Abstract
Stigma is a fundamental cause of health inequities. As such, stigma is a major barrier to HIV prevention, care, and treatment. This review will examine the concept of stigma, explicating the mechanisms of action of HIV-related stigma while also examining intersectional stigma and structural stigma. Instruments to measure HIV-related stigma and its mechanisms of action, as well as stigma enacted and experienced by HIV health care providers, will also be reviewed. This article will conclude with a review of stigma interventions, gaps in the literature, and priorities for future HIV, intersectional, and structural stigma research.
Keywords: HIV, intersectionality, review, stigma, structural stigma
Stigma is a fundamental cause of health inequities (Hatzenbuehler et al., 2013). Around the world, the lives of people living with HIV (PLWH) are often afflicted by stigma. In June 2006, the United Nations General Assembly, through its Political Declaration on HIV/AIDS (resolution 60/162), declared that tackling stigma is “a critical element in combating the global HIV/AIDS pandemic” (United Nations General Assembly, 2006, p. 2). In 2010, the National HIV/AIDS Strategy for the United States declared that ending stigma “is a critical component of curtailing the epidemic” (The White House Office of National AIDS Policy, 2010, p. 36).
Whether in the rural United States, sub-Saharan Africa, or elsewhere around the world, the stigma associated with HIV is a barrier to prevention, care, and treatment. HIV-related stigma is linked with individuals not knowing their HIV status; hesitancy or inability to disclose one’s status to family members, friends, sexual partners, and health care providers; delayed care seeking behaviors or nonengagement in care entirely; deferred antiretroviral therapy (ART) initiation and nonadherence; mental health problems, including depression and anxiety; and a diminished quality of life.
Throughout history, infectious diseases, and those affected by them, have been stigmatized. The HIV pandemic is no exception. This review will examine the concept of stigma, explicating the mechanisms of action of HIV-related stigma, while also examining intersectional stigma and structural stigma. Instruments to measure HIV-related stigma and its mechanisms of action, as well as stigma enacted and experienced by HIV health care providers, will also be reviewed. This article will conclude with a review of stigma interventions, gaps in the literature, and priorities for future HIV, intersectional, and structural stigma research.
Stigma
Before critically examining the construct of stigma, it is essential to recognize that stigma and discrimination are two unique phenomena. According to Hatzenbuehler et al. (2013), “stigma is defined as the co-occurrence of labeling, stereotyping, separation, status loss, and discrimination in a context in which power is exercised” (p. 813). “Discrimination—both at the individual level (i.e., the unequal treatment that arises from membership in a particular social group) and at the structural level (i.e., societal conditions that constrain an individual’s opportunities, resources, and well-being)—is a constitutive feature of stigma” (p. 813) Thus, stigma’s mechanisms of action incorporate elements, such as labeling and stereotyping, which are larger than discrimination (Phelan et al., 2008).
Much of the understanding of stigma emanates from the early work of Erving Goffman (Earnshaw & Chaudoir, 2009). In his 1963 book, Stigma: Notes on the Management of Spoiled Identity, Goffman linked stigma to “an attribute that is deeply discrediting” (Goffman, 1963, p. 3). Additionally, he recognized stigma as a social phenomenon that occurs when a person is evaluated as having an undesirable trait, attribute, or behavior and is subsequently deemed imperfect by societal standards. This devaluation or discrediting includes “tribal stigmas” (p. 4) linked to race, ethnicity, and religion; “physical deformities” (p. 4) including blindness, deafness, and the consequences of infectious diseases, like leprosy and smallpox; and “blemishes of individual character” (p. 4) including addiction, homosexuality, and mental illness (Goffman, 1963).
In 2001, Link and Phelan (2001) conceptualized stigma to occur when interrelated mechanisms—labeling, stereotyping, separation, status loss, and discrimination—converge. In this conceptualization, people are first labeled when differences are recognized. Next, the dominant culture connects the labeled person to an undesirable characteristic or negative stereotype. Then, labeled persons are placed in distinct categories to separate the “us” from “them.” Subsequently, labeled persons experience a loss of status and discrimination, producing inequities.
Finally, stigmatization is entirely contingent on access to social, economic, and political power that allows the identification of differentness, the construction of stereotypes, the separation of labeled persons into distinct categories, and the full execution of disapproval, rejection, exclusion, and discrimination (Link & Phelan, 2001, p. 367).
According to Hatzenbuehler et al. (2013), stigma is a fundamental cause of health inequities via various mechanisms (please refer to Figure 1). First, stigma reduces the availability of resources—money, power, prestige, and beneficial social connections. Second, social isolation as a mechanism to avoid stigma in turns diminishes social support. Third, to cope with the stigma, maladaptive coping behaviors (e.g., smoking, alcohol consumption, substance use) may further exacerbate the risk for other poorer health outcomes. Finally, stress—both physiologic and psychologic—plays an important role in the processes associated with stigma (Hatzenbuehler et al., 2013). As a result of stigma, individuals who are stigmatized experience stress as a result of their social position. Both external stressors (i.e., violence, discrimination, implicit bias, microaggressions) and internal stressors (i.e., anticipating rejection, self-stigmatization) are potent mediators of health outcomes. “In sum, stigma appears to have a corrosive influence on health” (Hatzenbuehler et al., 2013, p. 816).
Figure 1.
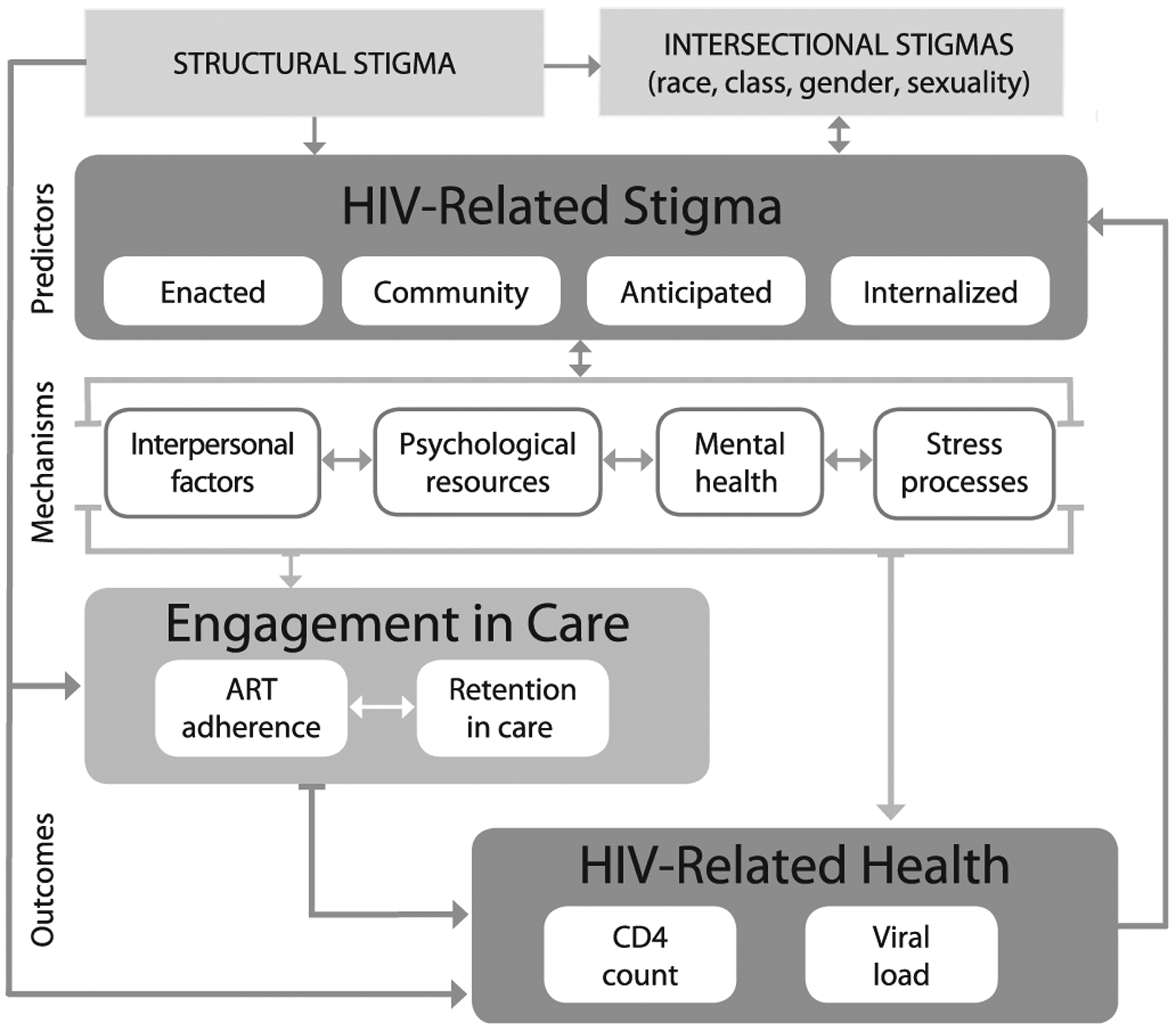
Conceptual framework for HIV-related stigma, engagement in care, and health outcomes. Note. Reprinted with permission. Turan, B., Hatcher, A. M., Weiser, S. D., Johnson, M. O., Rice, W. S., & Turan, J. M. (2017). Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American Journal of Public Health, 107(6), 863–869. doi: 10.2105/AJPH.2017.303744 The Sheridan Press.
