Abstract
Objectives
Focused research on pediatric agitation is lacking despite being a common mental and behavioral health (MBH) emergency. Prevalence of pediatric agitation remains unknown, and prior reports may have underestimated the rate of restraint use for pediatric agitation. This is the largest study to provide a focused evaluation of the prevalence and predictors of pediatric agitation and restraint use as well as the emergency department (ED) length of stay (LOS) and admission rates for agitated patients.
Methods
We reviewed records of patients aged ≤18 years with MBH needs who visited the pediatric ED of a tertiary care hospital during a 3‐year‐period. We identified and ascertained agitated/aggressive patients using documented signs/symptoms, International Classification of Diseases, Tenth Revision codes, and Behavioral Activity Rating Scale scores. We performed descriptive and multivariable analyses using SAS 9.4 (SAS Institute).
Results
Of 10,172 patients with MBH needs, 1408 (13.8%) were agitated/aggressive. Of these (n = 1408), 63.7% were boys, and the mean age was 11.9 years. Among agitated patients, the prevalence of restraint use was 28.7%, with a predominance of pharmacologic restraint with atypical antipsychotics. Non‐Hispanic Blacks were more likely to be agitated (adjusted odd ratio [aOR], 1.8; 95% CI, 1.2–2.7), but not restrained (aOR, 0.8; 95% CI, 0.3–1.8). Predictors of restraint use include history of attention deficit hyperactivity disorder (aOR, 2.2; 95% CI, 1.5–3.3), autism (aOR, 2.9; 95% CI, 1.9–4.5), conduct disorder (aOR, 1.7; 95% CI, 1.2–2.5), psychosis (aOR, 14.3; 95% CI, 2.5–271.8), and substance use/overdose states (aOR, 1.9; CI, 1.2–3.2). Restrained agitated patients had longer ED LOS (8.4 vs 5.0 hours; P < 0.0001) and higher admission rates (aOR, 2.6; 95% CI, 2.0–3.5). Depression (aOR, 0.4; 95% CI, 0.3–0.5) and suicidality (aOR, 0.2; 95% CI, 0.1–0.3) were protective against agitation and restraint use.
Conclusion
Prevalence of acute agitation and restraint use in pediatric EDs may be much higher than previously reported. Predictors of acute agitation and restraint use among MBH patients were consistent with prior reports. Restrained agitated patients had longer ED LOS and higher admission rates.
Keywords: aggression, agitation, emergency department, pediatric agitation, prevalence, restraint
1. INTRODUCTION
1.1. Background
Acute agitation is a common and challenging behavioral health emergency seen in the acute care setting. 1 , 2 , 3 The agitated child or adolescent poses a significant risk to self, staff, parent(s), and others. 4 , 5 Acute agitation can result in significant care disruption, property destruction, and unnecessary resource use. 6 Therefore, anticipation, prompt recognition, and early intervention are needed to avoid significant injuries and process disruption from behavioral escalation. 6
Typically, a child with mental and behavioral health (MBH) needs may present to the emergency department (ED) acutely agitated or become agitated while in the ED. The standard ED setting is not well suited for the mentally ill or agitated patient. 7 , 8 Rooms are generally compact and restrictive, and the environment is frequently noisy, stressful, and overstimulating with limited access to therapeutic spaces. 4 , 7 Agitated children in the ED are usually in prolonged crisis mode due to constant surveillance and restriction of usual freedom and activities of daily living. These factors may cause significant mood disruption and behavioral escalation in at‐risk patients.
A survey of 38 North American academic children's hospitals showed that >80% of respondents encountered an agitated patient at least once a month. 1 Another national survey of pediatric emergency physicians showed that more than three‐fourths experience 1 or more verbal threats per week, 77% reported 1 or more physical attacks annually, and 25% reported actual staff injury. 9 A majority of these assaults were from agitated patients and caregivers. 9 , 10 , 11 , 12
Unfortunately, many ED physicians lack the appropriate training and resources to proactively address acute agitation to avoid behavioral escalation, injuries, and use of restraint. 4 , 7 , 13 , 14 Only a third of hospitals have a formalized training process for physicians, and there is a lack of consensus standard of care for the agitated child in the acute care setting. 13 Treatment decisions are usually reactive rather than anticipatory and often depend on the provider's comfort rather than an evidence‐based approach to care. 4 Until recently, there was only 1 solution for the agitated patient in the ED, “to restrain and medicate.” 15
Despite its significance, literature on the agitated pediatric patient is sparse. The true prevalence of pediatric agitation remains unknown. Until recently, 16 there were no clear evidence‐based guidelines for the management of acutely agitated children, leading to significant practice variation. Prior management recommendations were mostly based on expert opinions and adaptations from adult populations.
