Abstract
Asthma is a complicated disease defined by a combination of clinical symptoms and physiological characteristics. Typically, asthma is diagnosed by the presence of episodic cough, wheezing, or dyspnea triggered by variable environmental factors (allergens and respiratory infections), and reversible airflow obstruction. To date, the majority of asthmatic patients have been adequately controlled by anti-inflammatory/bronchodilating agents, but those with severe asthma (SA) have not been sufficiently controlled by high-dose inhaled corticosteroids-long-acting beta-agonists plus additional controllers including leukotriene modifiers. Accordingly, these uncontrolled patients provoke a special issue, because they consume high healthcare resources, requiring innovative precision medicine solutions. Recently, phenotyping based on biomarkers of airway inflammation has led to elucidating the pathophysiological mechanism of SA, where emerging evidence has highlighted the significance of eosinophil or neutrophil extracellular traps contributing to the development of SA. Here, we aimed to provide current findings about extracellular traps as a novel therapeutic target for asthma to address medical unmet needs.
Keywords: asthma, eosinophil, extracellular trap, neutrophil, therapeutics, unmet needs
Introduction
Asthma is well known as a chronic airway inflammatory disease with variable airway obstruction. Currently, approximately 300 million people worldwide suffer from asthma and more than 400 million will be affected by 2025.1 In particular, the prevalence of asthma tends to increase in low- and high-income countries. Asthmatic patients have typical asthma symptoms as well as the evidence of reversible airflow obstruction evaluated by spirometry and bronchodilator test. Among them, patients with severe asthma (SA, accounting for 10% of asthmatic patients) suffer from more frequent asthma exacerbations even on maintaining high-dose inhaled corticosteroids (ICSs).2,3 Moreover, SA could affect patients throughout ages from child to adult.4 To date, many efforts to classify asthma phenotypes,5,6 identify various biomarkers,7 and develop multiple therapeutic agents8 have been made to manage SA. Nevertheless, a growing need to find a unique target for asthma treatment is increasing because some patients with SA still remains uncontrolled. Recently, circulating eosinophil extracellular traps (EETs) and neutrophil extracellular traps (NETs) have been highlighted as novel biomarkers for SA.9 Moreover, these molecules containing DNAs and granule proteins have been suggested to enhance airway inflammation related to asthma severity. Therefore, this review mainly focused on discussing future directions for new therapeutic targets by understanding pathophysiological mechanisms of SA related to extracellular trap formation.
Definition of SA
Up to now, many definitions of SA have been suggested worldwide.10,11 The European Respiratory Society (ERS)/American Thoracic Society (ATS) guidelines define SA as asthma that requires treatment with high-dose ICSs plus second controller medications and/or systemic corticosteroids to maintain asthma control or that remains uncontrolled despite the aforementioned medications (having asthma exacerbation more than 2 times per year). However, the recent Global Initiative for Asthma (GINA) guideline defines SA if asthma is uncontrolled despite adherence to maximal optimized therapy (step 4/5 treatment including medium-to-high-dose ICSs plus second controllers and/or systemic corticosteroids) and management of comorbid conditions.10,11 Based on current clinical control status and risk factors, the World Health Organization has also defined SA as uncontrolled asthma which can result in the risk of frequent severe exacerbations (or death), adverse reactions to medications, and/or chronic morbidity.12
Classification of SA
T2-High Asthma
Asthma has been described from various points of view, characterizing comorbidities, microbial composition, viral infections, and inflammatory status.13 Especially, SA can be broadly classified into 2 major phenotypes including T2-high and T2-low asthma, although it shows more diverse phenotypes with complexity. Patients with T2-high asthma show persistent blood or sputum eosinophilia even with maintaining anti-inflammatory medications (treatment-refractory).5,14 In T2-high asthma, immune cells including mast cells, basophils, T helper 2 (Th2) cells, and group 2 innate lymphoid cells (ILC2) are abundantly found in the airway mucosa, contributing to severe clinical outcomes and lower lung functions.15,16 In addition, increased levels of immunoglobulin E (IgE) and type 2 cytokines (interleukin [IL]-4, IL-5, and IL-13) are involved in type 2 airway inflammation.17 In SA, T2-high asthma has shown different features according to onset age with/without eosinophilia.18 Early-onset allergic asthma (also known as extrinsic/atopic asthma) is the most common phenotype (estimated 40% to 50% in patients with SA), in which lower lung function is associated with increased levels of transforming growth factor-beta.19,20 Late-onset eosinophilic asthma (around 20%, asthma symptoms developed in adult age) has higher blood/sputum eosinophil counts (whether allergic or non-allergic type) and is associated with a high prevalence of chronic rhinosinusitis (CRS) and nasal polyps (NPs).21 Aspirin-exacerbated respiratory disease (AERD) is a unique phenotype showing moderate-to-severe upper (CRS with/without NPs) and lower airway (asthma) symptoms. Overproduction of cysteinyl leukotrienes and prostaglandin D2, along with intense eosinophilic inflammation and mast cell activation, is the key finding of the pathogenetic mechanism of AERD.22
T2-Low Asthma and Other Phenotypes
T2-low asthma has been recognized as non-eosinophilic but neutrophilic asthma (NA) related to atypical bacterial infection, smoking experience, and obesity,23 presenting distinct clinical characteristics compared to T2-high asthma. Patients with T2-low asthma usually have more than 40–60% neutrophils in their sputum.24 The presence of airway neutrophilia has been associated with poor responses to corticosteroid treatment.24 Moreover, patients with T2-low asthma have lower levels of FeNO and total IgE as well as lower atopy rates.25 In particular, patients with occupational asthma (especially isocyanate- or grain flour-induced) are likely related to T2-low asthma.26 However, some patients with T2-high asthma have sputum neutrophilia as well as eosinophilia (mixed granulocytic asthma) and present frequent asthma exacerbations with progressive lung function decline.27,28 For instance, mounting evidence has demonstrated that obesity is involved in steroid resistance as well as in the development of asthma.29–32 Patients who suffer from obese asthma can show both eosinophilic and neutrophilic inflammation in the airways, with uncontrolled asthma symptoms.33–35 Although several mediators including tumor necrosis factor alpha, IL-6, and vascular endothelial growth factor have been suggested to reflect the pathogenic mechanism of obese asthma,36 many aspects of such a phenotype of asthma remain largely questionable. As overlapping characteristics with complexity are frequently found in patients with SA, a broader approach may be required to identify a novel target and to prevent poor asthma outcomes.
