Abstract
We explored experiences with telemedicine among persons with HIV (PWH) during the first wave of the coronavirus disease 2019 (COVID-19) pandemic. A convenience sample of adults (>18 years) receiving care in an urban clinic in Atlanta were invited to participate. Patients completed a structured survey that assessed the usefulness, quality, satisfaction, and concerns with telemedicine services (telephone calls) received during the first wave of the COVID-19 pandemic (March–May 2020). Demographic, plasma HIV-1 RNA, and CD4+ T cell count data were obtained through medical chart abstraction. Bootstrapped t-tests and chi-square tests were used to examine differences in patient experiences by age, sex, and race. Of 406 PWH contacted, 101 completed the survey (median age 55 years, 84% men, 77% Black, 98% virally suppressed, median CD4 count 572 cells/μL). The main HIV care disruptions experienced were delays in follow-up visits (40%), difficulty getting viral load measured (35%), and difficulty accessing antiretroviral therapy (21%). Participant ratings for quality (median score 6.5/7), usefulness (median score 6.0/7), and satisfaction (median score 6.3/7) with telemedicine were high. However, 28% of patients expressed concerns about providers' ability to examine them and about the lack of laboratory tests. More women had concerns about providers' ability to examine them (92% vs. 50%, p = .005) and about the safety of their personal information (69% vs. 23%, p = .002) compared with men. No age or race differences were observed. Although PWH are generally satisfied with telephone-based telemedicine, concerns with its use were notable, particularly among women. Future HIV telemedicine models should address these.
Keywords: quality improvement, health services research, telehealth, implementation
Introduction
Mitigation efforts against the propagation of coronavirus disease 2019 (COVID-19) forced an abrupt transition to telemedicine for HIV care delivery. Synchronous telemedicine was adopted across the United Kingdom with unprecedented speed and even became a reimbursable service, including through Medicaid and Medicare.1 This rapid transition was supported by pre-pandemic evidence showing telemedicine improves clinical outcomes in the general population and may even reduce health care costs.2 Among the HIV population, studies show telemedicine can improve viral suppression.3 The COVID-19 pandemic forced an abrupt telemedicine rollout for HIV care, and the best way to serve patients through telemedicine remains to be determined.4
Telemedicine is the practice of medicine using technology to deliver care at a distance.5 To determine if telemedicine-based HIV care is effective and equitable, it is important to explore patient experiences and satisfaction with these services.6 Furthermore, disparities in access to telemedicine should be identified and addressed as vulnerable patients may be experiencing these.7,8 Finally, patient acceptability, satisfaction, and concerns with telemedicine need to be explored, as these factors may impact its uptake, as well as retention in HIV care and rates of virologic suppression.9,10 For persons living with multiple comorbidities, disease control, and overall quality of life11 may also be negatively affected by the abrupt transition to telemedicine.
Exploring these issues is particularly important in metropolitan Atlanta, an area with high HIV incidence in the United States and where persons with HIV (PWH) experience numerous structural barriers to accessing care. Thus, we sought to explore patient experiences with telephone-based telemedicine during the first wave of the COVID-19 pandemic (March–May 2020) in the Southern United States. The information gathered in this study can help improve telemedicine services to more effectively reach and care for PWH.
Methods
This study was conducted at an urban, Ryan White-funded HIV clinic in Atlanta, Georgia, that serves over 6000 un/underinsured PWH. This study was conducted during the implementation of a telemedicine program to maintain access to care for PWH during the first wave of COVID-19 in the United States (March–May 2020). In addition to transitioning clinical care to telemedicine, there was also a clinic-wide effort to minimize in-person contact for several services such as pharmacy and social work/financial counseling. As part of this effort, the clinic scaled-up mail-order pharmacy services, paperwork, and laboratory requirements to remain enrolled in Ryan White/AIDS Drug Assistance Program were waived, and virtual avenues were created to submit paperwork for financial and social services.
