Abstract
Repairing of large bone injuries is an important problem in bone regeneration field. Thus, developing new therapeutic approaches such as tissue engineering using 3D scaffolds is necessary. Incorporation of some bioactive materials and trace elements can improve scaffold properties. We made chitosan/alginate/strontium-doped bioglass composite scaffolds with optimized properties for bone tissue engineering. Bioglass (BG) and Sr-doped bioglasses (Sr-BG) were synthesized using Sol–Gel method. Alginate-Chitosan (Alg/Cs) scaffold and scaffolds containing different ratio (10%, 20% and 30%) of BG (Alg/Cs/BG10, 20, 30) or Sr-BG (Alg/Cs/Sr-BG10, 20, 30) were fabricated using freeze drying method. Characterization of bioglasses/scaffolds was done using zeta sizer, FTIR, XRD, (FE) SEM and EDS. Also, mechanical strength, antibacterial effect degradation and swelling profile of scaffolds were evaluated. Bone differentiation efficiency and viability of MSCs on scaffolds were determined by Alizarin Red, ALP and MTT methods. Cell toxicity and antibacterial effect of bioglasses were determined using MTT, MIC and MBC methods. Incorporation of BG into Alg/Cs scaffolds amplified biomineralization and mechanical properties along with improved swelling ratio, degradation profile and cell differentiation. Mechanical strength and cell differentiation efficiency of Alg/Cs/BG20 scaffold was considerably higher than scaffolds with lower or higher BG concentrations. Alg/Cs/Sr-BG scaffolds had higher mechanical stability and more differentiation efficiency in comparison with Alg/Cs and Alg/Cs/BG scaffolds. Also, Mechanical strength and cell differentiation efficiency of Alg/Cs/Sr-BG20 scaffold was considerably higher than scaffolds with various Sr-BG concentrations. Biomineralization of Alg/Cs/BG scaffolds slightly was higher than Alg/Cs/Sr-BG scaffolds. Overall, we concluded that Alg/Cs/Sr-BG20 scaffolds are more suitable for repairing bone major injuries.
Subject terms: Regenerative medicine, Tissue engineering, Biotechnology, Cell biology, Stem cells, Materials science, Nanoscience and technology
Introduction
Bone is a multifunctional tissue consisting of organic phase and a mineral phase. The organic phase makes about 30% of bone composition and mainly consisting of type I collagen matrix, while the mineralized phase is 70% of bone composition and mostly includes hydroxyapatite1. Bone has a dynamic nature, in a way there is a balance between bone resorption and formation and it can renew itself through remodeling. Minor bone injuries often repair naturally with minimal intervention without the need for any intervention in healthy people. However, critical-sized or large bone injuries arising from infections, malignancies, trauma and explosions are outside the normal bone repair capacity and requires surgical interventions to restore initial function2,3. Implant placement and tissue grafting are two main approaches for regeneration of large bone injuries. These methods have many limitations and disadvantages including the donor’s unavailability, possibility of disease transmission and/or transplant rejection and need for revision surgery (in case of implant) and the high cost.
Therefore, there is a demand to make artificial bone graft alternatives (scaffolds) with optimized properties4 in terms of mechanical stability, biocompatibility, biodegradability, osteoinductivity and osteoconductivity. It should support cell adhesion, growth, migration and differentiation as well as early mineralization and formation of new bone and vessels. A scaffold with a bone-like material that has a large surface and an interconnected porous structure with suitable size may be appropriate for this purpose5. Also, a suitable scaffold must be cost effective for large-scale production6.
Chitosan as a natural, biocompatible, non-toxic, biodegradable and non-immunogen polymer is prepared from deacetylated chitin7,8 and extensively has been used for fabrication of porous scaffolds. Its large hydrophilic surface induces cell attachment, proliferation, differentiation and migration9. However, low mechanical stability of chitosan10 is not enough for bone engineering purposes mainly due to its swelling rate and in a result is unable to maintain its default shape for grafting. So, its mechanical properties should be improved for use in bone engineering approaches. Alginate also is a low-cost hydrophile anionic polymer with excellent properties in terms of biocompatibility, biodegradability and mechanical strength that is derived from a certain species of brown algae11. Calcium ions binding with its carboxyl groups promote production of hydrogel12. It is suggested that chitosan and alginate be combined to fabrication of a hybrid (composite) scaffold with improved mechanical characteristics due to covalent bonding between chitosan amine and alginate carboxyl groups13. In addition, to more improvement in bio-mineralization and mechanical stability of alginate-chitosan scaffolds, doping of bioglasses (bioactive glasses) has been proposed13,14.
Bioglasses are very similar to mineral phase of bone, because of that are interesting in the fabrication of bone substitute scaffolds15. Bioglasses are capable of establishing strong bonds with bone by making hydroxyapatite layer on bone surface along with releasing Na, Ca, Si, and P ions to exert their biological effects1. It has been reported that incorporation of bioglass to biopolymers amplifies the bone specific markers like osteocalcin, osteopontin and alkaline phosphatase16. Besides, bioactivity of these glasses can be tuned by addition of various ions such as zinc (Zn), magnesium (Mg), strontium (Sr) and etc.17. These trace elements can enhance the interactions between cells and composite18. Currently, strontium ranelate is administrated to treat osteoporosis because of its anti-resorptive and anabolic effects19. However, doping some cations such as Sr2+ may decrease formation of hydroxyapatite like crystals20. This is due to substituting CaO with SrO in bioactive glass which leads to reducing the calcium content in the composition21. In this study, calcium chloride (CaCl2) was employed for crosslinking of scaffolds and, thus, the reduced calcium content can be compensated to some extent. Consequently, the fabricated composite is more flexible and also stronger. Besides, the lack of Ca ions is compensated in the bioglass formulation22.
Herein, we synthesized Sr containing bioactive glasses. Subsequently, Sr-doped bioglasses were incorporated in composite scaffold based on chitosan and alginate to improve the mechanical strength and biological behavior of these scaffolds. Physicochemical characterization (e.g., chemical groups assessment, elemental analysis, crystal structure analysis, porosity, compression test, swelling ratio and degradation percentage) of the bioglass and composite scaffolds were carried out. Subsequently, the antibacterial tests and cellular tests including viability, alkaline phosphatase activity and calcium deposition assay were performed.
Materials and methods
Materials
All reagents and chemicals were highly pure and obtained from Sigma Aldrich (Darmstadt, Germany), unless mentioned. All cell culture media and materials were obtained from Gibco, Life Technologies (Paisley, UK). All tubes, tips and falcons were purchased from Biologix (USA). Plates, flasks and pipets were obtained from JetBioFil (China).
Synthesis and characterization of strontium doped bioglass
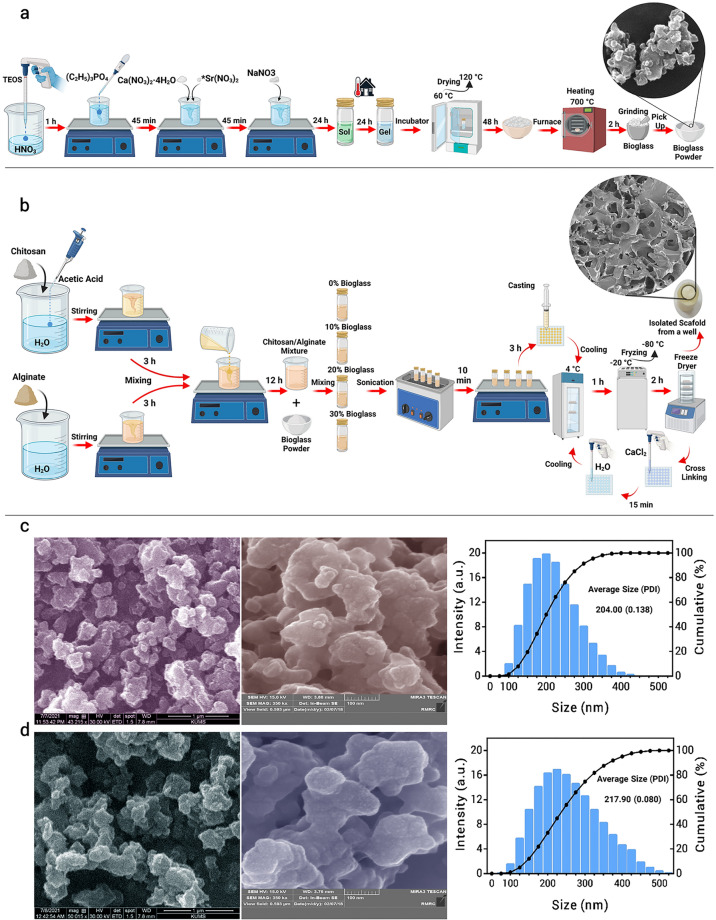
Sol–Gel process was applied to synthesize bioglass (BG) nano (sub-micron) particles23,24. First, 33.5 ml of Si(OC2H5)4(H2O:TEOS molar ratio = 18) was added to 50 ml HNO3 (1 M), and allowed to be hydrolyzed by nitric acid with mild stirring at room temperature. After 1 h, (C2H5)3PO4 (9 ml), Ca(NO3)2·4 H2O (20.13 g) and NaNO3 (13.52 g) were added separately to the reaction at 45 min intervals with continues stirring, in the order as mentioned. In order to make strontium containing bioglass (Sr-BG), Ca(NO3)2·4H2O (19.74 g) and Sr(NO3)2 (0.71 g) were added to the reaction. The mixture was placed on a magnet stirrer for 24 h at 25 °C. The resulting sol was again incubated for 24 h 25 °C without stirring to gel formation. The obtained gel was incubated at 60 °C for 24 h and thereafter at 120 °C for 24 h to remove all water content. Final stabilization phase was performed by heating of resulting powder at 700 °C (rate of 3 °C/min) in an electrical furnace for 2 h. Afterward, the powder was manually grinding and sieving to get homogeneous bioglass powder (Fig. 1a). The hydrodynamic diameter (Size) and zeta potential (surface charge) of BG and Sr-BG samples were determined using a dynamic light scattering instrument (DLS, Malvern Panalytical, Worcestershire, UK). The chemical bonds and crystal structure of samples were evaluated using Fourier transform infrared (FTIR) spectroscopy (Shimadzu, Japan) and X-ray diffraction (XRD, Bruker, Germany) method, respectively. The shape and size of the samples were evaluated by scanning electron microscopy (SEM, FEI, USA) and field emission scanning electron microscopy (FESEM, TESCAN MIRA3, Czech). Elemental analysis was conducted using energy dispersive spectroscopy (EDS, FEI, USA), respectively.
Figure 1.
Fabrication scheme of bioglass/scaffolds and morphology and size distribution of synthesized bioglasses. (a) Bioglasses synthesis steps, (b) Scaffolds fabrication steps. (c) BG morphology and size distribution, (d) Sr-BG morphology and size distribution. The average size of synthesized bioglasses is in the nanometer range.