In the context of HIV, stigma has numerous mechanisms of action (Turan et al., 2017). For example, enacted stigma is the discrimination, discounting, discrediting, devaluation, stereotyping, and/or prejudice by others because of one’s HIV status (Herek, 1999). Anticipated stigma relates to the concerns an individual living with HIV has about discrimination or adverse events that might happen should one’s HIV status become known by others (Earnshaw et al.,2013). Perceived, sometimes referred to as community, stigma is associated with a PLWH’s perception of the existence and severity of stigmatizing attitudes in the community (Derlage et al., 2002). Internalized stigma associated with HIV is a PLWH’s endorsement and acceptance of negative assumptions about their character because they have HIV; it includes self-deprecating feelings and cognitions, such as shame, self-blame, and embarrassment, and it is associated with the assimilation of these negative attitudes, beliefs, and feelings associated with self, threatening self-concept and self-esteem (Kalichman et al., 2009; Relf et al., 2015; Sayles et al., 2008). Table 1 provides the definitions associated with the various forms of HIV-related stigma.
Table 1.
Definitions of the Various Forms of HIV-Related Stigma
| Type of Stigma | Definition |
|---|---|
| HIV-related stigma | |
| Enacted or experienced (Herek, 1999) | Directly experienced by an individual |
| Manifested as discrimination, discounting, discrediting, devaluation, stereotyping, and/or prejudice by others because of one’s HIV status | |
| Perceived or community (Derlage et al., 2002) | A PLWH’s perceptions of the existence and severity of stigmatizing attitudes in the community |
| How much an individual believes that the public stigmatizes someone with HIV | |
| Anticipated (Earnshaw et al., 2013) | An individual’s expectations that others will treat them negatively in future situations because of their HIV status |
| Concerns a PLWH has about discrimination or adverse events that might happen, should one’s HIV status become known by others | |
| Internalized or self (Kalichman et al., 2009; Relf et al., 2015; Sayles et al., 2008) | PLWH’s endorsement and acceptance of negative assumptions about their character because they have HIV |
| Self-deprecating feelings and cognitions, such as shame, self-blame, and embarrassment | |
| When the negative attitudes, beliefs, and feelings associated with HIV are assimilated into self, threatening self-concept and self-esteem | |
| Intersectional stigma (Andersson et al., 2020; Caiola et al., 2014; Guidroz & Berger, 2009; Hankivsky, 2012). | The convergence of multiple stigmatized statuses (i.e., minoritized racial groups, sexual minorities, immigrants) or behaviors (i.e., sex work, substance use) varying as a function of one another with no one social category or behavior taking primacy |
| Structural stigma (Hatzenbuehler & Link, 2014) | The “societal-level conditions, cultural norms, and institutional practices that constrain the opportunities, resources, and wellbeing for stigmatized populations” (p. 2) |
Intersectional Stigma
As the body of knowledge regarding HIV-related stigma has developed, scientists acknowledge that HIV-related stigma is not a unidimensional construct (Relf et al.,2019) and rarely operates in isolation. Rather, the mechanisms of action of HIV-related stigma typically intersect with the multiple cooccurring statuses or positions of the person with HIV to generate some variation of intersectional stigma—for example, a Latinx man with HIV who identifies as gay and is an immigrant, or an African American women with HIV who has a low income and a mental health disability (Bowleg, 2012).
As a framework, intersectionality helps us to understand how multiple social statuses intersect at the micro level of an individual’s experience (e.g., race, gender, sexual orientation, disability, HIV status, and socioeconomic status) with interlocking systems of privilege and oppression at the macro level (e.g., racism, sexism, heterosexism, classism) to produce health inequalities (Bowleg, 2012). Hence, intersectional stigma is the convergence of multiple stigmatized statuses (i.e., minoritized racial groups, sexual minorities, immigrants) or behaviors (i.e., sex work, substance use) varying as a function of one another with no one social category or behavior taking primacy (Andersson et al., 2020; Caiola et al., 2014; Guidroz & Berger, 2009; Hankivsky, 2012).
A foundational tenet of intersectional stigma is that statuses associated with race, class, and gender are socially constructed, contextually grounded in history and geographical location, and only understood within the multilevel power structures in which they reside (Caiola et al., 2014; Guidroz & Berger, 2009; Hankivsky, 2012; Weber, 2006). In recent years, several useful conceptual frameworks have outlined the individual- and population-level mechanisms and consequences of intersectional stigma for HIV prevention and treatment (Birbek et al., 2019; Caiola et al., 2014; Earnshaw et al., 2013; Turan et al., 2017). The many intersectional “isms” and “phobias”—classism (socioeconomic status), heterosexism (homophobia), racism, transphobia (gender identity), xenophobia (prejudice toward people from different countries)—impinge upon a PLWH’s quality of life and well-being.
Structural Stigma
Structural stigma moves beyond the individual and interpersonal levels to the larger, macroand social level (Hatzenbuehler, 2016). As defined by Hatzenbuehler and Link (2014), structural stigma includes the “societal-level conditions, cultural norms, and institutional practices that constrain the opportunities, resources, and wellbeing for stigmatized populations” (p. 2). Structural stigma can be identified through state and national laws, regulations, and policies, as well as organizational policies and procedures, and is rooted in the related concept of institutional racism (Hatzenbuehler, 2016).
According to Nyblade et al. (2019), stigma in health facilities—one form of structural stigma, is widely documented, “ranging from outright denial of care, provision of sub-standard care, physical and verbal abuse, to more subtle forms, such as making certain people wait longer or passing their care off to junior colleagues” (p. 1). Furthermore, the literature also documents the stigma toward PLWH in health care settings by health care workers—another form of structural stigma—as a significant obstacle to care, treatment, and retention in care (Stringer et al., 2016). In a study by Stringer and colleagues in the Deep South (USA; 2016), several factors independently predicted stigmatizing attitudes by health care workers toward PLWH; these factors included Protestant religion, male gender, white race, working in an HIV/STI clinic type, the availability of postexposure prophylaxis (PEP), and perceptions of policy enforcement. Conversely, health care workers also experience stigma and discrimination in working with PLWH. A study by Kohi et al. (2010) conducted in five African countries (Lesotho, Malawi, South Africa, Swaziland [now Eswatini], and Tanzania) documented that HIV stigma experienced by nurses as providers of care for people living with HIV also contributed to their intent to migrate.
In the context of sexual minorities and HIV, structural stigma appears to be more “strongly related to actual enforcement practices of HIV criminalization, rather than to the mere presence or absence of such laws” (Tran et al., 2019, p. e107). In the 38-country European MSM (men who have sex with men) Internet Survey (EMIS), Panchankis et al. (2018) used a combination of laws and policies affecting sexual minorities, as well as a measure of attitudes by citizens of each country, to examine a variety of HIV outcomes. The results of this multinational study identified that MSM residing in countries with higher levels of stigma toward male homosexuality had reduced odds of being diagnosed with HIV and of having fewer partners but increased odds of engaging in sexual risk behaviors, having unmet prevention needs, not using testing services, and not discussing their sexual orientation in testing services. A study in the United States of MSM without HIV (N = 4,098), which adjusted for social- and state-level covariates, found that men who resided in states with lower levels of structural stigma had decreased odds of condomless anal intercourse and increased odds of awareness of PEP and preexposure prophylaxis, having taken PEP or preexposure prophylaxis, and comfort discussing male–male sex with health care providers (Oldenburg et al., 2015).
In recent conceptual work by Turan et al. (2017), structural stigma—“attitudes in societies, practices, structures, services, and laws that work to the disadvantage of minority groups” (p. 864)—was conceptualized to be related to engagement in care (ART adherence, retention), HIV clinical outcomes (CD4+ T-cell count, viral load), and intersectional stigmas. In this model, the various mechanisms of action of HIV-related stigma—enacted or experienced HIV stigma, perceived or community stigma, anticipated stigma, and self or internalized stigma—were related to multiple outcomes, including affective and cognitive functioning, ART adherence, retention in care, and physical health (Figure 1).
Background and Context
In their 1988 book, AIDS: The Burden of History, editors Elizabeth Fee and Daniel Fox placed the emerging AIDS epidemic in a historical context, critically examining issues of exclusion, public needs, private rights, and quarantine through a series of 12 essays. In the essay, AIDS: From Social History to Social Policy (Brandt, 1988, p. 163), Allan Brandt stated, “AIDS makes explicit, as few diseases could, the complex interaction of social, cultural, and biological forces.” The confluence of these forces shaped the domestic and global response that has been present throughout the epidemic.
Forty years since the beginning of the HIV epidemic, in every corner of the world, the intersection of these complex forces frequently manifest as the stigmas associated with HIV, which remain prevalent and problematic as the epidemic enters its fifth decade (Brent, 2016). These stigmas are more than just a sociocultural phenomenon rooted in history, and they thwart prevention efforts (Rueda et al., 2016). They are also deleterious predictors of adherence to antiretroviral (ART) medications (Katz et al., 2013; Rueda et al., 2016; Sweeney & Vanable, 2016), disclosure (Greef et al., 2008; Li et al., 2016; Relf et al., 2019), engagement in care (Rueda et al., 2016), quality of life (Holzemer et al., 2009; Relf et al., 2019; Rueda et al., 2016), and well-being (Lowther et al., 2014; Rueda et al., 2016).