During the spring of 2020, Atlanta had a shelter-in-place order for all residents for 1 month (March–April), followed by more limited shelter-in-place orders for those considered to be at high risk for severe COVID-19. During the week of March 9, 2020, clinicians shifted to informal telephone check-ins with patients who missed visits or were unable to attend their clinic visit. On March 16, 2020, formal telephone virtual visits were launched. Telephone visits were directed to patients who were virally suppressed and clinically stable, whereas in-person care remained available for patients who did not have access to telecommunication, were not virally suppressed, and/or had other urgent health needs. HIV clinicians contacted their patients to discuss having their visit shifted to a telephone visit versus remaining in-person, based on clinical stability.
In the context of this study, telemedicine refers to clinical visits conducted by telephone (without video) between the patient and HIV primary care provider. Through purposive sampling, 406 patients older than 18 years who received care between March and May 2020 through telemedicine were identified and invited to participate in the study. Contacted patients were selected purposively to mirror the age, race, and sex distributions of the overall patient population using telemedicine.
Because telephone visits were offered to patients who were virally suppressed, our sample included mostly well controlled, clinically stable patients. The March–May timeframe was selected to capture the most intensive months of telemedicine use and to explore 6-month post-telemedicine visit retention and viral load (VL) data. The survey was conducted between June and August 2020. The Emory University Institutional Review Board reviewed the study protocol and determined this was a quality improvement effort.
Patients who agreed to participate were asked to complete a structured survey by telephone or online (based on their preference). The survey was available in English and Spanish. In line with recommended methods in telemedicine research,12 the survey assessed the usability of telemedicine and concerns using two scales. The Telemedicine Usability Questionnaire assessed the usefulness, quality of clinician/patient interaction, and satisfaction with the telemedicine visit as rated by patients.13
Items are rated on a seven-point Likert scale, with answers ranging from 1 = disagree to 7 = agree, where the higher the rating the more favorable the assessment. The second scale assessed patient concerns with telemedicine14; the scale contains four items rated on a five-point scale ranging from 1 = extremely concerned to 5 = not at all concerned, with lower ratings indicating a higher concern level. This scale evaluated concerns with clinician ability to examine patients, patient communication limitations, the security of personal health information, and usage of mobile phone data.
Patient demographic characteristics, plasma HIV-1 RNA VL, and CD4+ T cell count data corresponding to March–May 2020 were obtained through electronic medical chart abstraction. Viral suppression was defined as VL <200 copies/μL. To assess retention in care, visit attendance (in-person or telephone) and VL values from June to December 2020 were also extracted from electronic medical records. The VL closest to the time of telemedicine visit and the latest VL of 2020 were extracted. Patients with ≥1 visit during June–December 2020 were considered retained in care, and patients with HIV-1 RNA <200 copies/μL were considered suppressed. For the entire clinic population, weekly number of visits by type (telephone and in-person), and proportion of suppressed VLs were extracted from the Emory Center for AIDS Research HIV Registry and plotted each week of 2020.
The study survey was built and managed using the system for Research Electronic Data Capture15 tools hosted at Emory University. Patient demographic characteristics were summarized using frequency counts and median/interquartile range (IQR). Bootstrapped Welch two-sample t-tests were performed to examine differences in mean ratings for quality, usefulness, satisfaction, and concerns with telemedicine by sex (men vs. women), age (younger than 50 vs. older than 50 years old), and race (Black/Hispanic Black vs. White/Hispanic White). Chi-square tests were used to examine differences in proportion of patients reporting concerns by age group, race, and sex (same groups as mentioned previously). Analyses were conducted in R programming language version 4.0.2.
