Abstract
Objective
In recognition that engagement in physical activities for persons living with dementia can be challenging in rural and northern communities, the objective of this study was to explore the factors influencing physical activity participation among persons living with dementia in rural/northern communities and to identify the locally-driven mitigation strategies participants used to address barriers to physical activity.
Setting
Interviews and focus groups were conducted in two locations in northern British Columbia, Canada including a rural community (<10 000 persons) and a medium-sized geographically isolated city (<80 000 persons). Both communities are located at substantial distances (>700 km) from larger urban centres.
Participants
Twenty-nine individuals participated including healthcare providers (n=8), community exercise professionals (n=12), persons living with dementia (n=4) and care partners (n=5).
Results
Rural and northern contextual factors including aspects of the built and natural environment were the main drivers of physical activity for persons living with dementia. Limited capacity in the health system to support physical activity due to a lack of referrals, poor communication mechanisms and limited resources for programming created challenges for physical activity participation. At the community level, local champions filled gaps in physical activity programming by leveraging informal networks to organise opportunities. Programme-level factors included a lack of consistency in staff, and challenges defining programme scope given limited population size and the fear of stigma for persons living with dementia.
Conclusions
Environmental context and limited access to specialised programming affect the opportunities for persons living with dementia to engage in physical activities. Rural and northern communities showed resiliency in providing physical activity opportunities yet remained fragile due to human resource challenges. Without reliable resources and sustained support from the health system, local champions remain vulnerable to burnout. Enhancing support for local champions may provide greater stability and support to physical activity promotion in rural and northern communities.
Keywords: Dementia, GERIATRIC MEDICINE, HEALTH SERVICES ADMINISTRATION & MANAGEMENT, Quality in health care, PUBLIC HEALTH, QUALITATIVE RESEARCH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
A study strength includes the engagement of diverse stakeholders (persons living with dementia, care partners, allied health providers experienced in providing community exercise programs and healthcare professionals) contributing varying perspectives.
A strength of employing a qualitative approach was our ability to describe in-depth the challenges participants faced at varying levels of the social–ecological model.
A strength of the study is the inclusion of participants from two separate communities enabling a reflection on different needs and environments.
A limitation of this study is the relatively fewer participants living with dementia or mild cognitive impairment compared with other participant groups.
As this study was conducted prior to the COVID-19 pandemic, the impact of the pandemic restrictions and social distancing protocols on physical activity experiences of persons living with dementia is unknown.
Introduction
Dementia is an umbrella term used to describe progressive declines in cognition which may affect a person’s behaviour and ability to perform activities of daily living. The most common form of dementia is Alzheimer’s disease. More than 55 million persons are currently living with dementia worldwide.1 Due to a rapidly ageing population, it is projected that this number will rise to 78 million persons in 2030 and 139 million persons in 2050.1 In Canada, 6.7% of persons aged over 65 are living with dementia.2 As there is currently no cure for dementia, there is growing urgency to develop and implement strategies to support the well-being of persons living with dementia and their care partners.
There is much diversity and heterogeneity across rural communities in Canada based on sociospatial characteristics (eg, population size, population density, distance from urban centre), social representation, population demographics and resource availability.3 4 Although there is no clear consensus on what constitutes a rural community,5 common definitions are based on a combination of population size, distance from an urban centre and access to services. In Canada, the provincial ‘north’ is a term commonly used to identify the northern and more sparsely populated (eg, rural, remote) areas, which may also experience similarities in arctic/subarctic climates, political marginalisation, economic dependency on natural resource development and larger proportions of Indigenous populations.6 Persons living in rural and northern communities face increased barriers to physical activity (eg, transportation, snow/ice) and have fewer opportunities to engage in physical activity through specialised programming,7 contributing to an increased risk of non-communicable disease and disability compared with their urban counterparts. Characteristics specific to the rural context may directly and/or indirectly influence physical activity opportunities and capabilities among older adults.8 As northern and rural communities have a relatively greater proportion of older adults and a population that is ageing faster than the general population,9 the need to develop strategies to address context-specific barriers is urgent.
Physical activity is one of the best non-pharmacological strategies to support persons living with dementia to remain active and enhance quality of life.10 11 For older adults living with dementia or mild cognitive impairment, which includes declines in memory, attention and cognitive functioning that exceed that typically expected by age or educational level, physical activity can enhance and help maintain physical fitness, balance, mobility, functional ability and cognition.12–15 In addition to physical and cognitive benefits, physical activity has broader impacts including social inclusion and feelings of purpose, which contribute to overall well-being and quality of life.16 17 Barriers that can prevent persons living with dementia from engaging in physical activity include stigma and lack of knowledge associated with dementia.18 Persons living with dementia were found to spend more of their time engaged in sedentary behaviours when compared with age-matched cognitively healthy controls19 and were less likely to meet physical activity guidelines20 when compared with persons with no cognitive impairment.
Despite the well-known benefits of physical activity, there remains a need to develop physical activity interventions for persons living with dementia that address each level of the social–ecological model.21 A social–ecological approach to physical activity considers the interacting factors that influence opportunities at the levels of policy, community, organisational (institutional), interpersonal and individual.22 23 For persons living with dementia, individual issues affecting memory, declines in cognitive abilities, and changes in mobility may impact physical activity behaviours differently across the course of the illness.24–26 The barriers to engagement in physical activity are amplified by the stigma surrounding a diagnosis of dementia (eg, interpersonal relationships) and lack of knowledge by exercise providers on how to accommodate and adapt programming for varying and dynamic needs (eg, lack of knowledge and programming barriers).16 Prior research exploring physical activity barriers and opportunities for persons living with dementia has often focused on individual-level factors, with limited attention to environmental and community-specific factors affecting the inclusion of rural-dwelling persons living with dementia in physical activities.23 26 A focus on environmental and systems-level factors is particularly important for understanding behaviour in rural and northern communities where the context shapes opportunities for active living. Taking a systems approach to physical activity promotion, exercise providers and allied healthcare providers who are aware of the unique needs of persons living dementia can be crucial enablers of physical activity for older adults by fostering positive (or negative) experiences and environments for physical activity.17 27
Care partners are uniquely positioned to raise awareness about factors influencing the behaviours and choices of persons living with dementia. The sharing of this person-specific knowledge with physical activity providers may inform intervention development and allow for tailoring of the programme by healthcare professionals and allied health providers to better meet the individual needs of persons living with dementia.26 27
Therefore, the objectives of this study were to: (1) explore the factors influencing physical activity participation among persons living with dementia or mild cognitive impairment in rural and northern communities in Canada and (2) identify locally-driven solutions to salient barriers to assist in the development of tools and resources for persons living with dementia, their care partners, allied health providers and healthcare professionals in rural and northern communities in Canada.
