Abstract
Introduction:
Cyclic vomiting syndrome (CVS) is a functional gastrointestinal disorder which leads to multiple hospitalizations and causes significant impairment of quality of life. Cannabis use is common in patients with CVS, and there are limited data on the national trends in the prevalence of its use in the United States.
Methods:
We used the National Inpatient Sample (NIS) database from 2005 to 2014 and identified hospitalizations with a primary diagnosis of CVS by utilizing the International Classification of Diseases, 9th revision Clinical Modification (ICD-9 CM) coding system. The primary objective of the study was to analyze the prevalence and trends in cannabis use in CVS patients. We also assessed healthcare resource utilization associated with cannabis use.
Results:
A total of 129 090 hospitalizations with a primary diagnosis of CVS were identified and included in the study. In the United States, the overall rate of cannabis use among these patients was 104 per 1000 hospitalizations (N = 13 460). Over the last decade, the prevalence of cannabis use increased by 10-fold, from 2.2% in 2005 to 21.2% in 2014.
Conclusion:
Our analysis of the national database suggests that nearly 1 in 5 CVS hospitalizations have concurrent cannabis use. This prevalence is significantly rising over the last decade, perhaps due to changing legislation and increased utilization of cannabis. Age younger than 35, male gender, African American and Native American race, personal history of alcohol abuse and tobacco use were some of the strongest predictors of cannabis use.
Keywords: cannabis use, cyclic vomiting syndrome, healthcare cost and resource utilization, National Inpatient Sample Database
1 |. INTRODUCTION
Cyclic vomiting syndrome (CVS) is a complex functional gastrointestinal disorder with unclear pathogenesis and is characterized by recurrent episodes of nausea and vomiting.1–3 Although once thought to be the disease of childhood, CVS has been increasingly diagnosed in the adult population.4,5 Acute symptom flares of CVS result in significant impairment of physical health due to the inability to tolerate oral feeds and medications, serious dehydration and electrolyte abnormalities.6,7 Recurrent episodes of CVS flares also lead to poor quality of life.7 These symptom flares frequently require hospitalizations for intravenous hydration and medication administration.8,9 Previous studies have reported that the estimated burden of CVS related adult US hospitalizations was approximately $400 Million (US $) for the years of 2010 and 2011.8
There is a significant phenotypic overlap between cyclic vomiting syndrome and cannabinoid hyperemesis syndrome (CHS).10,11 Many CVS patients self-medicate with cannabis to alleviate the symptoms; hence, the distinction between these conditions becomes difficult to diagnose. However, both CVS and CHS are diagnostically distinct entities as classified by Rome IV criteria.6,11–14 The mainstay of basic management in both conditions is symptomatic care with intravenous hydration and control of nausea and vomiting. In addition to symptomatic and supportive care, there is documented effectiveness of the tricyclic antidepressants for the pharmacological management in cyclic vomiting syndrome.15–18
There has been a constant change in the US federal and state regulations pertaining to cannabis.9,19,20 At the federal level, The Controlled Substance Act of 1970 classifies cannabis as a scheduled 1 substance.21,22 Despite these regulations, it is one of the most commonly used substances in the United States. Medical use of cannabis has been legalized in 33 states, while its recreational use is legal in 10 states.19,22,23 As a result of changes in state regulations, the prevalence of cannabis use has been increasing in the hospitalized population within the United States.24,25 Several recent studies have also shown an increase in the number of CVS related hospitalizations after changes in the cannabis regulations in some states.8,9 There is a paucity of data exploring national trends of cannabis use in CVS patients. In the current study, we aimed to evaluate the national trends of cannabis use in cases hospitalized with CVS and identified the associated demographic characteristics in this patient population. We also analyzed the healthcare burden related to cannabis use among CVS hospitalizations.
2 |. METHODS
2.1 |. Data source
We used the Nationwide Inpatient Sample (NIS) database from 2005 to 2014. The NIS database is developed and maintained by the Healthcare Cost and Utilization Project (HCUP) and is utilized in decision making at the national, state and community levels. NIS database is the largest publicly available all-payer inpatient healthcare database in the United States. The HCUP is an initiative of the Agency for Healthcare Research and Quality (AHRQ). NIS database contains de-identified information regarding more than 7 million unweighted annual hospitalizations and 35 million weighted annual US hospital stays. From 2005 to 2014, NIS included around 7–8 million discharges yearly from 1051 to 4411 hospitals in 37–45 states throughout the United States. The NIS is the Unites States’ most comprehensive source of hospital data, which enables researchers to study healthcare delivery and patient outcomes. It is a discharge-level database which contains de-identified clinical and nonclinical data elements at both the patient and hospital level. As a result, multiple admissions for a single patient are considered separate discharges and are entered separately in the database. Patient-level data points include age, gender, race, income in the patient’s zip code and principal diagnosis (up to 29 secondary diagnoses using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9 CM) coding system, up to 15 procedures using the ICD-9 CM procedural codes). Hospital level data include hospital teaching status, bed size, and hospital location (urban/rural). The NIS also contains information regarding discharge disposition including death and resource utilization including length of hospital stay and total hospitalization charges.
2.2 |. Study population
Patients with a principal diagnosis of CVS were included in the study using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9 CM) coding system [ICD-9 CM code 536.2]. Patients were excluded if they were less than 18 years of age. We also excluded cases who had a secondary diagnosis of gastroparesis (N = 11 154), psychogenic vomiting syndrome (N = 53), postoperative nausea or vomiting (N = 15), and pregnancy-associated nausea vomiting. Patients with associated cannabis use were then identified. We reviewed previously published manuscripts on the topic and identified a reliable algorithm to select patients with cannabis use.9,24,25 The ICD-9 CM diagnostic codes used to identify cases are listed in the Appendix 1.