Results
Of 406 telemedicine users contacted, 101 agreed to complete the survey. The responder sample was older (median age 55 vs. 51 years), had a higher proportion of female participants (17% vs. 9%) and a lower proportion of Hispanic participants (2% vs. 8%) than nonresponders. Among survey respondents, median age was 55 years (IQR = 10), 84% were men, and 77% were Black. Twenty-five percent had completed college and 30% were employed full time (Table 1). The first language was English for 90% of respondents, Spanish for 8%, and other for 2% (German, Creole, and Somalian). The survey was available in Spanish for those who preferred that option.
Table 1.
Descriptive Patient Characteristics. Data Are Presented as Median (Interquartile Range) or Proportion
| Variable | All (N = 101) |
|---|---|
| Age (years) | 55 (10) |
| Male sex (at birth) | 84% |
| Race | |
| African American | 78% |
| White | 17% |
| Hispanic | 5% |
| Education | |
| Completed college | 25% |
| Some college | 33% |
| Completed high school | 29% |
| No high school | 9% |
| Employment status | |
| Employed (full/part time) | 47% |
| Self-employed | 7% |
| Unemployed | 12% |
| Unable to work | 21% |
| Retired | 7% |
| Income | |
| <$20,000 | 53% |
| $20,000 to $49,999 | 28% |
| ≥$50,000 | 6% |
| Health insurance | |
| Ryan White/ADAP | 61% |
| Medicare/Medicaid | 28% |
| Unsure | 10% |
| Virally suppressed | 98% |
| CD4 cell count (cells/mm3) | 572 (402) |
ADAP, AIDS Drug Assistance Program.
From March to May 2020, median CD4 cell count was 572 cells/μL (IQR = 402) and 98% were virally suppressed. The main HIV care disruptions reported during this period were delays in follow-up visits (40%), difficulty getting VL measured (35%), and difficulty accessing antiretroviral therapy (21%). Among all respondents (n = 101), 37% reported they had switched from pharmacy pick-up to mail delivery for obtaining their antiretroviral medications.
The median number of telemedicine visits per patient was 1 (IQR = 1.0), and each visit had an average duration of 15 min (IQR = 14.3). Patient ratings for the quality (median score 6.5/7), usefulness (median score 6.0/7), and satisfaction (median score 6.3/7) with telemedicine were high overall (Table 2). Patients had no major concerns with the use of telemedicine in general (median score 4.3/5, where 5 = not at all concerned). However, when asked about specific concerns, 28% of patients reported their main concerns were not being able to examine them well, and the lack of laboratory work/clinical tests. Women expressed greater concern about telemedicine use than men (mean 3.3 vs. 4.2; 95% confidence interval, −1.26 to −0.44; p = .0006).
Table 2.
Telemedicine Measures by Sex. Data Are Presented as Median (Interquartile Range)
| All (N = 101) | Men (n = 85) | Women (n = 16) | |
|---|---|---|---|
| Usefulness scale scorea | 6.0 (1.7) | 6.0 (1.7) | 5.7 (2.0) |
| Telehealth improves my access to health care services | 5.0 (3.0) | 5.0 (3.0) | 5.0 (3.0) |
| Telehealth saves me time traveling to a hospital/clinic | 7.0 (1.0) | 7.0 (1.0) | 7.0 (1.0) |
| Telehealth provides for my health care needs | 6.0 (3.0) | 6.0 (3.0) | 6.0 (2.0) |