Curiously, stigma is embedded in all our social interactions and our social groups, so that even within stigmatized communities, there is HIV stigma. For example, among communities of gay men, HIV-related stigma exists. In a literature review by Smit et al. (2012), they identified a growing division between gay men living with HIV and gay men without HIV. This division has resulted in a fragmentation within gay communities based on perceived and actual HIV status. A community that was once coalesced around addressing the epidemic and combating its related stigma and discrimination is now experiencing division based on HIV status.
HIV Stigma and American Society
Throughout history, infectious diseases have been feared for their “contagion” (Sontag, 1989). In the early years of the HIV epidemic, the high mortality rate, lack of treatment options, the conservative political environmental, attitudes toward homosexuality, and historical construction of infectious disease created a perfect storm for the stigma associated with HIV and toward PLWH or people living with AIDS (PLWA) to develop in the United States. In a study by Herek et al. (2002), changes in HIV-related stigma in the United States did improve between 1991 and 1999. In this study, as detailed in Table 2, support for coercive policies decreased significantly between 1991, 1997, and 1999—the study’s three data collection points. Regarding negative feelings toward PLWA, there was a decline between 1991 and 1997. Similarly, there were also declines over the years regarding avoidant intentions (Herek et al., 2002). However, in 1999, 1 in four respondents in this national probability household survey conducted in the 48 contiguous United States agreed with the statement, “People who got AIDS through sex or drug use have gotten what they deserve,” whereas nearly one out of two respondents agreed with the statement, “People with AIDS are responsible for their illness” (Herek et al., 2002). These two statements illustrated the assignment of blame linked to persons with HIV.
Table 2.
Changes in Public Attitudes Toward People With AIDS Between 1991 and 1999 in the United States
| 1991 | 1997 | 1999 | |
|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | |
| Support for coercive policies | Response: “agree” or “strongly agree” | ||
| People with AIDS should be legally separated from others to protect the public health | 34.4 (30.4–38.4) | 16.6 (14.6–18.6) | 12.0 (9.5–14.5) |
| The names of people with AIDS should be made available to the public so that others can avoid them | 28.8 (25.0–32.6) | 18.6 (16.5–20.7) | 16.3 (13.5–19.1) |
| People who got AIDS through sex or drug use have gotten what they deserve | 20.3 (16.9–23.7) | 28.1 (25.7–30.5) | 24.8 (21.5–28.1) |
| Most people with AIDS are responsible for their illness | not asked | 53.5 (50.9–56.1) | 48.3 (44.5–52.1) |
| Negative feelings toward people with AIDS | Response: “somewhat” or “very” afraid, disgusted | ||
| Afraid | 34.6 (30.6–38.6) | 20.0 (17.8–22.2) | 20.2 (17.1–23.3) |
| Disgusted | 26.6 (22.8–30.4) | 18.3 (16.2–20.4) | 16.0 (13.2–18.8) |
| Intentions to avoid contact with people with AIDS | Response: % who would avoid people with AIDS in this situation | ||
| Suppose you had a young child who was attending school where one of the students was known to have AIDS | 14.9 (11.8–18.0) | 9.9 (8.3–11.5) | 8.5 (6.4–10.6) |
| Suppose you worked in an office where one of the men working with you developed AIDS | 18.6 (15.3–21.9) | 11.7 (9.9–13.5) | 9.1 (6.9–11.3) |
| Suppose you found out that the owner of the small neighborhood grocery store where you like to shop has AIDS | 45.2 (41.0–49.4) | 32.2 (29.7–34.7) | 29.3 (25.8–32.8) |
Acknowledgement: The data reported in this table are from: Herek, G. M., Capitanio, J. P., & Widaman, K. F. (2002). HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. American Journal of Public Health, 92(3), 371–377, doi: 10.2105/ajph.92.3.371.
In the most recent study identified inthe literature, Pitasi et al. (2018), using a probability-based national sample, identified that stigmatizing attitudes toward PLWH remain in the United States. Overall, 17.5% (95% CI,16.3–18.6) strongly or somewhat agreed with the statement, “I would be afraid to be around a person with HIV/AIDS because I would be worried I could get infected” with men (19.4%, 95% CI = 17.7–21.1), heterosexuals (17.7%, 95% CI = 16.9–18.9), persons with lower levels of education (<high school, 20.8%, 95% CI = 16.6–25.0; high school, 20.15%, 95% CI = 17.9–22.2), and those with lower annual incomes (<$25,000, 19.3%, 95% CI = 16.6–22.1; $25,000–$49,999 = 20.6%, 95% CI = 18.2–23.0) having higher rates of agreement (Pitasi et al., 2018). The US Census region with the highest rates of being afraid to be around a PLWH was the South—the epicenter of the US HIV epidemic—with a rate of 19.9% (95% CI = 18.0–21.9; Pitasi et al., 2018). Similarly, 12.5% (95% CI = 11.6–13.5) strongly or somewhat agreed that “people who have HIV/AIDS have participated in illicit and/or immoral activities” (Pitasi et al., 2018) Again, men, heterosexuals, those with the lowest income level ($<25,000), and respondents from the US South Census region had higher stigmatizing attitudes (Pitasi et al., 2018). Finally, more than one in five respondents (21.1%, 95% CI = 20.0–22.3) agreed that there was a lot of prejudice and discrimination toward PLWH and PLWA in the United States (Pitasi et al., 2018).
Pivotal Events to Address the Stigma Associated with HIV and AIDS
In one of the domestic epicenters of the early AIDS epidemic in the United States, San Francisco, California, the San Francisco General Hospital opened Ward 5B on 25 July 1983. This 12-bed clinical unit was composed of a group of caregivers assembled to confront the emerging AIDS epidemic in San Francisco (San Francisco Public Library, 2003). What they created was a clinical unit committed to “acceptance and compassion at a time when others were calling for isolation and rejection. They saw fellow human beings where others saw only disease and contagion” (San Francisco Public Library, 2003, p. 2); they confronted stigma and discrimination with compassion and acceptance, providing a model for others on how to provide stigma-free care for PLWA.
In 1988, the World Health Organization (WHO) declared December 1 each year as World AIDS Day. This first ever global health day was designated “for people worldwide to unite in the fight against HIV, to show support for people living with HIV, and to commemorate those who have died from an AIDS-related illness” (World AIDS Day, n.d., para. 1). In 1991, a group of visual AIDS artists created a red ribbon as a visual symbol “to demonstrate compassion for people living with HIV and their care givers” (UNAIDS, 2006). According to UNAIDS (2006), “today the Red Ribbon has become an international symbol of solidarity and support for people living with HIV. Wearing a red ribbon is a simple and powerful way to challenge the stigma and prejudice surrounding AIDS” (para. 6).
A decade later, the 2000 International AIDS Conference was held in Durban, South Africa—a geographic location devastated by the epidemics of HIV and AIDS. The theme of this conference, “Break the Silence,” was fraught with political and scientific disputes about South Africa’s President, Thabo Mbeki’s, unwillingness to declare that HIV causes AIDS (e.g., Swarns & Altman, 2000); however, in the moving closing ceremony of this international AIDS conference, Nelson Mandela asked the global community to put aside the political controversy, declaring “We need to break the silence, banish stigma and discrimination, and ensure total inclusiveness within the struggle against AIDS; those who are infected with this terrible disease do not want stigma, they want love” (Mandela, 2000, para. 20). Also, in 2000, for the first time ever, the United Nations Security Council, through Resolution 1308, recognized that HIV and AIDS had “a uniquely devastating impact on all sectors and levels of society” and “…if unchecked, may pose a risk to stability and security” (United Nations Security Council, 2000, p. 1). These pivotal events helped to break the silence surrounding HIV and AIDS and its associated stigma.
Measuring HIV-Related Stigma
In 2000, HIV-related stigma became recognized for its harmful role in the HIV epidemic. Subsequently, HIV-related stigma research accelerated. Initially, there were no psychometrically sound instruments or scales to measure HIV-related stigma. Instead, investigators used proxy measures, such as depression, self-esteem, and anxiety. One of the first and most prominently recognized scales to measure HIV-related stigma in the nursing and HIV literature was developed by Berger et al. (2001). Their instrument, The HIV Stigma Scale, is a 40-item instrument that yields a total HIV-related stigma score and subscores in four domains—personalized stigma, disclosure concerns, negative self-image, and concern with public attitudes toward PLWH. This instrument has been translated into numerous languages, includes a shortened version (Bunn et al., 2007) and has been adapted to specific populations, including Asians living in the United States (Kamitani et al., 2018), Spanish-speaking urban PLWH in Peru (Franke et al., 2010) and Puerto Rico (Jimenez et al., 2010), and youth (Wright et al., 2007); Table 3 provides an overview of these instruments. Over the years, numerous other instruments have been developed to measure internalized stigma (Hernansaiz-Garrido & Alonso-Tapia, 2017; Kalichman et al., 2009; Sayles et al., 2008; Van Rie et al., 2008; Visser et al., 2008); Table 4 provides an overview of these instruments. Recognizing that health systems and health care workers also create stigmatizing experiences, several instruments have been developed that relate to this type of stigma (Nyblade et al., 2013; Preston et al., 1995; Rutledge et al., 2011; Uys et al., 2009; Wagner et al., 2014); Table 5 provides an overview of these instruments.
Table 3.
