pregnant women and patients, who were not in complete renal remission44, regardless of lupus nephritis history, were excluded. Patients who began anti-thrombotic therapy or add-on immunosuppressants or increased their glucocorticoid dose after starting the HCQ treatment were excluded from the study. Informed consent was obtained from all participants. The study was approved by the ethics committee of Kagawa University (Heisei30-047).
Treatment and outcomes
Patients were administered oral HCQ sulfate (Plaquenil; Sanofi-Winthrop, Paris, France) continuously for at least 3 months. HCQ was administered at a dose based on the ideal body weight (IBW) calculated using the modified Broca’s method: 200 mg daily for patients with IBW < 46 kg; 200 mg and 400 mg on alternate days for IBW ≥ 46 kg and < 62 kg; and 400 mg daily for IBW ≥ 62 kg. The primary endpoint was the change in proinflammatory cytokine concentrations with additional HCQ administration. Clinical parameters (age, sex, HCQ dose, immunological biomarkers, disease activity indices, and skin scores) were recorded before and after HCQ treatment. Disease activity was evaluated using the SELENA-SLEDAI 2011 criteria45. Cutaneous disease activity was evaluated using the CLASI46. In accord with the CLASI improvement criteria of Klein et al.47, the principal investigator designated the CLASI score as improved, unchanged, or worse compared with the previous visit. Patients classified as improved were defined as ‘CLASI responders,’ and those classified as unchanged or worse were defined as ‘CLASI non-responders.’ Immunological activity was determined by measuring the serum levels of complement factors (C3, C4, and CH50), anti-double stranded DNA (dsDNA) antibodies, and counts of total white blood cells, lymphocytes, and platelets. Complete blood counts were measured using the multi-item automated hematology analyzer XN-3000. The complement factors were measured using the following assay kits: N-assay TIA C3-SH Nittobo, N-assay TIA C4-SH Nittobo, and auto CH50-L “Seiken” II. Anti-double-stranded DNA antibodies were measured using the MESACUP DNA-II test “ds” until October 2017 and the STACIA MEBLux test dsDNA kit since November 2017. The dsDNA antibody assay kit was changed during the study period, but there were no changes in the test kits for the same patients. Specific ELISA kits were used to measure serum IFN-α (Human IFN alpha Platinum ELISA Kit, Thermo Fisher Scientific Inc., Carlsbad, CA, USA) according to the manufacturers’ instructions. Serum TNF-α, IL-2, IL-6, IL-8, VEGF-A, MCP-1, MIP-1α, and IL-1 receptor antagonist (IL-1ra) were measured using a multiplex immunoassay (Luminex Assay, R&D Systems Minneapolis, MN, USA).
Statistical analysis
Data are presented as the mean ± SD unless otherwise noted. Immunological biomarkers and proinflammatory cytokine levels were compared using paired t test for continuous variables or the Wilcoxon signed-rank test for non-normally distributed data. The relationship between the clinical SLE improvement index and the baseline levels of proinflammatory cytokines and the change in proinflammatory cytokine levels before and after HCQ administration was analyzed using the Wilcoxon rank sum (Mann–Whitney U) test. The association between the clinical SLE improvement index and the rate of change in proinflammatory cytokines was analyzed using the Mann–Whitney U test. The association between pro-inflammatory cytokine levels and clinical variables was determined using correlation analyses (Spearman’s correlation coefficient). All p values were two-sided, and p < 0.05 was considered significant. Data were analyzed using JMP 15 software (SAS Institute, Cary, NC, USA).
Ethical approval
The study was approved by the ethics committee of Kagawa University (Heisei30-047) and was prospectively registered. All participants gave their written informed consent before entering the study. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgements
We thank Enago (https://www.enago.jp) for editing a draft of this manuscript. We wish to acknowledge Nobuyuki Miyatake for his assistance with statistical analysis.