1.2. Importance and goals
Prior studies, most of which are limited by sample size, have estimated the prevalence of acute agitation (2.0%–12.0%) based on restraint use rates in the acute care settings. 16 , 17 , 18 , 19 This inferential statistic likely underestimates the true prevalence because the majority of pediatric agitations are de‐escalated without restraint use. Furthermore, the prevalence of restraint use in the acute care setting may also have been underreported through the inclusion of all MBH visits to the ED in its calculation.
This study provides a relatively robust and focused review of the experience of acutely agitated patients seen in the pediatric ED (PED). We believe our study is the largest single‐center study to provide a focused descriptive report of the prevalence, demographic and clinical characteristics, and care provided for agitated pediatric patients with MBH needs in the PED. In addition, the design and conduct of the study potentially addresses some of the methodologic and analytic issues observed in prior studies.
The primary objective of this study was to evaluate the prevalence and predictors of acute agitation and restraint use among agitated pediatric patients in the PED. Secondarily, we evaluated ED visit pattern, length of stay (LOS), and admission rates for these agitated pediatric patients.
2. METHODS
2.1. Study design and setting
This is a retrospective observational study involving chart review of patients aged ≤18 years who presented to the PED from January 2017 to December 2019 with MBH needs. This study was approved by the institutional review board under waiver of consent. The University of Texas Southwestern Children's Health System is a premier pediatric tertiary health care system in urban North Texas. Our busy PED is the only level 1 trauma center in North Texas, with an annual volume of >170,000 visits before the pandemic. This is 1 of the highest volumes and most diverse population of patients nationwide. As a major provider of MBH services to a diverse population of patients with mental health needs in North Texas, we receive referrals from all of North Texas and neighboring states.
2.2. Institutional agitation guideline and care teams
Institutionally, MBH patients presenting to the PED are first screened and stabilized by a PED provider before making further evaluation to determine and exclude an underlying medical cause of the patient's symptoms. Thereafter, the mental health assessment team (MHAT; a team of psychiatrists and trained psychiatric social workers) are consulted for further evaluation, risk assessment, need for treatment, and determination of disposition. Typically, all patients visiting the ED with MBH concerns are seen and evaluated by the MHAT.
Specifically for acutely agitated and disruptive patients, the hospital has established an agitation management guideline and a behavioral emergency response team (BERT) to provide a systematic and predictive approach to caring for the agitated child. The BERT is a strategic multidisciplinary collaborative (comprising the patient's bedside nurse, on‐site clinical provider, administrative supervisor, psychiatry consultant, social work staff, a psychiatry registered nurse, a pharmacist, and security personnel) that proactively responds to agitation concerns, assists in diffusing an escalating patient, and facilitates the use of the least restrictive interventions where non‐pharmacologic de‐escalation strategies fail. 20 For severely agitated patients with significant safety concerns as determined by the BERT using the validated Behavioral Activity Rating Scale (BARS) score (5 = mild agitation, 6 = moderate agitation, and 7 = severe agitation), 21 a collaborative decision by the BERT is required for physical or pharmacologic restraint use in line with the agitation guideline. Restrained patients are monitored and re‐evaluated frequently, with real‐time documentation of events during restraint. The guideline, which includes a list of protocolized medications used for agitation care, is included as part of the supplementary materials.
2.3. Study definitions
The Bottom Line.
Acute agitation is a common and challenging behavioral health emergency. However, there is a lack of focused research on pediatric agitation, and the prevalence of agitation and restraint use in the emergency department remain unknown. This study suggests that the prevalence of pediatric agitation and restraint use may be higher than previously reported.
We defined acute agitation as a verbal and/or motor restlessness associated with a feeling of inner tension and often accompanied by irritability and a predisposition to aggression or violence. 2 , 22 We considered the acutely agitated patient as one who presented to the ED with a complaint of agitation/aggression or who became agitated/aggressive while boarding in the ED (Figures 1 and 3). Restraints were either physical or pharmacological. Pharmacologic restraint involves use of a psychotropic medication (usually an antipsychotic or a benzodiazepine) in a crisis situation to help the child contain out‐of‐control aggressive behavior. Physical restraint involves manual holding of a patient or use of a mechanical device such as wrist or ankle straps. 18 , 23 ED LOS was defined as the median LOS for the population under consideration, 24 and the admission rate was defined as the proportion of visits that resulted in inpatient admission/transfer. Prolonged ED LOS was defined as any ED LOS longer than the median LOS for the population under review. 24
FIGURE 1.
