Abstract
Background
Fractures of the distal femur (the part of the thigh bone nearest the knee) are a considerable cause of morbidity. Various different surgical and non‐surgical treatments have been used in the management of these injuries but the best treatment remains controversial.
Objectives
To assess the effects (benefits and harms) of interventions for treating fractures of the distal femur in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 September 2014); the Cochrane Central Register of Controlled Trials (The Cochrane Library, 2014, Issue 8); MEDLINE (1946 to August week 4 2014); EMBASE (1980 to 2014 week 36); World Health Organization (WHO) International Clinical Trials Registry Platform (January 2015); conference proceedings and reference lists without language restrictions.
Selection criteria
Randomised and quasi‐randomised controlled clinical trials comparing interventions for treating fractures of the distal femur in adults. Our primary outcomes were patient‐reported outcome measures (PROMs) of knee function and adverse events, including re‐operations.
Data collection and analysis
Two review authors independently selected studies and performed data extraction and risk of bias assessment. We assessed treatment effects using risk ratios (RR) or mean differences (MD) and, where appropriate, we pooled data using a fixed‐effect model.
Main results
We included seven studies that involved a total of 444 adults with distal femur fractures. Each of the included studies was small and assessed to be at substantial risk of bias, with four studies being quasi‐randomised and none of the studies using blinding in outcome assessment. All studies provided an incomplete picture of outcome. Based on GRADE criteria, we assessed the quality of the evidence as very low for all reported outcomes, which means we are very uncertain of the reliability of these results.
One study compared surgical (dynamic condylar screw (DCS) fixation) and non‐surgical (skeletal traction) treatment in 42 older adults (mean age 79 years) with displaced fractures of the distal femur. This study, which did not report on PROMs, provided very low quality evidence of little between‐group differences in adverse events such as death (2/20 surgical versus 1/20 non‐surgical), re‐operation or repeat procedures (1/20 versus 3/20) and other adverse effects including delayed union. However, while none of the findings were statistically significant, there were more complications such as pressure sores (0/20 versus 4/20) associated with prolonged immobilisation in the non‐surgical group, who stayed on average one month longer in hospital.
The other six studies compared different surgical interventions. Three studies, including 159 participants, compared retrograde intramedullary nail (RIMN) fixation versus DCS or blade‐plate fixation (fixed‐angle devices). None of these studies reported PROMS relating to function. None of the results for the reported adverse events showed a difference between the two implants. Thus, although there was very low quality evidence of a higher risk of re‐operation in the RIMN group, the 95% confidence interval (CI) also included the possibility of a higher risk of re‐operation for the fixed‐angle device (9/83 RIMN versus 4/96 fixed‐angle device; 3 studies: RR 1.85, 95% CI 0.62 to 5.57). There was no clinically important difference between the two groups found in quality of life assessed using the 36‐item Short Form in one study (23 fractures).
One study (18 participants) provided very low quality evidence of there being little difference in adverse events between RIMN and non‐locking plate fixation. One study (53 participants) provided very low quality evidence of a higher risk of re‐operation after locking plate fixation compared with a single fixed‐angle device (6/28 locking plate versus 1/25 fixed‐angle device; RR 5.36, 95% CI 0.69 to 41.50); however, the 95% CI also included the possibility of a higher risk of re‐operation for the fixed‐angle device. Neither of these trials reported on PROMs.
The largest included study, which reported outcomes in 126 participants at one‐year follow‐up, compared RIMN versus locking plate fixation; both implants are commonly used in current practice. None of the between‐group differences in the reported outcomes were statistically significant; thus the CIs crossed the line of no effect. There was very low quality evidence of better patient‐reported musculoskeletal function in the RIMN group based on Short Musculoskeletal Function Assessment (0 to 100: best function) scores (e.g. dysfunction index: MD ‐5.90 favouring RIMN, 95% CI ‐15.13 to 3.33) as well as quality of life using the EuroQoL‐5D Index (0 to 1: best quality of life) (MD 0.10 favouring RIMN, 95% CI ‐0.01 to 0.21). The CIs for both results included a clinically important effect favouring RIMN but also a clinically insignificant effect in favour of locking plate fixation.
Authors' conclusions
This review highlights the major limitations of the available evidence concerning current treatment interventions for fractures of the distal femur. The currently available evidence is incomplete and insufficient to inform current clinical practice. Priority should be given to a definitive, pragmatic, multicentre randomised controlled clinical trial comparing contemporary treatments such as locked plates and intramedullary nails. At minimum, these should report validated patient‐reported functional and quality‐of‐life outcomes at one and two years. All trials should be reported in full using the CONSORT guidelines.
Plain language summary
Treatments for breaks in the lower part of the thigh bone in adults
Background and aim
Breaks (fractures) of the lower part of the thigh bone (distal femur) are debilitating and painful injuries. The reduced mobility after these injuries is also an important cause of ill‐health. Sometimes these fractures happen in people who have previously had a knee replacement; this can make treatment of the fracture more complicated.
Many treatments have been used in the management of these injuries. Historically, people were treated in bed with weights holding the leg straight (traction). More recently, surgical fixation of the broken bone has become routine. Methods of surgical fixation include using plates and screws or rods inside the thigh bone to hold the fracture in place while it heals. The technology of these implants has become increasingly advanced with components that 'lock' together, forming a 'locked' device. Despite these advances, the best management of these injuries remains controversial.
This review set out to evaluate the effects, primarily on function, of different methods for treating fractures of the lower end of the femur in adults.
Search results and quality of the evidence
We searched the scientific literature up to September 2014 and found seven relevant studies with 444 participants with these fractures. One study compared surgery with non‐surgical treatment and the other six studies compared the use of different surgical implants. Each of the studies was small and was designed in a way that may affect the reliability of their findings. Most studies did not report on patient‐reported outcomes measures of function. We judged the quality of the reported evidence was very low and thus we are not certain that these results are true.
Key results
The study comparing surgical fixation with non‐surgical intervention (traction and wearing a brace) did not confirm there was any difference between the two treatments in terms of re‐operations or repeat traction and bone healing. However, there were more complications such as pressure sores associated with prolonged immobilisation in the traction group, who stayed on average one month longer in hospital.
Five studies compared one type of nail versus one of three different types of plate fixation. One study compared locked with non‐locked plate fixation. The evidence available for the four comparisons did not confirm that any of the surgical implants were superior to any other surgical implant for any outcomes, including re‐operation for complications such as lack of bone healing and infection.
Conclusions
The review found that the available evidence was very limited and insufficient to inform current clinical practice. Further research comparing commonly used surgical treatments is needed.
Background
Description of the condition
Fractures of the distal femur (the part of the thigh bone nearest the knee) account for 4% to 6% of all femoral fractures (Kolmert 1982), and about 0.4% of all adult fractures (Court‐Brown 2006). Annual incidences of between 4.5 and 11.7 per 100,000 people have been reported (Arneson 1988; Court‐Brown 2006). Fractures of the distal femur typically occur in two groups of individuals: younger people sustaining high‐energy trauma, such as motor vehicle accidents; and after a fall in older adults, typically women, with osteoporosis. Eighty‐five per cent of distal femoral fractures occur in older adults (Martinet 2000). However, over recent decades, a third group has emerged ‐ people with periprosthetic fractures occurring around previous total knee replacements. Periprosthetic fractures have a reported incidence of 0.6% of primary and 1.7% of revision knee arthroplasties at five years post‐operatively (Meek 2011).
There are various classification systems for distal femoral fractures but fractures can broadly be classified as those that occur with or without extension into the knee joint (intra‐ and extra‐articular). Extra‐articular fractures are the most common (Martinet 2000), and these are often comminuted (Zlowodzki 2006). Fractures around the undulating growth plate of the distal femur in skeletally immature people predispose them to a high incidence of growth arrest. Children require very different surgical treatment and follow‐up compared with adults with these fractures and are not included in this review (Wall 2012). For periprosthetic fractures, an additional consideration is whether the knee replacement is still functional (i.e. not loose following the injury) and the compatibility of the surgical approach and implants with the knee arthroplasty components that are in situ.
Description of the intervention
Distal femoral fractures can be treated either surgically or conservatively (non‐operatively). non‐operative treatment, which is usually reserved for less severe injuries such as undisplaced fractures, generally involves some form of immobilisation such as hinged knee braces for more stable fractures to immobilisation in a long‐leg cast for six to 12 weeks followed by bracing. Stabilisation is the initial step in the treatment of distal femoral fractures. A variety of options are available including a long‐leg splint, cast, skin or skeletal traction. In people with polytrauma, an external fixator may be used until definitive treatment is possible. These interventions act to reduce discomfort and prevent any further soft tissue injury.
Definitive surgical interventions include:
intramedullary nailing with either antegrade or retrograde approaches, usually fixed with interlocking screws;
open reduction and plating with angled blade plate, dynamic condylar screw (DCS) or condylar buttress plate;
indirect reduction using locking plate systems, for example, Less Invasive Stabilization System (LISS);
external fixation with ring or axial frames;
total knee replacement (replacement of both the distal femur and the proximal tibia). This usually requires the use of a hinged prosthesis, or a revision femoral replacement component. The use of standard femoral components is rarely possible.
Periprosthetic fractures around a total knee replacement can often be treated using the same techniques as are available when no prosthesis is in situ if the knee replacement is not loose. Certain factors need to be taken into consideration in periprosthetic fractures such as the width of the intercondylar box (to allow retrograde nail passage), the amount of bone remaining on the distal fragment and the space available for fixation devices; the lattermost may be compromised by the intercondylar box in posterior stabilised or constrained implants or stems. These factors may make certain treatments less desirable or impossible. Fractures around a loose total knee replacement mandate revision of the prosthesis rather than fixation alone. Coincident proximal prostheses such as hip replacements or metalwork from previous proximal femoral fracture fixation may make certain treatments less feasible; surgeons may favour retrograde nailing when a proximal sliding hip screw is in situ and plating where a hip arthroplasty is present in order to reduce the risk of future fracture between the implants.
How the intervention might work
Treatment of these fractures, whether surgical or non‐surgical, seeks to stabilise the fracture to allow the natural healing process to occur. Bone healing requires adequate 'biology' in the form of blood supply to the fracture site ‐ this may be made worse by surgery if soft tissues are stripped from the bone or potentially improved by surgery with bone grafting, bringing osteoprogenitor cells to the fracture site. Bone healing also requires an appropriate mechanical environment; fracture ends must be reduced and opposed enough to allow new bone to bridge the gap and the fracture must be held rigidly enough for healing to occur. How rigidly these fractures should be held depends on the fracture pattern and is still an area of debate. If fracture healing does not occur, people may experience pain and metalwork may fatigue and break.
Non‐surgical interventions aim to hold the fracture in an acceptable position until it is healed enough to allow knee movement and weight‐bearing. This can take a long time and prolonged immobilisation may lead to knee stiffness and pain (Crist 2008), as well as other complications such as pressure sores, chest infection and venous thromboembolic phenomena. It may be difficult to achieve adequate reduction of the fracture and holding it still enough for the fracture to unite may also not be possible especially in obese people. Compared with surgery, non‐surgical treatment may have a higher complication risk in terms of non‐union and malunion, with serious functional consequences (Butt 1996a).
The aim of surgical treatment is to re‐position the fractured bone, including reducing the articular surfaces within the knee joint if disrupted, restore limb alignment and hold it in this position until bony union. Although fractures of the distal femur may be comminuted (multi‐fragmentary) making anatomical reduction of all fracture fragments impossible or impractical, restoration of sagittal, coronal and rotational alignment of the bone should be achievable in all cases regardless of the complexity of the fractures. Surgical fixation should allow a mechanical environment suitable for bone healing. It should also allow earlier range of movement of the knee and potentially earlier weight‐bearing. Older people with osteoporosis who are at high risk of fracture fixation failure, such as in very distal fractures or intra‐articular fractures, may benefit from total knee arthroplasty (Rosen 2004), as may people with pre‐existing symptomatic arthritis of the affected joint. The main disadvantage of surgical intervention is the potential for surgical complications including implant failure and additional damage to local blood supply resulting in non‐union and infection (Foster 2006).
