Abstract
Background
In response to the spread of SARS‐CoV‐2 and the impact of COVID‐19, national and subnational governments implemented a variety of measures in order to control the spread of the virus and the associated disease. While these measures were imposed with the intention of controlling the pandemic, they were also associated with severe psychosocial, societal, and economic implications on a societal level. One setting affected heavily by these measures is the school setting. By mid‐April 2020, 192 countries had closed schools, affecting more than 90% of the world’s student population. In consideration of the adverse consequences of school closures, many countries around the world reopened their schools in the months after the initial closures. To safely reopen schools and keep them open, governments implemented a broad range of measures.
The evidence with regards to these measures, however, is heterogeneous, with a multitude of study designs, populations, settings, interventions and outcomes being assessed. To make sense of this heterogeneity, we conducted a rapid scoping review (8 October to 5 November 2020). This rapid scoping review is intended to serve as a precursor to a systematic review of effectiveness, which will inform guidelines issued by the World Health Organization (WHO). This review is reported in line with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) checklist and was registered with the Open Science Framework.
Objectives
To identify and comprehensively map the evidence assessing the impacts of measures implemented in the school setting to reopen schools, or keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic, with particular focus on the types of measures implemented in different school settings, the outcomes used to measure their impacts and the study types used to assess these.
Search methods
We searched the Cochrane COVID‐19 Study Register, MEDLINE, Embase, the CDC COVID‐19 Research Articles Downloadable Database for preprints, and the WHO COVID‐19 Global literature on coronavirus disease on 8 October 2020.
Selection criteria
We included studies that assessed the impact of measures implemented in the school setting. Eligible populations were populations at risk of becoming infected with SARS‐CoV‐2, or developing COVID‐19 disease, or both, and included people both directly and indirectly impacted by interventions, including students, teachers, other school staff, and contacts of these groups, as well as the broader community. We considered all types of empirical studies, which quantitatively assessed impact including epidemiological studies, modelling studies, mixed‐methods studies, and diagnostic studies that assessed the impact of relevant interventions beyond diagnostic test accuracy. Broad outcome categories of interest included infectious disease transmission‐related outcomes, other harmful or beneficial health‐related outcomes, and societal, economic, and ecological implications.
Data collection and analysis
We extracted data from included studies in a standardized manner, and mapped them to categories within our a priori logic model where possible. Where not possible, we inductively developed new categories. In line with standard expectations for scoping reviews, the review provides an overview of the existing evidence regardless of methodological quality or risk of bias, and was not designed to synthesize effectiveness data, assess risk of bias, or characterize strength of evidence (GRADE).
Main results
We included 42 studies that assessed measures implemented in the school setting. The majority of studies used mathematical modelling designs (n = 31), while nine studies used observational designs, and two studies used experimental or quasi‐experimental designs. Studies conducted in real‐world contexts or using real data focused on the WHO European region (EUR; n = 20), the WHO region of the Americas (AMR; n = 13), the West Pacific region (WPR; n = 6), and the WHO Eastern Mediterranean Region (EMR; n = 1). One study conducted a global assessment and one did not report on data from, or that were applicable to, a specific country.
Three broad intervention categories emerged from the included studies: organizational measures to reduce transmission of SARS‐CoV‐2 (n = 36), structural/environmental measures to reduce transmission of SARS‐CoV‐2 (n = 11), and surveillance and response measures to detect SARS‐CoV‐2 infections (n = 19). Most studies assessed SARS‐CoV‐2 transmission‐related outcomes (n = 29), while others assessed healthcare utilization (n = 8), other health outcomes (n = 3), and societal, economic, and ecological outcomes (n = 5). Studies assessed both harmful and beneficial outcomes across all outcome categories.
Authors' conclusions
We identified a heterogeneous and complex evidence base of measures implemented in the school setting. This review is an important first step in understanding the available evidence and will inform the development of rapid reviews on this topic.
Plain language summary
Which school‐based measures designed to contain the COVID‐19 pandemic have been evaluated to date, and how were they evaluated?
Why is this question important?
To combat the spread of SARS‐CoV‐2 and the impact of COVID‐19, countries worldwide have taken a variety of public health measures. In many countries, shutting schools was one of the earliest responses. By mid‐April 2020, 192 countries had closed schools, affecting more than 90% of the world’s student population. This severely disrupted school, family and work life, with likely negative impacts including:
‐ a worsening of children’s and adolescents’ health and well‐being; ‐ increases in inequalities between children and adolescents from disadvantaged and more privileged backgrounds; ‐ possible decreased parental income and job security; ‐ possible loss of parental economic productivity.
Given the potential negative consequences of school closures, many countries have since reopened schools. To avoid disease transmission among students, between staff and students, and beyond, a range of school‐based measures have been put in place. These include:
‐ students and staff wearing face masks and regularly washing their hands; ‐ adapting school activities (for example, not singing in music classes); ‐ improving ventilation systems; and ‐ screening suspected cases of infection.
To date, we know little about which school‐based measures designed to contain COVID‐19 have been evaluated, and how they have been evaluated. It is important to find this out, so that, in time, we can compare the effectiveness of different measures and inform future policy guidelines.
We set out to identify and map the evidence on school‐based measures to contain COVID‐19. This work is intended to form the basis of a future review about the effectiveness of these measures. This review will inform guidelines issued by the World Health Organization (WHO).
How did we identify and map the evidence?
First, we searched for studies that evaluated any intervention set in schools designed to prevent the spread of COVID‐19. We considered all types of studies, and a broad range of outcomes, including:
‐ infectious disease transmission; ‐ other harmful or beneficial effects on health; ‐ wider implications for society, the economy, and the population.
We then grouped studies according to how similar or different they were. This allowed us to gauge:
‐ which types of study have been used to evaluate measures to date; ‐ where studies have been conducted; ‐ which types of intervention have been evaluated; and ‐ which outcomes have been studied.
What did we find?
We found 42 studies.
Type of study
Thirty‐one studies used mathematical modelling designs, to predict the effects of measures on populations. Two studies used experimental designs, in which researchers divide people or settings into groups to compare the effects of different measures. Nine studies used observational designs, in which researchers simply observed the effect of the intervention.
Study setting
Studies were conducted in Europe (20 studies), North and South America (13 studies), the West Pacific (6 studies), and the Eastern Mediterranean (1 study). Most studies evaluated measures in more than one school setting (for example, primary education and secondary education). Three studies focused on secondary schools.
Type of intervention
Studies evaluated three broad types of measure:
1. Organizational measures to reduce transmission of SARS‐CoV‐2 (36 studies): these included:
‐ measures designed to limit risks of disease transmission between people who come into contact with each other (such as face‐masks and physical distancing policies); and ‐ measures to reduce opportunities for contact (for example, staggered arrival, break and departure times).
2. Structural or environmental measures to reduce transmission of SARS‐CoV‐2 (11 studies): for example, dividing up school playgrounds or improving air circulation.
3. Surveillance and response measures to detect SARS‐CoV‐2 infections (19 studies): these included:
‐ testing, tracing, and symptom screening; and ‐ isolation of confirmed cases or quarantine of suspected cases.
Outcomes studied
Studies assessed the effects of measures on:
‐ SARS‐CoV‐2 transmission (29 studies), including the number of new cases or the average number of people to whom one infected person will pass the virus (reproduction number R); ‐ healthcare use (8 studies), for example, the number of hospitalizations; ‐ other health outcomes (3 studies), for example, the risk of developing hand eczema (a skin condition); and ‐ societal, economic, and other population‐level outcomes (5 studies), including cost.
What are the implications of our findings?
A wide range of school‐based measures designed to contain COVID‐19 have been evaluated to date. To evaluate these, researchers have used different methods and investigated different outcomes. This review is an important first step in gauging what evidence is available, and will inform future rapid reviews on this topic.
Background
Introduction and context
In December 2019 the novel coronavirus, SARS‐CoV‐2, was first reported in Wuhan, China. Over the subsequent weeks, the virus and the associated disease, COVID‐19, spread internationally and, on 11 March 2020, the World Health Organization (WHO) declared a pandemic (WHO 2020a). The effects of an infection with SARS‐CoV‐2 range from no or limited symptoms to various systemic impacts, including severe pneumonia, acute respiratory distress, renal failure, damage to other internal organs, and death (CDC 2020a; Matthay 2020; Yelin 2020). There is also increasing concern about long COVID, which describes a range of long‐term effects in patients with mild or severe disease such as post‐intensive care syndrome, post‐viral fatigue syndrome, and long‐term COVID syndrome (NIHR 2020a). To contain the spread of SARS‐CoV‐2 and the impact of COVID‐19, national and subnational governments have implemented a variety of measures (Prem 2020). One setting where measures were implemented from a very early stage is the school setting. By mid‐April 2020, 192 countries had closed schools, affecting more than 90% (nearly 1.6 billion) of the world’s student population (UNESCO 2020a).
School closures represent a community‐based, non‐pharmaceutical intervention that has been implemented in response to previous communicable disease outbreaks, notably influenza (Smith 2020; WHO 2019). Children may play a key role in the transmission of many viral diseases (Worby 2015). With regard to influenza, school‐aged children and adolescents have high contact rates with their peers (Mossong 2008), spend longer periods of time with their contacts (Mossong 2008), tend to be more susceptible to infection than other age groups (Cauchemez 2009), and have increased viral shedding compared to other age groups (Cauchemez 2009). By closing schools, children are prevented from being in close proximity to each other, teachers, and other staff working in the school environment. This may reduce transmission between individuals within and outside of the school setting, such as caregivers and relatives (Prem 2020). The effectiveness of these measures is, however, subject to debate. For influenza epidemics, there is inconclusive evidence: one systematic review found that school closures reduced the peak of the epidemic by around 30% and shifted its peak by 11 days (Bin Nafisah 2018). Limited evidence from modelling studies and observational studies included in another review suggests that the reduction in occurrence and transmission of influenza following school closures varied widely, from 1% to 50% (Rashid 2015). Additionally, it was found that the timing of initiation as well as the duration of school closures were critical, with proactive closures being superior to reactive closures (Bin Nafisah 2018; Jackson 2013; Jackson 2014).
To our knowledge, to date only one systematic review by Viner and colleagues (Viner 2020a), has synthesized the evidence on the use, effectiveness and cost‐effectiveness of school closures and various school‐based social distancing practices on infection rates and transmission during coronavirus outbreaks (i.e. SARS‐CoV‐1, MERS‐CoV, SARS‐CoV‐2). However, most included studies reported data from previous severe acute respiratory syndrome (SARS) outbreaks or were modelling studies, as peer‐reviewed empirical evidence on COVID‐19 was not yet available. Due to the substantial heterogeneity of included studies, Viner and colleagues did not conduct meta‐analysis. One widely cited modelling study on COVID‐19, also included in Viner 2020a, predicted that school and university closures implemented alongside a range of other interventions, could prevent between 2% and 4% of deaths (Ferguson 2020). Emerging evidence based on more recent modelling studies found the effectiveness of combined school and university closures to be much higher than initially predicted, contributing to a 21% to 55% reduction in the reproduction number R (Brauner 2020).
School closures, however, also have significant broader psychosocial, societal, and economic implications, including considerable costs and negative consequences (Christakis 2020; Kneale 2020; Viner 2020a), both in the short term and longer term (Smith 2020). For children and adolescents, school closures are likely to have negative impacts on educational outcomes, but also on their physical and mental health (Golberstein 2020; UNESCO 2020b). For parents and caregivers, school closures cause a major disruption to their family and work life and there are likely impacts on job and income security, and psychosocial health (Kneale 2020). On a macro level, school closures might have broader implications such as loss of parental economic productivity, which might ultimately lead to a decrease in gross domestic product (Kneale 2020). In addition, disadvantaged children and families are likely to carry a substantially higher proportion of the associated costs (e.g. impact on educational attainment), thereby increasing existing inequalities (Crawley 2020; Viner 2020a; Viner 2020b).
In consideration of these wide‐ranging and potentially harmful consequences, many stakeholders have advocated for the reopening of schools, arguing that the harms are likely to outweigh the potential benefits of school closures (Liu 2020). This debate has been fuelled by evolving evidence around the role of children in the transmission of SARS‐CoV‐2. When contracting COVID‐19, the disease is less severe among children, with around 90% of children showing no, mild, or moderate symptoms (Castagnoli 2020; Dong 2020; Ludwigsson 2020). A small proportion of children develop severe disease (multisystem inflammatory syndrome (MIS‐C)) and require intensive care and prolonged ventilation (Feldstein 2020; Götzinger 2020). Despite this, a fatal outcome is rare (Götzinger 2020). Further, children may be less likely to become infected upon pathogen exposure than adults (Li 2020), as suggested by a recent systematic review (Viner 2020c), and further primary studies (Davies 2020a; Jing 2020). Transmission of SARS‐CoV‐2 by infected younger children (under 12 to 14 years) appears to be lower than transmission by adults, even though robust evidence is lacking (Viner 2020c). Adolescents, however, seem to be comparable to adults when it comes to transmitting SARS‐CoV‐2 (Dattner 2020; Fontanet 2020a; Park 2020). Regarding teachers and other school staff, limited evidence suggests that transmission of the virus may be more likely among adults than between children and adults (Macartney 2020). An ongoing systematic review on COVID‐19 transmission in schools will likely provide further insights (Xu 2020).
In view of the above, many countries around the world reopened their schools in the months after the initial closures (Bonell 2020; Couzin‐Frankel 2020; Dibner 2020; WHO 2020b). In doing so, countries have implemented a broad range of measures at the macro level (e.g. national or state legislation), at the level of the school, at the level of cohorts within the school setting (e.g. grades, classes, or faculty/school staff), and at the individual level (including high‐risk individuals).
Rationale for conducting a scoping review
Schools can be conceptualized as complex systems, whereby an intervention interacts with the diverse agents in the system to generate changes in behaviours (Keshavarz 2010). While several reviews have addressed questions around the role of schools in the transmission of SARS‐CoV‐2 and their influence on the course of the pandemic (Fadlallah 2020; NCCMT 2020; Public Health Ontario 2020; Viner 2020c), they have not considered the interplay of measures implemented in the school setting in a comprehensive manner. Instead, they have focused on the role of children in transmission (NCCMT 2020), rather than a broader set of outcomes, or examined school closures only (Viner 2020c), rather than addressing the broad range of measures implemented to keep schools open. To our knowledge, there is no review that assesses the range of measures that are implemented to minimize SARS‐CoV‐2 transmission in and around schools and that examines implications for health and society beyond SARS‐CoV‐2 transmission.
Objectives
To identify and comprehensively map the evidence assessing the impacts of measures implemented in the school setting to reopen schools, or keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic, with particular focus on the types of measures implemented in different school settings, the outcomes used to measure their impacts and the study types used to assess these.
Methods
We conducted a rapid scoping review to meet these objectives. The goal of a scoping review is to identify and map the available evidence (Anderson 2008; Munn 2018). Scoping reviews are particularly useful in areas with emerging evidence, as they provide an overview of a body of literature with regard to key concepts, the types of studies available, and related research gaps (Munn 2018). As a precursor for a systematic review, they are particularly helpful in identifying or categorizing interventions, outcomes, or populations of relevance (Munn 2018). Scoping reviews involve several stages including:
identifying the research question;
identifying relevant studies;
selecting eligible studies;
charting the data; and
collating, summarizing and reporting the results (Arksey 2005).
