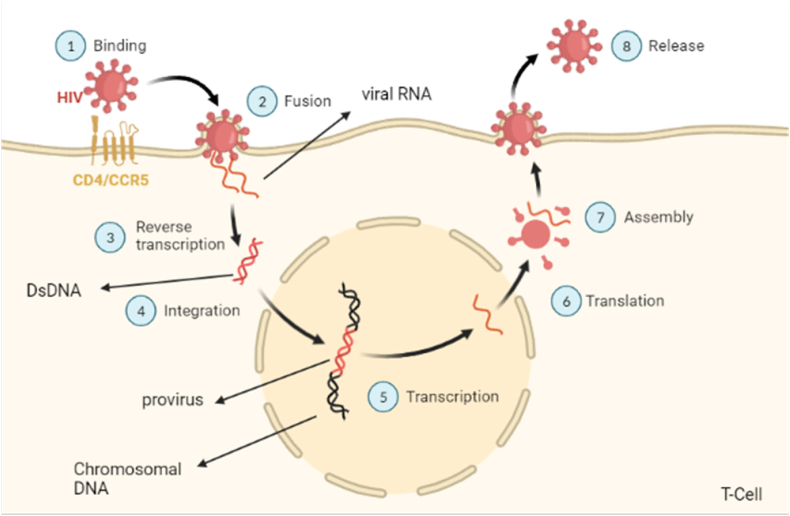
The human immunodeficiency virus (HIV) is an RNA virus belonging to the retrovirus family's lentiviruses (slow viruses) subgroup, its transmission modes include anal or vaginal intercourse with an infected partner, transfer from mother to baby (perinatal transmission), tainted needles, syringes, and drug injection devices [1]. The mechanism by which HIV infects human T-cell is shown in Fig. 1. Geographically, Pakistan lies in the Asia-Pacific region that, according to UNAIDS, dwells more HIV-positive people than Sub-Saharan Africa. The Asia-Pacific area is home to around 5.8 million HIV-positive persons [2]. According to the World Health Organization (WHO), around 38 million individuals worldwide are living with HIV/AIDS as of 2020, with 1.7 million being children under the age of 15. Approximately 36.3 million individuals have died as a result of the infection so far. In the year 2020 alone, around 150,000 new HIV infections in children under the age of 15 were registered. The bulk of HIV/AIDS-related fatalities in children and adults have happened in Africa, Asia, and the Pacific [3].
Fig. 1.
Mechanism of infection of T cell by HIV.
From 2010 to 2018, the number of HIV-positive people in Pakistan more than doubled, from 67,000 in 2010 to 160,000 in 2018. A 57% overall increase (from 14000 to 22000) in new infections was observed during this time period. This quick-rising percentage of infections included a 38% increase among young people aged 15–24 years [2]. With an increase in incidence from 0.08 in 2010, to 0.12 in 2019 [4], Pakistan offsets the decline in cases in other countries of the Asia-Pacific region. To our despair, the control over this increased peak of HIV-positive cases seems to be difficult, indicated by the statistics showing that from 190,000 cases of people living with HIV in 2019 to 210,000 cases in 2020. And it just does not stop there; the figure of 240,000 cases of people living with HIV till June 2021, adds to the dismay [5]. Between April 24 and July 15, 2019, approximately 80% of the 930 HIV-positive persons confirmed in Ratodero, a tiny village in Pakistan's Sindh province, were youngsters under the age of five. HIV infections in children have been related to having numerous injections, which means that the same syringes were used on one or more children by healthcare practitioners as part of therapy [6].
According to the Sindh AIDS Control Programme (SACP), 42,533 persons would have been screened by November 30, 2020, with 1438 HIV-positive patients being registered at the Ratodero ART Centre. There were a total of 1076 children among them, with 666 boys and 410 girls. According to the SACP, 34 children and four adults have died as a result of the Ratodero pandemic [7]. In the last 2 years of the COVID-19 pandemic, a 12% decline in new HIV infections in the Asia-Pacific region was noticed- but to our disappointment, it put the increase of infections in some countries including Pakistan off the grid. Owing to the factors like the flaws in HIV case reporting, variation in HIV interventions, lack of commitment by healthcare officials as well as the lack of effective community engagement partially resulting from social discrimination or stigma, Pakistan noticed an increase in HIV incidence per 1000 population [2].