The underlying mechanisms and aims of management of periprosthetic fractures are similar to the above but, as described above, consideration is required in terms of whether the knee replacement is still functional (i.e. not loose following the injury) and the potential interaction of new implants with those already in situ.
Why it is important to do this review
Fractures of the distal femur are challenging to treat. Many surgical interventions have been developed for their treatment. New interventions are being developed and more traditional interventions are losing favour (Zlowodzki 2006). We reviewed the current evidence available and compared the outcomes of different treatment modalities to guide best practice. This review also helps identify key areas that require further research.
Objectives
To assess the effects (benefits and harms) of interventions for treating fractures of the distal femur in adults.
We defined a priori the following broad objectives:
To compare different methods of non‐surgical treatment
To compare surgical versus non‐surgical treatment
To compare different methods of surgical treatment
We considered three distinct patient populations: those sustaining a fracture in a normal (native) knee or in bone near an intact knee replacement or in bone near a loose knee replacement.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised and quasi‐randomised (method of allocating participants to a treatment that is not strictly random, e.g. by hospital number) controlled clinical trials evaluating one or more interventions for treating fractures of the distal femur.
Types of participants
We included adults with an acute fracture of the distal femur. We anticipated that the distal femur would be defined variably perhaps using a classification system such as AO (distal femur = category 33) (Marsh 2007; Müller 1990), or perhaps more simply as principally beyond the isthmus or involving the distal metaphysis. We excluded trials exclusively reporting on children (skeletally immature participants) but we would have included those containing adults with a subgroup of children where the proportion of children was small and similar in the intervention groups, or separate data were available for the adult subpopulation. Iatrogenic fractures typically sustained during arthroplasty surgery were not eligible. However, acute periprosthetic fractures around established arthroplasties were included.
We also planned to include, but present separately, trials including adults with an in situ knee arthroplasty (of any type). As treatment options for participants with an intact knee replacement are distinct from those for a loose knee replacement, our initial intention was to also consider these separately.
Types of interventions
Any and all comparisons between those interventions described in the Description of the intervention were eligible for this review. Interventions were grouped as: non‐surgical treatment, retrograde intramedullary implants, antegrade intramedullary implants and fixed‐angle plates (i.e. locking plates), non‐fixed‐angle plates, those with a single fixed‐angle distal screw (e.g. DCS), external fixators and arthroplasty. Pharmacological interventions were not eligible.
We grouped the comparisons under the three objectives. We established the following provisional hierarchy a priori to define the 'control' intervention for comparisons between different non‐surgical interventions and between different surgical interventions. For non‐surgical interventions, we defined the treatment that involves the least immobilisation (such as duration of cast immobilisation) as the control. For surgical interventions, we selected the control treatment in the following order:
non‐fixed‐angle plates;
single component fixed‐angle plates;
locking plates;
external fixators;
antegrade intramedullary implants;
retrograde intramedullary implants;
arthroplasty.
Types of outcome measures
The primary focus was on long‐term functional outcome, preferably measured at one year or more.
Primary outcomes
Validated patient‐reported functional outcomes of the knee (e.g. Western Ontario and McMaster Universities Arthritis Index (WOMAC), Oxford Knee Score (OKS)).
Adverse events (e.g. infection, secondary or re‐operation).
Secondary outcomes
Patient‐reported quality of life (e.g. EuroQoL 5 Dimensions (EQ‐5D)).
Pain, using validated scores (e.g. visual analogue scale (VAS)).
Objective performance measures (e.g. Get up and go test, walking speed).
Symptomatic non‐union.
Malunion.
Resource use.
Timing of outcome assessment
As we expected most studies reported outcomes at a number of follow‐up times. We considered less than six months as short term, between six and 12 months as intermediate‐term follow‐up and greater than 12 months as long‐term follow‐up.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (9 September 2014); the Cochrane Central Register of Controlled Trials (The Cochrane Library, 2014, Issue 8); MEDLINE (1946 to August week 4 2014); MEDLINE In‐Process & Other Non‐Indexed Citations (8 September 2014) and EMBASE (1980 to 2014 week 36). There were no language restrictions.
The MEDLINE strategy followed guidelines outlined within the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). The subject‐specific strategy was combined with the sensitivity‐maximising version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE (Lefebvre 2011). Appendix 1 shows the search strategies for The Cochrane Library, MEDLINE and EMBASE.
We also searched the World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal for ongoing and recently completed trials (22 January 2015) (seeAppendix 1), and identified conference abstracts by searching The Bone & Joint Journal orthopaedic proceedings (2006 to 2013) (seeAppendix 1).
Searching other resources
We checked the reference lists from identified trials for any additional relevant trials.
Data collection and analysis
Selection of studies
Two review authors (MZ and JM) independently identified potentially eligible trials from the electronic search results. Each review author (MZ, JM and XG) obtained full texts of all potentially eligible studies and independently reviewed them. We attempted unsuccessfully to contact all trial authors to request further information regarding trial methods. Where disagreement existed concerning eligibility, we reached consensus through discussion amongst all review authors.
Data extraction and management
Each review author (MZ, JM, and XG) independently extracted data from each included trial report using a pre‐piloted data collection form. We recorded details of study methods, participants, interventions and outcomes. We resolved any disagreements through discussion. The data collected were entered into Review Manager software (RevMan 2014) by one review author (XG) and checked by another review author (NP). No attempt was made to mask the trial reports.
Assessment of risk of bias in included studies
Two review authors (MZ and JM) independently assessed risk of bias in included studies using Cochrane's 'Risk of bias' tool (Higgins 2011b). This tool assesses randomisation (sequence generation and allocation concealment), blinding (of participants and personnel; and outcome assessment), completeness of outcome data, selection of outcomes reported and other sources of bias. The 'other sources of bias' that we assessed were major imbalances in important baseline confounders (e.g. age or type of fracture) and performance bias such as that resulting from lack of comparability in the experience of care providers. No attempt was made to mask the trial reports.
Where disagreement existed concerning the assessment, we reached consensus through discussion amongst all review authors.
Measures of treatment effect
For dichotomous outcomes, we used risk ratios (RR) with 95% confidence intervals (CI). For continuous data, such as functional scores, we calculated mean differences (MD) with 95% CI. We had planned that where studies reported various instruments to measure the same continuous outcome, we would calculate standardised mean differences (SMD) with 95% CI.
Unit of analysis issues
We were aware of potential unit of analyses issues arising from inclusion of participants with bilateral fractures. There was a report of just one person with bilateral fractures (Hartin 2006), but there was insufficient information to quantify the small difference this would have made to study findings.
We expected that most studies would report outcomes at a number of follow‐up times. We had planned to present these within the short‐, medium‐ and long‐term follow‐up categories stipulated in Types of outcome measures; however, inadequate data were available to perform separate analyses at each time point.
As expected, studies reported simple parallel‐group designs. If other designs had been reported (e.g. cluster‐randomised designs), we would have used generic inverse variance methods to combine data where appropriate.
Dealing with missing data
We attempted to contact study authors where data or study information were missing, but did not receive any replies.
Where data continued to be missing for binary outcomes, we planned to class these outcomes as treatment failures (worst‐case analysis). Similarly, where there were missing data for continuous outcomes, we planned to make a conservative estimate of the treatment effect by attributing outcomes in the treatment group values two standard deviations from the mean of the distribution. We aimed to present effect sizes with and without these adjustments ('as‐reported' and 'worst‐case analyses') in order to check the effect of these assumptions (seeSensitivity analysis). Unfortunately, insufficient data were available in the reports of the studies to apportion data loss to one or other of the treatment groups.
Where standard deviations were not specifically reported, we determined these from standard errors, CIs or exact P values, if available.
Assessment of heterogeneity
We first assessed the degree of statistical heterogeneity between studies visually from inspection of the forest plot. Heterogeneity was more formally tested using the Chi2 test and I2 statistic (Higgins 2003). We set a conservative P value for Chi2 of less than 0.1 to indicate significant heterogeneity between studies. We interpreted values of I2 as follows: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% indicated considerable heterogeneity (Deeks 2011).
Assessment of reporting biases
Insufficient studies were available to complete the planned funnel plots.
Data synthesis
There were insufficient studies to report the results for the three patient populations (normal (native) knee, intact knee replacement, loose knee replacement) described in Types of participants separately, as we had planned. Where appropriate, we pooled results of comparable groups of trials using a fixed‐effect model. This model was chosen since there were few studies suitable for pooling and there was little statistical heterogeneity and also little clinical diversity between studies. Where we performed a meta‐analysis, we presented a summary estimate of the effect size with 95% CI.
Subgroup analysis and investigation of heterogeneity
Possible subgroup analyses that were specified a priori included:
-
Age:
over 60 years (as a surrogate for osteoporosis).
-
Fracture severity:
extra‐articular versus intra‐articular;
by fracture classification (e.g. main categories of the AO classification) if sufficient data were available;
open (Gustilo and Anderson Grade II or III) versus closed (closed or Gustilo and Anderson Grade I) (Gustilo 1976).
Insufficient data were available to support the reporting of such analyses. We had planned to investigate whether the results of subgroups were significantly different by inspecting the overlap of CIs and performing the test for subgroup differences available in Review Manager 5 (RevMan 2014).
We had planned that if one or more studies appeared to be a clear outlier, we would check the data for these studies carefully for errors or other methodological or clinical reasons why they might differ from the other studies. If good reason had been found why the studies differed from the majority then we would have noted this, and removed the studies from the main meta‐analyses. Insufficient data were available to facilitate such analyses.
Sensitivity analysis
If sufficient data had been available, we planned to perform sensitivity analyses to examine various aspects of trial and review methodology, 'worst case' and as 'reported analyses' as described in Dealing with missing data, the selection of statistical model (fixed‐effect versus random‐effects) for pooling, the effects of excluding trials at high or unclear risk of bias, such as selection bias arising from the lack of allocation concealment, and exclusion of 'outlier' trials.
'Summary of findings' tables
Insufficient data were available to summarise the results for the main comparisons usefully in a 'Summary of findings' table. We used the GRADE approach to assess the quality of the evidence for each comparison (GRADE 2004). This system qualifies recommendations based upon the quality of the supporting evidence as one of four categories, the highest of which is reserved for randomised controlled studies. However, the quality of the evidence may be downgraded against five specified criteria: high risk of bias, lack of generalisability of evidence, unexplained statistical heterogeneity, imprecision of effect estimates or high risk of publication bias (Schünemann 2011).
Results
Description of studies
Results of the search
The search was completed in September 2014. We found 720 records from the following databases: Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (18 records); Cochrane Central Register of Controlled Trials (92), MEDLINE (356), EMBASE (179), the WHO International Clinical Trials Registry Platform (11) and Bone & Joint Journal Orthopaedic Proceedings (64). We received notice of another trial report at editorial review. We removed 169 duplicates and screened 551 records. Of these, we excluded 525 and assessed 26 full‐text articles for eligibility. A summary of the study selection process is shown in Figure 1.
1.

Study flow diagram.
The search identified 22 studies (published in 26 reports) for potential inclusion. Upon further analysis, we included seven studies (Butt 1996b; Christodoulou 2005; Dar 2009; DeCoster 1995; Hartin 2006; Leighton 2011; Tornetta 2013), excluded nine (Firoozabadi 2012; Gao 2013; Han 2011; Horneff 2013; Markmiller 2004; Petsatodis 2010; Thomas 1981; Tornetta 2000; Vallier 2012), and identified five ongoing studies (NCT00644397; NCT01553630; NCT01693367; NCT01766648; NCT01973712). Tornetta 2013 is an interim report of on an ongoing study. The final study is awaiting classification (Hanschen 2014).
Included studies
The seven included studies involved 444 adults (445 fractures) and no children (Butt 1996b; Christodoulou 2005; Dar 2009; DeCoster 1995; Hartin 2006; Leighton 2011; Tornetta 2013). These are summarised below, with a full summary for each study detailed in the Characteristics of included studies table.