They can comprise an optional stakeholder consultation stage (Arksey 2005). In contrast to systematic reviews, scoping reviews do not usually critically appraise included studies. Some methodological expectations for Cochrane intervention reviews are not necessary or suitable for scoping reviews, such as those relating to the synthesis of effectiveness data (with or without meta‐analysis), assessment of bias across study results, and application of GRADE to assess confidence in synthesized results.
After we had developed the protocol (Pfadenhauer 2020), we conducted the review over a four‐week period from the point of the search (search date 8 October 2020).
Key question
We addressed the following key question in this rapid scoping review: what studies are available that have assessed the impacts of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic?
Criteria for considering studies for this review
We included studies that quantitatively assessed the impact of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic. Given that the aim of this review is to identify and map the evidence base and given that the scoping review methodology allows for flexibility (Tricco 2016), we did not impose strict limitations with regard to the types of populations, specific interventions in the school setting, outcomes, and study designs considered. This allowed us to inductively describe and categorize these aspects, and subsequently update our understanding of the complex interplay of measures implemented in the school setting. Table 1 and Table 2 provide specific inclusion and exclusion criteria, respectively.
1. Inclusion criteria.
| Population |
|
| Setting |
|
| Interventions |
|
| Study designs |
|
aInternationally, there are important differences with regards to starting and finishing ages; we did not exclude studies that comprised students outside of this age range if students attended a year level corresponding to the primary or secondary educational stage.
2. Exclusion criteria.
| Population |
|
| Setting |
|
| Interventions |
|
| Study designs |
|
We drew on direct evidence regarding SARS‐CoV‐2/COVID‐19 only. We excluded studies assessing other viral acute diseases with epidemic/pandemic potential, such as SARS, Middle East respiratory syndrome (MERS) and (pandemic) influenza for multiple reasons, including: increasing availability of studies concerned with SARS‐CoV‐2/COVID‐19; limited transferability of evidence from pandemics or outbreaks caused by other pathogens (e.g. influenza); and inherent discrepancies between interventions implemented during the COVID‐19 pandemic and interventions implemented in previous pandemics or outbreaks – previous school measures tended to be highly localized, short‐term and reactive while current measures are more generic and long‐term and have much broader implications (Kneale 2020).
Description of the school setting and interventions of interest
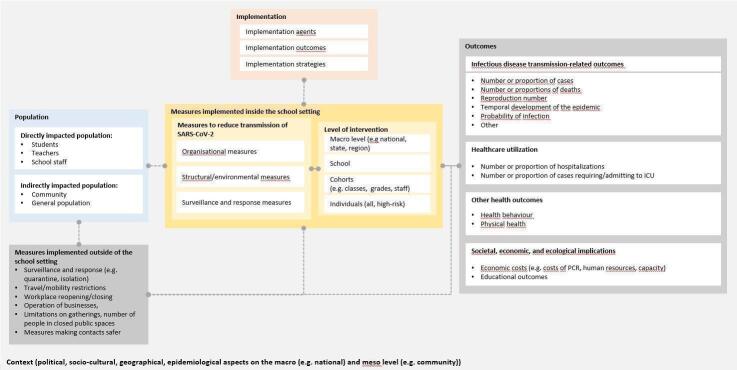
In the following, we elaborate on our a priori understanding of the system in which the measures to safely reopen schools or to keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic are implemented. To further our understanding, we developed an a priori system‐based logic model shown in Figure 1. This was informed by two published logic models on the topic (Bonell 2020; Kneale 2020); a framework to facilitate evidence‐based decision‐making during COVID‐19 (Stratil 2020); and WHO's documentation of school‐based measures implemented in countries of the WHO European Region (WHO 2020c). We used this a priori understanding in planning the data extraction and evidence mapping; it underwent a process of adaptation as we inductively integrated subcategories during the mapping. The system‐based logic model aided us in visualizing a priori how measures implemented in the school setting could be conceptualized, following the PICO (population, intervention, comparison and outcome) scheme. These components are described below.
1.
The system‐based logic model visualizes our a priori conceptualization of measures implemented in the school setting, following the PICO (population, intervention, comparison and outcome) scheme. The impact of measures implemented in the school setting is also dependent on measures implemented in the wider community (e.g. mask regulations) or on a national level (e.g. travel bans)
Setting
Schools are environments in which educational services are provided to children with diverse backgrounds, characteristics, abilities, and needs. The age of students ranges from about four to about 18 years, depending on a country’s educational system (e.g. in some countries school starts as early as four years, in others as late as seven years). We consider schools to be any setting with the primary purpose of providing education to children. Most countries distinguish between primary or elementary education and secondary education. Primary, elementary or basic school usually constitutes the first school type children attend as part of their (compulsory) education, however, some countries refer to the first year of compulsory education as preschool. It typically lasts six years, although its duration can range between four and seven years, and typically lasts until the ages of 10 to 12 (UNESCO 2012). Students usually enter secondary school between the ages of 10 and 13, with 12 being the most common age (UNESCO 2012). Depending on the context, schools for secondary school age groups may be referred to as secondary, middle or high school (UNESCO 2012).
For this review, we defined the school setting as the school, the school grounds, school vehicles, or any activity organized by or linked to the school. Measures might affect activities carried out in the classroom, during breaks, during dining, in hallways, in bathrooms, in faculty rooms, or during transportation and movement around the campus. Further, by ‘in and around’ the school, we refer to activities such as public transportation to and from the school, as well as activities between students, staff, and other populations that take place before and after school, which would not have taken place if schools were not open. These include structured activities such as participation in sports, after‐school child care or other extracurricular activities, as well as informal activities such as leisure time before and after school and long lunch breaks for older students, and businesses or cafés visited by students and staff throughout the school day. Schools may have less or no formal control over these activities, but school‐related measures may nevertheless affect SARS‐CoV‐2 transmission as a result of or during these activities.
Population
A range of individuals is affected by measures implemented in the school setting. These include those directly impacted in the school setting, such as students, their teachers and other school staff, as well as those individuals who facilitate activities or transportation around schools (e.g. bus drivers, coaches). Other populations affected less directly and outside of the school setting include parents and carers, families and friends of students, teachers and school staff, as well as members of the wider community in which schools are embedded.
Intervention
Many measures may be implemented in the school setting, which can broadly be categorized as follows.
Measures addressing screening, testing and subsequent action: monitoring of COVID‐19‐associated symptoms that may prompt COVID‐19 testing, strategies to screen or test individuals or groups (e.g. students or school staff with symptoms or elevated temperature, or who have had contact with infected individuals) and subsequent actions, which could include self‐isolation of confirmed cases and reactive dismissal and quarantine of potentially infected individuals or groups (e.g. if individuals, cohorts, classes, grades or entire schools are dismissed after a COVID‐19 case is suspected or confirmed in students or school staff or in their contacts).
Measures addressing behaviour: measures addressing the behaviour of students or school staff, or both (e.g. mask mandates, distancing regulations, hygiene and cleaning concepts).
Measures addressing the organization and administration of school activities: measures addressing the availability, structure and timing of school activities (e.g. cohorting, alternating physical presence, staggered arrival, departure, dining and breaks, and (reduced) availability of extracurricular activities).
Changes to infrastructure and environment: altering the physical environment (e.g. improving airflow or ventilation, adding physical barriers to help individuals avoid contact, adapting forms of transportation, such as walking or bus).
This list of intervention categories may not be exhaustive, and we expect our understanding of the types of interventions to develop because of this scoping review.
Outcomes
School measures are intended to positively influence the course of the pandemic, through improvements in infectious disease transmission‐related outcomes, such as reductions in the number of cases detected in students, teachers and school staff; the number of cases averted among students, teachers and school staff; the number of cases averted among contacts of students, teachers and school staff, as well as among the broader community. However, these measures also have wide‐ranging implications beyond disease transmission, which can be harmful or beneficial. Notably, they are likely to affect other health outcomes, such as physical health, psychosocial well‐being, mental health and the maintenance of essential school‐based services including health services and services affecting health or health behaviours. Additionally, they are likely to affect educational outcomes among children and have broader societal, economic and environmental consequences.
Context and implementation
All measures implemented within the school setting will inevitably be influenced by the context in which they are implemented and the way they are being implemented. We define context as a set of characteristics and circumstances that include active and unique factors within which the intervention and its implementation are embedded (Pfadenhauer 2017). Context comprises seven domains, namely geographical, epidemiological, socio‐cultural, socio‐economic, ethical, legal and political (Pfadenhauer 2017). Interactions can occur on a macro, meso and micro level. Implementation is an actively planned and deliberately initiated effort with the intention to bring a given intervention into policy and practice within a particular setting (Pfadenhauer 2017). We were particularly interested in the following.
Implementation strategies (i.e. methods and means to ensure the adoption and sustainment of interventions)
Implementation agents (i.e. all individuals and organizations engaged with deciding to implement, implementing or being affected by the intervention)
Implementation outcomes (i.e. fidelity, adherence, uptake, acceptability, and cost). Fidelity is concerned with the degree to which an intervention is implemented as intended (Rabin 2008); adherence is concerned with participants’ behaviours (Persch 2013).
Search methods for identification of studies
We searched the following electronic databases on 8 October 2020.
MEDLINE Ovid (1946 to 2 October 2020); searched 8 October 2020
Embase Ovid (1996 to 7 October 2020); searched 8 October 2020
Our search strategy was structured around two main search concepts: SARS‐CoV‐2/COVID‐19 and school settings. We developed the initial search strategy for MEDLINE and adapted it for the other databases. Please see Appendix 1 for the full search strategies.
We additionally searched the following COVID‐19‐specific databases.
CDC COVID‐19 Research Articles Downloadable Database for bioRxiv, medRxiv and SSRN preprints (cdc.gov/library/researchguides/2019novelcoronavirus/researcharticles.html)
WHO COVID‐19 Global literature on coronavirus disease (search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov): this includes published and prepublication journal articles.
The Cochrane COVID‐19 Study Register (covid-19.cochrane.org/): this includes published articles, trials registry records and preprints.
We also conducted forward and backward citation searches of all relevant systematic reviews and guidelines retrieved by our search strategy (see Table 3), and included eligible studies identified through these searches. We searched Scopus, which allows for downloading titles and abstracts for retrieved items, for all published studies. For all other studies that were not indexed in Scopus (i.e. reports, guidelines, preprints), we conducted the searches in Google Scholar.
3. Reviews and guidelines used for snowball searches.
| # | Review/guideline |
| 1 | D'Angelo D, Coclite D, Napoletano A, Fauci AJ, Latina R, Iacorossi L, et al. Strategies for exiting COVID‐19 lockdown for workplace and school: a scoping review protocol (D'Angelo 2020). |
| 2 | COVID‐19 Emergency Response Key Places Protection and Disinfection Technology Team, Chinese Center for Disease Control and Prevention. Health protection guideline of schools and other educational institutions during COVID‐19 outbreak (CCDCP 2020a). |
| 3 | Strategy and Policy Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. Interim guidelines for prevention and control of COVID‐19 for students back to school (CCDCP 2020b). |
| 4 | Araújo LA, Veloso CF, Souza MC, Azevedo JM, Tarro G. The potential impact of the COVID‐19 pandemic on child growth and development: a systematic review (Araújo 2020). |
| 5 | Cohen R, Delacourt C, Gras‐Le Guen C, Launay E; French Pediatric Society. COVID‐19 and schools. Guidelines of the French Pediatric Society (Cohen 2020). |
| 6 | Fardin MA. COVID‐19 and anxiety: a review of psychological impacts of infectious disease outbreaks (Fardin 2020). |
| 7 | Kneale D, O'Mara‐Eves A, Rees R, Thomas J. School closure in response to epidemic outbreaks: systems‐based logic model of downstream impacts (Kneale 2020). |
| 8 | Nussbaumer‐Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID‐19: a rapid review (Nussbaumer‐Streit 2020). |
| 9 | Abadio de Oliveira W, da Silva JL, Monezi Adrade AL, De Micheli D, Carlos DM, Iossi Silva MA, et al. Adolescents’ health in times of COVID‐19: a scoping review (Abadio de Oliveira 2020). |
| 10 | Viner RM, Mytton OT, Bonell C, Melendez‐Torres GJ, Ward J, Hudson L, et al. Susceptibility to and transmission of COVID‐19 amongst children and adolescents compared with adults: a systematic review and meta‐analysis (Viner 2020c). |
| 11 | Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID‐19: a rapid systematic review (Viner 2020a). |
| 12 | WHO. Considerations for school‐related public health measures in the context of COVID‐19: annex to considerations in adjusting public health and social measures in the context of COVID‐19 (WHO 2020c). |
| 13 | Juneau CE, Pueyo T, Bell M, Gee G, Collazzo P, Potvin L. Evidence‐based, cost‐effective interventions to suppress the COVID‐19 pandemic: a systematic review (Juneau 2020). |
| 14 | Brooks SK, Smith LE, Webster RK, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children's social contact: rapid evidence review (Brooks 2020). |
| 15 | New York State Education Department. Recovering, rebuilding, and renewing: the spirit of New York’s schools ‐ reopening guidance (NYSED 2020). |
| 16 | Simon A, Huebner J, Berner R, Munro AP, Exner M, Huppertz H‐I, et al. Measures to maintain regular operations and prevent outbreaks of SARS‐CoV‐2 in childcare facilities or schools under pandemic conditions and co‐circulation of other respiratory pathogens (Simon 2020). |
| 17 | Walger P, Heininger U, Knuf M, Exner M, Popp W, Fischbach T, et al. Children and adolescents in the COVID‐19 pandemic: schools and daycare centers are to be opened again without restrictions. The protection of teachers, educators, carers and parents and the general hygiene rules do not conflict with this (Walger 2020). |
| 18 | CDC. Operating schools during COVID‐19: CDC's considerations (CDC 2020b). |
| 19 | CDC. Interim considerations for testing for K‐12 school administrators and public health officials (CDC 2020c). |
| 20 | Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM. What settings have been linked to SARS‐CoV‐2 transmission clusters? (Leclerc 2020). |
| 21 | National Collaborating Centre for Methods and Tools. Rapid evidence review: what is the specific role of daycares and schools in COVID‐19 transmission? (NCCMT 2020). |
To retrieve unpublished reports or studies not published in journals, we conducted a Google search and screened the first 10 pages of results ranked by relevance (100 web pages).
An experienced information specialist (RF) designed all database search strategies. Results were limited to the year 2020, which is when publications around the COVID‐19 pandemic began to appear. We did not apply any language limits.
Study selection
After deduplication, review authors (CJS, CK, JR, KW, LMP, MC, ShK, SK) double‐screened all titles and abstracts in duplicate, excluding all studies that were clearly irrelevant. We moved studies marked as unclear forward to the next stage. For all studies deemed potentially relevant or unclear at the title/abstract screening stage, review authors (CK, HL, JB, KG, KW, LMP, MC, ShK, SK, and SV) double‐screened the full text in duplicate. In case of any discrepancies, the two review authors who had screened the study in question discussed it further; where necessary including a third review author (HL, JB, SK, LMP) or the larger review team in further discussions to achieve consensus. At this stage, we made a final decision regarding inclusion or exclusion.
We used Endnote to manage collection and deduplication of records. For title and abstract screening, we used Rayyan (rayyan.qcri.org/welcome), a web‐based application, designed for citation screening for systematic reviews. We documented and reported reasons for the exclusion of full texts using Microsoft Excel (Microsoft Corporation 2018).
