Abstract
Introduction:
Burn injuries are under-appreciated trauma, associated with substantial morbidity and mortality. It is necessary to refer patients in need of specialized care to more specialized centers for treatment and rehabilitation of burn injuries. This systematic review aimed to assess the adherence to referral criteria for burn patients.
Methods:
An extensive search was conducted on Scopus, PubMed, and Web of Science online databases using the relevant keywords from the earliest to October 7, 2021. The quality of the included studies was assessed using the appraisal tool for cross-sectional studies (AXIS tool).
Results:
Among a total of 7,455 burn patients included in the nine studies, 60.95% were male. The most frequently burned areas were the hands (n=3) and the face (n=2). The most and least common burn mechanisms were scalds (62.76%) and electrical or chemical (2.88%), respectively. 51.88% of burn patients had met ≥ 1 referral criteria. The overall adherence to the referral criteria for burn patients was 58.28% (17.37 to 93.39%). The highest and lowest adherence rates were related to Western Cape Provincial (WCP) (26.70%) and National Burn Care Review (NBCR) (4.97%) criteria, respectively.
Conclusion:
The overall adherence to the referral criteria for burn patients was relatively desirable. Therefore, well-designed future studies are suggested in order to uncover approaches to improve adherence to referral criteria for burn patients.
Key Words: Burns, Guideline adherence, Referral and consultation, Systematic review
1. Introduction:
Burn injuries are under-appreciated trauma associated with substantial morbidity and mortality (1-9). Based on the report by World Health Organization, 11 million burns occur annually worldwide, 180,000 are fatal (10). Therefore, it is necessary to refer patients in need of specialized care to more specialized centers for treatment and rehabilitation of burn injuries (11).
Meanwhile, referral criteria for transferring burn patients to burn specialty centers have been proposed by various burn associations in the USA, the United Kingdom, and Australia and New Zealand (11). However, despite using referral criteria for burn patients for more than two decades, there is still limited information on adherence to these criteria. In the Netherlands, adherence to the Emergency Management of Severe Burns (EMSB) criteria in patients primarily presenting to a non-burn center was 70.03% (11) Two studies in the USA showed that adherence to the American Burn Association (ABA) and EMSB criteria in patients primarily presenting to a non-burn center was 48.00% and 54%, respectively (12, 13). However, a study in the United Kingdom found that adherence to the British Burns Association (BBA) criteria in burn patients was 25.31% (14). The need to adhere to these criteria worldwide and the possible improved outcomes for burn patients cannot be overemphasized, hence the need to conduct this systematic review.
Limited and contradictory studies have been published on adherence to referral criteria for burn patients. This systematic review aimed to assess the adherence to referral criteria for burn patients.
2. Methods:
This systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines (15).
2.1. Search strategy
An extensive search was conducted on Scopus, PubMed, and Web of Science online databases using keywords such as "Burns", "Guideline adherence", “Patients”, and "Referral criteria" from the earliest to October 7, 2021. For example, the search strategy in PubMed/MEDLINE database was ((“Guideline Adherence”) OR (“Policy Compliance”) OR (“Protocol Compliance”) OR (“Institutional Adherence”) OR (“Adherence, Institutional”)) AND ((“Referral Criteria”) OR (“Hospital Referral”) OR (“Guidelines”) OR (“Standards”) OR (“Reference Standards”) OR (“Criteria”) OR (“Referral”) OR (“Consultation”) OR (“Consultation and Referral”)) AND ((“Burns”) OR (“Patients”) OR (“Clients”)). Keywords were extracted from the medical subject headings and combined using Boolean operators (AND/OR). Two researchers performed the search steps, independently. In the present systematic review, the gray literature such as conference presentations, expert opinion, dissertations, research and committee reports, and ongoing research were not seriously searched because they did not fully depict the results, and the results may completely change when they are not published. Gray literature is defined as papers that are produced in print and electronic formats but are not controlled by commercial publishers (16).