2.3 |. Study objectives and variables
The primary objective was to describe the prevalence and annual trends in cannabis use among patients hospitalized with cyclic vomiting syndrome. Secondary objectives were as follows: assess the resource utilization as measured by the length of hospital stay and total hospitalization cost; and, identify the independent predictors associated with the cannabis use. Multiple potential confounders were collected and accounted for during the analysis including age, gender, race, comorbidities with Elixhauser comorbidity index, number of procedures, insurance status and primary payer, hospital factors including region, hospital bed size, hospital location, and teaching status. Length of hospital stay, total hospitalization charges, and patients’ demographics were directly obtained from the NIS database. The Healthcare Cost and Utilization Project (HCUP) provides data that contains hospital-specific cost-to-charge ratios based on all-payer inpatient cost and are adjusted for inflation over the years using the consumer price index and presented in US dollars. Comorbidity burden was assessed using Elixhauser’s comorbidity index which is a method for measuring patient comorbidity based on ICD-9-CM diagnosis codes found in administrative data. 26
2.4 |. Statistical analysis
All statistical analyses were performed using the SPSS Statistical software v25.0 (IBM Corp, Chicago, Illinois). A bivariate analysis with Pearson’s chi-squared test was used to compare the demographics, covariates, and outcomes of interest among the study groups. Two-sided p-values were reported, and a value less than 0.05 was considered to be statistically significant. We used a multivariable logistic regression model to adjust for the pertinent demographic variables and confounders. The Healthcare Cost and Utilization Project (HCUP) comorbidity software was used to generate Elixhauser comorbidities from ICD-9 CM diagnosis codes. We adjusted for age, gender, race, insurance status, comorbidities, Elixhauser comorbidity index. We used general linear model and performed multivariate analysis to calculate adjusted mean differences in length of stay and hospital cost of care. The strength of association for cannabis use with patient and demographic characteristics was tested using multivariable regression analysis. The following variables were assessed to see if they independently predicted the likelihood of cannabis use in patients admitted with CVS: age, gender, race, comorbidities including alcohol abuse and depression, region and location of hospital, teaching status, and primary payer status.
3 |. RESULTS
3.1 |. Patient and hospital characteristics
A total of 129 090 hospitalizations with CVS as the primary diagnosis were included in our analysis. The mean age of the study cohort was 47.2 years, and 65.7% of patients were females. 58% (N = 75,483) of cases belonged to the age group 50 or below. The majority of the patients were Caucasians (72.1%) and with private insurance (36.3%), were cared for at large bed size hospitals (57.2%), and were weekday admissions (75.1%). Patient demographics have been summarized in Table 1.
TABLE 1.
Demographic characteristics of cases with CVS and cannabis use
| Cannabis use |
Total |
|||
|---|---|---|---|---|
| Baseline characteristic | No N = 115 630 (89.58%) |
Yes N = 13 460 (10.42%) |
N = 129 090 | P-value |
| Age (y) | ||||
| Mean (SD) | 48.99 (SD 18.53) | 32.37 (SD 10.77) | 47.28 (SD 18.59) | <0.001 |
| Age group | ||||
| 18–35 | 32 442 (28.1%) | 9240 (68.6%) | 41 682 (32.3%) | <0.001 |
| 36–50 | 30 719 (26.6%) | 3082 (22.9%) | 33 801 (26.2%) | |
| 51–65 | 28 358 (24.5%) | 1098 (8.2%) | 29 456 (22.8%) | |
| >65 | 24 111 (20.9%) | 40 (0.3%) | 24 151 (18.7%) | |
| Gender | ||||
| Men | 36 909 (31.9%) | 7359 (54.7%) | 44 268 (34.3%) | <0.001 |
| Women | 78 721 (68.1%) | 6101 (45.3%) | 84 822 (65.7%) | |
| Race | ||||
| White | 85 036 (73.5%) | 8004 (59.5%) | 93 040 (72.1%) | <0.001 |
| Black | 17 451 (15.1%) | 3528 (26.2%) | 20 979 (16.3%) | |
| Hispanic | 8181 (7.1%) | 1278 (9.5%) | 9459 (7.3%) | |
| Asian 0or Pacific islander | 1648 (1.4%) | 124 (0.9%) | 1772 (1.4%) | |
| Native American | 766 (0.7%) | 176 (1.3%) | 942 (0.7%) | |
| Other | 2548 (2.2%) | 350 (2.6%) | 2898 (2.2%) | |
| Insurance status: Primary expected payer | ||||
| Medicare | 39 165 (33.9%) | 1162 (8.6%) | 40 327 (31.2%) | <0.001 |
| Medicaid | 20 528 (17.8%) | 4494 (33.4%) | 25 022 (19.4%) | |
| Private insurance | 42 713 (36.9%) | 4191 (31.1%) | 46 904 (36.3%) | |
| Self-pay | 8644 (7.5%) | 2735 (20.3%) | 11 379 (8.8%) | |
| No charge | 799 (0.7%) | 247 (1.8%) | 1046 (0.8%) | |
| Other | 3781 (3.3%) | 631 (4.7%) | 4412 (3.4%) | |
| Region of hospital | ||||
| Northeast | 17 239 (14.9%) | 2978 (22.1%) | 20 217 (15.7%) | <0.001 |
| Midwest | 23 657 (20.5%) | 3310 (24.6%) | 26 967 (20.9%) | |
| South | 48 730 (42.1%) | 3705 (27.5%) | 52 435 (40.6%) | |
| West | 26 004 (22.5%) | 3467 (25.8%) | 29 471 (22.8%) | |
| Bed size of hospital | ||||
| Small | 19 633 (17.0%) | 2202 (15.0%) | 21 655 (16.8%) | <0.001 |
| Medium | 30 309 (26.2%) | 3271 (24.3%) | 33 580 (26.0%) | |
| Large | 65 688 (56.8%) | 8167 (60.7%) | 73 855 (57.2%) | |
| Location/teaching status of hospital | ||||
| Rural | 18 682 (16.2%) | 1333 (9.9%) | 10 015 (15.5%) | <0.001 |
| Urban non-teaching | 48 758 (42.2%) | 4245 (31.5%) | 53 003 (41.1%) | |
| Urban teaching | 48 190 (41.7%) | 7882 (58.6%) | 56 072 (43.4%) | |
| Admission day | ||||
| Weekday | 87 086 (75.3%) | 9913 (73.6%) | 96 999 (75.1%) | <0.001 |
| Weekend | 28 544 (24.7%) | 3547 (26.4%) | 323 091 (24.9%) | |
Abbreviation: SD, standard deviation.
3.2 |. Prevalence and trends of cannabis use in hospitalized CVS patients
Over the last decade, total CVS related hospitalizations increased by 60% from 2005 (N = 10 054) to 2014 (N = 16 140). We found that 10.4% (N = 13 460) of all hospitalizations with the primary diagnosis of CVS had a concurrent diagnosis of cannabis use. Prevalence of cannabis use in CVS patients increased by 10-fold from 2005 (2.2%) to 2014 (21.2%). Figure 1 shows the graphical presentation of the changes over last decade.
FIGURE 1.