Design
Four included studies were quasi‐randomised controlled trials (Butt 1996b; Christodoulou 2005; Dar 2009; DeCoster 1995), and two studies were randomised controlled trials (Hartin 2006; Tornetta 2013). There was insufficient information for Leighton 2011 to establish the study design type but it is likely to have been randomised.
Study size
The study population sizes at allocation varied but generally small: 18 participants (DeCoster 1995), 22 participants with 23 fractures (Hartin 2006), 42 participants (Butt 1996b), 53 participants (Leighton 2011), 73 participants (Dar 2009), 80 participants (Christodoulou 2005), and 156 participants (Tornetta 2013).
Setting
All of the studies were conducted in the hospital setting. Four studies were single‐centre studies: Butt 1996b in the UK, Christodoulou 2005 in Greece, Dar 2009 in India and DeCoster 1995 in the USA. The remaining three studies were multicentre trials: Hartin 2006 conducted a two‐centre trial in Australia, Leighton 2011 conducted a six‐centre trial in Canada and Tornetta 2013 conducted a multicentre trial involving 22 centres in the USA. The opening year of participant recruitment ranged from 1988 in Butt 1996b to 2007 in Tornetta 2013. The period of recruitment was not stated for DeCoster 1995 or confirmed for Leighton 2011 and Tornetta 2013.
Participants
Information on gender was reported for five studies: Christodoulou 2005 (25 men, 47 women), Dar 2009 (41 men, 27 women), Hartin 2006 (7 men, 16 women), Leighton 2011 (18 men, 35 women) and Tornetta 2013 (71 men, 55 women). In studies that provided information about age (Christodoulou 2005; Dar 2009; DeCoster 1995; Tornetta 2013), participant age varied between 16 and 90 years. Butt 1996b restricted participants to those over 60 years and therefore recruited an older population (mean age: 79 years) than the other included studies. In contrast, the mean age of participants, all of whom had open fractures resulting from high‐energy trauma, was 35 years in DeCoster 1995. Hartin 2006 excluded participants who were skeletally immature but reported no maximum age limit.
Butt 1996b included participants with displaced fractures of the distal femur. Christodoulou 2005, Hartin 2006, and Leighton 2011 included participants with supracondylar distal femur fractures. Dar 2009 included participants with only closed distal femur fractures, whereas DeCoster 1995 included only participants with open distal femur fractures. Hartin 2006 was the only study to report periprosthetic fractures with one periprosthetic fracture in each group. These could not be separated for analysis. Tornetta 2013 recruited only participants with AO/ASIF 33A1‐3 (extra‐articular) or C1 (simple complete articular) fractures of the distal femur.
Interventions
Only Butt 1996b reported a comparison between surgical and non‐surgical treatment. Butt 1996b reported outcomes after DCS fixation, with or without medial bone grafting, compared with non‐surgical treatment. The non‐operative treatment consisted of skeletal traction with Denham pin and Thomas splint, followed by splint removal and Perkin's exercises at three to four weeks, followed by a functional cast brace at six to eight weeks.
The other six studies compared different methods of surgical treatment (Christodoulou 2005; Dar 2009; DeCoster 1995; Hartin 2006; Leighton 2011;Tornetta 2013).
DeCoster 1995 compared retrograde intramedullary nailing (RIMN) versus indirect reduction and non‐fixed‐angle buttress plate fixation. In both groups articular fragments were reduced and held with lag screws. Range of motion exercises were started immediately post‐operatively and weight‐bearing was allowed when there was radiographic evidence of callus.
Christodoulou 2005, Dar 2009, and Hartin 2006 compared RIMN with fixation using a single fixed‐angle device. Christodoulou 2005 used the intercondylar notch approach in the RIMN participants, locking the nail with two proximal and two or three distal screws. In the plate group, a 95° angle blade plate was used, with or without primary autologous bone grafting. Dar 2009 and Hartin 2006 reported similar comparisons between RIMN and DCS; fractures were reduced closed and the DCS inserted percutaneously in the study reported by Dar 2009 and an open approach used in Hartin 2006.
Leighton 2011 reported a comparison between a locking plate system (LISS) with a DCS.
Tornetta 2013 reported a comparison between two commonly used contemporary implants ‐ a reamed, locked RIMN and a locking plate.
Outcomes
Length of follow‐up ranged between 12 months (Tornetta 2013) and a mean of 30 months (Dar 2009). Follow‐up schedules were not provided for Butt 1996b and Leighton 2011. Only two studies reported patient‐rated outcome measures: Hartin 2006 reported on the 36‐item Short Form (SF‐36) health survey results at a minimum of 12 months and Tornetta 2013 reported patient‐reported functional and quality of life scores. All trials reported on adverse events, including re‐operations, and failure of union. Other clinical outcome measures reported included categories based on Schatzker and Lambert criteria (full extension, loss of flexion, valgus/varus/rotational deformity, pain, joint congruency) (Schatzker 1979) reported in Butt 1996b and Christodoulou 2005.
Excluded studies
Tornetta 2000 reported "all patients with femoral shaft fractures", excluding fractures within 3 cm from knee joint. We excluded this study because it was not possible to extract the data specific to distal femoral fractures. Despite efforts, we were unable to contact the corresponding author.
Ongoing studies
Full details of the five ongoing studies are presented in the Characteristics of ongoing studies table. NCT01973712 will report a performance outcome (timed up and go test) following a comparison of the common contemporary interventions for these fractures ‐ retrograde nails and locking plates. Two studies will report functional and performance outcomes following the comparison of two different types of locking screw technology in anatomical angular‐stable locking plates (NCT01693367; NCT01766648). NCT00644397 will report the comparison between locking plates and a single fixed‐angle device and NCT01553630 the effect of contemporaneous bone grafting on locking plate fixation. Both of these last two studies will focus on radiographic outcomes and adverse effects. The participants included in each of the studies are comparable ‐ adults with displaced fractures of the distal femur, the majority of which will be closed and extra‐articular, although each study has subtly differing eligibility criteria. Each study is planned to be relatively small and it is anticipated that none of the studies will provide a definitive answer.
Studies awaiting classification
Full details of the single study awaiting classification can be found in the Studies awaiting classification table. Hanschen 2014 reports a small multicentre study involving 27 participants with periprosthetic fractures fixed with one of two types of locking screws locked to an anatomical angular‐stable locking plate. Outcomes include pain, adverse events and patient‐reported functional scores.
Risk of bias in included studies
The quality of reporting of the studies varied but was generally poor, with trials reports being limited to conference abstracts in three studies (DeCoster 1995; Leighton 2011; Tornetta 2013). A detailed description of the assessment of the risk of bias is given in the Characteristics of included studies table. Figure 2 presents a summary of the assessment of the risk of bias in each study.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Only Hartin 2006 was at low risk of selection bias reflecting a valid method of random sequence generation with allocation concealment. Tornetta 2013 reported a valid method of random sequence generation but gave insufficient details to be establish there was allocation concealment. The method of randomisation was not reported by Leighton 2011, which is thus at unclear risk of bias. The other four studies were quasi‐randomised based on either date of admission (Butt 1996b) or alternation (Christodoulou 2005; Dar 2009; DeCoster 1995), and were therefore at high risk of bias.
Blinding
The nature of the interventions being compared in the included studies meant that no blinding of treatment providers was possible. Lack of blinding of trial participants was confirmed in Leighton 2011 and Tornetta 2013. Participant blinding was also very unlikely in the other five trials. Thus, all seven included trials were at high risk of performance bias.
All seven trials were at high risk of detection bias. None of the trials reported blinding of outcome assessment. Lack of blinding of outcome assessors was confirmed in Hartin 2006, where clinical assessment was made by the operating surgeon, and in Leighton 2011 and Tornetta 2013, which were described as open‐label trials in their trial registration documents.
Incomplete outcome data
All seven studies were at unclear risk of attrition bias for various reasons. Loss to follow‐up was not reported in DeCoster 1995 and Leighton 2011; and not split by treatment group in three other studies (Christodoulou 2005; Dar 2009; Tornetta 2013). As well as loss to follow‐up, the effect on outcome of the cross‐over in Butt 1996b was unknown. The same uncertainty applied to the participant with bilateral fractures included in Hartin 2006.
Selective reporting
The poor quality of reporting of outcome measurement in the methods and results hampered the assessment of the risk of bias from selective reporting of outcomes. No protocols were available for comparing with the trial reports. However, both Leighton 2011 and Tornetta 2013 are registered with clinicaltrials.gov. Leighton 2011 was at high risk of selection bias because of the failure to report on patient‐reported function and quality‐of‐life measures listed in the trial registration document. The others were at unclear risk of reporting bias.
Other potential sources of bias
Imbalance in baseline characteristics
The three studies that adequately reported baseline participant demographics showed no significant imbalances in characteristics between treatment groups (Christodoulou 2005; Dar 2009; Hartin 2006). The remaining studies were at unclear risk from this bias.
Care provider expertise
Since none of the included studies reported on the experience of the care providers for any of the interventions, we judged these at unclear risk of bias for this item.
Effects of interventions
Different methods of non‐surgical treatment
None of the studies reported comparisons of different methods of non‐surgical treatment.
Surgical versus non‐surgical treatment
Only Butt 1996b reported a comparison of surgical and non‐surgical treatment. Butt 1996b compared DCS fixation versus skeletal traction followed by bracing in 42 people over 60 years of age (mean age 79 years) with displaced fractures of the distal femur. Two people, one of whom died in hospital, in the traction group were excluded because they should have been judged unfit for surgery. Moreover, one person in the surgery group was crossed over to the traction group when the person's family refused permission for surgery. Since our attempts to contact the authors were unsuccessful, the data presented below were based on 'treatment received' and not intention‐to‐treat.
Primary outcomes
Butt 1996b did not report on validated patient‐reported functional outcome measures (PROMs).
None of the between‐group differences in clinically relevant adverse events reported in Butt 1996b were statistically significant; these were death (2/20 surgical versus 1/20 non‐surgical), re‐operation or repeat procedures (1/20 surgical versus 3/20 non‐surgical), which were all for loosening of implant or traction pins (1 versus 3), deep vein thrombosis (1 versus 3), urinary tract infection (1 versus 4), pneumonia (1 versus 4), pressure sores (0 versus 4) and superficial wound or pin‐tract infection (2 versus 2); see Analysis 1.1. Of note, however, is that the complications, such as pressure sores, more associated with immobilisation and longer hospital stays occurred in greater numbers in the traction group.
1.1. Analysis.
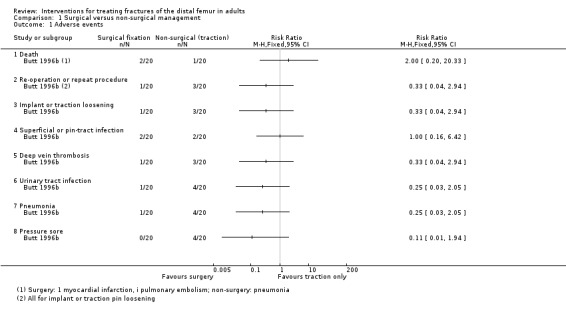
Comparison 1 Surgical versus non‐surgical management, Outcome 1 Adverse events.
Secondary outcomes
Based on a categorical rating system that included clinical and radiological outcomes (extension, flexion, valgus/varus/rotational deformity, pain, joint congruency), Butt 1996b found greater numbers with excellent or good treatment outcomes in the surgery group (9/17 surgical versus 6/19 non‐surgical; analysis not done). There was no significant difference between the two groups in delayed union (1/17 surgical versus 2/19 non‐surgical) or malunion (1/17 surgical versus 3/19 non‐surgical); see Analysis 1.2. Mean hospital stay was on average 33 days shorter in the surgery group (39 days (range 20 to 79) surgical versus 62 days (range 40 to 120) non‐surgical).
1.2. Analysis.
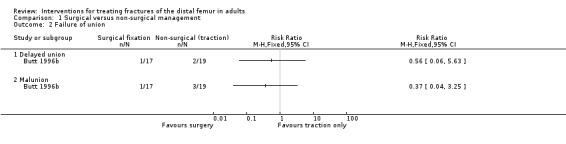
Comparison 1 Surgical versus non‐surgical management, Outcome 2 Failure of union.