Overview of Instruments to Measure HIV-Related Stigma Among People Living With HIV
| Author/Year | Stigma Domains | Instrument Properties |
|---|---|---|
| Berger et al., 2001 | Enacted Internalized Perceived |
40 items, 4-point Likert Languages: Amharic, Bahasa, Chinese, English, Japanese, Polish, Portuguese, Spanish, Swedish, Tamil, Thai Subscales: personalized stigma (18 items); disclosure concerns (8 items); negative self-image (8 items); concern with public attitudes (8 items) |
|
Bunn et al., 2007 Adapted version of Berger et al., 2001 |
Enacted Internalized Perceived |
32 items, 4-point Likert Language: English Subscales: enacted stigma (11 items); disclosure concerns (8 items); negative self-image (7 items); concern with public attitudes (6 items) |
|
Wright et al., 2007 Adapted version of Berger et al., 2001 |
Enacted Internalized Perceived |
10 items, 5-point Likert Population: Youth living with HIV Subscales: personalized stigma (3 items); disclosure (2 items); negative self-image (3 items); public attitudes (2 items) |
|
Kamitani et al., 2018 Adapted version of Wright et al., 2007 |
Enacted Internalized Perceived |
13 items Asian persons living with HIV in the United States Subscales: personalized stigma/disclosure (7 items); negative self-image (3 items); public attitudes (3 items) |
|
Franke et al., 2010 Adapted version of Berger et al., 2001 |
Enacted Internalized Perceived |
21 items, 4-point Likert Population: Spanish speaking, urban PLWH in Peru Subscales: enacted stigma (5 items); disclosure concerns (5 items); negative self-image (6 items); concern with public attitudes (5 items) |
|
Jimenez et al., 2010 Adapted version of Berger et al., 2001 |
Enacted Internalized Perceived |
17 items, 4-point Likert Spanish speaking, Latinx PLWH in Puerto Rico Subscales: personalized stigma (5 items); disclosure concerns (4 items); negative self-image (5 items); concern with public attitudes (3 items) |
| Holzemeret al., 2007 | Enacted Internalized |
33 items, 4-point Likert Languages: Afrikaans, Chichewa, IsiZulu, Sesotho, Seswati, Setswana, Swahili Subscales: verbal abuse (8 items); negative self-perception (5 items); health care neglect (7 items); social isolation (5 items); fear of contagion (6 items); workplace stigma (2 items) |
| Friedland et al., 2020; Global Network of People Living with HIV (GNP+), 2008 | Name of tool: People Living with HIV Stigma Index and the People Living with HIV Stigma Index 2.0 Designed for PLWH to administer the interview to PLWH Available in 55 languages and has been administered in more than 100 countries Domains of the People Living with HIV Stigma Index 2.0: disclosure, experience with stigma and discrimination, internalized stigma and resilience, interactions with health services, human rights and effect change, stigma and discrimination experienced for reasons other than HIV, personal experience related to stigma and discrimination |
Resources: Stevelink et al., 2012; Earnshaw & Chaudoir, 2009.
Note. PLWH = persons Living with HIV.
Table 4.
Overview of Instruments to Measure Internalized HIV-Related Stigma Among People Living With HIV
| Author/Year | Stigma Domains | Instrument Properties |
|---|---|---|
| Kalichman et al., 2009 | Internalized | 12 items, dichotomous Languages: Afrikaans, English, Swati, Xhosa |
| Sayles et al., 2008 | Internalized | 28 items, 5-point Likert Languages: English, Kinyarwanda, Swahili Subscales: Stereotypes (12 items); disclosure concerns (5 items); social relationships (6 items); self-acceptance (4 items) |
| Visser et al., 2008 | Internalized | 6 items, dichotomous Languages: IsiZulu, English, Sepedi, Setswana |
| Van Rie et al., 2008 | Internalized | 21 items, 4-point Likert Languages: English, Malayu, Thai Subscales: Community perspective toward HIV/AIDS (11 items); patient perspective toward HIV/AIDS (10 items) |
Resources: Stevelink et al., 2012; Earnshaw & Chaudoir, 2009.
Table 5.
Overview of Instruments to Measure Stigma Among Nurses and Health Care Workers
| Author/Year | Stigma Domains | Instrument Properties |
|---|---|---|
| Nyblade et al., 2013 | Drivers Enacted Stigma toward pregnant WLWH |
18 core questions |
| Languages: Arabic, Chinese, English, Spanish, Swahili | ||
| Domains | ||
| Drivers: health facilities policies and work environment (7 items); fear (1 item); attitudes toward PLWH (1 item); shame (1 item); willingness to treat key populations (1 item) | ||
| Enacted: observed (1 item); extra infection precautions (1 item); secondary stigma (1 item) | ||
| Stigma toward pregnant women living with HIV among facility staff who care for pregnant women: fear (1 item); opinions (1 item); observed (1 item) | ||
| Supplemental scale: attitudes toward PLWH (5 items) | ||
| Preston et al., 1995 | Name of tool | |
| 21 items | ||
| Domains | ||
| Attitudes about people with HIV subscale (1 item) | ||
| Attitudes about nursing care concerns (12 items) | ||
| Attitudes about social–professional concerns (8 items) | ||
| Rutledge et al., 2011 | Awareness Acceptance Action |
Name of tool: The HIV/AIDS Provider Stigma Inventory |
| 81 items, 7-point Likert | ||
| Domains | ||
| Awareness: Global (42 items) | ||
| Label (12 items) | ||
| Associate (4 items), transmit (4 items), censure (4 items) | ||
| Stereotype (19 items) | ||
| Gay (4 items), injection drug use (8 items), many sex partners (7 items) | ||
| Outgroup (5 items) | ||
| Discriminate (6 items) | ||
| Transmit (3 items), censure (3 items) | ||
| Acceptance: global (20 items) | ||
| Label (4 items) | ||
| Stereotype (6 items) | ||
| Outgroup (4 items) | ||
| Discriminate (6 items) | ||
| Action: global (19 items) | ||
| Uys et al., 2009 | Nurses stigmatizing patients Nurses being stigmatized | Name of Tool: HIV/AIDS Stigma Instrument—Nurse (HASI-N) |
| 19 items | ||
| Domains | ||
| Nurses stigmatizing patients (10 items) | ||
| Nurses being stigmatized (9 items) | ||
| Wagner et al., 2014 | Name of Tool: Health Care Provider HIV/AIDS Stigma Scale (HPASS) | |
| 30 items | ||
| Domains | ||
| Prejudice subscale (13 items) | ||
| Stereotypes subscale (11 items) | ||
| Discrimination subscale (6 items) |
Resources: Stevelink et al., 2012; Earnshaw & Chaudoir, 2009.
Note. PLWH = people living with HIV; WLWH – women living with HIV.
Interventions to Address HIV-Related Stigma
The Cost of HIV-Related Stigma
In 2016, Robert Brent established a methodology to assign an economic value to the benefits associated with HIV stigma reduction interventions and programs. Using data from the Research on Older Adults with HIV study, conducted in New York City, HIV-related stigma was measured using the HIV-Stigma Scale (Berger et al., 2001), which has a range of 40 (no/lowest level of stigma) to 160 (highest level of stigma). In his model, the direct effect of reducing the score by one point on the HIV Stigma Scale was valued at 854 USD. When considering the direct and indirect effects, the value of lowering the stigma score by one point equated to 1,104 USD (Berger et al., 2001). If an intervention were to eliminate stigma in a single PLWH scoring at the highest level on the Berger scale (moving from a score of 160 to 40), the associated cost savings would be 132,480 USD. Although economic consideration should not be the sole focus of any stigma reduction intervention or program, it is an important consideration that has been frequently overlooked.
Overview of HIV-Related Stigma Interventions
During the past two decades, numerous reviews (systematic reviews, scoping reviews, literature reviews) have examined HIV stigma reduction interventions (Brown et al., 2003; Dunbar et al., 2020; Ingram et al., 2019; Kane et al., 2019; Kemp et al., 2019; Ma et al., 2019; Mahajan et al., 2008; Mak et al., 2017; Pantelic et al., 2019; Rao et al., 2019; Reif et al., 2015; Sengupta et al., 2011; Stangl et al., 2013). Overall, the types of HIV stigma reduction interventions highlighted in these reviews can be categorized as individual-level interventions, health care professional interventions, group-level interventions, and multilevel interventions (Reif et al., 2015). From an ecological perspective, these interventions can be organized as (a) individual level only, (b) at the individual and relational level, (c) at the individual and structural level, and (d) at the structural level only (Pantelic et al., 2019).
Prior to 2011, only two systematic reviews of HIV-related stigma reduction interventions had been published (Brown et al., 2003; Mahajan et al., 2008), largely reflecting the paucity and quality of intervention studies aimed at reducing HIV-related stigma to that point. In 2011, Sengupta et al. (2011) aimed to build on prior reviews by conducting a systematic review and narrative synthesis of intervention studies that measured pre- and postintervention HIV-related stigma, whether the intervention was aimed at reducing HIV-related stigma, with the hope that by casting a broader net in the literature they might find a larger pool of interventions affecting stigma to review. Two years later, Stangl et al. (2013) published a systematic review and narrative synthesis of interventions of any design aiming to reduce HIV-related stigma and HIV-related discrimination (N = 48), with a novel focus of including the rapidly increasing number of structural and biomedical intervention approaches. Mak et al. (2017) then offered the first and only attempt to date to use a meta-analytic approach, empirically evaluating the effectiveness of HIV-related stigma-reduction interventions (N = 77) and testing moderators that may increase their effectiveness. Thirty-five of the studies meeting the inclusion criteria (N = 77) lacked enough statistical data for meta-analysis; thus, narrative synthesis of those 35 studies was ultimately combined with the 42 studies in the meta-analysis (Mak et al., 2017).