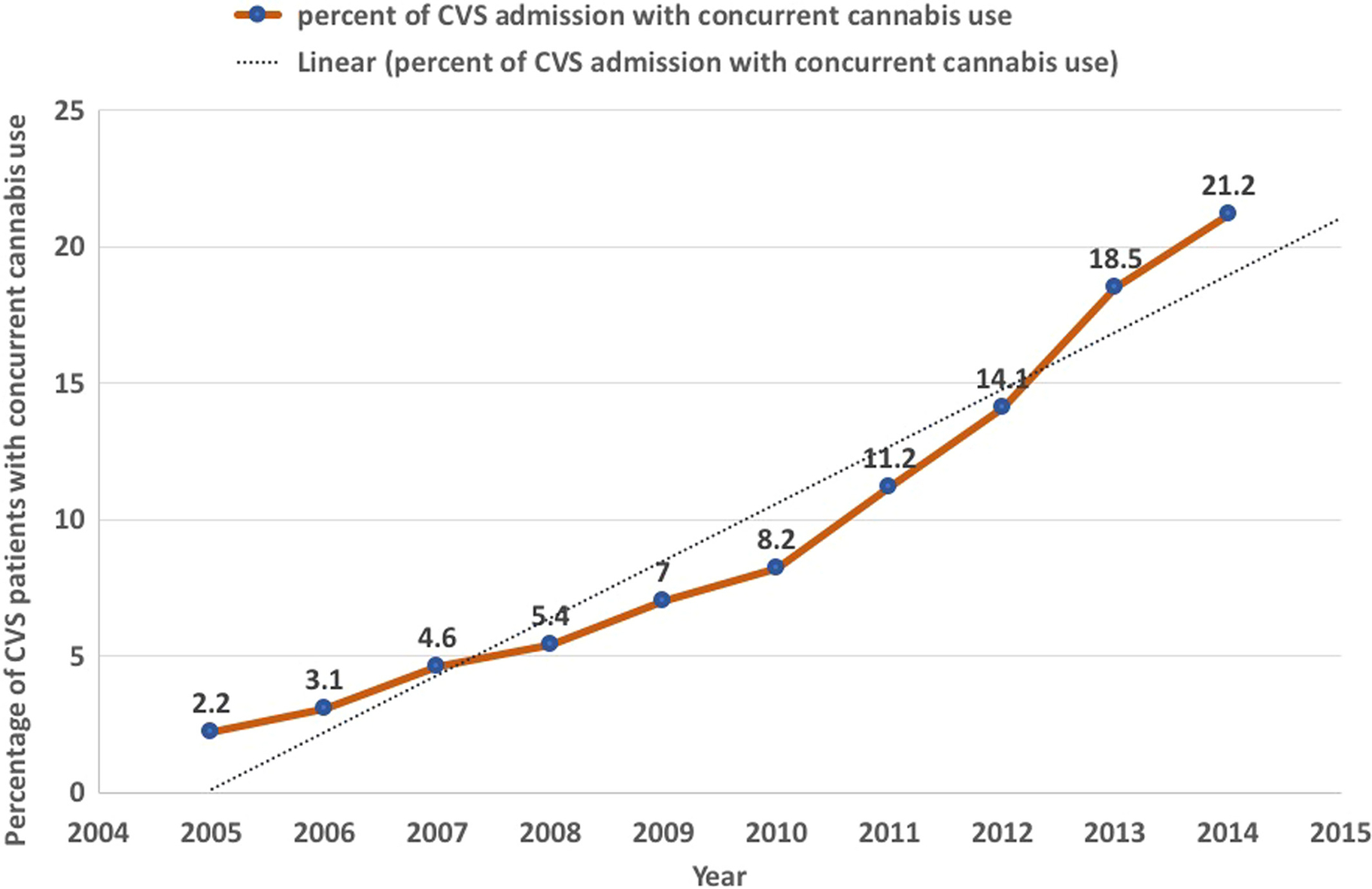
Graphical presentation of year-wise overall trend of cannabis use in CVS patients
We found a significant increase in the cannabis use among CVS patients below age 35 (Figure 2). In these patient populations, the prevalence of cannabis use increased from 57 per 1000 hospitalizations to 417 per 1000 hospitalizations over the last decade. In 2014, almost half of the hospitalized CVS patients below the age of 35 had a diagnosis of current cannabis use. Both prevalence and increase in the rate of cannabis use were consistently lower in older age groups. Prevalence was twice as much in men compared to women (Figure 3). While prevalence of cannabis use has increased in men and women both, the overall rate of increase was higher in women. We found that prevalence of cannabis use was higher in Native American, Black and Hispanic CVS patients when compared to Caucasians (Figure 4). A steady consistent increase in the prevalence of cannabis use was noted across all four regions in the United States. We noted the highest increase in cannabis use in US states in the Midwest region (Wisconsin, Michigan, Illinois, Indiana, Ohio, Missouri, North Dakota, South Dakota, Nebraska, Kansas, Minnesota, Iowa) (Figure 5).
FIGURE 2.
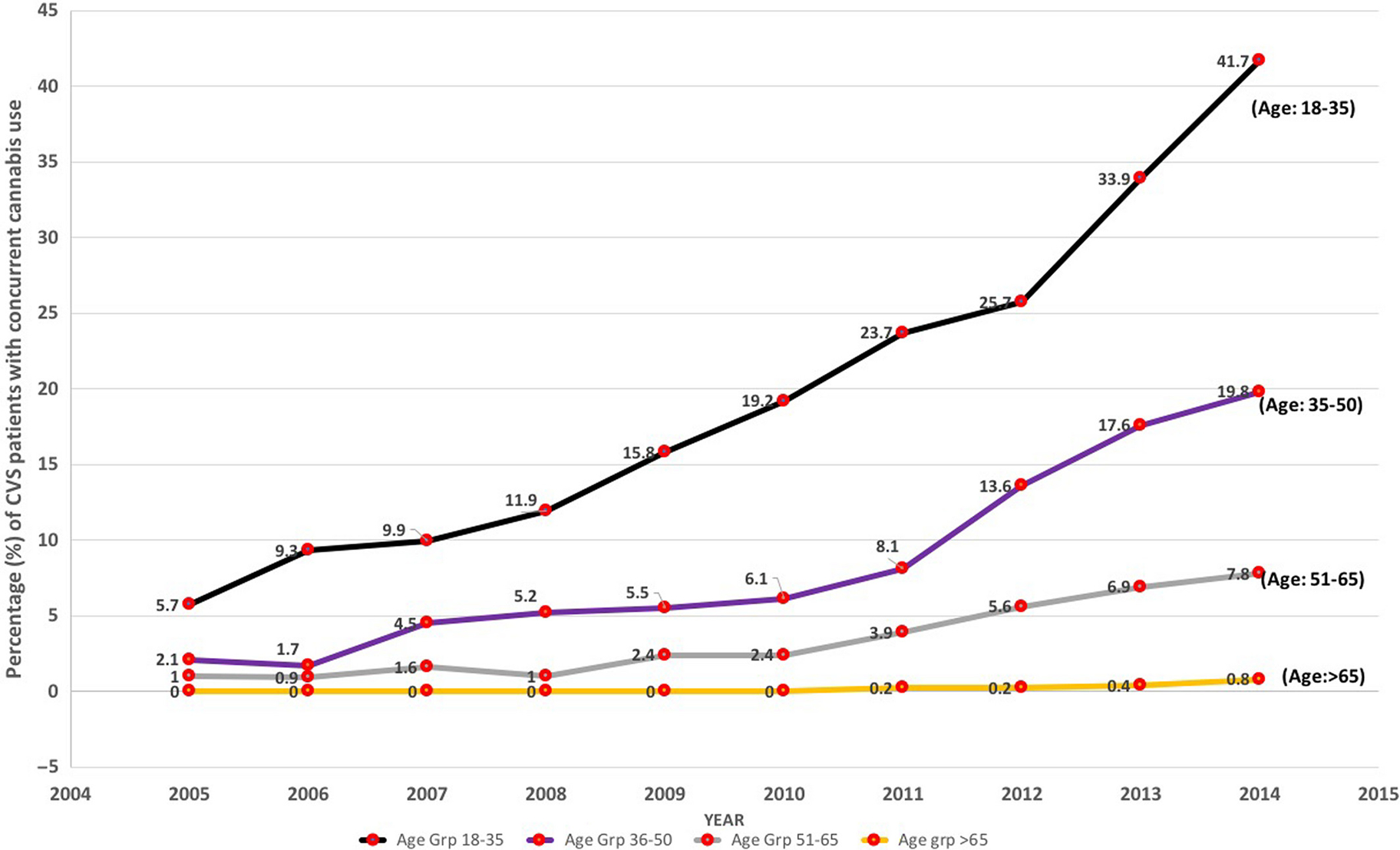
Comparison of trend of cannabis use across age groups
FIGURE 3.