Comparison of different methods of surgical treatment
Five trials compared different methods of surgical management (Christodoulou 2005; Dar 2009; DeCoster 1995; Hartin 2006; Leighton 2011). These trials were grouped into three classes of comparison, determined by the groups in the Types of interventions.
Retrograde intramedullary nail versus single fixed‐angle device
Three studies, including 159 participants, compared RIMN fixation versus DCS or blade‐plate fixation (Christodoulou 2005; Dar 2009; Hartin 2006). The allocation of participants who were lost to follow‐up was not reported and our attempts to contact the authors were unsuccessful. Therefore, we analysed the data only on an 'as‐reported' basis.
Primary outcomes
None of the three studies reported any validated PROMs of function.
We pooled data for re‐operation, death and individual adverse events where data were available from two or more studies (Analysis 2.1). Non‐union alone or in addition to another complication such as infection was the reason for eight of 13 re‐operations reported by the three studies. Around twice as many re‐operations occurred in the RIMN group (9/83 RIMN versus 4/96 fixed‐angle device; 3 studies: RR 1.85, 95% CI 0.62 to 5.57). Hartin 2006 also reported a debridement for infection in the RIMN group but it is not clear whether this person went on to have another operation later on. Hartin 2006 reported there was one death in the RIMN group compared with two, one of which was in hospital, deaths in the fixed‐angle device group. The group allocation of the five deaths in Christodoulou 2005 was unknown. The 95% CIs for between‐group differences for both of the above outcomes and all named complications (infection, pneumonia, urinary tract infection, acute renal failure, pressure sores, haematoma, implant failure, nail protrusion) crossed the line of no effect and varied in their direction of effect. Dar 2009 reported an absence of intra‐operative complications and deep vein thrombosis.
2.1. Analysis.
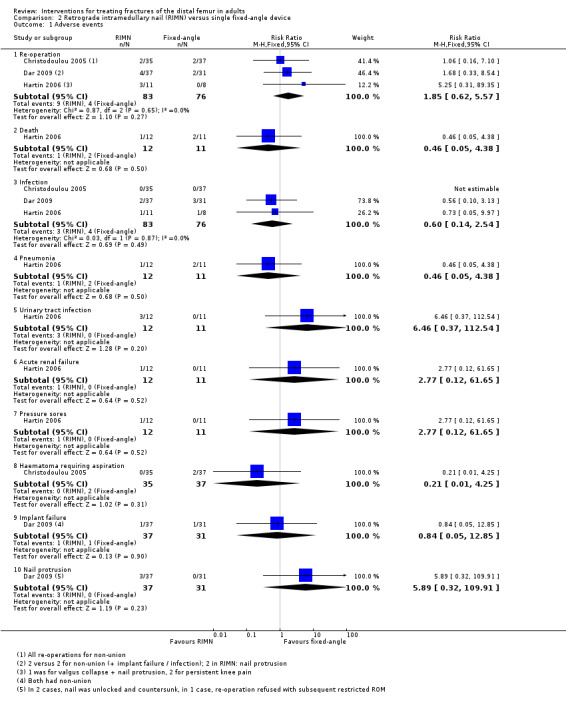
Comparison 2 Retrograde intramedullary nail (RIMN) versus single fixed‐angle device, Outcome 1 Adverse events.
Secondary outcomes
Hartin 2006 reported both mental and physical quality of life using the SF‐36 health‐related quality of life outcome tool. The general health surveys were completed at approximately 20 months in both groups, representing long‐term follow‐up. There was no statistically or clinically significant difference in quality of life between groups in either the physical component (MD ‐0.30, 95% CI ‐11.84 to 11.24; 1 study, 16 participants) or the mental component (MD ‐3.30, 95% CI ‐15.34 to 8.74; 1 study, 16 participants) (Analysis 2.2).
2.2. Analysis.
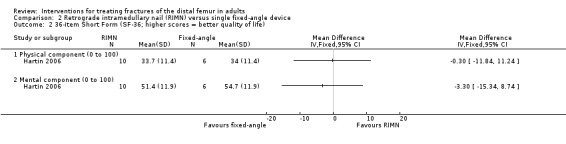
Comparison 2 Retrograde intramedullary nail (RIMN) versus single fixed‐angle device, Outcome 2 36‐item Short Form (SF‐36; higher scores = better quality of life).
Based on a categorical rating system that included clinical and radiological outcomes (extension, flexion, valgus/varus/rotational deformity, pain, joint congruency), Christodoulou 2005 found similar numbers with excellent or good treatment outcomes in the two groups (29/35 RIMN versus 30/37 fixed‐angle; analysis not done).
All three studies reported on symptomatic non‐union and malunion. Non‐union was defined variably but within our defined intermediate window; after six months (Hartin 2006), 28 weeks (Dar 2009), and nine months (Christodoulou 2005). The pooled estimate demonstrated no significant difference in non‐union (5/83 RIMN versus 4/76 fixed‐angle; RR 1.10, 95% CI 0.33 to 3.71; 3 studies, 159 participants) (Analysis 2.3). Malunion was reported at similar time points to non‐union. Again, the pooled estimate showed no significant difference in malunion (3/83 RIMN versus 1/76 fixed‐angle; RR 1.84, 95% CI 0.28 to 11.97; 3 studies, 159 participants) (Analysis 2.3).
2.3. Analysis.
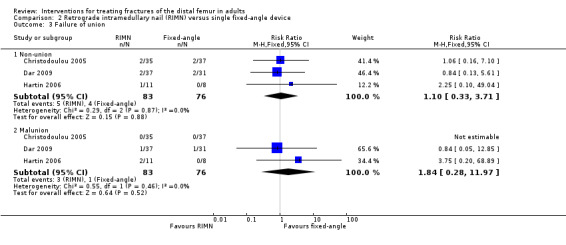
Comparison 2 Retrograde intramedullary nail (RIMN) versus single fixed‐angle device, Outcome 3 Failure of union.
None of the studies reported pain scores or performance measures. However, Christodoulou 2005 reported similar numbers of participants in the two groups regained full mobility (30/35 RIMN versus 31/37 fixed‐angle; analysis not done), with one participants of each group becoming newly bedridden. Hartin 2006 reported similar results in the two groups in the numbers who were able to walk without walking aids (5/11 RIMN versus 4/8 fixed‐angle) at follow‐up of 12 months or over.
Two studies reported length of hospital stay (Christodoulou 2005; Hartin 2006). Mean length of hospital stay was three days shorter for RIMN participants of Christodoulou 2005 (mean 16.4 days RIMN versus 19.2 days fixed‐angle; MD 2.80 days, 95% CI 2.20 to 3.40). In Hartin 2006, the mean length of hospital stay was 36 days in the RIMN group and 38 days in the fixed‐angle device group.
Retrograde intramedullary nail versus non‐locking plate fixation
DeCoster 1995 compared RIMN versus buttress plate fixation in 18 participants with open distal femur fractures.
Primary outcomes
DeCoster 1995 did not report on validated PROMs.
DeCoster 1995 reported that two RIMN group participants versus one plate group participant had complications. These were one late infection in RIMN group and two delayed unions, one in each group (seeAnalysis 3.1). Subsequent treatment for infection was not described.
3.1. Analysis.
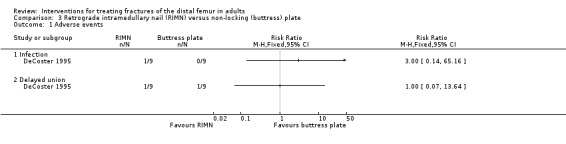
Comparison 3 Retrograde intramedullary nail (RIMN) versus non‐locking (buttress) plate, Outcome 1 Adverse events.
Secondary outcomes
Based on a categorical rating system that included clinical outcomes (knee range of motion and pain) and radiological outcomes (angulation and shortening), DeCoster 1995 reported there was no difference in functional outcome between the treatment groups (five participants in each group had excellent or good results). All fractures healed, delayed union occurring in one participant of each group (seeAnalysis 3.1).
Locking plate versus single fixed‐angle device
Leighton 2011 compared a locking plate (LISS) versus a DCS in 53 participants with a supracondylar fracture of the distal femur.
Primary outcomes
Leighton 2011 reported no validated PROMs, although measurement of these was indicated in the registration document of this trial.
There was a greater number of participants having a re‐operation in the LISS group (6/28 locking plate versus 1/25 fixed‐angle device; RR 5.36, 95% CI 0.69 to 41.50; P value = 0.11; seeAnalysis 4.1). The six re‐operations in the LISS group resulted from non‐union, early loss of reduction and knee arthrofibrosis. The re‐operation in the DCS group resulted from a non‐union.
4.1. Analysis.
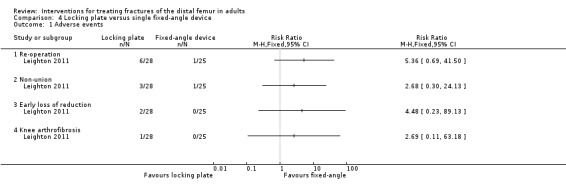
Comparison 4 Locking plate versus single fixed‐angle device, Outcome 1 Adverse events.
Secondary outcomes
Only the non‐union was reported. There were three participants with non‐union in the LISS group and one participant with non‐union in the DCS group (seeAnalysis 4.1).
Retrograde intramedullary nail versus locking plate
Tornetta 2013 was the only study to report a comparison between contemporary implants, a reamed, locked, RIMN and a locking plate, in 156 participants with AO/ASIF A1, 2, 3 and C1 fractures of the distal femur. Incomplete one‐year results were reported in a conference abstract. Due to a combination of incompletely reported outcomes (no measures of variance were reported) and a lack of details on the treatment group of the 30 participants loss to follow‐up at one year, we were unable to report a 'completed‐case' analysis. Rather we have assumed data to have been missing at random and performed analyses using group size as 'per‐allocation'.
Primary outcomes
Tornetta 2013 reported functional outcome using the Short Musculoskeletal Function Assessment (SMFA). This is made up of two component standardised indices ‐ dysfunction and bother indices, where higher scores represent worse function. There was no statistically significant differences between treatments in the two components of the SMFA (dysfunction: MD ‐5.90 favouring RIMN, 95% CI ‐15.13 to 3.33; bother: MD ‐8.20 favouring RIMN; 95% CI ‐19.63 to 3.23; 156 participants; seeAnalysis 5.1). Tornetta 2013 referred to a minimum clinical relevance score of 5.5 for this outcome. Revision surgery was reported for non‐union or failure in 5% of nails and 8% of plates (the denominators are not clear for this outcome). Denominators were provided for the removal of implants or components of implants (8/54 RIMN versus 6/60 plate; RR 1.48 favouring locking plate, 95% CI 0.55 to 4.00; 114 participants; seeAnalysis 5.2). One death and five venous thromboembolic events were reported but not categorised by treatment group.
5.1. Analysis.
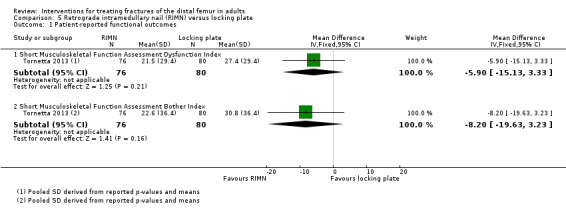
Comparison 5 Retrograde intramedullary nail (RIMN) versus locking plate, Outcome 1 Patient‐reported functional outcomes.
5.2. Analysis.
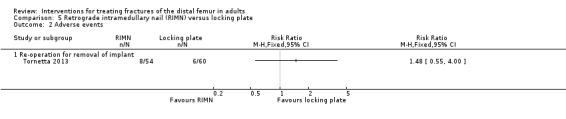
Comparison 5 Retrograde intramedullary nail (RIMN) versus locking plate, Outcome 2 Adverse events.
Secondary outcomes
The EQ‐5D score was used to report quality of life outcomes in both groups. This widely used outcome tool comprises five questions that can be converted to a population‐specific utility index where a score of 1.0 represents maximum quality of life. Although favouring the RIMN group, and including a clinically important difference, the CI crossed the line of no effect (MD 0.10 favouring RIMN, 95% CI ‐0.01 to 0.21 in favour of RIMN; 156 participants; see Analysis 5.3).
