Abstract
In Canada, people from culturally and linguistically diverse (CALD) backgrounds are at a greater risk of developing a chronic illness, and are more likely to experience adverse health effects and challenges in accessing high-quality care compared with Canadian-born individuals. This, in part, has been attributed to having inadequate access to information and resources needed to manage their illness(es). A qualitative descriptive design and inductive content analysis were used to explore the information needs of 24 CALD patients with chronic illnesses. Participants identified medical, lifestyle, and psychosocial information needs. How much information was needed depended on such antecedents as illness trajectory, severity, and perception. Most information needs remained unmet. A number of communication strategies were identified to bridge language barriers that go beyond translation and are based on effective health education strategies. Findings can help health care professionals better identify CALD patients’ information needs and provide strategies that go beyond translation.
Keywords: ethnicity, qualitative research, information seeking, chronic illness, self-management, culturally and linguistically diverse communities, Canada
Introduction
Canada has one of the largest culturally and linguistically diverse (CALD) populations among the G7 countries (Statistics Canada, 2011). According to the 2016 Canadian census, 21.9% of the Canadian population was foreign-born, 72.5% of which did not identify English or French (both official languages of Canada) as their mother tongue (Statistics Canada, 2017).
CALD individuals are at a greater risk of developing a chronic illness, and are more likely to experience adverse health effects and challenges in accessing high-quality care compared with Canadian-born individuals (Gushulak et al., 2011). Many studies have documented the “healthy immigrant effect,” whereby upon arrival immigrants report better physical and mental health compared with Canadian-born individuals, but within 5 years, these health indicators drop significantly, lower than newly arrived immigrants (Betancourt & Roberts, 2010; De Maio & Kemp, 2010; Fuller-Thomson et al., 2011; Hyman & Jackson, 2010; Ng, 2011). These health disparities have prompted research into the needs of CALD patients to improve the delivery of supportive care and enhance chronic illness management (Harrison et al., 2009).
Among the several domains of supportive care needs, information needs have been identified as being the most pressing among CALD individuals diagnosed with chronic illnesses (Butow et al., 2013; O’Callaghan et al., 2016). Information needs are generally defined as “a perceived gap between what an individual knows and what he or she wants to know to achieve a certain goal” (Lambert & Loiselle, 2007, p. 1013). Most studies in the CALD literature do not address information needs directly, but rather have indirectly identified these through exploring experiences of CALD patients in self-management or evaluating the knowledge of their chronic disease (Cha et al., 2012; Finucane & McMullen, 2008; Shaw et al., 2015).
CALD groups face unique barriers in meeting their information needs, such as language and culture, both of which influence their health literacy (i.e., ability to access, understand, evaluate, and communicate health information; Hoffman-Goetz et al., 2014; Visram, 2013; Zanchetta et al., 2013). CALD populations often score below the national averages for health literacy (Murray et al., 2008). Without an adequate level of health literacy, CALD populations may encounter difficulty understanding health information, navigating health services, making treatment choices, and engaging in self-care for chronic disease management, further contributing to health disparities within this population (Hoffman-Goetz et al., 2014; Marshall et al., 2010; Ridpath et al., 2012).
To address the need for information, current interventions for CALD populations include translating health information into different languages and/or presenting the information at a low reading grade level with pictures (Simich, 2009). Although these translated patient education materials might overcome language barriers, they are often not culturally relevant and therefore cannot adequately fulfill CALD patients’ information needs (Simich, 2009). Hoffman-Goetz et al. (2014) advised that instead of a “one-size-fits-all approach” using translated materials, health care professionals (HCPs) should consider other strategies (e.g., use of culturally competent interpreters, creation of a safe environment where cultural conversations can take place) to increase access and understanding of health information.
Given Canada’s large CALD population and chronic disease burden, it is important to understand how to best support CALD patients in managing chronic illness. The purpose of this study was to explore CALD patients’ information needs, access to, and understanding of health information to manage chronic illnesses. The research questions were as follows:
Research Question 1: What are the information needs of CALD patients in managing their chronic illness(es)?
Research Question 2: How do CALD patients diagnosed with chronic illness(es) access and understand health information?
Research Question 3: What are the opinions of CALD patients on translated patient education materials?
Method
Design
A qualitative descriptive design was used to answer the study questions. This qualitative approach is well suited to obtain a clear description of a specific phenomenon from the perspective of those experiencing it (Magilvy & Thomas, 2009; Sandelowski, 2000). The COnsolidated criteria for REporting Qualitative research (COREQ) were used in the reporting of this study (Tong et al., 2007). Ethical approvals were obtained from the university and affiliated health care institutions.
Sample and Setting
Using convenience sampling, 25 participants were recruited from outpatient clinics, a patient information resource center, or inpatient units of large university-affiliated hospitals in Montreal, Quebec, Canada (see Figure 1). The inclusion criteria were as follows: (a) Chinese, Greek, Italian, or Middle Eastern origin (foreign born); (b) main language spoken at home is neither English nor French; (c) proficient in neither English nor French; (d) diagnosed with at least one physical chronic illness; and (e) aged 18 years or older. These specific ethnic groups were chosen as they are among the largest ethnic groups in Montreal (Statistics Canada, 2012). Exclusion criteria were: (a) living more than 40 km away from the hospital, and (b) diagnosed with an acute, unstable psychiatric disorder as assessed by the referring clinician. These criteria were chosen to ensure feasibility in terms of travel for patients and researchers, and based on the assumption that patients who cannot adequately express themselves due to a psychiatric disorder may constrain data collection. The final data set contained 24 interview transcripts; one interview was not included for analysis due to poor quality of the audio recording.
Figure 1.
Study flow diagram.
Recruitment
Treating clinicians identified eligible participants, and then a research assistant (RA) speaking the patient’s language approached them at a scheduled time to review the study objectives and the recruitment package (containing the invitation letter, consent form, survey, and stamped addressed envelope). If an RA speaking the participants’ language was not available, interpreters were used. All materials were available in English and French, in addition to the targeted languages. Once the RA explained the study, participants signed the informed consent form and were given the choice to complete the interview at that time or at a later scheduled time with the RA (face-to-face or over the telephone). None of the participants knew the RAs before the study.
Data Collection
Semistructured interviews were conducted either in patients’ homes or private rooms in the clinical setting. Interviews lasted 30 to 135 minutes and were audio recorded. Bilingual trained RAs (male and female) conducted most of the interviews with some interviews conducted with the help of professional or informal interpreters. Family members or friends accompanying the patient were the interpreters in 10 of the 24 interviews. All interviews followed an English semistructured interview guide (see Supplementary Material S1), which was translated into Chinese, French, Greek, Italian, and Arabic. Translated patient education materials (see Supplementary Material S2) relating to the participant’s main diagnosis were obtained from various patient education resource websites and presented, in hard copy format, at the interview to engage the patients during the interview to talk about their experience with similar materials. Interviews concluded with participants completing a sociodemographic questionnaire.