| Quality scale scorea | 6.5 (1.5) | 6.5 (1.5) | 6.5 (0.8) |
| I could easily talk to my provider using telehealth | 7.0 (2.0) | 7.0 (2.0) | 7.0 (2.0) |
| I could hear my provider clearly using telehealth | 7.0 (0.3) | 7.0 (0.5) | 7.0 (0.0) |
| I felt I was able to express myself effectively | 7.0 (1.0) | 7.0 (1.0) | 7.0 (1.0) |
| I can hear my provider as well as if we met in person | 7.0 (2.0) | 7.0 (2.0) | 6.0 (2.0) |
| Satisfaction scale scorea | 6.3 (2.0) | 6.0 (2.0) | 6.3 (1.0) |
| I feel comfortable communicating with my provider using telehealth | 7.0 (1.0) | 7.0 (1.0) | 7.0 (1.0) |
| Telehealth is an acceptable way to receive health care services | 6.0 (3.0) | 6.0 (3.0) | 6.0 (2.0) |
| I would use telehealth services again | 7.0 (1.0) | 7.0 (1.5) | 7.0 (0.0) |
| Overall, I am satisfied with this telehealth system | 7.0 (2.0) | 6.5 (2.0) | 7.0 (2.0) |
| Concerns scale scoreb | 4.3 (1.3) | 4.5 (1.5) | 3.5 (0.5)c |
| My doctor is not able to examine me well | 3.0 (3.0) | 3.5 (3.0) | 2.0 (2.0) |
| My personal information is not safe | 5.0 (2.0) | 5.0 (1.0) | 3.0 (2.0) |
| I am not able to express myself very well | 5.0 (1.0) | 5.0 (0.0) | 4.0 (2.0) |
| I use too much data on my phone service or internet | 5.0 (0.0) | 5.0 (0.0) | 5.0 (0.0) |
Bold values indicate the overall scores from each of the domains: usefulness, quality, satisfaction, and concerns.
Measured on a scale form 1 = strongly disagree to 7 = strongly agree. Higher scores reflect more favorable ratings.
Measured on a scale form 1 = extremely concerned to 5 = not at all concerned. Lower scores reflect higher concerns.
Mean significantly higher in women than men in bootstrapped Welch t-test (3.3 vs. 4.2, 95% CI, −1.26 to −0.44, p = .0006).
CI, confidence interval.
Specifically, more women than men had concerns about providers' ability to examine them well (92% vs. 50%, p = .005), and about the safety of their personal information (69% vs. 23%, p = .001). There were no significant age or race differences observed in any telemedicine-related measures. Finally, nine patients reported they anticipate barriers to continued use of telemedicine for their HIV care. The main barriers identified were poor telephone service/connectivity, the cost of telephone/WiFi services, difficulty expressing themselves/communicating with their provider, and problems with the device being used.
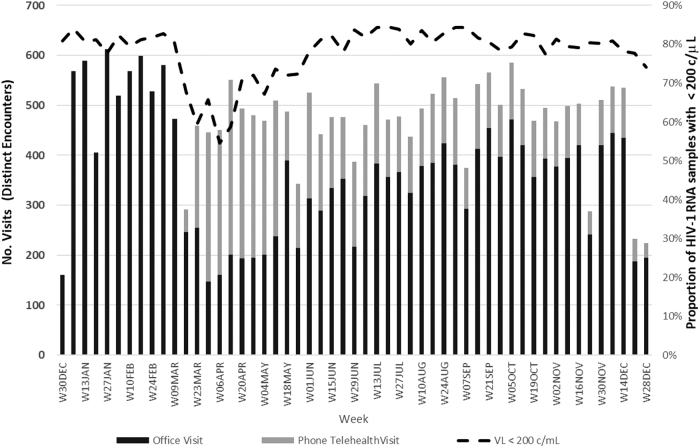
Figure 1 provides the distribution of telephone-based and office-based visits along with proportion of suppressed VLs over the course of 2020. Telephone-based visits comprised more than half of the visits from March 30 to May 17 with closer to two thirds of visits during March 30 to April 12. The median difference in days between the survey completion date and the last VL available was 26 days (Q1 = 25, Q3 = 79). The proportion of undetectable VLs dropped dramatically at the time when telephone-based visits peaked likely reflecting a purposeful effort to minimize in-person well visits.
FIG. 1.
Type of clinical encounters and proportion of HIV-1 RNA samples with virologic suppression throughout 2020.
