Abstract
Background
Hypoxemia is one of the feared critical events intraoperatively and postoperatively. Undetected postoperative oxygen hypoxemia may lead to pulmonary hypertension, hyperkalemia, respiratory and cardiac failure even brain ischemia, and lastly, it may end up with multiorgan failure. The main purpose of this study was to determine the incidence and associated factors for postoperative hypoxemia among elective surgical patients received anesthesia in Dessie Comprehensive Specialized Hospital.
Methods
Prospective observational study was conducted in Dessie comprehensive Specialized Hospital from March to June 2021. The study included elective surgical patients. The data was collected with structured questionnaires, and direct measurement of oxygen saturation with pulse oximetry. Statistical analysis was done by using the Statistical Package of Social Science version 23.
Results
A total of 298 patients enrolled with a response rate of 94% in the study. Among the study participants, 167 (56%) were females and 131 (44%) were males. The Mean (±Standard Deviation) age was 37.62 ± 15.75 years. The incidence of hypoxemia was 24.5% (95% of Confidence Interval 19.34, 30.62) among 298 postoperative patients. Associated factors with postoperative hypoxemia were age greater than 55 years, preoperative saturation below 95%, type of anesthesia, postoperative pain score, and postoperative muscular strength, The patient age below 55 years had 84% less likely to develop hypoxemic episodes postoperatively when we compare age above 55-year-old. A patient who received general anesthesia had a chance of developing hypoxia eight times than those who received regional anesthesia. A patient who can keep grip for 15 s had 60% less likely to develop hypoxemia than those who can keep a grip for 15 s postoperatively.
Conclusion
This study showed that there was a high incidence of postoperative hypoxemia among elective surgical patients in the study area. The high-risk patients should be identified and postoperative oxygen therapy should be initiated for those high-risk patients.
Keywords: Postoperative hypoxemia, Associated factors, Dessie, Ethiopia
Highlights
-
•
Hypoxemia is one of the feared critical events intraoperatively and postoperatively.
-
•
High incidence of postoperative hypoxemia among elective surgical patients.
-
•
Age, preoperative arterial oxygen saturation, general anesthesia, postoperative pain score and postoperative muscular strength were associated with postoperative hypoxemia.
1. Background
Hypoxemia is defined as inadequate tissue oxygenation due to either inadequate blood flow or arterial oxygen content [1]. Hypoxemia is one of the feared critical events during anesthesia and surgery. Severe hypoxemia can result in respiratory arrest or leave the victim with neurological disabilities [2]. Arterial desaturation has two main causes, diminished arterial oxygen tension and increased arterial oxygen tension differences. Lung function almost always deteriorates during anesthesia. This deterioration may be due to decreased functional residual capacity and increased airway closure, a ventilation/perfusion (V/Q) imbalance, or the development of atelectasis [3].
Undetected postoperative oxygen hypoxemia may lead to pulmonary hypertension, hyperkalemia, respiratory and cardiac failure even brain ischemia, and finally, it may end up with multiorgan failure [4]. Some pieces of literature also stated that early postoperative hypoxemia is a trigger for postoperative respiratory complications [5]. A study done in Thailand presented that obesity, epidural analgesia, and subcostal incision are risk factors for postoperative oxygen desaturation. Similarly, Xue FS et al. showed that severe hypoxia is highly associated with thoracoabdominal surgeries [6,7].
Only 0.8% of the patients experienced oxygen desaturation when they were transferred with oxygen supplementation. The most significant predictor of desaturation was transported without oxygen. The practice pattern showed that 43% of the patients were transferred with oxygen supplementation [8]. Standard monitoring with peripheral oxygen saturation and appropriate oxygen administration should be required during postoperative oxygen administration to avoid both hypoxemia and hyperoxia [9]. Despite previous studies presented globally, the incidence of postoperative hypoxemia was not known in the study area. The purpose of this study was to assess the incidence and predisposing factors of postoperative hypoxemia at DCSH, PACU from March to June/2021.