2.2. Inclusion and exclusion criteria
In this review, studies published in English, focusing on adherence to referral criteria for burn patients were included (Table 1). The corresponding authors were contacted in cases of lack of access to articles or where relevant data was missing.
2.3. Study selection
EndNote X8 software was used to manage the data. Duplicate articles were removed, first electronically and then manually. Title, abstract, and full text of articles were assessed based on inclusion/exclusion criteria. The reference list of eligible studies was reviewed to prevent missing relevant information. In case of disagreement between researchers, the articles were evaluated by a third researcher.
2.4. Data extraction and quality assessment
Assessment of the quality of included studies was performed by two researchers. The researchers extracted information from the included studies. The information included the name of the first author, year of publication, location, sample size, male/female ratio, age, source of data collection, length of stay, burn mechanism, number of referral criteria met, the most frequently burned area, rate of adherence to referral criteria, the highest and lowest rates of adherence to referral criteria, instrument, and key results. The quality of the included studies was assessed using the appraisal tool for cross-sectional studies (AXIS tool). This tool evaluates the quality of the included studies using 20 items (17).
Table 1.
Eligibility Criteria
| Criteria | Inclusion | Exclusion |
|---|---|---|
| Participants | Burn patients Patients of all age groups |
Animal studies |
| Outcomes | Rate of adherence to referral criteria for burn patients The highest and lowest rate of adherence to referral criteria |
- |
| Study Design | Cross-Sectional Retrospective |
Case reports Experimental studies Letters to editors Conferences Reviews |
| Time Frame | The earliest to October 5, 2021 | - |
Figure 2.
Assessment of the quality of the included articles.
Table 2.
Basic characteristics of the studies included in this systematic review
| First Author/year | Study period | Design | Source of data collection | Sample Size | M/F ratio | Age* (years) |
|---|---|---|---|---|---|---|
| Chipp et al., 2008 (14) United Kingdom |
2004 | Retrospective | West Midlands Regional Burns Unit |
561 | 53.00/47.00 | N/A |
| Carter et al., 2010 (12) USA |
2006 to 2007 | Retrospective | North Carolina Hospital Association Patient Data System |
2,036 | 66.80/33.20 | 48.05 (SD=17.75) |
| Rose et al., 2010 (22) United Kingdom |
2010 (6-month period) | Retrospective | Administrative database | 190 | 55.26/44.74 | 0 to 15 |
| Baartmans et al., 2012 (18) Netherlands |
2002 to 2004 & 2007 to 2008 | Retrospective | Dutch National Trauma Registry | 622 | 63.51/36.49 | > 15 |
| Davis et al., 2012 (13) USA |
2008 | Retrospective | ICD-9 | 750 | N/A | 39.00 (SD=23.00) |
| Reiband et al., 2014 (21) Denmark |
2011 (3-months period) | Retrospective | ICD-10 | 97 | 70.10/29.90 | 10 months to 71 years |
| Boissin et al., 2017 (19) South Africa |
2011 to 2015 | Retrospective | Administrative database | 1,165 | 55.71/44.29 | 0 to 12 |
| Chambers et al., 2021 (20) Canada |
2018 to 2019 | Retrospective | Administrative database | 244 | 62.30/37.70 | 0.50 to 87 |
| Van Yperen et al., 2021 (11) Netherlands |
2014 to 2018 | Retrospective | Dutch National Trauma Registry | 1,790 | N/A | N/A |
* at time of injury; ICD-9: International Classification of Diseases-9th revision; ICD-10: International Classification of Diseases-10th revision; SD: Standard Deviation; N/A: not available.
Table 3.