Author contributions
All authors were involved in drafting the manuscript or reviewing it for important intellectual content, and all authors approved the final version to be submitted for publication. R.W. and H.D. planned the study and wrote the manuscript. R.W. conducted the study and interpreted the results together with K.U., S.N., H.S., T.K., M.K. T.M., K.S., M.M., R.M., and H.D. M.M.F.M. and N.K. reviewed the manuscript for intellectual content. All authors read and approved the final manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liu Z, Davidson A. Taming lupus—A new understanding of pathogenesis is leading to clinical advances. Nat. Med. 2012;18:871–882. doi: 10.1038/nm.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chasset F, Arnaud L. Targeting interferons and their pathways in systemic lupus erythematosus. Autoimmun. Rev. 2018;17:44–52. doi: 10.1016/j.autrev.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Bauer JW, et al. Interferon-regulated chemokines as biomarkers of systemic lupus erythematosus disease activity: A validation study. Arthritis Rheum. 2009;60:3098–3107. doi: 10.1002/art.24803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Idborg H, et al. TNF-α and plasma albumin as biomarkers of disease activity in systemic lupus erythematosus. Lupus Sci. Med. 2018;5:e000260. doi: 10.1136/lupus-2018-000260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mao YM, et al. Increased circulating interleukin-8 levels in systemic lupus erythematosus patients: A meta-analysis. Biomark. Med. 2018;12:1291–1302. doi: 10.2217/bmm-2018-0217. [DOI] [PubMed] [Google Scholar]
- 6.Grondal G, et al. Cytokine production, serum levels and disease activity in systemic lupus erythematosus. Clin. Exp. Rheumatol. 2000;18:565–570. [PubMed] [Google Scholar]
- 7.Adhya Z, et al. Soluble TNF-R1, VEGF and other cytokines as markers of disease activity in systemic lupus erythematosus and lupus nephritis. Lupus. 2019;28:713–721. doi: 10.1177/0961203319845487. [DOI] [PubMed] [Google Scholar]
- 8.Fanouriakis A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 2019;78:736–745. doi: 10.1136/annrheumdis-2019-215089. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz-Irastorza G, et al. Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: A systematic review. Ann. Rheum. Dis. 2010;69:20–28. doi: 10.1136/ard.2008.101766. [DOI] [PubMed] [Google Scholar]
- 10.Willis R, et al. Effect of hydroxychloroquine treatment on pro-inflammatory cytokines and disease activity in SLE patients: Data from LUMINA (LXXV), a multiethnic US cohort. Lupus. 2012;21:830–835. doi: 10.1177/0961203312437270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sacre K, Criswell LA, McCune JM. Hydroxychloroquine is associated with impaired interferon-alpha and tumor necrosis factor-alpha production by plasmacytoid dendritic cells in systemic lupus erythematosus. Arthritis Res. Ther. 2012;14:R155. doi: 10.1186/ar3895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misra DP, Negi VS. Interferon targeted therapies in systemic lupus erythematosus. Mediterr. J. Rheumatol. 2017;28:13–19. doi: 10.31138/mjr.28.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schrezenmeier E, Dörner T. Mechanisms of action of hydroxychloroquine and chloroquine: Implications for rheumatology. Nat. Rev. Rheumatol. 2020;16:155–166. doi: 10.1038/s41584-020-0372-x. [DOI] [PubMed] [Google Scholar]
- 14.Martin A. Inflammatory markers in systemic lupus erythematosus. J. Autoimmun. 2020;110:102374. doi: 10.1016/j.jaut.2019.102374. [DOI] [PubMed] [Google Scholar]
- 15.Brohawn PZ, et al. Type I interferon gene signature test-low and -high patients with systemic lupus erythematosus have distinct gene expression signatures. Lupus. 2019;28:1524–1533. doi: 10.1177/0961203319885447. [DOI] [PubMed] [Google Scholar]
- 16.Tsokos GC, Lo MS, Reis PC, Sullivan KE. New insights into the immunopathogenesis of systemic lupus erythematosus. Nat. Rev. Rheumatol. 2016;22:716–730. doi: 10.1038/nrrheum.2016.186. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds JA, et al. Cytokine profiling in active and quiescent SLE reveals distinct patient subpopulations. Arthritis Res. Ther. 2018;9:173. doi: 10.1186/s13075-018-1666-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soliman S, Mohan C. Lupus nephritis biomarkers. Clin. Immunol. 2017;185:10–20. doi: 10.1016/j.clim.2016.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Mathian A, et al. Ultrasensitive serum interferon-α quantification during SLE remission identifies patients at risk for relapse. Ann. Rheum. Dis. 2019;78:1669–1676. doi: 10.1136/annrheumdis-2019-215571. [DOI] [PubMed] [Google Scholar]
- 20.Willis R, et al. Clinical associations of proinflammatory cytokines, oxidative biomarkers and vitamin D levels in systemic lupus erythematosus. Lupus. 2017;26:1517–1527. doi: 10.1177/0961203317706557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Umare V, et al. Effect of proinflammatory cytokines (IL-6, TNF-α, and IL-1β) on clinical manifestations in Indian SLE patients. Mediat. Inflamm. 2014;2014:385297. doi: 10.1155/2014/385297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monzavi SM, et al. Efficacy analysis of hydroxychloroquine therapy in systemic lupus erythematosus: A study on disease activity and immunological biomarkers. Inflammopharmacology. 2018;26:1175–1182. doi: 10.1007/s10787-018-0512-y. [DOI] [PubMed] [Google Scholar]
- 23.Lee YH, Song GG. Urinary MCP-1 as a biomarker for lupus nephritis: A meta-analysis. Z Rheumatol. 2017;76:357–363. doi: 10.1007/s00393-016-0109-z. [DOI] [PubMed] [Google Scholar]