Novel Targets for SA
Eosinophil Extracellular Traps
Eosinophils are classically considered a protector against parasitic infections as well as an effector contributing to allergic diseases such as asthma, atopic dermatitis, rhinitis, and eczema. In addition, they fulfill an important immune response against bacterial and fungal infections by forming EETs.37,38 Eosinophils can release extracellular traps in response to subsequent stimuli such as IL-5, interferon gamma, C5a, eotaxin, and lipopolysaccharide (LPS).39–41 According to the current literature, EET formation is associated with the intracellular nicotinamide adenine dinucleotide phosphate (NADPH) oxidase signaling pathway, which is linked to the overproduction of reactive oxygen species.39 In addition, the terminology EETosis was coined to describe the process by which eosinophils undergo their death cell program to produce EETs without natural necrosis or apoptosis.42 The components of EETs are a web-like scaffold of chromatin filaments mixed with several granule proteins. Among various granule proteins contained in EETs, eosinophil cationic protein is capable of causing tissue damage in asthma; eosinophil peroxidase contributes to the activation of immune systems and even triggers autoimmune responses.43 However, serum eosinophil derived neurotoxin (EDN) level was significantly correlated with EET-forming eosinophil counts in patients with SA.44 Regarding the activation mechanism of persistent eosinophilia in SA, the role of EETs has been suggested to have harmful effects on upper and lower airway mucosae in patients with SA. Recent studies have demonstrated that significantly higher EET-forming eosinophil counts were noted in patients with SA than in those with non-SA, which further induced production of epithelium-derived cytokine (thymic stromal lymphopoietin [TSLP] and IL-33), leading to ILC2 and eosinophil activation followed by enhancing T2-high airway inflammation.45 Taken together, EETs from activated eosinophils are new targets for the diagnosis and treatment of SA. Further understanding about EET formation and function may lead to better diagnosis and management of SA.
Neutrophil Extracellular Traps
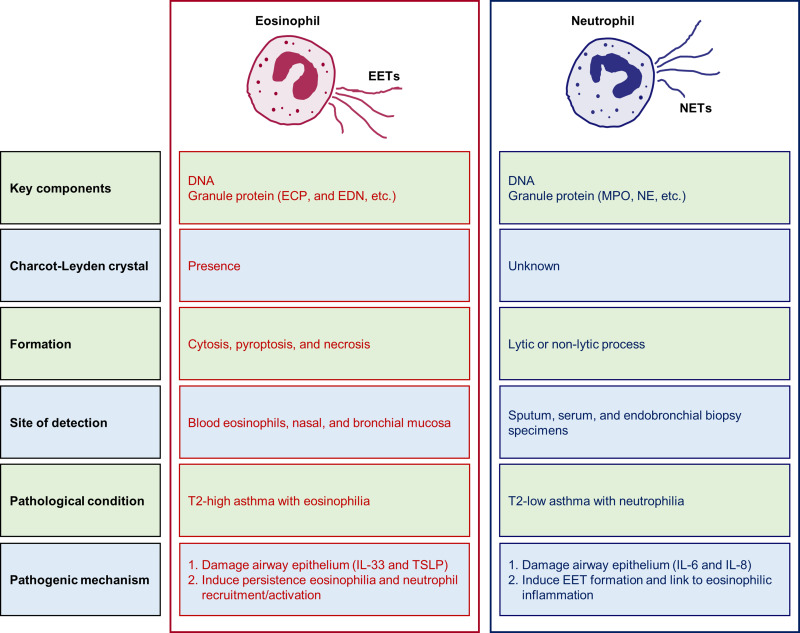
Neutrophils are first-line inflammatory cells that migrate from the circulation blood into the inflammatory area in response to various exogenous factors, where they can engulf and kill the invading bacteria.46 In response to IL-8, phorbol myristate acetate (PMA), or LPS, activated neutrophils released a web-like structure called NETs, which were made up of DNA and granule proteins.47,48 To date, three major mechanisms have been shown to induce NET formation: NADPH oxidase 2 (Nox2)-dependent pathway with PMA stimulation, Nox2-independent pathway with A23187 or ionomycin stimulation, and mitochondrial ROS-dependent pathway with LPS or complement factor C5a receptor stimulation.49 Currently, the significance of NETs is emphasized in various diseases including cardiovascular disease, metabolic diseases, certain