Referral criteria for the management of burn patients
|
Author/year
Criteria |
Description |
|---|---|
| Chipp et al., 2008 (14) BBA |
Criteria for Complex Bum
>15 % adults
|
|
Carter
et al.,
2010 (12); Davis
et al.,
2012 (13) & Chambers
et al.,
2021 (20)
ABA |
|
|
ose
et al.,
2010 (22)
NBCR |
Age
Under 5yrs and over 60yrs Site Involvement Face, Hands, Feet, Perineum, Flexures particularly neck or axilla, circumferential or full-thickness burns of limbs, torso, or neck Inhalation Injury Excluding pure carbon monoxide poisoning Mechanism of Injury
|
|
Baartmans
et al.,
2012 (18) & Van Yperen
et al.,
2021 (11)
EMSB |
|
|
Reiband
et al.,
2014 (21)
NBC |
|
|
Boissin
et al.,
2017 (19)
WCP |
|
TBSA: Total Body Surface Area; MI: Myocardial Infarction; BBA: British Burns Association; ABA: American Burn Association; NBCR: National Burn Care Review; EMSB: Emergency Management of Severe Burns; NBC: National Burn Center; WCP: Western Cape Provincial.
3. Results
3.1. Study selection
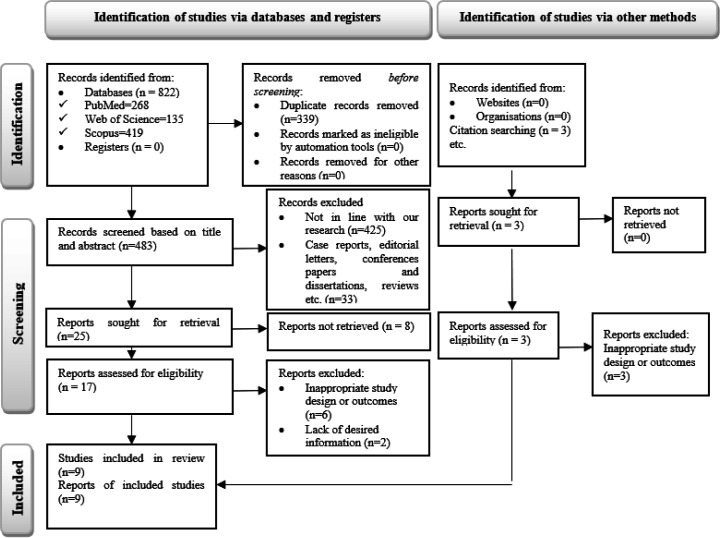
A total of 822 studies (PubMed=268, Web of Science=135, and Scopus=419) were obtained via an initial database search, and three studies were obtained using the assessment of the reference list of eligible studies. Also, 216 and 123 duplicate records were removed electronically and manually, respectively. In the screening stage of the title and abstract of studies, out of 483 studies, 425 articles were removed due to the obvious irrelevance of their topics with this research and 33 studies were excluded due to the type of the studies (animal studies, experimental studies, case reports, editorial letters, conferences papers and dissertations, reviews, etc). After assessment of the full-text of 17 studies, six articles were excluded due to inappropriate study design or outcomes and two articles were excluded due to lack of desired information. Finally, nine studies (11-14, 18-22) were included in this systematic review (Figure 1).
3.2. Study characteristics
Among the 7,455 burn patients included in the nine studies (11-14, 18-22), 60.95% were male. All studies had a retrospective design. Of the studies included, two were in the USA (12, 13), two were in the United Kingdom (14, 22), two were in the Netherlands (11, 18), one was in Canada (20), one was in Denmark (21), and one was in South Africa (19) (Table 2). Of the included studies, three studies assessed the ABA criteria (12, 13, 20), two studies evaluated the EMSB criteria (11, 18), one study assessed the BBA criteria (14), one study evaluated the National Burn Care Review (NBCR) criteria (22), one study assessed the National Burn Center (NBC) criteria (21), and one study evaluated the Western Cape Provincial (WCP) criteria (19) (Table 3).