Methods
Patient and public involvement
This work was guided by a large stakeholder advisory team including persons with dementia, care partners, physical activity providers, researchers and healthcare experts. This advisory team provided direction to the research team which was used to inform design and guide this work.
Study context
This study was nested within a larger national project aimed at developing resources and materials to support Dementia-Inclusive Choices for Exercise project (www.dementiaexercise.com).27 28 We report on the formative work conducted in northern British Columbia, Canada, highlighting the perspectives of those living in rural and northern geographies. Framed by a social–ecological approach to understanding physical activity, opportunities for persons living with dementia are informed by interpersonal, intrapersonal, social and built environmental and policy factors.22 Thus, it is important to co-create knowledge with diverse communities based on population size and geographical location, aligning with basic principles of patient-oriented research.29 Interviews and focus groups were conducted in two locations in northern British Columbia, Canada; a rural community (population less than 10 000 persons) and a medium-sized geographically isolated city (population less than 80 000 persons). Both communities are considered rural based on distance from urban centre and access to health services.30
Participant recruitment
Purposive and snowball sampling strategies were employed to recruit exercise providers, allied health providers, persons living with dementia or mild cognitive impairment and care partners for persons living with dementia. Purposive non-probability sampling, commonly used in qualitative studies, allowed for the invitation of participants who were most representative or informative to participate.31 Recruitment materials were initially shared in community locations (eg, posters placed on notice boards at the Alzheimer Society and in a local memory clinic; notice placed in community newsletter) to recruit persons living with dementia and their family care partners. Local health systems stakeholders assisted in recruitment of healthcare professionals and exercise providers who delivered exercise programmes for older adults and/or persons living with dementia (eg, rehabilitation programmes, geriatric outreach programmes, community exercise programmes).
Seven semistructured focus groups and one interview were conducted with 29 participants, including: healthcare professionals (eg, physiotherapists, rehabilitation assistants, registered nurses; n=8); allied health providers experienced in providing community exercise programmes (n=12); persons living with mild to moderate dementia or cognitive impairment (n=4) and care partners of persons living with dementia or cognitive impairment (n=5). Four focus groups involved both healthcare professionals and allied health providers, one focus group involved both care partners and a person living with dementia, one focus group involved only persons with dementia, and one focus group involved only care partners. The interview was conducted with a person living with dementia unable to participate in a focus group setting. Participant age and gender were not collected to protect participant confidentiality given the relatively small number of healthcare professionals and allied health providers in this region. Focus groups lasted approximately 2 hours for healthcare professionals and allied health providers and approximately 1 hour for care partners and/or persons living with dementia or cognitive impairment. Participants provided informed written consent/assent ahead of the session date and reconfirmed verbal consent/assent prior to the session commencing. All participants living with dementia were deemed to have the capacity to provide consent, which was reconfirmed by their care partners. While there is no set number of participants or focus groups as a rule in qualitative research, 29 participants were considered an acceptable number of participants for this exploratory research as it fits within the commonly accepted sample size ranging from 15 to 30 participants for qualitative research.32 At the conceptual level, concordance was observed in findings across differing participant groups and across both sites, suggesting that saturation was achieved.33
Focus group sessions
Focus group sessions, tailored to the participant type, followed a semistructured guide based on previous iterations used by the research team.28 The focus groups were facilitated by an experienced moderator (SF) with support from a graduate student research assistant (RF) who took notes and managed recording devices. The semistructured approach allowed probing into emerging issues and themes, where appropriate. Focus groups enabled exploration of interactive social contexts and provided insight into participant perspectives and attitudes.34 35 Group processes helped participants identify and clarify their perspectives with each other and encouraged increased depth of description and discussion among participants, providing more detailed responses to prompts.36 Two of the focus group scripts used are available in online supplemental file 1 (for persons with dementia) and online supplemental file 2 (for allied healthcare providers).
bmjopen-2022-060860supp001.pdf (56.8KB, pdf)
bmjopen-2022-060860supp002.pdf (127.2KB, pdf)
Data analysis
An inductive thematic analysis of transcripts was guided by Braun and Clarke’s six steps.37 38 Beginning with familiarisation of the data, a multidisciplinary team of researchers experienced in qualitative analyses (SF (gerontology) and CP (exercise physiology)) along with a research trainee (KW (health sciences)) read and reread the transcripts, writing initial thoughts from the data (step 1). All three researchers (SF, CP and KW) are women who live in northern British Columbia. Each have their own lived experience interacting with and supporting persons living with dementia and care partners as well as experience interacting with community service providers. The engagement of team members from diverse backgrounds enabled robust discussion and consideration of patterns in the data and understanding from various viewpoints (eg, from the perspectives of supporting healthy ageing, to optimising physical activity and exercise opportunities). To capture broad perspectives on the data, researchers independently identified and coded the transcripts (step 2) and developed initial themes by identifying patterns in the data set (step 3). Initial themes were then discussed as a group to develop rich descriptions and definitions using a white board to map connections between ideas (step 4). Final themes were established and defined, with subthemes generated as appropriate within each overall theme (step 5). Data extracts (quotes), identified to best describe each theme/subtheme, are presented with a narrative summary (step 6).