From June to December 2020, the clinic largely returned to in-person visits (Fig. 1). Of patients who had a telephone visit between March and May 2020, 78% had an in-person visit, 7% had a telephone visit, and 15% had no visit from June to December 2020. Among those with in-person visits, 90% were virally suppressed and 10% did not have a laboratory value. Finally, of the 15 patients with no visits from June to December 2020, 12 remained in care (based on visit rescheduling or laboratory values available) and three were lost to follow-up.
Discussion
This study examined patient experiences receiving telephone-based telemedicine HIV care services, during the first wave of the COVID-19 pandemic in the Southern United States (March–May 2020). PWH included in this study were generally satisfied with the telemedicine services they received, although some participants had concerns regarding its use. Specifically, patients expressed concerns around the ability to ensure physical examinations, laboratory work, and data privacy/safety.
More women expressed concerns with telemedicine use than men, which suggest addressing concerns about telemedicine use may require different approaches for men and women. Although our findings may not be generalizable to other telemedicine platforms or ethnic groups, they support additional study of telemedicine use among PWH to inform strategies for telemedicine model development and implementation in HIV care beyond the pandemic.
As reported in a recent study from Atlanta,16 we found PWH in this study experienced care disruptions during the first COVID-19 wave, namely difficulty getting VL measured and accessing antiretroviral therapy. However, such disruptions did not appear to have a negative impact on HIV control as the proportion of patients virally suppressed was maintained at 96% from March–May 2020 to June–December 2020. This may be a result of the rapid transition to telemedicine enacted by the clinic, ensuring patients did not miss scheduled appointments.
Using telephone-based care provided a mechanism to maintain clinical visits with patients during a time when in-person care was forced to decrease. However, patients with advanced HIV/AIDS or clinical instability in March–May 2020 were still encouraged to be seen in-person. A similar approach was also implemented by an AIDS service organization in Birmingham, Alabama, where essential in-person services were continued for the highest needs PWH and telemedicine services were offered for less critical, ongoing care.17
In line with findings from a study exploring attitudes toward telemedicine use among PWH,14 we found telemedicine was generally well-accepted by patients, although they noted some concerns with its use. Specifically, patients expressed concerns about ensuring physical examinations, lack of laboratory work, and data privacy/safety. These concerns are related to limiting or eliminating in-person clinic visits during the COVID-19 pandemic, which has been previously identified as a main disruption to HIV care.16 Although clinicians made informed decisions about keeping patients out of clinic owing to their clinical stability, patients perceived the lack of physical examination or lack of laboratory work as negative or suboptimal care.
This may reflect a need to better communicate with patients the intent of telemedicine visits and directly address the lack of physical examination/laboratory work while providing reassurance that a temporary gap in those services should not be a detriment to one's health. Furthermore, the use of video-based telehealth can overcome some of the barriers to physical examination that a telephone visit creates.
This is the first study to find sex differences in concerns with telemedicine use among HIV patients. We found more women expressed concerns with providers' ability to examine them, and with the safety of their personal information. This aligns with findings from a study among students in a U.S. public university, where women were found to have more concerns about data privacy than men.18 Another study among 148,402 U.S. adults conducted during the early phase of the COVID-19 pandemic found women were less likely than men to use video for their telemedicine visits,8 but specific concerns were not explored.
Patient concerns about data privacy and quality of care are prominent in telemedicine and will require strategies to address them as this model keeps expanding beyond COVID-19.19 In the setting of HIV care, addressing patient telemedicine concerns is crucial because patients who express concerns are less likely to use telemedicine in the future.14 Strategies to address concerns with telemedicine are required to promote retention in care and this will likely require different approaches for men and women.
Our findings should be interpreted with consideration of the following limitations. The data are self-reported and thus prone to social desirability and recall bias. The patient sample was selected purposively to resemble the characteristics of the overall clinic population but does not ensure representativeness. Because we aimed to mirror the sex distribution of the clinic population, the number of women included in the study was small and sex differences should be interpreted with caution. The fact that we did not find age or race differences in any telemedicine measure may be owing to the unequal sample sizes we had for each age and race group; however, this can also be explained by the fact that we examined telephone visits as opposed to other telemedicine platforms that require certain technology, equipment, and literacy.