Fabrication and characterization of composite scaffolds
A solution of chitosan was made by mixing required amount of chitosan powder (5% w/v, low molecular weight, deacetylation degree of 75–85%) in deionized water containing 5.8% (v/v) acetic acid. A solution of 5% (w/v) of alginate was prepared by dissolving the required amount of alginic acid sodium salt in deionized water. Then, each solution was stirred for 2–3 h in order to gain a uniform and clear mixture. Afterward, equal volume of chitosan and alginate solutions (50–50%) were mixed by 12 h stirring at room temperature. In the next step, required amount of BG or Sr-BG powders were added to the chitosan-alginate solution to obtain samples containing 10%, 20% and 30% of bioglasses (Alg/Cs/BG10, 20, 30) or Sr-BG (Alg/Cs/Sr-BG10, 20, 30). The control samples (Alg/Cs) did not contain any BG or Sr-BG. Subsequently, solutions were homogenized by 10 min sonication (Shenzhen Codyson, China) and 2–3 h stirring at room temperature. The final suspension was casted into 48-well plates and kept at 4 °C for 1 h followed by freezing at − 20 °C. Afterward, plates were incubated at − 80 °C for 2 h and immediately lyophilized in a freezer dryer (Christ, Germany) for 48 h to completely be dried. The fabricated scaffolds were immersed in 1% (w/v) calcium chloride for 15 min in order to cross-linking followed by and washing in deionized water. Subsequently, samples were frozen again at − 20 °C after one hour incubation at 4 °C. Finally, samples were lyophilized again in freezer dryer for 48 h (Fig. 1b). The Zeta potential (surface charge), chemical groups, surface morphology and elemental analysis of scaffolds were performed by DLS, FTIR, SEM, EDS and methods, respectively.
Antibacterial activity of bioglasses and scaffolds
The antibacterial of BG and Sr-BG powders was evaluated by determining of minimum inhibitory (MIC) and bactericidal (MBC) concentrations against standard Staphylococcus aureus (S. aureus) ATCC 25923 and Escherichia coli (E. coli) ATCC 25922. First, bacteria were cultured in Mueller Hinton broth at 37 °C, overnight. Different concentrations of BG and Sr-BG powders (100–1000 μg/ml) was poured into different well of a microplate. After adding Mueller Hinton broth, a bacterial concentration equivalent of 0.5 McFarland was added to microplate wells. Negative control well contained the Mueller Hinton broth and BG or Sr-BG powders without bacteria. After 24 h incubation at 37 °C, presence of bacteria in wells was examined by culturing of samples on Mueller Hinton agar. MBC and MIC concentrations were considered as lowest concentration of BG or Sr-BG powders which kills all test microorganisms and prevents visible growth, respectively. This test done in triplicate (n = 3). The antimicrobial effect of scaffolds was evaluated by agar well diffusion assay. The microbial culture medium (Mueller Hinton agar) was prepared, poured into bacterial culture plates and wells with 7 mm diameter was created in plates. A uniform culture of bacteria was prepared using cotton swabs from the 0.5 McFarland bacteria suspension prepared on plate surface. Physiological serum (100 μl) containing 200 mg/ml of scaffolds was added to the plate wells and incubated at 37 °C for 24 h, and finally inhibition zone around the scaffolds were measured and compared with standard antibiotics controls (Vancomycin for S. aureus and Ciprofloxacin for E. coli).
Scaffolds porosity and pore size measurement
Porosity, average pore size and pore size distribution of scaffolds was determined by Image J analysis on electron microscope images. The porosity was calculated by dividing surface area of pores by total area of the image. First, SEM information in the lower part of the images was removed. Then, true scales were introduced to software and SEM images type changed into 16-bit. For Binarization, image threshold was adjusted until all pores completely covered but other area was not selected (just the pores should be colorful). After proper thresholding, porosity measurement was done in the analyze menu. Porosity was determined in two SEM image for each scaffold sample. Also, the pore size was measured in scaffolds pores (n ≈ 100) of SEM images and mean pore size and pore size distribution was reported.
Scaffolds in vitro bioactivity
In vitro bioactivity test was performed by immersing the scaffolds specimens in simulated body fluid (SBF). First, scaffolds sections were obtained with similar dimensions (thickness: 2 mm diameter: 10 mm). The required volume of SBF for immersion of scaffolds was calculated by formula, which V is required volume in ml and S is scaffolds surface area in mm2. Scaffolds sections were soaked in calculated SBF volume for 7 and 14 days at 37 °C and then washed in deionized water and lyophilized. Subsequently, dried specimens (three section per sample) were evaluated using SEM25.
Scaffolds mechanical test
The compression testing as a valuable test to determine scaffolds mechanical behavior was performed in a manner previously described26. Three cylindrical specimens (Height: 10 mm, Diameter: 10 mm) for each scaffold were undergone compression testing via universal mechanical tester (SANTAM, STM-20). All tests were done in vertical direction with speed of 2 mm per minutes at 25 °C. The specimens were compressed to about of their primary height and stress strain curve was obtained and also mechanical strength was determined. The elastic modulus of each scaffold was obtained from its compressive stress strain curve. The mechanical test was repeated three times for each sample.
Scaffold degradation test
The initial weight of scaffolds specimens (Thickness: 10 mm, Diameter: 10 mm) was measured using a high precision analytical balance. In vitro degradation test was done by soaking of scaffolds in PBS (pH 7.4, 37 °C) for 3, 7, 14 and 21 days. Two thirds of PBS solution was replaced with fresh solution once every three days. At mentioned times, the specimens were withdrawn from PBS, and lyophilized after washing in deionized water and soaking in ice cold ethanol for 2 h. The scaffold degradation percentage was calculated using following formula: , which W0 and Wf are initial weight and final weight, respectively. This test was repeated three times for each sample.
Scaffold swelling test
The scaffolds were cut into sections with about 10 mm thickness and 10 mm diameter. The dry weight of specimens was measured by a high precision analytical balance (Mettler Toledo, Germany). Then, specimens were immersed in buffered phosphate solution (PBS) and incubated at 37 °C. The wet weight and dimensions of the specimens was measured at different time intervals for 24 h. Before weighing, the surface water of the specimens was removed by a filter paper. The scaffold swelling percentage was calculated using following formula: , which Ww and Wd are wet weight and dry weight, respectively. All tests were performed in triplicate and the mean values were reported.
Isolation and characterization of mesenchymal stem cells (MSCs)
MSCs were extracted from bone marrow of 14-weeks old male Wistar rats. All animal procedures were performed according to ethical guidelines of working with laboratory animals approved in ethical committee of Baqiyatallah University of Medical Sciences (IR.BMSU.REC.1399.498). In this study, animals that were killed for educational purposes were used for MSCs isolation. Briefly, Animals were scarified under deep anesthesia (75 mg ketamine, 5 mg xylazine per kg). Both femur and tibia of rats was harvested and peripheral tissues was removed. Afterward, harvested bones were soaked in 70% ethanol for a few seconds and then washed with PBS containing 2% penicillin (pen)/streptomycin (strep). Both ends of the bones were excised and the bone marrow was flashed out using DMEM culture medium (low glucose) containing 1.5% pen-strep and 10% fetal bovine serum (FBS). The gained suspension was filtered by a 200-mesh sieve and centrifuged at 2000 rpm for 10 min. The supernatant was discarded and pellet was resuspended in DMEM medium containing 10% FBS and 1.5% pen-strep and transferred into T25 flasks containing same media. Flasks were incubated at 37 °C, 5% CO2 and high relative humidity. The medium was replaced after 2 days with DMEM medium containing 10% FBS and 1% pen-strep in order to remove non adherent cells. Cells was passaged when reached 90% confluency using 0.25% Trypsin/EDTA. After three passages, cells were harvested for bone differentiation, cell toxicity assay and characterizing using flowcytometry for cell expressing cell surface markers including CD44, CD90, CD29, CD34, and CD45.
Cell attachment on scaffolds
Cell attachment on scaffolds was evaluated using fluorescence and SEM. Briefly, 2 days after cell seeding on scaffolds, medium was withdrawn and cell containing scaffolds were rinsed twice with cold PBS and fixed by 15 min in 4% formaldehyde at 25 °C. Afterward, cell staining was done by 20 min incubation in 2 µM propidium iodide solution at 25 °C and cell containing scaffolds were photographed under a fluorescence microscope (Olympus, Japan). For SEM imaging, cell containing scaffolds were fixed and then dehydrated by submerging them in ascending ethanol concentrations (30, 50, 70, 80, 90, and 100%) at 37 °C for 5 min each. Finally, images were obtained using SEM.
Cellular toxicity
Cell toxicity of synthesized bioglasses and fabricated scaffolds was evaluated using MTT (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide) assay. Bioglasses were sterilized by soaking in 70% ethanol and UV light irradiation for 1 h. Scaffolds were cut into sections with about 1 mm thickness and 6 mm diameter and sterilized by exposing them to UV light for 1 h. Prepared and sterilized scaffold sections was inserted in 96-well culture plates (one scaffold per well) and the number of 4000 cell per well was seeded on each scaffold section. Also, 4000 cells were seeded in scaffold free plate wells. Sterilized bioglasses were added to plate wells with final concentrations of 0.5 mg/ml 24 h after cell seeding. Cell toxicity of scaffolds were evaluated at the times of 3 and 7 days after seeding. Cell toxicity of bioglasses were evaluated at the times of 1, 3 and 5 days after adding them to cells cultured in the plates. At the above-mentioned times, MTT solution was added to plate wells (0.5 mg/ml) and plates maintained in incubator (37 °C, 5% CO2) for 3 h. Afterward, culture medium of plates was withdrawn and replaced by 100 μl Dimethyl sulfoxide (DMSO) for dissolving of formazan crystals. Finally, plates were incubated at room temperature for 10–15 min with gentle shaking and absorbance of plates were measured by an ELISA plate reader (Tecan's Sunrise, Austria) at 570 nm wavelength27. In the MTT assay, there were four replicates for each sample.
Osteogenic differentiation protocol
Scaffold sections (Thickness: 1 mm, Diameter: 10 mm) were sterilized by UV light for 1 h and placed in 24-well culture plates (one scaffold per well). Before cell seeding, 200 μl complete medium (low glucose DMEM with 10% FBS and 1% Pen-Strep) was poured on top of the scaffolds and plate was maintained in incubator (37 °C, 5% CO2) for 1 h. Then, bone marrow derived MSCs with a density of 104 per well (suspended in low medium volume ~ 200 μl) were seeded onto scaffolds in dropwise manner. The plate was again maintained in incubator (37 °C, 5% CO2) for 10 min and immediately volume of medium in wells was increased to 1 ml with complete medium. One day after seeding, the culture media was withdrawn and osteogenic media was added (low glucose DMEM, 1% Pen-Strep, 10% FBS, 10 nM dexamethasone, 10 mM β-glycerol phosphate, 50 μM ascorbic acid). Thereafter, half of osteogenic medium of wells was changed every day for 21 days. In the time points of 3, 7, 14 and 21 differentiation process were monitored by measuring calcium deposition amount and alkaline phosphatase enzyme activity.
Alizarin red staining
Amount of calcium deposition onto scaffolds during differentiation process was measured by alizarin red staining assay. Briefly, plate media was withdrawn and scaffolds were rinsed two times with PBS. The samples were fixed by 20 min incubation in 10% formaldehyde followed by washing in PBS. Then, 200 μl of alizarin red solution 1%, adjusted to pH 4.5 with ammonia solution, was dropped on the scaffolds and incubated at 25 °C for 2–3 min. After that, scaffolds were rinsed using acidic PBS (pH 4.2) many times to remove any excess dye and photographed under a light microscope (Motic, China). For quantitative analysis, samples were treated with acetic acid 10% for 30 min at 25 °C under mild shaking. Finally, dissolved dyes were transferred into a 96-well plate and its absorbance reading was done at 550 nm wavelength. Alizarin red standard curves was obtained by measuring optical absorption of its various concentrations at 550 nm wavelength. Calcium content was determined given that a molecule alizarin red binds with two molecules of calcium28. In this test, there were three replicates for each sample.