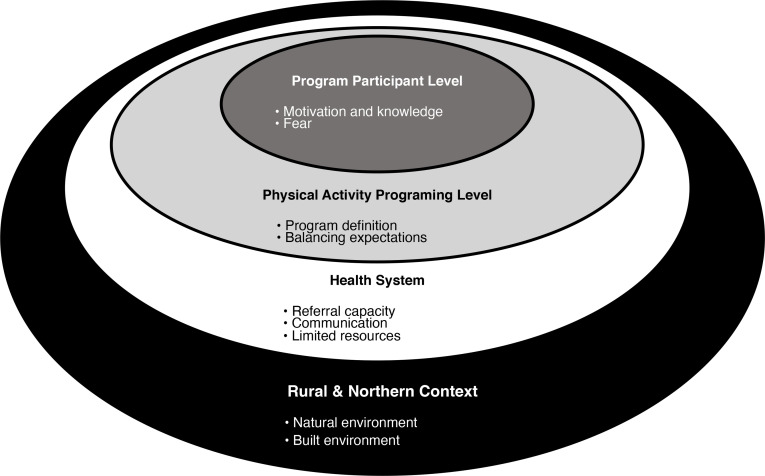
Using the social–ecological model as a guide,22 39 themes were deductively mapped using a white board and post-it notes and plotted according to user, programme, health system and broader community (contextual) levels to describe the factors influencing physical activity for persons living with dementia. Locally driven mitigation strategies and solutions described by participants to overcome barriers to physical activity were identified across each of the four levels. Analysis was conducted using Microsoft Word and Excel software.
Results
Factors influencing participation in physical activity for persons living with dementia were organised into four themes according to the social–ecological model: northern and rural context, health system, physical activity programming and programme participant level (figure 1). Identified challenges and mitigations strategies were also mapped to the social–ecological model (table 1).
Figure 1.
Key findings by theme organised according to the social–ecological model.
Table 1.
Identified challenges and mitigations strategies mapped to the social–ecological model
| Level | Identified challenges | Mitigation strategies |
| Northern and rural context |
|
|
| Health system |
|
|
|
|
|
| Physical activity programme |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Programme participant |
|
|
|
|
|
|
|
Northern and rural context: unique features of the northern and rural context in Canada both promote and limit physical activity
The Canadian northern and rural environmental context underpinned all aspects concerning health and physical activity for persons living with dementia. The local and regional context shaped programme opportunities, availability, accessibility and preferences.
Natural environment
Elements including weather (eg, harsh winter conditions and wildfires), geographic location (eg, isolation from urban centres and from physical activity opportunities), wildlife (eg, presence of bears, cougars and moose) and lack of daylight in the winter months influenced willingness and abilities of persons living with dementia to engage in physical activity. One care partner noted: ‘By 7 o’clock it’s really dark, and I don’t really feel that safe going in the dark by myself … the temperature in the winter might be okay, but it might a sheet of ice’. Participants reported the need to adapt to changes in weather to maintain daily physical activities including outdoor walking.
I have to wear the tall boots. So, I get my boots on, that means they go right up to the knee and so you can stomp into the snow. Sometimes you put cleats on them so you don’t slip. And I always have my poles. It’s very important to have the poles. It’s beautiful, you know (person living with dementia).
Long-time residents of Canadian rural and northern communities described the easy access to natural environments including rivers, lakes and forest trails as a facilitator of outdoor physical activity engagement for all persons including those living with dementia. As one participant explained:
I used to do exercise that was more like go lift weights and workout and now it’s like, no, unless it’s fun. I like dancing. I like walking the dog in the forest or somewhere off-leash where I can just wander around in the trees and the mushrooms. It’s hard to get me to go fast. I don’t go fast, but you can get me to go up a hill (person living with dementia).
Furthermore, one care partner of a person living with dementia emphasised how immersing themselves in the natural environment contributed not only to their ability to be physically active but also related to how they conceptualise and find positive meaning in activity as a way to be outside and seek goals beyond fitness.
I like the freedom of being away from it all in the woods, on the water—that’s really important. In the backyard, no phones. And you just respond as you go and you’re thinking of something you want to do, you do it. That’s freedom. That’s exercise. That’s a good feeling (care partner of person living with dementia).
Built environment
Although a lack of facilities and vast geographic distance to the nearest urban centre were mentioned as barriers, participants described some of the unique built environmental features that facilitated physical activity. Participants valued the accessible infrastructure in their community: ‘We actually have this incredible sidewalk system here … [it’s] designed so that every street has access to this sidewalk system that is maintained by the municipality to get to downtown, to do grocery shopping, and so on’ (person living with dementia). Furthermore, participants shared how city planners in their rural community had considered the needs of an ageing population when designing the sidewalk (eg, cloverleaf and crescent patterns) to purposefully support safe and accessible physical activity for persons with cognitive impairments.
Health system: limitations of the health system lead to development of local solutions
The overarching structure of the healthcare system impacted access to physical activity opportunities through three main facets: the referral process and policies, communication processes and resource availability. Each subsequently impacted physical activity opportunities for programme end-users.
Lack of capacity and mechanisms for referrals
Healthcare professionals and allied health providers struggled with the process of referring persons with dementia to specialised physical activity programmes due to lack of capacity and resources throughout the system (eg, staffing, limited programme offerings) and absence of clear mechanisms in place to facilitate the referral process. When responsibility and accountability for referrals was unclear, it led to inaccuracies and gaps in assessment documentation, which subsequently resulted in delayed or failed referrals. In some cases, when exercise providers received inaccurate and incomplete documentation during the referral process, it resulted in duplication of health assessments and additional workload. One healthcare professional noted:
What’s on the piece of paper doesn’t quite identify what the person’s needs are. So, a lot of extra digging needs to go into that. So, whether the person needs to see a geriatrician which is more sort of the medical component, it’s triaged that way (healthcare professional).
For persons with dementia and their care partners, the lack of a clear referral process or advice from their healthcare provider led to confusion and lack of awareness about where to seek trusted information about safe physical activity opportunities. One participant described their frustration noting:
It’s been an ongoing question, where can we get more information. “Read about it.” Okay, we’ve read about it. Who can we talk to? “Alzheimer’s group” or a contact or “your GP, he can help”. We’ve been through all that and there isn’t any (care partner of person living with dementia).