2. Methods
The prospective observational study was conducted in the PACU of DCSH from March to June 2021. DCSH. Ethical clearance was obtained from Wollo University College of Medicine and Health Science. Preoperatively informed consent was taken from patients included in the study. They were informed that they have free will to abandon the study at any time. The data was kept secret in a way that only the researchers got access to it. The article has been registered with a unique identifying number of researchregistry7721 and the work has been reported in line with the STROCSS criteriae [10]. All adult ASA I, II, and III patients who operated in DCSH during the study period, from March to June 2021 those who are sent to the PACU are included in the study. Anemic patients, OSA, and obstetric patients were excluded from this study. Institutional based consecutive sampling technique method was used to conduct this study during the study period.
2.1. Sample size determination
The sample size was determined by the following assumptions; since there is a previous study in Gondar [11], we were used 26.7% of a single proportion, 95% confidence interval, and margin of error to tolerate 0.05. The sample size is to be taken using the following formula.
| N = z2P(1-P)/d2 |
| n= (1.96)2x (0.267) (1–0.267)/ (0.05)2=300 |
So with adjustment for non-response 5%, n= (300 + 15) = 315.Where: n = sample size; P = 26.7% of proportion: q = 1-p; d = desired degree of precision.
Z = is the standard normal value at 95% confidence level
2.2. Data collection procedure
The data was collected through document review, direct patient observation, and measurement of oxygen saturation by pulse oximetry (Lifebox Pulse Oximeter 2019). A patient received general anesthesia reversal of muscle blockage was done with neostigmine at 0.05 mg kg-1 and atropine at 0.01 mg kg-1 intravenously and patients were extubated when they respond to command after the completion of the surgery, there was no peripheral nerve stimulator in the study area. Peripheral arterial oxygen saturation measurement was started immediately when the patient was transferred to the PACU then measured continuously within the first hour. The quality was maintained by checking the consistency, clarity, and completeness of the anesthetic sheet, registration books, individual chart. The data were collected by an employed structured questionnaire.
Data was collected post-operatively by reviewing the charts with a structured questionnaire which includes age, sex, physical status, type of surgery, history of co-morbidities, and their post-operative events and outcomes will be recorded carefully. The data was entered by using Epi info 7 and analyzed by SPSS 23.00 version statistical software. The incidence of hypoxemia was expressed as descriptive statistics and logistic regression was used to adjust or control the possible confounding factors and to identify associated factors for postoperative hypoxemia. The cut point for Statistical significance was P < 0.05.
2.3. Operational definitions
Elective surgery: a procedure that is scheduled in advance because it does not involve a medical emergency.
Hypoxemia: Decrease in SPO2 level <90% in pulse oximetry reading for at least 3 min.
Grip Strength: a measure of muscular strength to monitor residual neuromuscular blockade, clinically [12]. Muscular strength score (1 = keeps grip for >15 seconds and 0 = does not keep grip or keeps it for less than 15 seconds).
Mild Pain: level of pain on numerical rating scale between 1 and 3.
Moderate pain: level of pain on the numerical rating scale between 4 and 6.
No pain: level of pain 0 on the numerical rating scale.
Numerical Rating Scale: pain assessment tool which expresses 0 up to 10.
Severe Pain-level of pain on the numerical pain scale ranging from 7 to 10.
3. Results
3.1. Sociodemographic characteristics
A total of two hundred ninety-eight patients enrolled with a response rate of 94% in the study. Fifteen patients were excluded from analysis for incomplete data. Among the study participants, 167 (56%) were females and 131 (44%) were males. The Mean (±Standard Deviation) age was 37.62 ±15.75 years (Table 1).
Table 1.