Alkaline phosphatase assay
The ALP activity was determined by p-nitrophenyl phosphate (pNPP) method using a commercial kit (Pars Azmoon, Iran). First, the media was withdrawn, scaffolds were rinsed with PBS two times and cell lying were done using NP40 lysis buffer. Then, well contents were moved into a 2 ml microtube, centrifuged at 4000 rpm for 5 min and supernatant was transferred into a 96-well plate. After that ALP substrate (pNPP) was added to every well and incubated at 37 °C for 30 min. Finally, reaction was stopped and plate absorbance was read by an ELISA plate reader at 405 nm wavelength. The ALP activity of samples was expressed as Unit/L. In this test, there were three replicates for each sample.
Statistical analysis
Quantitative and qualitative data are expressed as mean (standard deviation) and frequency (percent), respectively. Data analysis was done using one-way ANOVA test followed by tukey post hoc test. P < 0.05 was considered significant in all statistical tests. SPSS version V. 22 and Graph Pad Prism V. 6 were used for statistical analysis.
Ethics code
IR.BMSU.REC.1399.498.
Results
Characterization of bioglasses
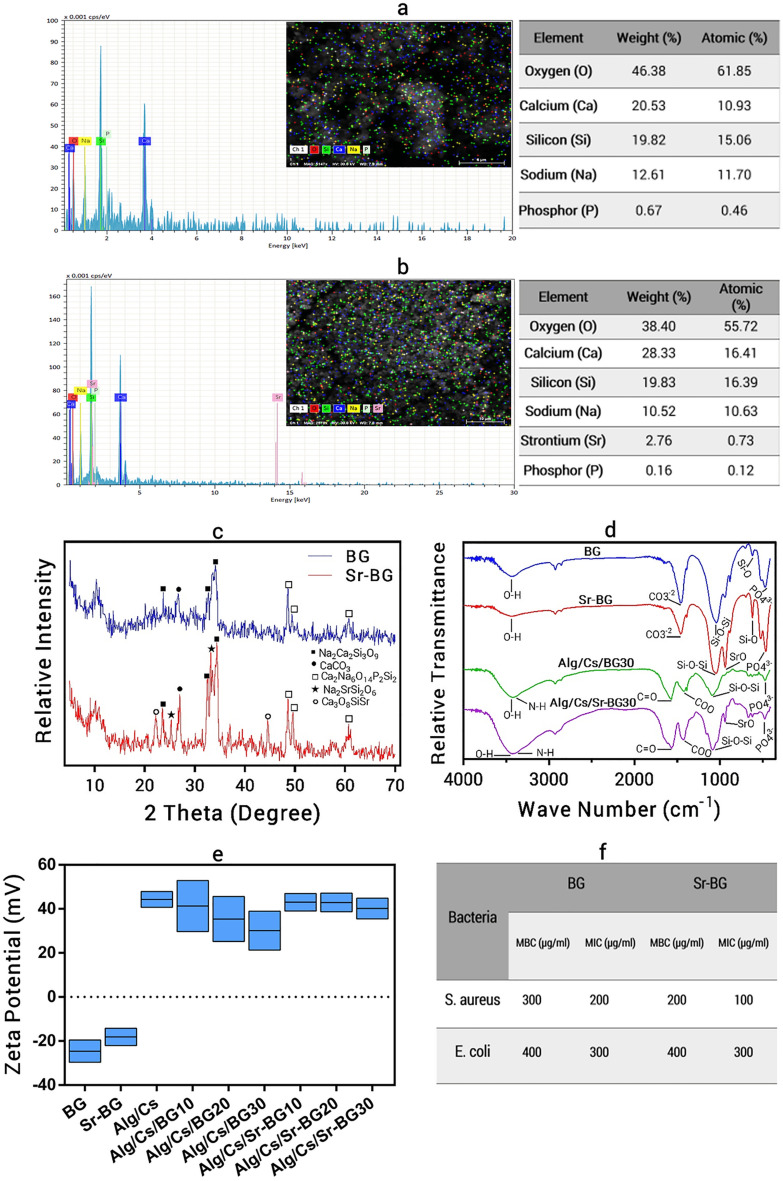
The synthesis steps of bioglass are shown in Fig. 1a. The size and morphology of bioglasses were investigated using SEM and DLS. As shown in Fig. 1c,d, BG and Sr-BG are irregular in shape and their average size is about 200 nm. The high potential zeta increases stability of these particles and prevents their aggregation. The EDS profiles (Fig. 2a,b) indicates the presence of bioglass-specific elements such as sodium, calcium, phosphorus and silicon in the particles structure. The presence of strontium in Sr-BG is obvious. The XRD patterns of BG and Sr-BG are shown in Fig. 2c. Three peaks of combeite (Na2Ca2Si3O9), calcium carbonate (CaCO3) and clinophosinaite (Ca2Na6O14P2Si2) are observed in XRD pattern of both bioglass and Sr-BG particles. Emergence of new peaks in strontium doped bioglasses are related to disodium strontium phyllo-disilicate (Na2SrSi2O6) and calcium strontium silicate (Ca3O8SiSr) crystal systems. The FTIR spectra of BG and Sr-BG samples are brought in Fig. 2d. The bands ranges of 1070 cm−1, 630 cm−1, and 480 cm−1 are related to Si–O–Si, Si–O and PO4–3 groups, respectively, while the peaks at range of 940 cm−1 is correlated with Sr–O bonding. The zeta potential of BG and Sr-BG was − 24.6 (± 5.02) and − 18.1 (± 3.91), respectively (Fig. 2e).
Figure 2.
EDS profile and XRD pattern of bopglasses, FTIR spectra and zeta potential of bioglasses/scaffolds and antimicrobial activity of bioglasses. (a) BG EDS profile, (b) Sr-BG EDS profile, (c) XRD pattern of BG and Sr-BG, (d) FTIR spectra of BG, Sr-BG, Alg/Cs/BG30 and Alg/Cs/Sr-BG30, (e) Zeta potential of bioglasses/scaffolds, (f) Antimicrobial activity of bioglasses.
Antibacterial activity of bioglasses
The antibacterial effect of BG and Sr-BG powders against gram-positive and gram-negative bacteria was evaluated by determining MBC and MIC concentrations (Fig. 2f). MBC and MIC of BG was 300 μg/ml and 200 μg/ml for S. aureus and 400 μg/ml and 300 μg/ml for E. coli, respectively. MBC and MIC of Sr-BG was 200 μg/ml and 100 μg/ml for S. aureus and 400 μg/ml and 300 μg/ml for E. coli.
Characterization of scaffolds
The fabrication steps of scaffolds are shown in Fig. 1b. The surface charge of fabricated scaffolds was measured using DLS (Fig. 2e). A high positive charge of scaffolds leads to good cell-to-scaffold interaction and improved cell attachment. As shown in the Fig. 2e, the positive charge of the scaffolds surface is reduced by increasing the concentration of bioglasses. Surface morphology was evaluated of scaffolds using SEM (Fig. 3a–g). The microscopic and submicron surface roughness and porous structure of the scaffolds with their interconnected pores is excellent for cell attachment and three-dimensional cell growth. The incorporation of BG (presence of Si, Na, Ca and P elements) and Sr-BG (presence of Si, Na, Ca, P and Sr elements) is shown in EDS elemental mapping and profiles (Figs. 4a, S1). The presence of carbon and nitrogen element are attributed to chitosan/alginate in scaffolds. Also, incorporation of BG and Sr-BG particles into scaffolds was confirmed using FTIR (Fig. 2d). The peaks range of 3400–3500 cm−1, 1600 cm−1, and 1460 cm−1 are attributed to O–H, N–H, C=O and COO bonds, respectively. The Si–O–Si and PO4–3 bonds can be observed in FTIR spectra of Alg/Cs/BG30 and Alg/Cs/Sr-BG30 scaffolds. However, Sr–O bonding only can be seen in FTIR spectra of Alg/Cs/Sr-BG30 scaffold.
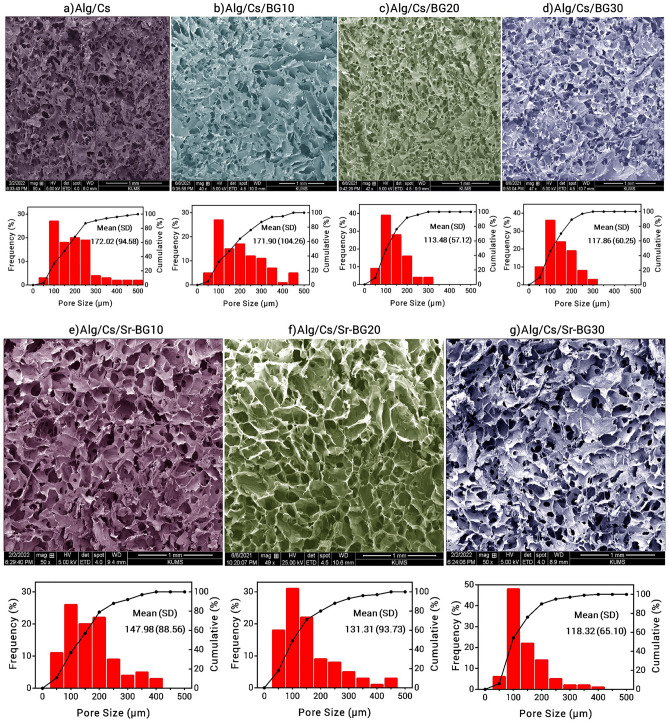
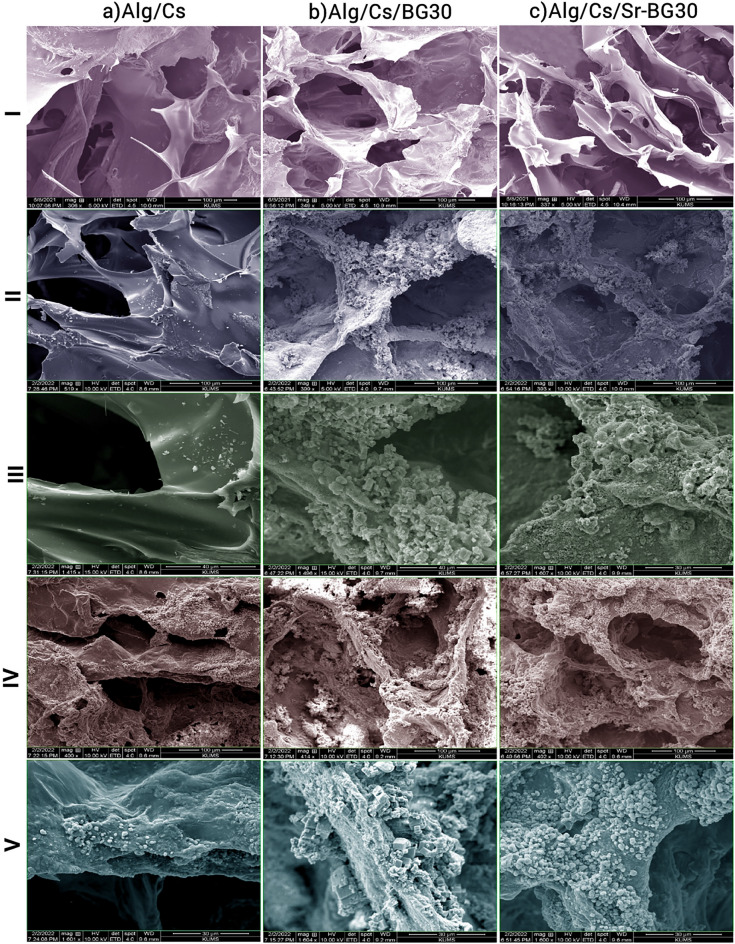
Figure 3.