For both the title and abstract, and full‐text screening stages, we developed screening guidance forms to ensure that all review authors screened similarly and consistently. All review authors screened 10% of the search results and discussed discrepancies before starting to screen titles and abstracts. After having screened approximately 300 titles and abstracts and approximately 50 full texts, we discussed inconsistencies and challenges encountered within the review team. We continually updated the screening guidance. Additionally, we collected and clarified all uncertainties in screening on a rolling basis. We discussed these in regular online meetings to ensure consistency in screening across multiple review authors.
Extraction and charting of data
One review author (AM, CK, HL, JB, JMS, JR, KG, KS, KW, LMP, ShK, SK and SV) extracted and charted study characteristics and data into the categories of the data extraction form in Microsoft Excel (Microsoft Corporation 2018). These categories included a priori categories, based on our initial understanding of the school system, as well as inductive subcategories that we developed as new concepts emerged. A priori categories included the population (e.g. age group), setting (e.g. type of school), and context (e.g. geographical context, community); types of interventions (e.g. policies addressing behaviours), comparisons (where available), outcomes of interest (e.g. health, economic, and social impact), and study designs (e.g. epidemiologic study, modelling study). The review team pilot‐tested the extraction form (Appendix 2) on two studies and subsequently revised it. One experienced review author (JMS, AM) reviewed all extracted data.
Collation, summary and reporting of the results
We collated, summarized and reported the extracted data. Specifically, we aimed to define, summarize, and present clusters of types of interventions, outcomes of interest, and study designs using a priori‐defined categories and emerging/inductively developed categories. One review author (AM, HL, JB, KS, LMP and ShK) conducted mapping per category outlined in the a priori logic model (Figure 1). A second review author double‐checked all data presented in the tables, text and graphics.
We also aimed to advance the a priori logic model by integrating factors (subcategories) that were missing or might be represented in a suboptimal manner. We particularly looked for additional or more refined intervention types, outcomes, resource and implementation aspects, and contextual factors that might impede or facilitate the implementation of the intervention. Importantly, we tried to establish a better classification of measures implemented in the school setting, paying attention to what happens both at schools themselves and outside of the immediate school environment.
Results
Results of the search
Our searches retrieved 1660 records after deduplication (search date: 8 October 2020). After title and abstract screening, we assessed 156 studies at the full‐text screening stage, 37 of which we included. Through forward and backward searches, we identified five additional studies that met our inclusion criteria that were not captured in our database searches (Buonsenso 2020; Gandolfi 2020; Gill 2020; Isphording 2020; Panovska‐Griffiths 2020a). We therefore included 42 studies in this scoping review (see Characteristics of included studies). The PRISMA flow chart describes the study selection process (Tricco 2018; Figure 2). Reasons for excluding selected studies are summarized in the Characteristics of excluded studies.
2.
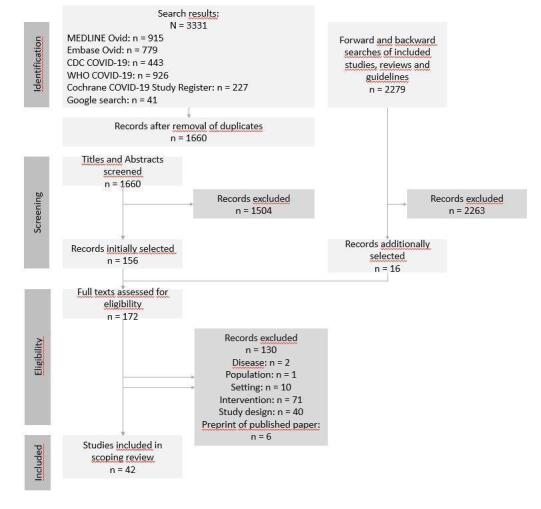
The review flowchart showing an overview of our searching and screening procedures
Description of studies
There was a high level of heterogeneity among the included studies in terms of study types, populations, the measures implemented or modelled, and the outcomes assessed. We have provided short descriptions of a selection of exemplary studies to demonstrate the range of studies and the heterogeneity between them in Table 4. We chose these studies, as each represents a rough cluster of similar studies within the included studies.
4. Short description of selected included studies.
| Study ID | Short description |
| Burns 2020 | This study primarily looked at isolation measures and subsequent symptom monitoring and their impact on transmission of SARS‐CoV‐2 and influenza. It modelled scenarios in a typical primary school setting in the USA. Primarily, the study used a deterministic, compartmental SEIR model of symptom‐based isolation that accounted for the timing of symptoms, viral shedding, and the population structure. This model was inferential, and therefore allowed for inferences to be made about the impact of these measures on the number of cases, and the attack rate of the virus. The study also assessed other intervention types, albeit to a lesser degree. In terms of interventions to reduce contact, the study modelled the effects of smaller class sizes. The study also assessed strategies to promote compliance to isolation measures, including remote monitoring, penalties for non‐compliance, provision of thermometers, and other strategies to help with maintenance of home isolation. The study also modelled outcomes related to vaccine availability and uptake. |
| Gill 2020 | This study used an agent‐based model, refined based on emerging evidence and extended to incorporate effects of quarantines and temporary school shutdowns in response to COVID‐19 cases in the school community. In this study, agents were defined as students, teachers, and other school staff such as bus drivers, learning and working in settings managed by the school. The study authors simulated the interactions of individuals, incorporating available data on infection spread and mitigation strategies that included measures to reduce opportunities for contacts (i.e. physical distancing, staggered start, break, and finish times; alternating attendance; formation of cohorts) or measures to make contacts safer (i.e. wearing masks), to predict the likely spread of disease in a school. The study also looked at reactive measures in which a positive test result would lead to quarantine of the infected person’s direct contacts, defined in the model as all students and staff who shared a class or a bus with the infected person. The study modelled ‘typical’ primary, middle, and secondary school settings in Pennsylvania, USA and looked and three key outcomes: 1. Relative total number of infections among students and staff. 2. Percentage of days in the school building for a typical student. 3. Estimated number of actual infections in the school based on recent detected infections. |
| Isphording 2020 | This study used a quasi‐experimental study design to compare differences in the number of newly confirmed cases across German states that implemented reopening measures. Because of the staggered nature of states returning to school in Germany, states that had not yet reopened with measures in place were used as controls. Several different intervention types and measures were assessed. In terms of measures to make contacts safer, the study assessed the impact of face mask policies, hand hygiene policies, policies that focused on respiratory etiquette and other, physical‐distancing policies (mandated distancing on the school yard), modification of activities in order to reduce risk of transmission (e.g. not singing or using wind instruments in music class), and exemption of high‐risk students from classes. Measures to reduce the opportunity for contacts included staggered start, break and finish times, alternating attendance (e.g. different students attending on different days, weeks), formation of fixed cohorts, and cancellation of activities (e.g. music class, physical activity, school trips). Measures related to infrastructure included enhanced ventilation systems. Measures related to surveillance included quarantine of cases and contacts, and free testing. The study looked at outcomes in the primary and secondary school setting as well as in the general population, stratified into four age groups (0–14, 15–34, 35–59, 60+). The main outcome of interest was the number of cases at three months' follow‐up. |
| Macartney 2020 | This paper described a prospective cohort study of all children (aged ≤ 18 years) and staff who attended school or early childhood education and care (ECEC) settings while considered infectious. The study looked primarily at surveillance measures and assessed infections following school reopening without control or counterfactual; this descriptive nature meant that inferences cannot be drawn about the impact of the relevant measures. All cases (or their parents or carers) were interviewed at diagnosis to determine links to known COVID‐19 cases, ascertain movements, and identify close contacts while infectious, including at educational facilities. All close contacts quarantined at home for 14 days, had regular text message or telephone call contact to enquire about symptoms, and were instructed to be tested if they developed COVID‐19‐related symptoms at designated COVID‐19 testing facilities. The study also looked at reactive school closures for 1 or 2 days after the identification of a positive case. The study looked at primary and secondary school settings in Australia and included students (ages 5‐18 years) and staff. It also included students six weeks to five years in ECEC settings, although this is not relevant to this review. SARS‐CoV‐2 transmission was the key outcome of interest. |
| ECEC: early childhood education and care; SEIR: Susceptibility‐Exposed‐Infected‐Recovered | |
The majority of studies (n = 29) were published on preprint servers, four were published as reports (Gill 2020; Isphording 2020; Monod 2020; NCIRS 2020), and nine as journal publications (Campbell 2020; Ehrhardt 2020; Gandolfi 2020; Kim 2020; Macartney 2020; Otte Im Kampe 2020; Panovska‐Griffiths 2020b; Simonsen 2020; Stein‐Zamir 2020).
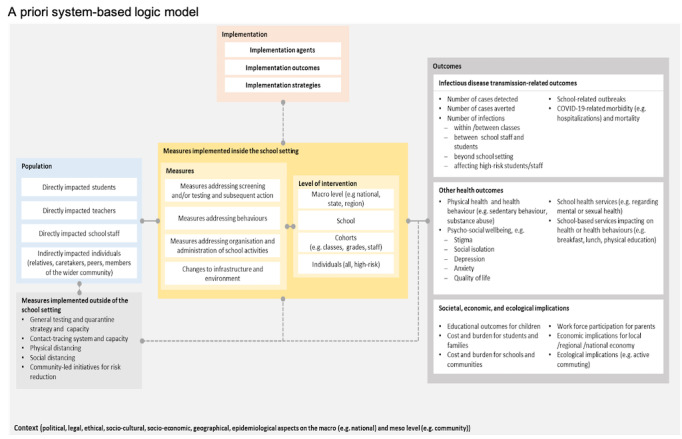
In the sections below, we describe our results according to the categories included with the a priori logic model (Figure 1). We elaborate on whether and how the results were consistent with this logic model. Where they differed, we adapted the a priori model. Key differences between the two iterations related to the outcomes assessed by the studies. The a posteriori logic model is shown in Figure 3. Figure 4, an evidence gap map, summarizes the distribution of studies related to the study types, intervention, and outcome categories.
3.
The system‐based logic model, an updated version of the a priori logic model, visualizes our posteriori conceptualization of measures implemented in the school setting, following the PICO (population, intervention, comparison and outcome) scheme. The impact of measures implemented in the school setting is also dependent on measures implemented in the wider community (e.g. mask regulations) or on a national level (e.g. travel bans)
4.

Evidence gap map in which each square represents the case in which a single included study evaluated a type of school measure (rows) against an outcome category (columns); additionally, the study type is provided (colour).
Study types
The included studies fall into three broad types of study: experimental/quasi‐experimental, observational and mathematical modelling studies. The majority of the included studies employed a mathematical modelling design (n = 31); nine studies used an observational/epidemiological design (Buonsenso 2020; Ehrhardt 2020; Macartney 2020; NCIRS 2020; Otte Im Kampe 2020; Simonsen 2020; Sparks 2020a; Stein‐Zamir 2020; Yoon 2020), and two studies an experimental or quasi‐experimental design (Isphording 2020; Curtius 2020); the one experimental study (Curtius 2020), was combined with mathematical modelling.
Experimental or quasi‐experimental studies
Of the two studies employing an experimental or quasi‐experimental approach, one assessed the installation of an air purifier in classrooms and its effect on airborne transmission of SARS‐CoV‐2 (Curtius 2020); the other used the opportunity of staggered school starts after the summer holidays in Germany to assess measures implemented in the different states, treating the states still on summer holiday as control (Isphording 2020).
Mathematical modelling studies
Within the group of mathematical modelling studies, included studies employed compartmental models, such as those using variations of the Susceptibility‐Exposed‐Infected‐Recovered (SEIR) model, agent‐based models such as COVASIM, which were sometimes combined with compartmental modelling, and other forms of modelling.
Observational/epidemiological studies
The observational/epidemiological studies included surveillance studies or cohort studies tracking the occurrence of cases or other relevant outcomes over time (Buonsenso 2020; Ehrhardt 2020; Macartney 2020; NCIRS 2020; Otte Im Kampe 2020; Simonsen 2020; Sparks 2020a; Stein‐Zamir 2020; Yoon 2020).
Another important aspect regarding the study type, as well as the specific analytical methods employed, relates to whether the study was inferential or descriptive in nature. Inferential studies (n = 34) allow inferences to be made about the impact of relevant school measures on outcomes. Descriptive studies (n = 8) provide information on both school measures and outcomes of interest, however, these do not provide an explicit link between the two, that is, it remains unclear whether or to what extent the intervention led to the outcome (Buonsenso 2020; Ehrhardt 2020; Macartney 2020; NCIRS 2020; Otte Im Kampe 2020; Stage 2020; Stein‐Zamir 2020; Yoon 2020).
Populations
As conceptualized in our a priori logic model (Figure 1), and as demonstrated in the included studies (Characteristics of included studies), populations can be grouped into two broad categories in which outcomes were assessed: individuals who were directly impacted and those who were indirectly impacted. We defined the population of interest in the included studies as those populations for whom outcomes were reported.
Directly impacted individuals
Directly impacted individuals included students, teachers, and staff of schools assessed in the included studies. Most studies (n = 25) assessed students as the main population (Anchordoqui 2020; Buonsenso 2020; Burns 2020; Campbell 2020; Cohen 2020; Curtius 2020; Ehrhardt 2020; Espana 2020; Gandolfi 2020; Gill 2020; Head 2020; Johnson 2020; Keeling 2020; Kraay 2020; Landeros 2020; Macartney 2020; Munday 2020; NCIRS 2020; Otte Im Kampe 2020; Phillips 2020; Simonsen 2020; Sparks 2020a; Sparks 2020b; Stein‐Zamir 2020; Yoon 2020). Teachers (n = 17) (Buonsenso 2020; Campbell 2020; Cohen 2020; Curtius 2020; Espana 2020; Gill 2020; Head 2020; Johnson 2020; Keeling 2020; Macartney 2020; NCIRS 2020; Otte Im Kampe 2020; Phillips 2020; Sparks 2020a; Sparks 2020b; Stein‐Zamir 2020; Yoon 2020), and school staff (n = 14) (Buonsenso 2020; Campbell 2020; Cohen 2020; Gill 2020; Johnson 2020; Keeling 2020; Macartney 2020; NCIRS 2020; Otte Im Kampe 2020; Phillips 2020; Sparks 2020a; Sparks 2020b; Stein‐Zamir 2020; Yoon 2020), were usually assessed as a subpopulation together with students. In eight studies, authors looked at students only, without considering teachers and other school staff (Anchordoqui 2020; Burns 2020; Ehrhardt 2020; Gandolfi 2020; Kraay 2020; Landeros 2020; Munday 2020; Simonsen 2020).
Indirectly impacted individuals
Under indirectly impacted individuals, four studies assessed the wider community with direct links to schools (Head 2020; Johnson 2020; Otte Im Kampe 2020; Phillips 2020). Most modelling studies examined the broader population (e.g. the entire population of a city, state or country). In 23 studies, the population of interest was the general population of all ages in the respective country or state; two studies focused on all pediatric cases within the general population (Macartney 2020; Yoon 2020).
Settings
Most included studies assessed interventions in more than one school setting (i.e. primary education, secondary education). Three studies focused on secondary schools only (Curtius 2020; Panovska‐Griffiths 2020a; Stein‐Zamir 2020). Schools were often considered as one of multiple settings in which measures were implemented; in such studies, authors evaluated, for example, the impact of reopening of schools alongside other population‐based measures on broad health outcomes (e.g. cases or hospitalisation in the general population).