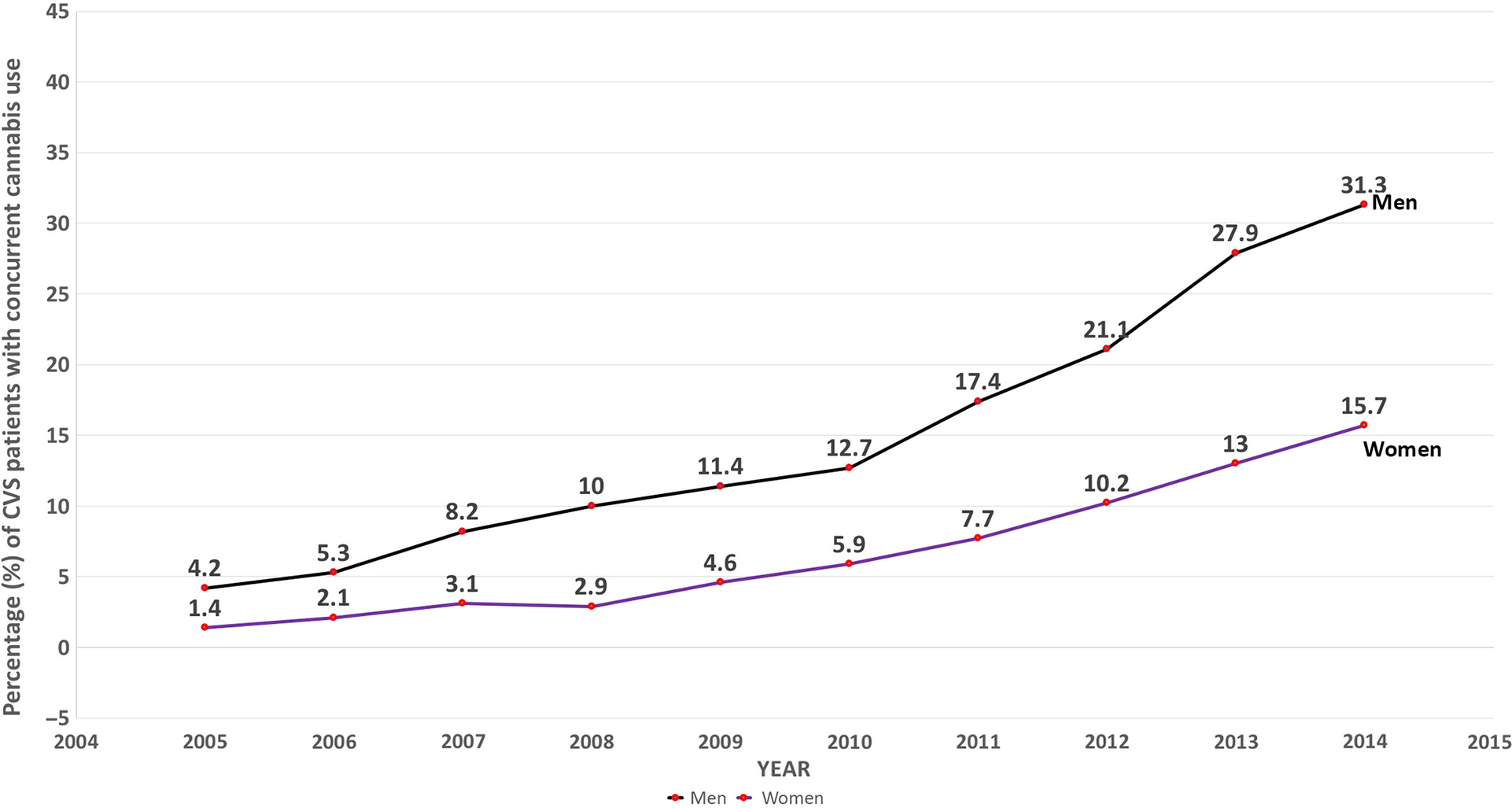
Comparison of trend of cannabis use across gender
FIGURE 4.

Comparison of trend of cannabis use across races
FIGURE 5.