Data Analysis
Interviews were transcribed directly into English by a translator. To ensure the quality of translation, transcripts were subsequently spot-checked by independent professionals, proficient in English and in the languages in which the interviews were conducted (Squires, 2009). In the absence of a priori framework and given the relatively fragmented knowledge in the area, data from transcripts were analyzed using inductive content analysis, to capture participants’ experiences and perspectives within the context of their life stories (Elo & Kyngäs, 2008). Four experienced qualitative RAs analyzed the transcripts independently, and discussed their open coding at regular meetings, resolving disagreements via discussion. Two RAs analyzed the first nine transcripts, and two analyzed all 24. The RAs immersed themselves in the data by reading the transcripts several times to understand the main ideas of the interview (Sandelowski, 1995). Key phrases in the transcripts were highlighted and summarized to form codes that were consistent with the participants’ statements. Similar codes were then grouped into categories and organized into a coding framework based on the interview guide to ensure consistency (Elo & Kyngäs, 2008; Polit & Beck, 2017). Themes were then abstracted from the categories and discussed with the research team with the objective of reaching consensus (Elo & Kyngäs, 2008; Shenton, 2004). Themes stayed close to the language of the participants as much as possible and conveyed an underlying pattern discerned from the data (Sandelowski & Barroso, 2003). The sociodemographic questionnaires completed by participants were analyzed using descriptive statistics to provide a description of the sample.
Trustworthiness
Credibility was optimized (a) with member checks throughout interviews to verify participants’ intended meaning, (b) with peer debriefing among the authors to discuss data interpretation, and (c) by training interpreters to be familiar with qualitative research methods (Lincoln & Guba, 1985; Squires, 2008). To ensure credibility of the transcripts, all interpreters, transcribers, and spot-checkers worked independently (Squires, 2009). To ensure credibility and dependability, an iterative process of data analysis and collection was used, with the interview guide being modified as key themes emerged (Lincoln & Guba, 1985). Audio recordings, field notes, demographic questionnaires, interview guides, and interview transcripts as well as products of data analysis were kept as an audit trail to enhance confirmability and dependability. Transferability was strengthened through thick descriptions of the methods, as well as the use of the sociodemographic questionnaire (Shenton, 2004).
Results
Participants
Participants represented a diverse cultural population and spoke Cantonese (n = 10), Greek (n = 6), Italian (n = 4), Mandarin (n = 3), or Arabic (n = 1). Slightly more than half of participants were men (n = 14, 58.3%). Age ranged from 42 to 86 years old: M (SD) = 68.7 (12.38), median (interquartile range [IQR]) = 69.0 (21). The number of years lived in Canada ranged from 9 to 58 years: M (SD) = 35.6 (15.97), median (IQR) = 33.5 (29). Slightly more than half of participants (57%) reported that they had completed elementary-level schooling as their highest education level. For more details on the study sample, see Table 1. Flow of participants through the study is detailed in Figure 1.
Table 1.
Participant Characteristics (N = 24).
| Characteristics | n | % |
|---|---|---|
| Age (years) | ||
| 18–60 | 5 | 20.8 |
| 61–70 | 6 | 25.0 |
| 71–80 | 4 | 16.7 |
| 81–90 | 5 | 20.8 |
| 4.4 | 4 | 16.7 |
| Gender | ||
| Male | 14 | 58.3 |
| Female | 10 | 41.7 |
| CALD groups | ||
| Chinese | 13 | 54.2 |
| Greek | 6 | 25.0 |
| Italian | 4 | 16.7 |
| Arabic | 1 | 4.2 |
| Education completed | ||
| Elementary | 12 | 56.5 |
| Secondary | 5 | 21.7 |
| 4.4 | 1 | 4.3 |
| Bachelor’s | 3 | 13.0 |
| 4.4 | 3 | 4.3 |
| Years in Canada | ||
| 1–15 | 2 | 8.3 |
| 16–30 | 9 | 37.5 |
| 31–45 | 4 | 16.7 |
| 46–60 | 9 | 37.5 |
| Employment | ||
| Full- or part-time | 2 | 8.3 |
| Unemployed | 4 | 16.7 |
| Retired | 17 | 70.8 |
| 4.4 | 1 | 4.2 |
| Primary diagnoses | ||
| Cardiovascular | 23 | |
| Endocrine/metabolic | 12 | |
| Renal | 9 | |
| Cancer | 7 | |
| Musculoskeletal | 5 | |
| Gastrointestinal | 3 | |
| Neurological | 2 | |
| Psychiatric | 2 | |
| Other | 4 | |
Note. CALD = culturally and linguistically diverse.
Variability in Health Information Needs
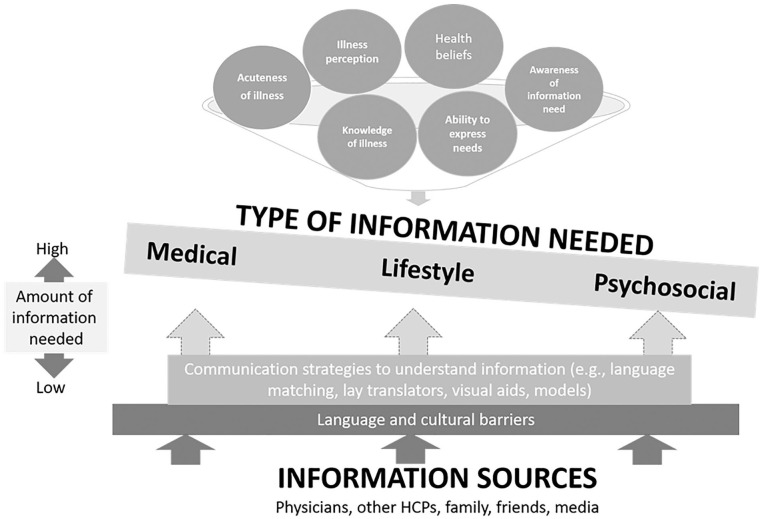
The key findings are summarized in Figure 2. Eliciting data on participants’ information needs was more multifaceted than simply generating a list of topics. In understanding participants’ information needs, a number of antecedents were revealed (indicated at the top of Figure 2). Early on in the interviews, it became apparent that participants who identified more information needs were those who viewed their illness as a challenge; “gave up”; had limited previous knowledge about their illness; and/or held beliefs about health, illness, and what quality care entailed that were incompatible with the approaches espoused by their treating teams. More information needs were also articulated by those closer in time to diagnosis, and those who described more severe symptoms and treatment side effects when compared with those who described their illness as “not a big deal”. Another antecedent pertained to participants’ level of comfort in expressing their information needs, either during the interview or in interactions with HCPs. In addition, participants sometimes were not aware that they had an information need until these were brought to their awareness through the discussion with the interviewer. One participant, when asked what information she wanted, responded that she had “never thought about it”.