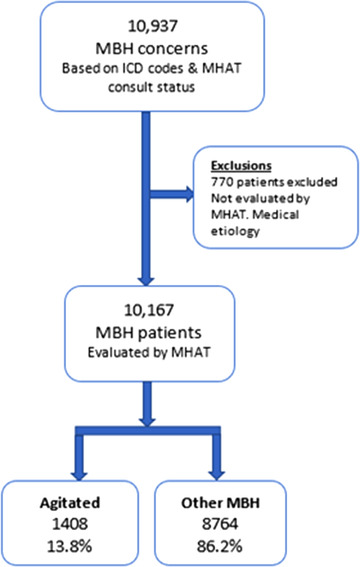
Flowchart of all mental and behavioral health (MBH) visits. ICD, International Classification of Diseases; MHAT, mental health assessment team
FIGURE 3.

Distribution of the agitated population (N = 1408). ED, emergency department
2.4. Participant selection and inclusion/exclusion criteria
Electronic health record search was performed to first identify all patients with MBH needs based on International Classification of Diseases, Tenth Revision (ICD‐10) diagnosis codes (supplemental data) and ED evaluation by the MHAT. We then identified and ascertained agitated/aggressive patients using clinical encounter documentation of presenting complaints, signs and symptoms, ICD‐10 diagnosis codes, BARS scores, and restraint use status. We excluded all patients aged >18 years, those with neuropsychiatric symptoms determined to be caused by an underlying medical or traumatic condition, and patients who were not evaluated by the MHAT. MBH patients who eloped or left without a clear disposition status were excluded from our secondary analyses.
2.5. Data collection/outcomes
Data elements collected for each patient included age, sex, race, ethnicity, insurance type, date of visit, prior visits, anthropometric data, presenting complaint(s), clinical diagnoses, BARS score, restraint status and types, ED medications, ED LOS, disposition, and MHAT evaluation status. Primarily, we sought to describe the prevalence and predictors of pediatric agitation and restraint use for agitated patients. Secondarily, we evaluated the ED visit pattern, ED LOS, and the admission rate for agitated patients.
2.6. Analysis
We performed descriptive statistics, means with standard deviations for continuous (normally distributed) variables, and frequencies with percentages for categorical variables. Specifically, because ED LOS was a non‐parametric continuous variable, we used median and interquartile range (IQR) for summary statistics, whereas the Wilcoxon rank sum test was used for the comparison of medians. In addition, we categorized age and ED LOS into clinically meaningful descriptive intervals. For categorical variables, we performed appropriate univariate and multivariable analyses using chi‐square (χ2) and logistic regression modeling to evaluate the prevalence and predictors of pediatric agitation and restraint use at the α = 0.05 statistical significance level. We reported adjusted odd ratios (aORs) with confidence intervals (CIs) or P values as appropriate. All analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC).
3. RESULTS
Of 10,172 patients with MBH needs who were evaluated by the MHAT, 1408 (13.8%) were agitated/aggressive (Figure 1). Of these (n = 1408), 63.7% were boys, mean age was 11.9 ± 3.6 years, 25.0% self‐identified as Hispanic, and 74.2% identified as non‐Hispanic. In terms of race, 68.5% were White, 22.2% were Black, and 2.2% were Asian (Table 1).
TABLE 1.
Demographic and diagnostic characteristics
| Description | Agitated, n = 1408 | Non‐agitated, n = 8764 |
|---|---|---|
| Age, continuous, y | ||
| Mean (±SD) a | 11.9 (±3.6) | 13.6 (±2.8) |
| Median (IQR) | 12.0 (9.1–15.0) | 14.0 (11.9–15.8) |
| Description | n (%) | n (%) |
|---|---|---|
| Sex | ||
| Female | 511 (36.2) | 5429 (61.9) |
| Male a | 897 (63.7) | 3335 (38.1) |
| Age, categorized | ||
| 0 < 10 y | 452 (32.1) | 958 (10.9) |
| 10 to 18 y | 956 (67.9) | 7806 (89.1) |
| Ethnicity | ||
| Hispanic | 351 (24.9) | 3137 (35.8) |
| Non‐Hispanic a | 1045 (74.2) | 5539 (63.2) |
| Unknown | 12 (0.9) | 88 (1.0) |
| Race | ||
| White | 964 (68.5) | 6148 (70.1) |
| Black | 312 (22.2) | 1431 (16.3) |
| Asian | 31 (2.2) | 166 (1.9) |
| AIAN | 3 (0.2) | 11 (0.1) |
| NHPI | 1 (0.1) | 7 (0.1) |
| Other b | 56 (4.0) | 728 (8.3) |
| Unknown | 41 (2.9) | 273 (3.1) |
| Year | ||
| 2017 | 434 (30.8) | 2360 (26.9) |
| 2018 | 414 (29.4) | 2963 (33.8) |
| 2019 | 560 (39.8) | 3441 (39.3) |
| Diagnosis c | ||
| Suicidality | 405 (28.7) | 5307 (60.6) |
| Self‐harm behavior | 156 (11.1) | 1513 (17.3) |
| Depression | 215 (15.3) | 3189 (36.4) |
| Psychosis a | 16 (1.1) | 28 (0.3) |
| Anxiety disorder | 199 (14.1) | 1579 (18.0) |
| Overdose/poisoning | 99 (7.0) | 950 (10.8) |
| Substance use | 106 (7.5) | 763 (8.7) |
| ADHD a | 213 (15.1) | 610 (7.0) |
| Conduct disorder a | 257 (18.3) | 232 (2.7) |
| Autism a | 159 (11.3) | 152 (1.7) |
| Panic disorder | 22 (1.6) | 197 (2.2) |
| Bipolar a | 53 (3.8) | 141 (1.6) |
| ODD a | 45 (3.2) | 92 (1.0) |
| Schizophrenia | 7 (0.5) | 24 (0.3) |
| DMDD a | 43 (3.1) | 49 (0.6) |
Note: Data are provided as mean ± standard deviation, median (interquartile range), or number (percentage).