Socio-demographic characteristics of participants at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia; 2021 (N = 298).
| Variable | Category | Postoperative SPO2 |
|
|---|---|---|---|
| Hypoxemia |
Not Hypoxemia |
||
| N (%) | N (%) | ||
| Sex | Male | 92 (30.87) | 39 (13.08) |
| Female | 113 (37.91) | 34 (11.40) | |
| Age | <55 | 205 (68.79) | 54 (18.12) |
| ≥55 | 20 (6.71) | 19 (6.37) | |
| BMI | Below 18.5 | 42 (14.09) | 14 (4.69) |
| 18.5–24.9 | 166 (55.70) | 50 (16.77) | |
| Above 25 | 17 (5.70) | 9 (3.02) | |
| History of smoking | Yes | 8 (2.68) | 4 (1.34) |
| No | 217 (72.81) | 69 (23.15) | |
| ASA | I | 174 (58.38) | 35 (11.74) |
| II | 51 (17.11) | 31 (10.40) | |
| III | 2 (0.67) | 5 (1.68) | |
| Coexisting diseasesa | Yes | 38 (12.75) | 13 (4.36) |
| No | 187 (62.75) | 60 (20.13) | |
Hypertension, Diabetes Mellitus, Pulmonary diseases, Heart diseases.
3.2. Types of anesthesia and type of surgery
General anesthesia and general surgery was the common type of anesthesia and type of surgery during the study period respectively (Table 2).
Table 2.
Type of Anesthesia and Surgery among surgical patients in Dessie Comprehensive Specialized Hospital, Northeast Ethiopia, 2021(N = 298).
| Variable | Category | Postoperative SPO2 |
|
|---|---|---|---|
| Normal |
Hypoxia |
||
| N (%) | N (%) | ||
| Type of Anesthesia | General anesthesia | 182 (61.07) | 67 (22.48) |
| Regional anesthesia | 43 (14.42) | 6 (2.01) | |
| Type of procedure | General surgery | 143 (47.98) | 37 (12.41) |
| Urological surgery | 23 (7.71) | 20 (6.71) | |
| Gynecological procedures | 22 (7.38) | 4 (1.34) | |
| Orthopedic procedures | 28 (9.39) | 5 (1.67) | |
| Others a | 9 (3.02) | 7 (2.34) | |
| Duration of surgery | Below 120 min | 158 (53.02) | 41 (13.75) |
| 120 min and above | 67 (22.48) | 32 (10.73) | |
| Estimated blood loss | <500 ml | 219 (73.48) | 66 (22.14) |
| ≥500 ml | 9 (3.02) | 4 (1.34) | |
Maxillofacial surgeries, Ear, Nose, and Throat surgeries.
3.3. Intraoperative anesthesia and analgesia
Suxamethonium was the only intubating muscle relaxant and halothane (78.5%) was the commonest maintenance inhalational agent with a patient who took general anesthesia. Among patients who took regional anesthesia, bupivacaine was the only induction agent both for spinal anesthesia and peripheral nerve block. Tramadol was the most (60.7%) common type of intraoperative analgesia by the following diclofenac, potent opioids, and paracetamol with 38.9%,11.7%, and 3.4% respectively (Table 3).
Table 3.
Type of intraoperative anesthetic agents in Dessie Comprehensive Specialized Hospital, Northeast Ethiopia, 2021(N = 298).
| Category | Drugs | Frequency(n) | Percent (%) |
|---|---|---|---|
| Analgesic used | Paracetamol | 10 | 3.4 |
| Tramadol | 138 | 46.3 | |
| Diclofenac | 66 | 22.1 | |
| Tramadol and Diclofenac | 59 | 16.4 | |
| Potent opioids | 35 | 11.7 | |
| Total | 308a | 103.4a | |
| Induction Agents | Ketamine | 52 | 17.4 |
| Thiopental | 91 | 30.5 | |
| Propofol | 85 | 28.5 | |
| Ketamine with propofol | 21 | 7.0 | |
| Total | 249b | 85.6b | |
| Maintenance gas agent | Halothane | 234 | 78.52 |
| Isoflurane | 15 | 5.03 | |
| Total | 249b | 83.55b | |
| Intraoperative muscle relaxants | Vecuronium | 211 | 70.8 |
| Pancuronium | 38 | 12.7 | |
| Total | 249b | 85.6b |
The total was above the number of participants one patient took more than one drug.
The total was below the number of participants which include only General anesthesia.