Because >98% of the telehealth visits during the study period were telephone visits, we did not explore video visits. Because of both implementation challenges and patient preference, telephone visits predominated and we hope this study provides a comparison point for future studies on the acceptability of video visits among similar low-income patient populations. Finally, telemedicine visits were offered to patients who were virally suppressed, whereas those not suppressed were encouraged to continue with in-person visits; hence, whether telemedicine services are acceptable and useful to PWH who experience barriers to achieving HIV control remains unknown.
Conclusion
The COVID-19 pandemic has pushed HIV care organizations to abruptly implement telemedicine approaches (video and telephone calls) to continue health care delivery. Our data and previous studies offer numerous lessons to inform the continued and future use of telemedicine in HIV care.
First, video communication should be used whenever possible, as this has been associated with greater patient understanding and satisfaction compared with telephone communication.20 Provider education and training on optimal communication through telemedicine can also be considered to enhance patient trust and connection.6 Related to this is clearly communicating the timeline and goals of telemedicine visits, including patient assurance that telemedicine is a temporary/complementary tool that does not replace their in-person care.
Second, disparities in access to, and benefit from, telemedicine should be addressed.21 Telemedicine models should be designed to address the digital barriers found in rural populations, older adults, racial/ethnic minority populations, and those with low socioeconomic status, limited health literacy, and limited English proficiency22,23 at the outset. Finally, hybrid models (telemedicine and in-person visits) that adapt to patient needs and preferences (or public health circumstances) are likely necessary to improve overarching access to HIV care.
Such a model has already been proposed where certain procedures that require a physical appointment (e.g., drawing blood) are carried out in person, whereas assessments that do not require in-person interaction (e.g., self-reported medication use) can be carried out using telemedicine.21 Although the best way to implement telemedicine for PWH is yet to be identified,4 these data suggest telemedicine as a feasible, complementary tool to grow and expand current HIV service delivery that may be tailored to PWH who may benefit most from this innovative and adaptable method of HIV care.
Authors' Contributions
K.I.G. and J.A.C. designed the study, conducted statistical analyses, provided interpretation of study findings, and drafted the article. M.G., B.S., J.S., and J.R. conducted the data collection/medical chart abstraction, contributed to interpretation of findings, critically revised the article and approved submission. N.S.S., L.F.C., C.D.L., C.A.M., V.C.M., M.L.N., V.D.C., and W.S.A. provided guidance for study design and statistical analyses, contributed to interpretation of findings, critically revised the article and approved submission.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
K.I.G. is supported by the National Heart, Lung and Blood Institute (1K01HL149479-01). C.D.L. is supported by the National Institute of Allergy and Infectious Diseases (K23AI124913). C.A.M. is supported by the National Heart, Lung and Blood Institute (K23HL152903). This study received support from the Emory Center for AIDS Research (P30AI050409). V.C.M. has received investigator-initiated research grants (to the institution) and consultation fees from Eli Lilly, Bayer, Gilead Sciences, and ViiV.
References
- 1. Verma S: Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19. Health Affairs Blog 2020. Available at https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/, accessed March 8, 2021.
- 2. Agency for Healthcare Research and Quality, Effective Health Care Program: Telehealth for acute and chronic care consultations. Available at https://effectivehealthcare.ahrq.gov/topics/telehealth-acute-chronic/research (2019), accessed March 8, 2021. [PubMed]
- 3. Ohl ME, Richardson K, Rodriguez-Barradas MC, et al. : Impact of availability of telehealth programs on documented HIV viral suppression: A Cluster-Randomized Program Evaluation in the Veterans Health Administration. Open Forum Infect Dis 2019;6:ofz206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Armstrong WS, Agwu AL, Barrette EP, et al. : Innovations in HIV care delivery during the COVID-19 pandemic: Policies to strengthen the Ending the Epidemic Initiative—A Policy Paper of the Infectious Diseases Society of America and the HIV Medicine Association. Clin Infect Dis 2021;72:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American Academy of Family Physicians: Telehealth and Telemedicine: Available at https://www.aafp.org/about/policies/all/telehealth-telemedicine.html accessed March 8, 2021.