Each of the prior systematic reviews focused broadly on HIV-related stigma reduction interventions but largely emphasized public stigma-reduction efforts (group-level interventions), reflecting the literature of the time. Mirroring a more recent trend in stigma-reduction interventions, the works of Pantelic et al. (2019) and Ma et al. (2019) shifted the focus toward systematic examination of interventions specifically aimed at reducing self-stigma or internalized stigma in PLWH. Pantelic et al. (2019) further differentiated their focus by only examining self-stigma or internalized stigma interventions (N = 20) implemented in low- and middle-income settings. In the most recent systematic review available at the time of publication, the authors examined stigma-reduction efforts aimed at improving health-related quality of life (HRQoL), the so-called fourth 90 of the UNAIDS 90–90–90 targets for people with HIV, which they argued requires solutions beyond ART and viral suppression (Andersson et al., 2020).
The evolution in specificity and focus of the systematic reviews in the past decade reflects the increased numbers of (Mak et al., 2017) and progression in HIV-related stigma-reduction intervention approaches (Ma et al., 2019; Pantelic et al., 2019). Notable progress had been made in the variety of populations targeted (Mak et al., 2017; Stangl et al., 2013), the expansion of structural and biomedical approaches (Pantelic et al., 2019; Stangl et al., 2013), and a geographical shift in intervention work to include more low- and middle-income countries (Pantelic et al., 2019; Stangl et al., 2013).
According to the work by Dunbar et al. (2020), the mechanistic approach of stigma reduction interventions can be classified into one of three types. First, a mechanism used across some studies focuses on hope and confidence building to move toward self-acceptance. Second, numerous other studies focused on socialization with peers—frequently through support groups or PLWH networks—which allows sharing of experience and acquisition of new knowledge and perspective. Third, community-focused interventions generally concentrate on increasing awareness of stigmatizing language and actions/behaviors.
Structural Stigma Interventions and HIV
Structural interventions modify the environment and influence choice options, helping to influence health behaviors or attitudes (Adimora & Auerbach, 2010; Sipe et al., 2017). According to Adimora and Auerbach (2010), most structural-level interventions have focused on low- and middle-income settings, with little attention given to structural-level interventions in the United States. For example, when examining structural intervention proximally linked to preventing HIV, numerous interventions exist, including comprehensive sexual health education, universal condom availability, expanded syringe access for persons who use drugs, universal health care coverage, and stable housing (Adimora & Auerbach, 2010). Broader, more distally connected, structural interventions associated with HIV prevention and treatment include addressing racial and ethnic disparities in criminal sentencing, the promotion and equitable access to early childhood education, and the elimination or reduction of poverty (Adimora & Auerbach, 2010). When structural interventions for HIV prevention are analyzed, they can essentially be categorized into seven categories—access, policy/procedure, mass media, physical structure, capacity building, community mobilization, and the social determinants of health (Sipe et al., 2017).
Using the HIV prevention structural intervention framework described above, structural-level interventions associated with HIV-related stigma can be aligned with these seven identified categories. For example, decriminalization of HIV laws helps reduce the stigma associated with HIV through policy. Another policy-level structural intervention includes recognizing HIV as a potential disability, which ensures protections under the Americans with Disabilities Act. The Ryan White Care Act is a structural policy-level intervention because it increased access to HIV care and treatment programs, including access to ART. The President’s Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis, and Malaria (commonly referred to as the Global Fund) are global policy-level interventions that initially included community mobilization, capacity building, and expansion of physical structures throughout much of sub-Saharan Africa and high prevalence countries in other regions of the world. The U.S. Department of Housing and Urban Development’s Housing Opportunities for Persons with AIDS program increased access to stable housing through grants to local communities, states, and nonprofit organizations, addressing the social determinants of health through policy.
Recognizing that PLWH frequently live with multiple stigmatizing statuses—being a person of color, being gay or transgender, being poor, being a woman—an intersectional perspective is essential to contextualize the experiences and consequences of living with multiple stigmatized identities (Turan et al., 2019). According to Dunbar et al. (2020), “stigma interventions are more effective when multiple strategies are implemented together to address complex health programmes, such as HIV prevention and care continuum” (p. 721). This assertion was supported in a systematic study of interventions to address self-stigma (internalized stigma) among PLWH by Pantellic et al. (2018); in this systematic review, 13 studies that targeted structural risks, with or without individual-level intervention components, consistently yielded significant reductions in self-stigma; however, most interventions target a single level (individual, health care professional, group) or a single domain of stigma (Stangl et al., 2013). Furthermore, very few stigma intervention studies examined the impact of the intervention on HIV-related outcomes (ART adherence, engagement in care). Unfortunately, in a systematic review of stigma interventions by Sengupta et al. (2011), “only 2 of 14 effective studies were considered good studies, based on quality, the extent to which the intervention focused on reducing HIV/AIDS stigma, and the statistics reported to demonstrate effectiveness” (p. 1075). Overall, most HIV-related stigma research does not use an intersectional, multilevel approach and does not include distal outcomes such as engagement in care, adherence, biomarkers of treatment effectiveness, and quality of life.
As a collective, the reviews highlight some approaches that work. Findings from the combination meta-analysis and systematic review suggested that overall, the stigma-reduction interventions to date, which were largely aimed at reducing public stigma, made small, but significant, effect sizes in the improvement of attitudes toward PLWH (Mak et al., 2017). Interventions with health care providers (sample type), interventions conducted in the community (intervention setting), and interventions with two or more sessions (dosage) all significantly moderated effect sizes in the meta-analysis (Mak et al., 2017). Biomedical (Stangl, et al., 2013) and structural (Pantelic et al., 2019; Stangl et al., 2013) interventions, such as wider availability of ART and economic strengthening, demonstrated effectiveness but were found to be more effective when combined with individual-level strategies to create a multilevel approach (Pantelic et al., 2019). Several individual-level interventions aimed at reducing self-stigma demonstrated effectiveness (Ma et al., 2019; Pantelic et al., 2019), with two nurse-led studies serving as exemplars for demonstrating long-term (≥3 months) effects (Barroso et al., 2014; Miles et al., 2003).
Gaps in the Evidence and Future Priorities
Despite advances in HIV-related stigma-reduction efforts, the systematic reviews of the past decade highlight persistent gaps in the state of evidence. Repeatedly, the reviewers suggested that most of the studies reviewed were of low methodological quality (Andersson et al., 2020; Ma et al., 2019; Mak et al., 2017; Sengupta et al., 2011), citing concerns about study design (Andersson et al., 2020) internal validity (Sengupta et al., 2011), poor randomization techniques (Mak et al., 2017), and the varied use of psychometrically sound outcome measures validated for use and scalable across multiple countries (Mak et al., 2017; Sengupta et al., 2011; Stangl et al., 2013). Only one of the systematic reviews assessing study quality rated that the majority of the studies reviewed were of high quality (Stangl et al., 2013), which may be a reflection of the lack of standardization and variety of tools used by the reviewers to assess study quality.
Consistent calls to action for improved HIV-related stigma-reduction efforts were also noted across the reviews. Sengupta et al. (2011) and Stangl et al. (2013) both called for trials demonstrating public health significance (i.e., influence on health outcomes) beyond stigma reduction. Several reviewers called for interventions targeted at multiple domains (i.e., internalized, anticipated, enacted) of stigma (Mak et al., 2017; Stangl et al., 2013), intersectional stigma (Andersson et al., 2020; Pantelic et al., 2019; Stangl et al., 2013), and multiple socioecological levels of stigma (Stangl et al., 2013), as well as new research methods for effectively evaluating such complexity (Ma et al., 2019; Stangl et al., 2013). Ma et al. (2019) illuminated the largely untapped potential of low-cost technologically delivered interventions, particularly for participants living in remote areas, and suggested that they may enhance study participation in highly stigmatized groups concerned with issues of privacy and confidentiality. Finally, two of the reviews highlighted the need for community engagement in development, implementation, and evaluation of stigma-reduction interventions (Ma et al., 2019; Pantelic et al., 2019), as well as the need for more accountability from academic publishing for reporting such involvement (Pantelic et al., 2019). Finally, other gaps identified in the literature include the absence of theoretical frameworks guiding HIV-related stigma research (Kemp et al., 2019); the lack of stigma intervention research targeting key populations (Pantelic et al., 2019); and issues associated with cost and sustainability (Kemp et al., 2019), as well as scalability of HIV-related stigma interventions.
Specific Priorities for Future HIV-Related Stigma Research
First, HIV-related stigma intervention research needs to use a longitudinal design (Brown et al., 2003; Kane et al., 2019; Reif et al., 2015). Without a longitudinal design, the ability to identify the efficacy of an HIV-related stigma intervention on distal care continuum outcomes (adherence, engagement in care) is limited. In addition, to evaluate an intervention’s durability, a longitudinal design is required. Furthermore, examination of intervention efficacy on biomarkers associated with the care continuum (viral load, CD4+ T-cell count) must account for the known pharmacologic parameters associated with observed changes (3 to 6 months for viral load) and so requires multiple time points to evaluate distal effect.
