Highlights
-
-
Kyrieleis arteritis is a rare manifestation in posterior uveitis
-
-
Kyrieleis arteritis is most frequently reported in ocular toxoplasmosis.
-
-
The pathogenesis still highly debated.
-
-
It is characterized by the presence of focal, segmental plaques or exudates within retinal arteries.
-
-
These plaques are usually reversible.
-
-
The prognosis is usually good.
1. Introduction
Kyrieleis arteritis, also known as segmental retinal arteritis (SRA) is a rare condition, with not completely known pathogenesis. First described by Werner Kyrieleis in 1933 [1]. It is characterized by the presence of focal, segmental plaques or exudates within retinal arteries. These plaques are usually reversible. SRA has been reported essentially in infectious posterior uveitis and has been rarely reported in inflammatory posterior uveitis (Behçet disease and sarcoidosis). SRA have been described frequently in ocular toxoplasmosis and may be its initial manifestation. The plaques are typically situated near or distant from the retinitis or retinochoroiditis and they usually involve the proximal branches of the central retinal artery [2]. This case report has been reported in line with the SCARE criteria [3].
2. Case presentation
A 60-year-old immunocompetent woman presented at our department of ophthalmology in Sousse Tunisia, with a 1-week history of floaters and decreased vision in the right eye (RE). Her past history was significant for systemic hypertension.
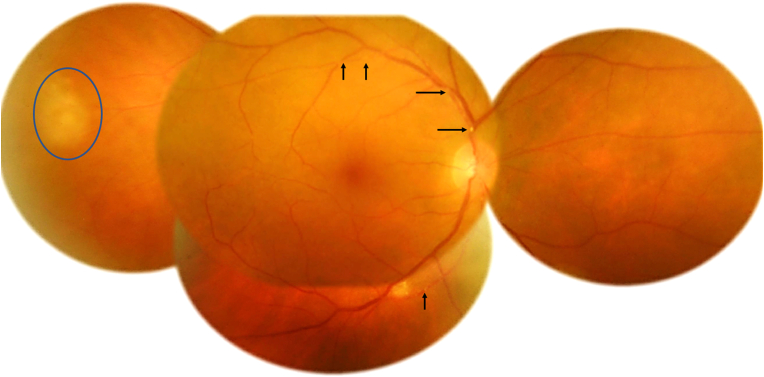
On initial examination, best corrected visual acuity (BCVA) was 20/50 in the RE and 20/20 in the left eye. Intra ocular pressures were normal. Slit-lamp examination of the RE revealed 2+ of anterior chamber cellular activity. There were no keratic precipitates nor synechiae. Dilated examination of the posterior segment revealed 2+ vitritis and 2+ haze. Fundus examination showed a segmental retinal arteritis with small white plaques placed in a beaded pattern affecting temporal branches of the central retinal artery as well as a focal area of retinochoroiditis in the temporal periphery (Fig. 1).
Fig. 1.
Fundus photograph of the right eye exhibiting segmental retinal arteritis with small white plaques placed in a beaded pattern affecting temporal branches of the central retinal artery (black arrows) as well as a focal area of retinochoroiditis in the temporal periphery (blue circle). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
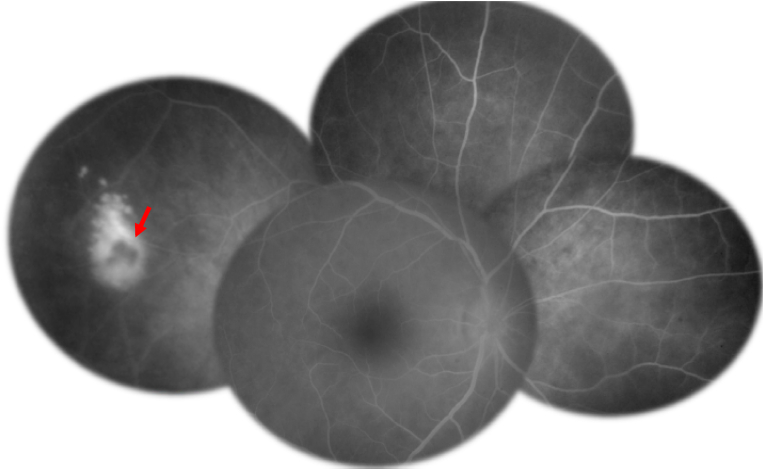