SEM image and pore size distribution of scaffolds. (a) Alg/Cs, (b) Alg/Cs/BG10, (c) Alg/Cs/BG20, (d) Alg/Cs/BG30, (e) Alg/Cs/Sr-BG10, (f) Alg/Cs/Sr-BG20, (g) Alg/Cs/Sr-BG30.
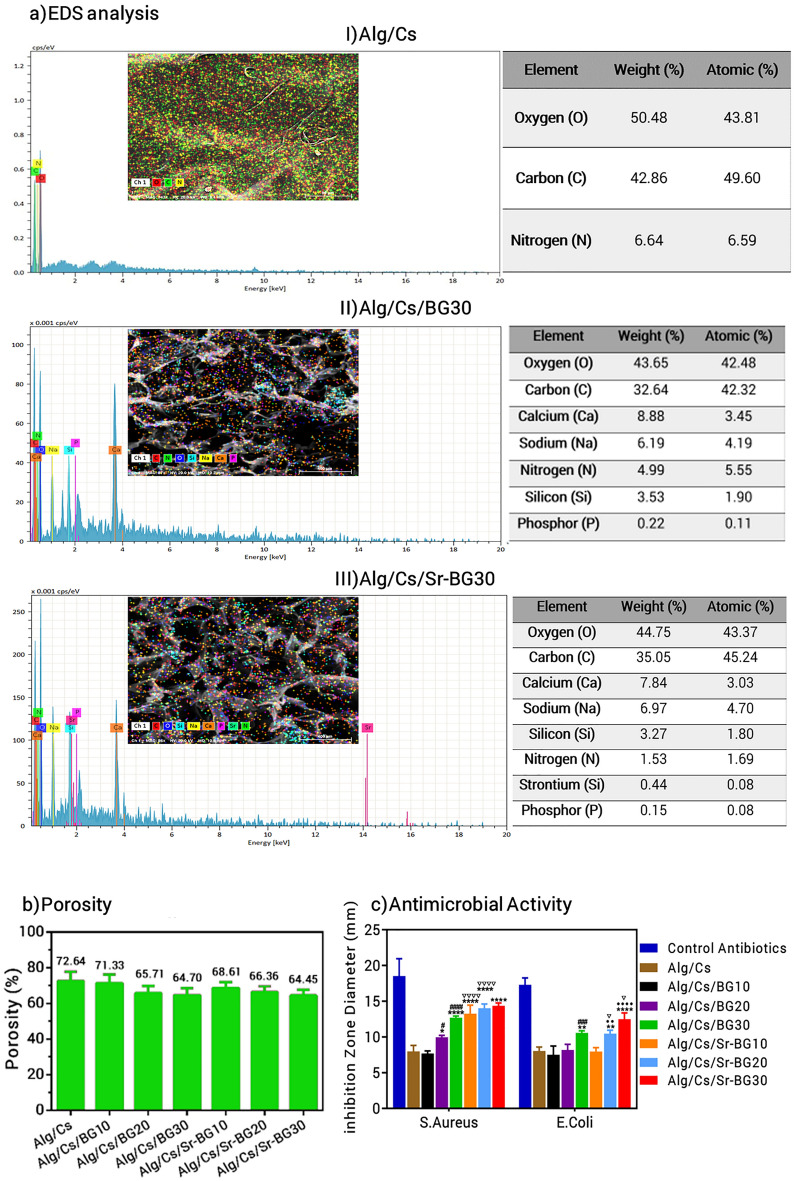
Figure 4.
EDS analysis, Porosity and Antimicrobial activity of scaffolds. (a) EDS analysis: (I) Alg/Cs, (II) Alg/Cs/BG30 and (III) Alg/Cs/Sr-BG30. (b) Porosity, (c) Antibacterial activity. Significant difference with Alg/Cs group at p < 0.05 (*), p < 0.01 (**), p < 0.0001 (****). Significant difference with Alg/Cs/BG10 group at p < 0.05 (#), p < 0.001 (###), p < 0.0001 (####). Significant difference with Alg/Cs/Sr-BG10 group at p < 0.01 (··), p < 0.0001 (····). Significant difference between Alg/Cs/BG and Alg/Cs/Sr-BG groups at p < 0.05 (⛛), p < 0.05 (⛛⛛⛛⛛).
Scaffolds porosity and pore size
The porosity percent of Alg/Cs, Alg/Cs/BG10, Alg/Cs/BG20, Alg/Cs/BG30, Alg/Cs/Sr-BG10, Alg/Cs/Sr-BG20 and Alg/Cs/Sr-BG30 scaffolds was 72.64 (± 5.26), 71.31 (± 4.94), 65.71 (± 3.99), 64.70 (± 3.80), 68.61 (± 3.40), 66.36 (± 3.30) and 64.09 (± 3.20), respectively (Figs. 4b, S2a–g). The pore size of fabricated scaffolds was varied from less than 50 μm to 500 μm. The average pore size of Alg/Cs, Alg/Cs/BG10, Alg/Cs/BG20, Alg/Cs/BG30, Alg/Cs/Sr-BG10, Alg/Cs/Sr-BG20 and Alg/Cs/Sr-BG30 scaffolds was 172.02 (± 94.58), 171.90 (± 104.26), 113.48 (± 57.12), 117.86 (± 60.25), 147.98 (± 88.56), 131.31 (± 93.73) and 118.32 (± 65.10) μm, respectively (Fig. 3a–g).
Antibacterial activity of scaffolds
Alg/Cs/BG20, 30 and Alg/Cs/Sr-BG10, 20, 30 scaffolds showed significant antibacterial activity against S. aureus. Alg/Cs/BG30 and Alg/Cs/Sr-BG20, 30 scaffolds exhibited significant antibacterial effect against E. coli. Addition of strontium into scaffolds increased antibacterial effects of scaffolds against S. aureus more considerably than E. coli (Figs. 4c, S3a).
Scaffolds in vitro bioactivity
Following 7 and 14-days immersion in SBF at 37 °C, scaffolds samples were harvested and analyzed in order observing hydroxyapatite like phase deposition on the scaffolds surface. Before and After 7 and 14-days immersion, SEM images were taken (Fig. 5I–V). Almost no deposits were observed on Alg/Cs scaffold after 7 days incubations, however some depositions were formed following 14 days incubation. It seems, amount of deposition of crystals in Alg/Cs/BG30 scaffold is relatively higher than Alg/Cs/Sr-BG30 scaffold at 7 and 14 days of incubation.
Figure 5.
SEM images of scaffolds surface for evaluating biomineralization. (a) Alg/Cs, (b) Alg/Cs/BG30 and (c) Alg/Cs/Sr-BG30 scaffolds, (I) before submerging, (II) after 7 days submerging (100 μm scale), (III) after 7 days submerging (30 μm scale), (IV) after 14 days submerging (100 μm scale), (V) after 14 days submerging (30 μm scale).
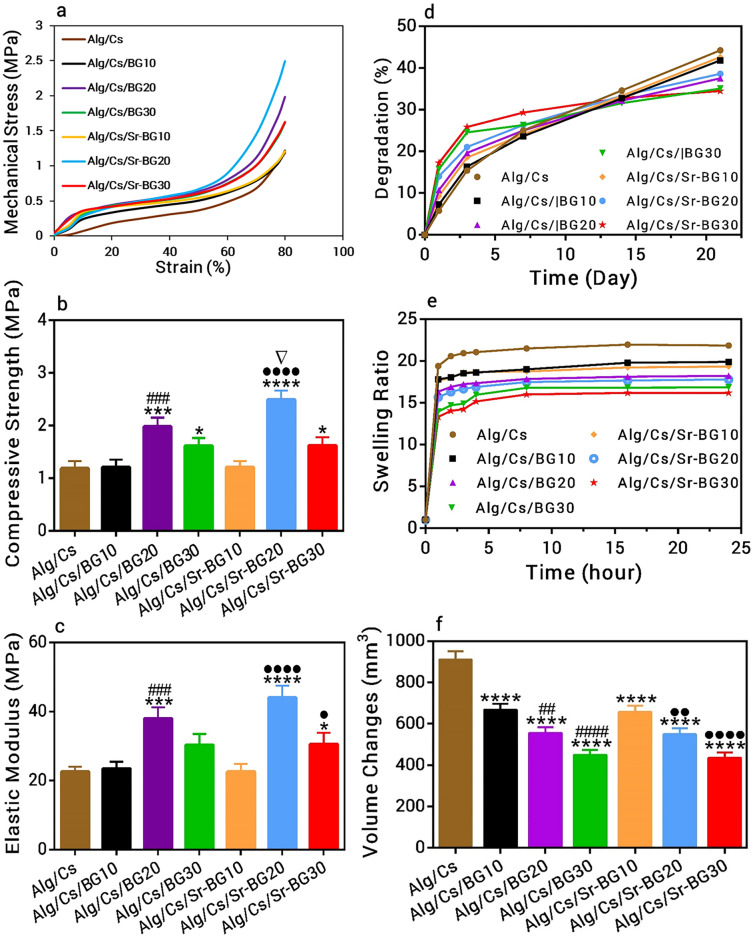
Scaffolds mechanical test
The compressive strength and also elastic modulus of different scaffolds was measured using a mechanical test machine. The highest mechanical strength was related to Alg/Cs/Sr-BG20 scaffold followed by Alg/Cs/BG20 scaffold. The Alg/Cs, Alg/Cs/BG10 and Alg/Cs/Sr-BG10 scaffolds had similar mechanical properties. The Alg/Cs/BG30 and Alg/Cs/Sr-BG30 scaffolds had intermediate mechanical strength; higher than that of Alg/Cs, Alg/Cs/BG10 and Alg/Cs/Sr-BG10 scaffolds and lower than that of Alg/Cs/Sr-BG20 and Alg/Cs/BG20 scaffolds (Fig. 6a–c).
Figure 6.
Mechanical test, degradation and swelling profile of scaffolds. (a) Stress–strain curve, (b) Compressive strength, (c) Elastic Modules, (d) Degradation profile, (e) Swelling profile and (f) Volume changes during swelling. Significant difference with Alg/Cs group at p < 0.05 (*), p < 0.001 (***), p < 0.0001 (****). Significant difference with Alg/Cs/BG10 group at p < 0.01 (##), p < 0.001 (###), p < 0.0001 (####). Significant difference with Alg/Cs/Sr-BG10 group at p < 0.05 (·), p < 0.01 (··), p < 0.0001 (····). Significant difference between Alg/Cs/BG and Alg/Cs/Sr-BG groups at p < 0.05 (⛛).
Scaffolds degradation rate
Degradation percentage of different scaffolds were examined following 21 days soaking in PBS. In the first 12 days, the highest degradation percentage was related to the Alg/Cs/Sr-BG30 followed by Alg/Cs/BG30. In this time period, degradation ratio was gradually decreased by decreasing bioglass concentration. After 12th day, the degradation rate of bioglass containing scaffolds decreased, so that highest amount of observed degradation was related to Alg/Cs Scaffold followed by Alg/Cs/Sr-BG10 and Alg/Cs/BG10 scaffolds (Fig. 6d).
Scaffolds swelling profile
Alg/Cs scaffold showed highest swelling rate compared to Alg/Cs/BG or Alg/Cs/Sr-BG Scaffolds. Incorporation of BG or Sr-BG particles into scaffolds has been reduced the water uptake capacity of related scaffolds. Also, scaffolds water uptake ability was decreased gradually with increasing the concentration of BG or Sr-BG in their structure. However, it seems that doping of strontium in BG has no impact on the swelling behavior of BG-containing scaffolds (Fig. 6e). Dimensional changes of scaffolds following swelling was in accordance with their swelling changes (Fig. 6f).