Abbreviations: ADHD, attention deficit hyperactivity disorder; AIAN, American Indian and Alaskan Native; DMDD, disruptive mood dysregulation disorder; IQR, interquartile range; NHPI, Native Hawaiian/Pacific Islander; ODD, oppositional defiant disorder; SD, standard deviation.
Univariate predictors of acute agitation.
Mostly Hispanic ethnicity.
Some patients had >1 diagnosis category.
In absolute terms, agitation‐related visits increased significantly from 434 visits in 2017 to 560 visits in 2019, which is an ≈29.0% increase during the 3‐year period (P = 0.001; Figure 2). However, among all MBH visits, there was a proportionate decrease in agitation‐related visits from 15.5% in 2017 to 14.0% in 2019 (Table 1 and Figure 2). Similarly, we observed a 34.2% absolute increase in restraint use (n = 117 in 2017 to n = 157 in 2019) among agitated patients, but the proportion of patients restrained per year remained relatively stable (P = 0.285).
FIGURE 2.
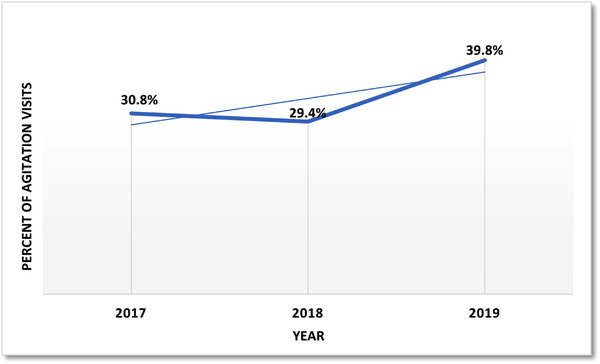
Agitation visits by year
The prevalence of agitation among all MBH patients (n = 10,172) was 13.8%. Figure 3 shows the distribution of the agitated/aggressive subpopulation. Observed prevalence of restraint use among agitated patients (n = 1408) was (28.8%; Table 2). Among agitated patients, 21.2% (n = 298) received pharmacologic restraint only, 3.1% (n = 44) received physical restraint only, and 4.5% (n = 63) had both. The prevalence of restraint was computed based on any use during a given visit, irrespective of the number of times restraint was needed during that visit.
TABLE 2.