Context
Of the studies that were conducted in real‐world contexts or that used real data from a given country, 20 used data from the WHO European region (EUR), 13 from WHO region of the Americas (PAH; Anchordoqui 2020; Bracis 2020; Burns 2020; Campbell 2020; Cohen 2020; Espana 2020; Gill 2020; Head 2020; Johnson 2020; Keskinocak 2020; Landeros 2020; Monod 2020; Phillips 2020), six from the WHO Western Pacific region (WPR; Kim 2020; Macartney 2020; McBryde 2020; NCIRS 2020; Yoon 2020; Zhang 2020), and one from WHO Eastern Mediterranean Region (EMR; Stein‐Zamir 2020). One study that looked at indicators for reopening conducted a global assessment (Gandolfi 2020); one study did not report on a country to which the findings are applicable or from which data were used to validate the model (Kraay 2020). Figure 5 illustrates the geographical distribution of where studies were conducted or from which data were used.
5.
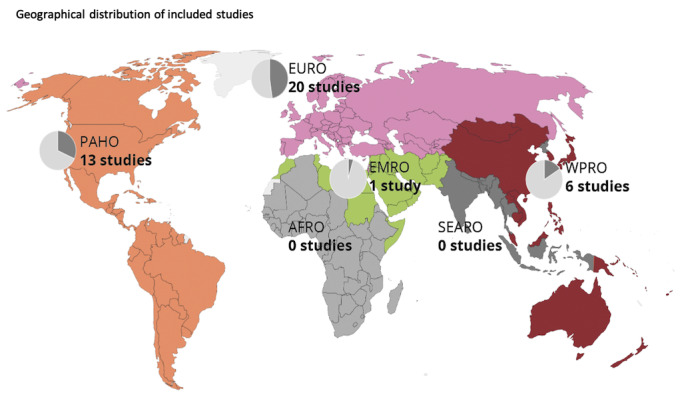
The geographical distribution of where studies occurred or from where data were drawn, categorized using the WHO world region categorization.
Abbreviations: AFRO: African Region; EMRO: Eastern Mediterranean Region; EURO: European Region; PAHO: Region of the Americas; SEARO: South‐East Asian Region; WPRO: Western Pacific Region.
Note: total number of studies included is 42; one study conducted a global assessment (Buonsenso 2020); one study did not report on a country from which data were use to validate the model or to which the findings are applicable (Keeling 2020)
Most included studies did not report explicitly on contextual factors. Instead, relevant factors such as geographical phenomena (e.g. weather conditions (Sparks 2020a; Stein‐Zamir 2020)), transportation to school (Stein‐Zamir 2020), political issues (e.g. regulations around class size (Kim 2020; Stein‐Zamir 2020)), duration of school hours (Kim 2020; Stein‐Zamir 2020), acceptance of non‐pharmaceutical interventions, and epidemiological factors (e.g. burden of disease in the respective communities) were described by the study authors as potentially mediating the successful implementation of measures. Factors relating to the physical environment of the school, such as classroom size and space for outdoor activities, were also reported as determinants of the successful implementation of measures (Kraay 2020; Stage 2020; Stein‐Zamir 2020).
Interventions
Included studies fell into three broad intervention categories: organizational measures to reduce transmission of SARS‐CoV‐2, structural and environmental measures to reduce transmission of SARS‐CoV‐2, and surveillance and response measures in relation to SARS‐CoV‐2 infections. This categorization was an adaptation made to our a priori logic model based on factors emerging from the data. Our a priori logic model (Figure 1), assumed that interventions could take place on a number of different levels, including the macro level, the school level, the cohort level, or the individual level. Most studies that clearly reported the level on which the intervention was implemented examined the macro or school level, with measures targeting cohorts or individuals being much less reported. Measures assessed in modelling studies lacked details with regards to the level or levels targeted.
Organizational measures to reduce transmission of SARS‐CoV‐2
The impact of organizational measures to reduce transmission of SARS‐CoV‐2 was assessed or modelled in 36 studies (Anchordoqui 2020; Balabdaoui 2020; Bracis 2020; Buonsenso 2020; Burns 2020; Cohen 2020; Coletti 2020; Di Domenico 2020; Ehrhardt 2020; Espana 2020; Gill 2020; Head 2020; Isphording 2020; Johnson 2020; Keeling 2020; Keskinocak 2020; Kim 2020; Kraay 2020; Landeros 2020; Macartney 2020; McBryde 2020; Monod 2020; Munday 2020; NCIRS 2020; Otte Im Kampe 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Panovska‐Griffiths 2020c; Phillips 2020; Simonsen 2020; Sparks 2020a; Sparks 2020b; Stage 2020; Stein‐Zamir 2020; Yoon 2020; Zhang 2020). This category describes two types of measures: measures to make contacts safer and measures to reduce the opportunity for contact.
Measures to make contacts safer included interventions such as face mask policies, hand hygiene policies, respiratory etiquette, general physical distancing policies, as well as the modification of activities to reduce the risk of transmitting SARS‐CoV‐2 (e.g. not singing in music classes (Isphording 2020; Yoon 2020)).
Measures to reduce the opportunity for contact included staggered arrival, break and departure times (Isphording 2020), alternating attendance (e.g. daily or weekly rotations (Head 2020)), phased reopening of schools (e.g. small cohort of students returning initially (Stage 2020)), formation of cohorts (e.g. bubbles or pods to which specific students are assigned), cancellation of activities (e.g. physical education classes) and stay‐at‐home policies for sick students and staff.
Four studies were unspecific about what actual measures the models represented, and instead modelled a reduction in contacts within the target population (Balabdaoui 2020; Coletti 2020; Kim 2020; Monod 2020).
Structural and environmental measures to reduce transmission of SARS‐CoV‐2
The impact of structural and environmental measures to reduce transmission of SARS‐CoV‐2 was assessed or modelled in 11 studies (Curtius 2020; Ehrhardt 2020; Isphording 2020; Johnson 2020; Kraay 2020; Landeros 2020; McBryde 2020; NCIRS 2020; Otte Im Kampe 2020; Sparks 2020a; Yoon 2020). These studies evaluated structural changes implemented to facilitate physical distancing (e.g. school yard division (Isphording 2020)), distance between desks (Isphording 2020), removal of furniture (Sparks 2020a), enhancements or changes to ventilation systems (Curtius 2020; Ehrhardt 2020; Isphording 2020; Johnson 2020), and enhancements to cleaning regimens (Ehrhardt 2020; Isphording 2020; Kraay 2020; NCIRS 2020; Sparks 2020a).
Surveillance and response measures in relation to SARS‐CoV‐2 infections
Nineteen studies assessed or modelled surveillance and response measures in relation to SARS‐CoV‐2 infections. Surveillance measures included testing, tracing, and symptom screening (e.g. fever screening). Response measures included isolation of confirmed cases (Burns 2020; Di Domenico 2020), quarantine of suspected cases and contacts of confirmed and suspected cases (Buonsenso 2020; Head 2020; Isphording 2020; Kim 2020; Macartney 2020; NCIRS 2020), and reactive school closures (Garchitonerena 2020; Johnson 2020). Overall, however, policies about response measures were rarely reported. One study reported on a policy in which, upon detection of a positive case, relevant groups were immediately quarantined, with other groups remaining in school and being closely monitored for additional new cases (Isphording 2020). Management of symptomatic cases was also heterogeneous, including quarantining symptomatic cases for 14 days (Isphording 2020), and symptom‐based isolation for one or a few days only (Burns 2020).
Co‐interventions assessed or reported in the studies were surveillance and response, travel/mobility restrictions, workplace reopening/closing, operation of businesses, limitations on gatherings, number of people in closed public spaces, and general measures making contacts safer (e.g. masks, hand hygiene, physical distance). These measures were implemented on the macro (i.e. national, regional) or meso (i.e. community) level.
Outcomes
The outcomes assessed in the included studies mostly fall into four broad subcategories: transmission‐related outcomes, healthcare utilization, other health outcomes and societal, economic, and ecological implications. This categorization corresponds well to our a priori logic model (Figure 1), with healthcare utilization being the only broad outcome category not prespecified in the model. The outcome category most commonly addressed by the body of literature was transmission‐related outcomes (assessed in 38 studies), followed by healthcare utilization (assessed in 10 studies (Balabdaoui 2020; Bracis 2020; Coletti 2020; Di Domenico 2020; Espana 2020; Head 2020; Keeling 2020; Sneppen 2020; Stage 2020; Stein‐Zamir 2020)), societal, economic and ecological outcomes (assessed in 5 studies (Campbell 2020; Cohen 2020; Gandolfi 2020; Gill 2020; Phillips 2020)), and other health outcomes (assessed in 4 studies (Keeling 2020; McBryde 2020; Simonsen 2020; Sparks 2020a)).
Transmission‐related outcomes
Within the transmission‐related outcomes, studies assessed the number or proportion of cases (n = 29), the reproduction number R (n = 12) Balabdaoui 2020; Bracis 2020; Brooks‐Pollock 2020; Cohen 2020; Keeling 2020; Kraay 2020; Landeros 2020; McBryde 2020; Monod 2020; Panovska‐Griffiths 2020b; Phillips 2020; Zhang 2020), the number or proportion of deaths (n = 10; Balabdaoui 2020; Bracis 2020; Cohen 2020; Espana 2020; Head 2020; Keeling 2020; Keskinocak 2020; Monod 2020; Panovska‐Griffiths 2020b; Panovska‐Griffiths 2020c), the temporal development of the epidemic (n = 3; Johnson 2020; Keskinocak 2020; Landeros 2020), or the probability of an infection (n = 2; Anchordoqui 2020; Sparks 2020b). Other outcomes in that category were, for example, number of outbreaks in school settings (Otte Im Kampe 2020), number of schools infected (Sparks 2020b), or the concentration of aerosol particles containing virus RNA within a room (Curtius 2020).
Healthcare utilization
For healthcare utilization, studies frequently reported the number or proportion of hospitalizations (n = 8), followed by the number or proportion of cases requiring intensive care (n = 3).
Other health outcomes
Among other health outcomes, we encountered outcomes related to health behaviours, such as contact rates (n = 3; Sparks 2020a; Keeling 2020; McBryde 2020), and physical health (n = 1; Simonsen 2020), such as prevalence and risk of hand eczema.
Societal, economic, and ecological outcomes
Only five studies assessed outcomes included in the societal, economic, and ecological outcomes category. These can be captured by two subcategories, namely economic and educational implications. Outcomes assessing economic implications included cost, human resources and capacity (n = 1; Campbell 2020). For educational implications, reported outcomes primarily related to school attendance (n = 4; Cohen 2020; Gandolfi 2020; Gill 2020; Phillips 2020), including the number of remote teaching days and the number of days lost due to school closure.
Implementation
Overall, the studies did not report rich details on implementation of the respective measures. With regards to implementation outcomes, adherence and fidelity to the intervention were commonly mentioned as critical mediating factors for the effectiveness of a measure. In modelling studies, authors modelled aspects of implementation, such as country‐level variation in response efficacy, adherence to different measures, testing capacities and the diagnostic test accuracy of measures implemented for screening (e.g. fever screening). Adherence and fidelity to measures (e.g. guidelines) were assessed or mentioned in the observational/epidemiological and experimental/quasi‐experimental studies.
With regard to those implementing the interventions (i.e. implementation agents), four groups emerged as being important: agents on the national or subnational level (i.e. (public) health authorities, policy‐makers, ministry of education), agents in the school setting (i.e. school staff (e.g. headmasters, teachers, administrative staff), students), as well as agents outside of the school setting (i.e. healthcare professionals (Campbell 2020), (public) health officials).
We identified very little information on strategies used to implement an intervention (e.g. enforcement). Only one study reported enforcement strategies for surveillance measures, such as remote monitoring of isolation, penalty for non‐compliance, help in maintaining home isolation as well as provision of thermometers for screening. With regards to implementing guidelines issued by health authorities, two studies reported difficulties considering the interpretation and implementation of guidelines with regards to the dose and prevention of adverse effects of handwashing (Simonsen 2020; Sparks 2020a).
Discussion
Summary of results
In this scoping review, we identified 42 studies and provide a broad overview of the currently available evidence related to the impact of measures implemented in the school setting to safely reopen schools or keep schools open, or both, during the SARS‐CoV‐2/COVID‐19 pandemic. This review does not report on the effectiveness of these measures. In this section, we describe the identified study base as well as important gaps.
The geographical spread of these studies shows that research is not distributed equally across the globe. Most of the studies were either conducted in or modelled on data for countries in the WHO‐EUR and WHO‐PAH. While there were some studies from the WHO‐WPR and WHO‐EMR, there was a stark absence of studies from the WHO South‐East Asia Region (WHO‐SEAR) and the WHO African Region (WHO‐AFR). Except for one Chinese study (Zhang 2020), no studies were conducted in low‐ and middle‐income countries. Studies often took a broad population perspective, assessing the impact of school measures at the population level (e.g. for an entire city, state or country). In studies looking specifically at in‐school populations, most assessed students as a broad group ranging from approximately five to 18 years of age. While this broad age category provided some insight into how school measures can be implemented across entire schools, such broad categorizations do not allow for understanding of unique issues that might apply to only certain age groups. Indeed, the impact of these school measures may affect children, adolescents, and teenagers differently, and understanding the impact of school measures across different age groups would be useful for decision makers and implementers. Relatively few studies assessed the impact of measures on directly affected populations, such as students, teachers, school staff, relatives and other close contacts, which is partly attributable to the study type (i.e. modelling studies) and to the fact that measures implemented in the school setting are often implemented to reduce SARS‐CoV‐2 transmission in the community.
Most studies evaluated or modelled the impact of organizational measures to reduce transmission of SARS‐CoV‐2. These measures aimed to either make contacts safer or to reduce the opportunity for contact. Many of the included modelling studies that assessed these measures assumed reduced levels of contact within schools, and attributed this to coverage of, and adherence to, the measures. They therefore did not assess direct impact of the measures on SARS‐CoV‐2 transmission, and instead described the consequences of reopening schools with reduced transmission rates and assumed that this reduction had occurred due to the measures they described. Relatively few studies focused on structural/environmental measures and surveillance and response measures. Most studies also considered the presence (and sometimes varying intensity) of other non‐school‐related co‐interventions, which also seek to contain the SARS‐CoV‐2 pandemic. These co‐interventions included restrictions on mobility, social distancing policies, bans on mass gatherings, and the reopening (and reclosing) of workplaces.
The mapping clearly showed that school measures are mostly assessed with regards to their potential to reduce transmission of SARS‐CoV‐2. A much smaller proportion of studies looked at other outcomes of interest, including other health outcomes and societal, economic and ecological outcomes. For example, none of the included studies assessed the economic implications in parents or caretakers (e.g. job loss, loss of income). Also, no studies looked at the effect of these measures on the psychosocial well‐being and mental health of students, teachers and other school staff.
Studies were inconsistent in their consideration and reporting of context and implementation that may be critical in understanding whether measures implemented in schools are effective or not. Regarding the stage of the pandemic, most studies assessed the implementation of measures in schools when the burden of SARS‐CoV‐2 infections was comparatively low, that is, after the large surges seen between February and May 2020. Further, most studies did not discuss equity and the differences in implementation of interventions in high‐, middle‐, and low‐income settings. Indeed, most of the studies presented, used data from, or were focused on, high‐income countries, but regional differences, or even school‐level differences relating to socio‐economic status might heavily influence how interventions are implemented and taken up, and this was rarely commented on within the identified studies. This is important, as many of the interventions described would require financial resources, and the availability of space for effective implementation.