Despite the current efforts of the National Aids Control Program, provincial authorities, and the UNAIDS, out of the 200,000 people infected with HIV in the country, a mere 12% are reported to be taking antiretrovirals [4]. Underfunding, healthcare workers' reallocation, and overburdening imposed by the COVID-19 pandemic can only worsen the scenario by decreasing the human resource and facilities needed to diagnose and manage HIV, transport medicines, and take other measures to contain its spread. As per an estimate by Hogan et al., disruption of medical services amid the COVID-19 pandemic could result in a 10% rise in deaths caused by HIV in the developing world over the next 5 years [8]. There have been an estimated 82000 deaths attributed to AIDS in Pakistan as of 2020 [4]. The comparison between COVID-19 and HIV has been shown in Table 1. Rotadero is the locality where more than 1400 individuals were tested positive for HIV in 2019, making a prevalence rate of 2% in contrast to 0.2% in the remainder of the country [7]. This alarming rate was attributed to the misuse and improper disposal of syringes in clinics, a fact that not only reflects the neglect in the country's fundamental healthcare system but also sheds light on the ignorance which poses another difficulty in managing any transmissible disease. Despite the fact that the National AIDS Control Programme (NACP), with the assistance of the Global Fund, has established 45 HIV treatment centers across the country's four provinces, people living with HIV frequently have to travel long distances to receive necessary treatment and pay out-of-pocket to cover travel costs. Due to a scarcity of infectious disease specialists, ART clinics are rarely handled by professionals. Physicians and other primary care providers, in particular, lack competence and training in HIV-positive children's care [5].
Table 1.
Comparison between HIV and COVID-19.
| Features | HIV | COVID-19 |
|---|---|---|
| Phylogenetically | Lentivirus | Beta corona virus |
| Transmission | Sexual, parenteral, direct contact | Air by small drops of saliva |
| Targets | CD4 surface protein | ACE2 receptors |
| Symptoms | Fever, joint pain, swollen lymph nodes, shingles, pneumonia, etc | Fever, loss of taste and smell, sore throat, shortness of breath, etc |
| Death percentage | ≥95% | 1–4% |
Access to food aid and several Government-run schemes have been made available, however, they depend on the national identity card verification, another basic item not in the possession of several transgenders. As a solution, the Khwaja Sara Society (KSS) has claimed to be working closely with authorities to ensure a several-month stock of antiretroviral medicines in case their delivery is hampered by lockdowns [9]. Similarly, other high-risk groups such as sex workers and intravenous drug users, where antiretroviral use is only limited to 5% and 16.2% of the affected respectively [2], represent an abandoned population that deserves special resource direction to limit the rising HIV cases in the face of the pandemic. The UNAIDS Country Director for Pakistan and Afghanistan has attested that the organization is working closely with the federal and provincial governments, and other people's associations to help overcome barriers in the provision of HIV services in this COVID-19 crisis. UNAIDS in collaboration with ‘Pakistan Common Management Unit for AIDS, TB, and Malaria’ has also established helplines for facilitation. Furthermore, a two-month stock of antiretroviral medicines has been allocated through the Global Fund in case of unanticipated events [9].
Some of the strategies that have shown a promising future to reduce the global HIV epidemic are declining sexual interactions with commercial sex, growing condom use, strenuous HIV testing policy with focused counseling and follow-up of HIV-positive individuals, tracing of sexual partners, rising education, increase access to antiretroviral drugs, reduction in multiple sexual relationships, delay in age at first sex, and a reduction in casual sex. Because Pakistan has a concentrated HIV pandemic and the illness has a low prevalence in the general population, routine mass screening programs are rarely carried out, and diagnostic tests are conducted on suspicion or referral.