MSCs characterization
Isolated MSCs were characterized morphologically (Fig. S3b) and also by measuring of expressing level of some surface markers using flowcytometry (Fig. S3c). High level of expression of positive surface markers (CD44, CD90 and CD29) and low expression level of negative surface markers (CD34 and CD45) indicates the high purity of isolated MSCs.
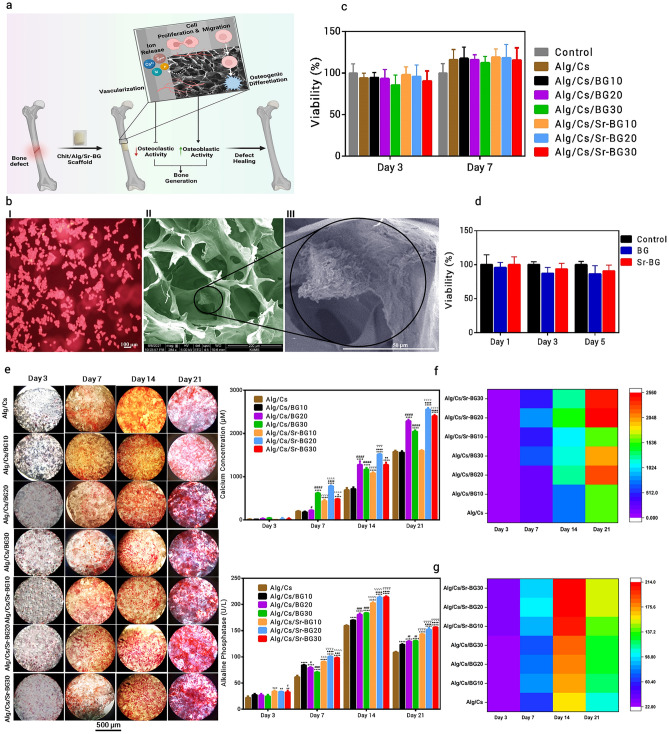
Cell attachment, viability and differentiation
Potential clinical application of fabricated scaffold is shown in Fig. 7a. Major bone defects can be filled by fabricated scaffolds for accelerating bone healing procedure. As shown, released ions from scaffold can provoke different cellular responses. These bone substitute scaffolds could induce stem cell proliferation and differentiation as well as vascularization into porous structure of scaffolds. Strontium-doped bioglass in scaffolds increase bone formation and prevents bone reabsorption.
Figure 7.
Potential clinical application and cellular studies results. (a) Potential clinical application, (b) Scaffold cell adhesion: (I)Florescence image, (II) SEM image and (III) Magnified SEM image, (c) Toxicity of scaffolds, (d) Bioglass toxicity, (e) Alizarin red staining of scaffolds, (f) Calcium content of scaffolds, (g) Alkaline phosphatase activity of scaffolds, Significant difference with Alg/Cs group at p < 0.01 (**), p < 0.001 (***), p < 0.0001 (****). Significant difference with Alg/Cs/BG10 group at p < 0.05 (#), p < 0.01 (##), p < 0.0001 (####). Significant difference with Alg/Cs/Sr-BG10 group at p < 0.05 (·), p < 0.01 (··), p < 0.001 (···), p < 0.0001 (····). Significant difference between Alg/Cs/BG and Alg/Cs/Sr-BG groups at p < 0.05 (⛛), p < 0.001 (⛛⛛⛛), p < 0.0001 (▽▽▽▽).
Fluorescence and SEM images showed excellent cell-scaffold interaction (Fig. 7b). The MTT assay was used for evaluating bioglass toxicity and also measuring viability of cells on different scaffolds. As shown in Fig. 7c,d, there were no significant difference among different groups in terms of cell viability (p > 0.05). Osteogenic differentiation process of MSCs on different scaffolds was evaluated using alizarin red assay (qualitative and quantitative) and alkaline phosphatase assay (Fig. 7e,f,g). Qualitative alizarin red test showed that calcium deposition in Alg/Cs/Sr-BG20 sample followed by Alg/Cs/BG20, Alg/Cs/Sr-BG30 and Alg/Cs/BG30 samples is higher than Alg/Cs/Sr-BG10, Alg/Cs/BG10 and Alg/Cs samples (Fig. 7e). Quantitative alizarin red test (Fig. 7f, calcium content) findings were in accordance with qualitative alizarin red test. However, Alkaline phosphatase activity was increased gradually by increasing BG or Sr-BG concentrations in scaffolds (Fig. 7g). Also, higher Alkaline phosphatase activity was observed in Alg/Cs/Sr-BG samples than Alg/Cs/BG samples. Alkaline phosphatase activity together with calcium deposition were increased in different samples over time. But there was an exception for the 21st day that alkaline phosphatase activity decreased compared to the 14th day.
Discussion
Given the high incidence of large bone defects raised from different injuries and obstacles in current therapies such as bone grafting, major advances are needed in bone regeneration techniques. Thus, researchers have proposed new treatment approaches such as bone repairing using 3D scaffolds29. Scaffolds fabricated from natural materials are most hopeful because of their excellent features including biocompatibility and biodegradability24. Incorporation of bioactive glasses into natural polymers can enhance mechanical and biological properties of scaffolds. Bioglasses act as mineralization agents and have osteoconductive properties that can improve bone formation and bonding to the adjacent hard (bone) and soft tissues23. Also, trace elements have been extensively used as regenerative supplies in bone defect healing. Strontium is a metal ion that is broadly found in the bone and its promoting effects in bone renewal has been revealed29. In present study, we made chitosan/alginate/strontium doped bioglass composite scaffolds with optimized features for bone tissue engineering.
First, nanosized (~ 200 nm) bioglasses were synthesized using sol–gel method. This nano (sub-micron) particles provide higher surface area of bioactive glass and in a result more binding sites for cell adhesion and bone formation3. The size of nanoparticles has direct effect on their biological activity30. Panda et al., reported that nano-scale environment is favorable for stem cell attachment, propagation and differentiation through an increase in reciprocal interactions between extracellular matrix and cells31. SEM and FESEM images of bioglasses showed irregular shape and homogenous size. The size of the bioglasses in the SEM and FESEM images appeared to be smaller than the size measured by the DLS. The difference in size gained by these methods may be due that (FE)SEM measures the real size, whereas the DLS measures the hydrodynamic radius, which includes the hydration layer and is larger than the real size32. In consistent with previous studies, our synthesized nanoparticles have negative zeta potential33. The zeta potential shows the degree of repulsion between suspension particles. A high negative or positive zeta potential (± 25 mV or higher) will confer particle stability and prevent their aggregation33.
The weak peaks in XRD patterns of bioglasses indicates the presence of an amorphous compound or substance with semi-crystalline form. These peaks were fitted to combeite (Na2Ca2Si3O9), calcium carbonate (CaCO3) and clinophosinaite (Ca2Na6O14P2Si2)34. After strontium incorporation, disodium strontium phyllo-disilicate (Na2SrSi2O6) and calcium strontium silicate (Ca3O8SiSr( peaks were emerged34,35. Chen et al., found that development of combeite phase is more promising because it gives the scaffolds higher mechanical stability and converts into bioactive and biodegradable crystalline phase of calcium phosphate after placement in vivo36. In previous published works, growth of small crystals on amorphous glasses in result of sintering have been reported35. The amorphous or semicrystalline form of the bioglass will support easy reaction with body fluid and its conversion to hydroxyapatite37. The presence of Sr trace element in bioglass structure was further confirmed by EDS elemental composition analysis. In accordance with previously published works the main elements in bioglass and Sr doped bioglass were calcium, phosphor, sodium and silicon38. Release of these soluble ions from the bioglasses can direct cellular phenomena and trigger biological responses, including angiogenesis39. The main FTIR peaks in bioglass and Sr doped bioglass were including ~ 1070 cm−1, ~ 630 cm−1, and ~ 480 cm−1 that were related to Si–O–Si, Si–O and PO4–3 groups, respectively40,41. But, the peak at 940 cm−1 was only observed in Sr-doped bioglass and was related to Sr–O bonding34. Si–O–Si and PO4–3 bonds also can be observed in FTIR spectra of scaffolds, while Sr–O bond was only observed in Alg/Cs/Sr-BG30 scaffold. The peaks range of 3400–3500 cm−1, 1600 cm−1, and 1460 cm−1 in scaffolds were attributed to O–H, N–H, C=O and COO bonds of alginate/chitosan25.
EDS elemental analysis revealed the uniform distribution of BG or Sr-BG specific elements in throughout the scaffolds’ structure. These bioactive materials have the supportive surface properties for cellular adhesion and multiplication and inducing new bone formation. In addition to bioactive factors, cell adhesion ability can also be affected by surface charge of scaffolds. In our study, fabricated scaffolds had a positive surface charge that gradually decreased by increasing the concentration of bioglasses. Numerous researches have showed that cells more efficiently adhere to surfaces with positive charge rather than neutral or negatively charged surfaces42,43. Other important factor affecting cell adhesion on polymers surfaces irrespective of the bioactive materials, cell type and surface charge is surface roughness of substrate. Microscopic and submicron roughness, similar to what existed in our fabricated scaffolds, has positive effects on cell adhesion as well as cell growth44.
The SEM images illustrated the highly porous nature of all fabricated scaffolds. The size of these interconnected pores was varied from less than 50 μm to 500 μm. The mean of pore size was ranged between 113.48 and 172.02 μm. The porous structure of scaffolds with variable pore sizes is essential for cell migration, neovascularization, nutrient/waste product diffusion and formation of new bone tissues45. The minimal and maximal acceptable pore size for tissue engineering purposes is 75 μm and 900 μm, respectively. The pore sizes far from this range, it is either very small for adequate material exchange/cell migration, or too large that reduces the area/volume ratio and in a result slows new bone tissue formation. The porosity of our fabricated scaffolds was ranged between 64 and 72%. In Karimi et al., study porosity of chitosan/alginate composite scaffolds was ranged between 66 to 72 percent25. However, in Zamani et al. study, porosity of scaffolds was over 80%26. The natural cancellous (spongy) bone is composed from trabecular bone with a porosity of about 50 to 90 percent, and cortical or compact bone generally has 10–20% porosity. An increase in bone porosity led to reduced bone density and increased chance of bone fracture46.
In some researches it has stated that a porosity of 90% or higher is optimal for bone tissue engineering purposes47,48. However, as mentioned, higher porosity led to a reduction in mechanical stability of bone/scaffolds. So, determining the balance between porosity and mechanical strength is an essential challenge to make bone substitute scaffolds25. In this regard, most researches, including our study, have used scaffolds with lower porosity from 55 to 74% in order to maintain mechanical strength49. The porosity of scaffolds was decreased slightly by increasing the bioglass concentration. Also, the average pore size of Alg/Cs/BG20 and Alg/Cs/BG30 scaffolds and Alg/Cs/Sr-BG20 and Alg/Cs/Sr-BG30 scaffolds were lower than Alg/Cs, Alg/Cs/BG10 and Alg/Cs/Sr-BG10 scaffolds, respectively. It seems that presence of bioglass increases the thickness of the pore wall and thus reduces their size. So, reducing the size of the pores eventually leads to a reduction in porosity. Another probable reason is that the ice crystals size produced during freeze drying maybe affected mainly due to the interaction between bioglass particles with water molecules50.