3.4. Postoperative hypoxemia incidence
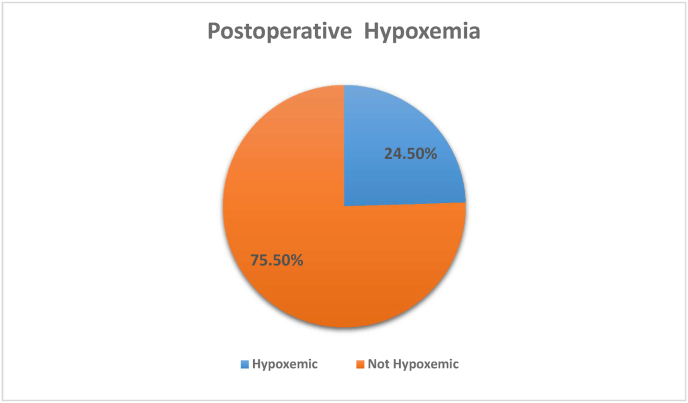
The incidence of hypoxemia is 24.5% (73) (95% of Confidence Interval of 19.34, 30.62) among 298 postoperative patients. Among those hypoxic patients, only 34% of patients got oxygen administration postoperatively in the PACU. The episode of postoperative hypoxemia was decreased with time in the recovery room regardless of postoperative oxygen supplementation (Fig. 1).
Fig. 1.
Incidence of postoperative hypoxemia at Dessie Comprehensive Specialized Hospital, Northeast Ethiopia,2021(N = 298).
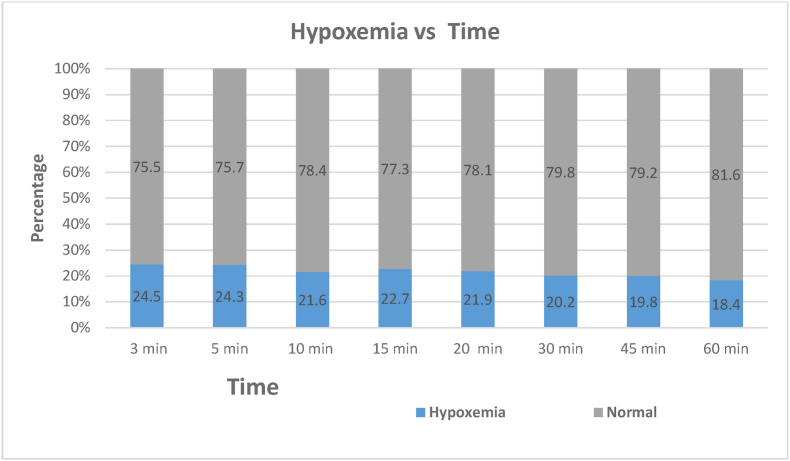
3.4.1. Hypoxemia vs time
The episode of hypoxemia was not constant with time in the PACU. Seventy-three (24.5%) patients developed hypoxemia with the first 3 min then decreased to 55 (18.4%) patients at one 1 h (Fig. 2).
Fig. 2.
The incidence of postoperative hypoxemia with time respect in PACU, Dessie Comprehensive Specialized Hospital, 2021(N = 298).
3.5. Associated factors with postoperative hypoxemia
Associated factors with postoperative hypoxemia were age greater than 55 years old, preoperative saturation below 95%, type of anesthesia, postoperative pain score, and postoperative muscular strength, The patient age below 55 years had 84.3% or less likely to develop hypoxemic episodes postoperatively when we compared age above 55-year-old. A patient who received general anesthesia had a chance of developing hypoxemia eight times than those who received regional anesthesia. A patient who had a muscular strength score of 1 had 60% less likely to develop hypoxemia than those who had 0 scores postoperatively. There is no significant difference between those patients who suffer severe and moderate pain to develop postoperative hypoxemia (Table 4).
Table 4.