Figure 2.
Summary of key findings—Overview of noted patterns among the transcripts in antecedents, the types of needs, and information sources to address these needs.
Note. HCPs = health care professionals.
Types of Information Needs
Three categories of information needs were noted across the interviews: medical, lifestyle, and psychosocial information. However, these categories of information needs were not equally expressed either during the interview or to the treating team, as illustrated by the seesaw in Figure 2. Details of these information needs are presented in the following sections, and specific topics identified by participants are summarized in Table 2.
Table 2.
Information Needs Identified by Study Participants (N = 24) also found that family plays a
| Medical Information | Lifestyle Information | Psychosocial Information |
|---|---|---|
| Etiology, diagnosis, including diagnostic test results and other disease indicators (n = 13 a ) | Culturally relevant dietary modifications (n = 9) | Impact on family (n = 19) |
| Treatment plans and options (n = 11) | Overall health promotion and disease prevention (n = 7) | Practical and logistical concerns (n = 19) |
| Disease progression and clinical prognosis (n = 10) | Exercise (n = 5) | Emotional impact of chronic illnesses (n = 11) |
| Medication and side effects of medication (n = 8) | Changes to ADLs (n = 2) | |
| Health status at routine checkups (n = 8) | ||
| Explanation on surgeries and postoperative management (n = 4) | ||
| Related potential comorbidities that may develop (n = 2) |
Note. ADLs = activities of daily living.
The numbers represent the number of participants mentioning a particular need. The totals are not mutually exclusive, that is, a participant may have identified multiple needs.
Getting a handle on my health situation: Medical information needs most likely to be expressed
Information needs pertaining to patients’ medical conditions were most often expressed in encounters with HCPs and were those typically listed first by participants during the interviews, with several participants identifying more than one need. Medical information needs were expressed by participants despite having received their diagnosis decades ago and pertained not only to the illness participants were dealing with at the time of the interview but also conditions they anticipated manifesting in the future. For example, one Chinese participant diagnosed with cancer mentioned that the “elderlies all have the three high”—referring to high blood pressure, high cholesterol, and high blood sugar, and expressed a keen interest in learning about all three.
Culturally specific treatment information needs were mentioned particularly by Chinese participants wanting to balance Traditional Chinese Medicine (TCM) and Western medicine. The majority of Chinese patients expressed preference for Western medicine in dealing with “serious” conditions, but specified that TCM was better suited to alleviate the symptoms of minor health conditions such as colds or to manage side effects. The few participants who favored TCM over Western medicine (n = 2) felt that TCM had fewer side effects, or they had not achieved the desired outcomes using Western medicine and turned to TCM as a last resort.
Knowing how to integrate and adapt lifestyle habits: Lifestyle information needs expressed during medical encounters, but information received not always pertinent
Lifestyle needs were articulated by almost half of participants (see Table 2 for topics). Culturally relevant dietary information needs were identified predominantly by Chinese participants due to differences between Chinese and Western dietary behaviors and beliefs. Although a handful of participants had been referred to nutritionists or dieticians, most perceived the information received as being culturally irrelevant, a view predominately shared by the Chinese participants. For instance, some participants discussed their belief that depending on the illness, they will favor “hot” or “cold” foods. Therefore, when one participant was advised to consume milkshakes as a protein supplement while on chemotherapy, this was inconsistent with his or her belief that eating “cold foods” was “not good” for one’s health.
Exercise was another lifestyle information need expressed, including wanting advice on the amount and intensity of exercise that would be most appropriate. Participants desired to obtain recommendations on aspects such as the optimal duration of walking, and whether they could garden and lift heavy items. Conversations regarding exercise between patients and HCPs were not part of routine medical encounters and were confined to targeted questions asked by patients or their caregivers. Whereas most participants considered the exercise recommendations received from HCPs useful, some participants admitted to challenges in implementing them due to lack of motivation: “They ask me to go exercise . . . but I’m lazy so I don’t.”
Other lifestyle information needs, including general health maintenance, health promotion, healthy aging, and activities of daily living (ADLs), were not typically discussed during medical encounters, due to the importance devoted to medical needs, and the belief that “In Canada [. . .] there is no much health maintenance thing due to peoples’ good knowledge of health care.” One participant was frustrated that her physicians did not offer “advice, about . . . [other] assistance method[s] . . . [like] physical therapy” to help with ADLs. However, she believed it was because she could not articulate her needs properly: “I don’t know what to say to completely match my feelings.”
Overall, considering the challenges related to the inadequacy of nutrition advice received from HCPs, the limited discussions regarding exercise, and lack of advice regarding other lifestyle aspects, most participants fulfilled their lifestyle needs outside of the clinical encounters. This issue is explored further in the section titled “Addressing Information needs.”
Dealing with fears and worries: Psychosocial information needs least likely to be expressed
Psychosocial information needs were least likely to be expressed explicitly during medical encounters and during the interviews, requiring more probing, or were revealed when discussing the translated patient education materials. Despite this, 20 participants articulated some kind of psychosocial information need, mostly pertaining to emotional impact of chronic illnesses (e.g., anxiety, stress, and fear of the unknown; see Table 2). For example, one participant said, “I have fear [t]hat I’m going to be one day like my husband [. . .] I don’t deal [… with this]. It is there. And I can’t do anything.” Another psychosocial information need was the impact on family, whereby participants highlighted the burden of illness on their children, who were required to take time off work to accompany their parents to medical appointments and translate information. For practical considerations, whereas most participants appreciated that the costs related to treatment and medication were covered under Canadian public health insurance, others referred to the economic burden related to services that were not covered (e.g., physiotherapy, translation services required in the absence of family members). Psychosocial needs seemed to emerge for many participants from having unmet medical information needs.
Addressing Information Needs: Accessing and Understanding Health Information
Although medical information needs were often expressed, most participants reported that these needs remained unmet, followed by psychosocial and lifestyle information needs. The extent to which information needs were met depended on the source of information and the extent to which communication strategies were put in place to overcome language barriers. This interaction is illustrated at the bottom of Figure 2. Participants relied on three different sources of information, each is now described in turn.
Professional sources
HCPs were the most common source to meet medical information, including doctors (n = 24), nurses (n = 11), pharmacists (n = 8), and nutritionists (n = 7). Participants placed a high value on the knowledge brokered by HCPs due to their “accuracy,” “trustworthiness,” and “experience”: “Whatever [the doctors] tell us, we do.”
Linguistic mismatch between participants and their HCPs was a barrier for all participants (to some extent) and one participant likened it to a “wall”. This barrier was recognized to be customary: “I don’t understand French so I don’t know what [the nurse] is talking about. I am accustomed to the difficulty.” Another participant spoke about being left in the dark:
The specialist that I had before gave me information, but he gave it to me in the way that he wanted, not in a way that was easy for me to understand. [. . .] He didn’t explain very well. He was too abrupt. [. . .] When someone is in the dark, it is completely useless. If the doctor doesn’t give information, he is completely in the dark.