Difficulty in communication and fragmented access to information leads to lack of knowledge
Challenges with clear and consistent communication were recognised as a barrier across all participant groups. One participant described these communication challenges noting:
Word finding difficulties depending on the type of dementia can be a challenge for the person who’s struggling to communicate, and for other participants as well. Maybe the person with dementia who also has word finding difficulties they’re not intentionally being dishonest, but their stories change depending on the wording that they’re using because they can’t find their words and then other participants are concerned for them because they just heard a story that’s not necessarily true, but the person with dementia couldn’t find the words to accurately tell what was going on. So, some communication barriers (allied health provider).
Participants expressed a desire for access to resources and information specific to dementia, the disease process and how to support physical activity opportunities that were safe and inclusive.
Persons living with dementia and care partners described the existing resources as inconsistent, inaccessible or otherwise unavailable. One participant shared: ‘My mother had Alzheimer’s, my grandmother had Alzheimer’s as well, and I’ve never come across any information that walks you through what to expect. That would be very helpful’ (Care partner of person living with dementia). While recognising healthcare professionals as a key communication mechanism for information and educational resources about physical activity, one care partner shared:
The professionals don’t have the time for this (sharing information related to dementia), unless you have an appointment. Like if you’re on a list, it could be 3 months, could be 6 months, it could be a year, or could be really soon (care partner of person living with dementia).
In response, care partners connected informally to each other to promote knowledge sharing by leveraging community networks and using existing communication channels within the community. Close community connections, many based on decades of living in the same community, enabled persons living with dementia and their care partners to communicate their needs directly to healthcare professionals and allied health providers through informal relationships. Within smaller and geographically isolated communities, participants described a lack of anonymity, noting it was common to run into each other at the grocery store, public events or in their neighbourhood, allowing for informal connection and information exchange. Participants shared print copies of resources regarding physical activity and communicated by telephone to help compensate for the lack of accessibility to information formally from healthcare professionals and exercise providers.
Limited resources lead to ongoing need for flexibility, creativity and advocacy
Participants emphasised the complexity of securing necessary resources to support high quality and sustainable exercise programming.
Maybe we touched on this when we talked about barriers and the priorities for the health care team at this team, education and community integration doesn’t often come up as a high priority. It’s very task-oriented health care. Like, this happened, give them this treatment, they’re done. But helping with educating on, these are the things that are available in the community for you to participate in because this is going to be an ongoing—aging is not going to stop when you leave this hospital. Having more process-oriented approach and more education and more community integration, but unfortunately, due to resources that isn’t always a priority (allied health provider).
Participants described the importance of flexibility and creativity to overcome the inability of the health systems to provide physical activity opportunities, often due to limited funding, lack of infrastructure, and substantial gaps in human resources. In particular, participants shared their frustrations surrounding the limited specialized dementia care and services due to the limited human resources. This is especially prevalent within small and heterogeneous populations, as one participant noted:
There’s just one or two staff for a different, very broad population sometimes because they don’t have the same levels of functioning, but we only have … just the bare amount of staff, right. Maybe that’s also a challenge. We don’t have enough people (allied health provider).
Inadequate human resources can also lead to lack of specialist knowledge regarding exercise and dementia, contributing to unmet goals and objectives of both the programme providers as well as participants. The shortage and/or absence of trained care providers caused changes in programme design commonly by adjusting from physical to psychosocial goals. The flexibility to adjust the focus of the programme allowed activities to remain operational. One exercise provider described that when healthcare professionals were unable to provide formal rehabilitation programmes or exercise providers were unavailable to provide structured activities in their community, they pivoted to offer a social programme instead. However, in doing so, they were also aware of the need to provide supports that fell within their own scope of practice.
We have to be really mindful in terms of each other’s scopes, so we can’t do exercise- whatever’s called technically “exercise classes.” However, we can do thing that are fun and fitness, which would be like kick ball and badminton (allied health provider).
To mitigate the lack of trained formal healthcare professionals and exercise providers, community champions built capacity by engaging volunteers and student trainees. One participant emphasised that:
Most of the groups … we use the students for. And it was a student actually that made the falls group. [They] did all the prep for it, everything. Got it all in line and all the stuff out to the doctors. We just kept it. The same with the fit group; we just kept it. And they love it … -And it works well, too (healthcare professional).
Participants described making use of public spaces such as local recreation centres to organise informal activity opportunities and participate in group programmes in lieu of formal exercise facilities (eg, fitness club, community recreation centre), which may or may not be available. In one community, participants shared their use of a public multipurpose area for physical activity.
One of three recreation facilities…(includes) a multi-purpose facility. There’s tennis courts outside. There’s community rooms where events could be held, meetings could be held. There’s a gymnasium there. They do program sports, so you could go play at badminton (care partner of person living with dementia).
Physical activity programming: flexibility is needed to adapt to diverse community needs and preferences as well as expertise available
Healthcare professionals and allied health providers described the value of working towards defining physical activity programmes including a clear set of characteristics, naming, and the need for trained programme staff. Addressing each aspect is key to creating and sustaining a successful physical activity programme. However, challenges experienced in northern and rural communities in Canada are described below.
Defining physical activity programmes is needed but can affect accessibility for persons living with dementia
Participants discussed challenges when determining whether to define and clearly label a physical activity programme as focused and inclusive of persons living with dementia or to keep the focus more generic. Use of a clear definition acknowledging a specific focus of the programme designed for persons living with dementia was thought to improve clarity in participant eligibility and feelings of inclusion. It was also expressed that this may limit the willingness of some persons living with dementia to attend due to the stigma associated with dementia and cognitive impairment. This sentiment was expressed in relation to those living in small rural Canadian settings, where some people who wished to keep their diagnosis of dementia confidential were potentially risking their privacy if they attended a physical activity programme designed and labelled for persons living with dementia. The stigma associated with dementia was mitigated in small communities by offering the programmes at neutral locations within the community, changing the language to enhance inclusion and normalising the environment. One care partner commented that the stigma associated with dementia was still evident in their community and impacted their choices in physical activity: “And there’s a stigma attached to it in our minds. Not necessarily that anymore, but there has been in our past lives—a person not right, something wrong upstairs, here in the cortex” (care partner of person living with dementia). One healthcare professional also noted ‘If there’s an Alzheimer’s group, but somebody doesn’t like to acknowledge that they have Alzheimer’s then you might not want to suggest that they go to an Alzheimer’s group…so that could actually be a barrier” (healthcare professional).