Associated factors for postoperative hypoxemia in Dessie Comprehensive Specialized Hospital, Northeast Ethiopia; 2021 (N = 298).
| Variable | Category | Postoperative saturation |
p-value | CI 95% |
||
|---|---|---|---|---|---|---|
| Not hypoxia | Hypoxia | COR | AOR | |||
| Age | <55 | 205 | 54 | 0.001 | 0.277 (0.138,0.556) | 0.157 (0.055,0.419) |
| ≥55 | 20 | 19 | 1 | |||
| Preoperative SPO2 | ≤94% | 105 | 57 | 0.001 | 4.071 (2.205,7.158) | 4.497 (2.220, 9.110) |
| › 94% | 120 | 16 | 1 | 1 | ||
| Type of anesthesia | General anesthesia | 182 | 67 | 0.002 | 2.638 (1.074, 6.482) | 8.013 (2.207, 29.091) |
| Regional anesthesia | 43 | 6 | 1 | 1 | ||
| Muscular strength | 1 | 184 | 40 | 0.01 | 0.270 (0.152, 0.478) | 0.392 (0.193, 0.796) |
| 0 | 41 | 33 | 1 | 1 | ||
| Postoperative pain score | No | 34 | 5 | <0.001 | 0.122 (0.057,0.262) | 0.114 (0.032,0.411) |
| Mild | 114 | 15 | 0.001 | 0.136 (0.046,0.403) | 0.182 (0.073, 0.454) | |
| Moderate | 52 | 26 | 0.772 | 0.463 (0.225,0.951) | 0.880 (0.370, 2.091) | |
| Severe | 25 | 27 | 1 | 1 | ||
Multivariate logistic regression analysis was done. P-value less than 0.05 was statistically significant.
AOR = Adjusted odds ratio, COD = crude odds ratio, CI = confidence interval.
4. Discussion
The goal of this observational study was to find out how common postoperative hypoxemia is and what factors contribute to it in elective surgery patients. In the research location, there were no local postoperative hypoxemia management protocols. The incidence of postoperative hypoxemia is 24.5% (n = 73). This study showed that higher than a study done in Canada by Walker. The possible reason for this difference may be 57.8% of patients transferred from the operation room to PACU with oxygen administration in their study and also they investigated retrospectively [13]. Another observational study which was done in Gondar University Hospital showed that among 26.7% of patients, hypoxic events were observed for the first 20 min in PACU admission. Which is similar to the finding in this research [11]. Similar to this study a study in Addis Abeba Ethiopia incidence was 22.7% [14]. As Zhang et al. showed that the incidence of hypoxemia at PACU was 2.79% [15] but there was oxygen supplementation during the patient transfer from OR to PACU in their study. Another study investigated retrospectively which showed that postoperative desaturation was 12.1% which was lower than this study despite they included only patients who took general anesthesia [16]. An observational study done by Siriussawakul and his colleagues showed that the incidence of postoperative desaturation was 38% which is high when we compare with this study, that we incorporated all operated patients regardless of the surgical site but they focused only on abdominal surgery. The possible reason may be that they focused on abdominal surgery [7]. Although there was a difference in the incidence of postoperative hypoxemia between this study and other research, the incidence of hypoxemia in this study was higher because we included all types of surgical procedures, anesthetic types, elective surgery patients, and excluded OSA sufferers. Poor PACU setup, monitoring standards, and postoperative oxygen administration in the PACU all contributed to this distinction.
There were different factors for the incidence of postoperative hypoxemia in PACU. The patient's age, preoperative oxygen saturation, type of anesthetic, level of pain, and postoperative muscular strength were all independent risk factors for postoperative hypoxemia in this study. A cohort study presented that obesity is the factor that was associated with high intraoperative hypoxia when we compared with normal BMI, overweight and obesity III patients experienced hypoxemia 2.63 and 1.27 times respectively. AOR of prolonged hypoxemia increased with BMI from 3.29 (95% CI, 1.79–6.23) with class I obesity to 9.20 (95% CI, 4.74–18) with class III obesity. But in this study, patient BMI was not associated with postoperative hypoxia. This distinction may be due to patient's factor. Only 26 patients had a BMI of above 25 kg/m2 which was small when we compared Kindale's study [17].