ED LOS, disposition, BARS score, and restraint data
| Description | Agitated, n = 1408 | Non‐agitated, n = 8764 |
|---|---|---|
| ED LOS, h | ||
| Mean (±SD) | 11.1 (±17.7) | 8.6 (±11.4) |
| Median (IQR) | 5.8 (3.8–10.3) | 5.3 (3.8–8.4) |
| Description | n (%) | n (%) |
|---|---|---|
| ED LOS, categorized | ||
| 0 < 4 h | 378 (26.9) | 2459 (28.1) |
| 4 < 10 h | 664 (47.1) | 4571 (52.1) |
| 10 < 24 h | 228 (16.2) | 1235 (14.1) |
| 24 < 72 h | 115 (8.2) | 435 (5.0) |
| ≥72 h | 23 (1.6) | 64 (0.7) |
| Disposition | ||
| Admit/transfer | 448 (31.8) | 2176 (24.8) |
| Discharged | 925 (65.7) | 6403 (73.1) |
| AMA | 32 (2.3) | 173 (2.0) |
| LWBS | 2 (0.1) | 4 (0.1) |
| Eloped | 0 (0.0) | 6 (0.1) |
| BARS score | ||
| 0 to 4 | 426 (43.3) | 4935 (100.0) |
| 5 to 7 | 559 (56.8) | 0 (0.00) |
| Missing | 423 (–) | 3829 (–) |
| Restraint | ||
| Overall a | 405 (28.7) | 250 (2.9) |
| Physical | 107 (7.6) | 0 (0.0) |
| Pharmacologic b | 361 (25.6) | 250 (2.8) |
| Lorazepam | 145 (10.3) | 89 (1.0) |
| Haloperidol | 38 (2.7) | 12 (0.1) |
| Olanzapine | 184 (13.1) | 94 (1.1) |
| Risperidone | 66 (4.7) | 54 (0.6) |
| Ziprasidone | 114 (8.1) | 36 (0.4) |
Note: Data are provided as mean ± standard deviation, median (interquartile range), or number (percentage). BARS scores: 5 = mild agitation, 6 = moderate agitation, and 7 = severe agitation.
Abbreviations: AMA, left against medical advice; BARS, Behavioral Activity Rating Scale; ED, emergency department; IQR, interquartile range; LOS, length of stay; LWBS, left without being seen; SD, standard deviation.
Some patients received a combination of physical and pharmacologic restraints and a combination of psychotropic medications for agitation.
Medications for acute agitation care per institutional policy.
Common psychotropic medications used for pharmacologic restraint include olanzapine (51.0%), risperidone (18.3%), ziprasidone (31.6%), haloperidol (10.5%), and lorazepam (40.1%). Of the patients who were pharmacologically restrained, ≈35.0% received a combination of 2 or more psychotropic medications. Common combinations include lorazepam and haloperidol or lorazepam and an atypical antipsychotic. Few agitated patients also received diphenhydramine (n = 10) or hydroxyzine (n = 6) as monotherapy.
Compared with non‐agitated patients, agitated/aggressive patients were more likely to be boys, non‐Hispanic Black, admitted/transferred for inpatient care, or be assigned a higher BARS score (Tables 1 and 2). Independent predictors of acute agitation in the multivariable logistic regression model adjusted for age, sex, ethnicity, and ED LOS include non‐Hispanic Black descent, a history of psychosis, autism, attention deficit hyperactivity disorder (ADHD), conduct disorder, oppositional defiant disorder, disruptive mood dysregulation disorder, and bipolar disorder. On the contrary, mood disorders such as depression, suicidality, and self‐harm were associated with a decreased risk of agitation/aggression (Table 3).
TABLE 3.
Multivariable predictors of agitation and restraint use
| Predictors | aOR a | 95% CI |
|---|---|---|
| Predictors of agitation/aggression | ||
| Non‐Hispanic Black | 1.8 | 1.2–2.7 |
| ADHD | 1.9 | 1.5–2.4 |
| Autism | 7.1 | 5.1–9.9 |
| Bipolar disorder | 2.8 | 1.9–4.2 |
| Conduct disorder | 5.4 | 4.2–7.1 |
| DMDD | 3.2 | 1.9–5.3 |
| ODD | 1.7 | 1.1–2.7 |
| Psychosis | 4.2 | 1.8–9.4 |
| Depression | 0.4 | 0.3–0.5 |
| Suicidality | 0.2 | 0.1–0.3 |
| Predictors of restraint use among agitated patients | ||
| BARS score (5–7) | 7.1 | 5.0–10.0 |
| ADHD | 2.2 | 1.5–3.3 |
| Autism | 2.9 | 1.9–4.5 |
| Conduct disorder | 1.7 | 1.2–2.5 |
| Overdose/substance use | 1.9 | 1.2–3.2 |
| Psychosis | 14.3 | 2.5–271.8 |
| Non‐Hispanic Black | 0.8 | 0.3–1.8 |
Note: BARS scores: 5 = mild agitation, 6 = moderate agitation, and 7 = severe agitation.
Abbreviations: ADHD, attention deficit hyperactivity disorder; aOR, adjusted odds ratio; BARS, Behavioral Activity Rating Scale; CI, confidence interval; DMDD, disruptive mood dysregulation disorder; ODD, oppositional defiant disorder.
Adjusted for age, sex, ethnicity, and ED length of stay.