septic conditions, autoimmune, and inflammatory diseases.50–54 In particular, NET-forming neutrophil counts were higher in patients with SA than in those with non-SA, contributing to the severity of airway inflammation by inducing eosinophil activation/degranulation as well as epithelial damage.55 The effect of NETs on inflammasome activation has been demonstrated in patients with SA.56 In addition, increased levels of extracellular DNA in sputum that negatively correlated with FEV1% was noted in NA patients with the exacerbation-susceptible phenotype.47 Moreover, our group clarified epithelial-derived molecules (S100 calcium-binding protein A9 and serum amyloid A1), which were higher in the sera of NA, could induce NETs, further increasing neutrophilic airway inflammation.57–59 Taken together, NETs are a key mediator of ongoing neutrophilic activation/degranulation, becoming an additional therapeutic target for NA. Here, different characteristics between EETs and NETs in the progression of SA are summarized in Figure 1.
Figure 1.
Comparison of characteristics between EETs and NETs in the progression of severe asthma.
Abbreviations: DNA, deoxyribonucleic acid; ECP, eosinophil cationic protein; EDN, eosinophil-derived neurotoxin; EETs, eosinophil extracellular traps; MPO, myeloperoxidase; NE, neutrophil elastase; NETs, neutrophil extracellular traps; IL, interleukin; TSLP, thymic stromal lymphopoietin.
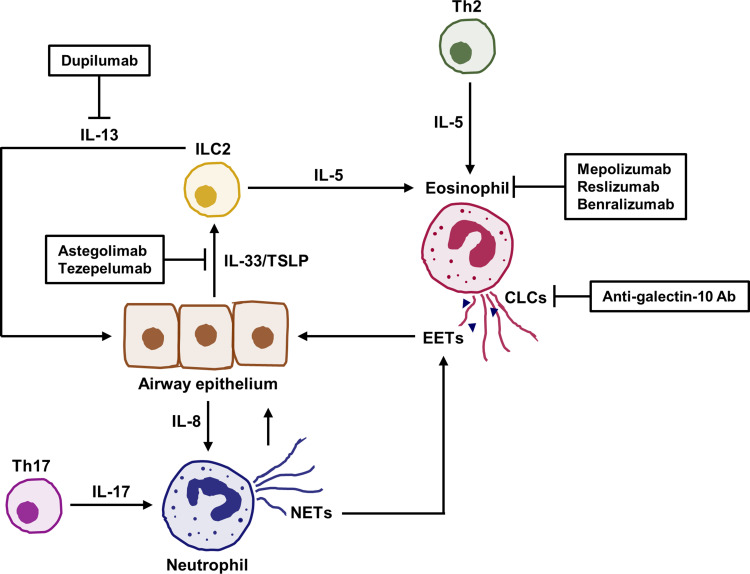
Treatment of SA
The GINA guideline recommends step 4/5 treatment for SA, where several biologics have been approved (via various randomized placebo-controlled clinical trials) and applied in real-world practice.60,61 Such biologics have many advantages in that they give the high efficacy of asthma treatment with relatively low risk.62 Moreover, these biologics targeting SA may be applicable for regulating the effect of extracellular traps released from eosinophils or neutrophils on disrupting immune responses in the airways of SA (Figure 2). Previous studies have demonstrated that corticosteroids may not suppress NET/EET-mediated airway inflammation,63–68 therefore further additional biologics are critical to control SA.
Figure 2.
Application of recent biologics for regulation of extracellular trap formation and function in severe asthma. IL-5 is essential for inducing eosinophil activation to release extracellular traps. EETs containing various molecules as well as CLCs are involved in stimulation of airway epithelium, which contributes to neutrophil recruitment or activation. NETs could damage airway epithelium and trigger EET formation related to eosinophilic inflammation. Moreover, alarmins including IL-33 and TSLP enhance production of IL-5 and IL-13 from ILC2, leading to exacerbations of airway inflammation. In each process, biologics may show a potential benefit for regulating immune responses in severe asthma.
Abbreviations: Ab, antibody; CLCs, Charcot-Leyden crystals; ILC2s, group 2 innate lymphoid cell; Th1, T helper 2 cell; Th17, T helper 17 cell.