3.3. Methodological Quality of included study
As presented in Figure 2, all included studies had justifications for sample size. Two studies did not define statistical significance. Six studies did not identify limitations. Four studies did not report funding sources or conflicts of interest, while four studies did not indicate the ethical approval/informed consent protocols used.
3.4. Characteristics of burn patients
As shown in Table 3, the average length of stay in the hospital for burn patients was seven days. The most frequently burned areas were the hands (n=3) (12, 20, 22) and the face (n=2) (14, 19). The most and least common burn mechanisms were scalds (62.76%) and electrical or chemical (2.88%), respectively (Figure 3). 51.88% of burn patients had met ≥ 1 referral criteria (Table 3).
3.5. Adherence to referral criteria for burn patients
The overall adherence to the referral criteria for burn patients was 58.28% (17.37 to 93.39%) (Table 4). The highest and lowest rates of adherence were related to WCP (26.70%) and NBCR (4.97%) criteria, respectively (Figure 4).
4. Discussion:
This systematic review showed that most frequently burned areas were the hands and the face. The most and least common burn mechanisms were scalds (62.76%) and electrical or chemical (2.88%), respectively. 51.88% of burn patients had met ≥ 1 referral criteria. The overall adherence to the referral criteria for burn patients was 58.28%. The highest and lowest adherence rates were related to WCP (26.70%) and NBCR (4.97%) criteria, respectively.
As presented in this study, most commonly burned areas were the hands and the face. The greater prevalence of burns on the hands and face can be expected because these body parts are not usually covered. However, differences in burn areas may be due to differences in variables such as culture, customs, habits, geopolitical and climatic location in different societies. For example, in wars such as the Iraq and Vietnam wars, most of the injured areas were the face and hands due to explosions (23). Sunburn on the hands and the face is more common in parts of Spain and on cyclists (24). Therefore, although most burns occur on the hands and face, further studies are needed to assess the factors associated with it.
Based on the present study's findings, the most and least common burn mechanisms were scalds (62.76%) and electrical or chemical (2.88%), respectively. Scalds are more common in children (under 14 years old) and are caused by hot liquids. This finding was supported by a study in Iraq (25). Children are more prone to scalds at home due to their mobility. On the other hand, electrical and chemical burns are less common due to lower exposure of people. However, it is suggested that future studies pay more attention to different age groups in different types of burns.
As presented in the present study, 51.88% of burn patients had met ≥ 1 referral criteria. There were differences in the number of referral criteria met in the studies, which can be explained by different referral criteria, family preferences, distance to the burn center, and insurance status (11).
The overall adherence to the referral criteria for burn patients was 58.28%. Also, the highest and lowest adherence rates were related to WCP (26.70%) and NBCR (4.97%) criteria, respectively. However, there were many differences in studies in terms of adherence to referral criteria. For example, a study in South Africa found that adherence to the referral criterion is 93.4% (19). In contrast, another study in the United Kingdom found that this adherence was 25.31% (14). This discrepancy may be due to differences in study design, applicable referral criteria, outcome criteria, and definition of adherence between different studies (11, 14, 19).
4.1. Implications for education, practice, and management
Adherence to referral criteria for burn patients will improve patient outcomes and ensure that burn patients are managed according to the latest evidence-based approaches. Findings of this systematic review indicate that much improvement is needed in educating hospital staff regarding making the necessary and timely referrals of burn patients based on laid down criteria. This calls for strategies that can improve adherence to referral criteria and reduce burn complications. The creation of a comprehensive burn system under the supervision of a burn specialist and the development of standards and evidence-based protocols for burn control, allocation of sufficient resources to burn systems and units, the hiring of adequate human resources, appropriate burn dressing and care, development of appropriate programs for regular visits to patients by burn specialists, and holding appropriate workshops for patients and health care providers can help manage burn patients.