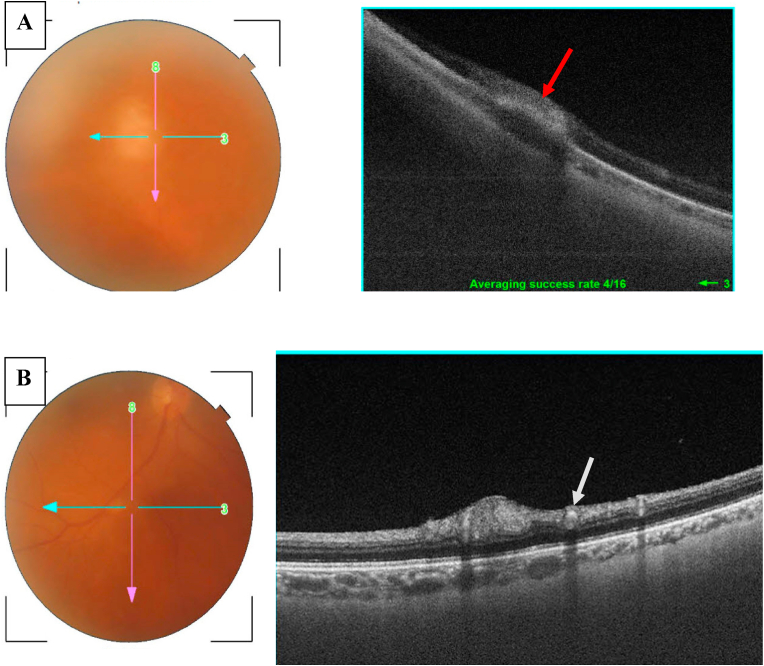
Fluorescein angiography (FA) of the RE showed a centripetal impregnation of the retinitochoroiditis. The arterial plaques did not demonstrate any phenomenon of filling defects or leakage of fluorescein dye (Fig. 2). Swept source OCT of the retinochoroiditis exhibited a focal area of retinal hyperreflectivity with choroidal thickening (Fig. 3-A) and OCT scan along the arterial plaque revealed hyperreflectivity of the wall with normoreflective lumen (Fig. 3-B).
Fig. 2.
Fluorescein angiography of the right eye showing a centripetal impregnation of the retinochoroiditis (red arrow). The arterial plaques did not demonstrate any phenomenon of filling defects or leakage of fluorescein dye. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
A: Swept source OCT of the retinochoroiditis exhibiting a focal area of retinal hyperreflectivity with choroidal thickening (red arrow). B: OCT scan along the arterial plaque revealing hyperreflectivity of the wall with normoreflective lumen (white arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Laboratory tests revealed positive serum antibodies to Toxoplasma gondii detected by enzyme-linked immunosorbent assay (ELISA) technique: anti-Toxoplasma IgG titer=>300 with high level of IgM (titer = 1.3). The patient tested negative for human deficiency virus (HIV) by ELISA technique and TPHA, VDRL tests were negative. Chest X ray was normal and Mantoux test was negative.
The diagnosis of a presumed acquired toxoplasmic retinochoroiditis with associated segmental retinal arteritis was made and the patient was treated with pyrimethamine 100 mg loading dose then 50 mg daily, folinic acid 15 mg daily associated with azithromycin 500 mg loading dose then 250 mg. Forty-eight hours after introducing antiparasitic treatment, the patient received 60 mg per day oral prednisolone (0.75 mg per kilogram of body weight). The treatment was continued for a total duration of 6 weeks with progressive tapering of the corticosteroids. The patient also received dexamethasone and mydriatics eyedrops initially to control the pain and the anterior segment inflammation.
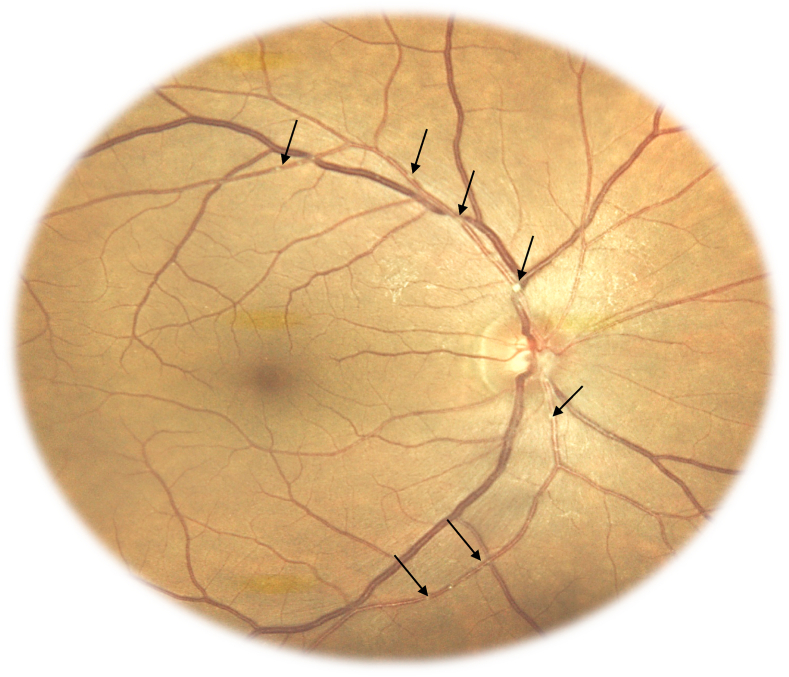
Three weeks after the initiation of the treatment, BCVA in RE was 20/25, the inflammatory reaction of the anterior segment disappeared and vitreous inflammation receded. The arterial plaques were still present and more visible and there was a decrease in the size of retinochoroiditis (Fig. 4).