To date, three antibodies targeting anti-IL-5 (Mepolizumab and Reslizumab) or IL-5R antibodies (Benralizumab) have been approved as an add-on treatment for patients with severe eosinophilic asthma who experience severe exacerbations and persistently eosinophilia. Mepolizumab has the effect on the alpha subunit of IL-5 to inhibit interactions between IL-5 and its receptor on the surface of eosinophils, reducing the rates of asthma exacerbation.60,61 Reslizumab targeting IL-5 could also significantly reduce asthma exacerbation and improve lung function.69–71 Benralizumab has a unique function in eosinophil apoptosis mediated by natural killer cells, improving lung function and reducing systemic oral corticosteroid requirement.72,73 In severe eosinophilic asthma, eosinophils are more activated to induce EET formation possibly due to high levels of IL-5 and other factors.37,44 In terms of the importance of IL-5 contributing to EET production,39 these biologics may be effective in preventing SA patients with the T2-high phenotype by inhibiting eosinophil activation.
Another humanized monoclonal antibody targeting IL-4 receptor alpha (Dupilumab) has been approved and applied as an add-on therapy for severe eosinophilic asthma and upper airway disease, such as CRS and NPs.2 This agent could significantly reduce asthma exacerbation as well as improve lung function in asthma and nasal symptoms in patients with CRS/NPs by blocking IL-4/IL-13 signaling pathways, suggesting that it could be more beneficial for asthmatic patients and CRS/NP patients having the T2-high phenotype (higher eosinophilia and/or FeNO level). In addition, a previous paper has demonstrated increased levels of EETs in the subepithelial regions of patients with NPs.74 Although the pathogenic mechanism of EETs involved in the formation of NPs remains unclear, EET-mediated IL-13 production from ILC2s could be related to structural modification of epithelium.45,75 Considering that patients with severe eosinophilic asthma or those with AERD are highly associated with CRS/NPs, this agent could be beneficial for controlling both upper and lower airway inflammation.
Regarding T2-low asthma, the GINA and ERS/ATS guidelines recommend a few options of additional treatment in asthmatics who have failed the step 5 treatment. Among them, anti-ST2 antibody (Astegolimab) reduced the asthma exacerbation rate in uncontrolled patients with low blood eosinophils.76 Although the function of IL-33 in EET formation remains uncertain, neutrophils as well as eosinophils express ST2 on their surfaces;77 therefore, this antibody is a new therapeutic target for T2-low SA. In addition, anti-TSLP antibody (Tezepelumab) significantly reduced asthma exacerbations and increased lung function in severe uncontrolled asthmatic patients.78 Based on recent randomized clinical trials, this anti-TSLP antibody has already been approved in the US. Considering that TSLP has been suggested as a direct stimulator inducing EETs,40 further investigations are needed to evaluate whether anti-TSLP antibody could control EET-derived T2-high airway inflammation in SA. Furthermore, recent studies have demonstrated that EETs associated with Charcot-Leyden crystal (CLC) production could be a possible mechanism of mixed granulocytic asthma. Our previous study has demonstrated that NETs could stimulate eosinophil degranulation and EDN release. These findings suggest that close interactions between eosinophils and neutrophils may contribute to developing the phenotype of mixed granulitic asthma, presenting more severe phenotype in patients with T2-high phenotype.42,79 Currently, the contribution of CLCs to the disease process is enigmatic, but CLCs could be found in any tissue with severe eosinophilic inflammation.80 However, antibodies targeting the crystallization interface of galectin-10 (a major component of CLCs) have been shown to effectively control disease in a humanized mouse model of asthma.81 Therefore, these antibodies may be a candidate biologic for SA but whether these antibodies could disrupt crystal-laden plugs needs to be clarified through investigational trials.
Future Directions
Although there have been many investigations into SA treatment, there are still unmet needs as to who show no response to step-wise pharmacologic treatment and suffer from asthma exacerbation. In this aspect, we require distinct approaches, for detection of novel biomarkers and unresolved pathophysiological pathways. Validation of new targets may provide an insight into the pathophysiology of SA for better diagnosis and treatment, suggesting that EETs and NETs may contribute to developing the phenotypes of persistent T2-high asthma, mixed granulocytic asthma, or severe T2-low asthma as well as progressive lung function decline and steroid insensitivity. In addition, further studies are needed to elucidate various factors (microbes, damage-associated molecular patterns, and immunoglobulins) for EET/NET formation, depending on each phenotype of SA.
Conclusions
Medical unmet needs still remain largely unsolved in SA representing an asthma phenotype becoming uncontrolled despite treatment of high-dose inhaled glucocorticoids with additional controllers. Here, we suggest the significance of EETs (persistent severe eosinophilic inflammation) and NETs (severe neutrophilic inflammation interacting with eosinophils) as novel target molecules to overcome these conditions. Regulation of extracellular trap formation and function according to asthma phenotypes may help address uncontrolled patients with SA.
Acknowledgments
We would like to thank for Seoul Medical Paper Consulting for English language editing.