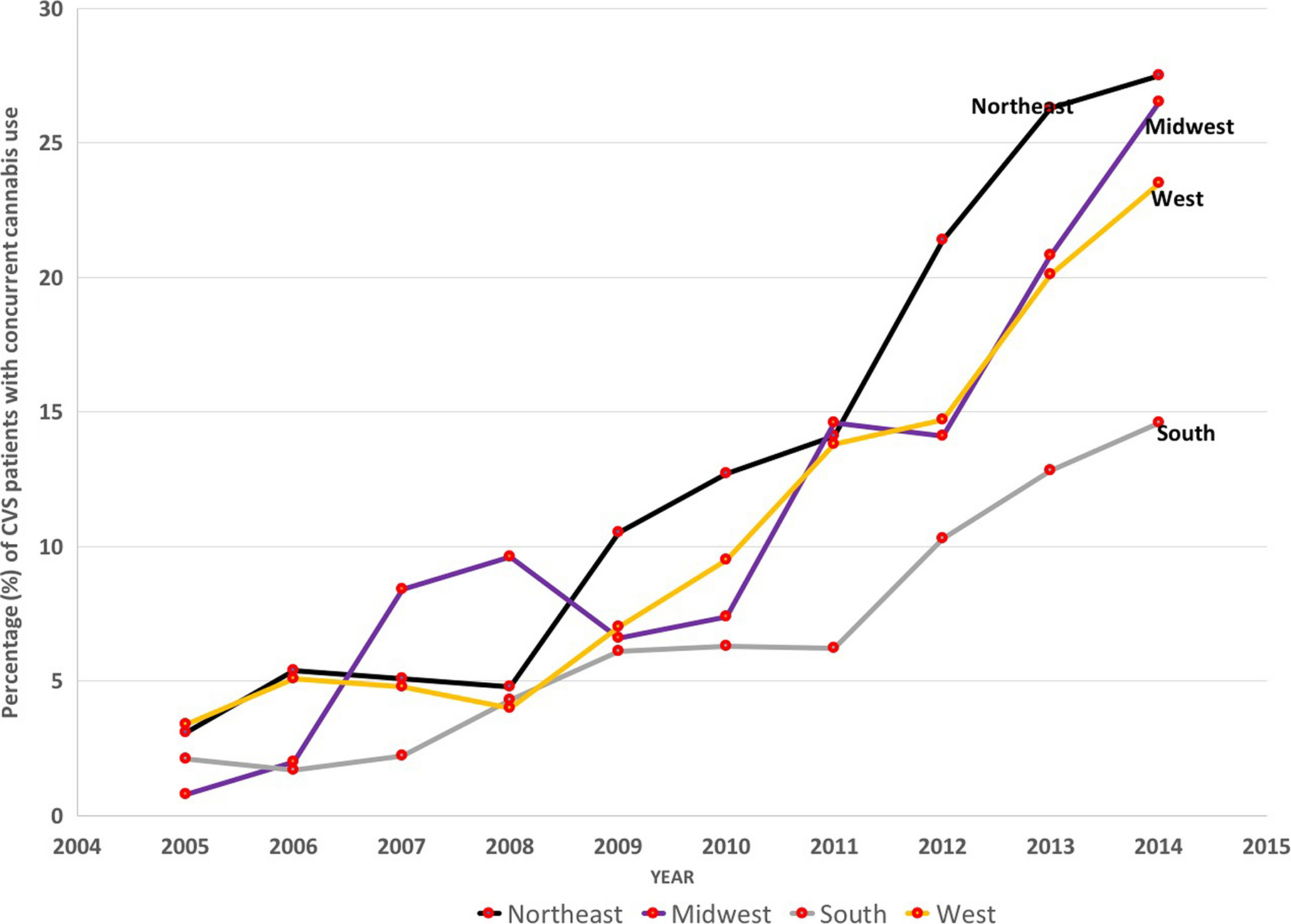
Comparison of trend of cannabis use across US regions
3.3 |. Healthcare resource utilization
The mean length of stay (LOS) in cannabis users (2.59 days) was shorter in comparison with those who did not use cannabis (3.56 days). We performed multivariate analysis for length of stay and adjusted for confounders including age, gender, race, insurance status, hospital region, hospital bed size and teaching status, weekend admissions, comorbidities with Elixhauser comorbidity index and in-hospital mortality. Despite these adjustments, LOS for cannabis users was relatively shorter. (Adjusted mean difference 0.28 days (95% confidence interval 0.197–0.376, P < .05). The mean total hospitalization cost for patients with cannabis use ($ 4831) was lower than those who did not use cannabis ($ 5813). After performing multivariate analysis and adjusting for confounders, we found that concurrent cannabis use did not have significant impact on healthcare-related cost. The mean adjusted difference in total hospitalization costs was $ −17.8 (P > .05).
3.4 |. Independent predictors for cannabis use in patients with CVS
Table 2 shows the independent predictors associated with cannabis use in patients with CVS. The variables found to independently increase the odds of cannabis use in these patients were younger age, male gender, personal history of generalized anxiety disorder and schizophrenia, concurrent alcohol and tobacco use, self-pay status, hospitalization in urban hospitals. CVS patients admitted in the western states were more likely to have concurrent cannabis use followed by midwestern and northeastern states
TABLE 2.
Multinomial logistic regression analysis of factors associated with cannabis use in cases admitted with primary diagnosis of CVS
| 95% confidence interval for adjusted OR |
||||
|---|---|---|---|---|
| Variable | Adjusted Odds Ratio | Lower limit | Upper limit | P-value |
| Age groups | ||||
| 18–35 | R | - | - | - |
| 36–50 | 0.411 | 0.391 | 0.432 | <0.001 |
| 51–65 | 0.208 | 0.194 | 0.223 | <0.001 |
| >65 | 0.017 | 0.013 | 0.024 | <0.001 |
| Gender | ||||
| Men | 2.251 | 2.158 | 2.349 | <0.001 |
| Women | R | - | - | |
| Race | ||||
| White | R | - | - | - |
| Black | 1.832 | 1.738 | 1.931 | <0.001 |
| Hispanic | 1.344 | 1.248 | 1.448 | <0.001 |
| Asian or Pacific Islander | 0.709 | 0.580 | 0.867 | 0.001 |
| Native American | 2.573 | 2.104 | 3.146 | <0.001 |
| Other | 1.304 | 1.144 | 1.486 | <0.001 |
| Alcohol abuse | ||||
| Yes | 1.858 | 1.706 | 2.024 | <0.001 |
| No | R | - | - | - |
| Tobacco use | ||||
| Yes | 2.898 | 2.770 | 3.030 | <0.001 |
| No | R | - | - | - |
| Generalized anxiety disorder | ||||
| Yes | 1.237 | 1.030 | 1.485 | 0.022 |
| No | R | - | - | - |
| Personal history of schizophrenia | ||||
| Yes | 2.457 | 0.607 | 10.0 | >0.05 |
| No | R | - | - | - |
| Depression | ||||
| Yes | 1.034 | 0.979 | 1.092 | >0.05 |
| No | R | - | - | - |
| Primary expected payer | ||||
| Medicare | R | - | - | - |
| Medicaid | 1.953 | 1.808 | 2.110 | <0.001 |
| Private insurance | 1.255 | 1.163 | 1.354 | <0.001 |
| Self-pay | 2.479 | 2.277 | 2.699 | <0.001 |
| No charge | 2.896 | 2.435 | 3.444 | <0.001 |
| Others | 1.669 | 1.483 | 1.877 | <0.001 |
| Hospital region | ||||
| Northeast | 0.894 | 0.840 | 0.950 | <0.001 |
| Midwest | 0.857 | 0.803 | 0.914 | <0.001 |
| South | 0.538 | 0.508 | 0.570 | <0.001 |
| West | R | - | - | - |
| Hospital bed size | ||||
| Small | 1.003 | 0.944 | 1.066 | >0.05 |
| Medium | 0.933 | 0.888 | 0.981 | 0.006 |
| Large | R | - | - | - |
| Location/teaching status of hospital | ||||
| Rural | 0.593 | 0.551 | 0.637 | <0.001 |
| Urban non-teaching | 0.614 | 0.586 | 0.644 | <0.001 |
| Urban teaching | R | - | - | - |
Abbreviation: R, reference category.