Such linguistic challenges seemed to deter participants’ health-seeking behaviors, as explained by one participant: “Those Chinese, they don’t come to these hospitals. They are scared to come in, because nobody translates.”
Participants did identify several communication strategies to bridge the communication gap with HCPs. One strategy for almost half of the participants was to find an HCP who spoke their language. Two participants explained how Chinese-speaking pharmacists acted as information sources on their medications: “Every time I pick up a new drug, he explains to me [. . .] So when we don’t fully understand, he will go on Internet and pull out all the information for us.” Patients even went as far as consulting reputable physicians in their home countries.
Another common strategy to overcome linguistic mismatch was to rely on lay sources (family members and, to a lesser extent, friends) to provide translation and help navigate the health care system. This was particularly important for participants who did not have a basic command of English or French (representing the majority of participants interviewed). For the few participants in this situation and who had no family involved, understanding health information proved to be impossible, with one patient reporting: “Now I gave up. I don’t try to find anything.” Few participants independently hired a private translator, with one participant reporting that her HCP hired a translator.
Participants with basic command of either English or French described fewer challenges in understanding information. One patient explained she understood information in French (but not English) due to its similarity to Italian: “When I go to the doctor, I speak to him in French and he understands me. When he talks to me, I understand him.” Although this was a starting point to communicate with HCPs, communication was often limited to “casual talk” and “simple communication” leading to only a “basic understanding” or incomplete understanding between the patient and HCP. One patient stated, “Mostly it is only the doctor who speaks (while I only listen), sometimes I can understand [only] basically, because I find it hard to express.” Challenges related to medical terminology were commonly highlighted: “Yeah, I understand, but some word for medical terms, I not understand.” Another patient explained, “It’s as if they are speaking another language, a language that only they can understand, even if it’s in Italian.” To overcome such barriers, half of these participants also relied on lay sources to translate and few relied on translation dictionaries.
Other communication strategies included the following: speaking “slowly,” using return demonstration, body gestures, “models” and “pictures”. These methods required HCPs to “take [the] time” to be supportive and “make sure they would understand” (patient’s daughter). For example, one participant who had changed treating physicians stated that she trusted the new physician more because “he explains things very clearly to me”. Short visits and continuity of care issues were barriers to using these strategies:
And when we would go see the doctor well it would just be like a 5 minute visit and in and out and we would be getting comments like “I’m not God” you know did my best and we would leave and say well I guess we’re going to continue praying to God.
Lay sources
Lay sources were a key source of lifestyle and psychosocial information, and included friends (n = 10), family (n = 6), coworkers (n =1), and experience gained from real life and/or self-study (n = 7) (i.e., cultural beliefs/practices, experiential learning, and day-to-day experiences). Most participants expressed relying on lay sources as intermediaries in the communication of health information: “I need [my children] because I don’t understand everything but in the hospital there is no people speak Italian,” especially if that person had medical knowledge.
Some patients also discussed the importance of relying on their own lay experiences, whether it was based on cultural beliefs or traditional practices. For example, one patient described her knowledge of dietary recommendations founded in traditional Greek culture: “The wild dandelions, that sprout [. . .] They clean the blood. They help with the kidneys. All this we know from Greece.”
Media sources
Media sources included TV and radio broadcasts, printed materials, and the internet. Almost half of participants spoke of health programming that was available in their native language on TV or on the radio. Broadcasts were not only a source of specific information relating to patients’ diagnoses but further acted as sources of information on other illnesses and health maintenance/promotion. One participant explained, “On TV there is a program in Italian where they explain all of these things [. . .] about dialysis [. . .] It’s a medical program [. . .] [there’s] even the same thing with diabetes.” Information provided via media was not only valued because it was in their native language but also because it was facilitated by professional sources: “I have been watching the Beijing channel, those doctors are very smart.”
Participants also spoke of printed materials, including newspapers, books, translation dictionaries, and English or French pamphlets or booklets received from hospitals or HCPs. However, due to linguistic mismatches, pamphlets in English or French remained inaccessible for about half of the participants who received them, and translation help from a lay source was needed: “I didn’t really . . . go through that booklet. Well it’s English and French, so it was mostly my son who reads it.” Even if the information in these pamphlets was translated, it remained culturally inappropriate:
I gave it to my niece to read, and after [. . .] she told me if I followed the diet in the book, it wouldn’t be good, because I’m Chinese, [the dietician is] Western. If I eat like Western people, it won’t work.
To be able to understand the pamphlets, many also “look in the dictionary” for terms. The use of “clear information,” “easy words and pictures”, and linguistic resemblances to their native language facilitated understanding the information pamphlet despite it being written in English or French. About a quarter of participants obtained books or pamphlets in their own language. As explained by one patient, “I even bought many illustrated books on my disease when I went back to China to study my disease [. . .] I went through those books for many […] over again and again.”
All participants shown translated pamphlets during the interview (see Supplementary Material S2) had never seen them beforearticipants highlighted the value of these pamphlets as a supplement to the verbal explanations provided by HCPs—as a “reference” and a “reminder”. Although there was recognized value in having the education material in their native language, those with some command of English or French stated that the vocabulary was more critical than the language itself, highlighting that “technical terms” should be avoided, even if translated into their language. If medical vocabulary was necessary, one participant recommended that a bilingual glossary of terms be included allowing them to map the English or French words into their native language. In addition, attention should be devoted to the readability of the material, including the use of visual aids to strengthen comprehension, the literacy level, and design features such as font size.
Sixteen participants discussed the internet or “online medicine”, with half (n = 8) reporting that they relied on it as a source of information. For most participants, the internet was used to overcome language barriers (n = 6), either as a translation tool or to search for disease-specific information in their native language. One patient explained, “On YouTube, when you want to search for something, you can type in the Chinese word for it. Those not using the internet (n = 8) did not have access to a computer/internet or did not know how to use this technology. Of note, among nonusers, the value of “online medicine” did not go unrecognized.
Discussion
This study explored the health information needs of CALD patients, the extent to which these were met/unmet, how information was accessed and understood, and their opinions regarding translated patient education materials. Information needs of CALD patients were more nuanced than a list of topics desired by patients, and were characterized by information wants, challenges in accessing and understanding information, and the extent to which an illness was perceived as challenging. This finding is consistent with prior research (Nicholas & Herman, 2009) demonstrating that “information needs” are often used when in fact they are “information wants [which] are what an individual would like to have” (p. 19). Many individuals have “dormant” or “unrecognized needs,” as they might not be aware of the information desired until they are exposed to it (Nicholas & Herman, 2009, p. 19). This issue was most apparent in the case of psychosocial needs in our study. Therefore, it is important to provide information based on information wants but also to include what someone might need or should have to achieve their goals (Nicholas & Herman, 2009). As our data revealed that participants were often unaware of all of their needs, HCPs play an essential role in ensuring that CALD patients complete a needs assessment that includes a range of needs. Studies among CALD communities (Goris et al., 2013; Henderson & Kendall, 2011a) have also proposed the use of community navigators to fulfill this role. These navigators not only perform needs assessments tailored to CALD communities but also respond to patients’ needs by assisting in health promotion, facilitating access to services, and supporting HCPs in accessing translation services and making culturally and linguistically appropriate referrals.