Biomineralization results showed highest hydroxyapatite like phase formation on the surface of BG containing Sr-BG than Srbioglass containing scaffolds. Pure Alg/Cs scaffolds had lowest deposits among all scaffolds, because calcium and phosphorus are two main ions for formation of hydroxyapatite51. Since the scaffolds were cross linked by calcium chloride, so some formed deposits in Alg/Cs scaffolds maybe related to small size calcium crystals. Lower deposits amount in Sr-BG containing scaffolds than BG containing one may be due to substituting of calcium by strontium, in a result their lower calcium content and lower deposits formation21. Hydroxyapatite can stablish robust bonds with collagen produced by osteoblasts26. As discussed, the formation of hydroxyapatite is mainly due to the degradation of bioglass content in the scaffolds. First phase in bioactive glass degradation is replacing the released ions from bioglass with proton (H+) from the surrounding media. Thus, higher concentration of H+ ions in solution can accelerate the onset of bioglass degradation52. Consequently, ion release from bioactive glasses occurs significantly quicker at acidic environment, leading to higher concentration of calcium and phosphate ions in the solutions. This results in considerably faster formation and more precipitation of apatite in acidic solutions53. It was shown that ion release (e.g., calcium and phosphate) from bioglass is much faster at acidic pH than physiological one54. In another study, faster ion release and apatite formation was reported at low pH owing to higher concentration of protons being available in environment for ion exchange with modifier cations55.
Swelling and water uptake ability of scaffolds is necessary for diffusion of56. Also, early swelling provokes cellular attachment and proliferation57. In present study, water uptake ability of scaffolds was reduced by increasing bioglass concentration, which may due to decline in average pore size and porosity. Another possible reason is the reduction of polymer content of scaffolds, because scaffold swelling ability mainly is due to the bonding of polymer chains with H2O molecules58. Degradation ratio of scaffolds was proportional to their swelling ratio. In this way, lower degradation ratio during 21 days was related to Alg/Cs/BG30 and Alg/Cs/Sr-BG30 scaffolds and higher degradation ratio during 21 days was related to Alg/Cs, Alg/Cs/BG10 and Alg/Cs/Sr-BG10 scaffolds. Therefore, adding bioglass into Alg/Cs scaffold prevents its rapid degradation and making it suitable for long term performance. It seems that bioglass reduces scaffold hydrophilicity and also dissolution of bioglass particles can buffers the solution at the surface of scaffold, as a result slow down its degradation. Also, some dissolved ions including calcium released from bioglass can cross link the chitosan-alginate matrix and retard scaffold degradation. In this study, incorporation of strontium in bioglass had no effect on the degradation and swelling profile of BG containing scaffolds. As a rule, water uptake ability, degradation ratio and porosity of scaffolds could also affect their mechanical strength26,59,60.
The bone substitutes scaffolds must have enough mechanical stability to tolerate the external forces suitably and preserve their integrity so long as new bone is formed. Mechanical properties of scaffolds were evaluated by plotting stress–strain curve and measuring the elastic modulus. We showed that adding bioglass to Alg/Cs scaffold improves its mechanical stability. This finding is in line with the composite theories61. It is possible that addition of bioactive glass into scaffold content stabilize polymer bonds. Also, Mechanical properties of bioglass containing scaffolds was enhanced in presence of Sr. It has been Sown that replacement of CaO by SrO with higher ionic radius, increases the number of interactions in bioglass bonding network62. Nevertheless, mechanical strength was decreased with more increasing in the bioglass concentration. Higher mechanical strength and elastic modulus in Alg/Cs/BG20 or Sr-BG20 than Alg/Cs/BG30 or Sr-BG30 may be due to the instability of the polymer bonds at higher concentrations of bioglass. On other that, in higher bioglass concentrations the possibility of accumulation and inconsistent dispersion of this particles increased and can cause bioglass/polymer interface defects26. So, optimum bioglass percentage for higher mechanical strength was 20%. In general, with considering mechanical strength of cortical (90–209 MPa) and cancellous (1.5–45 MPa) bone63, our fabricated scaffolds can be appropriate for bone repairing of cancellous bones.
Our synthesized bioglasses and Sr doped bioglasses slightly reduced cell survival in applied concentration (0.5 mg/ml) but not significantly in comparison with control group. However, viability of cell treated with Sr-BG was more similar to control group and higher than those treated with bioglass, which is in agreement with previous works on other Sr-doped bioceramics64. However, BG and Sr-BG had significant antibacterial effect in lower concentrations (< 400 µg/ml). Sr-BG showed higher antibacterial effect against S. aureus (MBC = 200 µg/ml) compared to BG (300 µg/ml), but in the case of E. coli, there was no difference between the BG and Sr-BG. Baheiraei et al., reported that strontium substitution enhances antibacterial effect of BG against S. aureus more than E. coli65. According to previous studies, BG, even without any addition, can inhibit growth many bacteria mainly due to increased pH generated by Na ion release66. Also, increasing osmotic pressure caused by dissolution of other ions including Sr, Si, Ca and P is unfavorable for bacterial growth65. Therefore, more antibacterial effect of Sr-BG than BG can be in a result of the higher concentration of the released ions. Sr has larger ionic radius than Ca and significantly increase the bioglass solubility and ionic release rate67. Antibacterial activity is an important and determining property for nanocomposites68. We observed a weak antibacterial effect for Alg/Cs scaffold only against S. aureus that also has been reported in other studies69, while addition of high concentration BG or Sr-BG increased antibacterial effects of scaffolds against both S. aureus and E. coli. Strontium addition into scaffolds increased antibacterial effects against S. aureus more than E. coli. These finding shows that antibacterial effects of fabricated scaffolds are mainly due to the presence of BG or Sr-BG.
Shoaib et al., revealed that different concentration of bioactive glass nanoparticles (0–100 μg/ml) have no significant cytotoxic effect on NHFB and MG-63 cell lines70. Zheng et al., reported that 100 μg/ml concentration of bioglass nanoparticles had no significant toxicity towards human MSCs71. Rismanchian et al., indicated that bioactive glasses have no significant inhibitory effect on fibroblasts cells growth at different concentrations up to 1.5 mg/ml72. Amudha et al., showed that proliferation rate of NIH3T3 cells after treatment with Sr-doped bioglass samples resembles the control group and is higher than those treated with Sr-free bioglass73. In Zhu et al., study substitution of calcium with Sr in mesoporous CaSiO3 materials increased proliferation of MC3T3-E1 cells compared to control and mesoporous Sr-free CaSiO374. Also, we indicated that there is no significant difference among different scaffolds and also between them with control group regarding cell growth at day 3 and 7. It is noteworthy that cell viability on scaffolds was slightly lower and higher than control group at day 3 and 7, respectively. In addition, viability of cells on Alg/Cs/Sr-BG scaffolds were slightly higher than Alg/Cs/BG Scaffolds at all times. Highest cell viability was related to Alg/Cs/Sr-BG10 followed by Alg/Cs/BG10 scaffolds and decreased negligibility with increase in bioglass concentration, likely due to high amount of released ions75. In Zhao et al., study cell proliferation rate was higher in 5Sr-BG scaffolds than BG scaffolds and control group at all time, but reduced in 10Sr-BG scaffolds76. Also, our scaffolds especially Alg/Cs/BG20 and Alg/Cs/Sr-BG20,30 scaffolds were as good as popular scaffolds such as PCL based one regarding viability results77.
Differentiation process was evaluated using qualitative/quantitative alizarin red assay and alkaline phosphatase test. Alizarin red test showed that calcium deposition in Alg/Cs/Sr-BG20 sample followed by Alg/Cs/BG20, Alg/Cs/Sr-BG30 and Alg/Cs/BG30 samples is higher than Alg/Cs/Sr-BG10, Alg/Cs/BG10 and Alg/Cs samples. Thus, moderate concentration of bioglass promotes more bone formation than lower or higher concentrations. Bone formation amount was higher in Alg/Cs/Sr-BG scaffolds than Alg/Cs/BG Scaffolds. Some reduction in calcium deposition in scaffolds containing 30% BG or Sr-BG may be due to a slight reduction in cell proliferation in result of accumulation of high level of released ions75. Released ions from bioactive glasses are identified to effect osteogenic markers like alkaline phosphatase and improve osteogenesis by regulation of genes that induce cell differentiation towards mature osteoblasts29,78–81. Also, bioglasses provides an appropriate substrate for the cell attachment and expansion82. It has been reported that doping of strontium in bioglass provokes more bone formation and prevents bone reabsorption83. Strontium accelerates osteogenic differentiation by inducing several pathways such as Ras/MAPK, Ca sensing receptor and Wnt/β-Catenin signaling and prevents osteoclastogenesis by inhibiting interaction of Rank ligand with regarding receptor84. Zhao et al., reported that Sr-containing mesoporous bioactive glass scaffolds have enhanced vascularization and osteogenesis properties than non-Sr samples85. ALP results were in accordance with alizarin red results with the difference that there was no considerable difference between Alg/Cs/Sr-BG20 and Alg/Cs/Sr-BG30 scaffolds or between Alg/Cs/BG20 and Alg/Cs/BG30 scaffolds regarding ALP activity especially in day 14 and 21. This inconsistency can originate from the fact that ALP activity is normalized by cell number, therefore its result cannot be affected by change in cell proliferation rate86. Alkaline phosphatase activity was increased along with calcium deposition in different samples over time. But there was an exception for the 21st day that alkaline phosphatase activity decreased compared to the 14th day. Previous studies have mentioned that alkaline phosphatase activity is a primary (early-stage) marker of osteogenic differentiation87, i.e., its highest activity in mature osteoblasts which declining in differentiated osteoblasts into osteocytes88. Ahmadi et al., reported similar results89. Also, this finding of our study is consistent with Nanda et al., study90,91. When we compare our Alg/Cs/BG20 and Alg/Cs/Sr-BG20,30 scaffolds with well-known scaffolds such as PCL on new bone generation (calcium deposition and ALP), they have similar clinical potential to them92,93.
Conclusion
We made chitosan alginate scaffolds containing different concentrations of bioglass or Sr doped bioglass. These scaffolds had optimal and desirable characteristics regarding porosity, mechanical strength, degradation and swelling profile, biomineralization, antibacterial activity, cell proliferation and differentiation. Adding bioglass into Alg/Cs matrix improved some scaffold characteristics such as mechanical stability, degradation and swelling profile, biomineralization, antibacterial effects, and cell differentiation. Also, incorporation of Sr into bioglass containing Alg/Cs scaffold led to reinforcement of mechanical strength and more efficient cell differentiation and antibacterial activity when compared with pure Alg/Cs scaffold or Sr-free bioglass containing scaffolds. However, some features such as mechanical stability and cell differentiation showed better enhancement in optimal concentration of BG or Sr-BG 20% compared to lower or high concentrations. It should be noted, biomineralization was relatively higher in BG containing scaffolds than Sr-BG containing scaffolds, anywhere this difference was not considerable. Therefore, it can be said that Alg/Cs/Sr-BG20 scaffold (because of excellent mechanical and biological features) are more suitable for repairing large bone injuries. In order to more biological investigation of fabricated scaffolds, we will design animal studies in the future works.
Supplementary Information
Author contributions
H.M.: Investigation; methodology; data acquisition; formal analysis; writing—original draft. M.G.: Investigation; project administration; Supervision. M.M.M.: Methodology, validation, writing—review and editing. M.R.N.: Investigation, methodology, validation. P.M.: Formal analysis; writing—review and editing; validation. E.S.: Investigation; methodology; project administration; supervision.
Data availability
Data are available on reasonable request from the corresponding author.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-024-76673-7"
Change history
10/22/2024
This article has been retracted. Please see the Retraction Notice for more detail: 10.1038/s41598-024-76673-7
Contributor Information
Masoud Ghorbani, Email: Dr.ghorbani62@yahoo.com.