Participants also expressed that labelling a programme as ‘exercise’ can be interpreted in different ways. For some, ‘exercise’ may be viewed as an opportunity to enhance and maintain health, while for others, exercise can be intimidating and exclusive. One exercise professional described this issue:
I have to re-approach all the time. If I approach someone and say, “Do you want to come exercise?” They’ll scoff at the thought of exercise. “I’m 94. I’m not going to exercise, today.” But then if I say, “Hey, want to come play a game with me.” Then they’re all for it (allied health provider).
At the same time, the lack of a clear definition for exercise was not always perceived as detrimental as it can allow for fluidity in roles. For rural communities in Canada with limited capacity, flexibility in job roles and volunteer engagement allowed programmes to continue to run. For example, one participant described how labelling a programme as a social activity allowed it to be offered by a variety of providers:
We’re not physio. We do fun and fitness. Like [when] physio is unable to come one morning because they’re doing other things or when they’re short staffed, then we do fun and fitness, so we do a game, like bowling (allied health provider).
Balancing programme design to meet everyone’s needs and expectations
No singular physical activity programme or method of delivery emerged as a one size fits all answer to ensure inclusivity for all persons living with dementia, at all times, and in all locations. Instead, participants shared the importance of intentional decisions around programme design and details including scheduling, programme location, participant eligibility and method of programme delivery (eg, standing, sitting or mixed classes) to meet the needs of those within their area. These decisions can be difficult when serving a small but diverse group, as in rural communities in Canada, when balancing finite human and financial resources. If a programme is too general, it may risk not being effective for anyone attending as noted by one exercise provider:
The problem is that … I don’t think that anybody’s really getting enough individual program in order to actually make an impact … Even with the stretching, they’re not necessarily getting positioned in the exact right place, but it’s one instructor and 20-25 people. So I think programming where you have a ratio … depending on what the abilities of those four people are, or three people, the helper could be helping the one that’s needing more assistance and that could travel (allied health provider)
Additionally, participants discussed the challenge of balancing routine and structure within the programmes, keeping the programme flexible enough to keep those participating engaged and meet their expectations while maintaining enough structure to achieve physical fitness goals. Flexibility in programme provision, programme design and provider roles was identified as a mitigation strategy, which enabled providers to be responsive to the needs and preferences of persons living with dementia, scheduling and practitioner scope of practice.
Programme participant level: supportive providers with flexibility are needed to help persons with dementia overcome challenges and fears
Participants shared unique experiences with physical activity based on the interaction between the rural environmental setting, the person living with dementia and their care partner where applicable.
Motivation and knowledge about physical activity
Participation in physical activity requires a conscious investment of time and personal resources. Persons living with dementia and care partners described difficulties balancing multiple demands and had difficulty prioritising physical activity due to other scheduled health-related appointments or commitments. When asked about what gets in the way of physical activity, one participant living with dementia explained there were often “Other activities that weren’t scheduled, or you’re already committed to”. Participants living with dementia noted the importance of a positive attitude and personal motivation towards physical activity participation as a critical enabler, for example:
I would enjoy more exercise. They have to change it up so it’s not always the same because you do get bored. I don’t care who you are, you get bored, so if you change the program a little bit every once in a while, then you’re more likely to keep attending (person living with dementia).
Participants living with dementia further expressed how challenging it was to find trustworthy information about physical activity, impacting their ability to engage in regular activity:
You know, the world’s a big place and I think the internet has a lot of good information. I don’t know how to access that, but I know the girls do, and I think it gives you a wide variety of information and choices. I don’t know what other source. I mean, I’m sure there are other sources. I haven’t a doubt that’s the only one (Person living with dementia).
Similarly, participants identified that having instructors who are knowledgeable about exercise and familiar with supporting persons living with dementia to be active, would be an important facilitator supporting their participation in physical activity.
I would like to actually see whether or not they’ve got trainers there that could show me. I’m not comfortable going into a weight room thinking, Oh, what I should be doing with this?…That would be good if there were people there that would teach you how to use weights (person living with dementia).
Fear can prevent participation
For persons living with dementia, a variety of fears were reported which prevented engagement in physical activity programming. These fears included: the fear of being institutionalised if the programme was held within a long-term care facility, the fear of getting lost when needing to take public transportation to attend an exercise class and the fear of injury from falling. Care partners further expressed negative feelings towards physical activity participation due to anticipation of the progressive loss of control and declining physical abilities of the person living with dementia as their disease progressed. For one care partner, they described how the fear not only led to distress but also that it was also an indicator for them of disease progression.
Mom doesn’t do a lot of exercise. She gets lost very quickly, now, and forgets where she is or where she’s going. She’s really nervous of falling. She’s terrified of snow. Like if there’s snow or ice, she doesn’t want to walk in it or she gets really stressed. Like she’ll panic because there’s snow or ice. She’s really nervous of falling down. That’s her biggest thing that she’s going to fall down. And with my mom, if she falls down, she doesn’t get, from a crawl to a stand is sometimes impossible. My mom would stand up and it’s really hard for her to stand up. And that’s something, that for me has been an indicator with both my parents when they couldn’t get up from getting down, whether it’s in the bathtub or when it’s something’s on the floor and they go down to get it and then they’re stuck and they can’t figure out how to get up and it’s—and then fear comes because they realize they can’t get up, but they’re like, “But I’m supposed to be able to get up and I can’t get up.” And so, I don’t know how to explain it, except that it’s terrifying for them, and it’s heartbreaking to witness, but it’s also heartbreaking for each of them (care partner of person with dementia).