CALD participants in this study were more likely to articulate medical information needs than lifestyle and psychosocial information needs. This finding resonates with data from other studies involving non-CALD and CALD populations with chronic illnesses (Kent et al., 2012; Kwok & White, 2014; Mooney et al., 2014). Non-CALD patients have similarly perceived the role of their HCP as primarily assisting them with medical issues and frequently experienced difficulties in articulating nonmedical issues (Ançel, 2012; janeane et al., 2020). These difficulties are compounded in the CALD population by language and cultural barriers in addition to lower health literacy (Leung et al., 2014; Ng & Omariba, 2010). There is a large body of evidence regarding the benefits of patient-reported outcome (PRO) screening, including facilitating discussions around patients’ supportive care needs and decreased symptom severity (Howell et al., 2015; Jack et al., 2013; Kotronoulas et al., 2014; Skaczkowski et al., 2020). The screening of PRO, using standardized self-administered questionnaires, is undertaken in both CALD and non-CALD populations. However, evidence indicates that there are differences in how CALD patients complete these questionnaires (e.g., family members complete the questionnaire), which might limit the benefits of PRO screening (Skaczkowski et al., 2020).
Our study also unveiled unique culturally specific information needs regarding TCM. Chinese participants emphasized the need for information on TCM as a treatment option and a method to maintain health. TCM is embedded in everyday life for Chinese immigrants who often self-prescribe it in conjunction with Western medicine (Chen et al., 2010). In China, the integration of Western medicine and TCM is commonplace (Wang & Xiong, 2012). Nonetheless, the literature highlights the lack of knowledge related to TCM among HCPs in North America and suggests that they are not well equipped to support these patients (Bertrand, 2012).
CALD participants in our study reported a strong preference for obtaining illness information from their physicians. This reliance on physicians as a source of information is likely to be influenced by cultural norms and health beliefs (Lim et al., 2009), whereby physicians are regarded as having the authoritative knowledge and the main role in the management of the illness (Leung et al., 2014; Piredda et al., 2008). In addition, when physicians were actively engaged in communicating accurate and clear information with patients, they were entrusted with care. This is in line with findings from Henderson and Kendall (2011b) who found that HCPs who use “their knowledge of a client’s culturally-specific health beliefs, values, and alternative treatments to facilitate the medical consultation [. . .] inspire higher levels of trust” (p. 198). This places physicians in a gatekeeper role with substantial responsibility to ensure that CALD patients have all the required information. In a recent meta-analysis of health education interventions for CALD patients, reviewed interventions were most efficacious in increasing CALD patients’ knowledge when they were delivered by HCPs in comparison with lay providers (Lambert et al., 2021).
Family and, to a lesser extent, friends, coworkers, and acquaintances were the most frequently peferred sources for lifestyle and psychosocial information and often acted as interpreters. A recent qualitative study among caregivers of CALD patients also found that family plays a central role in brokering health information (Schaffler et al., 2019). Similarly, a recent meta-analysis suggested that lay providers might be particularly effective in providing culturally adapted lifestyle advice that produces measurable changes in disease markers (Lambert et al., 2021). The preference for different sources of information according to the type of information sought points to a need for alternate models of care, where there might be a partnership between HCPs and potentially community-based bilingual navigators to assist patients in accessing and understanding the information they need (without necessarily having to translate the information). In recent years, several studies have documented the benefits of using such community navigators in improving outcomes for CALD patients, notably increased uptake of health maintenance activities (Goris et al., 2013; Henderson et al., 2011; Henderson & Kendall, 2011a; Lewin et al., 2010). These navigators can help CALD patients navigate the health care system, identify where/who to go to for their unmet needs, and access translation services to further their understanding of information. They also support HCPs in providing care that is compatible with patients’ beliefs.
Practical Implications
This study highlighted a number of communication strategies that clinicians can use to overcome linguistic barriers with CALD patients, beyond providing translated education materials. Many of these can be distilled to known effective health education strategies (e.g., use of visual aids and models). In addition, given the strong reliance of CALD patients on family members and friends for interpretation, HCPs need to recognize the importance of establishing relations with this support network. Furthermore, culturally relevant needs assessment tools, such as the Patient Assessment of Chronic Illness Care (PACIC; Glasgow et al., 2005; Schmittdiel et al., 2008), could be useful in routine care to identify areas in which CALD patients may have unmet needs. CALD populations may benefit from these needs assessment tools delivered by community navigators that are tailored to address their unique linguistic and cultural health care challenges. Our findings also highlighted the importance of increasing knowledge and understanding of TCM to be integrated into HCP curricula to better address the health information needs of this population. Finally, although not a finding in our study, other studies have cautioned about the fine line between cultural sensitivity and stereotyping whereby generalizations are created about representatives of certain cultural and ethnic groups (Campinha-Bacote, 2018). The recent literature underscores the importance of developing cultural competence along with cultural humility, both at the level of individual HCPs and at the level of health care organization, in the delivery of culturally appropriate and equitable health care (Campinha-Bacote, 2018; Fitzgerald & Campinha-Bacote, 2019). A recently developed Intersectionality Approach to Cultural Competemility can help HCPs
to maintain both an attitude and a lens of cultural competence and cultural humility as they engage in cultural encounters, obtain cultural knowledge, demonstrate the cultural skill of conducting a culturally sensitive cultural assessment, and become culturally aware of both their own biases and the presence of “isms” (e.g., racism, sexism, ableism, classism, ageism, anti-Semitism, heterosexism, colorism, ethnocentrism). (Campinha-Bacote, 2018)
Study Limitations
These results need to be interpreted in light of the study’s limitations. First, we interviewed a small number of individuals from a limited number of ethnic groups recruited from clinics in Quebec. In addition, our sample included predominantly elderly patients with low educational attainment. Conclusions regarding each one of these CALD populations need to be interpreted with caution. Second, despite rigorous methods to maintain trustworthiness, cross-lingual research risks compromising conceptual equivalence of participants’ responses, especially in the presence of idioms and phrases that do not have English translations. The analysis of transcripts was conducted in English, and while we acknowledge this as a limitation, this practice is not uncommon and can result in high-quality data (van Nes et al., 2010).