Funding Statement
This research was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) grant funded by the Ministry of Health and Welfare, Republic of Korea (Grant no. HR16C0001).
Disclosure
The authors report no conflicts of interest for this work and that there are no financial or other issues that might lead to conflicts of interest.
References
- 1.Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;7:246. doi: 10.3389/fped.2019.00246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bachert C, Han JK, Desrosiers M, et al. Efficacy and safety of dupilumab in patients with severe chronic rhinosinusitis with nasal polyps (LIBERTY NP SINUS-24 and LIBERTY NP SINUS-52): results from two multicentre, randomised, double-blind, placebo-controlled, parallel-group Phase 3 trials. Lancet. 2019;394(10209):1638–1650. doi: 10.1016/S0140-6736(19)31881-1 [DOI] [PubMed] [Google Scholar]
- 3.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi: 10.1183/09031936.00202013 [DOI] [PubMed] [Google Scholar]
- 4.Poddighe D, Brambilla I, Licari A, Marseglia GL. Omalizumab in the therapy of pediatric asthma. Recent Pat Inflamm Allergy Drug Discov. 2018;12(2):103–109. doi: 10.2174/1872213X12666180430161351 [DOI] [PubMed] [Google Scholar]
- 5.Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med. 2012;18(5):716–725. doi: 10.1038/nm.2678 [DOI] [PubMed] [Google Scholar]
- 6.Robinson D, Humbert M, Buhl R, et al. Revisiting Type 2-high and Type 2-low airway inflammation in asthma: current knowledge and therapeutic implications. Clin Exp Allergy. 2017;47(2):161–175. doi: 10.1111/cea.12880 [DOI] [PubMed] [Google Scholar]
- 7.Lee Y, Quoc QL, Park HS. Biomarkers for severe asthma: lessons from longitudinal cohort studies. Allergy Asthma Immunol Res. 2021;13(3):375–389. doi: 10.4168/aair.2021.13.3.375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McGregor MC, Krings JG, Nair P, Castro M. Role of biologics in asthma. Am J Respir Crit Care Med. 2019;199(4):433–445. doi: 10.1164/rccm.201810-1944CI [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Granger V, Taille C, Roach D, et al. Circulating neutrophil and eosinophil extracellular traps are markers of severe asthma. Allergy. 2020;75(3):699–702. doi: 10.1111/all.14059 [DOI] [PubMed] [Google Scholar]
- 10.Holguin F, Cardet JC, Chung KF, et al. Management of severe asthma: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2020;55(1):1900588. doi: 10.1183/13993003.00588-2019 [DOI] [PubMed] [Google Scholar]
- 11.Reddel HK, Bacharier LB, Bateman ED, et al. Global initiative for asthma strategy 2021: executive summary and rationale for key changes. Eur Respir J. 2022;59(1):2102730. doi: 10.1183/13993003.02730-2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bush A, Zar HJ. WHO universal definition of severe asthma. Curr Opin Allergy Clin Immunol. 2011;11(2):115–121. doi: 10.1097/ACI.0b013e32834487ae [DOI] [PubMed] [Google Scholar]
- 13.Ricciardolo FL, Bertolini F, Carriero V, Sprio AE. Asthma phenotypes and endotypes. Minerva Med. 2021;112(5):547–563. doi: 10.23736/S0026-4806.21.07498-X [DOI] [PubMed] [Google Scholar]
- 14.Woodruff PG, Modrek B, Choy DF, et al. T-helper type 2–driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med. 2009;180(5):388–395. doi: 10.1164/rccm.200903-0392OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gibson PG, Saltos N, Borgas T. Airway mast cells and eosinophils correlate with clinical severity and airway hyperresponsiveness in corticosteroid-treated asthma. J Allergy Clin Immunol. 2000;105(4):752–759. doi: 10.1067/mai.2000.105319 [DOI] [PubMed] [Google Scholar]
- 16.Poddighe D, Mathias CB, Brambilla I, Marseglia GL, Oettgen HC. Importance of basophils in eosinophilic asthma: the murine counterpart. J Biol Regul Homeost Agents. 2018;32(2):335339. [PubMed] [Google Scholar]
- 17.Sim S, Choi Y, Park HS. Potential metabolic biomarkers in adult asthmatics. Metabolites. 2021;11(7):430. doi: 10.3390/metabo11070430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miranda C, Busacker A, Balzar S, Trudeau J, Wenzel SE. Distinguishing severe asthma phenotypes: role of age at onset and eosinophilic inflammation. J Allergy Clin Immunol. 2004;113(1):101–108. doi: 10.1016/j.jaci.2003.10.041 [DOI] [PubMed] [Google Scholar]
- 19.Moore WC, Peters SP. Severe asthma: an overview. J Allergy Clin Immunol. 2006;117(3):487–494; quiz 495. doi: 10.1016/j.jaci.2006.01.033 [DOI] [PubMed] [Google Scholar]
- 20.Lee JH, Haselkorn T, Borish L, Rasouliyan L, Chipps BE, Wenzel SE. Risk factors associated with persistent airflow limitation in severe or difficult-to-treat asthma: insights from the TENOR study. Chest. 2007;132(6):1882–1889. doi: 10.1378/chest.07-0713 [DOI] [PubMed] [Google Scholar]