Second, it is critical that future HIV-related stigma research uses experimental designs (randomized clinicaltrial), or at least a control group of some fashion, in order to determine the efficacy or effectiveness of the intervention (Paudel & Baral, 2015; Rao et al., 2019; Reif et al., 2015). Third, future HIV-related stigma research needs to be sufficiently powered. It is critical for scientists to conduct a power analysis and report these parameters in the peer-reviewed literature (Dunbar et al., 2020; Pantelic et al., 2019; Reif et al., 2015; Sengupta et al., 2011). For studies that do not report the sample size calculations, the risk of a Type II error is increased, making it difficult to determine if a stigma intervention was truly ineffective or if the study was simply underpowered to detect a change in stigma (Pantelic et al., 2019); The fourth area of priority relates to measurement issues (Kemp et al., 2019; Mahajan et al., 2008; Rao et al., 2019; Sengupta et al., 2011; Stangl et al., 2013).Toofrequently, instruments arenotrigorously being adapted across cultures, threatening linguistic relevance and contextual sensitivity and specificity (Rao et al., 2019). Furthermore, the use of standardized, psychometrically established instruments is recommended. The use of a single stigma question or a subsample of selected questions, and not the full instrument, is not recommended because it is difficult to measure the complex constructs of stigma in a single or limited number of items (Sengupta et al., 2011); such an approach increases the risk of measurement error. Further the use of standardized psychometrically established instruments allows evaluation of intervention impact (Stevelink et al., 2012), improves comparability of findings across studies (Kemp et al., 2019), and can help program implementers correctly identify and assist individuals or groups (Earnshaw & Chaudoir, 2009; Mahajan et al., 2008), experiencing heightened stigma. Also related to measurement is the near absence of instruments available to measure intersectional stigma (Mahajan et al., 2008; Pantelic et al., 2019; Rao et al., 2019; Turan et al., 2019).
Fifth, authors need to report, and journal editors need to require, that peer-reviewed articles reporting the results of HIV-related stigma intervention research include detailed, transparent description of the intervention (Kemp et al., 2019) and details about intervention implementation processes (Kemp et al., 2019; Pantelic et al., 2019; Reif et al., 2015), including information about the mode of delivery and dose. Additionally, when HIV-related stigma interventions are adapted across cultures, the details associated with adaptation must be explicated to allow for replicability and to ensure credibility of adaptation.
Policy Implications
In September 2016, the Presidential Advisory Committee on HIV/AIDS (PACHA), subcommittee on Disparities convened a national summit “to create a framework for HIV-related stigma across federal agencies and the wider HIV service community, find ways the federal government can eliminate HIV-related stigma and discrimination, and enhance the resiliency of people living with HIV” (AIDS United, 2016, https://www.aidsunited.org/Blog/Default.aspx?id53481, para 4). In March 2017, PACHA formally released its recommendations from the Stigma Reduction Summit; these recommendations are available at https://files.hiv.gov/s3fs-public/PACHA-Final-Stigma-Reduction-Summit-Recommendations-March-13-2017.pdf. Overall, there were seven areas of focus with a total of 17 specific recommendations. Unfortunately, many of the recommendations have not been implemented because of the change in presidential administrations and a refocusing on Ending the HIV Epidemic.
Conclusions
HIV-related stigma, intersectional stigma, and structural stigma are barriers to HIV prevention, care, and treatment and are inextricably linked to health disparities. Stigma, in all its forms, is rooted in history, culture, language, and context. Over the past decade, as documented in several systematic reviews, stigma interventions are starting to be developed and tested; however, there remain significant gaps in stigma intervention research. Future HIV stigma intervention research should be longitudinal by design, use standardized instruments, and be adapted to the context of the stigma experience.
Key Considerations.
Stigma—a complex phenomenon with many mechanisms of action—is a barrier to HIV prevention, care, and treatment across populations and geographies.
Multilevel interventions appear to have the most impact on improving care and treatment outcomes among people living with HIV.
Future research needs to use more rigorous designs (RCTs, control groups) and follow study participants longitudinally to evaluate the impact of stigma reduction interventions on prevention, care, and treatment outcomes.
Acknowledgments
The study was supported by the Fogarty International Center/National Institutes of Health, through award number R21TW011247 (M. Relf/L. Nyblade, MPIs) and the Duke University Center for AIDS Research (CFAR), an NIH funded program (5P30 AI064518).
Footnotes
Disclosures
The authors report no real or perceived vested interests related to this article that could be construed as a conflict of interest. As with all peer-reviewed manuscripts published in JANAC, this article was reviewed by two impartial reviewers in a double-blind review process. One of JANAC’s associate editors handled the review process for the paper, and the Editor-in-Chief, Michael Relf, and Editorial Assistant, Lauren Holt, had no access to the paper in their roles as editors or reviewers.
References
- Adimora AA, & Auerbach J (2010). Structural interventions for HIV prevention in the United States. Journal of Acquired Immune Deficiency Syndrome, 55, S132–S135. doi: 10.1097/QAI.0b013e3181fbcb38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- AIDS United. (2016). PACHA focuses on stigma reduction. https://www.aidsunited.org/Blog/Default.aspx?id53481
- Andersson GZ, Reinius M, Erikson LE, Svedhem V, Esfahani FM, Deuba K, Rao D, Lyatuu GW, Giovenco D, & Ekstrom AM (2020). Stigma reduction interventions in people living with HIV to improve health-related quality of life. Laboratory Hematology, 7, e129–e140. doi: 10.1016/S2352-3018(19)30343-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso J,Relf M,Williams M,Arscott J,Moore E,Caiola C,&Silva S (2014). A randomized controlled trial of the efficacy of a stigma reduction intervention for HIV-infected women in the Deep South. AIDS Patient Care and STDs, 28, 489–498. doi: 10.1089/apc.2014.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger BE, Ferrans CE, & Lashley FR (2001). Measuring stigma in people with HIV: Psychometric assessment of the HIV stigma scale. Research in Nursing & Health, 24, 518–529. doi: 10.1002/nur.10011 [DOI] [PubMed] [Google Scholar]
- Birbeck GL, Bond V, Earnshaw V, & El-Nasoor ML (2019). Advancing health equity through cross-cutting approaches to health-related stigma. BMC Medicine, 17, 40. doi: 10.1186/s12916-019-1282-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: Intersectionality – an important theoretical framework for public health. American Journal of Public Health, 102, 1267–1273. doi: 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt AM (1988). AIDS: from social history to social policy. In Fee E & Fox DM (Eds.), AIDS: The burden of history. University of California Press. [Google Scholar]
- Brent RJ (2016). The value of reducing stigma. Social Science & Medicine, 151, 233–240. doi: 10.1016/j.socscimed.2016.01.014 [DOI] [PubMed] [Google Scholar]
- Brown L, Macintyre K, & Trujillo L (2003). Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention, 15, 49–69. doi: 10.1521/aeap.15.1.49.23844 [DOI] [PubMed] [Google Scholar]
- Bunn JY, Solomon SE, Millar C, & Forehand R (2007). Measurement of stigma in people with HIV: A re-examination of the HIV Stigma Scale. AIDS Education and Prevention, 19, 198–208. doi: 10.1521/aeap.2007.19.3.198 [DOI] [PubMed] [Google Scholar]
- Caiola C, Docherty SL, Relf M, & Barroso J (2014). Using an intersectional approach to study the impact of social determinants of health for African American mothers living with HIV. ANS. Advances in Nursing Science, 37(4), 287–298. doi: 10.1097/ANS.0000000000000046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derlage VJ, Winstead BA, Greene K, Serovich J, & Elwood WN (2002). Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. Journal of Health Psychology, 2, 415–432. doi: 10.1177/1359105302007004330 [DOI] [PubMed] [Google Scholar]
- Dunbar W, Labat A, Raccurt C, Sohler N, Pape JW, Maulet N, & Coppieters Y (2020). A realist systematic review of stigma reduction interventions for HIV prevention and care continuum outcomes among men who have sex with men. International Journal of STD & AIDS, 31(8), 712–723. doi: 10.1177/0956462420924984 [DOI] [PubMed] [Google Scholar]
