ABSTRACT
Aim:
The aim is to study the complications of neonatal thoracotomy and its preventive measures.
Methods:
We retrospectively reviewed 53 neonates who underwent thoracotomy from January 2017 to December 2019 for a period of 3 years. Patient demographic data, primary disease for which they underwent thoracotomy, postoperative complications (immediate and delayed) during follow-up were documented.
Results:
During 3-year period, 53 neonates underwent thoracotomy for various surgical pathologies. The indications were esophageal atresia with tracheoesophageal fistula (n = 49), eventration of diaphragm (n = 3), congenital lobar emphysema of left upper lobe of lung (n = 1). Most of them were right posterolateral thoracotomies (n = 48, 90.56%) and left posterolateral thoracotomy was done in only 5 cases (9.43%). Associated anomalies were seen in 22 cases, such as cardiac (n = 19), renal (n = 4) and gastrointestinal (n = 5). Associated comorbidities seen in 14 cases; preterm (n = 4), low birth weight (n = 13), delayed presentation (n = 6). Early postoperative complications such as pneumonia (34%, n = 18) and wound infection (11.3%, n = 6) were noted. Delayed complications include musculoskeletal abnormalities (n = 19, 35.8%) and esthetic complications such as asymmetry of chest (5.6%).
Conclusion:
Neonatal thoracotomy is associated with complications such as pneumonia, wound infections, and musculoskeletal abnormalities such as asymmetry of chest and scoliosis. These can be prevented by adequate postoperative pain relief, muscle-sparing thoracotomies, avoiding tight closures, and nerve injuries. Long-term follow-up is required because these complications may manifest later on also. Early detection and institution of physiotherapy may help.
KEYWORDS: Esthetic complications, musculoskeletal deformity, neonatal thoracotomy, pneumonia
INTRODUCTION
Neonatal thoracotomy is one of the most commonly performed surgery by pediatric surgeons. Most common indications include esophageal atresia (EA) with tracheoesophageal fistula, congenital diaphragmatic eventration, pulmonary pathologies such as congenital lobar emphysema (CLE), cystic diseases of lung, and duplication cysts. Right posterolateral thoracotomy (PLT) is frequently performed procedure. Division of latissimus dorsi and serratus anterior muscles during the procedure may lead to early complications such as postoperative pain, pneumonia and late complications such as asymmetry of chest, scoliosis, and cosmetic or esthetic complications.[1] Muscle sparing thoracotomies, avoiding nerve injuries, and tight closure of ribs and thorax may help to prevent these complications.
Methods
The current study is a descriptive observational study by retrospective review of medical records from January 2017 to December 2019. All the neonates who underwent thoracotomy were included in the study, and the standard muscle dividing PLT was performed in all cases. Neonates with vertebral anomalies and cardiac surgeries were excluded from the study. Patient demographic data, primary pathology for which they underwent thoracotomy, associated anomalies, comorbidities, and postoperative complications were documented. Minimum follow-up period was 6 months and maximum up to 2 years.
RESULTS
Total 53 patients were included in the study. Indications for thoracotomy were EA (n = 49, 92.45%), eventration of diaphragm (n = 3, 5.66%), and CLE (n = 1, 1.88%). Out of 53, 27 were males and 26 were females. Mean age at thoracotomy was 2.6 days. Associated comorbidities include low birth weight (n = 14, 26.4%), delayed presentation, i.e. after day 3 of life (n = 6, 11.3%) and preterm (n = 4, 7.54%). Associated congenital anomalies noted were cardiac (n = 19, 35.84%), renal (n = 4, 7.54%), and gastrointestinal (n = 5, 9.43%). Majority of the patients underwent right PLT (n = 48, 90.56%) and left PLT was done in 5 patients (9.43%). Two patients underwent repeat thoracotomy because of esophageal anastomotic leak with mediastinitis requiring drainage and lavage. Early complications observed during the study include pneumonia (n = 18, 34%) and wound infection (n = 6, 11.3%). Delayed complications include asymmetry of chest (n = 3, 5.6%) and musculoskeletal abnormalities such as scoliosis/pectus excavatum/pectus carinatum (n = 19, 35.8%) [Figure 1].