4.2. Implications for future research
The findings of this systematic review can help improve referral patterns in burn patients admitted to non-burn centers. However, not all referral criteria are appropriate for managing burn patients, and some require serious revision. There is also a need for further research on whether modifying some referral criteria or training physicians in non-burn centers can increase adherence to referral criteria.
4.3. Limitations
This systematic review had several limitations. Although this systematic review was conducted based on the PRISMA checklist, it was not registered in the international prospective register of systematic reviews (PROSPERO) database, and a public protocol does not exist. Despite a comprehensive systematic search in this review, researchers may not have found all studies published in this area. Also, language bias cannot be ignored because only English language studies were included in the present study.
5. Conclusion:
Although the overall adherence to the referral criteria for burn patients was relatively desirable, there is room for improvement. The highest and lowest adherence rates were related to WCP (26.70%) and NBCR (4.97%) criteria, respectively. Therefore, it is suggested to perform well-designed studies that will focus on interventions to improve adherence to referral criteria for burn patients in the future.
6. Declarations:
6.1. Acknowledgment
None
6.2. Authors’ contributions
Study concept and design by all authors; Data acquisition by all authors; Data interpretation by all authors; drafting the manuscript by all authors; Revision of the manuscript by all authors; the final version of the manuscript is approved by all authors.
6.3. Conflict of interest
The authors declare no conflict of interest.
6.4. Funding and support
None.
6.5. Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.Miri S, Mobayen M, Aboutaleb E, Ezzati K, Feizkhah A, Karkhah S. Exercise as a rehabilitation intervention for severe burn survivors: Benefits & barriers. Burns. 2022 doi: 10.1016/j.burns.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 2.Mobayen M, Ch MH, Ghazanfari MJ, Sadeghi M, Mirmasoudi SS, Feizkhah A, et al. Antibiotics as a two-edged sword: The probability of endotoxemia during burned wound treatment. Burns. 2022;48(3):730–1. doi: 10.1016/j.burns.2022.02.012. [DOI] [PubMed] [Google Scholar]
- 3.Mobayen M, Feizkhah A, Ghazanfari MJ, Toolaroud PB, Mobayen M, Osuji J, et al. Intraoperative three-dimensional bioprinting: A transformative technology for burn wound reconstruction. Burns. 2022 doi: 10.1016/j.burns.2022.03.014. [DOI] [PubMed] [Google Scholar]
- 4.Mobayen M, Ghazanfari MJ, Feizkhah A, Mobayen M, Zeydi AE, Karkhah S. Effects of COVID-19 pandemic on burns care. Burns. 2022 doi: 10.1016/j.burns.2022.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mobayen M, Ghazanfari MJ, Feizkhah A, Zeydi AE, Karkhah S. Machine learning for burns clinical care: Opportunities & challenges. Burns. 2022;48(3):734–5. doi: 10.1016/j.burns.2022.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Mobayen M, Zolfagharzadeh H, Feizkhah A, Ghazanfari MJ, Toolaroud PB, Mobayen M, et al. Application of cell appendages for the management of burn wounds. Burns. 2022 doi: 10.1016/j.burns.2022.05.004. [DOI] [PubMed] [Google Scholar]
- 7.Feizkhah A, Mobayen M, Ghazanfari MJ, Toolaroud PB, Vajargah PG, Mollaei A, et al. Machine learning for burned wound management. Burns. 2022 doi: 10.1016/j.burns.2022.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Jeschke MG, van Baar ME, Choudhry MA, Chung KK, Gibran NS, Logsetty S. Burn injury. Nat Rev Dis Primers. 2020;6(1):1–25. doi: 10.1038/s41572-020-0145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amir Alavi S, Mobayen MR, Tolouei M, Noursalehi I, Gholipour A, Gholamalipour N, et al. Epidemiology and outcome of burn injuries in burn patients in Guilan province, Iran. Qom Univ Med Sci J. 2013;7(5):35–41. [Google Scholar]
- 10.WH O. Burns . 2018. [Available from: https://www.who.int/en/news-room/fact-sheets/detail/burns.