Fig. 4.
Fundus photograph of the right eye 3 weeks after the initiation of the treatment showing that vitreous inflammation has receded and the arterial plaques were still present and more visible (black arrows).
This case report has been reported in line with the SCARE criteria [3].
3. Discussion
Segmental retinal arteritis is a rare manifestation in posterior uveitis, most frequently reported in ocular toxoplasmosis [2]. Kyrieleis described this clinical entity in tuberculous uveitis in 1933 [1]. It is always associated with inflammation, reflecting its severity but it does not worsen the prognosis [4].
Only few cases have been reported in literature [4]. This rare condition has been reported particularly in association with infectious posterior uveitis: toxoplasmosis [5], syphilis [6], Mediterranean spotted fever [7], acute retinal necrosis due to HSV-2 [8], and VZV [9], but has also been described in posterior uveitis with inflammatory origin: Behçet disease and sarcoidosis [2].
SRA is characterized by the presence of white-yellowish exudates placed in a beaded pattern which do not extend beyond the thickness of the artery [4,10]. This entity should be differentiated from vascular sheathing and frosted branch angiitis where we notice the presence of inflammation in full thickness of the vascular wall, seen as vascular staining and leakage in FA. In SRA there is no evidence of occlusive phenomenon nor leakage, possibly because the inflammation is not transmural and limited to the endothelium [4]. In our case, the FA did not exhibit any staining nor leakage of the arterial walls.
Until this day, the composition of the arterial plaques in SRA and their position relative to the arterial wall still not yet been determined. Different hypotheses have been advanced about the pathogenesis of segmental arteritis.
Griffin and Bodian [11], hypothesized that the plaques represented exudates migration from an adjacent retinochoroiditis focus to the periarterial sheaths.
In 1960, Blach [12] supposed that the plaques could be either a focal inflammation of the arterial wall, or deposition formed by immune cells or amorphous inflammatory material.
Some authors speculated that these deposits were constituted of cellular and inflammatory material within the arterial walls [13].
A study of Pichi and al [4], tried to unravel the nature of the plaques. Based on multimodal retinal imaging, the study suggested that the plaques do not represent periarterial or endoluminal injury, but the inflammation of the arterial endothelium within the vessel wall itself. Consequently, it calls in question the validity of the term “periarteritis” and proposed to shift the nomenclature to “arteritis”.
In a recent study published in 2021 [14], authors described the vascular anatomy and intraluminal flow characteristics of segmental retinal arteritis using OCT and OCT angiography. They demonstrated that the plaques were associated with narrowing of the intraluminal flow signal on OCT angiography, and suggested that since SRA is also associated with indocyanine green signal during active inflammation, it is likely to be to a disruption in the arterial endothelium or medial vessel. In our case, the OCT scan along the arterial plaques shows a hyperreflectivity of the wall with normal reflectivity of the lumen.
Nevertheless, in absence of pathological exam of the plaques in SRA, their pathogenesis still highly debated.
4. Conclusion
Kyrieleis arteritis is a rare manifestation in posterior uveitis. Only few cases have been reported in literature. The composition of the arterial plaques in SRA and their position relative to the arterial wall still not yet been determined but multimodal imaging suggest that the plaques are associated with endothelial damage.
Ethical approval
None.
Sources of funding
No source of funding.
Author contribution
All authors made a significant contribution to this paper.
Trial registry number
1. Name of the registry:
2. Unique Identifying number or registration ID:
3. Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Guarantor: Ilhem Sellem M.D.
E-mail: Ilhem.sellem@gmail.com.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
The authors declare no conflict of interest.
Contributor Information
Ahmed Mahjoub, Email: mahjoubahmed68@yahoo.fr.
Nadia Ben Abdesslem, Email: nadiabenabdesslem@gmail.com.
Nesrine Zaafrane, Email: nzaafrane@gmail.com.
Ilhem Sellem, Email: ilhem.sellem@gmail.com.
Fedi Sahraoui, Email: fedishr@gmail.com.
Hela Nouri, Email: Nouri.hela05@gmail.com.
Rahma Bel Hadj, Email: belhadjrahma08@gmail.com.