5.3. Analysis.
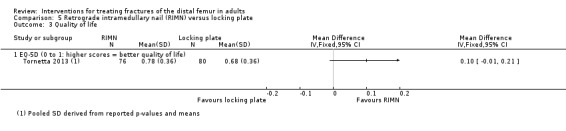
Comparison 5 Retrograde intramedullary nail (RIMN) versus locking plate, Outcome 3 Quality of life.
Complications of union (malunion and non‐union) were variably reported, likely due to the interim nature of the report and the difficulty of defining union. Malunion was defined as malalignment in any plane greater than five degrees and non‐union as implant failure requiring re‐operation. There were no significant differences between RIMN and locking plate groups for either of these outcomes (seeAnalysis 5.4).
5.4. Analysis.
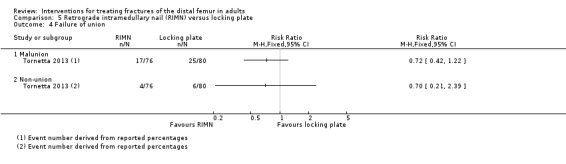
Comparison 5 Retrograde intramedullary nail (RIMN) versus locking plate, Outcome 4 Failure of union.
Discussion
Summary of main results
We found seven studies that involved 344 participants (345 fractures). Each of the included studies was small and assessed to be at substantial risk of bias.
The single study comparing surgical (DCS) versus non‐surgical (skeletal traction) treatment in 42 older adults did not report on participant‐rated outcome measures. There was very low quality evidence of little difference between the two groups in death, re‐operations or repeat procedures, and other adverse effects including delayed union. However, while the findings were not statistically significant, there were more complications such as pressure sores associated with prolonged immobilisation in the non‐surgical group, who stayed on average one month longer in hospital.
Six studies reported comparisons between different surgical interventions.
Three studies, including 159 participants, compared RIMN fixation versus DCS or blade‐plate fixation. None of these studies reported PROMS relating to function. The very low quality evidence did not show a significant treatment effect in any of the reported outcome measures. Thus, although there was very low quality evidence of a higher risk of re‐operation in the RIMN group, the 95% CI also included the possibility of a higher risk of re‐operation for the fixed‐angle device. One study making this comparison found no clinically important difference between the two groups in quality of life assessed using the SF‐36.
One study (18 participants) provided very low quality evidence of there being little difference in adverse events between RIMN and non‐locking plate fixation. One study (53 participants) provided very low quality evidence of a higher risk of re‐operation after locking plate fixation compared with a single fixed‐angle device; however, the 95% CI also included the possibility of a higher risk of re‐operation for the fixed‐angle device. Neither of these trials reported on PROMS.
The largest included study, which reported outcomes in 126 participants at one‐year follow‐up, compared RIMN versus locking plate fixation. None of the between‐group differences in the reported outcomes were statistically significant; thus the CIs crossed the line of no effect. There was very low quality evidence of better patient‐reported musculoskeletal function and quality of life in the RIMN group. The CIs for both results included a clinically important effect favouring RIMN but also a clinically insignificant effect in favour of locking plate fixation.
Overall completeness and applicability of evidence
Completeness of the evidence
Only limited data were available for single comparisons, ranging 18 to 159 participants with distal femur fractures. Only two of the studies reported any PROMs of either function or quality of life. Data for three studies were only reported in conference abstracts; one of these reported on interim findings at one‐year follow‐up.
Application of the evidence to current practice
There are several factors that may affect the application of the evidence to current practice.
The studies included participants with both open and closed fractures of the distal femur. Additionally, the studies' eligibility criteria were comparatively broad, reflecting the population sustaining this injury. However, none of the studies reported outcomes in participants with a fracture about an in situ knee arthroplasty.
There was a trend towards early surgical intervention in these and related long‐bone fractures that requires consideration. It is unlikely that surgeons would now be in a position of equipoise regarding surgical and non‐surgical treatment of such injuries. Moreover, there is also a push to reduce prolonged stays in hospital. Therefore, despite the comparative lack of evidence reported in this review to support surgical intervention, it is unlikely that any randomised trial investigating this comparison could now be conducted.
The majority of data concerned the comparison between an intramedullary nail and a DCS. Currently the DCS is not in frequent use and has been largely replaced by locking plate technology. However, the small study comparing locking plates versus the DCS only provided very limited evidence of effect on re‐operation and non‐union. Despite this lack of evidence, locking plate technology has become widespread around the world. The single study reporting a comparison of contemporary implants (retrograde nails versus locking plates) was small, and at this stage has only reported interim results. A full report of this study, preferably presenting only the results at two years, would enhance our understanding of differences between common, contemporary treatments.
Although the studies were small, they were performed in several centres in six different countries. The eligibility criteria were broad and reflected the population that sustains this injury. Whilst the implants reported in many of the studies have fallen out of current favour, this small sample likely reflects the generality of this population quite well. As none of the included studies included participants with fractures around a knee arthroplasty, this review is currently unable to inform clinical practice in people with this complex injury.
The included studies reported few patient‐reported functional outcome measures or health economics measurements, and few data regarding health‐related quality of life. Such tools are increasingly accepted as the principal means of determining the clinical and cost effectiveness of treatments and would therefore influence the availability of these treatments in some healthcare systems.
Quality of the evidence
The risk of bias of the studies was assessed to be substantial, reflecting the high risk of selection bias in the four quasi‐randomised trials and the high risks of performance and detection biases from lack of blinding in all seven included trials. Thus, in our assessment of the quality of the evidence using GRADE, we downgraded the evidence for all reported outcomes for each reported comparison by one level for study limitations. None of the studies reported a sample size calculation and each was small. It is reasonable to expect therefore that these studies were under‐recruited and not adequately powered. The possibility of a type II error in these studies is considerable. Even for the comparison where pooling was possible, the total number of participants available for pooling was small (159 participants). Thus, we further downgraded the quality of the evidence for all outcomes in all comparisons by two levels for serious imprecision. Thus, we judged the quality of the available evidence to be very low, meaning that we are very uncertain about the estimates.
Potential biases in the review process
None of the authors of this report have been involved in any of the included trials and none have any commercial or other conflict of interest.
We have predominantly searched the published literature. Despite efforts to contact experts, we have not found any unpublished studies. Trial registration was limited over the period that most of these studies were conducted. Therefore, it is possible that some, perhaps commercially sponsored and negative, trials were not published. Hence, some data may exist that we have not included in this review. Our attempts to obtain further information and data from the trial investigators were unsuccessful, unfortunately.
Agreements and disagreements with other studies or reviews
We identified two systematic reviews comparing interventions in the treatment of distal femoral fractures. One review concerned the treatment of fractures of the distal femur around a native knee (Zlowodzki 2006). This was mainly a review of case series and only included one quasi‐randomised controlled trial (Butt 1996b). They found no significant difference in outcome between interventions, in line with the results of this review. The second review concerned the treatment of fractures of the distal femur around a total knee replacement (Herrera 2008). This was a review of case series only. They found reduced RRs for developing non‐union and revision surgery when retrograde nail was compared with a traditional non‐locked plate and also when retrograde nail or locked plates were compared with non‐operative treatment. However, there was substantial diversity amongst the included studies and the non‐randomised nature of treatment allocation allows for the introduction of substantial bias. No randomised controlled trials concerning periprosthetic fractures were found in this review to compare with these conclusions.
Authors' conclusions
Implications for practice.
This review highlighted the serious limitations of the available evidence concerning current treatment of fractures of the distal femur in adults. The currently available evidence is incomplete and insufficient to inform current clinical practice.
Implications for research.
In order to determine the effectiveness of contemporary treatments in the management of fractures of the distal femur, well‐conducted, adequately powered randomised controlled trials are needed. We recommend priority should be given to a multicentre randomised trial that focuses primarily on the currently incompletely explored comparison between the retrograde nail and locking plate. We suggest that the eligibility criteria of such a trial should be broad so as to include as representative a sample of participants as possible. Ideally, the trial would include a separate subgroup of people who sustain fractures about a knee arthroplasty. The trial design needs to allow for the technical difficulties of fixing some types of fracture, for example, severely comminuted AO/ASIF C3 fractures or those about a knee arthroplasty where the condylar elements separation precludes nail introduction. Fully pragmatic eligibility criteria where the details of this decision are left with the treating surgeon may be able to overcome these difficulties whilst still reporting outcomes for the full spectrum of this injury. We strongly recommend that a future trial reports primarily on validated disease/region‐specific patient‐reported functional outcome measures and patient‐reported quality‐of‐life measures, such as the EuroQoL 5 Dimensions. Furthermore, measures of cost‐effectiveness are key to enabling widespread uptake of a clinically effective technology. At minimum, follow‐up should be reported at one and two years. All trials should be reported in full using the CONSORT guidelines.
Acknowledgements
We thank Tim Chesser, Helen Handoll, John Keating and Mario Lenza for helpful editorial comments about drafts of the review. We also thank Joanne Elliott, Lindsey Elstub and Laura MacDonald for their editorial support. We are grateful to Helen Handoll and Haris Vasiliadis for their helpful editorial review of the protocol.
This project was supported by the National Institute for Health Research (NIHR) via Cochrane Infrastructure funding to the Cochrane Bone, Joint and Muscle Trauma Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley Online Library)
#1 MeSH descriptor: [Femur] this term only (585) #2 MeSH descriptor: [Fractures, Bone] this term only (1196) #3 MeSH descriptor: [Fracture Fixation] explode all trees (1248) #4 MeSH descriptor: [Fracture Healing] this term only (402) #5 #2 or #3 or #4 (2383) #6 #1 and #5 (36) #7 MeSH descriptor: [Femoral Fractures] this term only (210) #8 (femur* or femoral*) near/3 fractur*:ti,ab,kw (Word variations have been searched) (1281) #9 #6 or #7 or #8 (1293) #10 distal* or condyl* or supracondyl* or epicondyl* or transcondyl* or intercondyl* or bicondyl* or transchondral* or periprosth*:ti,ab,kw (Word variations have been searched) (6786) #11 #9 and #10 (92) [Trials]
MEDLINE (Ovid)
1 Femur/ (31151) 2 Fractures, Bone/ (48036) 3 exp Fracture Fixation/ (47561) 4 Fracture Healing/ (9359) 5 2 or 3 or 4 (89128) 6 1 and 5 (2108) 7 Femoral Fractures/ (13097) 8 ((femur* or femoral*) adj3 fractur*).tw. (15639) 9 6 or 7 or 8 (23661) 10 (distal* or condyl* or supracondyl* or epicondyl* or transcondyl* or intercondyl* or bicondyl* or transchondral* or periprosth*).tw. (209463) 11 9 and 10 (3512) 12 Randomized controlled trial.pt. (387879) 13 Controlled clinical trial.pt. (89783) 14 randomized.ab. (307772) 15 placebo.ab. (159394) 16 Drug therapy.fs. (1741471) 17 randomly.ab. (222071) 18 trial.ab. (320544) 19 groups.ab. (1401611) 20 or/12‐19 (3439307) 21 exp Animals/ not Humans/ (4007028) 22 20 not 21 (2953854) 23 11 and 22 (356)
EMBASE (Ovid)
1 Femur Condyle/ or Femur/ (37307) 2 exp Fracture/ (205414) 3 exp Fracture Fixation/ (66502) 4 2 or 3 (224607) 5 1 and 4 (6189) 6 Femur Fracture/ (15352) 7 ((femur* or femoral*) adj3 fractur*).tw. (18604) 8 5 or 6 or 7 (30324) 9 (distal* or condyl* or supracondyl* or epicondyl* or transcondyl* or intercondyl* or bicondyl* or transchondral* or periprosth*).tw. (249619) 10 8 and 9 (4704) 11 exp Randomized Controlled Trial/ or exp Single Blind Procedure/ or exp Double Blind Procedure/ or Crossover Procedure/ (398891) 12 (random* or RCT or placebo or allocat* or crossover* or 'cross over' or trial or (doubl* adj1 blind*) or (singl* adj1 blind*)).ti,ab. (1302622) 13 11 or 12 (1376462) 14 (exp Animal/ or Animal.hw. or Nonhuman/) not (exp Human/ or Human Cell/ or (human or humans).ti.) (5461907) 15 13 not 14 (1209928) 16 10 and 15 (179)
Bone & Joint Journal Orthopaedic Proceedings
www.boneandjoint.org.uk/search/advanced
Advanced search
Title: femur femoral (words – any) Abstract or title: fracture* Full text or abstract or title: random* Limit from 2006 to present Narrow search by Orthopaedic Proceedings
Total = 64
World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal
apps.who.int/trialsearch
Advanced search
Search in Title field using: fem* AND distal AND fracture*
Total = 11
Data and analyses
Comparison 1. Surgical versus non‐surgical management.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Death | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Re‐operation or repeat procedure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Implant or traction loosening | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Superficial or pin‐tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.5 Deep vein thrombosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.6 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.7 Pneumonia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.8 Pressure sore | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Failure of union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Delayed union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Malunion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Retrograde intramedullary nail (RIMN) versus single fixed‐angle device.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse events | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Re‐operation | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [0.62, 5.57] |
| 1.2 Death | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.05, 4.38] |
| 1.3 Infection | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.14, 2.54] |
| 1.4 Pneumonia | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.05, 4.38] |
| 1.5 Urinary tract infection | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.46 [0.37, 112.54] |
| 1.6 Acute renal failure | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.77 [0.12, 61.65] |
| 1.7 Pressure sores | 1 | 23 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.77 [0.12, 61.65] |
| 1.8 Haematoma requiring aspiration | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.25] |
| 1.9 Implant failure | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.05, 12.85] |
| 1.10 Nail protrusion | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.89 [0.32, 109.91] |
| 2 36‐item Short Form (SF‐36; higher scores = better quality of life) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Physical component (0 to 100) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Mental component (0 to 100) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Failure of union | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Non‐union | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.33, 3.71] |
| 3.2 Malunion | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.84 [0.28, 11.97] |
| 4 Length of hospital stay (days) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | ‐2.80 [‐3.40, ‐2.20] |