COVID-19 has strained the country's healthcare resources thin, diverting critical resources away from HIV treatment and prevention initiatives. COVID-19, when combined with existing inadequate HIV prevention techniques, has accelerated the spread of HIV infections. The ineffective approaches and attitudes have only led to disillusionment. It is past time to adopt strong steps to combat the HIV danger, especially in light of the rising number of infections as a result of the disruption produced by COVID-19. We must direct our attention to this problem as quickly as possible, or else our previous accomplishments and future hopes would be in vain.
Ethical approval
The present study includes printed and published information; therefore, the formal ethical clearance was not applicable for this study.
Funding
None.
Declaration of competing interest
The authors declare that there is no conflict of interests.
Acknowledgments
Not applicable.
Contributor Information
Govinda Khatri, Email: govindakhatri550@gmail.com.
Abdul Moiz Sahito, Email: sahitomoiz@gmail.com.
Mishal Shan Siddiqui, Email: mishalshansiddiqui@gmail.com.
Minaam Farooq, Email: minaamkemu2018@gmail.com.
Rida Fatima, Email: ridafatima290@gmail.com.
Qasim Mehmood, Email: qasimmehmood1051@gmail.com.
Mohammad Mehedi Hasan, Email: mehedi.bmb.mbstu@gmail.com.
References
- 1.Center for disease control and prevention (CDC) About HIV/AIDS. 2020. https://www.cdc.gov/hiv/basics/whatishiv.html
- 2.UNAIDS Western and central Africa HIV summit. 2021. https://www.unaids.org/en
- 3.World health organization (WHO) HIV/AIDS. 2021. https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- 4.UNAIDS Pakistan. 2021. https://www.unaids.org/en/regionscountries/countries/pakistan
- 5.National AIDS Control Programme Pakistan. 2020. https://nacp.gov.pk/
- 6.Mir F., Mahmood F., Siddiqui A.R., Baqi S., Abidi S.H., Kazi A.M., Nathwani A.A., Ladhani A., Qamar F.N., Soofi S.B., Memon S.A., Soomro J., Shaikh S.A., Simms V., Khan P., Ferrand R.A. HIV infection predominantly affecting children in Sindh, Pakistan, 2019: a cross-sectional study of an outbreak. Lancet Infect. Dis. 2020;20:362–370. doi: 10.1016/S1473-3099(19)30743-1. [DOI] [PubMed] [Google Scholar]
- 7.DAWN The forgotten children of Ratodero - Pakistan. 2020. https://www.dawn.com/news/1593308
- 8.Hogan A.B., Jewell B.L., Sherrard-Smith E., Vesga J.F., Watson O.J., Whittaker C., Hamlet A., Smith J.A., Winskill P., Verity R., Baguelin M., Lees J.A., Whittles L.K., Ainslie K.E.C., Bhatt S., Boonyasiri A., Brazeau N.F., Cattarino L., Cooper L.V., Coupland H., Cuomo-Dannenburg G., Dighe A., Djaafara B.A., Donnelly C.A., Eaton J.W., van Elsland S.L., FitzJohn R.G., Fu H., Gaythorpe K.A.M., Green W., Haw D.J., Hayes S., Hinsley W., Imai N., Laydon D.J., Mangal T.D., Mellan T.A., Mishra S., Nedjati-Gilani G., Parag K.V., Thompson H.A., Unwin H.J.T., Vollmer M.A.C., Walters C.E., Wang H., Wang Y., Xi X., Ferguson N.M., Okell L.C., Churcher T.S., Arinaminpathy N., Ghani A.C., Walker P.G.T., Hallett T.B. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Global Health. 2020;8:e1132–e1141. doi: 10.1016/S2214-109X(20)30288-6/ATTACHMENT/BE016118-8E8E-4D35-91BA-55D6F23B89A6/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.UNAIDS Keeping HIV treatment available in Pakistan during COVID-19. 2020. https://www.unaids.org/en/resources/presscentre/featurestories/2020/april/20200415_pakistan