Azer Ben Alaya, Email: benalayaazer40@gmail.com.
Fethi Krifa, Email: fkrifa@yahoo.fr.
Mahjoub Hachemi, Email: hachmi.mahjoub.oph@gmail.com.
References
- 1.Kyrieleis W. Uber atypische gerfaesstuberkulose der netzhaut. Arch. Augenheilkd. 1933;107:182–190. [Google Scholar]
- 2.Chazalon E., Conrath J., Ridings B., Matonti F. Artérite de Kyrieleis : présentation de deux cas et revue de la littérature [Kyrieleis arteritis: report of two cases and literature review] J. Fr. Ophtalmol. 2013 Mar;36(3):191–196. doi: 10.1016/j.jfo.2012.03.014. French. Epub 2013 Jan 24. PMID: 23352707. [DOI] [PubMed] [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G. For the SCARE Group, the SCARE 2020 guideline: updating Consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 4.Pichi F., Veronese C., Lembo A., Invernizzi A., Mantovani A., Herbort C.P., Cunningham E.T., Jr., Morara M., Ricci F., Neri P., Nucci P., Ciardella A.P., Staurenghi G., Lowder C.Y., Srivastava S.K. New appraisals of Kyrieleis plaques: a multimodal imaging study. Br. J. Ophthalmol. 2017 Mar;101(3):316–321. doi: 10.1136/bjophthalmol-2015-308246. Epub 2016 Jun 6. PMID: 27267451. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz P.L. Segmental retinal periarteritis as a complication of toxoplasmosis. Ann. Ophthalmol. 1977 Feb;9(2):157–162. PMID: 843015. [PubMed] [Google Scholar]
- 6.Krishnamurthy R., Cunningham E.T., Jr. Atypical presentation of syphilitic uveitis associated with Kyrieleis plaques. Br. J. Ophthalmol. 2008 Aug;92(8):1152–1153. doi: 10.1136/bjo.2007.124693. PMID: 18653612. [DOI] [PubMed] [Google Scholar]
- 7.Khairallah M., Ladjimi A., Chakroun M., Messaoud R., Yahia S.B., Zaouali S., Romdhane F.B., Bouzouaia N. Posterior segment manifestations of Rickettsia conorii infection. Ophthalmology. 2004 Mar;111(3):529–534. doi: 10.1016/j.ophtha.2003.04.012. PMID: 15019331. [DOI] [PubMed] [Google Scholar]
- 8.Witmer M.T., Levy-Clarke G.A., Fouraker B.D., Madow B. Kyrieleis plaques associated with acute retinal necrosis from herpes simplex virus type 2. Retin. Cases Brief Rep. 2011 Fall;5(4):297–301. doi: 10.1097/ICB.0b013e3181f66aac. PMID: 25390418. [DOI] [PubMed] [Google Scholar]
- 9.Francés-Muñoz E., Gallego-Pinazo R., López-Lizcano R., García-Delpech S., Mullor J.L., Díaz-Llopis M. Kyrieleis' vasculitis in acute retinal necrosis. Clin. Ophthalmol. 2010 Jul 30;4:837–838. doi: 10.2147/opth.s11960. PMID: 20689738; PMCID: PMC2915872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wise Gn. Ocular periarteritis nodosa; report of two cases. AMA Arch Ophthalmol. 1952 Jul;48(1):1–11. doi: 10.1001/archopht.1952.00920010004001. PMID: 14932555. [DOI] [PubMed] [Google Scholar]
- 11.Griffin A.O., Bodian M. Segmental retinal periarteritis. Am. J. Ophthalmol. 1959;47(4):544–548. doi: 10.1016/s0002-9394(14)76470-0. [DOI] [PubMed] [Google Scholar]
- 12.Blach R.K. Segmental lesions of the retinal arteries. Br. J. Ophthalmol. 1960 Sep;44(9):562–566. doi: 10.1136/bjo.44.9.562. PMID: 18170639; PMCID: PMC509988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Orzalesi N., Ricciardi L. Segmental retinal periarteritis. Am. J. Ophthalmol. 1971 Jul 30;72(1):55–59. doi: 10.1016/0002-9394(71)91590-x. PMID: 5571211. [DOI] [PubMed] [Google Scholar]
- 14.Tsui E., Leong B.C.S., Mehta N., Gupta A., Goduni L., Cunningham E.T., Jr., Freund K.B., Lee G.D., Dedania V.S., Yannuzzi L.A., Modi Y.S. Evaluation of segmental retinal arteritis with optical coherence tomography angiography. Retin. Cases Brief Rep. 2021 Nov 1;15(6):688–693. doi: 10.1097/ICB.0000000000000900. PMID: 31313702. [DOI] [PubMed] [Google Scholar]