2.4. Analysis.
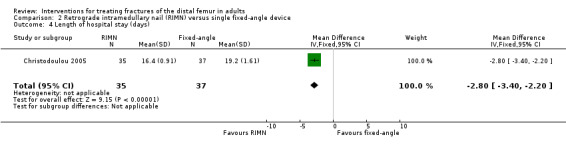
Comparison 2 Retrograde intramedullary nail (RIMN) versus single fixed‐angle device, Outcome 4 Length of hospital stay (days).
Comparison 3. Retrograde intramedullary nail (RIMN) versus non‐locking (buttress) plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Delayed union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Locking plate versus single fixed‐angle device.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Re‐operation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Early loss of reduction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.4 Knee arthrofibrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Retrograde intramedullary nail (RIMN) versus locking plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Patient‐reported functional outcomes | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 Short Musculoskeletal Function Assessment Dysfunction Index | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐5.90 [‐15.13, 3.33] |
| 1.2 Short Musculoskeletal Function Assessment Bother Index | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐8.2 [‐19.63, 3.23] |
| 2 Adverse events | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Re‐operation for removal of implant | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Quality of life | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 EQ‐5D (0 to 1: higher scores = better quality of life) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Failure of union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Malunion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Butt 1996b.
| Methods | Quasi‐randomised controlled trial: allocation was according to the treatment preference of the consultant on‐call at time of admission. 4 consultants were involved in the study, 2 opted for surgical treatment and 2 opted for non‐surgical treatment | |
| Participants | Setting: Russell's Hall Hospital, Dudley, UK Size: 42 participants; 20 in the surgical group, 22 in the non‐surgical group Recruitment period: January 1988 to March 1991 Baseline characteristics: surgical group: 20 participants, mean age 77.6 years. Non‐surgical group: 22 participants, mean age 80.5 years. Sex and fracture type were not reported Inclusion criteria: > 60 years with displaced fractures of the distal femur Exclusion criteria: people who were physiologically unfit for surgery |
|
| Interventions | All participants received low‐dose warfarin as thromboprophylaxis. Participants were then allocated to either:
|
|
| Outcomes | Schedule: not formally reported but until "union had been achieved" Outcomes: Schatzker and Lambert criteria (full extension, loss of flexion, valgus/varus/rotational deformity, pain, joint congruency), length of hospital stay, deep vein thrombosis, urinary tract infection, pneumonia, wound and pin tract infection, pressure sores, delayed union, malunion, loosening of implant or traction pin, death |
|
| Notes | Attempt at personal communication unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quotes: "randomised controlled trial"; "prospective study"; "Each of the four consultants remained on call for a week at a time; two opted for operative treatment and the others treated all patients by traction" Comment: quasi‐randomised study |
| Allocation concealment (selection bias) | High risk | Predictable allocation ‐ allocation based on treatment preference of on‐call consultant |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | This study compared surgical vs. non‐surgical treatment and so it was not possible to blind either participants or personnel |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention was made of blinding of outcome assessment. Additionally, outcome assessment was poorly reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 20 participants were allocated to surgical treatment and 22 to non‐surgical treatment. 1 participant crossed over from the surgical to non‐surgical group and 2 participants were excluded after allocation from the non‐surgical group. In the final per‐protocol analysis, 17 participants were analysed in the surgical group and 19 in the non‐surgical group. Overall attrition was 6/44, but the cross‐over gives rise to concern |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available. Timing of outcome assessment not given |
| Imbalance in baseline characteristics (selection bias) | Unclear risk | Only age was reported and, therefore, it was not possible to judge this item |
| Care provider expertise (performance bias) | Unclear risk | Each intervention was carried out under the care of a consultant surgeon: 2 consultants performed the operative treatment and 2 consultants supervised the non‐operative treatment. However, details of providers of the specific intervention are not specified |
Christodoulou 2005.
| Methods | Quasi‐randomised controlled trial: allocation alternated between interventions after stratification by fracture type | |
| Participants | Setting: Hippokratio General Hospital, Thessaloniki, Greece Size: 80 participants; 35 in the nail group and 37 in the plate group (allocation not reported in 8 participants, 5 of whom died and 3 who were lost to follow‐up) Recruitment period: January 1994 to June 1999 (2000 in abstract) Baseline characteristics: 25 men, 47 women; median age 73.2 years (range 60‐88). All fractures were closed without substantial soft tissue damage. Fracture types in the nail group were AO/ASIF A1 34%, A2 40%, A3 14%, C1 9%, C2 3%; and the plate group were A1 35%, A2 35%, A3 16%, C1 8%, C2 6%. Age, sex and other variables not reported Inclusion criteria: supracondylar fracture of the femur Exclusion criteria: not reported |
|
| Interventions | Participants were allocated to either:
A tourniquet and wound drainage was used for all participants. Prophylactic perioperative antibiotics and postoperative anticoagulants were used in all participants. Continuous passive motion was started on the 2nd or 3rd postoperative day and mobilisation with partial weight‐bearing on 4th or 5th day |
|
| Outcomes | Schedule: 6, 12, 24 and 52 weeks and annually thereafter. Mean follow‐up was 28 months (18‐42 months) Outcomes: Schatzker and Lambert criteria (full extension, loss of flexion, valgus/varus/rotational deformity, pain, and joint congruency), length of hospital stay, operation time, blood loss, radiological union, clinical union, complications, death |
|
| Notes | Attempt at personal communication was unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "allocation alternated between each intervention after stratification by AO fracture classification" Comment: quasi‐randomised |
| Allocation concealment (selection bias) | High risk | The next intervention for each fracture type was known |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The nature of the interventions means that the operating surgeons were not blinded. There were no details relating to participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention was made of blinding of outcome assessment. Additionally, outcome assessment was poorly reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 10% participants were lost to follow‐up: 5 died and 3 changed address. The allocation of these participants was not reported and they were not included in the final analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available |
| Imbalance in baseline characteristics (selection bias) | Low risk | Quote: "there were no differences concerning the pre‐injury condition of the patients in both groups" Comment: in addition reported baseline fracture classifications were similar as would be expected due to stratification prior to allocation |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions not stated |
Dar 2009.
| Methods | Quasi‐randomised controlled trial: allocation alternated between interventions | |
| Participants | Setting: Government Medical College Srinagar, Kashmir, India Size: 73 participants, 37 in the nail group and 31 in the plate group (5 participants were lost to follow‐up) Recruitment: period: September 2002 to December 2004 Baseline characteristics: 41 mem, 27 women; mean age 48 years (range 21‐75). Fracture types in the nail group were AO/ASIF A1 6, A2 11, A3 16, C1 2, C2 2; and the plate group were A1 4, A2 9, A3 12, C1 3, C2 3 Inclusion criteria: not reported Exclusion criteria: not reported |
|
| Interventions | Participants were allocated to either:
Primary bone grafting was not used in any participants. Active‐ and passive‐assisted exercises of the knee joint were started on the second day postoperatively and participants were mobilised on the third postoperative day with the help of crutches. Full weight‐bearing was permitted only after the clinical and radiological union of the fracture |
|
| Outcomes | Schedule: weekly for 3 months, monthly for 12 months, and then every 3 months for a mean 30 months (range 24 to 36) Outcomes: operation time, blood loss, time to union, union risk, range of motion, deep vein thrombosis, shortening and malalignment, postoperative infection, implant failure, hardware prominence, non‐union, delayed union and stiffness |
|
| Notes | Attempt at personal communication was unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "the patients were allocated to two groups randomly one after the other" Comment: we have interpreted this as meaning that allocation was alternated. Hence, it was quasi‐randomised |
| Allocation concealment (selection bias) | High risk | The allocation was predictable as it alternated between interventions |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The nature of the interventions means that the operating surgeons were not blinded. There were no details relating to participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention was made of blinding of outcome assessment. Additionally, the method of outcome assessment was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Only 5 of 73 participants were lost to follow‐up although the allocation of these participants was not reported. (If randomised by alternation, then is it possible that all 5 participants were in the dynamic condylar screw group.) Thus, placing this at unclear risk of bias |
| Selective reporting (reporting bias) | Unclear risk | No protocol was available |
| Imbalance in baseline characteristics (selection bias) | Low risk | Baseline characteristics were appropriately reported and similar |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions were not stated |
DeCoster 1995.
| Methods | Quasi‐randomised controlled trial: allocation alternated between interventions | |
| Participants | Setting: University of New Mexico, Albuquerque, USA Size: 18 participants Recruitment period: not reported. Baseline characteristics: mean age 35 years (range 19‐45). Sex not reported. Fractures included were AO/ASIF type A3 (5 fractures), C1 (1 fracture), C2 (7 fractures), C3 (5 fractures) Inclusion criteria: severe open, Gustilo grade 3A or 3B, distal femur fractures. All injuries caused by high‐energy trauma Exclusion criteria: not reported |
|
| Interventions | All participants were initially treated with debridement and irrigation of the wound and fracture. Articular fragments were reduced and held with lag screws. The articular component of the fracture was then reduced and fixed to the diaphysis of the femur using either:
Range of motion exercises were commenced immediately postoperatively and weight‐bearing was allowed after the appearance of callus on plain radiographs |
|
| Outcomes | Schedule: not specifically reported but the mean participant follow‐up was variably reported as 28 months (range 18‐46) and 26 months (range 17 to 50) in the abstract Outcomes: operative time, blood loss, time to union, functional outcome (rating scale based on clinical and radiological measures) and complications |
|
| Notes | Only an abstract reporting this study was available. Attempt at personal communication was unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "were alternately treated with either retrograde nail or plate" Comment: quasi‐randomised |
| Allocation concealment (selection bias) | High risk | The allocation was predictable as it alternated between interventions |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The nature of the interventions means that the operating surgeons were not blinded. There were no details relating to participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention was made of blinding of outcome assessment. Additionally, the methods of outcome assessment was not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers lost to follow‐up were not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Imbalance in baseline characteristics (selection bias) | Unclear risk | Baseline characteristics between groups were not reported |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions were not stated |
Hartin 2006.