Most studies used mathematical models to approximate the impact of the implementation of a given school measure on the population of interest. The methods used in these modelling studies ranged widely, and each needs to be considered in the context of the specific assumptions and decisions made when constructing and applying the model. Few included studies can be considered ‘real‐world’ studies, meaning that they evaluate the impact of a measure implemented in a real school on a real population. The few studies of this nature tended to be descriptive, which precludes making robust inferences about effectiveness.
The conceptualization of this scoping review was informed by an a priori logic model. Throughout the extraction and mapping process, we combined the broad categories developed a priori and inductively developed subcategories. The a posteriori logic model thus reflects the areas within the wider school system that are currently assessed by scientific studies. Comparing the two logic models, several adaptations emerged. First, we collapsed the four population groups into broader population groups due to the types of populations encountered in the included studies. Moreover, our conceptualization of intervention changed substantially throughout the reflective‐analytic process. With regards to outcomes, a new category (healthcare utilization) emerged; while this was captured in the a priori model, it emerged as its own category after analysis. There were minor changes in the co‐intervention box as well as in the context categories reflective of the encountered evidence, while there were no changes to the implementation aspects included in the a priori logic model.
Strengths and limitations
While we endeavoured to conduct a rapid scoping review that followed published guidance, (Arksey 2005; Munn 2018), we faced a number of challenges and limitations. First, although we developed and registered the protocol on the Open Science Framework (Pfadenhauer 2020), the studies that we identified indicated that we needed to adapt the protocol in two important ways. First, many of the studies that we identified assessed the impact of measures implemented within the school on transmission within the broader community or even within the general population, even if they did not have any direct connection with the school setting. Our initial criterion indicated excluding populations that were not impacted by measures implemented in the school setting, so we added the general population to the indirectly impacted populations so that we would capture the studies looking at broader population impacts. Another adaptation that we made to the protocol was that we extended our snowball searches by snowballing not only reviews, but also guidelines to avoid missing any relevant reports that might have been citing or cited by the guideline. The studies we identified via snowballing were either reports or preprints that were published after we ran our searches (Buonsenso 2020; Isphording 2020; Panovska‐Griffiths 2020a), or publications published in journals not indexed in any of the covered databases (Gandolfi 2020; Gill 2020).
Another limitation to our review is that we limited the setting to primary and secondary schools, and therefore did not consider early childhood or university settings. These settings are important in their own right, however, given the differences in the ages of these target groups and the non‐compulsory nature of childcare and education in these settings, the measures chosen and their implementation modalities are likely to be different. School closures triggered by criteria outside of the school setting, for example, where schools are closed because the level of transmission within a community, city, or larger geographical region crosses a certain threshold, have been in the past, and may continue to be a relevant policy instrument. However, given that the relevant trigger is not embedded within the school context, we did not consider such measures. Additionally, existing and ongoing systematic reviews have investigated the effectiveness of general school closures (Viner 2020a), as well as their short‐ and long‐term impacts (Xu 2020).
Our searches were limited to databases concerned primarily with health, thus we might have missed a body of literature focused on social, economic and educational outcomes. We also did not consider Chinese databases and might therefore have missed Chinese language studies.
There were also some limitations to the studies that we identified, which made screening for eligibility challenging. We emphasized quality assurance throughout the review process, by developing guidance for all key steps, by calibrating the screening and extraction forms, as well as by maintaining a register of rolling questions and by taking time for multiple reflective discussions within the team, often on a daily basis. We conducted both screening stages in duplicate, and an experienced review author checked all data extractions in full. Multiple individuals undertook the mapping of the data, with several group discussions to ensure that categories were clear, consistent and accurately reflected the content of the studies. Making decisions with regards to eligibility and subsequent data extraction was challenged by a lack of reporting. In particular with regards to measures such as school closures, study authors provided little detail on whether or not they were assessing proactive or reactive school closures. All borderline cases were discussed within the team and then decided upon. Lastly, the majority of the studies included in this review are preprints, which did not undergo peer review.
Authors' conclusions
Implications for a subsequent effectiveness review
While this scoping review did not set out to answer the question of which school measures are effective in reducing transmission within and beyond the school setting, it provides a systematic overview of the body of literature with regards to study types, populations, interventions, settings and outcomes. In a next step, we plan to perform a full evidence synthesis on the evidence base most informative for decision makers, whether that is on the full body of evidence or a specific subset. Regardless of the specific question, there will be some issues as well as challenges accompanying the synthesis of this evidence base that will need to be considered when moving forward. These issues and challenges are related both to the existing (and upcoming) evidence base, as well as the dynamic nature of the SARS‐CoV‐2 pandemic. In order to provide an overview of the evidence base, at this stage, we mapped each study against a number of types of interventions. For some types of interventions, e.g. measures to make contacts safer, multiple specific interventions may have been implemented ‐ mask policy, hand hygiene policies, etc. Although we have not teased these apart completely to the specific individual interventions and components in such cases, we will do so in conducting the subsequent rapid review.
With regard to the identified evidence base, most of the studies are mathematical modelling studies, and the extent to which these can approximate the real world varies. Many of the included modelling studies, for example, assessed a hypothetical reduction of contacts to mimic an intervention implemented in a school setting; however, the question of how such a reduction in contacts can be accomplished in real life remains unresolved. Additionally, the quality of the included modelling studies varies widely. How to determine which types of modelling studies are most informative, as well as how to appraise, summarize and synthesize these in a meaningful way will require careful consideration. The inclusion, summary and synthesis of observational studies, although much closer to the ‘real world’ in design and conduct, is also subject to challenges. Such studies are often descriptive in nature; although these may be informative in describing the situation as it unfolds, they may not allow conclusions to be drawn about the effectiveness of a particular measure (Grimes 2002). Experimental and quasi‐experimental studies represent a strong option for evaluating the effectiveness of such population‐level measures (Bärnighausen 2017), however given the difficulty of designing and conducting such studies during an ongoing pandemic only few have been conducted to date.
Concerning the identified gaps, it would be advisable to extend the number and types of databases searched. The surprising lack of evidence from specific regions clearly points towards databases with a different geographical scope (e.g. Chinese Biomedical Literature (CBM), Latin American and Caribbean Health Sciences Literature (LILACS)). With regards to the limited number of societal, educational, economic and ecological outcomes we encountered, it would be beneficial to add topic‐specific databases (e.g. EconLit, Scopus or PsycINFO). Considering the relatively high percentage of studies identified through snowballing, it is moreover highly recommended to conduct extensive supplemental or grey literature searching.
Additionally, as the questions relevant to decision makers change, the research being conducted will likely change to reflect this. Taking experimental and quasi‐experimental studies as an example: whereas only few are currently available, as more schools aim to open safely and remain open, more such studies will likely become available. This highlights the importance of rapid evidence syntheses that can deliver answers in a compressed time frame, yet also remain up to date, either through frequent updates or the conduct of a living evidence synthesis.
Implications for research and practice
There is an urgent need for empirical research assessing the effectiveness of measures to reduce contacts and to make contacts safer within the school setting. While modelling studies provide insights into the potential effect of contact reductions, they do not provide real‐world evidence on how this can be achieved and the multiple consequences for health and society this entails.
We touched upon context and implementation as influential factors. While we flagged qualitative studies during screening, it was beyond the scope of this scoping review to systematically assess these studies in depth. We suspect, however, that assessing these studies in a more systematic manner would create meaningful insights that should be considered by decision makers alongside considerations of effectiveness.
There are also challenges related to conducting high‐quality research during a pandemic. The pandemic is dynamic in nature with significant temporal and geographical variation, with the situation between and within countries, but also within different regions, cities and potentially even neighbourhoods within a country, changing fast and in an unpredictable manner. The specific circumstances under which research is conducted, for example, current levels of transmission and active co‐interventions, are critical in determining what measures work.
This dynamic nature also implies that the current questions of relevance to decision makers may change over the next months. How vaccinations influence what measures are most appropriate in schools, for example, is currently not being discussed; soon, however, as vaccines become available, this will likely become a question of critical relevance. This highlights the importance of the regular involvement of relevant stakeholders in defining research questions of relevance – both on a primary and secondary level.
What's new
| Date | Event | Description |
|---|---|---|
| 21 December 2020 | Amended | CEO‐sys added to Acknowledgements |
History
Review first published: Issue 12, 2020
Acknowledgements
We would like to acknowledge the support of the COVID‐19 evidence ecosystem (CEO‐sys) project, funded by the German Federal Ministry of Education and Research.
We would like to acknowledge valuable peer reviews from Martin Weber (World Health Organization Regional Office for Europe), Susan E Coffin (Division of Infectious Diseases, Children’s Hospital of Philadelphia, Division of Disease Control, Philadelphia Department of Public Health, Philadelphia, PA, USA) and Susanne Carai (Universitaet Witten/Herdecke and World Health Organization Regional Office for Europe). We are extremely grateful to Robin Featherstone (Information Specialist, Cochrane Editorial and Methods Department) for having designed and executed our searches and Ruth Foxlee (Information Specialist, Cochrane Editorial and Methods Department) for peer reviewing the searches. Thanks to ARGO for comments on the Abstract, Chantelle Garritty and Kayleigh Kew (Methods Editors, Cochrane Editorial and Methods Department), Lisa Bero (Network Senior Editor, Cochrane Public Health and Health Communications Network), Luke Wolfenden (Co‐ordinating Editor, Cochrane Public Health), Jodie Doyle (Managing Editor, Cochrane Public Health), Helen Wakeford and Clare Dooley (Managing Editors, Cochrane Editorial and Methods Department). Special thanks to Denise Mitchell for copy‐editing the review and Nicole Pitcher for writing the Plain Language Summary.
Appendices
Appendix 1. Search strategy and results
Database: Ovid MEDLINE(R) ALL 1946 to 2 October 2020
Date search conducted: 8 October 2020
Strategy:
1 Coronavirus/ (3713)
2 Coronavirus Infections/ (31302)
3 COVID‐19.rs. (26503)
4 severe acute respiratory syndrome coronavirus 2.os. (22499)
5 (2019 nCoV or 2019nCoV or 2019‐novel CoV).tw,kf. (1174)
6 (corona vir* or coronavir* or neocorona vir* or neocoronavir*).tw,kf. (35720)
7 COVID.mp. (55300)
8 COVID19.tw,kf. (669)
9 (nCov 2019 or nCov 19).tw,kf. (86)
10 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").mp. (18201)
11 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").mp. (25853)
12 or/1‐11 [Set 1: SARS‐CoV‐2] (72085)
13 School Teachers/ (1517)
14 Schools/ (38621)
15 Students/ (59533)
16 ((campus* or class* or employee* or pupil* or staff* or student$1 or teacher$1) adj3 (college$1 or elementary or junior or middle* or primary or secondary)).tw,kf. (53786)
17 educational setting$1.tw,kf. (1527)
18 (gradeschool* or highschool* or kindergarten* or school* or schoolbus*).tw,kf. (294854)
19 or/13‐18 [Set 2: Primary or secondary school settings] (366883)
20 and/12,19 [Sets 1 & 2] (929)
21 ((clos* or open* or re entry or re open* or re start* or reopen* or restart* or resum* or suspen*) and (highschool$1 or kindergarten* or school$1)).ti. (815)
22 20 or 21 [Concept searches combined with specific title search] (1658)
23 limit 22 to "humans only (removes records about animals)" (1654)
24 limit 23 to yr="2020‐Current" (916)
25 remove duplicates from 24 (915)
Database: Ovid Embase 1974 to 7 October 2020
Date search conducted: 8 October 2020
Strategy:
1 coronaviridae/ (1017)
2 exp coronavirinae/ (19921)
3 exp coronavirus infection/ (21317)
4 (2019 nCoV or 2019nCoV or 2019‐novel CoV).ti,ab,kw. (1140)
5 (corona vir* or coronavir* or neocorona vir* or neocoronavir*).ti,ab,kw. (35715)
6 COVID.af. (52458)
7 COVID19.ti,ab,kw. (637)
8 (nCov 2019 or nCov 19).ti,ab,kw. (57)
9 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").af. (17487)
10 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").af. (17097)
11 or/1‐10 [Set 1: SARS‐CoV‐2] (82429)
12 elementary student/ (1502)
13 high school/ (20605)
14 high school student/ (7857)
15 kindergarten/ (2845)
16 middle school/ (1776)
17 middle school student/ (1363)
18 primary school/ (12778)
19 *school/ (17776)
20 school teacher/ (1574)
21 *student/ (26541)
22 ((campus* or class* or employee* or pupil* or staff* or student$1 or teacher$1) adj3 (college$1 or elementary or junior or middle* or primary or secondary)).ti,ab,kw. (66174)
23 educational setting$1.ti,ab,kw. (1772)
24 (gradeschool* or highschool* or kindergarten* or school* or schoolbus*).ti,ab,kw. (354198)
25 or/12‐24 [Set 2: Primary or secondary school settings] (424031)
26 and/11,25 [Sets 1 & 2] (905)
27 ((clos* or open* or re entry or re open* or re start* or reopen* or restart* or resum* or suspen*) and (highschool$1 or kindergarten* or school$1)).ti. (608)
28 26 or 27 [Concept searches combined with specific title search] (1429)
29 (animal experiment/ or exp animal/) not exp human/ (4990006)
30 28 not 29 (1420)
31 limit 30 to yr="2020‐Current" (795)
32 remove duplicates from 31 (779)
Database: Cochrane COVID‐19 Study Register
URL:covid-19.cochrane.org (searched via the Cochrane Register of Studies: crsweb.cochrane.org)
Date search conducted: 8 October 2020
Strategy:
#1. ((campus* OR class* OR employee* OR pupil* OR staff* OR student* OR teacher*) ADJ3 (college* or elementary OR junior OR middle* OR primary OR secondary)):TI,AB (90)
#2. (educational NEXT setting*):TI,AB (2)
#3. (gradeschool* OR highschool* OR kindergarten* OR school* OR schoolbus*):TI,AB (379)
#4. #1 OR #2 OR #3 (443)
Contents note: The Cochrane COVID‐19 Study Register contains study references from ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), PubMed, Embase.com, medRxiv and other hand‐search articles from publishers' websites.
Database: WHO COVID‐19 Global literature on coronavirus disease
URL:search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov
Date search conducted: 8 October 2020
Strategy:
(tw:(school* AND (elementary OR grade* OR high* OR junior OR kindergarten* OR middle* OR primary OR secondary))) OR (tw:(highschool*)) (926)
Contents note: The WHO Global COVID‐19 Health literature database contains primarily research (published AND/OR pre‐publication) journal articles from PubMed, Web of Science, Global Index Medicus, Embase. In addition, Lanzhou University submits on a daily basis citations from CNKI as well as a number of Chinese journal publishers.