Among agitated patients, independent predictors of restraint use in a multivariable model adjusted for age, sex, ethnicity, and ED LOS were history of psychosis, autism, substance use, ADHD, conduct disorder, and overdose/poisoning. Race and specifically non‐Hispanic Black descent were not significant predictors of restraint use (aOR, 0.9; 95% CI, 0.6–1.4). History of depression and suicidality were associated with decreased odds of restraint (aOR, 0.5; 95% CI, 0.4–0.7; Table 3).
The admission rate for agitated patients (31.8%) was higher than non‐agitated patients (24.8%; Table 1). This rate was much higher for agitated patients who were restrained (54.2%; Table 5). In a multivariable model, agitated patients who were restrained were more likely to be admitted (aOR, 2.6; 95% CI, 2.0–3.5) and also had significantly longer ED LOS (median, 8.4; IQR, 5.3–18.9 hours) compared with unrestrained patients (median, 5.0; IQR, 3.6–8.2 hours; P < 0.0001). This was true even after adjusting for the effect of admission status on ED LOS (Tables 4 and 5). Of the restrained agitated patients, ≈44.2% boarded in the ED for at least 10 hours, with 19.8% boarding for 24 hours or more.
TABLE 5.
Agitated patients stratified by restraint status
| Description | Restrained, n = 405 | Unrestrained, n = 1004 |
|---|---|---|
| Age, y | ||
| Median (IQR) | 14.0 (10.6–16.0) | 11.3 (8.9–14.4) |
| ED LOS, h | ||
| Median (IQR) | 8.4 (5.3–18.9) | 5.0 (3.6–8.2) |
| Description | n (%) | n (%) |
|---|---|---|
| Age (categorized) | ||
| 10‐18 y | 311 (76.8) | 645 (64.3) |
| 0 < 10 y | 94 (23.2) | 358 (35.7) |
| ED LOS (categorized) | ||
| ≥72 h | 14 (3.5) | 9 (0.9) |
| 24 < 72 h | 66 (16.3) | 49 (4.9) |
| 10 < 24 h | 99 (24.4) | 129 (12.9) |
| 0 < 10 h | 226 (55.8) | 816 (81.4) |
| Disposition | ||
| Admit/transfer | 211 (54.2) | 237 (24.1) |
| Discharged | 178 (45.8) | 747 (75.9) |
| BARS score | ||
| 5–7 | 304 (84.2) | 255 (40.9) |
| 0–4 | 57 (15.8) | 369 (59.1) |
Note: Data are provided as median (interquartile range) or number (percentage). BARS scores: 5 = mild agitation, 6 = moderate agitation, and 7 = severe agitation.
Abbreviations: BARS, Behavioral Activity Rating Scale; ED, emergency department; LOS, length of stay.
TABLE 4.
Multivariable predictors of admission/prolonged ED LOS among agitated patients
| Predictors | aOR a | 95% CI |
|---|---|---|
| Predictors of admission/transfer | ||
| Restraint use | 2.6 | 2.0–3.5 |
| BARS score (5–7) | 2.3 | 1.7–3.1 |
| Psychosis | 5.8 | 1.3–40.6 |
| Substance use | 1.9 | 1.2–3.0 |
| ADHD | 1.7 | 1.2–2.5 |
| Overdose/poisoning | 7.0 | 4.0–12.8 |
| ODD | 2.7 | 1.3–6.1 |
| Predictors of prolonged ED LOS | ||
| Restraint use | 1.8 | 1.3–2.4 |
| Substance use | 2.1 | 1.2–3.8 |
Note: BARS scores: 5 = mild agitation, 6 = moderate agitation, and 7 = severe agitation.
Abbreviations: ADHD, attention deficit hyperactivity disorder; aOR, adjusted odds ratio; BARS, Behavioral Activity Rating Scale; CI, confidence interval; ED, emergency department; LOS, length of stay; ODD, oppositional defiant disorder.
Adjusted for age, sex, ethnicity, ED LOS.
Adjusted for age, sex, and ED LOS.
Despite the strengths of this study, there are several limitations. First, this is a retrospective single‐center study. It is likely that our data may not have captured regional variation in the care of the agitated child, and our study results may not be generalizable to some populations. However, the comparable results of this study to prior studies ratify its applicability in similar settings with a clear institutional framework and policy to guide the care of the agitated child. Second, our data only captured agitated patients with mental health concerns who were seen and evaluated by the MHAT. Therefore, it is likely that we may have missed a few patients with other medical or traumatic cause of agitation, creating a potential for selection bias. Third, it was difficult to clearly delineate oral psychoactive medications used for restraint from scheduled maintenance medications, creating a potential for misclassification and overestimation of pharmacologic restraint use. However, such misclassification, if present, is likely very minimal because we only included protocolized medications used for acute agitation with documentation to show medication use in the setting of acute agitation. Psychotropic medications used for agitation (mono‐ or combination therapy) during a given ED visit were also counted once. We also did not consider antihistamine monotherapy as pharmacologic restraint because these medications are not protocolized for agitation. However, it is possible that some providers may have prescribed antihistamines for agitation.