Figure 1.
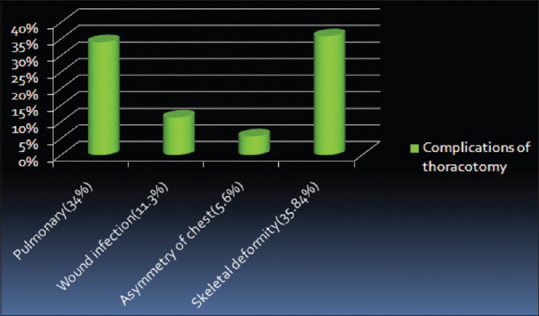
Bar chart showing complications of thoracotomy during the follow-up
DISCUSSION
Incidence of thoracic and spinal deformities following thoracotomy for EA and congenital heart disease has been reported as 18%–50% and after lung resections, it was 38%–76%.[2,3,4] Indications for thoracotomy include EA, eventration of diaphragm, congenital diaphragmatic hernia, congenital esophageal stenosis; pulmonary pathologies such as congenital airway malformations and cystic diseases of lung; duplication cysts, mediastinal tumors, and congenital cardiac diseases such as patent ductus arteriosus and coarctation of aorta.[1] The indications for thoracotomy in our study include EA (n = 49, 92.45%), eventration of diaphragm (n = 3, 5.66%), and CLE (n = 1, 1.88%).
Right PLT is the standard and most frequently performed procedure.[5] According to the study of Turkyilmaz et al., left PLT was associated with more complications.[6] Increased number of thoracotomies increases complications, especially musculoskeletal deformities.[1] In the current study, right posterolateral thoracotomy was done in 48 patients (90.56%) as it is the standard technique and left PLT was done in 5 patients (9.43%).
Complications after thoracotomy can be divided into, musculoskeletal, esthetic and pulmonary complications apart from the individual procedure-related complications. Musculoskeletal deformities include winging of scapula, ipsilateral elevation of shoulder, scoliosis (cobb's angle >10°), pectus excavatum or carinatum, crowding of ribs, rib fusion, and limitation of arm abduction [Figure 2]. Esthetic complications include wound infection, chest asymmetry or asymmetry of level of nipples, fixation of skin cicatrix to bony thorax, maldevelopment of pectoral muscles, and impairment of breast development in females [Figure 3]. Pulmonary complications include pneumonia, atelectasis, effusion, empyema, pneumothorax, mediastinal shift, mediastinitis due to anastomotic leaks in cases of EA, bronchopleural fistula, and recurrent respiratory infections[7,8].
Figure 2.
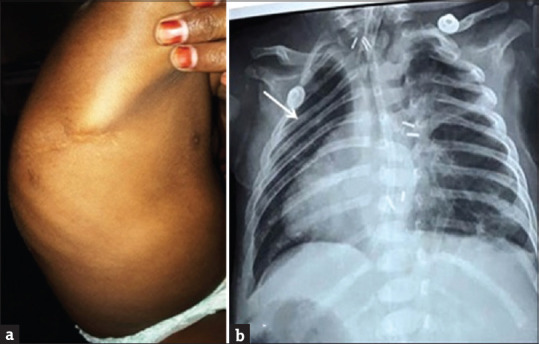
Musculoskeletal deformities – (a) kyphoscoliosis, (b) crowding of ribs, during follow-up after thoracotomy
Figure 3.