Source: CDC COVID‐19 Research Articles Downloadable Database, current to 8 October 2020
Subset searched via EndNote: 11,507 preprints from bioRxiv (n = 1849), medRxiv (n = 7101) and SSRN (n = 2557)
URL: www.cdc.gov/library/researchguides/2019novelcoronavirus/researcharticles.html
Date search conducted: 8 October 2020
Strategy:
1. Title Contains "school", Or Title Contains "highschool" (66)
2. Any field Contains "school", AND Any field Contains "student" (46)
3. Any field Contains "school", AND Any field Contains "teacher" (15)
4. Any field Contains "school", AND Any field Contains "transmi" (175)
5. Any field Contains "educational setting" (4)
6. Any field Contains "kindergarten" (9)
[or/1‐6] (227)
Source: Google
URL: www.google.com
Date search conducted: 8 October 2020
Strategy:
Search 1
(coronavirus | covid | SARS‐CoV‐2) (children | pupil | staff | student | teacher) ("educational setting" | "educational settings" | gradeschool | highschool | kindergarten | school)
Searched the first 10 pages of results (n = 100)
Kept 41
Appendix 2. Data extraction form
Study information
Study ID
Study title
Publication year
Study source (journal, report, preprint publication)
For preprint publication only: date of publication
Study design
Study type (e.g. modelling study, cross‐sectional study, econometric study)
Data type (e.g. modelling vs. observational data)
Verbal summary of study (e.g., stochastic discrete event simulation model)
Comments
Population and setting
-
Population group targeted by intervention (students, teaching staff, school staff, parents, other family members, other individuals outside school)
Type of population (i.e. students vs. teachers vs. school staff)
Age
Risk profile (e.g. elevated risk of infection, adverse health effects due to COVID‐19, students with special learning needs, students from disadvantaged families)
Characteristics of school (e.g. socio‐economic status of school location or student’s families, catchment area)
Study setting (e.g., primary school, high school, other school forms)
Comments
Intervention
-
Broad measure category
Organizational measures to reduce transmission of SARS‐CoV‐2,
Structural/environmental measures to reduce transmission of SARS‐CoV‐2, and
Surveillance and response measures in relation to SARS‐CoV‐2 infections
Verbal summary of the measures
Duration of the intervention
Level of intervention (i.e. individual, cohort, school, macro, multiple)
Comments
Implementation
Implementation outcomes (e.g. adherence, fidelity)
Implementation strategies (e.g. enforcement, communication and feedback)
Implementation agents (e.g. parents, teachers, bus drivers)
Context
Country in which measure is implemented
Geographical, socio‐cultural, socio‐economic, ethical, political, legal, and epidemiological context on the macro (e.g. international, national or state level) and meso level (e.g. community)
Co‐interventions
Time point of intervention (use WHO database to determine disease burden at that time)
Comments
Outcomes (repeated for each outcome)
-
Outcome category
Transmission‐related outcomes,
Healthcare utilization,
Other health outcomes and
Societal, economic, and ecological implications.
Description of outcome
Outcome attributable to measures (yes/no)
Level on which outcome is assessed (i.e. students, teachers, staff, wider community, general population)
Length of follow‐up
Estimate related to the impact of measure(s) implemented in the school setting
Summary of overall impact of measure(s) implemented in the school setting
Comments
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anchordoqui 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: students Setting: primary school |
|
| Interventions | Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: not reported |
|
| Notes | ||
Balabdaoui 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Switzerland WHO region: EURO Participants: general population Setting: not reported |
|
| Interventions |
Organizational Measures reducing opportunity for contacts (unspecified) |
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 5 months |
|
| Notes | ||
Bracis 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: general population Setting: not reported |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: until December 2020 |
|
| Notes | ||
Brooks‐Pollock 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: general population Setting: primary school |
|
| Interventions |
Organizational
Surveillance measures
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 25 weeks |
|
| Notes | ||
Buonsenso 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Italy WHO region: EURO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: ~ 1 month |
|
| Notes | ||
Burns 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: students Setting: primary school |
|
| Interventions |
Organization
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: not reported |
|
| Notes | ||
Campbell 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Canada WHO region: PAHO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Surveillance
|
|
| Outcomes |
Economic outcomes
Follow‐up: no time limit |
|
| Notes | ||
Cohen 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: King County, WA, USA WHO region: PAHO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Organization
Surveillance measures
|
|
| Outcomes |
Transmission‐related outcomes
Educational outcomes
Follow‐up: various, up to 3 months |
|
| Notes | ||
Coletti 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Belgium WHO region: EURO Participants: general population Setting: not reported |
|
| Interventions |
Organizational
|
|
| Outcomes |
Healthcare utilization
Follow‐up: 3.5 months |
|
| Notes | ||
Curtius 2020.
| Study characteristics | ||
| Methods | Inferential Modelling/experimental |
|
| Participants | Country: Germany WHO region: EURO Participants: students, teachers Setting: secondary school |
|
| Interventions |
Structural/environmental
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 2 h |
|
| Notes | ||
Di Domenico 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Ile‐de‐France, France WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: 2 months |
|
| Notes | ||
Ehrhardt 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Germany WHO region: EURO Participants: students Setting: primary school, secondary school |
|
| Interventions |
Organizational
Structural/environmental
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 3 months |
|
| Notes | ||
Espana 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Indiana, USA WHO region: PAHO Participants: students, teachers Setting: not reported |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
|
|
| Notes | ||
Gandolfi 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: all countries WHO region: global Participants: students Setting: not reported |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Educational outcomes
Follow‐up: 2 months |
|
| Notes | ||
Garchitonerena 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: 32 European countries WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: various, up to 5 months |
|
| Notes | ||
Gill 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Pennsylvania, USA WHO region: PAHO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Educational outcomes
Follow‐up: not reported |
|
| Notes | ||
Head 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: San Francisco Bay Area, USA WHO region: PAHO Participants: students, teachers, community Setting: primary school, secondary school |
|
| Interventions |
Organization
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: 4 months |
|
| Notes | ||
Isphording 2020.
| Study characteristics | ||
| Methods | Inferential Experimental |
|
| Participants | Country: Germany WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Structural/environmental
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 3 months |
|
| Notes | ||
Johnson 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: students, teachers, staff, community Setting: primary school, secondary school |
|
| Interventions |
Organization
Structural/environmental
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 4 months |
|
| Notes | ||
Keeling 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Other health outcomes
Follow‐up: not reported |
|
| Notes | ||
Keskinocak 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Georgia, USA WHO region: PAHO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: various; 3‐3.5 months |
|
| Notes | ||
Kim 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Korea WHO region: WPRO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 2 months |
|
| Notes | ||
Kraay 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: not reported WHO region: not reported Participants: students Setting: not reported |
|
| Interventions |
Organizational
Structural/environmental
|
|
| Outcomes |
Transmission‐related outcomes:
Follow‐up: not reported |
|
| Notes | ||
Landeros 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: students Setting: primary school, secondary school |
|
| Interventions |
Organizational
Structural/environmental
Surveillance measures
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 24 weeks |
|
| Notes | ||
Macartney 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Australia WHO region: WPRO Participants: students, teachers, staff, general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 30 weeks |
|
| Notes | ||
McBryde 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Australia WHO region: WPRO Participants: general population Setting: not reported |
|
| Interventions |
Organizational
Structural/environmental
|
|
| Outcomes |
Transmission‐related outcomes
Other health outcomes
Follow‐up: not reported |
|
| Notes | ||
Monod 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: USA WHO region: PAHO Participants: general population Setting: primary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 90 days |
|
| Notes | ||
Munday 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: students Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: not reported |
|
| Notes | ||
NCIRS 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Australia WHO region: WPRO Participants: students, teachers, staff Setting: primary school, secondary school |
|
| Interventions |
Organizational
Structural/environmental
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 3 months |
|
| Notes | ||
Otte Im Kampe 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Germany WHO region: EURO Participants: students, teachers, staff, community Setting: primary school, secondary school |
|
| Interventions |
Organizational
Structural/environmental
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 7 months |
|
| Notes | ||
Panovska‐Griffiths 2020a.
| Study characteristics | ||
| Methods | Inferential Modeling |
|
| Participants | Country: UK WHO region: EURO Participants: general population Setting: secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 18 months |
|
| Notes | ||
Panovska‐Griffiths 2020b.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 4 months |
|
| Notes | ||
Panovska‐Griffiths 2020c.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: general population Setting: secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 18 months |
|
| Notes | ||
Phillips 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Canada WHO region: PAHO Participants: students, teachers, staff, community Setting: primary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Educational outcomes
Follow‐up: unlimited |
|
| Notes | ||
Simonsen 2020.
| Study characteristics | ||
| Methods | Inferential Observational |
|
| Participants | Country: Denmark WHO region: EURO Participants: students Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Other health outcomes
Follow‐up: not reported |
|
| Notes | ||
Sneppen 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Denmark, Sweden, Norway (some data) WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: not reported |
|
| Notes | ||
Sparks 2020a.
| Study characteristics | ||
| Methods | Inferential Observational |
|
| Participants | Country: UK WHO region: EURO Participants: students, teachers, staff Setting: primary school |
|
| Interventions |
Organizational
Structural/environmental
|
|
| Outcomes |
Other health outcomes
Follow‐up: not reported |
|
| Notes | ||
Sparks 2020b.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: UK WHO region: EURO Participants: students, teachers, staff Setting: primary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: not reported |
|
| Notes | ||
Stage 2020.
| Study characteristics | ||
| Methods | Descriptive Modelling |
|
| Participants | Country: Denmark, Germany, Norway, Sweden WHO region: EURO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: 1‐2 months |
|
| Notes | ||
Stein‐Zamir 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Israel WHO region: EMRO Participants: students, teachers, staff Setting: secondary school |
|
| Interventions |
Organizational
Surveillance
|
|
| Outcomes |
Transmission‐related outcomes
Healthcare utilization
Follow‐up: until June 2020 |
|
| Notes | ||
Yoon 2020.
| Study characteristics | ||
| Methods | Descriptive Observational |
|
| Participants | Country: Korea WHO region: WPRO Participants: students, teachers, staff, general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
Surveillance
Infrastructural/environmental
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: 5 months |
|
| Notes | ||
Zhang 2020.
| Study characteristics | ||
| Methods | Inferential Modelling |
|
| Participants | Country: Chiina WHO region: WPRO Participants: general population Setting: primary school, secondary school |
|
| Interventions |
Organizational
|
|
| Outcomes |
Transmission‐related outcomes
Follow‐up: not reported |
|
| Notes | ||
AFRO: African Region; EMRO: Eastern Mediterranean Region; EURO: European Region; ICU: intensive care unit; PAHO: Region of the Americas, RT‐PCR: reverse transcription polymerase chain reaction; SEARO: South‐East Asian Region; WPRO: Western Pacific Region
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adler 2020 | Measures not eligible |
| Alsing 2020 | Measures not eligible |
| Ayoub 2020 | Study not conducted in school setting |
| Borch 2020 | Measures not eligible |
| Cheng 2020 | Measures not eligible |
| Davies 2020b | Measures not eligible |
| Dub 2020 | Measures not eligible |
| Esra 2020 | Measures not eligible |
| Fontanet 2020a | Measures not eligible |
| Fontanet 2020b | Measures not eligible |
| Islam 2020 | Measures not eligible |
| Iwata 2020 | Measures not eligible |
| Jackson 2020 | Measures not eligible |
| Karatayev 2020 | Measures not eligible |
| Nazif‐Munoz 2020 | Measures not eligible |
| Ng 2020 | Measures not eligible |
| Pham 2020 | Measures not eligible |
| Qin 2020 | Measures not eligible |
| Rypdal 2020 | Measures not eligible |
| Szablewski 2020 | Study not conducted in school setting |
Contributions of authors
ShK, LMP, JB and ER: defined the study scope and developed the study protocol with significant intellectual input from all review authors.
ShK, LMP and JB: co‐ordinated the entire study process.
CJS, CK, JR, KW, LMP, MC, ShK and SK: conducted title and abstracts screening.
CK, HL, JB, KG, KW, LMP, MC, ShK, SK and SV: conducted full‐text screening.
AM, CK, HL, JB, JMS, JR, KG, KS, KW, LMP, ShK, SK and SV: extracted data.
AM, HL, JB, KS, LMP and ShK: conducted the mapping.
ShK, LMP and JB drafted the manuscript.
All the study authors read, critically revised and approved the manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
COVID‐19 evidence ecosystem (CEO‐sys) project by the German Federal Ministry of Education and Research directed to our institution, the University of Munich (LMU), Germany
Declarations of interest
All authors (ShK, LMP, MC, KG, CJS, CK, SK, HL, AM, JR, ER, KS, BS, JMS, SV, KW, JB) declare being part of the scientific secretariat that supports the development of a living interdisciplinary, evidence‐based and consensus‐based guideline on measures to prevent and control SARS‐CoV‐2 transmission in schools, recently registered with the Association of the Scientific Medical Societies (AWMF) in Germany (www.awmf.org/en/clinical-practice-guidelines/detail/anmeldung/1/ll/027-076.html).
CJS, MC and ER are involved in the conduct of an ongoing study that, after completion, is likely to be eligible for inclusion in the review (COVID Kids Bavaria, funded by the State of Bavaria, Germany).
ER is a member of the scientific advisory board of the Bavarian Health and Food Safety Authority that has issued guidance on schooling during COVID‐19, but has not been involved with developing this guidance. She is a member of the WHO Regional Office for Europe's Technical Advisory Group on Schooling during COVID‐19 and, in this role, is involved with advising the WHO Regional Office for Europe on the issue.