- 21.Lee HY, Ye YM, Kim SH, et al. Identification of phenotypic clusters of nonsteroidal antiinflammatory drugs exacerbated respiratory disease. Allergy. 2017;72(4):616–626. doi: 10.1111/all.13075 [DOI] [PubMed] [Google Scholar]
- 22.Woo SD, Luu QQ, Park HS. NSAID-Exacerbated Respiratory Disease (NERD): from pathogenesis to improved care. Front Pharmacol. 2020;11:1147. doi: 10.3389/fphar.2020.01147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuruvilla ME, Lee F, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019;56(2):219–233. doi: 10.1007/s12016-018-8712-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Israel E, Reddel HK, Drazen JM. Severe and difficult-to-treat asthma in adults. N Engl J Med. 2017;377(10):965–976. doi: 10.1056/NEJMra1608969 [DOI] [PubMed] [Google Scholar]
- 25.Loza MJ, Djukanovic R, Chung KF, et al. Validated and longitudinally stable asthma phenotypes based on cluster analysis of the ADEPT study. Respir Res. 2016;17(1):165. doi: 10.1186/s12931-016-0482-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi Y, Lee Y, Park HS. Neutrophil activation in occupational asthma. Curr Opin Allergy Clin Immunol. 2019;19(2):81–85. doi: 10.1097/ACI.0000000000000507 [DOI] [PubMed] [Google Scholar]
- 27.Hastie AT, Mauger DT, Denlinger LC, et al. Mixed sputum granulocyte longitudinal impact on lung function in the severe asthma research program. Am J Respir Crit Care Med. 2021;203(7):882–892. doi: 10.1164/rccm.202009-3713OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaur R, Chupp G. Phenotypes and endotypes of adult asthma: moving toward precision medicine. J Allergy Clin Immunol. 2019;144(1):1–12. doi: 10.1016/j.jaci.2019.05.031 [DOI] [PubMed] [Google Scholar]
- 29.Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175(7):661–666. doi: 10.1164/rccm.200611-1717OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gibson PG, Reddel H, McDonald VM, et al. Effectiveness and response predictors of omalizumab in a severe allergic asthma population with a high prevalence of comorbidities: the Australian Xolair Registry. Intern Med J. 2016;46(9):1054–1062. doi: 10.1111/imj.13166 [DOI] [PubMed] [Google Scholar]
- 31.Gibeon D, Batuwita K, Osmond M, et al. Obesity-associated severe asthma represents a distinct clinical phenotype: analysis of the British Thoracic Society Difficult Asthma Registry Patient cohort according to BMI. Chest. 2013;143(2):406–414. doi: 10.1378/chest.12-0872 [DOI] [PubMed] [Google Scholar]
- 32.Choi Y, Kim M, Kim SJ, Yoo HJ, Kim SH, Park HS. Metabolic shift favoring C18:0 ceramide accumulation in obese asthma. Allergy. 2020;75(11):2858–2866. doi: 10.1111/all.14366 [DOI] [PubMed] [Google Scholar]
- 33.Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169–1179. doi: 10.1016/j.jaci.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haldar P, Pavord ID, Shaw DE, et al. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med. 2008;178(3):218–224. doi: 10.1164/rccm.200711-1754OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Moore WC, Meyers DA, Wenzel SE, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181(4):315–323. doi: 10.1164/rccm.200906-0896OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tashiro H, Takahashi K, Sadamatsu H, et al. Biomarkers for overweight in adult-onset asthma. J Asthma Allergy. 2020;13:409–414. doi: 10.2147/JAA.S276371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mukherjee M, Lacy P, Ueki S. Eosinophil extracellular traps and inflammatory pathologies—untangling the web. Front Immunol. 2018;9:2763. doi: 10.3389/fimmu.2018.02763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choi Y, Sim S, Park HS. Distinct functions of eosinophils in severe asthma with type 2 phenotype: clinical implications. Korean J Intern Med. 2020;35(4):823–833. doi: 10.3904/kjim.2020.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yousefi S, Gold JA, Andina N, et al. Catapult-like release of mitochondrial DNA by eosinophils contributes to antibacterial defense. Nat Med. 2008;14(9):949–953. [DOI] [PubMed] [Google Scholar]
- 40.Morshed M, Yousefi S, Stöckle C, Simon HU, Simon D. Thymic stromal lymphopoietin stimulates the formation of eosinophil extracellular traps. Allergy. 2012;67(9):1127–1137. doi: 10.1038/nm.1855 [DOI] [PubMed] [Google Scholar]
- 41.Kim HJ, Sim MS, Lee DH, et al. Lysophosphatidylserine induces eosinophil extracellular trap formation and degranulation: implications in severe asthma. Allergy. 2020;75(12):3159–3170. doi: 10.1111/all.14450 [DOI] [PubMed] [Google Scholar]