- 24.Ghafouri-Fard S, Shahir M, Taheri M, Salimi A. A review on the role of chemokines in the pathogenesis of systemic lupus erythematosus. Cytokine. 2021;146:155640. doi: 10.1016/j.cyto.2021.155640. [DOI] [PubMed] [Google Scholar]
- 25.Lan L, Han F, Lang X, Chen J. Monocyte chemotactic protein-1, fractalkine, and receptor for advanced glycation end products in different pathological types of lupus nephritis and their value in different treatment prognoses. PLoS One. 2016;11:e0159964. doi: 10.1371/journal.pone.0159964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ruchakorn N, et al. Performance of cytokine models in predicting SLE activity. Arthritis Res. Ther. 2019;21:287. doi: 10.1186/s13075-019-2029-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rainsford KD, et al. Therapy and pharmacological properties of hydroxychloroquine and chloroquine in treatment of systemic lupus erythematosus, rheumatoid arthritis and related diseases. Inflammopharmacology. 2015;23:231–269. doi: 10.1007/s10787-015-0239-y. [DOI] [PubMed] [Google Scholar]
- 28.Lenert PS. Targeting Toll-like receptor signaling in plasmacytoid dendritic cells and autoreactive B cells as a therapy for lupus. Arthritis Res. Ther. 2006;8:203. doi: 10.1186/ar1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Torigoe M, et al. Hydroxychloroquine efficiently suppresses inflammatory responses of human class-switched memory B cells via Toll-like receptor 9 inhibition. Clin. Immunol. 2018;195:1–7. doi: 10.1016/j.clim.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 30.Wakiya R, et al. Hydroxychloroquine modulates elevated expression of S100 proteins in systemic lupus erythematosus. Lupus. 2019;28:826–833. doi: 10.1177/0961203319846391. [DOI] [PubMed] [Google Scholar]
- 31.Urban CF, et al. Neutrophil extracellular traps contain calprotectin, a cytosolic protein complex involved in host defense against Candida albicans. PLoS Pathog. 2009;5:e1000639. doi: 10.1371/journal.ppat.1000639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salemme R, et al. The role of NETosis in systemic lupus erythematosus. J. Cell. Immunol. 2019;1:33–42. doi: 10.33696/immunology.1.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frangou E, et al. REDD1/autophagy pathway promotes thromboinflammation and fibrosis in human systemic lupus erythematosus (SLE) through NETs decorated with tissue factor (TF) and interleukin-17A (IL-17A) Ann. Rheum. Dis. 2019;78:238–248. doi: 10.1136/annrheumdis-2018-213181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fousert E, Toes R, Desai J. Neutrophil extracellular traps (NETs) take the central stage in driving autoimmune responses. Cells. 2020;8:915. doi: 10.3390/cells9040915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang S, et al. Hydroxychloroquine inhibiting neutrophil extracellular trap formation alleviates hepatic ischemia/reperfusion injury by blocking TLR9 in mice. Clin. Immunol. 2020;216:108461. doi: 10.1016/j.clim.2020.108461. [DOI] [PubMed] [Google Scholar]
- 36.Smith CK, et al. Neutrophil extracellular trap-derived enzymes oxidize high-density lipoprotein: An additional proatherogenic mechanism in systemic lupus erythematosus. Arthritis Rheumatol. 2014;66:2532–2544. doi: 10.1002/art.38703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boone BA, et al. Chloroquine reduces hypercoagulability in pancreatic cancer through inhibition of neutrophil extracellular traps. BMC Cancer. 2018;22:678. doi: 10.1186/s12885-018-4584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao H, et al. S100A9-induced release of interleukin (IL)-6 and IL-8 through toll-like receptor 4 (TLR4) in human periodontal ligament cells. Mol. Immunol. 2015;67:223–232. doi: 10.1016/j.molimm.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 39.Takagi R, et al. S100A9 increases IL-6 and RANKL expressions through MAPKs and STAT3 signaling pathways in osteocyte-like cells. Biomed. Res. Int. 2020;19:7149408. doi: 10.1155/2020/7149408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nishikawa Y, et al. Calprotectin induces IL-6 and MCP-1 production via Toll-like receptor 4 signaling in human gingival fibroblasts. J. Cell. Physiol. 2017;232:1862–1871. doi: 10.1002/jcp.25724. [DOI] [PubMed] [Google Scholar]
- 41.Kim DH, et al. Suppressive effects of S100A8 and S100A9 on neutrophil apoptosis by cytokine release of human bronchial epithelial cells in asthma. Int. J. Med. Sci. 2020;4:498–509. doi: 10.7150/ijms.37833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tan EM, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–1277. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 43.Petri M, et al. Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64:2677–2686. doi: 10.1002/art.34473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bertsias GK, et al. Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann. Rheum. Dis. 2012;71:1771–1782. doi: 10.1136/annrheumdis-2012-201940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petri M, et al. Combined oral contraceptives in women with systemic lupus erythematosus. N. Engl. J. Med. 2005;353:2550–2558. doi: 10.1056/NEJMoa051135. [DOI] [PubMed] [Google Scholar]
- 46.Albrecht J, et al. The CLASI (Cutaneous Lupus Erythematosus Disease Area and Severity Index): An outcome instrument for cutaneous lupus erythematosus. J. Investig. Dermatol. 2005;125:889–894. doi: 10.1111/j.0022-202X.2005.23889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Klein R, et al. Development of the CLASI as a tool to measure disease severity and responsiveness to therapy in cutaneous lupus erythematosus. Arch. Dermatol. 2011;147:203–208. doi: 10.1001/archdermatol.2010.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.