Supplemental Material
Supplemental material, sj-pdf-1-qhr-10.1177_10497323211040769 for Chronic Illness Management in Culturally and Linguistically Diverse Patients: Exploring the Needs, Access, and Understanding of Information by Sylvie Lambert, Ekaterina Loban, Jane Li, Tracy Nghiem, Jamie Schaffler, Christine Maheu, Sylvie Dubois, Nathalie Folch, Elisa Gélinas-Phaneuf and Andréa Maria Laizner in Qualitative Health Research
Supplemental material, sj-pdf-2-qhr-10.1177_10497323211040769 for Chronic Illness Management in Culturally and Linguistically Diverse Patients: Exploring the Needs, Access, and Understanding of Information by Sylvie Lambert, Ekaterina Loban, Jane Li, Tracy Nghiem, Jamie Schaffler, Christine Maheu, Sylvie Dubois, Nathalie Folch, Elisa Gélinas-Phaneuf and Andréa Maria Laizner in Qualitative Health Research
Author Biographies
Sylvie Lambert (RN, PhD) is Associate Professor at the Ingram School of Nursing, McGill University, a Canada Research Chair (Tier 2), and a Principal Investigator at the St. Mary’s Research Centre. Her research focuses on self-management interventions, cultural adaptation of evidence-based interventions, and patient-reported outcomes (including psychometrics).
Ekaterina Loban (MA, LLM) is a doctoral candidate in the Department of Family Medicine at McGill University. Areas of research interest include multi-stakeholder partnerships, the organizational aspects of primary health care and medical law and ethics.
Jane Li (RN, MSc(A)) is a Nurse Practitioner in the Complex Malignant Hematology Program at the Princess Margaret Cancer Centre in Toronto, Ontario. Jane received her Master of Science in Nursing degree from McGill University, during which her research project focused on studying the information needs of culturally and linguistically diverse patients in managing chronic illnesses.
Tracy Nghiem (RN, MSc (A)) is a Nurse Practitioner candidate at the Ingram School of Nursing at McGill University. Areas of research interest include access to health care, self-management of chronic illnesses, and mHealth.
Jamie Schaffler (RN, MSc(A)) is a Master’s trained registered nurse with experience working in internal and emergency medicine. Her research interests include working with vulnerable populations such as culturally and linguistically diverse groups, those who face health inequalities, and socially and economically disadvantaged persons.
Christine Maheu (RN, PhD) is an Associate Professor at the Ingram School of Nursing, McGill University. Areas of research include cancer survivorship and transition, cancer and work, and clinical trials in fear of cancer recurrence.
Sylvie Dubois (RN, PhD) is an Associate Professor and the Dean at the Faculty of Nursing, University of Montreal. Areas of research include oncology, management, and nurses and patients education.
Nathalie Folch (PhD, kinesiologist) is Assistant Director - Research, Partnership and Management, at Nursing Directorate of the University of Montreal Hospital Center (CHUM) - Montreal, Canada, and researcher at the CHUM Research Centre. Her research focuses on nursing research, patient partnership, oncology and project management.
Élisa Gélinas-Phaneuf (RN, MSc) is the Head of Specialized Nursing Service – Development of nursing practice and professional skills at Integrated Health and Social Services of Central Monteregie. Areas of research include chronic illness management, nursing research and patient partnerships.
Andréa Maria Laizner (RN, PhD) is an Associate Investigator in the Cancer Research Program of the Research Institute of the McGill University Health Centre and Assistant Professor at the Ingram School of Nursing, McGill University. Her research focuses on care of patients and their families in a variety of clinical contexts, including family functioning and psychosocial adjustment in families at diagnosis as well as later in the illness trajectory, such as palliative care.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Réseau de recherche en interventions en sciences infirmières du Québec (RRISIQ). Sylvie Lambert is supported by a Canadian Institutes of Health Research (CIHR) Canada Research Chair.
ORCID iDs: Sylvie Lambert  https://orcid.org/0000-0002-9202-9251
https://orcid.org/0000-0002-9202-9251
Supplemental Material: Supplemental Material for this article is available online at journals.sagepub.com/home/qhr. Please enter the article’s DOI, located at the top right hand corner of this article in the search bar, and click on the file folder icon to view.
References
- Ançel G. (2012). Information needs of cancer patients: A comparison of nurses’ and patients’ perceptions. Journal of Cancer Education, 27(4), 631–640. 10.1007/s13187-012-0416-2 [DOI] [PubMed] [Google Scholar]
- Bertrand S. W. (2012). Registered nurses integrate Traditional Chinese Medicine into the triage process. Qualitative Health Research, 22(2), 263–273. 10.1177/1049732311421681 [DOI] [PubMed] [Google Scholar]
- Betancourt M., Roberts K. C. (2010). Chronic disease patterns for immigrants to Canada: A recent data analysis. Health Research Policy Bulletin, 17, 22–23. [Google Scholar]
- Butow P. N., Bell M. L., Aldridge L. J., Sze M., Eisenbruch M., Jefford M., . . . Psycho-Oncology Co-Operative Research Group (PoCoG) CALD Team. (2013). Unmet needs in immigrant cancer survivors: A cross-sectional population-based study. Supportive Care in Cancer, 21(9), 2509–2520. 10.1007/s00520-013-1819-2 [DOI] [PubMed] [Google Scholar]
- Campinha-Bacote J. (2018). Cultural competemility: A paradigm shift in the cultural competence versus cultural humility debate—Part I. OJIN: The Online Journal of Issues in Nursing, 24(1), 1–10. [Google Scholar]
- Cha E., Yang K., Lee J., Min J., Kim K. H., Dunbar S. B., Jennings B. M. (2012). Understanding cultural issues in the diabetes self-management behaviors of Korean immigrants. The Diabetes Educator, 38(6), 835–844. 10.1177/0145721712460283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. J., Kendall J., Shyu Y. I. (2010). Grabbing the rice straw: Health information seeking in Chinese immigrants in the United States. Clinical Nursing Research, 19(4), 335–353. 10.1177/1054773810372542 [DOI] [PubMed] [Google Scholar]
- De Maio F. G., Kemp E. (2010). The deterioration of health status among immigrants to Canada. Global Public Health, 5(5), 462–478. 10.1080/17441690902942480 [DOI] [PubMed] [Google Scholar]
- Elo S., Kyngäs H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. [DOI] [PubMed] [Google Scholar]
- Finucane M. L., McMullen C. K. (2008). Making diabetes self-management education culturally relevant for Filipino Americans in Hawaii. The Diabetes Educator, 34(5), 841–853. 10.1177/0145721708323098 [DOI] [PubMed] [Google Scholar]
- Fitzgerald E., Campinha-Bacote J. (2019). An intersectionality approach to the process of cultural competemility—Part II. OJIN: The Online Journal of Issues in Nursing, 24(2). [Google Scholar]