- Earnshaw VA & Chaudoir SR (2009). From conceptualizing the measuring stigma: A review of the stigma mechanism measures. AIDS and Behavior, 13, 1160–1177. doi: 10.1007/s10461-009-9593-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, & Copenhaver MM (2013). HIV stigma mechanisms and well-being among PLWH: A test of the HIV stigma framework. AIDS and Behavior, 17, 1785–1795. doi: 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke MF, Muñoz M, Finnegan K, Zeladita J, Sebastian JL, Bayona JN, & Shin SS (2010). Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS and Behavior, 14, 189–199. doi: 10.1007/s10461-008-9474-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedland BA, Gottert A, Hows J, Baral SD, Sprague L, Nyblade L, McClair TL, Anam F, Geibel S, Kentutsi S, Tamoufe U, Diof D, Amenyeiwe U, Malloris C, Pulerwitz J, & PLHIV Stigma2.0 Study Group. (2020). The people living with hiv stigma Index 2.0: generating critical evidence for change worldwide. AIDS, 34 (Suppl. 1), S5–S18. doi: 10.1097/QAD.0000000000002602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Network of People Living with HIV (GNP+). (2008). PLHIV Stigma Index: GNP+. https://www.gnpplus.net/our-solutions/hiv-stigma-index-2/ [Google Scholar]
- Goffman E (1963). Stigma: Notes on the management of spoiled identity. Prentice Hall. [Google Scholar]
- Greef M, Phetlhu R, Makoae LN, Dlamini PS, Holzemer WL, Naidoo JR, Kohi TW, Uys LR, & Chirwa ML (2008). Disclosure of HIV status: Experiences and perceptions of persons living with HIV/AIDS and nurses involved in their care in Africa. Qualitative Health Research, 18, 311–324. doi: 10.1177/1049732307311118 [DOI] [PubMed] [Google Scholar]
- Guidroz K, & Berger MT (2009) A conversation with founding scholars of intersectionality: Kimberle Crenshaw, Nira Yuval-Davis, and Michelle Fine. In Berger MT & Guidroz K (Eds.), The intersectional approach: Transforming the academy through race, class & gender (pp. 45–61). The University of North Carolina Press. [Google Scholar]
- Hankivsky O (2012). Women’s health, men’s health, and gender and health: Implications of intersectionality. Social Science & Medicine, 74, 1712–1720. doi: 10.1016/j.socscimed.2011.11.029 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2016). Structural stigma and health inequalities: Research evidence and implications for psychological science. American Psychologist, 71, 742–751. doi: 10.1037/amp0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, & Link BG (2014). Introduction to the special issue on structural stigma and health. Social Science & Medicine, 103, 1–6. doi: 10.1016/j.socscimed.2013.12.017 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, & Link BG (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103, 813–821. doi: 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM (1999). AIDS and stigma. American Behavioral Scientist, 42, 1106–1116. doi: 10.1177%2F0002764299042007004 [Google Scholar]
- Herek GM, Capitanio JP, & Widaman KF (2002). HIV-related stigma and knowledge in the United States: Prevalence and trends, 1991–1999. American Journal of Public Health, 92, 371–377. doi: 10.2105/ajph.92.3.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernansaiz-Garrido H, & Alonso-Tapia J (2017). Internalized HIV stigma and disclosure concerns: Development and validation of two scales in Spanish-speaking populations. AIDS & Behavior, 21, 93–105. doi: 10.1007/s10461-016-1305-1 [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Human S, Arudo J, Rosa ME, Hamilton MJ, Corless I, Robinson L, Nicholas PK, Wantland DJ, Moezzi S, Willard S, Kirksey K, Portillo C, Sefcik E, Rivero-Mednez M, & Maryland M (2009). Exploring HIV stigma and quality of life for persons living with HIV infection. The Journal of the Association of Nurses in AIDS Care, 20, 161–168. doi: 10.1016/j.jana.2009.02.002 [DOI] [PubMed] [Google Scholar]
- Holzemer WL, Uys LR, Chirwa ML, Greeff M, Makoae LN, Kohi TW, Dlamini PS, Stewart AL, Mullan J, Phetlhu RD, Wantland D, & Durrheim K (2007). Validation of the HIV/AIDS Stigma Instrument—PLWA (HASI-P). AIDS Care, 19, 1002–1012. doi: 10.1080/09540120701245999 [DOI] [PubMed] [Google Scholar]
- Ingram L, Stafford C, Deming ME, Anderson JD, Robillard A, & Li X (2019). A systematic mixed studies review of the intersections of social–ecological factors and HIV stigma in people living with HIV in the U.S. South. The Journal of the Association of Nurses in AIDS Care, 30, 330–343. doi: 10.1097/JNC.0000000000000076 [DOI] [PubMed] [Google Scholar]
- Jimenez JC, Puig M, Ramos JC, Morales M, Asencio G, Sala AC, Castro E, Velez Santori E, Santiago L, & Zorrilla C (2010). Measuring HIV felt stigma: A culturally adapted scale targeting PLWHA in Puerto Rico. AIDS Care, 22, 1314–1322. doi: 10.1080/09540121003758481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta N, & Ginindza T (2009). Measuring AIDS stigmas in people living with HIV/AIDS: The Internalized AIDS-Related Stigma Scale. AIDS Care, 21, 87–93. doi: 10.1080/09540120802032627 [DOI] [PubMed] [Google Scholar]
- Kamitani E, Chen JL, Portillo C, Tokumoto J, & Dawson-Rose C (2018). Shortened and culturally appropriate HIV stigma scale for Asians living with HIV in the United States: Psychometric analysis. The Journal of the Association of Nurses in AIDS Care, 29, 560–569. doi: 10.1016/j.jana.2018.02.007 [DOI] [PubMed] [Google Scholar]
- Kane JC, Elafros MA, Murray SM, Mitchell EMH, Augustinavicius JL, Causevic S, & Baral SD (2019). A scoping review of health-related stigma outcomes for high-burden diseases in low and middle-income countries. BMC Medicine, 17, 17. doi: 10.1186/s12916-019-1250-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, & Tsai AC (2013). Impact of HIV-related stigma on treatment adherence: Systematic review and meta-synthesis. Journal of the International AIDS Society Electronic Resource, 16 (3 Suppl. 2), 18640. doi: 10.7448/IAS.16.3.1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp CG, Jarrett BA, Kwon CS, Song L, Jetté N, Sapag JC, Bass J, Murray L, Rao D, & Baral S (2019). Implementation science and stigma reduction interventions in low- and middle-income countries: A systematic review. BMC Medicine, 17, 6. doi: 10.1186/s12916-018-1237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohi TW, Portillo CJ, Durrheim K, Dlamini PS, Makoae LN, Greeff M, Chirwa M, Naidoo J, Uys LR, & Holzemer WL (2010). Does perceived HIV stigma contribute to nurses’ intent to migrate in five African countries? The Journal of the Association of Nurses in AIDS Care, 21, 134–143. doi: 10.1016/j.jana.2009.09.004 [DOI] [PubMed] [Google Scholar]
- Li H, Li X, Zhang L, & Chow E (2016). Effects of multiple types of stigma on the probability of HIV disclosure to sex partners: A systematic review. Sexual Health, 13(6), 516–529. doi: 10.1071/SH16089 [DOI] [PubMed] [Google Scholar]
- Link BG & Phelan JC (2001). Conceptualizing stigma. Annual Review of Sociology, 27, 363–385. doi: 10.1146/annurev.soc.27.1.363 [DOI] [Google Scholar]
- Lowther K, Selman L, Harding R, & Higginson IJ (2014). Experience of persistent psychological symptoms and perceived stigma among people with HIV on antiretroviral therapy (ART): A systematic review. International Journal of Nursing Studies, 51(8), 1171–1189. doi: 10.1016/j.ijnurstu.2014.01.015 [DOI] [PubMed] [Google Scholar]
- Ma PHX, Chan ZCY, & Loke AY (2019). Self-stigma reduction interventions for people living with HIV/AIDS and their families: A systematic review. AIDS and Behavior, 23(3), 707–741. doi: 10.1007/s10461-018-2304-1 [DOI] [PubMed] [Google Scholar]
- Mahajan AP, Sayles JN, Patel VA, Remien RH, Sawires SR, Ortiz DJ, Szekeres G, & Coates TJ (2008). Stigma in the HIV/AIDS epidemic: A review of the literature and recommendations for the way. AIDS, 22(Suppl. 2), S67–S79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak WWS, Mo PKH, Ma GYK, & Lam MYY (2017). Meta-analysis and systematic review of studies on the effectiveness of HIV stigma reduction programs. Social Science & Medicine, 188, 30–40 [DOI] [PubMed] [Google Scholar]
- Mandela N (2000). Closing Address by Former President Nelson Mandela. XIII International AIDS Conference. Durban, South Africa. https://actupny.org/reports/durban-mandela.html [Google Scholar]
- Miles MS, Holditch-Davis D, Eron J, Black BP, Pedersen C, & Harris DA (2003). An HIV self-care symptom management intervention for African American mothers. Nursing Research, 52, 350–360. doi: 10.1097/00006199-200311000-00002 [DOI] [PubMed] [Google Scholar]