In recognition that these fears are common for persons living with dementia, healthcare professionals and allied health providers noted the importance for fall prevention training for those individuals.
Building up the confidence [of persons living with dementia] in terms of getting up from a fall I think is important because fear of falling is a barrier to a lot of community participation, recreation and leisure participation in particular is what I’m referring to, but yeah, fear of falling is a big barrier for getting out and then people are at risk for social isolation (allied health provider)
Discussion
This study explored factors influencing physical activity participation for persons living with dementia in northern and rural communities in Canada and the strategies implemented in these settings to mitigate barriers to physical activity participation. From the perspectives of healthcare professionals, allied health providers, persons living with mild to moderate dementia and care partners, key points that emerged were the lack of health system support for physical activity participation, and substantial gaps in tailored exercise programme offerings and knowledge needed to provide accessible, inclusive opportunities for physical activity. Often in rural and northern communities, these challenges are compounded and interlinked (eg, accessibility to use a neutral location to offer a programme may not be available in the winter months or may experience scheduling challenges in the winter months due to competing demands for limited indoor space; reliability of public transportation may differ between winter and summer schedules or safety in walking outdoors may be affected by hours of sunlight by season or whether wildlife such as bears are active or hibernating).
In response to the substantial gaps experienced at the system level, community-driven initiatives emerged. Community-based solutions, developed in response to gaps in available services and supports, relied on a limited number of community champions to provide physical activity programming. These community-specific initiatives were organically tailored to address the needs of the community of focus with consideration of the unique environmental context and finite human and financial resources available. Fear of injury and stigma associated with a dementia diagnosis demand a multi-programme response with flexibility, inclusivity and knowledge, not only for persons living with dementia but also for care partners who support persons living with dementia to engage in physical activity.
The individual-level factors influencing physical activity for persons living with dementia, including fear, stigma, cognitive function and lack of knowledge, are commonly reported in the literature.26 While these are still true for people living in northern and rural communities in Canada, fear and stigma are heightened due to the smaller population size and lack of dementia-related knowledge due to limited access to trained providers or appropriate facilities. With small populations in rural communities, it can become increasingly difficult for person living with dementia and their care partners to protect their privacy as it is not possible to remain anonymous when attending community programming.40 In some cases, especially when individuals perceive their actions may be observed and discussed by others in their rural communities, they may prefer to engage in group activities in a neighbouring community; however, this may involve substantial investment of resources, including travel time and costs.40 Commonly in rural communities, while individual-level barriers persist, environmental and community-level factors create an additional barrier that must be overcome to engage in physical activity, which is particularly true for persons living with dementia.41
Context is essential to understand the factors influencing physical activity participation for persons living with dementia in northern and rural communities in Canada. In alignment with our previous work, the natural environment can both enhance physical activity participation and exercise (eg, proximity to outdoor recreation) and at the same time can also limit physical activity (eg, winter weather, ice).7 While the availability of facilities and accessible locations suitable for exercise provision and access to specialised exercise providers is a facilitator of physical activity for persons living with dementia in urban areas,27 our findings highlight the near-complete absence of such facilities and providers in northern and rural communities in British Columbia. This reinforces the importance to consider the links between the availability of infrastructure, networks and resources with the degree of urbanisation in the community.42 While it is common for exercise providers to have limited knowledge of dementia and training regarding inclusive practices in physical activities,28 this is amplified in rural communities by the continued reliance on exercise providers without formal training (eg, rehabilitation or recreation providers) working ‘off the side of their desk’ to meet community needs. The lack of trained and specialised staff leads to inconsistent programme content and availability, fragmentation of programme accessibility across different communities and limited capacity for formal assessment. The lack of health systems’ leadership, authority, regulation and quality control specific to physical activity programming have left individuals living in northern and rural communities in British Columbia to take a community-driven, grass-roots approach to support inclusion of persons living with dementia in physical activity and an over-reliance on non-profit community organisations. In response to the lack of leadership from the health system to support northern and rural communities in British Columbia, individual community champions have emerged, focused on building and enhancing community-level programmes to address existing deficits. When access to the programme relies on knowledge and awareness of community champions and informal networks, persons living with dementia and care partners who are not well connected and already engaged in the community may be unable to access physical activity programming. The issues identified in this study, which are present at the individual, community and system levels of the social–ecological model, echo the priorities and Canadian call to action described by Njkiforuk (2018) to ‘support equitable action on rural and remote physical activity promotion across Canada’.43 Furthermore, these findings warrant a collaborative response between communities and health systems to enhance equity in the ability of persons living with dementia to access physical activity supports, especially in Canadian northern and rural communities.
This study provides insight into the factors affecting physical activity participation for persons living with dementia involving participants across two rural and northern communities in British Columbia, Canada. The engagement of diverse stakeholders in this geographic region using a qualitative approach allowed us to capture diverse perspectives on the existing deficits and has helped to identify gaps in tailored exercise programme offerings and knowledge necessary to provide accessible, inclusive opportunities for physical activity. While a qualitative approach was deemed the most appropriate method to answer our research questions, further research may consider employing a quantitative research approach to gather both objective and subjective perspectives of participants and to increase the sample size. As the geographical focus of this work was limited to two northern and rural communities in Canada, findings may not be transferable to other communities such as urban centres or other countries with differing healthcare systems and resources. More research is needed to understand whether other northern and rural communities in Canada rely heavily on local community-specific initiatives. Furthermore, a limitation of this study is the limited number of participants living with dementia or mild cognitive impairment who participated in this study (n=4/29). While allied health providers and healthcare professionals who participated in the study provided valuable reflections on the challenges they have observed, they are limited in their ability to comment specifically on individual-level factors and the lived experiences of persons living with dementia and their care.