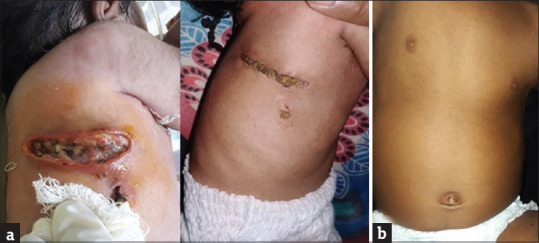
Esthetic complications after thoracotomy; (a) infected thoracotomy wound healed by secondary intension (b) asymmetry of the level of nipples
Musculoskeletal complications
Standard PLT involves division of serratus anterior and latissimus dorsi. These muscles are in the developing stage in neonatal period and injury to these may lead to atrophy of the muscles and musculoskeletal deformities.[2] Fragile neonatal thorax is susceptible for musculoskeletal deformities due to negative intrapleural pressure and dead space after lung resection and pulmonary hypoplasia in cases of congenital diaphragmatic defects.[9] Degree of ossification is lowest during neonatal period which is an independent risk factor.[10] Thoracotomy and neonatal period are also independent risk factors for the development of musculoskeletal deformities. Muscle sparing thoracotomy (MST) and thoracoscopic surgery may help in decreasing these musculoskeletal deformities. According to the study of Burford et al., musculoskeletal deformities after standard PLT were 53.8% whereas it is 9.7% with thoracoscopic surgery.[11] In our study, musculoskeletal abnormalities such as scoliosis/pectus excavatum/pectus carinatum were observed in 19 patients (35.8%) [Figure 2]. Tight chest wall closures and rib resections can also cause musculoskeletal deformities. Periosteal closure also causes rib fusion hence avoided.[12] Most common risk factor for musculoskeletal deformities in our study was tight chest wall closure. None of our patients had rib resections or documented evidence of nerve injury. Most of these deformities are subclinical and do not require active treatment. None of our patients required active treatment as there is no functional deficit. Phrenic nerve injury during thoracotomy causing hemidiaphragmatic paresis was also reported in the literature.[12] Majority of these musculoskeletal deformities develop 3–4 years after thoracotomy, and hence, long-term follow-up is recommended.[13]
Esthetic complications
Cosmesis-related complications are also one of the most common complications after thoracotomy. These include bad scar which can occur if the thoracotomy wound is infected, maldevelopment of pectoral muscles and chest asymmetry or asymmetry at the level of nipples, ipsilateral elevation of shoulder, fixation of skin cicatrix to bony thorax and impairment of breast development in females. In our study, wound infection leading to bad scar was seen in 11.3% of patients [Figure 3a]. These patients were managed with regular dressings and antibiotics, allowing the wound to heal by secondary intention. Chest asymmetry showing abnormality at the level of nipples was observed in 5.6% of our patients during follow-up [Figure 3b]. Anterolateral thoracotomy interferes with ipsilateral breast development because of the chance of injury to the developing breast bud. Posterolateral thoracotomies were associated with musculoskeletal deformities. MST will have smaller incision leading to superior cosmetic results when compared to standard PLT and reduced soft tissue injury causing less postoperative pain.[14] Acute postoperative pain may lead to decline in lung function and reduced shoulder girdle function; return of shoulder function will be earlier in case of MST. The disadvantage with MST is seroma formation.[15]
The incidence of musculoskeletal and esthetic complications can be reduced by MST, thoracoscopic surgery and avoiding tight chest wall closure, periosteal fusion, rib resection, nerve injury (phrenic), and avoiding injury to developing breast bud, especially in anterolateral thoracotomies.