4 |. DISCUSSION
We used the largest nationwide all-payer inpatient database to evaluate the trends of cannabis use in patients hospitalized with cyclic vomiting syndrome. We found a steady increase in the prevalence of cannabis use in hospitalized CVS patients over the last decade. Among hospitalized CVS patients, a concurrent cannabis use did not result in a significant difference in healthcare resource utilization as measured by hospital LOS and total hospitalization cost.
Our study confirms the previously reported trend of an increase in cannabis use in the inpatient and the outpatient population within the United States. 24,25,27 Previously, Hasin et al reported that the prevalence of cannabis use has doubled from 4.5% to 9.5% in the last decade in adults in the United States and overall 30% of these cannabis users advance further and develop cannabis use disorder. 27,28 Charilau et al studied the NIS database and found a threefold increase in the prevalence of cannabis use in the hospitalized US population in the last decade. 25 We observed that this increase in prevalence of cannabis use was more substantial in CVS patients. We found that the prevalence of cannabis use in CVS patients has increased by 10-fold over the last decade. A previous study conducted by Bhandari et al utilized the Colorado state-inpatient-database and assessed the prevalence of cannabis use in CVS patients. Their study had found that the prevalence of cannabis use was 13% in CVS patients hospitalized in the state of Colorado.9 Our study found that the overall prevalence of cannabis use in CVS patients nationwide is slightly less at 10.5%. This lower rate is likely because our study population was representative of the national data. Over the last decade, the prevalence of cannabis use increased from 2.1% in 2005 to 21.4% in 2014, which means that nearly 1 in 5 admissions with the primary diagnosis of CVS had concurrent cannabis use. Our analysis showed that cannabis use was most prevalent in younger CVS patients and two-thirds of cannabis users belonged to the age group of 18 to 35. We also studied the trends of cannabis use and found that the population between ages 35 and 50 was the group which showed the most striking increase in cannabis use from 2.0% in 2005 to 20.6% in 2014. A study by Charilaou et al evaluated the trend of cannabis use among hospitalized population and observed that cannabis use was decreasing in patients below age 50; however, in CVS patients our observation showed a consistent steady increase across all age groups. 25
We found that the majority of hospitalized CVS patients were women (67%); however, cannabis use was more common in men (55% of cannabis users were men). We also observed that cannabis use is substantially increasing in women which showed 11-fold increase during the study period. Majority of CVS hospitalizations (72.1%) and cannabis users (59.5%) were Caucasians. In 2014, highest prevalence of cannabis was noted in African Americans (28.9%), followed by Hispanics (25.6%). During our study period, the highest increase in cannabis use was observed in Hispanic CVS patients (21-fold increase) while the increase in cannabis use was relatively similar for Caucasians and African Americans with overall ninefold increase in the prevalence. The prevalence of cannabis use was consistently on the rise across all regions within the United States. Interestingly, it remained comparatively lower in the southern states. We found that CVS patients hospitalized in the Midwest showed the highest (33-fold) increase in the prevalence from 2005 to 2014. Overall, we observed a consistent increase in cannabis use across all of the studied demographics.
Multiple factors could be playing a role in this effect which resulted in a consistent increase in cannabis use. This observed increase is likely due to the impact of changes in the legislation and legalization of marijuana use for both medical and recreational use. Additionally, cannabis is increasingly being studied for its utility in several medical conditions and has also shown promising results in many of these studies. 12,29–34 Cannabis has shown usefulness for gastrointestinal disorders such as irritable bowel syndrome, Crohn’s disease, and ulcerative colitis by alleviating nausea and optimizing nutritional status. 35–38 Another reason for the increase in cannabis use is the changes in public perception regarding cannabis. 39–41 Currently, the majority of American people support cannabis legalization and a record high support has been documented in recent years. 42–45 Fewer Americans perceive cannabis use as risky. 41,46 Previous studies have shown that with the decrease in the perceived risk, the usage of marijuana has increased.47 Despite the general perception in its favor, cannabis use has continued to be an important public health concern with many studies showing adverse outcome related to cannabis use, such as cognitive decline,48 psychosis,49,50 poor quality of life,51 adverse effect on male reproductive system and fertility,52 worse pregnancy outcomes 53 and a spectrum of cardiovascular 54,55 and neurological complications.56,57 Therefore, caution is indicated in the utilization of cannabis.
We compared the differences in healthcare utilization in CVS patients based on their cannabis use status. We used the length of stay (LOS) and hospital cost of care as a surrogate for healthcare utilization. We accounted for the confounding effects of demographic and clinical confounders and calculated the adjusted length of stay and the adjusted cost of care. In our study, we did not find a substantial difference in LOS and the cost of care between cannabis users and nonusers. Our finding suggests that cannabis use was not associated with an increase in the utilization of healthcare resources in patients hospitalized with CVS.
In our study, we identified several risk factors associated with an increased likelihood of cannabis use in CVS patients. We found that age less than 35 and male gender were the strongest demographic predictors of concurrent cannabis use. We also found that the Native American CVS patients had the highest risk of cannabis use followed by African Americans and Hispanics. We observed that CVS patients with concurrent tobacco and alcohol abuse were also more likely to be cannabis users. In regards to the associated psychiatric comorbidities, we did not find a significant association of cannabis use with the personal history of schizophrenia and depression; however, our analysis showed that the CVS patients with concurrent anxiety were more likely to have cannabis use. CVS patients admitted to a large urban teaching hospital had higher odds of using cannabis. Patients admitted in the western states of the United States were more likely to use cannabis in comparison with other regions. These predictors can help the clinician in identifying CVS patients with a higher likelihood of concurrent cannabis use.
Our study has several limitations. This study is a large database observational study that does not allow for an individual chart review. Moreover, our data were obtained from an administrative database. It has been documented that claims-based databases are susceptible to inaccurately entered or missing codes. Our study is retrospective, and even though we used a robust statistical analysis to adjust for confounding factors, there is still a risk for residual confounding. We would also like to highlight that this perceived increase in cannabis use could at least partially be due to more established guidelines in diagnosing CVS. Rome criteria for CVS were established in 2006 and knowledge about this condition has increased since then. 6 CHS was also first described in 2004 and awareness regarding the association of cannabis with these disorders has also increased. Therefore, the recognition bias could be contributing to both the observed trends in the increase in hospitalizations due to CVS, as well as, the increase in the documented cannabis use in CVS patients. 58 Another limitation of the current study is due to possible differences and errors in reporting of cannabis use for different US states because the current study includes the states where cannabis is legal, as well as, those where cannabis use is still not legalized.