| Methods | Randomised controlled trial | |
| Participants | Settings: 2 regional trauma centres in New South Wales, Australia Size: 22 participants with 23 supracondylar fractures of the femur, 12 were allocated to the nail group and 11 to the plate group Recruitment period: August 2001 to October 2003 Baseline characteristics: 7 men, 16 women; mean age 68 years Inclusion criteria: all AO/ASIF type 33‐A and 33‐C type fractures Exclusion criteria: AO/ASIF type 33A1.1 (avulsion fractures). Skeletally immature participants. Those with concurrent ipsilateral proximal or mid‐shaft fractures of the femur |
|
| Interventions | Surgery was performed in a manner consistent with the AO principles is all cases. Participants were allocated to either:
Postoperatively, all participants reviewed intravenous antibiotics for 36 hours. Active range of motion exercises were permitted immediately and participants were not permitted to weight‐bear for 12 weeks or until evidence of callus formation was seen on plain radiographs |
|
| Outcomes | Schedule: not specifically reported but a minimum of 12 months (mean follow‐up 20 months, range 12‐36 months) Outcomes: operation time, blood transfusion requirement, length of hospital stay, wound infection, complications, death, union, malalignment and shortening, infection, knee flexion and extension loss, 36‐item Short Form and re‐operation |
|
| Notes | 3 participants in the blade plate group had their procedure augmented; 1 received a dynamic condylar screw and 2 received additional buttress plates or interfragmentary screws Attempt at personal communication was unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization was carried out by a remote source, contactable by telephone, using odd and even numbers from a random number table in blocks of 10" Comment: appropriate method of sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "randomization was carried out by a remote source, contactable by telephone, using odd and even numbers from a random number table in blocks of 10" Comment: distant randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The nature of the interventions means that the operating surgeons were not blinded. There were no details relating to participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "clinical assessment was made at follow up by the relevant operating surgeon" Comment: thus, there was no blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 4 of 22 participants were not available for complete follow‐up: 3 died and 1 was lost to follow‐up. Only data from 16 participants were available for the quality of life assessment. 1 person had a bilateral fracture; the group was not identified |
| Selective reporting (reporting bias) | Unclear risk | No protocol or trial registration document was available |
| Imbalance in baseline characteristics (selection bias) | Low risk | Baseline characteristics were appropriately reported and similar |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions were not stated |
Leighton 2011.
| Methods | Randomised controlled trial | |
| Participants | Settings: 6 academic centres, Canada Size: 53 participants, 28 allocated to Less Invasive Stablization System (locking plate) and 25 to dynamic condylar screw fixation Recruitment period: 5 years; start date was March 2003 at trial registration Baseline characteristics: 18 men, 35 women Inclusion criteria: fracture of the distal femur. Aged ≥ 16 years; injury occurred in last 14 days Exclusion criteria: C3 fractures (complete articular fractures) (criterion did not appear at trial registration) |
|
| Interventions | Participants were allocated to either:
|
|
| Outcomes | Schedule: not reported Outcomes: non‐union, reoperation, complications |
|
| Notes | Only an abstract reporting this study was available. Attempt at personal communication was unsuccessful Trial registration document stated the "estimated enrollment" was 150 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "thirty five females and 18 males were included in the study and appropriately randomised" Comment: method of randomisation was not reported |
| Allocation concealment (selection bias) | Unclear risk | Method of randomisation and allocation concealment were not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "masking: open label" (trial registration) Comment: the nature of the interventions means that the operating surgeons were not blinded. This also confirms that there was also no participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "masking: open label" (trial registration) This confirms that there was no blinding of outcome assessors Additionally, outcome assessment is poorly reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers lost to follow‐up were not reported |
| Selective reporting (reporting bias) | High risk | No protocol was available. However, the trial registration document referred to the measurement of participant function: "LEM [lLower Extremity Measure], SMFA [Short Musculoskeletal Function Assessment] and SF‐36 [36‐item Short Form] questionnaires"; these were not reported in the abstract |
| Imbalance in baseline characteristics (selection bias) | Unclear risk | Baseline characteristics split by treatment group were not reported |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions were not stated |
Tornetta 2013.
| Methods | Randomised controlled trial | |
| Participants | Setting: multicentre study (22 listed in trial registration document) in USA Size: 156 participants, 80 allocated to locking plate and 76 to intramedullary nail group Recruitment period: February 2007 to (estimated) December 2012, expected date of completion December 2013) Baseline characteristics: mean age 51 years (range 16‐90), 71 men, 55 women (of the 126 completing follow‐up), mean Injury Severity Score 12.6 (range 9‐43), 34% fractures were open Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Participants were allocated to either:
|
|
| Outcomes | Schedule: 3, 6 and 12 months; 12‐month follow‐up reported so far; planned to be up to 24 months Outcomes: patient‐reported functional and quality of life scores (Short‐Form 12 questions version 2 (SF‐12v2), EuroQol‐5D (EQ‐5D), Short Musculoskeletal Function Assessment (SMFA), Knee Society Score), clinical assessment, re‐operation, non‐union, malunion, infection, compartment syndrome, knee range of motion |
|
| Notes | Communication with authors was unsuccessful. This is likely to be an interim report of available 1‐year data prior to study completion, which is estimated to be December 2015 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization scheme was with permutated blocks for open and closed fractures using a HIPAA [Health Insurance Portability and Accountability Act]‐compliant computer‐based system" Comment: appropriate sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "masking: open label" (trial registration) Comment: the nature of the interventions means that the operating surgeons were not blinded. This also confirms that there was also no participant blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "masking: open label" (trial registration) This confirms that there was no blinding of outcome assessors Additionally, outcome assessment is poorly reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "156 patients were randomized ... 126 patients were followed" Comment: 81% follow‐up but allocations of those participants who were lost were not reported |
| Selective reporting (reporting bias) | Unclear risk | The majority of outcomes described in the trial registry entry have been reported in the conference abstract. However, no data were reported beyond the 1‐year stage despite follow‐up planned out to 2 years |
| Imbalance in baseline characteristics (selection bias) | Unclear risk | Quote: "There were no differences in demographic information or injury pattern" Comment: however, there are no supporting data |
| Care provider expertise (performance bias) | Unclear risk | Providers of interventions were not stated |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Firoozabadi 2012 | Not a randomised or quasi‐randomised controlled trial |
| Gao 2013 | Not a randomised or quasi‐randomised controlled trial |
| Han 2011 | Not a randomised or quasi‐randomised controlled trial |
| Horneff 2013 | Not a randomised or quasi‐randomised controlled trial |
| Markmiller 2004 | Not a randomised or quasi‐randomised controlled trial |
| Petsatodis 2010 | Not a randomised or quasi‐randomised controlled trial |
| Thomas 1981 | Not a randomised or quasi‐randomised controlled trial |
| Tornetta 2000 | Participants were "all patients with femoral shaft fractures", excluding fractures within 3 cm from knee joint. It was not possible to extract the data specific to distal femoral fractures |
| Vallier 2012 | Not a randomised or quasi‐randomised controlled trial |
Characteristics of studies awaiting assessment [ordered by study ID]
Hanschen 2014.
| Methods | Interventional, block‐randomised, multicentre controlled trial |
| Participants | 27 participants recruited between 2008 and 2011 Inclusion criteria:
|
| Interventions | All surgeons were experienced specialists. Depending on the fracture classification, a standardised anterolateral or additional medial approach was used for the reduction of intra‐articular fragments. After temporary fixation of articular fragments the condyle block was adjusted to the axis of the femur and the whole leg. The locking plate was adjusted and temporarily fixated using K‐wires Participants were allocated to either:
All participants received perioperative antibiotics. Postoperatively, physiotherapy was commenced and active range of motion exercises were permitted immediately. Non‐weight‐bearing was recommended for 6‐8 weeks, followed by partial weight‐bearing until callus formation was apparent in radiographic follow‐up examinations |
| Outcomes | Primary outcome:
Secondary outcomes:
|
| Notes | Study fully reported but awaiting analysis |
Characteristics of ongoing studies [ordered by study ID]
NCT00644397.
| Trial name or title | Plate Fixation of Distal Femur Fractures: a Protocol for a Study of Two Plate Options |
| Methods | Randomised, prospective, multicentre study |
| Participants | 49 participants will be required in each group (based on previously reported malunion rates) Inclusion criteria:
Exclusion criteria:
|
| Interventions | 95º angled blade plate 4.5 mm condylar locking plate |
| Outcomes | Infection, non‐union, malunion, functional outcomes |
| Starting date | May 2006 |
| Contact information | Heather A Vallier, M.D., MetroHealth Medical Center, hvallier@metrohealth.org |
| Notes |
NCT01553630.
| Trial name or title | Reamed Locked Plating ‐ Metaphyseal Fractures of the Distal Femur and Tibia |
| Methods | Interventional, randomised study |
| Participants | Both men and women Inclusion criteria:
Exclusion criteria:
|
| Interventions | ORIF with reamed irrigator aspirator bone graft ORIF without reamed irrigator aspirator bone graft |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | May 2010 |
| Contact information | Barbara Steverson bsteverson@floridaortho.com |
| Notes |
NCT01693367.
| Trial name or title | A Multi‐Center Randomized Controlled Pilot Study of Dynamic Locking Screws 5.0 vs. Standard Locking Screws in Fracture of Distal Femur Treated With Locked Plate Fixation |
| Methods | Interventional, randomised, efficacy study. Single blinded (participant) |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions | DLS 5.0 (dynamic locking screws) SLS (standard locking screw) |
| Outcomes |
|
| Starting date | September 2102 |
| Contact information | Michael J Gardner, MD, Washington University School of Medicine |
| Notes |
NCT01766648.
| Trial name or title | Multicentre, Randomized Trial of Far Cortical Locking Versus Standard Constructs for Acute, Displaced Fractures of the Distal Femur Treated With Locked Plate Fixation |
| Methods | Interventional, randomised, efficacy study. Participants will be assigned to a single group |
| Participants | Estimated enrolment: 130 participants. Aged ≥ 18 years. Both men and women Inclusion criteria:
Exclusion criteria:
|
| Interventions | Far cortical locking screw fixation (experimental) Standard locking screw fixation (active‐comparator) |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | December 2013 |
| Contact information | Raman Johal, raman.johal@vch.ca |
| Notes |
NCT01973712.
| Trial name or title | Treatment of Periprosthetic Distal Femur Fractures: a Randomized Controlled Trial of Locking Plate Osteosynthesis Versus Retrograde Nailing |
| Methods | Allocation: randomised Intervention model: parallel assignment Masking: single blind (outcomes assessor) |
| Participants | Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Locked compression plating. A direct lateral approach to the distal femur will be employed utilising minimally invasive and indirect reduction techniques. After fracture reduction is achieved with the use of intra‐operative fluoroscopy, a locking plate will be provisionally implanted. Following confirmation of placement, definitive fixation will follow with multiple locking screws in the distal fragment and bicortical screw fixation proximally. A standard layered closure will follow Retrograde intramedullary nailing. The previous mid‐line knee incision will be employed to access to the knee joint, allowing exposure of the femoral start point via the open box in the femoral component. Following reaming of the canal, an appropriately sized retrograde nail will be inserted. Intra‐operative fluoroscopy will be used to confirm reduction. Both proximal and distal locking screws will be used to transfix the nail. A standard layered closure will follow |
| Outcomes | Primary outcomes:
Secondary outcomes:
|
| Starting date | May 2014 |
| Contact information | Contact: Milena Vicente vicentem@smh.ca Contact: Melanie MacNevin macnevinm@smh.ca St. Michael's Hospital, Toronto |
| Notes | Estimated enrolment 94 participants |
Differences between protocol and review
Types of interventions
We had initially anticipated that older designs of fixed‐angle implants, such as condylar plate or screw implants (DCS), might be readily grouped with more modern fixed‐angle plates, where the screw 'locks' to the plate. However, the included studies included comparisons between these interventions that prevented such a grouping. Therefore, we grouped extramedullary plating systems into non‐fixed‐angle plates, single component fixed‐angle plates (e.g. DCS) and locking plates.