- 11.Van Yperen DT, Van Lieshout EM, Nugteren LH, Plaisier AC, Verhofstad MH, Van der Vlies CH, et al. Adherence to the emergency management of severe burns referral criteria in burn patients admitted to a hospital with or without a specialized burn center. Burns. 2021;47(8):1810–7. doi: 10.1016/j.burns.2021.02.023. [DOI] [PubMed] [Google Scholar]
- 12.Carter JE, Neff LP, Holmes IV JH. Adherence to burn center referral criteria: are patients appropriately being referred? J Burn Care Res. 2010;31(1):26–30. doi: 10.1097/BCR.0b013e3181cb8efb. [DOI] [PubMed] [Google Scholar]
- 13.Davis JS, Dearwater S, Rosales O, Varas R, Quintana OD, Pizano L, et al. Tracking Non–Burn Center Care: What You Don't Know May Surprise You. J Burn Care Res. 2012;33(6):e263–7. doi: 10.1097/BCR.0b013e3182504450. [DOI] [PubMed] [Google Scholar]
- 14.Chipp E, Walton J, Gorman D, Moiemen NS. Adherence to referral criteria for burns in the emergency department. Eplasty. 2008;8:e26. [PMC free article] [PubMed] [Google Scholar]
- 15.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 16.Corlett RT. Trouble with the gray literature. Biotropica. 2011;43(1):3–5. [Google Scholar]
- 17.Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS) BMJ Open. 2016;6(12):e011458. doi: 10.1136/bmjopen-2016-011458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baartmans MG, Van Baar M, Boxma H, Dokter J, Tibboel D, Nieuwenhuis MK. Accuracy of burn size assessment prior to arrival in Dutch burn centres and its consequences in children: a nationwide evaluation. Injury. 2012;43(9):1451–6. doi: 10.1016/j.injury.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 19.Boissin C, Hasselberg M, Kronblad E, Kim S-M, Wallis L, Rode H, et al. Adherence to referral criteria at admission and patient management at a specialized burns centre: The case of the Red Cross War Memorial children’s hospital in Cape Town, South Africa. Int J Environ Res Public Health. 2017;14(7):732. doi: 10.3390/ijerph14070732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chambers SB, Garland K, Dai C, DeLyzer T. Adherence of Burn Outpatient Clinic Referrals to ABA Criteria in a Tertiary Centre: Creating Unnecessary Referrals? J Burn Care Res. 2021;42(6):1275–9. doi: 10.1093/jbcr/irab117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiband HK, Lundin K, Alsbjørn B, Sørensen AM, Rasmussen LS. Optimization of burn referrals. Burns. 2014;40(3):397–401. doi: 10.1016/j.burns.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Rose A, Hassan Z, Davenport K, Evans N, Falder S. Adherence to National Burn Care Review referral criteria in a paediatric emergency department. Burns. 2010;36(8):1165–71. doi: 10.1016/j.burns.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Kauvar DS, Wolf SE, Wade CE, Cancio LC, Renz EM, Holcomb JB. Burns sustained in combat explosions in Operations Iraqi and Enduring Freedom (OIF/OEF explosion burns) Burns. 2006;32(7):853–7. doi: 10.1016/j.burns.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Molinero DD, Paulano MR, Ruiz FR, Sánchez NB, de Gálvez Aranda MV, de Castro Maqueda G, et al. Sun Protection Behaviour and Sunburns in Spanish Cyclists. J Cancer Educ. . 2020:1–8. doi: 10.1007/s13187-020-01906-y. [DOI] [PubMed] [Google Scholar]
- 25.Al-Shamsi M, Othman N. The epidemiology of burns in Basra, Iraq. Ann Burns Fire Disasters. 2017;30(3):167–71. [PMC free article] [PubMed] [Google Scholar]