4. DISCUSSION
There is a paucity of original research specifically looking at the experience of acutely agitated pediatric patients in the ED. Based on a review of the existing literature, we believe our study is the largest single‐center study to provide a focused descriptive report of the prevalence, demographic and clinical characteristics, and care provided for agitated pediatric patients with MBH needs in the PED setting. Based on this study, the prevalence of acute agitation and restraint use were 13.8% and 28.8%, respectively, implying that more than two‐thirds of acutely agitated patients were managed with established de‐escalation strategies such as effective communication, environmental modifications, and behavioral interventions by our multidisciplinary collaborative team. 4 , 6 , 25
The true prevalence of pediatric acute agitation remains unknown despite prior attempts to extrapolate this prevalence from the rate of restraint use in the acute care setting. 18 , 26 This is because such inferential statistics generally underestimate the true prevalence of pediatric agitation due to significant selection bias by severity. The greater proportion of mild‐to‐moderate pediatric agitations in the acute care setting are diffused through de‐escalation strategies that do not require restraint use. Restraints are mostly used for severe acute agitation with immediate safety concern and risk for significant injury or care disruption. We used multiple data points (presenting complaints, documented signs and symptoms, ICD‐10 codes, BARS scores, and restraint use documentation) to ascertain cases of agitation/aggression. This probably explains why the observed prevalence of 13.8% is slightly above the upper limit (1.6%–11.8%) reported by Foster et al and other studies. 18 , 19 However, in contrast to our study, Rudolf et al reported a much higher proportion of patients presenting with a complaint of agitation (28.0%) among 229 patients who received antipsychotic medications. 27 In addition to sample‐size limitation, the inclusion criteria of this study potentially introduced significant selections bias, with a likely overestimation of the prevalence of agitation.
Acute agitation is multifactorial in origin. 3 – 5 Typically, it is a reactionary response to an acute stressor resulting from a complex interplay of personal, physical, and environmental factors. 3 Best practice guidelines for evaluation and treatment recommend a collaborative multimodal approach involving anticipation and proactiveness on the part of the ED provider, rapid risk assessment with ongoing re‐evaluations, strategic reduction of environmental triggers, mitigation of modifiable risk factors, and proactiveness in diffusing early signs of agitation through non‐pharmacologic de‐escalation strategies followed by individualized care that addresses the specific needs of the child. 4 , 6 , 16 , 25 Early and skillful use of non‐pharmacologic de‐escalation strategies has significantly reduced the need for pharmacologic and physical restraints. 20 , 28 Based on our study, more than two‐thirds of acute agitations were diffused by non‐pharmacologic de‐escalation strategies, which is consistent with prior report by Hopper et al, where verbal de‐escalation was used in 56 of 75 agitated patients. 12 Restraints are typically used in the setting of emergent safety concerns, usually after an unsuccessful initial attempt at de‐escalation.
Observed prevalence of restraint use among all MBH patients (6.4%) was very similar to prior reports. Dorfman and Mehta 18 showed that 6.8% of 1125 MBH patients were restrained, which is well within the range (1.6%–11.8%) reported by Foster et al. 19 However, it is likely that the use of all PED mental health visits may have underestimated the prevalence of restraint use in prior reports because the majority of PED mental health visits (suicidality, depression, and self‐harm behavior) are protective against restraint use, as observed in this and prior studies. 18 , 19 , 29 , 30 Besides, restraints are exclusively or predominantly used for agitated patients and rarely seen, if ever, among non‐agitated patients. Therefore, it is reasonable to posit that the true prevalence of restraint use should be estimated from the population of agitated patients only, not from all MBH visits to the ED.