CONCLUSION
Neonatal thoracotomy is associated with complications such as pulmonary, musculoskeletal, and esthetic, apart from the individual procedure-related complications. Adequate postoperative pain relief, frequent position change, and clearance of secretions may help in reducing the pulmonary complications. Thoracoscopic surgeries, muscle-sparing thoracotomies, avoiding nerve injuries, and tight closures may decease muculoskeletal and esthetic complications. Long-term follow-up is needed because these can occur later in life. Early detection and early institution of physiotherapy may decrease long-term complications.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Panda SS, Agarwala S, Bhatnagar V, Kabra SK, Jayaswal A, Bhalla AS. A survey of musculoskeletal and aesthetic abnormalities after thoracotomy in pediatric patients. J Indian Assoc Pediatr Surg. 2013;18:136–42. doi: 10.4103/0971-9261.121113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sistonen SJ, Helenius I, Peltonen J, Sarna S, Rintala RJ, Pakarinen MP. Natural history of spinal anomalies and scoliosis associated with esophageal atresia. Pediatrics. 2009;124:e1198–204. doi: 10.1542/peds.2008-3704. [DOI] [PubMed] [Google Scholar]
- 3.Bal S, Elshershari H, Celiker R, Celiker A. Thoracic sequels after thoracotomies in children with congenital cardiac disease. Cardiol Young. 2003;13:264–7. [PubMed] [Google Scholar]
- 4.Lawal TA, Gosemann JH, Kuebler JF, Glüer S, Ure BM. Thoracoscopy versus thoracotomy improves midterm musculoskeletal status and cosmesis in infants and children. Ann Thorac Surg. 2009;87:224–8. doi: 10.1016/j.athoracsur.2008.08.069. [DOI] [PubMed] [Google Scholar]
- 5.Pinheiro PF, Simões e Silva AC, Pereira RM. Current knowledge on esophageal atresia. World J Gastroenterol. 2012;18:3662–72. doi: 10.3748/wjg.v18.i28.3662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turkyilmaz Z, Sonmez K, Karabulut R. Postoperative outcome of thoracotomy in children. Clin Surg. 2016;1:1086. [Google Scholar]
- 7.Leo F, Venissac N, Pop D, Anziani M, Leon ME, Mouroux J. Anticipating pulmonary complications after thoracotomy: The FLAM Score. J Cardiothorac Surg. 2006;1:34. doi: 10.1186/1749-8090-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bell HE. Neonates and chest surgery. Thorax. 1965;20:1–7. doi: 10.1136/thx.20.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weaver AA, Schoell SL, Stitzel JD. Morphometric analysis of variation in the ribs with age and sex. J Anat. 2014;225:246–61. doi: 10.1111/joa.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaneko K, Ono Y, Tainaka T, Sumida W, Kawai Y, Ando H. Thoracoscopic lobectomy for congenital cystic lung diseases in neonates and small infants. Pediatr Surg Int. 2010;26:361–5. doi: 10.1007/s00383-010-2556-y. [DOI] [PubMed] [Google Scholar]
- 11.Burford JM, Dassinger MS, Copeland DR, Keller JE, Smith SD. Repair of esophageal atresia with tracheoesophageal fistula via thoracotomy: A contemporary series. Am J Surg. 2011;202:203–6. doi: 10.1016/j.amjsurg.2010.09.035. [DOI] [PubMed] [Google Scholar]
- 12.Wei S, Saran N, Emil S. Musculoskeletal deformities following neonatal thoracotomy: Long-term follow-up of an esophageal atresia cohort. J Pediatr Surg. 2017;52:1898–903. doi: 10.1016/j.jpedsurg.2017.08.062. [DOI] [PubMed] [Google Scholar]
- 13.Makita S, Kaneko K, Ono Y, Uchida H. Risk factors for thoracic and spinal deformities following lung resection in neonates, infants, and children. Surg Today. 2017;47:810–4. doi: 10.1007/s00595-016-1434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Askarpour S, Peyvasteh M, Ashrafi A, Dehdashtian M, Malekian A, Aramesh MR. Muscle-sparing versus standard posterolateral thoracotomy in neonates with esophageal atresia. Arq Bras Cir Dig. 2018;31:e1365. doi: 10.1590/0102-672020180001e1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Akcalli Y, Demir H, Tezcan B. The effect of standard postero-lateral versus muscle-sparing thoracotomy on multiple parameters. Ann Thorac Surg. 2003;76:1050–4. doi: 10.1016/s0003-4975(03)00565-4. [DOI] [PubMed] [Google Scholar]