- 42.Ueki S, Tokunaga T, Melo RCN, et al. Charcot-Leyden crystal formation is closely associated with eosinophil extracellular trap cell death. Blood. 2018;132(20):2183–2187. doi: 10.1182/blood-2018-04-842260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Diny NL, Rose NR, Cihakova D. Eosinophils in autoimmune diseases. Front Immunol. 2017;8:484. doi: 10.3389/fimmu.2017.00484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Choi Y, Le Pham D, Lee DH, Lee SH, Kim SH, Park HS. Biological function of eosinophil extracellular traps in patients with severe eosinophilic asthma. Exp Mol Med. 2018;50(8):1–8. doi: 10.1038/s12276-018-0167-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Choi Y, Kim YM, Lee HR, et al. Eosinophil extracellular traps activate type 2 innate lymphoid cells through stimulating airway epithelium in severe asthma. Allergy. 2020;75(1):95–103. doi: 10.1111/all.13997 [DOI] [PubMed] [Google Scholar]
- 46.Brinkmann V, Reichard U, Goosmann C, et al. Neutrophil extracellular traps kill bacteria. Science. 2004;303(5663):1532–1535. doi: 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- 47.Abdo M, Uddin M, Goldmann T, et al. Raised sputum extracellular DNA confers lung function impairment and poor symptom control in an exacerbation-susceptible phenotype of neutrophilic asthma. Respir Res. 2021;22(1):167. doi: 10.1186/s12931-021-01759-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choi Y, Pham LD, Lee DH, et al. Neutrophil extracellular DNA traps induce autoantigen production by airway epithelial cells. Mediators Inflamm. 2017;2017:5675029. doi: 10.1155/2017/5675029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Klopf J, Brostjan C, Eilenberg W, Neumayer C. Neutrophil extracellular traps and their implications in cardiovascular and inflammatory disease. Int J Mol Sci. 2021;22:(2):559. doi: 10.3390/ijms22020559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kimball AS, Obi AT, Diaz JA, Henke PK. The emerging role of NETs in venous thrombosis and immunothrombosis. Front Immunol. 2016;7:236. doi: 10.3389/fimmu.2016.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.D’Abbondanza M, Martorelli EE, Ricci MA, et al. Increased plasmatic NETs by-products in patients in severe obesity. Sci Rep. 2019;9(1):14678. doi: 10.1038/s41598-019-51220-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Camicia G, Pozner R, de Larranaga G. Neutrophil extracellular traps in sepsis. Shock. 2014;42(4):286–294. doi: 10.1097/SHK.0000000000000221 [DOI] [PubMed] [Google Scholar]
- 53.Barnado A, Crofford LJ, Oates JC. At the bedside: neutrophil extracellular traps (NETs) as targets for biomarkers and therapies in autoimmune diseases. J Leukoc Biol. 2016;99(2):265–278. doi: 10.1189/jlb.5BT0615-234R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mutua V, Gershwin LJ. A review of neutrophil extracellular traps (NETs) in disease: potential Anti-NETs therapeutics. Clin Rev Allergy Immunol. 2021;61(2):194–211. doi: 10.1007/s12016-020-08804-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pham DL, Ban GY, Kim SH, et al. Neutrophil autophagy and extracellular DNA traps contribute to airway inflammation in severe asthma. Clin Exp Allergy. 2017;47(1):57–70. doi: 10.1111/cea.12859 [DOI] [PubMed] [Google Scholar]
- 56. Lachowicz Scroggins ME, Dunican EM, Charbit AR, et al. Extracellular DNA, neutrophil extracellular traps, and inflammasome activation in severe asthma. Am J Respir Crit Care Med. 2019;199(9):1076–1085. doi: 10.1164/rccm.201810-1869OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Quoc QL, Choi Y, Thi Bich TC, Yang EM, Shin YS, Park HS. S100A9 in adult asthmatic patients: a biomarker for neutrophilic asthma. Exp Mol Med. 2021;53(7):1170–1179. doi: 10.1038/s12276-021-00652-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bich TCT, Quoc QL, Choi Y, et al. Serum Amyloid A1: a biomarker for neutrophilic airway inflammation in adult asthmatic patients. Allergy Asthma Immunol Res. 2022;14(1):40–58. doi: 10.4168/aair.2022.14.1.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kang N, Song WJ. Discovering biomarkers of neutrophilic asthma: a clinician’s perspective. Allergy Asthma Immunol Res. 2022;14(1):1–4. doi: 10.4168/aair.2022.14.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pavord ID, Korn S, Howarth P, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380(9842):651–659. doi: 10.1016/S0140-6736(12)60988-X [DOI] [PubMed] [Google Scholar]
- 61.Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371(13):1198–1207. doi: 10.1056/NEJMoa1403290 [DOI] [PubMed] [Google Scholar]