Despite these limitations, our study has several strengths. It provides a broader overview of the national landscape as it analyzes the nationwide trend of cannabis use among CVS patients. It uses the largest publicly available national inpatient database. The use of such a database minimizes the biases seen in the single-center or even smaller multi-center studies. This makes the results more generalizable across the country. With increases in cannabis legalization in the United States, the overall prevalence of cannabis use in CVS patients is expected to continue to rise. It is important to take note of this change in the national trend of cannabis use and to identify the risk factors associated with cannabis use.
In conclusion, the prevalence of cannabis use is increasing in patients with CVS and one out of five hospitalizations with CVS has concurrent cannabis use. Further larger prospective studies are needed to validate our findings.
Supplementary Material
Key Message.
Cannabis use has increased by 10-fold in patients hospitalized with CVS between 2005 to 2014. This could be due to the legalization of cannabis for both medical and recreational use in multiple states in the United States.
Predictors of cannabis use in CVS patients include younger age, male gender, race (Native American, African American and Hispanic), personal history of alcohol abuse, tobacco use and psychiatric disorders (Generalized anxiety disorder).
Patients with CVS who used cannabis had a lower overall length of stay and hospitalization cost.
Footnotes
CONFLICT OF INTEREST
Authors do not have any financial or non-financial disclosure, and there is no conflict of interest.
REFERENCES
- 1.Lacy BE, Parkman HP, Camilleri M. Chronic nausea and vomiting: evaluation and treatment. Am J Gastroenterol. 2018;113(5):647–659. [DOI] [PubMed] [Google Scholar]
- 2.Sagar RC, Ford AC. Cyclic vomiting syndrome: randomized controlled trials are also needed in adults. Am J Gastroenterol. 2017;112(11):1752–1753. [DOI] [PubMed] [Google Scholar]
- 3.Kovacic K, Sood M, Venkatesan T. Cyclic vomiting syndrome in children and adults: what is new in 2018? Curr Gastroenterol Rep. 2018;20(10):46. [DOI] [PubMed] [Google Scholar]
- 4.Davis A, Bryant JH. Cyclic Vomiting Syndrome. Treasure Island (FL): StatPearls;2018. [PubMed] [Google Scholar]
- 5.Prakash C, Staiano A, Rothbaum R, Clouse RE. Similarities in cyclic vomiting syndrome across age groups. Gastroenterology. 2000;118(4):A476. [DOI] [PubMed] [Google Scholar]
- 6.Hayes WJ, VanGilder D, Berendse J, Lemon MD, Kappes JA. Cyclic vomiting syndrome: diagnostic approach and current management strategies. Clin Exp Gastroenterol. 2018;11:77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pareek N, Fleisher DR, Abell T. Cyclic vomiting syndrome: what a gastroenterologist needs to know. Am J Gastroenterol. 2007;102(12):2832–2840. [DOI] [PubMed] [Google Scholar]
- 8.Bhandari S, Venkatesan T. Clinical characteristics, comorbidities and hospital outcomes in hospitalizations with cyclic vomiting syndrome: a nationwide analysis. Dig Dis Sci. 2017;62(8):2035–2044. [DOI] [PubMed] [Google Scholar]
- 9.Bhandari S, Jha P, Lisdahl KM, Hillard CJ, Venkatesan T. Recent Trends in cyclic vomiting syndrome - associated hospitalizations with liberalization of cannabis use in the State of Colorado. Intern Med J. 2018. [DOI] [PubMed] [Google Scholar]
- 10.Makani R, Parikh T. Psychiatric comorbidities with cyclic vomiting syndrome. Am J Psychiatry Residents’ J. 2017;12(11):4–6. [Google Scholar]
- 11.Aziz I, Palsson OS, Whitehead WE, Sperber AD, Simrén M, Törnblom H. Epidemiology, clinical characteristics, and associations for Rome IV functional nausea and vomiting disorders in adults. Clin Gastroenterol Hepatol. 2019;17:878–886. [DOI] [PubMed] [Google Scholar]
- 12.Adejumo AC, Li J, Akanbi O, Adejumo KL, Bukong TN. Reduced prevalence of alcoholic gastritis in hospitalized individuals who consume cannabis. Alcohol Clin Exp Res. 2018;43:270–276. [DOI] [PubMed] [Google Scholar]
- 13.Pattathan MB, Hejazi RA, McCallum RW. Association of marijuana use and cyclic vomiting syndrome. Pharmaceuticals. 2012;5(7):719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu X, Villamagna A, Yoo J. The importance of recognizing cannabinoid hyperemesis syndrome from synthetic marijuana use. J Med Toxicol. 2017;13(2):199–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee LY, Abbott L, Mahlangu B, Moodie SJ, Anderson S. The management of cyclic vomiting syndrome: a systematic review. Eur J Gastroenterol Hepatol. 2012;24(9):1001–1006. [DOI] [PubMed] [Google Scholar]
- 16.Blumentrath CG, Dohrmann B, Ewald N. Cannabinoid hyperemesis and the cyclic vomiting syndrome in adults: recognition, diagnosis, acute and long-term treatment. Ger Med Sci. 2017;15:Doc06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sunku B Cyclic vomiting syndrome: a disorder of all ages. Gastroenterol Hepatol. 2009;5(7):507–515. [PMC free article] [PubMed] [Google Scholar]
- 18.Prakash C, Clouse RE. Cyclic vomiting syndrome in adults: clinical features and response to tricyclic antidepressants. Am J Gastroenterol. 1999;94(10):2855–2860. [DOI] [PubMed] [Google Scholar]
- 19.Corroon J, Kight R. Regulatory status of cannabidiol in the United States: a perspective. Cannabis Cannabinoid Res. 2018;3(1):190–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dilley JA, Hitchcock L, McGroder N, Greto LA, Richardson SM. Community-level policy responses to state marijuana legalization in Washington State. Int J Drug Policy. 2017;42:102–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drug Enforcement Administration DoJ. Schedules of controlled substances: placement in schedule V of certain FDA-approved corresponding change to permit requirements drugs containing cannabidiol; Corresponding Change to Permit Requirements. Final order. Fed Regist. 2018;83(189):48950–48953. [PubMed] [Google Scholar]
- 22.Hoffmann DE, Weber E. Medical marijuana and the law. N Engl J Med. 2010;362(16):1453–1457. [DOI] [PubMed] [Google Scholar]
- 23.Mead A The legal status of cannabis (marijuana) and cannabidiol (CBD) under U.S. law. Epilepsy Behav. 2017;70(Pt B):288–291. [DOI] [PubMed] [Google Scholar]