In Canada, unintended consequences of pandemic restrictions (eg, physical distancing protocols) include reductions of physical activity.44 45 Disruptions in daily routines and limited engagement in physical activity during the COVID-19 pandemic have been reported to severely impacted persons living with dementia.46 Emerging evidence suggests that interdisciplinary prevention approaches to address physical inactivity related to pandemic restrictions and isolation are urgently needed especially for persons living with dementia.47 As our work was conducted prior to the COVID-19 pandemic, future research is needed to examine how pandemic restrictions and social distancing protocols were experienced in rural and northern communities in Canada and subsequently how COVID-19 pandemic may have impacted the ability of persons with dementia to engage in physical activity and have impacted the provision of local community-driven initiatives.
Conclusions
Physical activity opportunities and experiences for persons living with dementia living in northern and rural communities in Canada are shaped by the environmental context and limited accessibility to specialised programming. Local champions risk burnout by working to fill gaps left by absent health and non-profit sectors in small communities, limiting the long-term capacity and support in northern and rural communities for growing number of persons ageing with dementia in Canada. It is important to support existing community leaders in a way that respects local knowledge and expertise.
Supplementary Material
Footnotes
Twitter: @shanfree77
Contributors: All authors were actively engaged in this project in accordance with the ICMJE guidelines for authorship. As the guarantor and first author, SF accepts full responsibility for this work. SF and LEM were involved in all aspects of this research. CP was involved in all aspects of the manuscript development including data analysis, writing and editing. LB was involved in planning the project, data collection and editing of the manuscript. KR was involved in planning the project and editing of the manuscript. KW was involved in data analysis, drafting and editing the manuscript. SS was involved in drafting and editing the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s)
Ethics approval
Harmonised ethics approval was received for this study from the University of Northern British Columbia and University of British Columbia (H18-00392). Participants gave informed consent to participate in the study before taking part.
References
- 1.World Health Organization . Dementia fact sheet. World Health organization, 2021. Available: https://www.who.int/news-room/fact-sheets/detail/dementia [Accessed Sep 2021].
- 2.Public Health Agency of Canada . A dementia strategy for Canada: together we achieve -2021 annual report, 2022. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/dementia-strategy-annual-report-parliament-2021.html [Google Scholar]
- 3.Laurin F, Pronovost S, Carrier M. The end of the urban-rural dichotomy? towards a new regional typology for SME performance. J Rural Stud 2020;80:53–75. 10.1016/j.jrurstud.2020.07.009 [DOI] [Google Scholar]
- 4.Keating N, Phillips J. A critical human ecology perspective on rural ageing. Rural ageing: A good place to grow old, 2008: 1–10. [Google Scholar]
- 5.MacGregor-Fors I, Vázquez L-B. Revisiting ‘rural’. Sci Total Environ 2020;741:132789. 10.1016/j.scitotenv.2019.06.135 [DOI] [PubMed] [Google Scholar]
- 6.Coates K, Poelzer G, Macdonald-Laurier Institute publication . The next Northern challenge: the reality of the provincial North, 2014. Available: https://www.macdonaldlaurier.ca/files/pdf/MLITheProvincialNorth04-14-Final.pdf
- 7.Ward K, Pousette A, Pelletier CA. Not Everybody’s an Athlete, But They Certainly Can Move”: Facilitators of Physical Activity Maintenance in Older Adults in a Northern and Rural Setting. J Aging Phys Act 2020;6:854–63. 10.1123/japa.2019-0393 [DOI] [PubMed] [Google Scholar]
- 8.Winterton R, Warburton J, Keating N, et al. Understanding the influence of community characteristics on wellness for rural older adults: a meta-synthesis. J Rural Stud 2016;45:320–7. 10.1016/j.jrurstud.2015.12.010 [DOI] [Google Scholar]
- 9.Northern Health Authority . Healthy aging in the North: action plan. Northern health authority 2015, 2015. Available: https://www.northernhealth.ca/sites/northern_health/files/health-information/seniors/documents/healthy-aging-in-the-north-action-plan-2015.pdf [Accessed Aug 2021].
- 10.Vedel I, Sheets D, McAiney C. CCCDTD5: individual and community‐based psychosocial and other non‐pharmacological interventions to support persons living with dementia and their caregivers. A&D Transl Res & Clin Interv 2020;6:e12086. 10.1002/trc2.12086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alzheimer Society of Canada . Staying physically active, 2021. Available: https://alzheimer.ca/en/help-support/im-living-dementia/living-well-dementia/staying-physically-active
- 12.Blankevoort CG, van Heuvelen MJG, Boersma F, et al. Review of effects of physical activity on strength, balance, mobility and ADL performance in elderly subjects with dementia. Dement Geriatr Cogn Disord 2010;30:392–402. 10.1159/000321357 [DOI] [PubMed] [Google Scholar]
- 13.Eshkoor SA, Hamid TA, Mun CY, et al. Mild cognitive impairment and its management in older people. Clin Interv Aging 2015;10:687. 10.2147/CIA.S73922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ginis KAM, Heisz J, Spence JC, et al. Formulation of evidence-based messages to promote the use of physical activity to prevent and manage Alzheimer's disease. BMC Public Health 2017;17:209. 10.1186/s12889-017-4090-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erickson KI, Hillman C, Stillman CM, et al. Physical activity, cognition, and brain outcomes: a review of the 2018 physical activity guidelines. Med Sci Sports Exerc 2019;51:1242–51. 10.1249/MSS.0000000000001936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malthouse R, Fox F. Exploring experiences of physical activity among people with Alzheimer's disease and their spouse carers: a qualitative study. Physiotherapy 2014;100:169–75. 10.1016/j.physio.2013.10.002 [DOI] [PubMed] [Google Scholar]
- 17.Cedervall Y, Torres S, Åberg AC. Maintaining well-being and selfhood through physical activity: experiences of people with mild Alzheimer’s disease. Aging Ment Health 2015;19:679–88. 10.1080/13607863.2014.962004 [DOI] [PubMed] [Google Scholar]