Edited (no change to conclusions)
References
References to studies included in this review
Anchordoqui 2020 {published data only}
- Anchordoqui LA, Chudnovsky EM, Paul TC. Risk assessment of COVID-19 airborne infection during hybrid learning. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.24.20200782] [DOI] [Google Scholar]
Balabdaoui 2020 {published data only}
- Balabdaoui F, Mohr D. Age-stratified model of the COVID-19 epidemic to analyze the impact of relaxing lockdown measures: nowcasting and forecasting for Switzerland. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.05.08.20095059] [DOI] [Google Scholar]
Bracis 2020 {published data only}
- Bracis C, Burns E, Moore M, Swan D, Reeves DB, Schiffer JT, et al. Widespread testing, case isolation and contact tracing may allow safe school reopening with continued moderate physical distancing: a modeling analysis of King County, WA data. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.14.20174649] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks‐Pollock 2020 {published data only}
- Brooks-Pollock E, Read JM, McLean AR, Keeling MJ, Danon L. Using social contact data to predict and compare the impact of social distancing policies with implications for school re-opening. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.25.20156471] [DOI] [Google Scholar]
Buonsenso 2020 {published data only}
- Buonsenso D, De Rose C, Moroni R, Valentini P. SARS-CoV-2 infections in Italian schools: preliminary findings after one month of school opening during the second wave of the pandemic. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.10.10.20210328] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns 2020 {published data only}
- Burns A, Gutfraind A. Symptom-based isolation policies: evidence from a mathematical model of outbreaks of influenza and COVID-19. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.03.26.20044750] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020 {published data only}
- Campbell JR, Uppal A, Oxlade O, Fregonese F, Bastos ML, Lan Z, et al. Active testing of groups at increased risk of acquiring SARS-CoV-2 in Canada: costs and human resource needs. Canadian Medical Association Journal 2020;192(40):E1146-E1155. [DOI: 10.1503/cmaj.201128] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2020 {published data only}
- Cohen JA, Mistry D, Kerr CC, Klein DJ. Schools are not islands: balancing COVID-19 risk and educational benefits using structural and temporal countermeasures. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.08.20190942] [DOI] [Google Scholar]
Coletti 2020 {published data only}
- Coletti P, Libin P, Petrof O, Willem L, Steven A, Herzog SA, et al. A data-driven metapopulation model for the Belgian COVID-19 epidemic: assessing the impact of lockdown and exit strategies. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.20.20157933] [DOI] [PMC free article] [PubMed] [Google Scholar]
Curtius 2020 {published data only}
- Curtius J, Granzin M, Schrod J. Testing mobile air purifiers in a school classroom: reducing the airborne transmission risk for SARS-CoV-2. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.10.02.20205633] [DOI] [Google Scholar]
Di Domenico 2020 {published data only}
- Di Domenico L, Pullano G, Sabbatini CE, Boëlle P-Y, Colizza V. Expected impact of reopening schools after lockdown on COVID-19 epidemic in Île-de-France. www.epicx-lab.com/uploads/9/6/9/4/9694133/inserm-covid-19_report_school_idf-20200506.pdf [Preprint] 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ehrhardt 2020 {published data only}
- Ehrhardt J, Ekinci A, Krehl H, Meincke M, Finci I, Klein J, et al. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Wurttemberg, Germany. Eurosurveillance 2020;25(36):pii=2001587. [DOI: 10.2807/1560-7917.ES.2020.25.36.2001587] [DOI] [PMC free article] [PubMed] [Google Scholar]
Espana 2020 {published data only}
- Espana G, Cavany S, Oidtman RJ, Barbera C, Costello A, Lerch A, et al. Impacts of K-12 school reopening on the COVID-19 epidemic in Indiana, USA. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.22.20179960] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gandolfi 2020 {published data only}
- Gandolfi A. Planning of school teaching during COVID-19. Physica D. Nonlinear Phenomena 2020;415:132753. [DOI] [PMC free article] [PubMed] [Google Scholar]
Garchitonerena 2020 {published data only}
- Garchitorena A, Gruson H, Cazelles B, Roche B. Quantifying the efficiency of non-pharmaceutical interventions against SARS-COV-2 transmission in Europe. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.17.20174821] [DOI] [Google Scholar]
Gill 2020 {published data only}
- Gill B, Goyal R, Hotchkiss J. Operating schools in a pandemic: predicted effects of opening, quarantining, and closing strategies. Princeton, NJ: Mathematica. mathematica.org/our-publications-and-findings/publications/operating-schools-in-a-pandemic-predicted-effects-of-opening-and-quarantining-strategies 2020. [Google Scholar]
Head 2020 {published data only}
- Head JR, Andrejko K, Cheng Q, Collender PA, Phillips S, Boser A, et al. The effect of school closures and reopening strategies on COVID-19 infection dynamics in the San Francisco Bay Area: a cross-sectional survey and modeling analysis. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.06.20169797] [DOI] [Google Scholar]
Isphording 2020 {published data only}
- Isphording I, Lipfert M, Prestel N. School re-openings after summer breaks in Germany did not increase SARS-CoV-2 cases. Bonn, Germany: Institute of Labor Economics; ftp.iza.org/dp13790.pdf 2020.
Johnson 2020 {published data only}
- Johnson KE, Stoddard M, Nolan RP, White DE, Hochberg NS, Chakravarty A. In the long shadow of our best intentions: model-based assessment of the consequences of school reopening during the COVID-19 pandemic. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.18.20197400] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keeling 2020 {published data only}
- Keeling MJ, Tildesley MJ, Atkins BD, Penman B, Southall E, Guyver-Fletcher G, et al. The impact of school reopening on the spread of COVID-19 in England. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.04.20121434] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keskinocak 2020 {published data only}
- Keskinocak P, Asplund J, Serban N, Oruc Aglar BE. Evaluating scenarios for school reopening under COVID19. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.22.20160036] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2020 {published data only}
- Kim S, Kim YJ, Peck KR, Jung E. School opening delay effect on transmission dynamics of coronavirus disease 2019 in Korea: based on mathematical modeling and simulation study. Journal of Korean Medical Science 2020;35(13):e143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kraay 2020 {published data only}
- Kraay AN, Hayashi MA, Berendes DM, Sobolik JS, Leon JS, Lopman BA. Risk of fomite-mediated transmission of SARS-CoV-2 in child daycares, schools, and offices: a modeling study. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.10.20171629] [DOI] [PMC free article] [PubMed] [Google Scholar]
Landeros 2020 {published data only}
- Landeros A, Ji X, Lange KL, Stutz TC, Xu J, Sehl ME, et al. An examination of school reopening strategies during the SARS-CoV-2 pandemic. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.05.20169086] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macartney 2020 {published data only}
- Macartney K, Quinn HE, Pillsbury AJ, Koirala A, Deng L, Winkler N, et al. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child & Adolescent Health 2020;4(11):807-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
McBryde 2020 {published data only}
- McBryde ES, Trauer JM, Adekunle A, Ragonnet R, Meehan MT. Stepping out of lockdown should start with school re-openings while maintaining distancing measures. Insights from mixing matrices and mathematical models. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.05.12.20099036] [DOI] [Google Scholar]
Monod 2020 {published data only}
- Monod M, Blenkinsop A, Xi X, Hebert D, Bershan S, Bradley VC, et al. Age groups that sustain resurging COVID-19 epidemics in the United States. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.18.20197376] [DOI] [PMC free article] [PubMed] [Google Scholar]
Munday 2020 {published data only}
- Munday JD, Sherratt K, Meakin S, Endo A, Pearson CA, Hellewell J, et al. Implications of the school-household network structure on SARS-CoV-2 transmission under different school reopening strategies in England. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.21.20167965] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCIRS 2020 {published data only}
- National Centre for Immunisation Research and Surveillance (NCIRS). COVID-19 in schools and early childhood education and care services - the Term 2 experience in NSW. ncirs.org.au/sites/default/files/2020-08/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%202%20report_0.pdf 2020. [Google Scholar]
Otte Im Kampe 2020 {published data only}
- Otte Im Kampe E, Lehfeld AS, Buda S, Buchholz U, Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Eurosurveillance 2020;25(38):pii=2001645. [DOI: 10.2807/1560-7917.ES.2020.25.38.2001645] [DOI] [PMC free article] [PubMed] [Google Scholar]
Panovska‐Griffiths 2020a {published data only}
- Panovska-Griffiths J, Kerr CC, Waites W, Stuart RM, Mistry D, Foster D, et al. Modelling the potential impact of mask use in schools and society on COVID-19 control in the UK. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.28.20202937] [DOI] [PMC free article] [PubMed] [Google Scholar]
Panovska‐Griffiths 2020b {published data only}
- Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al. Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child & Adolescent Health 2020;4(11):817-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Panovska‐Griffiths 2020c {published data only}
- Panovska-Griffiths J, Kerr CC, Waites W, Stuart RM, Mistry D, Foster D, et al. The potential contribution of face coverings to the control of SARS-CoV-2 transmission in schools and broader society in the UK: a modelling study. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.28.20202937] [DOI] [Google Scholar]
Phillips 2020 {published data only}
- Phillips B, Browne D, Anand M, Bauch C. Model-based projections for COVID-19 outbreak size and student-days lost to closure in Ontario childcare centres and primary schools. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.07.20170407] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simonsen 2020 {published data only}
- Simonsen AB, Ruge IF, Quaade AS, Johansen JD, Thyssen JP, Zachariae C. High incidence of hand eczema in Danish schoolchildren following intensive hand hygiene during the COVID-19 pandemic: a nationwide questionnaire study. British Journal of Dermatology 2020;183(5). [DOI: 10.1111/bjd.19413] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sneppen 2020 {published data only}
- Sneppen K, Robert JT, Lone S. Impact of superspreaders on dissemination and mitigation of COVID-19. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.05.17.20104745] [DOI] [Google Scholar]
Sparks 2020a {published data only}
- Sparks SR, Aspinall WP, Brooks-Pollock E, Danon L, Cooke R, Barclay J, et al. A novel approach for evaluating contact patterns and risk mitigation strategies for COVID-19 in English primary schools with application of structured expert judgement. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.13.20170068] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sparks 2020b {published data only}
- Sparks SR, Aspinall WP, Cooke R, Scarrow JH. Quantifying threat from COVID-19 infection hazard in primary schools in England. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.07.20170035] [DOI] [Google Scholar]
Stage 2020 {published data only}
- Stage HB, Shingleton J, Ghosh S, Scarabel F, Pellis L, Finnie T. Shut and re-open: the role of schools in the spread of COVID-19 in Europe. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.24.20139634] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stein‐Zamir 2020 {published data only}
- Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al. A large COVID-19 outbreak in a high school 10 days after schools' reopening, Israel, May 2020. Eurosurveillance 2020;25(29):pii=2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yoon 2020 {published data only}
- Yoon Y, Kim K-R, Park H, Kim Sy, Kim Y-J. Stepwise school opening online and off-line and an impact on the epidemiology of COVID-19 in the pediatric population. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.03.20165589] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2020 {published data only}
- Zhang J, Litvinova M, Liang Y, Zheng W, Shi H, Vespignani A, et al. The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.03.20167056] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adler 2020 {published data only}
- Adler SO, Bodeit O, Bonn L, Goldenbogen B, Haffner JE, Karnetzki M, et al. Geospatially referenced demographic agent-based modeling of SARS-CoV-2-infection (COVID-19) dynamics and mitigation effects in a real-world community. pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/ppmedrxiv-20089235 [Preprint] 2020. [Google Scholar]
Alsing 2020 {published data only}
- Alsing J, Kirk T, Usher N, Crowley PJ. Containing COVID-19 outbreaks with spatially targeted short-term lockdowns and mass-testing. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.05.05.20092221] [DOI] [Google Scholar]
Ayoub 2020 {published data only}
- Ayoub HH, Chemaitelly H, Mumtaz GR, Seedat S, Awad SF, Makhoul M, et al. Characterizing key attributes of the epidemiology of COVID-19 in China: model-based estimations. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.08.20058214] [DOI] [PMC free article] [PubMed] [Google Scholar]
Borch 2020 {published data only}
- Borch L, Thorsteinsson K, Warner TC, Mikkelsen CS, Bjerring P, Lundbye-Christensen S, et al. COVID-19 reopening causes high risk of irritant contact dermatitis in children. Danish Medical Journal 2020;67(9):A05200357. [PubMed] [Google Scholar]
Cheng 2020 {published data only}
- Cheng L, Tieyong Z, Xinmiao FU. Little risk of the COVID-19 resurgence on students in China (outside Hubei) caused by school reopening. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.04.20053645] [DOI] [Google Scholar]
Davies 2020b {published data only}
- Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, on behalf of the Centre for the Mathematical Modelling of Infectious Diseases COVID-19 working group. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health 2020;5(7):e375-e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dub 2020 {published data only}
- Dub T, Erra E, Hagberg L, Sarvikivi E, Virta C, Jarvinen A, et al. Transmission of SARS-CoV-2 following exposure in school settings: experience from two Helsinki area exposure incidents. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.20.20156018] [DOI] [Google Scholar]
Esra 2020 {published data only}
- Esra RT, Jamesion L, Fox MP, Letswalo D, Ngcobo N, Mngadi S, et al. Evaluating the impact of non-pharmaceutical interventions for SARS-CoV-2 on a global scale. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.30.20164939] [DOI] [Google Scholar]
Fontanet 2020a {published data only}
- Fontanet A, Grant R, Tondeur L, Madec Y, Grzelak L, Cailleau I, et al. SARS-CoV-2 infection in primary schools in northern France: a retrospective cohort study in an area of high transmission. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.25.20140178] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fontanet 2020b {published data only}
- Fontanet A, Tondeur L, Madec Y, Grant R, Besombes C, Jolly N, et al. Cluster of COVID-19 in northern France: a retrospective closed cohort study. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.18.20071134] [DOI] [Google Scholar]
Islam 2020 {published data only}
- Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ 2020;370:m2743. [DOI] [PMC free article] [PubMed] [Google Scholar]
Iwata 2020 {published data only}
- Iwata K, Doi A, Miyakoshi C. Was school closure effective in mitigating coronavirus disease 2019 (COVID-19)? Time series analysis using Bayesian inference. International Journal of Infectious Diseases 2020;99:57-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2020 {published data only}
- Jackson ML. Low-impact social distancing interventions to mitigate local epidemics of SARS-CoV-2. Microbes & Infection (in press). [DOI: 10.1016/j.micinf.2020.09.006.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karatayev 2020 {published data only}
- Karatayev VA, Anand M, Bauch CT. Local lockdowns outperform global lockdown on the far side of the COVID-19 epidemic curve. Proceedings of the National Academy of Sciences of the United States of America 2020;117(39):24575-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nazif‐Munoz 2020 {published data only}
- Nazif-Munoz JI, Oulhote Y, Pena S. The global viralization of policies to contain the spreading of the COVID-19 pandemic: analyses of school closures and first reported cases. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.11.20128892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ng 2020 {published data only}
- Ng V, Fazil A, Waddell LA, Bancej C, Turgeon P, Otten A, et al. Projected effects of nonpharmaceutical public health interventions to prevent resurgence of SARS-CoV-2 transmission in Canada. CMAJ Canadian Medical Association Journal 2020;192(37):E1053-E64. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pham 2020 {published data only}
- Pham H. Estimating the COVID-19 death toll by considering the time-dependent effects of various pandemic restrictions. Mathematics 2020;8(9):1628. [Google Scholar]
Qin 2020 {published data only}
- Qin D-A, Wu W, Hu Y-J, Wang Z-J, Han X-l, Yan H-B, et al. A post-COVID-19 effect: increasing sport-related knee pain in adolescents after school reopening. SSRN [Preprint] 2020. [DOI: ] [Google Scholar]
Rypdal 2020 {published data only}
- Rypdal M, Rypdal VG, Jakobsen PK, Ytterstad E, Lovsletten O, Klingenberg C, et al. Modelling suggests limited change in the reproduction number from reopening Norwegian kindergartens and schools during the COVID-19 pandemic. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.08.14.20174896] [DOI] [PMC free article] [PubMed] [Google Scholar]