- 24.Patel RS, Katta SR, Patel R, et al. Cannabis use disorder in young adults with acute myocardial infarction: trend inpatient study from 2010 to 2014 in the United States. Cureus. 2018;10(8):e3241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charilaou P, Agnihotri K, Garcia P, Badheka A, Frenia D, Yegneswaran B. Trends of cannabis use disorder in the inpatient: 2002 to 2011. Am J Med. 2017;130(6):678–687.e677. [DOI] [PubMed] [Google Scholar]
- 26.Menendez ME, Neuhaus V, van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472(9):2878–2886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hasin DS, Saha TD, Kerridge BT, et al. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72(12):1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arterberry BJ, Treloar Padovano H, Foster KT, Zucker RA, Hicks BM. Higher average potency across the United States is associated with progression to first cannabis use disorder symptom. Drug Alcohol Depend. 2019;195:186–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adejumo AC, Adegbala OM, Adejumo KL, Bukong TN. Reduced incidence and better liver disease outcomes among chronic HCV infected patients who consume cannabis. Can J Gastroenterol Hepatol. 2018;2018:9430953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor BN, Sauls RS. Cannaboinoid Antiemetic Therapy. Treasure Island (FL): StatPearls; 2018. [PubMed] [Google Scholar]
- 31.Adejumo AC, Akanbi O, Adejumo KL, Bukong TN. Reduced risk of alcohol-induced pancreatitis with cannabis use. Alcohol Clin Exp Res. 2018. [DOI] [PubMed] [Google Scholar]
- 32.Hawkes N Cannabis based drugs: how will they be used in practice? BMJ. 2018;363:k4665. [DOI] [PubMed] [Google Scholar]
- 33.Milando R, Friedman A. Cannabinoids: potential role in inflammatory and neoplastic skin diseases. Am J Clin Dermatol. 2018. [DOI] [PubMed] [Google Scholar]
- 34.Rubin R The path to the first FDA-approved cannabis-derived treatment and what comes next. JAMA. 2018;320(12):1227–1229. [DOI] [PubMed] [Google Scholar]
- 35.Gonzalez-Rosales F, Walsh D. Intractable nausea and vomiting due to gastrointestinal mucosal metastases relieved by tetrahydrocannabinol (dronabinol). J Pain Symptom Manage. 1997;14(5):311–314. [DOI] [PubMed] [Google Scholar]
- 36.Swaminath A, Berlin EP, Cheifetz A, et al. The role of cannabis in the management of inflammatory bowel disease: a review of clinical, scientific, and regulatory information: commissioned by the Crohn’s and Colitis Foundation. Inflamm Bowel Dis. 2019;25(3): 427–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kafil TS, Nguyen TM, MacDonald JK, Chande N. Chande N: Cannabis for the treatment of Crohn’s disease. Cochrane Database Syst Rev. 2018;11:CD012853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kafil TS, Nguyen TM, MacDonald JK, Chande N. Chande N: Cannabis for the treatment of ulcerative colitis. Cochrane Database Syst Rev. 2018;11:CD012954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blevins CE, Marsh E, Banes KE, Stephens RS, Walker DD, Roffman RA. The implications of cannabis policy changes in Washington on adolescent perception of risk, norms, attitudes, and substance use. Subst Abuse. 2018;12:1178221818815491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leos-Toro C, Shiplo S, Hammond D. Perceived support for medical cannabis use among approved medical cannabis users in Canada. Drug Alcohol Rev. 2018;37(5):627–636. [DOI] [PubMed] [Google Scholar]
- 41.Parker MA, Anthony JC. A prospective study of newly incident cannabis use and cannabis risk perceptions: results from the United States Monitoring the Future study, 1976–2013. Drug Alcohol Depend. 2018;187:351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hartig H About six-in-ten Americans support marijuana legalization. http://www.pewresearch.org/fact-tank/2018/10/08/americans-support-marijuana-legalization/ Last accessed Dec 2018. 2018.
- 43.Poll: Majority in U.S. Support Medical Pot https://www.webmd.com/pain-management/news/20180730/poll-majority-in-us-support-medical-pot#1 Last accessed Dec 2018.
- 44.Poll: Legal Marijuana Support At Record High In U.S. https://www.forbes.com/sites/tomangell/2017/10/25/poll-legal-marijuana-support-at-record-high-in-us Last accessed Dec 2018.
- 45.Two in Three Americans Now Support Legalizing Marijuana https://news.gallup.com/poll/243908/two-three-americans-support-legalizing-marijuana.aspx Last accessed Dec 2018.
- 46.Pacek LR, Mauro PM, Martins SS. Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend. 2015;149:232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109(40):E2657–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Di Forti M, Marconi A, Carra E, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry. 2015;2(3):233–238. [DOI] [PubMed] [Google Scholar]
- 50.Sewell RA, Ranganathan M, D’Souza DC. Cannabinoids and psychosis. Int Rev Psychiatry. 2009;21(2):152–162. [DOI] [PubMed] [Google Scholar]
- 51.Lev-Ran S, Imtiaz S, Taylor BJ, Shield KD, Rehm J, Le Foll B. Gender differences in health-related quality of life among cannabis users: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2012;123(1–3):190–200. [DOI] [PubMed] [Google Scholar]
- 52.Hsiao P, Clavijo RI. Adverse effects of cannabis on male reproduction. Eur Urol Focus. 2018;4(3):324–328. [DOI] [PubMed] [Google Scholar]
- 53.Petrangelo A, Czuzoj-Shulman N, Balayla J, Abenhaim HA. Cannabis abuse or dependence during pregnancy: a population-based cohort study on 12 million births. J Obstet Gynaecol Can. 2019;41(5):623–630. [DOI] [PubMed] [Google Scholar]
- 54.Goyal H, Awad HH, Ghali JK. Role of cannabis in cardiovascular disorders. J Thorac Dis. 2017;9(7):2079–2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cottencin O, Karila L, Lambert M, et al. Cannabis arteritis: review of the literature. J Addict Med. 2010;4(4):191–196. [DOI] [PubMed] [Google Scholar]
- 56.Rumalla K, Reddy AY, Mittal MK. Recreational marijuana use and acute ischemic stroke: a population-based analysis of hospitalized patients in the United States. J Neurol Sci. 2016;364:191–196. [DOI] [PubMed] [Google Scholar]
- 57.Wolff V, Lauer V, Rouyer O, et al. Cannabis use, ischemic stroke, and multifocal intracranial vasoconstriction: a prospective study in 48 consecutive young patients. Stroke. 2011;42(6):1778–1780. [DOI] [PubMed] [Google Scholar]
- 58.Allen JH, de Moore GM, Heddle R, Twartz JC. Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut. 2004;53(11):1566–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