A patient age below 55 years old had less likely to develop postoperative hypoxemia similar to a study by Xiuhua Zhang [15].which may be explained by when age exceeds above 45 there is a decrement of lung elastic and an increment of closing capacity. Similar to this study Maity et al showed that 43.47% vs 17.24% was statistically significant (P = 0.03) among older and younger patients. This may result in a postoperative collapse of alveoli that end up with postoperative hypoxemia [2]. Preoperative patients in hemodynamic status are the main factor for postoperative hypoxia among those a patient who had a preoperative SPO2 below 95% had four times a chance of developing postoperative hypoxia. Similar to this study, a study in Debre tabor, Ethiopia incorporated 424 participants both emergency and elective surgical patients showed that preoperative SPO2 below 95% were associated with AOR of 3.001 [18]. General anesthesia was the main predictor for postoperative hypoxemia in this study. When we compared to previous studies the ratio is near to those studies done in Gondar in this study. Despite this, a crossectional study by Wolde et al. type of anesthesia was not significantly associated with postoperative hypoxemia. This difference may be due to postoperative follow up duration. They followed for 30 min, the follow-up duration increased may get to outcomes may be increased [14].
Postoperative pain score was associated with postoperative hypoxemia in this study. Patients who had mild pain scores and no pain had 82% and 88% less likely to develop postoperative hypoxia respectively when we compared a patient who had severe pain. An experimental study presented by Høiseth and his colleagues presented that peripheral tissue oxygen saturation was reduced by pain which may be the reason for the association between severe pain and hypoxemia but needs further investigation the association between pain severity and hypoxemia regardless of the type of analgesia [19]. A patient may get adequate surgical site analgesia did not develop hypoxemia due to adequate ventilation. In contrast to this research, previous studies reveal that opioid administration was highly associated with postoperative hypoxia. The patient becomes hypoxic after opioid administration which is related to the respiratory depressant effect of potent opioids [20]. This difference may be due to intraoperative and postoperative administration of opioids being limited on the study area which showed that only 11.7% of patients got opioid analgesia intraoperatively, and tramadol and diclofenac were the common perioperative analgesic medications [7,16,21]. This may be supported by another study that stated that the first 24 h after surgery represents a high-risk period for a respiratory event as a result of narcotic use [20].
Postoperative muscular strength was highly associated with postoperative hypoxemia with an AOR of 0.39 (0.193, 0.796). A patient who can keep grip above 15 s had 60% or less likely to develop postoperative hypoxia when we compared patients who can't. This may be due to there being not used a peripheral nerve stimulator to determine the level of muscle reversal before extubation in the study area and also may be residual neuromuscular blockage which is not measured in the PACU. Similar to this study previous studies showed that residual neuromuscular blockade was an independent risk factor for the critical respiratory event in the PACU. A case control study enrolled 7459 patients showed that residual neuromuscular blockage was associated with hypoxemia within first 15 min in the PACU [22,23].
5. Limitation of the study
This study was observational and within a short period postoperatively and did not follow hypoxemic patients after being discharged from PACU.
6. Conclusions and recommendations
The study showed that there was a high incidence of postoperative hypoxemia among elective surgical patients and the age of the patient, preoperative saturation, general anesthesia, moderate and severe pain, and postoperative muscular strength were highly associated with postoperative hypoxemia. Therefore, according to the current study, we recommended closely following to detect postoperative hypoxemia to manage it with an individualized base. We also suggest further studies with longer postoperative follow-up.
Ethical consideration
Ethical clearance was obtained from College of Medicine and Health Science Ethical Review Committee. Verbal and written informed consent was obtained from each study participant after full disclosure of the benefits and risks of participation in the study. The confidentiality of the participants’ data was ensured by removing identifiers and locking in the separate place.
Consent
Written informed consent was obtained from every study participant after a clear explanation of the purpose of their participation and not harmed by participants. Anyone who was not willing to participate in the study was informed that he or she would have the full right not to participate or stop at any time.
Ethical approval
Wollo University college of medicine and health science.
Sources of funding
Wollo University.