- Fuller-Thomson E., Noack A. M., George U. (2011). Health decline among recent immigrants to Canada: Findings from a nationally-representative longitudinal survey. Canadian Journal of Public Health, 102(4), 273–280. 10.1007/bf03404048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow R. E., Wagner E. H., Schaefer J., Mahoney L. D., Reid R. J., Greene S. M. (2005). Development and validation of the patient assessment of chronic illness care (PACIC). Medical Care, 43(5), 436–444. [DOI] [PubMed] [Google Scholar]
- Goris J., Komaric N., Guandalini A., Francis D., Hawes E. (2013). Effectiveness of multicultural health workers in chronic disease prevention and self-management in culturally and linguistically diverse populations: A systematic literature review. Australian Journal of Primary Health, 19(1), 14–37. 10.1071/py11130 [DOI] [PubMed] [Google Scholar]
- Gushulak B. D., Pottie K., Hatcher Roberts J., Torres S., DesMeules M. (2011). Migration and health in Canada: Health in the global village. CMAJ: Canadian Medical Association Journal, 183(12), E952–E958. 10.1503/cmaj.090287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison J. D., Young J. M., Price M. A., Butow P. N., Solomon M. J. (2009). What are the unmet supportive care needs of people with cancer? A systematic review. Supportive Care in Cancer, 17(8), 1117–1128. 10.1007/s00520-009-0615-5 [DOI] [PubMed] [Google Scholar]
- Henderson S., Kendall E. (2011. a). “Community navigators”: Making a difference by promoting health in culturally and linguistically diverse (CALD) communities in Logan, Queensland. Australian Journal of Primary Health, 17(4), 347–354. 10.1071/py11053 [DOI] [PubMed] [Google Scholar]
- Henderson S., Kendall E. (2011. b). Culturally and linguistically diverse peoples’ knowledge of accessibility and utilisation of health services: Exploring the need for improvement in health service delivery. Australian Journal of Primary Health, 17(2), 195–201. 10.1071/py10065 [DOI] [PubMed] [Google Scholar]
- Henderson S., Kendall E., See L. (2011). The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: A systematic literature review. Health & Social Care in the Community, 19(3), 225–249. 10.1111/j.1365-2524.2010.00972.x [DOI] [PubMed] [Google Scholar]
- Hoffman-Goetz L., Donelle L., Ahmed R. (2014). Health literacy in Canada: A primer for students. Canadian Scholars’ Press Inc. [DOI] [PubMed] [Google Scholar]
- Howell D., Molloy S., Wilkinson K., Green E., Orchard K., Wang K., Liberty J. (2015). Patient-reported outcomes in routine cancer clinical practice: A scoping review of use, impact on health outcomes, and implementation factors. Annals of Oncology, 26(9), 1846–1858. 10.1093/annonc/mdv181 [DOI] [PubMed] [Google Scholar]
- Hyman I., Jackson B. (2010). The healthy immigrant effect: A temporary phenomenon? Health Policy Research Bulletin (17), 17-21. Retrieved from https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/sr-sr/pubs/hpr-rpms/bull/2010-health-sante-migr-eng.pdf
- Jack C., Lixin O., Stephanie J. H. (2013). A systematic review of the impact of routine collection of patient reported outcome measures on patients, providers and health organisations in an oncologic setting. BMC Health Services Research, 13(1), Article 211. 10.1186/1472-6963-13-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janeane N., Anderson J., Carolyn G., Krukowski R. A., Schwartzberg L., Vidal G. A., . . . Ilana G. (2020). “Nobody Will Tell You. You’ve Got to Ask!”: An Examination of Patient-provider Communication Needs and Preferences among Black and White Women with Early-stage Breast Cancer. Health Communication, 10.1080/10410236.2020.1751383 [DOI] [PMC free article] [PubMed]
- Kent E. E., Arora N. K., Rowland J. H., Bellizzi K. M., Forsythe L. P., Hamilton A. S., . . . Aziz N. M. (2012). Health information needs and health-related quality of life in a diverse population of long-term cancer survivors. Patient Education and Counseling, 89(2), 345–352. 10.1016/j.pec.2012.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotronoulas G., Kearney N., Maguire R., Harrow A., Di Domenico D., Croy S., MacGillivray S. (2014). What is the value of the routine use of patient-reported outcome measures toward improvement of patient outcomes, processes of care, and health service outcomes in cancer care? A systematic review of controlled trials. Journal of Clinical Oncology, 32(14), 1480–1501. 10.1200/JCO.2013.53.5948 [DOI] [PubMed] [Google Scholar]
- Kwok C., White K. (2014). Perceived information needs and social support of Chinese-Australian breast cancer survivors. Supportive Care in Cancer, 22(10), 2651–2659. 10.1007/s00520-014-2252-x [DOI] [PubMed] [Google Scholar]
- Lambert S. D., Loiselle C. G. (2007). Health information-seeking behavior. Qualitative Health Research, 17(8), 1006–1019. 10.1177/1049732307305199 [DOI] [PubMed] [Google Scholar]
- Lambert S. D., Schaffler J. L., Ould Brahim L., Belzile E., Laizner A. M., Folch N., . . . Ciampi A. (2021). The effect of culturally-adapted health education interventions among culturally and linguistically diverse (CALD) patients with a chronic illness: A meta-analysis and descriptive systematic review. Patient Education and Counseling, 104(7), 1608–1635. 10.1016/j.pec.2021.01.023 [DOI] [PubMed] [Google Scholar]
- Leung A. Y., Bo A., Hsiao H. Y., Wang S. S., Chi I. (2014). Health literacy issues in the care of Chinese American immigrants with diabetes: A qualitative study. BMJ Open, 4(11), Article e005294. 10.1136/bmjopen-2014-005294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin S., Munabi-Babigumira S., Glenton C., Daniels K., Bosch-Capblanch X., van Wyk B. E., . . . Scheel I. B. (2010). Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database of Systematic Reviews, 2010(3), Article CD004015. 10.1002/14651858.CD004015.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim J. W., Gonzalez P., Wang-Letzkus M. F., Ashing-Giwa K. T. (2009). Understanding the cultural health belief model influencing health behaviors and health-related quality of life between Latina and Asian-American breast cancer survivors. Supportive Care in Cancer, 17(9), 1137–1147. 10.1007/s00520-008-0547-5 [DOI] [PubMed] [Google Scholar]
- Lincoln Y. S., Guba E. G. (1985). Naturalistic inquiry. SAGE. [Google Scholar]
- Magilvy J. K., Thomas E. (2009). A first qualitative project: Qualitative descriptive design for novice researchers. Journal for Specialists in Pediatric Nursing, 14(4), 298–300. 10.1111/j.1744-6155.2009.00212.x [DOI] [PubMed] [Google Scholar]