- 6. Mgbako O, Miller EH, Santoro AF, et al. : COVID-19, telemedicine, and patient empowerment in HIV care and research. AIDS Behav 2020;24:1990–1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nouri S, Khoong EC, Lyles CR, Karliner L: Addressing equity in telemedicine for chronic disease management during the Covid-19 pandemic. NEJM Catalyst 2020. Available at https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0123, accessed March 8, 2021.
- 8. Eberly LA, Kallan MJ, Julien HM, et al. : Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dang BN, Westbrook RA, Black WC, Rodriguez-Barradas MC, Giordano TP: Examining the link between patient satisfaction and adherence to HIV care: A structural equation model. PLoS One 2013;8:e54729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bulsara SM, Wainberg ML, Newton-John TRO: Predictors of adult retention in HIV care: A systematic review. AIDS Behav 2018;22:752–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lazarus JV, Safreed-Harmon K, Barton SE, et al. : Beyond viral suppression of HIV—The new quality of life frontier. BMC Med 2016;14:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Langbecker D, Caffery LJ, Gillespie N, Smith AC: Using survey methods in telehealth research: A practical guide. J Telemed Telecare 2017;23:770–779. [DOI] [PubMed] [Google Scholar]
- 13. Parmanto B, Lewis AN Jr., Graham KM, Bertolet MH: Development of the Telehealth Usability Questionnaire (TUQ). Int J Telerehabil 2016;8:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dandachi D, Dang BN, Lucari B, Teti M, Giordano TP: Exploring the attitude of patients with HIV about using telehealth for HIV care. AIDS Patient Care STDS 2020;34:166–172. [DOI] [PubMed] [Google Scholar]
- 15. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG: Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kalichman SC, Eaton LA, Berman M, et al. : Intersecting pandemics: Impact of SARS-CoV-2 (COVID-19) protective behaviors on people living with HIV, Atlanta, Georgia. J Acquir Immune Defic Syndr 2020;85:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kay ES, Musgrove K: From HIV to Coronavirus: AIDS service organizations adaptative responses to COVID-19, Birmingham, Alabama. AIDS Behav 2020;24:2461–2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rowan M, Dehlinger J: Observed gender differences in privacy concerns and behaviors of mobile device end users. Procedia Comput Sci 2014;37:340–347. [Google Scholar]
- 19. Raj M, DePuccio MJ, Stephenson AL, et al. : Addressing evolving patient concerns around telehealth in the COVID-19 era. Am J Manag Care 2021;27:e1–e3. [DOI] [PubMed] [Google Scholar]
- 20. Arnold M, Kerridge I: Accelerating the de-personalization of medicine: The ethical toxicities of COVID-19. J Bioeth Inq 2020;17:815–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guaraldi G, Milic J, Martinez E, et al.: HIV care models during the COVID-19 era. Clin Infect Dis 2020;ciaa1864. Published online 2020 Dec 19. [Google Scholar]
- 22. Nouri SS, Avila-Garcia P, Cemballi AG, Sarkar U, Aguilera A, Lyles CR: Assessing mobile phone digital literacy and engagement in user-centered design in a diverse, safety-net population: Mixed methods study. JMIR Mhealth Uhealth 2019;7:e14250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tsai HS, Shillair R, Cotten SR: Social support and “Playing Around”: An examination of how older adults acquire digital literacy with tablet computers. J Appl Gerontol 2017;36:29–55. [DOI] [PMC free article] [PubMed] [Google Scholar]