Assessment of risk of bias in included studies
Contrary to our initial intentions, we did not separate our assessments of risk of detection bias for subjective and objective outcome measures as we considered that rating was unlikely to be affected by the type of outcome for these sorts of trials.
Contributions of authors
All authors contributed to the development of the review and commented on and approved the final version. The guarantor of this review is Xavier Griffin.
Sources of support
Internal sources
-
University of Warwick, UK.
Salary provided to one or more of the authors.
External sources
No sources of support supplied
Declarations of interest
XLG: none known. NP: none known. MMZ: none known. JMcA: none known.
New
References
References to studies included in this review
Butt 1996b {published data only (unpublished sought but not used)}
- Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non‐operative treatment. Journal Bone and Joint Surgery. British Volume 1996;78(1):110‐4. [PubMed] [Google Scholar]
- Witt JD. Displaced fractures of the distal femur in elderly patients [Letter, comment]. Journal of Bone and Joint Surgery. British Volume 1996;78:998. [PubMed] [Google Scholar]
Christodoulou 2005 {published data only (unpublished sought but not used)}
- Christodoulou A, Terzidis I, Ploumis A, Metsovitis S, Koukoulidis A, Toptsis C. Supracondylar femoral fractures in elderly patients treated with the dynamic condylar screw and the retrograde intramedullary nail: a comparative study of the two methods. Archives of Orthopaedic Trauma Surgery 2005;125(2):73‐9. [DOI] [PubMed] [Google Scholar]
Dar 2009 {published data only (unpublished sought but not used)}
- Dar GN, Tak SR, Kangoo KA, Halwai MA. Bridge plate osteosynthesis using dynamic condylar screw (DCS) or retrograde intramedullary supracondylar nail (RIMSN) in the treatment of distal femoral fractures: comparison of two methods in a prospective randomized study. Turkish Journal of Trauma & Emergency Surgery 2009;15(2):148‐53. [PubMed] [Google Scholar]
DeCoster 1995 {published data only (unpublished sought but not used)}
- DeCoster TA, Behzadi K, Naraghi F, Moneim MS, Jabczenski F. Clinical comparison of retrograde nail versus plate fixation for severe open distal femur fractures [abstract]. Orthopaedic Transactions 1995;19(2):343. [Google Scholar]
Hartin 2006 {published data only (unpublished sought but not used)}
- Hartin NL, Harris I, Hazratwala K. Retrograde nailing versus fixed‐angle blade plating for supracondylar femoral fractures: a randomized controlled trial. ANZ Journal of Surgery 2006;76(5):290‐4. [DOI] [PubMed] [Google Scholar]
Leighton 2011 {published data only (unpublished sought but not used)}
- Hawsawi H, Leighton R, Presis A, Barron L, Trask K, Stephen D, et al. A prospective randomised multicentre trial comparing the Less Invasive Stabilisation System (LISS) to the mini invasive dynamic condylar system (DCS) for distal femur fractures. Journal of Bone Joint Surgery. British Volume 2012;94(Supp XXI):66. [Google Scholar]
- Leighton R, Dunbar M, Petrie D, Deluzio K, O'Brien P, Buckley R, et al. A prospective randomised multicentre trial comparing the Less Invasive Stabilisation System (LISS) to the mini invasive dynamic condylar system (DCS) for distal femur fractures. Journal of Bone Joint Surgery. British Volume 2011;93(Supp IV):305. [Google Scholar]
- Leighton RK. Prospective randomized clinical study to evaluate the effects of Less Invasive Stabilization System (LISS) plating techniques in distal femoral fractures. clinicaltrials.gov/ct2/show/NCT00552331 (accessed 9 September 2014).
Tornetta 2013 {published data only (unpublished sought but not used)}
- Tornetta III P. A multicenter randomized trial comparing IM nails and plate fixation in distal femur fractures. clinicaltrials.gov/show/NCT00429663 (accessed 1 June 2015).
- Tornetta III P, Egol KA, Jones CB, Ertl JP, Mullis B, Perez E, et al. Locked plating versus retrograde nailing for distal femur fractures: a multicenter randomized trial. Orthopaedic Trauma Association (conference proceedings); 2013 Oct 9‐12; Phoenix, Arizona. 2013.
References to studies excluded from this review
Firoozabadi 2012 {published data only}
- Firoozabadi R, McDonald E, Nguyen TQ, Buckley JM, Kandemir U. Does plugging unused combination screw holes improve the fatigue life of fixation with locking plates in comminuted supracondylar fractures of the femur?. Journal of Bone & Joint Surgery. British Volume 2012;94(2):241‐8. [DOI] [PubMed] [Google Scholar]
Gao 2013 {published data only}
- Gao K, Gao W, Huang J, Li H, Li F, Tao J, et al. Retrograde nailing versus locked plating of extra‐articular distal femoral fractures: comparison of 36 cases. Medical Principles & Practice 2013;22(2):161‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Han 2011 {published data only}
- Han HS, Kim DH, Kang SB. The use of a ti‐ni shape memory alloy ring bone fixator during the retrograde nailing of supracondylar femoral fractures. Knee Surgery Related Research 2011;23(4):231‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horneff 2013 {published data only}
- Horneff JG 3rd, Scolaro JA, Jafari SM, Mirza A, Parvizi J, Mehta S. Intramedullary nailing versus locked plate for treating supracondylar periprosthetic femur fractures. Orthopaedics 2013;36(5):561‐6. [DOI] [PubMed] [Google Scholar]
Markmiller 2004 {published data only}
- Markmiller M, Konrad G, Sudkamp N. Femur‐LISS and distal femoral nail for fixation of distal femoral fractures: are there differences in outcome and complications?. Clinical Orthopaedics Related Research 2004;426:252‐7. [DOI] [PubMed] [Google Scholar]
Petsatodis 2010 {published data only}
- Petsatodis G, Chatzisymeon A, Antonarakos P, Givissis P, Papadopoulos P, Christodoulou A. Condylar buttress plate versus fixed‐angle condylar blade plate versus dynamic condylar screw for supracondylar intra‐articular distal femoral fractures. Journal of Orthopaedic Surgery (Hong Kong) 2010;18:35‐8. [DOI] [PubMed] [Google Scholar]
Thomas 1981 {published data only}
- Thomas TL, Meggitt BF. A comparative study of methods for treating fractures of the distal half of the femur. Journal of Bone and Joint Surgery. British Volume 1981;63:3‐6. [DOI] [PubMed] [Google Scholar]
Tornetta 2000 {published data only}
- Tornetta P III, Tiburzi D. Reamed versus nonreamed antegrade femoral nailing. Journal Orthopaedic Trauma 2000;14(1):15‐9. [DOI] [PubMed] [Google Scholar]
Vallier 2012 {published data only}
- Vallier HA, Immler W. Comparison of the 95‐degree angled blade plate and the locking condylar plate for the treatment of distal femoral fractures. Journal of Orthopaedic Trauma 2012;26(6):327‐32. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Hanschen 2014 {published data only}
- Hanschen M, Aschenbrenner I, Fehske K, Kirchhoff S, Keil L, Holzapfel B, et al. Mono‐ versus polyaxial locking plates in distal femur fractures: a prospective randomized multicentre clinical trial. International Orthopaedics 2014;38(4):857‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
NCT00644397 {published data only}
- Vallier HA, Boyd AJ. Plate fixation of distal femur fractures: a protocol for a study of two plate options. clinicaltrials.gov/show/NCT00644397 (accessed 9 September 2014).
NCT01553630 {published data only}
- Watson D. Reamed locked plating ‐ metaphyseal fractures of the distal femur and tibia. clinicaltrials.gov/show/NCT01553630 (accessed 9 September 2014).
NCT01693367 {published data only}
- Gardner MJ, Nork SE. Dynamic locking screws 5.0 vs. standard locking screws in fracture of distal femur treated with locked plate fixation. clinicaltrials.gov/show/NCT01693367 (accessed 9 September 2014).
NCT01766648 {published data only}
- Johal R. Far cortical locking versus standard constructs for distal femur fractures (FCL). clinicaltrials.gov/show/NCT01766648 (accessed 9 September 2014).
NCT01973712 {published data only}
- Nauth A, Schemitsch E. Periprosthetic distal femur fracture. clinicaltrials.gov/ct2/show/NCT01973712 (accessed 13 February 2015).
Additional references
Arneson 1988
- Arneson TJ, Melton LJ 3rd, Lewallen DG, O'Fallon WM. Epidemiology of diaphyseal and distal femoral fractures in Rochester, Minnesota, 1965‐1984. Clinical Orthopaedics and Related Research 1988;(234):188‐94. [PubMed] [Google Scholar]
Butt 1996a
- Butt MS, Krikler SJ, Ali MS. Displaced fractures of the distal femur in elderly patients. Operative versus non‐operative treatment. Journal of Bone & Joint Surgery. British Volume 1996;78(1):110‐4. [PUBMED: 8898139] [PubMed] [Google Scholar]
Court‐Brown 2006
- Court‐Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37(8):691‐7. [DOI] [PubMed] [Google Scholar]
Crist 2008
- Crist BC, Della Rocca GJ, Murtha YM. Treatment of acute distal femur fractures. Orthopedics 2008;31(7):681‐90. [PUBMED: 18705562] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Foster 2006
- Foster MC, Komarsamy B, Davison JN. Distal femoral fractures: a review of fixation methods. Injury 2006;37(2):97‐108. [PUBMED: 16439229] [DOI] [PubMed] [Google Scholar]
GRADE 2004
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustilo 1976
- Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty‐five open fractures of long bones: retrospective and prospective analyses. Journal of Bone and Joint Surgery. American Volume 1976;58(4):453‐8. [PubMed] [Google Scholar]
Herrera 2008
- Herrera DA, Kregor PJ, Cole PA, Levy BA, Jonsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981‐2006). Acta Orthopaedica 2008;79(1):22‐7. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Higgins 2011b
- Higgins JPT, Altman DG, Sterne JAC. Chapter 8: Assessing risk of bias in included studies Table 8.5a. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Kolmert 1982
- Kolmert L, Wulff K. Epidemiology and treatment of distal femoral fractures in adults. Acta Orthopaedica Scandinavica 1982;53(6):957‐62. [PUBMED: 7180408 ] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Marsh 2007
- Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium ‐ 2007: Orthopaedic Trauma Association classification, database and outcomes committee. Journal of Orthopaedic Trauma 2007;21(Suppl 10):S1‐133. [DOI] [PubMed] [Google Scholar]
Martinet 2000
- Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury 2000;31(Suppl 3):C62‐3. [PUBMED: 11052383] [DOI] [PubMed] [Google Scholar]
Meek 2011
- Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri‐prosthetic fracture after primary and revision total hip and knee replacement. Journal of Bone and Joint Surgery. British Volume 2011;93(1):96‐101. [PUBMED: 21196551] [DOI] [PubMed] [Google Scholar]
Müller 1990
- Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. 1st Edition. Berlin: Springer Berlin Heidelberg, 1990. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rosen 2004
- Rosen AL, Strauss E. Primary total knee arthroplasty for complex distal femur fractures in elderly patients. Clinical Orthopaedics and Related Research 2004;(425):101‐5. [PUBMED: 15292794] [DOI] [PubMed] [Google Scholar]
Schatzker 1979
- Schatzker J, Lambert DC. Supracondylar fractures of the femur. Clinical Orthopaedics 1979;138:77‐83. [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al on behalf of the Cochrane Applicability and Recommendations Methods Group. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Wall 2012
- Wall EJ, May MM. Growth plate fractures of the distal femur. Journal of Paediatric Orthopaedics 2012;32(Suppl 1):S40‐6. [DOI] [PubMed] [Google Scholar]
Zlowodzki 2006
- Zlowodzki M, Bhandari M, Marek DJ, Cole PA, Kregor PJ. Operative treatment of acute distal femur fractures: systematic review of 2 comparative studies and 45 case series (1989 to 2005). Journal of Orthopaedic Trauma 2006;20(5):366‐71. [DOI] [PubMed] [Google Scholar]