- Marshall E. G., Wong S. T., Haggerty J. L., Levesque J. F. (2010). Perceptions of unmet healthcare needs: What do Punjabi and Chinese-speaking immigrants think? A qualitative study. BMC Health Services Research, 10, Article 46. 10.1186/1472-6963-10-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney J., Spalding N., Poland F., Grayson P., Leduc R., McAlear C. A., . . . Watts R. A. (2014). The informational needs of patients with ANCA-associated vasculitis-development of an informational needs questionnaire. Rheumatology, 53(8), 1414–1421. 10.1093/rheumatology/keu026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray T. S., Hagey J., Willms D., Shillington R., Desjardins R. (2008). Health literacy in Canada: A healthy understanding. Canadian Council on Learning. http://www.en.copian.ca/library/research/ccl/health/health.pdf [Google Scholar]
- Ng E. (2011). The healthy immigrant effect and mortality rates. Health Reports, 22(4), 25–29. [PubMed] [Google Scholar]
- Ng E., Omariba D. W. R. (2010). Health literacy and immigrants in Canada: Determinants and effects on health outcomes. http://en.copian.ca/library/research/ccl/health_lit_immigrants_canada/health_lit_immigrants_canada.pdf
- Nicholas D., Herman E. (2009). Assessing information needs in the age of the digital consumer (3rd ed.). Routledge. [Google Scholar]
- O’Callaghan C., Schofield P., Butow P., Nolte L., Price M., Tsintziras S., . . . Jefford M. (2016). “I might not have cancer if you didn’t mention it”: A qualitative study on information needed by culturally diverse cancer survivors. Supportive Care in Cancer, 24(1), 409–418. 10.1007/s00520-015-2811-9 [DOI] [PubMed] [Google Scholar]
- Piredda M., Rocci L., Gualandi R., Petitti T., Vincenzi B., De Marinis M. G. (2008). Survey on learning needs and preferred sources of information to meet these needs in Italian oncology patients receiving chemotherapy. European Journal of Oncology Nursing, 12(2), 120–126. 10.1016/j.ejon.2007.10.004 [DOI] [PubMed] [Google Scholar]
- Polit D. F., Beck C. T. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th ed.). Wolters Kluwer Health. [Google Scholar]
- Ridpath J. R., Larson E. B., Greene S. M. (2012). Can integrating health literacy into the patient-centered medical home help us weather the perfect storm? Journal of General Internal Medicine, 27(5), 588–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. (1995). Qualitative analysis: What it is and how to begin. Research in Nursing & Health, 18(4), 371–375. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. (2000). Focus on research methods—Whatever happened to qualitative description? Research in Nursing & Health, 23(4), 334–340. [DOI] [PubMed] [Google Scholar]
- Sandelowski M., Barroso J. (2003). Classifying the findings in qualitative studies. Qualitative Health Research, 13(7), 905–923. [DOI] [PubMed] [Google Scholar]
- Schaffler J. L., Tremblay S., Laizner A. M., Lambert S. (2019). Developing education materials for caregivers of culturally and linguistically diverse patients: Insights from a qualitative analysis of caregivers’ needs, access and understanding of information. Health Expectations, 22(3), 444–456. 10.1111/hex.12867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmittdiel J., Mosen D. M., Glasgow R. E., Hibbard J., Remmers C., Bellows J. (2008). Patient assessment of chronic illness care (PACIC) and improved patient-centered outcomes for chronic conditions. Journal of General Internal Medicine, 23(1), 77–80. 10.1007/s11606-007-0452-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw J., Zou X., Butow P. (2015). Treatment decision making experiences of migrant cancer patients and their families in Australia. Patient Education and Counseling, 98(6), 742–747. 10.1016/j.pec.2015.01.012 [DOI] [PubMed] [Google Scholar]
- Shenton A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22(2), 63–75. [Google Scholar]
- Simich L. (2009). Health literacy and immigrant populations. Public Health Agency of Canada. https://pdfs.semanticscholar.org/ebce/08b55090a75c701e73b91e51505a9d9f4899.pdf [Google Scholar]
- Skaczkowski G., Pejoski N., Kaur J., White V., Livingston P. M., Wilson C. (2020). Distress and problem assessment among people living with cancer from culturally and linguistically diverse backgrounds. Psycho-Oncology, 29(10), 1662–1669. 10.1002/pon.5503 [DOI] [PubMed] [Google Scholar]
- Squires A. (2008). Language barriers and qualitative nursing research: Methodological considerations. International Nursing Review, 55(3), 265–273. 10.1111/j.1466-7657.2008.00652.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires A. (2009). Methodological challenges in cross-language qualitative research: A research review. International Journal of Nursing Studies, 46(2), 277–287. 10.1016/j.ijnurstu.2008.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. (2011). Immigration and ethnocultural diversity in Canada: National household survey 2011. https://www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-010-x/99-010-x2011001-eng.pdf
- Statistics Canada. (2012). Focus on geography series, 2011 census. https://www12.statcan.gc.ca/census-recensement/2011/as-sa/fogs-spg/Index-eng.cfm
- Statistics Canada. (2017). Immigration and ethnocultural diversity: Key results from the 2016 census. https://www150.statcan.gc.ca/n1/daily-quotidien/171025/dq171025b-eng.htm
- Tong A., Sainsbury P., Craig J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. [DOI] [PubMed] [Google Scholar]
- van Nes F., Abma T., Jonsson H., Deeg D. (2010). Language differences in qualitative research: Is meaning lost in translation? European Journal of Ageing, 7(4), 313–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visram H. (2013). Patient barriers to insulin use in multi-ethnic populations. Canadian Journal of Diabetes, 37(3), 202–204. 10.1016/j.jcjd.2013.02.054 [DOI] [PubMed] [Google Scholar]
- Wang J., Xiong X. (2012). Current situation and perspectives of clinical study in integrative medicine in China. Evidence-Based Complementary and Alternative Medicine, 2012, Article 268542. 10.1155/2012/268542 [DOI] [PMC free article] [PubMed]
- Zanchetta M. S., Kaszap M., Mohamed M., Racine L., Maheu C., Masny D., . . . Kinslikh D. (2013). Construction of francophone families health literacy in a linguistic-minority situation. Alterstice-Revue Internationale de la Recherche Interculturelle, 2, 47–62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-qhr-10.1177_10497323211040769 for Chronic Illness Management in Culturally and Linguistically Diverse Patients: Exploring the Needs, Access, and Understanding of Information by Sylvie Lambert, Ekaterina Loban, Jane Li, Tracy Nghiem, Jamie Schaffler, Christine Maheu, Sylvie Dubois, Nathalie Folch, Elisa Gélinas-Phaneuf and Andréa Maria Laizner in Qualitative Health Research
Supplemental material, sj-pdf-2-qhr-10.1177_10497323211040769 for Chronic Illness Management in Culturally and Linguistically Diverse Patients: Exploring the Needs, Access, and Understanding of Information by Sylvie Lambert, Ekaterina Loban, Jane Li, Tracy Nghiem, Jamie Schaffler, Christine Maheu, Sylvie Dubois, Nathalie Folch, Elisa Gélinas-Phaneuf and Andréa Maria Laizner in Qualitative Health Research