- Nyblade L, Jain A, Benkirane M, Li L, Lohiniva AL, McLean R, Turan JM, Varas-Díaz N, Cintrón-Bou F, Guan J, Kwena Z, & Thomas W (2013). A brief, standardized tool for measuring HIV-related stigma among health facility staff: Results of field testing in China, Dominica, Egypt, Kenya, Puerto Rico and St. Christopher & Nevis. Journal of the International AIDS Society Electronic Resource, 16(3 Suppl. 2), 18718. doi: 10.7448/IAS.16.3.18718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyblade L, Stockton MA, Giger I, Bond V, Ekstrand ML, McLean R, Mitchell EMH, Nelson LE, Sapag JC, Siraprapasiri T, Turan J, & Wouters E (2019). Stigma in health facilities: Why it matters and how we can change it. BMC Medicine, 17, 25. doi: 10.1186/s12916-019-1256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Hatzenbuehler ML, Krakower D, Novak DS, Mimiaga MJ, & Mayer KH (2015). State-level structural sexual stigma and HIV prevention in a national online sample of HIV-uninfected MSM in the United States. AIDS, 29, 837–845. doi: 10.1097/QAD.0000000000000622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panchankis JE, Hatzenbuehler ML, Wang K, Burton CL, Crawford FW, Phelan JC, & Link BG (2018). The burden of stigma on health and well-being: A taxonomy of concealment, course, disruptiveness, aesthetics, origin, and peril across 93 stigmas. Personality & Social Psychology Bulletin, 44(4), 451–474. doi: 10.1177/01461672177413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantelic M, Steinert JI, Park J, Mellors S, & Murau F (2019). ‘Management of a spoiled identity’: Systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Global Health, 4(2), e001285. doi: 10.1136/bmjgh-2018-001285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paudel V, & Baral KP (2015). Women living with HIV/AIDS (WLHA), battling stigma, discrimination and denial and the role of support groups as a coping strategy: A review of literature. Reproductive Health, 12, 53. doi: 10.1186/s12978-015-0032-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, Link BG, & Dovidio JF (2008). Stigma and prejudice: One animal or two? Social Science & Medicine, 67, 358–367. doi: 10.1016/j.socscimed.2008.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitasi MA, Chavez PR, DiNenno EA, Jeffries WL, Johnson CH, Demeke H, August EM, & Bradley H (2018). Stigmatizing attitudes toward people living with HIV among adults and adolescents in the United States. AIDS and Behavior, 22, 3887–3891. doi: 10.1007/s10461-018-2188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston DB, Young EW, Koch PB, & Forti EM (1995). The Nurses’ Attitudes about AIDS Scale (NAAS): Development and psychometric analysis. AIDS Education & Prevention, 7, 443–454 [PubMed] [Google Scholar]
- Rao D, Elshafei A, Nguyen M, Hatzenbuehler ML, Frey S, & Go VF (2019). A systematic review of multi-level stigma interventions: State of the science and future directions. BMC Medicine, 17, 41. doi: 10.1186/s12916-018-1244-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif SS, Wilson S, & Berger M (2015). Interventions to address HIV-related stigma: Literature summary. https://southernaids.files.wordpress.com/2017/08/stigma-reduction-interventionliterature-revised-8-31-17-final1.pdf
- Relf MV, Pan W, Edmonds A, Ramirez C, Amarasekara S, & Adimora AA (2019). Discrimination, medical distrust, stigma, depressive symptoms, antiretroviral medication adherence, engagement in care and quality of life among women living with HIV in North Carolina: A mediated structural equation model. Journal of Acquired Immune Deficiency Syndrome, 81, 328–335. doi: 10.1097/QAI.0000000000002033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relf MV, Williams M, & Barroso J (2015). Voices of women facing HIV-related stigma in the Deep South. Journal of Psychosocial Nursing and Mental Health Services, 53, 38–47. doi: 10.3928/02793695-20151020-01 [DOI] [PubMed] [Google Scholar]
- Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, Wilson M, Logie CH, Shi Q, Morassaei S, & Rourke SB (2016). Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: A series of meta-analyses. BMC Ophthalmology, 6, e011453. doi: 10.1136/bmjopen-2016-011453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutledge S, Whyte J, Abell N, Brown K & Cesnales N (2011). Measuring stigma among health care and social service providers: The HIV/AIDS Provider Stigma Inventory. AIDS Patient Care and STDs, 25, 673–682. doi: 10.1089/apc.2011.0008 [DOI] [PubMed] [Google Scholar]
- San Francisco Public Library, San Francisco History Center, Collection Number SFH12. (2003). San Francisco General Hospital, AIDS Ward 5B/5A Archives, 1983–2003. San Francisco, CA. [Google Scholar]
- Sayles JN, Hays RD, Sarkisian CA, Mahajan AP, Spritzer KL, & Cunningham WE (2008). Development and psychometric assessment of a multidimensional measure of internalized HIV stigma in a sample of HIV-positive adults. AIDS and Behavior, 12(5), 748–758. doi: 10.1007/s10461-008-9375-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta S, Banks B, Jonas D, Miles MS, & Smith GC (2011). HIV interventions to reduce HIV/AIDS stigma: A systematic review. AIDS and Behavior, 15, 1075–1087. doi: 10.1007/s10461-010-9847-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipe TA, Barham TL, Johnson WD, Joseph HA, Tungol-Ashmon ML, & O’Leary A (2017). Structural interventions in HIV prevention: A taxonomy and descriptive systematic review. AIDS and Behavior, 21, 3366–3430. doi: 10.1007/s10461-017-1965-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit PJ, Brady M, Carter M, Fernandes R, Lamore L, Meulbroek M, Ohayon M, Platteau T, Rehberg P, Rockstroh JK, & Thompson M (2012). HIV-related stigma within gay communities: A literature review. AIDS Care, 24, 405–412. doi: 10.1080/09540121.2011.613910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sontag S (1989). AIDS and its metaphors. Farrar, Straus & Giroux. [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, & Baral S (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society Electronic Resource, 16(3 Suppl. 2), 18734. doi: 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevelink SAM, Wu I,C, Voorend CGN, & van Brakel WJ (2012). The psychometric assessment of internalized stigma instruments: A systematic review. Surgical and Radiologic Anatomy, 2. doi: 10.5463/SRA.v1i1,11 [DOI] [Google Scholar]
- Stringer KL, Turan B, McCormick L, Durojaiye M, Nyblade L, Kempg MC, Lichenstein B, & Turan JM (2016). HIV-related stigma among healthcare providers in the Deep South. AIDS and Behavior, 20, 115–125. doi: 10.1007/s10461-015-1256-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swarns RL, & Altman LK (2000). Amid controversy, South Africa opens World AIDS Forum. New York Times. https://archive.nytimes.com/www.nytimes.com/library/world/africa/071000africa-aids.html [Google Scholar]
- Sweeney SM, & Vanable PA (2016). The association of HIV-related stigma to HIV medication adherence: A systematic review and synthesis of the literature. AIDS and Behavior, 20, 29–50. doi: 10.1007/s10461-015-1164-1 [DOI] [PubMed] [Google Scholar]
- The White House Office of National AIDS Policy. (2010). National HIV/AIDS Strategy for the United States. https://obamawhitehouse.archives.gov/sites/default/files/uploads/NHAS.pdf
- Tran NK, Hatzenbuehler ML, & Goldstein ND (2019). Potential relationship netween HIV criminalization and structural stigma related to sexual orientation in the United States. Journal of Acquired Immune DeficiencySyndrome,80,e106–e108.doi: 10.1097/QAI.0000000000001961 [DOI] [PubMed] [Google Scholar]
- Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, & Turan JM (2017). Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. American Journal of Public Health, 107, 863–869. doi: 10.2105/AJPH.2017.303744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Elafros MA, Logie CH, Banik S, Turan B, Crockett KB, Pescosolido B, & Murray SM (2019). Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Medicine, 17, 7. doi: 10.1186/s12916-018-1246-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. (2006). Wear your red ribbon this World AIDS Day. https://www.unaids.org/en/resources/presscentre/featurestories/2006/november/20061130redribbonen
- United Nations General Assembly. (2006). Political Declaration on HIV/AIDS (Resolution 60/262). https://www.unaids.org/sites/default/files/sub_landing/files/20060615_hlm_politicaldeclaration_ares60262_en.pdf [Google Scholar]
- United Nations Security Council. (2000). Resolution 1308. http://unscr.com/en/resolutions/doc/1308
- Uys LR, Holzemer WL, Chirwa ML, Chirwa ML, Dlamini PS, Greeff M, Kohi TW, Makoae LN, Stewart AL, Mullan J, Phetlhu RD, Wantland DJ, Durrheim KL, Cuca YP, & Naidoo JR (2009). The development and validation of the HIV/AIDS Stigma Instrument-Nurse (HASI-N). AIDS Care, 21(2), 150–159. doi: 10.1080/09540120801982889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Rie A, Sengupta S, Pungrassami P, Balthip Q, Choonuan S, Kasetjaroen Y, Strauss RP, & Chongsuvivatwong V (2008). Measuring stigma associated with tuberculosis and HIV/AIDS in southern Thailand: Exploratory and confirmatory factor analyses of two new scales. Tropical Medicine & International Health, 13, 21–30. doi: 10.1111/j.1365-3156.2007.01971.x.19 [DOI] [PubMed] [Google Scholar]
- Visser MJ, Kershaw T, Makin JD, & Forsyth BWC (2008). Development of parallel scales to measure HIV-related stigma. AIDS and Behavior, 12(5), 759–771. doi: 10.1007/s10461-008-9363-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner AC, Hart TA, McShane KE, Margolese S, & Girard TA (2014). Health care provider attitudes and beliefs about people living with HIV: Initial validation of the health care provider HIV/AIDS stigma scale (HPASS). AIDS and Behavior, 18(12), 2397–2408. doi: 10.1007/s10461-014-0834-8 [DOI] [PubMed] [Google Scholar]
- Weber L (2006). Reconstructing the landscape of health disparities research: Promoting dialogue and collaboration between feminist intersectional and biomedical paradigms. In Schulz AJ & Mullings L (Eds.), Gender, race, class & health (pp. 2–59). John Wiley & Sons, Inc. [Google Scholar]
- World AIDS Day. (n.d.). About World AIDS Day. https://www.worldaidsday.org/about/
- Wright K, Naar-King S, Lam P, Templin T, & Frey M (2007). Stigma Scale Revised: Reliability and validity of a brief measure of stigma for HIV+ youth. Journal of Adolescent Health, 40(1), 96–98. doi: 10.1016/j.jadohealth.2006.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]