Author contribution
Authors' contributions this work was carried out in collaboration among all authors. AA (Amare Agmas) contributed to the conception and design of the study, acquired; analyzed and interpreted the data drafted, and revised the manuscript. KA (Kassaw Abegaz) participate in reviewing the design and methods of data collection, interpretation and preparation of the manuscript. Both authors participate in the preparation and critical review of the manuscripts. In addition, both authors read and approved the manuscript.
Research registration unique identifying number (UIN)
Researchregistry7721
Guarantor
Amare Agmas Andualem.
Provenance and peer review
The authors only sent to Annals of Medicine and Surgery peer review journal and still under review.
Not commissioned, externally peer-reviewed.
This paper was submitted to a non-commissioned journal for publication in a peer-reviewed journal.
Declaration of competing interest
The authors declare that there is no conflict of interest.
Acknowledgments
To the Wollo University, College of Medicine and Health Sciences for helping and facilitating to conduct this research. To data collectors for scarifying their time to collect quality data. Finally, to study participants for their positive response.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103747.
Contributor Information
Amare Agmas Andualem, Email: agmasaa3@gmail.com.
Kassaw Abegaz Yesuf, Email: micky.abegaz@gmail.com.
Abbreviations
- AOR
Adjusted Odds Ratio
- ASA
America Society of Anesthesiologists
- BMI
Body Mass index
- COR
Crude Odds Ratio
- CPAP
Continuous Positive Airway Pressure
- DCSH
Dessie Comprehensive Specialized Hospital
- GA
General Anesthesia
- IV
Intravenous
- OR
Operation Room
- OSA
Obstructive Sleep apnea
- PACU
Post-anesthesia care unit
- SPO2
Oxygen saturation
- WU
Wollo University
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Loiacono L.A., Shapiro D.S. Detection of hypoxia at the cellular level. Crit. Care Clin. 2010;26(2):409–421. doi: 10.1016/j.ccc.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Maity A., Saha D., Swaika S., Maulik S.G., Choudhury B., Sutradhar M. Detection of hypoxia in the early postoperative period. Anesth. Essays Res. 2012;6(1):34. doi: 10.4103/0259-1162.103369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karcz M., Papadakos P.J. Respiratory complications in the postanesthesia care unit: a review of pathophysiological mechanisms. Can. J. Respir. Ther.: CJRT= Revue canadienne de la therapie respiratoire: RCTR. 2013;49(4):21. [PMC free article] [PubMed] [Google Scholar]
- 4.Tyler I., Tantisira B., Winter P., Motoyama E. Continuous monitoring of arterial oxygen saturation with pulse oximetry during transfer to the recovery room. Surv. Anesthesiol. 1986;30(4):225–226. [PubMed] [Google Scholar]
- 5.Ramachandran S.K., Thompson A., Pandit J.J., Devine S., Shanks A.M. Retrospective observational evaluation of postoperative oxygen saturation levels and associated postoperative respiratory complications and hospital resource utilization. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0175408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xue F.S., Li B.W., Zhang G.S., Liao X., Zhang Y.M., Liu J.H., et al. The influence of surgical sites on early postoperative hypoxemia in adults undergoing elective surgery. Anesth. Analg. 1999;88(1):213–219. doi: 10.1097/00000539-199901000-00040. [DOI] [PubMed] [Google Scholar]
- 7.Siriussawakul A., Mandee S., Thonsontia J., Vitayaburananont P., Areewatana S., Laonarinthawoot J. Obesity, epidural analgesia, and subcostal incision are risk factors for postoperative desaturation. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2010;57(5):415–422. doi: 10.1007/s12630-010-9279-3. [DOI] [PubMed] [Google Scholar]
- 8.Siddiqui N., Arzola C., Teresi J., Fox G., Guerina L., Friedman Z. Predictors of desaturation in the postoperative anesthesia care unit: an observational study. Surv. Anesthesiol. 2014;58(4):196–197. doi: 10.1016/j.jclinane.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki S. Oxygen administration for postoperative surgical patients: a narrative review. J. Intensive Care. 2020;8(1):1–6. doi: 10.1186/s40560-020-00498-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathew G., Agha R., Albrecht J., Goel P., Mukherjee I., Pai P., et al. Strocss 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Inter. J. Sur. Open. 2021;37 doi: 10.1016/j.ijsu.2021.106165. [DOI] [PubMed] [Google Scholar]
- 11.Melesse D. Y., Z. A. Denu, H. G. Kassahun, A. F. Agegnehu. The incidence of early post-operative hypoxemia and its contributing factors among patients underwent operation under anesthesia at University of Gondar comprehensive and specialized referral hospital, Gondar, North West Ethiopia, 2018. A prospective observational study. Inter.l J. Surgery Open. 2020;22:38-46.