- 62.Krings JG, McGregor MC, Bacharier LB, Castro M. Biologics for severe asthma: treatment-specific effects are important in choosing a specific agent. J Allergy Clin Immunol Pract. 2019;7(5):1379–1392. doi: 10.1016/j.jaip.2019.03.008 [DOI] [PubMed] [Google Scholar]
- 63.Nabe T. Steroid-resistant asthma and neutrophils. Biol Pharm Bull. 2020;43(1):31–35. doi: 10.1248/bpb.b19-00095 [DOI] [PubMed] [Google Scholar]
- 64.Chen X, Li Y, Qin L, He R, Hu C. Neutrophil extracellular trapping network promotes the pathogenesis of neutrophil-associated asthma through macrophages. Immunol Invest. 2021;50(5):544–561. doi: 10.1080/08820139.2020.1778720 [DOI] [PubMed] [Google Scholar]
- 65.Dworski R, Simon HU, Hoskins A, Yousefi S. Eosinophil and neutrophil extracellular DNA traps in human allergic asthmatic airways. J Allergy Clin Immunol. 2011;127(5):1260–1266. doi: 10.1016/j.jaci.2010.12.1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dicker AJ, Crichton ML, Pumphrey EG, et al. Neutrophil extracellular traps are associated with disease severity and microbiota diversity in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(1):117–127. doi: 10.1016/j.jaci.2017.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hwang CS, Park SC, Cho H-J, Park DJ, Yoon JH, Kim CH. Eosinophil extracellular trap formation is closely associated with disease severity in chronic rhinosinusitis regardless of nasal polyp status. Sci Rep. 2019;9(1):8061. doi: 10.1038/s41598-019-44627-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lewis BW, Ford ML, Rogers LK, Britt RD Jr. Oxidative stress promotes corticosteroid insensitivity in asthma and COPD. Antioxidants. 2021;10(9):1335. doi: 10.3390/antiox10091335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Corren J, Weinstein S, Janka L, Zangrilli J, Garin M. Phase 3 study of Reslizumab in patients with poorly controlled asthma: effects across a broad range of eosinophil counts. Chest. 2016;150(4):799–810. doi: 10.1016/j.chest.2016.03.018 [DOI] [PubMed] [Google Scholar]
- 70.Castro M, Zangrilli J, Wechsler ME, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3(5):355–366. doi: 10.1016/S2213-2600(15)00042-9 [DOI] [PubMed] [Google Scholar]
- 71.Murphy K, Jacobs J, Bjermer L, et al. Long-term safety and efficacy of reslizumab in patients with eosinophilic asthma. J Allergy Clin Immunol Pract. 2017;5(6):1572–1581.e1573. doi: 10.1016/j.jaip.2017.08.024 [DOI] [PubMed] [Google Scholar]
- 72.FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–2141. doi: 10.1016/S0140-6736(16)31322-8 [DOI] [PubMed] [Google Scholar]
- 73.Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid–sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376(25):2448–2458. doi: 10.1056/NEJMoa1703501 [DOI] [PubMed] [Google Scholar]
- 74.Gevaert E, Zhang N, Krysko O, et al. Extracellular eosinophilic traps in association with Staphylococcus aureus at the site of epithelial barrier defects in patients with severe airway inflammation. J Allergy Clin Immunol. 2017;139(6):1849–1860 e1846. doi: 10.1016/j.jaci.2017.01.019 [DOI] [PubMed] [Google Scholar]
- 75.Bochner BS, Stevens WW. Biology and function of eosinophils in chronic rhinosinusitis with or without nasal polyps. Allergy Asthma Immunol Res. 2021;13(1):8–22. doi: 10.4168/aair.2021.13.1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kelsen SG, Agache IO, Soong W, et al. Astegolimab (anti-ST2) efficacy and safety in adults with severe asthma: a randomized clinical trial. J Allergy Clin Immunol. 2021;148(3):790–798. doi: 10.1016/j.jaci.2021.03.044 [DOI] [PubMed] [Google Scholar]
- 77.Johnston LK, Bryce PJ. Understanding interleukin 33 and its roles in eosinophil development. Front Med. 2017;4:51. doi: 10.3389/fmed.2017.00051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Menzies Gow A, Corren J, Bourdin A, et al. Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N Engl J Med. 2021;384(19):1800–1809. doi: 10.1056/NEJMoa2034975 [DOI] [PubMed] [Google Scholar]
- 79.Gevaert E, Delemarre T, De Volder J, et al. Charcot-Leyden crystals promote neutrophilic inflammation in patients with nasal polyposis. J Allergy Clin Immunol. 2020;145(1):427–430 e424. doi: 10.1016/j.jaci.2019.08.027 [DOI] [PubMed] [Google Scholar]
- 80.Allen JE, Sutherland TE. Crystal-clear treatment for allergic disease. Science. 2019;364(6442):738–739. doi: 10.1126/science.aax6175 [DOI] [PubMed] [Google Scholar]
- 81.Persson EK, Verstraete K, Heyndrickx I, et al. Protein crystallization promotes type 2 immunity and is reversible by antibody treatment. Science. 2019;365(6442):eaaw4295. doi: 10.1126/science.aaw4295 [DOI] [PubMed] [Google Scholar]