- 18.Kontos P, Grigorovich A, Dupuis S, et al. Raising the curtain on stigma associated with dementia: fostering a new cultural imaginary for a more inclusive Society. Crit Public Health 2020;30:91–102. 10.1080/09581596.2018.1508822 [DOI] [Google Scholar]
- 19.Hartman YAW, Karssemeijer EGA, van Diepen LAM, et al. Dementia patients are more sedentary and less physically active than age- and sex-matched cognitively healthy older adults. Dement Geriatr Cogn Disord 2018;46:81–9. 10.1159/000491995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Laurin D, Verreault R, Lindsay J, et al. Physical activity and risk of cognitive impairment and dementia in elderly persons. Arch Neurol 2001;58:498–504. 10.1001/archneur.58.3.498 [DOI] [PubMed] [Google Scholar]
- 21.Bowes A, Dawson A, Jepson R, et al. Physical activity for people with dementia: a scoping study. BMC Geriatr 2013;13:1–10. 10.1186/1471-2318-13-129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q 1988;15:351–77. 10.1177/109019818801500401 [DOI] [PubMed] [Google Scholar]
- 23.Stubbs B, Eggermont L, Soundy A, et al. What are the factors associated with physical activity (PA) participation in community dwelling adults with dementia? A systematic review of PA correlates. Arch Gerontol Geriatr 2014;59:195–203. 10.1016/j.archger.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 24.Hancox JE, van der Wardt V, Pollock K, et al. Factors influencing adherence to home-based strength and balance exercises among older adults with mild cognitive impairment and early dementia: promoting activity, independence and stability in early dementia (PrAISED). PLoS One 2019;14:e0217387. 10.1371/journal.pone.0217387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dening T, Thomas A. Oxford textbook of old age psychiatry. Oxford University Press, 2013: 1–823. [Google Scholar]
- 26.van Alphen HJM, Hortobágyi T, van Heuvelen MJG, Barriers vanHMJ. Barriers, motivators, and facilitators of physical activity in dementia patients: a systematic review. Arch Gerontol Geriatr 2016;66:109–18. 10.1016/j.archger.2016.05.008 [DOI] [PubMed] [Google Scholar]
- 27.Hobson N, Dupuis SL, Giangregorio LM, et al. Perceived facilitators and barriers to exercise among older adults with mild cognitive impairment and early dementia. J Aging Phys Act 2020;28:208–18. 10.1123/japa.2019-0010 [DOI] [PubMed] [Google Scholar]
- 28.Bechard LE, McDougall A, Mitchell C, et al. Dementia- and mild cognitive impairment-inclusive exercise: perceptions, experiences, and needs of community exercise providers. PLoS One 2020;15:e0238187. 10.1371/journal.pone.0238187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canadian Institutes of Health Research . Strategy for patient-oriented research: patient engagement framework, 2021. https://cihr-irsc.gc.ca/e/documents/spor_framework-en.pdf [Google Scholar]
- 30.Rural Coordination Centre of BC . Rural practice subsidiary agreement, 2021. Available: https://rccbc.ca/rccbc/about-the-jsc/rsa-communities/
- 31.Polit DF, Beck CT. Nursing research: principles and methods. 729. Lippincott Williams & Wilkins, 2004. [Google Scholar]
- 32.Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. Sage, 2013. [Google Scholar]
- 33.Denzin NK, Lincoln YS, eds. The Sage handbook of qualitative research. Sage, 2011. [Google Scholar]
- 34.Planning and research design for focus groups. Morgan DL. Focus groups as qualitative research. 16, 1997. [Google Scholar]
- 35.Wong LP. Focus group discussion: a tool for health and medical research. Singapore Med J 2008;49:256–60. [PubMed] [Google Scholar]
- 36.Tausch AP, Menold N. Methodological aspects of focus groups in health research: results of qualitative interviews with focus group moderators. Glob Qual Nurs Res 2016;3:2333393616630466. 10.1177/2333393616630466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clarke V, Braun V. Thematic analysis. in encyclopedia of critical psychology. Springer New York NY 2014:1947–52. 10.1037/13620-004 [DOI] [Google Scholar]
- 38.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 39.Spence JC, Lee RE. Toward a comprehensive model of physical activity. Psychol Sport Exerc 2003;4:7–24. 10.1016/S1469-0292(02)00014-6 [DOI] [Google Scholar]
- 40.Morgan DG, Semchuk KM, Stewart NJ, et al. Rural families caring for a relative with dementia: barriers to use of formal services. Soc Sci Med 2002;55:1129–42. 10.1016/S0277-9536(01)00255-6 [DOI] [PubMed] [Google Scholar]
- 41.Pelletier CA, White N, Duchesne A, et al. Barriers to physical activity for adults in rural and urban Canada: a cross-sectional comparison. SSM Popul Health 2021;16:100964. 10.1016/j.ssmph.2021.100964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gansefort D, Brand T, Princk C, et al. Community readiness for the promotion of physical activity in older adults—A cross-sectional comparison of rural and urban communities. Int J Environ Res Public Health 2018;15:453. 10.3390/ijerph15030453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nykiforuk CIJ, Atkey K, Brown S, Kayla A, Sara B, et al. Promotion of physical activity in rural, remote and Northern settings: a Canadian call to action. Health Promot Chronic Dis Prev Can 2018;38:419–35. 10.24095/hpcdp.38.11.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Di Sebastiano KM, Chulak-Bozzer T, Vanderloo LM. Don’t walk so close to me: physical distancing and adult physical activity in Canada. Frontiers in Psychology 2020;1895. 10.3389/fpsyg.2020.01895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gierc M, Riazi NA, Fagan MJ, et al. Strange days: adult physical activity and mental health in the first two months of the COVID-19 pandemic. Front Public Health 2021;9:325. 10.3389/fpubh.2021.567552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bacsu J-DR, O'Connell ME, Webster C, et al. A scoping review of COVID-19 experiences of people living with dementia. Can J Public Health 2021;112:400–11. 10.17269/s41997-021-00500-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Müller P, Achraf A, Zou L, et al. COVID‐19, physical (in‐) activity, and dementia prevention. Alzheimer’s & Dementia: Translational Research & Clinical Interventions 2020;6:e12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-060860supp001.pdf (56.8KB, pdf)
bmjopen-2022-060860supp002.pdf (127.2KB, pdf)
Data Availability Statement
No data are available.