- 12.Pei D.-Q., Zhou H.-M., Zhou Q.-H. Grip strength can be used to evaluate postoperative residual neuromuscular block recovery in patients undergoing general anesthesia. Medicine. 2019;98(2) doi: 10.1097/MD.0000000000013940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker M., Farmer R.G., Schelew B. Risk factors for oxygen desaturation on arrival in the postanesthesia care unit. Canadian Journal of Anesthesia/Journal canadien d'anesthésie. 2015;62(9):1019–1020. doi: 10.1007/s12630-015-0371-6. [DOI] [PubMed] [Google Scholar]
- 14.Wolde G., Awol M., Obsa M., Wesene N., Gemechu A., Tadesse E. Magnitude and associated factors of immediate postoperative hypoxemia among elective surgical procedures at Tikur Anbessa Specialized hospital, Addis Ababa, Ethiopia. J. Anesth. Clin. Res. 2018;9(821):2. [Google Scholar]
- 15.Tang S., Zhang L., Han W., Xue Y., Tian Y., Zhang X., et al. 2019. Incidence of Hypoxemia in a Post-anaesthesia Care Unit and Relevant Risk Factors: a Retrospective Study of 14604 Patients with General Anaesthesia. [Google Scholar]
- 16.Ishikawa M., Sakamoto A. Postoperative desaturation and bradypnea after general anesthesia in non-ICU patients: a retrospective evaluation. J. Clin. Monit. Comput. 2020;34(1):81–87. doi: 10.1007/s10877-019-00293-0. [DOI] [PubMed] [Google Scholar]
- 17.Kendale S.M., Blitz J.D. Increasing body mass index and the incidence of intraoperative hypoxemia. J. Clin. Anesth. 2016;33:97–104. doi: 10.1016/j.jclinane.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 18.Taye M.G., Molla A., Teshome D., Hunie M., Kibret S., Fentie Y., et al. Predictors of hypoxemia after general anesthesia in the early postoperative period in a hospital in Ethiopia: an observational study. Multidisciplinary Respiratory Medicine. 2021;16(1) doi: 10.4081/mrm.2021.782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Høiseth L.Ø., Hisdal J., Hoff I.E., Hagen O.A., Landsverk S.A., Kirkebøen K.A. Tissue oxygen saturation and finger perfusion index in central hypovolemia: influence of pain. Crit. Care Med. 2015;43(4):747–756. doi: 10.1097/CCM.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 20.Taylor S., Kirton O.C., Staff I., Kozol R.A. Postoperative day one: a high risk period for respiratory events. Am. J. Surg. 2005;190(5):752–756. doi: 10.1016/j.amjsurg.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Drummond G.B., Lafferty B. Oxygen saturation decreases acutely when opioids are given during anaesthesia. Br. J. Anaesth. 2010;104(5):661–663. doi: 10.1093/bja/aeq076. [DOI] [PubMed] [Google Scholar]
- 22.Murphy G.S., Szokol J.W., Marymont J.H., Greenberg S.B., Avram M.J., Vender J.S. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth. Analg. 2008;107(1):130–137. doi: 10.1213/ane.0b013e31816d1268. [DOI] [PubMed] [Google Scholar]
- 23.Xará D., Santos A., Abelha F. Adverse respiratory events in a post-anesthesia care unit. Arch. Bronconeumol. 2015;51(2):69–75. doi: 10.1016/j.arbres.2014.04.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.