Esmaeel Sharifi, Email: Esmaeel.sharifi@gmail.com.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-14329-0.
References
- 1.Erol-Taygun, M., Unalan, I., Idris, M. I. B., Mano, J. F. & Boccaccini, A. R. Bioactıve glass-polymer nanocomposites for bone tissue regeneration applications: A review. Adv. Eng. Mater.21(8), 1900287 (2019). [Google Scholar]
- 2.Bhatt, R. A. & Rozental, T. D. Bone graft substitutes. Hand Clin.28(4), 457–468 (2012). [DOI] [PubMed] [Google Scholar]
- 3.Haider, A., Waseem, A., Karpukhina, N. & Mohsin, S. Strontium-and Zinc-containing bioactive glass and alginates scaffolds. Bioengineering7(1), 10 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dave, K. & Gomes, V. G. Bioresorbable poly (lactic acid) and organic quantum dot-based nanocomposites: Luminescent scaffolds for enhanced osteogenesis and real-time monitoring. J. Nanostruct. Chem.2021, 1–12 (2021). [Google Scholar]
- 5.Polo-Corrales, L., Latorre-Esteves, M. & Ramirez-Vick, J. E. Scaffold design for bone regeneration. J. Nanosci. Nanotechnol.14(1), 15–56 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghassemi, T. et al. Current concepts in scaffolding for bone tissue engineering. Arch. Bone Joint Surg.6(2), 90 (2018). [PMC free article] [PubMed] [Google Scholar]
- 7.Bagheri, M., Validi, M., Gholipour, A., Makvandi, P. & Sharifi, E. Chitosan nanofiber biocomposites for potential wound healing applications: Antioxidant activity with synergic antibacterial effect. Bioeng. Transl. Med.7(1), e10254 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharifi, E., Chehelgerdi, M., Fatahian-Kelishadrokhi, A., Yazdani-Nafchi, F. & Ashrafi-Dehkordi, K. Comparison of therapeutic effects of encapsulated Mesenchymal stem cells in Aloe vera gel and Chitosan-based gel in healing of grade-II burn injuries. Regen. Ther.18, 30–37 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Muzzarelli, R. A. A. Chitosan composites with inorganics, morphogenetic proteins and stem cells, for bone regeneration. Carbohyd. Polym.83(4), 1433–1445 (2011). [Google Scholar]
- 10.Nikbakht, M., Karbasi, S., Rezayat, S. M., Tavakol, S. & Sharifi, E. Evaluation of the effects of hyaluronic acid on poly (3-hydroxybutyrate)/chitosan/carbon nanotubes electrospun scaffold: Structure and mechanical properties. Polym. Plast. Technol. Mater.58(18), 2031–2040 (2019). [Google Scholar]
- 11.Suárez-González, D. et al. Controlled nucleation of hydroxyapatite on alginate scaffolds for stem cell-based bone tissue engineering. J. Biomed. Mater. Res. A95(1), 222–234 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee, K. Y. & Mooney, D. J. Alginate: Properties and biomedical applications. Prog. Polym. Sci.37(1), 106–126 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim, H. L. et al. Preparation and characterization of nano-sized hydroxyapatite/alginate/chitosan composite scaffolds for bone tissue engineering. Mater. Sci. Eng. C54, 20–25 (2015). [DOI] [PubMed] [Google Scholar]
- 14.Venkatesan, J., Bhatnagar, I., Manivasagan, P., Kang, K. H. & Kim, S. K. Alginate composites for bone tissue engineering: A review. Int. J. Biol. Macromol.72, 269–281 (2015). [DOI] [PubMed] [Google Scholar]
- 15.Ll, H. The story of bioglass. J. Mater. Sci. Mater. Med.17(11), 967–978 (2006). [DOI] [PubMed] [Google Scholar]
- 16.Hatton, J. et al. Fabrication of porous bone scaffolds using alginate and bioactive glass. J. Funct. Biomater.10(1), 15 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoppe, A., Güldal, N. S. & Boccaccini, A. R. A review of the biological response to ionic dissolution products from bioactive glasses and glass-ceramics. Biomaterials32(11), 2757–2774 (2011). [DOI] [PubMed] [Google Scholar]
- 18.Dasgupta, S., Banerjee, S. S., Bandyopadhyay, A. & Bose, S. Zn-and Mg-doped hydroxyapatite nanoparticles for controlled release of protein. Langmuir26(7), 4958–4964 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reginster, J. Y. et al. Efficacy and safety of strontium ranelate in the treatment of knee osteoarthritis: Results of a double-blind, randomised placebo-controlled trial. Ann. Rheum. Dis.72(2), 179–186 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anand, V., Singh, K. J. & Kaur, K. Evaluation of zinc and magnesium doped 45S5 mesoporous bioactive glass system for the growth of hydroxyl apatite layer. J. Non. Cryst. Solids.406, 88–94 (2014). [Google Scholar]
- 21.Goh, Y. F., Alshemary, A. Z., Akram, M., Kadir, M. R. A. & Hussain, R. In vitro study of nano-sized zinc doped bioactive glass. Mater. Chem. Phys.137(3), 1031–1038 (2013). [Google Scholar]
- 22.Luo, Y., Lode, A., Wu, C., Chang, J. & Gelinsky, M. Alginate/nanohydroxyapatite scaffolds with designed core/shell structures fabricated by 3D plotting and in situ mineralization for bone tissue engineering. ACS Appl. Mater. Interfaces.7(12), 6541–6549 (2015). [DOI] [PubMed] [Google Scholar]
- 23.Sharifi, E. et al. Preparation of a biomimetic composite scaffold from gelatin/collagen and bioactive glass fibers for bone tissue engineering. Mater. Sci. Eng. C59, 533–541 (2016). [DOI] [PubMed] [Google Scholar]
- 24.Shamosi, A. et al. Differentiation of human endometrial stem cells into endothelial-like cells on gelatin/chitosan/bioglass nanofibrous scaffolds. Artif. Cells Nanomed. Biotechnol.45(1), 163–173 (2017). [DOI] [PubMed] [Google Scholar]
- 25.Karimi, M., Mesgar, A. S. & Mohammadi, Z. Development of osteogenic chitosan/alginate scaffolds reinforced with silicocarnotite containing apatitic fibers. Biomed. Mater.15(5), 055020 (2020). [DOI] [PubMed] [Google Scholar]
- 26.Zamani, D., Moztarzadeh, F. & Bizari, D. Alginate-bioactive glass containing Zn and Mg composite scaffolds for bone tissue engineering. Int. J. Biol. Macromol.137, 1256–1267 (2019). [DOI] [PubMed] [Google Scholar]
- 27.Sepahi, S., Kalaee, M., Mazinani, S., Abdouss, M. & Hosseini, S. M. Introducing electrospun polylactic acid incorporating etched halloysite nanotubes as a new nanofibrous web for controlled release of Amoxicillin. J. Nanostruct. Chem.11(2), 245–258 (2021). [Google Scholar]
- 28.Bou Assaf, R. et al. Evaluation of the osteogenic potential of different scaffolds embedded with human stem cells originated from Schneiderian membrane: An in vitro study. Biomed. Res. Int.2019, 1–10 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mosaddad, S. A. et al. Fabrication and properties of developed collagen/strontium-doped Bioglass scaffolds for bone tissue engineering. J. Market. Res.9(6), 14799–14817 (2020). [Google Scholar]
- 30.Zare, E. N. et al. Nonspherical metal-based nanoarchitectures: Synthesis and impact of size, shape, and composition on their biological activity. Small17(17), 2007073 (2021). [DOI] [PubMed] [Google Scholar]
- 31.Panda, J. J., Dua, R., Mishra, A., Mittra, B. & Chauhan, V. S. 3D cell growth and proliferation on a RGD functionalized nanofibrillar hydrogel based on a conformationally restricted residue containing dipeptide. ACS Appl. Mater. Interfaces.2(10), 2839–2848 (2010). [DOI] [PubMed] [Google Scholar]
- 32.Fissan, H., Ristig, S., Kaminski, H., Asbach, C. & Epple, M. Comparison of different characterization methods for nanoparticle dispersions before and after aerosolization. Anal. Methods6(18), 7324–7334 (2014). [Google Scholar]
- 33.Doostmohammadi, A. et al. Bioactive glass nanoparticles with negative zeta potential. Ceram. Int.37(7), 2311–2316 (2011). [Google Scholar]
- 34.Durgalakshmi, D. et al. Highly reactive crystalline-phase-embedded strontium-bioactive nanorods for multimodal bioactive applications. Biomater. Sci.6(7), 1764–1776 (2018). [DOI] [PubMed] [Google Scholar]
- 35.Fujikura, K. et al. Influence of strontium substitution on structure and crystallisation of Bioglass® 45S5. J. Mater. Chem.22(15), 7395–7402 (2012). [Google Scholar]
- 36.Chen, Q. Z. Boccaccini, 45S5 bioglass®-derived glass–ceramic scaffolds for bone tissue engineering. Biomaterials27, 2414–2425 (2006). [DOI] [PubMed] [Google Scholar]
- 37.Soni, R., Kumar, N. V., Chameettachal, S., Pati, F. & Rath, S. N. Synthesis and optimization of PCL-bioactive glass composite scaffold for bone tissue engineering. Mater. Today Proc.15, 294–299 (2019). [Google Scholar]
- 38.Kargozar, S. et al. Osteogenic potential of magnesium (Mg)-doped multicomponent bioactive glass: in vitro and in vivo animal studies. Materials.15(1), 318 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kermani, F. et al. Strontium-and cobalt-doped multicomponent mesoporous bioactive glasses (MBGS) for potential use in bone tissue engineering applications. Materials.13(6), 1348 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soleymani, E., Karbasi, S. & Monshi, A. Evaluation of the effects of nano-TiO2 on physical and mechanical properties of nano-bioglass 45S5 scaffold for bone tissue engineering. Sci. Iran.22(3), 1337–1345 (2015). [Google Scholar]
- 41.Goudarzi, Z., Parvin, N. & Sharifianjazi, F. Formation of hydroxyapatite on surface of SiO2–P2O5–CaO–SrO–ZnO bioactive glass synthesized through sol-gel route. Ceram. Int.45(15), 19323–19330 (2019). [Google Scholar]
- 42.Guo, S. et al. Parallel control over surface charge and wettability using polyelectrolyte architecture: Effect on protein adsorption and cell adhesion. ACS Appl. Mater. Interfaces.8(44), 30552–30563 (2016). [DOI] [PubMed] [Google Scholar]
- 43.Terada, A., Okuyama, K., Nishikawa, M., Tsuneda, S. & Hosomi, M. The effect of surface charge property on Escherichia coli initial adhesion and subsequent biofilm formation. Biotechnol. Bioeng.109(7), 1745–1754 (2012). [DOI] [PubMed] [Google Scholar]
- 44.Cai, S. et al. Recent advance in surface modification for regulating cell adhesion and behaviors. Nanotechnol. Rev.9(1), 971–989 (2020). [Google Scholar]
- 45.Mneimne, M., Hill, R. G., Bushby, A. J. & Brauer, D. S. High phosphate content significantly increases apatite formation of fluoride-containing bioactive glasses. Acta Biomater.7(4), 1827–1834 (2011). [DOI] [PubMed] [Google Scholar]
- 46.Abbasi, N., Hamlet, S., Love, R. M. & Nguyen, N. T. Porous scaffolds for bone regeneration. J. Sci. Adv. Mater. Dev.5(1), 1–9 (2020). [Google Scholar]