Szablewski 2020 {published data only}
- Szablewski CM, Chang KT, Brown MM, Chu VT, Yousaf AR, Anyalechi N, et al. SARS-CoV-2 transmission and infection among attendees of an overnight camp - Georgia, June 2020. Morbidity and Mortality Weekly Report. Surveillance Summaries : MMWR 2020;69(31):1023-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abadio de Oliveira 2020
Anderson 2008
- Anderson S, Allen P, Peckham S, Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Research Policy and Systems / BioMed Central 2008;6(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Araújo 2020
- Araújo LA, Veloso CF, Souza MC, Azevedo JM, Tarro G. The potential impact of the COVID-19 pandemic on child growth and development: a systematic review. Jornal de Pediatria 2020 Sep 23 [Epub ahead of print]. [DOI: 10.1016/j.jped.2020.08.008] [DOI] [PMC free article] [PubMed]
Arksey 2005
- Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8(1):19-32. [Google Scholar]
Bärnighausen 2017
- Bärnighausen T, Tugwell P, Røttingen J-A, Shemilt I, Rockers P, Geldsetzer P, et al. Quasi-experimental study designs series—paper 4: uses and value. Journal of Clinical Epidemiology 2017;89:21-9. [DOI] [PubMed] [Google Scholar]
Bin Nafisah 2018
- Bin Nafisah S, Alamery AH, Al Nafesa A, Aleid B, Brazanji NA. School closure during novel influenza: a systematic review. Journal of Infection and Public Health 2018;11(5):657-61. [DOI] [PubMed] [Google Scholar]
Bonell 2020
- Bonell C, Melendez-Torres GJ, Viner RM, Rogers MB, Whitworth M, Rutter H, et al. An evidence-based theory of change for reducing SARS-CoV-2 transmission in reopened schools. Health & Place 2020;64:102398. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brauner 2020
- Brauner JM, Mindermann S, Sharma M, Stephenson AB, Gavenčiak T, Johnston D, et al. The effectiveness of eight nonpharmaceutical interventions against COVID-19 in 41 countries. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.05.28.20116129] [DOI] [Google Scholar]
Brooks 2020
- Brooks SK, Smith LE, Webster RK, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children's social contact: rapid evidence review. Eurosurveillance 2020;25(13):2000188. [DOI: 10.2807/1560-7917.ES.2020.25.13.2000188] [DOI] [PMC free article] [PubMed] [Google Scholar]
Castagnoli 2020
- Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatrics 2020;174(9):882-9. [DOI] [PubMed] [Google Scholar]
Cauchemez 2009
- Cauchemez S, Ferguson NM, Wachtel C, Tegnell A, Saour G, Duncan B, et al. Closure of schools during an influenza pandemic. Lancet Infectious diseases 2009;9(8):473-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
CCDCP 2020a
- COVID-19 Emergency Response Key Places Protection and Disinfection Technology Team, Chinese Center for Disease Control and Prevention. Health protection guideline of schools and other educational institutions during COVID-19 outbreak. Zhonghua Yu Fang Yi Xue Za Zhi [Chinese Journal of Preventive Medicine] 2020;54(4):348-50. [DOI: 10.3760/cma.j.cn112150-20200217-00123] [DOI] [PubMed] [Google Scholar]
CCDCP 2020b
- Strategy and Policy Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. Interim guidelines for prevention and control of COVID-19 for students back to school. Zhonghua Liu Xing Bing Xue Za Zhi 2020;41(8):1195-6. [DOI: 10.3760/cma.j.cn112338-20200410-00550] [DOI] [PubMed] [Google Scholar]
CDC 2020a
- Centers for Disease Control and Prevention: DC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)-United States, February 12-March 16, 2020. Morbidity and Mortality Weekly Report. Surveillance Summaries : MMWR 2020;69(23):343-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2020b
- Centers for Disease Control and Prevention. Operating schools during COVID-19: CDC's considerations. www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/schools.html (accessed prior to 7 December 2020). [Google Scholar]
CDC 2020c
- Centers for Disease Control and Prevention. Interim considerations for testing for K-12 school administrators and public health officials. www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-testing.html (accessed prior to 7 December 2020). [Google Scholar]
Christakis 2020
- Christakis DA. School reopening—the pandemic issue that is not getting its due. JAMA Pediatrics 2020;174(10):928. [DOI: 10.1001/jamapediatrics.2020.2068] [DOI] [PubMed] [Google Scholar]
Cohen 2020
- Cohen R, Delacourt C, Gras-Le Guen C, Launay E, French Pediatric Society. COVID-19 and schools. Guidelines of the French Pediatric Society. ScienceDirect 2020;7(7):388-92. [DOI: 10.1016/j.arcped.2020.09.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Couzin‐Frankel 2020
- Couzin-Frankel J, Vogel G, Weiland M. School openings across globe suggest ways to keep coronavirus at bay, despite outbreaks. Science: sciencemag.org/news/2020/07/school-openings-across-globe-suggest-ways-keep-coronavirus-bay-despite-outbreaks 2020. [Google Scholar]
Crawley 2020
- Crawley E, Loades M, Feder G, Logan S, Redwood S, Macleod J. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatrics Open 2020;4(1):e000701. [DOI: 10.1136/bmjpo-2020-000701] [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Angelo 2020
- D'Angelo D, Coclite D, Napoletano A, Fauci AJ, Latina R, Iacorossi L, et al. Strategies for exiting COVID-19 lockdown for workplace and school: a scoping review protocol. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.09.04.20187971] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dattner 2020
- Dattner I, Goldberg Y, Katriel G, Yaari R, Gal N, Miron Y, et al. The role of children in the spread of COVID-19: using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.03.20121145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davies 2020a
- Davies NG, Klepac P, Liu Y, Prem K, Jit M, Pearson CA, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nature Medicine 2020;26(8):1205-11. [DOI] [PubMed] [Google Scholar]
Dibner 2020
- Dibner KA, Schweingruber HA, Christakis DA. Reopening k-12 schools during the COVID-19 pandemic: A report from the National Academies of Sciences, Engineering, and Medicine. JAMA 2020;324(9):833-4. [DOI] [PubMed] [Google Scholar]
Dong 2020
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145(6):e20200702. [DOI: 10.1542/peds.2020-0702] [DOI] [PubMed] [Google Scholar]
Fadlallah 2020
- Fadlallah R, Jamal D, Daher N, Masri R, Hemadi N. COVID-19 supplement on school re-opening (2 of 3): impact of school closure/reopening and school management practices on COVID-19 pandemic. Available from: aub.edu.lb/k2p/Documents/K2P COVID19 Supplement on School Re-opening (2 of 3) Impact of School Closure Reopening and School Management Practices on COVID19 Pandemic.pdf (accessed prior to 27 November 2020).
Fardin 2020
- Fardin MA. COVID-19 and anxiety: a review of psychological impacts of infectious disease outbreaks. Archives of Clinical Infectious Diseases 2020 Apr 2 [Epub ahead of print]. [DOI: 10.5812/archcid.102779] [DOI]
Feldstein 2020
- Feldstein LR, Rose EB, Horwitz SM, Collins JP, Newhams MM, Son MB, et al. Multisystem inflammatory syndrome in U.S. children and adolescents. New England Journal of Medicine 2020;383(4):334-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferguson 2020
- Ferguson N, Laydon D, Nedjati Gilani G, Imai N, Ainslie K, Baguelin M, et al. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf.
Golberstein 2020
- Golberstein E, Wen H, Miller BF. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics 2020;174(9):819-20. [DOI] [PubMed] [Google Scholar]
Götzinger 2020
- Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al. COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child & Adolescent Health 2020;4(9):653-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grimes 2002
- Grimes DA, Schulz KF. Descriptive studies: what they can and cannot do. Lancet 2002;359(9301):145-9. [DOI] [PubMed] [Google Scholar]
Jackson 2013
- Jackson C, Vynnycky E, Hawker J, Olowokure B, Mangtani P. School closures and influenza: systematic review of epidemiological studies. BMJ Open 2013;3(2):e002149. [DOI: 10.1136/bmjopen-2012-002149] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2014
- Jackson C, Mangtani P, Hawker J, Olowokure B, Vynnycky E. The effects of school closures on influenza outbreaks and pandemics: systematic review of simulation studies. PloS One 2014;9(5):e97297. [DOI: 10.1371/journal.pone.0097297] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jing 2020
- Jing QL, Liu MJ, Yuan J, Zhang ZB, Zhang AR, Dean NE, et al. Household secondary attack rate of COVID-19 and associated determinants. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.11.20056010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Juneau 2020
- Juneau CE, Pueyo T, Bell M, Gee G, Collazzo P, Potvin L. Evidence-based, cost-effective interventions to suppress the COVID-19 pandemic: a systematic review. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.20.20054726] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keshavarz 2010
- Keshavarz N, Nutbeam D, Rowling L, Khavarpour F. Schools as social complex adaptive systems: a new way to understand the challenges of introducing the health promoting schools concept. Social Science & Medicine (1982) 2010;70(10):1467-74. [DOI] [PubMed] [Google Scholar]
Kneale 2020
- Kneale D, O'Mara-Eves A, Rees R, Thomas J. School closure in response to epidemic outbreaks: systems-based logic model of downstream impacts. F1000Research 2020;9:352. [DOI: 10.12688/f1000research.23631.1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leclerc 2020
- Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Research 2020;5:83. [DOI: 10.12688/wellcomeopenres.15889.2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2020
- Li X, Xu W, Dozier M, He Y, Kirolos A, Theodoratou E. The role of children in transmission of SARS-CoV-2: a rapid review. Journal of Global Health 2020;10(1):011101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2020
- Liu C, He Y, Liu L, Li F, Shi Y. Children with COVID-19 behaving milder may challenge the public policies: a systematic review and meta-analysis. BMC Pediatrics 2020;20(410). [DOI: 10.1186/s12887-020-02316-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ludwigsson 2020
- Ludvigsson JF. Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica 2020;109(6):108-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Matthay 2020
- Matthay MA, Aldrich JM, Gotts JE. Treatment for severe acute respiratory distress syndrome from COVID-19. Lancet Respiratory Medicine 2020;8(5):433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Microsoft Corporation 2018 [Computer program]
- Microsoft Excel. Microsoft Corporation, 2018. office.microsoft.com/excel.
Mossong 2008
- Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLOS Medicine 2008;5(3):e74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Munn 2018
- Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology 2018;18(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCCMT 2020
- National Collaborating Centre for Methods and Tools (NCCMT). Rapid evidence review: What is the specific role of daycares and schools in COVID-19 transmission? Update 2020 September 18, 2020. Available from: nccmt.ca/uploads/media/media/0001/02/98cc589e2c1db4996ba0cb5d52daef448b175f24.pdf (accessed prior to 27 November 2020).
NIHR 2020a
- National Institute for Health Research (NIHR). Living with COVID19: a dynamic review of the evidence around ongoing COVID19 symptoms 2020. Available from: evidence.nihr.ac.uk/themedreview/living-with-covid19/ (updated 15 October 2020).
Nussbaumer‐Streit 2020
- Nussbaumer-Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD013574. [DOI: 10.1002/14651858.CD013574] [DOI] [PMC free article] [PubMed] [Google Scholar]
NYSED 2020
- New York State Education Department. Recovering, rebuilding, and renewing: the spirit of New York’s schools - reopening guidance. nysed.gov/common/nysed/files/programs/reopening-schools/nys-p12-school-reopening-guidance.pdf 2020.
Park 2020
- Park YJ, Choe YJ, Park O, Park SY, Kim Y-M, Kim J, et al. Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerging Infectious Diseases 2020;26(10):2465-8. [DOI: 10.3201/eid2610.201315] [DOI] [PMC free article] [PubMed] [Google Scholar]
Persch 2013
- Persch AC, Page SJ. Protocol development, treatment fidelity, adherence to treatment, and quality control. American Journal of Occupational Therapy 2013;67(2):146-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfadenhauer 2017
- Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, et al. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implementation Science 2017;12(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prem 2020
- Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health 2020;5(5):E261-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Public Health Ontario 2020
- Ontario Agency for Health Protection and Promotion (Public Health Ontario). COVID-19 pandemic school closure and reopening impacts. Toronto: Queen's Printer for Ontario; 2020. Available from: publichealthontario.ca/-/media/documents/ncov/main/2020/08/covid-19-school-closure-reopening-impacts.pdf?la=en.
Rabin 2008
- Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. Journal of Public Health Management and Practice 2008;14(2):117-23. [DOI] [PubMed] [Google Scholar]
Rashid 2015
- Rashid H, Ridda I, King C, Begun M, Tekin H, Wood JG, et al. Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatric Respiratory Reviews 2015;16(2):119-26. [DOI] [PubMed] [Google Scholar]
Simon 2020
- Simon A, Huebner J, Berner R, Munro AP, Exner M, Huppertz H-I, et al. Measures to maintain regular operations and prevent outbreaks of SARS-CoV-2 in childcare facilities or schools under pandemic conditions and co-circulation of other respiratory pathogens. GMS Hygiene and Infection Control 2020;15:Doc22. [DOI: 10.3205/dgkh000357] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2020
- Smith WC. Potential long-term consequences of school closures: Lessons from the 2013-2016 Ebola pandemic. researchsquare.com/article/rs-51400/v1 [Preprint] 2020. [DOI: 10.21203/rs.3.rs-51400/v1] [DOI] [Google Scholar]
Stratil 2020
- Stratil JM, Voss M, Arnold L. WICID framework Version 1.0: criteria and considerations to guide evidence-informed decision-making on non-pharmacological interventions targeting COVID-19. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.07.03.20145755] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tricco 2016
- Tricco AC, Lillie E, Zarin W, O'Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Medical Research Methodology 2016;16:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tricco 2018
- Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of Internal Medicine 2018;169(7):467-73. [DOI] [PubMed] [Google Scholar]
UNESCO 2012
- UNESCO Institute for Statistics. International standard classification of education: ISCED 2011. UNESCO Institute for Statistics, Montreal 2012.
UNESCO 2020a
- UNESCO. COVID-19 impact on education 2020. Available from: en.unesco.org/covid19/educationresponse (accessed prior to 27 November 2020).
UNESCO 2020b
- UNESCO. Education: from disruption to recovery. en.unesco.org/covid19/educationresponse (accessed prior to 27 November 2020).
Viner 2020a
- Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child & Adolescent Health 2020;4(5):397-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Viner 2020b
- Viner RM, Bonell C, Drake L, Jourdan D, Davies N, Baltag V, et al. Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Archives of Disease in Childhood 2020 Aug 3 [Epub ahead of print]. [DOI: 10.1136/archdischild-2020-319963] [DOI] [PMC free article] [PubMed]
Viner 2020c
- Viner RM, Mytton OT, Bonell C, Melendez-Torres G, Ward JL, Hudson L, et al. Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatrics 2020. [DOI: 10.1001/jamapediatrics.2020.4573] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walger 2020
- Walger P, Heininger U, Knuf M, Exner M, Popp W, Fischbach T, et al. Children and adolescents in the COVID-19 pandemic: schools and daycare centers are to be opened again without restrictions. The protection of teachers, educators, carers and parents and the general hygiene rules do not conflict with this. GMS Hygiene and Infection Control 2020;15:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2019
- World Health Organization (WHO). Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza: annex: report of systematic literature reviews. World Health Organization; 2019. who.int/influenza/publications/public_health_measures/publication/en/ (accessed prior to 27 November 2020).
WHO 2020a
- World Health Organization (WHO). WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 2020 (updated 11 March 2020). who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020.
WHO 2020b
- World Health Organization (WHO). WHO, UNICEF urge safe school reopening in Africa 2020. Available from: afro.who.int/news/who-unicef-urge-safe-school-reopening-africa.
WHO 2020c
- World Health Organization (WHO). Considerations for school-related public health measures in the context of COVID-19: annex to considerations in adjusting public health and social measures in the context of COVID-19, 14 September 2020. Available from: WHO/2019-nCoV/Adjusting_PH_measures/Schools/2020.2.
Worby 2015
- Worby CJ, Chaves SS, Wallinga J, Lipsitch M, Finelli L, Goldstein E. On the relative role of different age groups in influenza epidemics. Epidemics 2015;13:10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2020
- Xu W, Li X, Dozier M, He Y, Kirolos A, Lang Z, et al. What is the evidence for transmission of COVID-19 by children in schools? A living systematic review. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.10.11.20210658] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yelin 2020
- Yelin D, Wirtheim E, Vetter P, Kalil AC, Bruchfeld J, Runold M, et al. Long-term consequences of COVID-19: research needs. Lancet Infectious Diseases 2020;20(10):P1115-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Pfadenhauer 2020
- Pfadenhauer LM, Krishnaratne S, Burns J, Coenen M, Geffert K, Jung-Sievers C, et al. Measures implemented in the school setting to contain the COVID-19 pandemic: a scoping review protocol. Open Science Framework: osf.io/bm2xu 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]