- 47.Thavornyutikarn, B., Chantarapanich, N., Sitthiseripratip, K., Thouas, G. A. & Chen, Q. Bone tissue engineering scaffolding: Computer-aided scaffolding techniques. Prog. Biomater.3(2–4), 61–102 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sengers, B. G., Please, C. P., Taylor, M. & Oreffo, R. O. C. Experimental–computational evaluation of human bone marrow stromal cell spreading on trabecular bone structures. Ann. Biomed. Eng.37(6), 1165–1176 (2009). [DOI] [PubMed] [Google Scholar]
- 49.Kramschuster, A. & Turng, L. S. Fabrication of Tissue Engineering Scaffolds: Handbook of Biopolymers and Biodegradable Plastics Vol. 427 (William Andrew, 2013). [Google Scholar]
- 50.Shiraishi, N. et al. Preparation and characterization of porous alginate scaffolds containing various amounts of octacalcium phosphate (OCP) crystals. J. Mater. Sci. Mater. Med.21(3), 907–914 (2010). [DOI] [PubMed] [Google Scholar]
- 51.Bonjour, J. P. Calcium and phosphate: A duet of ions playing for bone health. J. Am. Coll. Nutr.30(sup5), 438S-448S (2011). [DOI] [PubMed] [Google Scholar]
- 52.Sanz-Herrera, J. A. & Boccaccini, A. R. Modelling bioactivity and degradation of bioactive glass based tissue engineering scaffolds. Int. J. Solids Struct.48(2), 257–268 (2011). [Google Scholar]
- 53.Bingel, L., Groh, D., Karpukhina, N. & Brauer, D. S. Influence of dissolution medium pH on ion release and apatite formation of Bioglass® 45S5. Mater. Lett.143, 279–282 (2015). [Google Scholar]
- 54.Blochberger, M., Hupa, L. & Brauer, D. S. Influence of zinc and magnesium substitution on ion release from Bioglass 45S5 at physiological and acidic pH. Biomed. Glass.1, 1 (2015). [Google Scholar]
- 55.Shah, F. A., Brauer, D. S., Desai, N., Hill, R. G. & Hing, K. A. Fluoride-containing bioactive glasses and Bioglass® 45S5 form apatite in low pH cell culture medium. Mater. Lett.119, 96–99 (2014). [Google Scholar]
- 56.Liu, M., Dai, L., Shi, H., Xiong, S. & Zhou, C. In vitro evaluation of alginate/halloysite nanotube composite scaffolds for tissue engineering. Mater. Sci. Eng. C49, 700–712 (2015). [DOI] [PubMed] [Google Scholar]
- 57.Yan, J. et al. Injectable alginate/hydroxyapatite gel scaffold combined with gelatin microspheres for drug delivery and bone tissue engineering. Mater. Sci. Eng. C63, 274–284 (2016). [DOI] [PubMed] [Google Scholar]
- 58.Kulig, D., Zimoch-Korzycka, A., Jarmoluk, A. & Marycz, K. Study on alginate–chitosan complex formed with different polymers ratio. Polymers8(5), 167 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mesgar, A. S., Mohammadi, Z. & Rasouli-Disfani, F. Bioactive monetite-containing whisker-like fibers reinforced chitosan scaffolds. J. Am. Ceram. Soc.100(10), 4719–4733 (2017). [Google Scholar]
- 60.Milojević, M. et al. Hybrid 3D printing of advanced hydrogel-based wound dressings with tailorable properties. Pharmaceutics.13(4), 564 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Clyne, T. W. & Hull, D. An Introduction to Composite Materials (Cambridge University Press, 2019). [Google Scholar]
- 62.Sergi, R., Bellucci, D., Salvatori, R., Anesi, A. & Cannillo, V. A novel bioactive glass containing therapeutic ions with enhanced biocompatibility. Materials.13(20), 4600 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Said, H. A. et al. Mechanical behavior of hydroxyapatite-chitosan composite: Effect of processing parameters. Minerals.11(2), 213 (2021). [Google Scholar]
- 64.Zhang, W. et al. Effects of strontium in modified biomaterials. Acta Biomater.7(2), 800–808 (2011). [DOI] [PubMed] [Google Scholar]
- 65.Baheiraei, N., Eyni, H., Bakhshi, B., Najafloo, R. & Rabiee, N. Effects of strontium ions with potential antibacterial activity on in vivo bone regeneration. Sci. Rep.11(1), 1–9 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Coraça-Huber, D. C., Fille, M., Hausdorfer, J., Putzer, D. & Nogler, M. Efficacy of antibacterial bioactive glass S53P4 against S. aureus biofilms grown on titanium discs in vitro. J. Orthop. Res.32(1), 175–177 (2014). [DOI] [PubMed] [Google Scholar]
- 67.Moghanian, A., Firoozi, S. & Tahriri, M. Characterization, in vitro bioactivity and biological studies of sol-gel synthesized SrO substituted 58S bioactive glass. Ceram. Int.43(17), 14880–14890 (2017). [Google Scholar]
- 68.Islamipour, Z., Zare, E. N., Salimi, F., Ghomi, M. & Makvandi, P. Biodegradable antibacterial and antioxidant nanocomposite films based on dextrin for bioactive food packaging. J. Nanostruct. Chem.2022, 1–16 (2022). [Google Scholar]
- 69.Asadpoor, M. et al. Antimicrobial activities of alginate and chitosan oligosaccharides against Staphylococcus aureus and Group B Streptococcus. Front. Microbiol.2021, 12 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shoaib, M. et al. Magnesium doped mesoporous bioactive glass nanoparticles: A promising material for apatite formation and mitomycin c delivery to the MG-63 cancer cells. J. Alloy. Compd.866, 159013 (2021). [Google Scholar]
- 71.Zheng, K. et al. ZnO quantum dots modified bioactive glass nanoparticles with pH-sensitive release of Zn ions, fluorescence, antibacterial and osteogenic properties. J. Mater. Chem. B.4(48), 7936–7949 (2016). [DOI] [PubMed] [Google Scholar]
- 72.Rismanchian, M., Khodaeian, N., Bahramian, L., Fathi, M. & Sadeghi-Aliabadi, H. In-vitro comparison of cytotoxicity of two bioactive glasses in micropowder and nanopowder forms. Iran. J. Pharm. Res. IJPR.12(3), 437 (2013). [PMC free article] [PubMed] [Google Scholar]
- 73.Amudha, S. et al. Enhanced mechanical and biocompatible properties of strontium ions doped mesoporous bioactive glass. Compos. B Eng.196, 108099 (2020). [Google Scholar]
- 74.Zhu, Y., Zhu, M., He, X., Zhang, J. & Tao, C. Substitutions of strontium in mesoporous calcium silicate and their physicochemical and biological properties. Acta Biomater.9(5), 6723–6731 (2013). [DOI] [PubMed] [Google Scholar]
- 75.Isaac, J. et al. Effects of strontium-doped bioactive glass on the differentiation of cultured osteogenic cells. Eur. Cell. Mater.21(130), e43 (2011). [DOI] [PubMed] [Google Scholar]
- 76.Zhao, R. et al. Evaluation of bioactive glass scaffolds incorporating SrO or ZnO for bone repair: In vitro bioactivity and antibacterial activity. J. Appl. Biomater. Funct. Mater.19, 22808000211040910 (2021). [DOI] [PubMed] [Google Scholar]
- 77.Niknam, Z. et al. Osteogenic differentiation potential of adipose-derived mesenchymal stem cells cultured on magnesium oxide/polycaprolactone nanofibrous scaffolds for improving bone tissue reconstruction. Adv. Pharm. Bull.12(1), 142–154 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jell, G. et al. Bioactive glass-induced osteoblast differentiation: A noninvasive spectroscopic study. J. Biomed. Mater. Res. A86(1), 31–40 (2008). [DOI] [PubMed] [Google Scholar]
- 79.Santocildes-Romero, M. E. et al. The osteogenic response of mesenchymal stromal cells to strontium-substituted bioactive glasses. J. Tissue Eng. Regen. Med.9(5), 619–631 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Schmitz, S. I. et al. Superior biocompatibility and comparable osteoinductive properties: Sodium-reduced fluoride-containing bioactive glass belonging to the CaO–MgO–SiO2 system as a promising alternative to 45S5 bioactive glass. Bioact. Mater.5(1), 55–65 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sharifi, E. et al. Mesoporous bioactive glasses in cancer diagnosis and therapy: Stimuli-responsive, toxicity, immunogenicity, and clinical translation. Adv. Sci.2021, 2102678 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ojansivu, M. et al. Bioactive glass induced osteogenic differentiation of human adipose stem cells is dependent on cell attachment mechanism and mitogen-activated protein kinases. (2018). [DOI] [PubMed]
- 83.Baier, M. et al. Strontium enhances osseointegration of calcium phosphate cement: A histomorphometric pilot study in ovariectomized rats. J. Orthop. Surg. Res.8(1), 1–8 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jiménez-Holguín, J. et al. Strontium-modified scaffolds based on mesoporous bioactive glasses/polyvinyl alcohol composites for bone regeneration. Materials.13(23), 5526 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zhao, S. et al. Three-dimensional printed strontium-containing mesoporous bioactive glass scaffolds for repairing rat critical-sized calvarial defects. Acta Biomater.12, 270–280 (2015). [DOI] [PubMed] [Google Scholar]
- 86.Wilkesmann, S., Westhauser, F. & Fellenberg, J. Combined fluorescence-based in vitro assay for the simultaneous detection of cell viability and alkaline phosphatase activity during osteogenic differentiation of osteoblast precursor cells. Methods Protoc.3(2), 30 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seyedjafari, E., Soleimani, M., Ghaemi, N. & Sarbolouki, M. N. Enhanced osteogenic differentiation of cord blood-derived unrestricted somatic stem cells on electrospun nanofibers. J. Mater. Sci. Mater. Med.22(1), 165–174 (2011). [DOI] [PubMed] [Google Scholar]
- 88.Wrobel, E., Leszczynska, J. & Brzoska, E. The characteristics of human bone-derived cells (HBDCS) during osteogenesis in vitro. Cell Mol Biol Lett.21(1), 1–15 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ahmadi, M. et al. Osteogenic differentiation of mesenchymal stem cells cultured on PLLA scaffold coated with Wharton’s Jelly. EXCLI J.16, 785 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Nguyen, L. T. H., Liao, S., Chan, C. K. & Ramakrishna, S. Electrospun poly (L-lactic acid) nanofibres loaded with dexamethasone to induce osteogenic differentiation of human mesenchymal stem cells. J. Biomater. Sci. Polym. Ed.23(14), 1771–1791 (2012). [DOI] [PubMed] [Google Scholar]
- 91.Nanda, H. S. et al. Collagen microgel-assisted dexamethasone release from PLLA-collagen hybrid scaffolds of controlled pore structure for osteogenic differentiation of mesenchymal stem cells. J. Biomater. Sci. Polym. Ed.25(13), 1374–1386 (2014). [DOI] [PubMed] [Google Scholar]
- 92.Rozila, I. et al. Polycaprolactone-based scaffolds facilitates osteogenic differentiation of human adipose-derived stem cells in a co-culture system. Polymers13(4), 597 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chuenjitkuntaworn, B., Osathanon, T., Nowwarote, N., Supaphol, P. & Pavasant, P. The efficacy of polycaprolactone/hydroxyapatite scaffold in combination with mesenchymal stem cells for bone tissue engineering. J. Biomed. Mater. Res. A104(1), 264–271 (2016). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on reasonable request from the corresponding author.