Based on the aforementioned premise, Mroczkowski et al 1 reported a restraint use prevalence of 15% to 23% among diagnostic subsets of agitated pediatric patients in a psychiatric ED. Sheridan et al 31 reported a prevalence of 33.0%, with 23.0% of patients receiving pharmacologic restraint. We observed a restraint use prevalence of 28.8% among all agitated patients, with pharmacologic restraint use in 21.0% of agitated patients. Another potential source of underestimation of restraint use in prior studies is the relatively narrow definition of pharmacologic restraint as intramuscular or intravenous administration of psychotropic medication for agitation control. 19 , 28 , 32 Use of oral psychotropic medication was not considered as pharmacologic restraint due to uncertainties about the indication for such medications. Although this remains a valid concern, in reality mildly agitated patients may be able to tolerate pro re nata oral medications for agitation control. 33
Despite existing practice variations, psychopharmacologic management of pediatric agitation has evolved significantly. Prior literature show a predominance of benzodiazepines, high‐potency neuroleptics, and antihistamines. 17 , 26 , 34 More recent literature are reporting an increasing use for the atypical antipsychotics. 1 This is likely due to the general lack of consensus guidelines for the evaluation and treatment of pediatric agitation in the past, in addition to reported adverse events associated with high‐potency antipsychotics and benzodiazepines. In a small 5‐year retrospective study, Kendrick et al 34 reported the use of lorazepam in 70.0% and chlorpromazine in 20.0% of patients receiving pharmacologic restraints. Recently, Foster et al reported the use of benzodiazepines in 56.0%, antipsychotics in 46.2%, and antihistamines in 32.0% of patients. 19 We observed a predominance of atypical antipsychotics (olanzapine, ziprasidone, and risperidone) followed by benzodiazepines (lorazepam). Similarly, Rudolf et al reported a comparable atypical antipsychotic use (olanzapine, 51.1%; aripiprazole, 26.6%) among PED psychiatric patients. 27
Predictors of acute agitation reported in prior studies include a history of disruptive behavior, autism spectrum disorder and intellectual disability, ADHD, psychosis, substance intoxication or withdrawal, and disruptive, impulse control, and conduct disorders. 4 , 19 , 32 , 34 Independent predictors of agitation and restraint use observed in this study were consistent with the observed predictors in prior studies. However, in contrast to a report by Foster et al, 19 non‐Hispanic Black descent was not an independent predictor of restraint use despite being a predictor of acute agitation. Dorfman and Mehta also showed that race, age, and insurance status were not significant predictors of restraint use. 18 Geographic variation in race and ethnicity may account for the observed differences. It is also possible that our study, like the study by Dorfman and Mehta, was underpowered to detect an association between race and restraint use.
Although we observed an absolute increase in agitation‐related visits and restraint use during the 3‐year study period, there was no proportionate increase in annual visits or restraint use. Similarly, Foster et al reported a 370% absolute increase in mental health visits requiring use of pharmacologic restraint, although the rate of restraint use remained constant during the 11‐year period. 19 This relatively stable rate may be attributable to the disproportionate increase in suicidality, self‐harm, and depression‐related visits in recent years, which are generally protective against aggressive behavior and restraint use. Furthermore, in keeping with prior reports, our study establishes that restraint use was independently associated with longer ED LOS and higher admission rates. 27 , 32 Prior studies have suggested that restraint use may be an indicator of more severe disease state, leading to higher admission rates. 32
In conclusion, acute agitation remains a relatively common behavioral health emergency seen in the ED. Based on this study, the prevalence of pediatric agitation and restraint use in the acute care setting may be much higher than previously reported. Restrained agitated patients had longer ED LOS and higher admission rate. Predictors of acute agitation and restraint use among MBH patients were consistent with prior reports.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Matthias M. Manuel conceptualized and designed the study, supervised institutional review board submission of study protocol, coordinated and supervised data collection and cleaning, carried out initial data analyses, drafted the initial manuscript, and reviewed and revised the manuscript. Sing‐Yi Feng and Kenneth Yen actively participated in the design, drafting, and revision of the study protocol, including the review and revision the manuscript for important intellectual content. In addition, Kenneth Yen reviewed statistical analyses and study results for appropriacy and accuracy. Faisalmohemed Patel was actively involved in the conceptualization and design of this study, participated in drafting the study protocol, and supervised institutional review board submission and data collection in addition to critically reviewing the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Supporting information
Supporting Information
Biography
Matthias M. Manuel is a Pediatric Emergency Medicine Fellow at the University of Texas Southwestern Children's Medical Center in Dallas, Texas.

Manuel MM, Feng S‐Y, Yen K, Patel F. The agitated pediatric patient located in the emergency department: The APPLIED observational study. JACEP Open. 2022;3:e12766. 10.1002/emp2.12766
Supervising Editor: Bernard Chang, MD, PhD.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see https://www.icmje.org). The authors have stated that no such relationships exist.
Presentation/Meetings: Abstract was submitted to the 2022 Pediatric Academic Society Conference, Denver, CO.
REFERENCES
- 1. Mroczkowski M. 28.4 Pediatric agitation management in the psychiatric emergency department: the evidence base. J Am Acad Child Adolesc Psychiatry. 2017;56(10):S43. 10.1016/j.jaac.2017.07.168 [DOI] [Google Scholar]
- 2. Bhatia R, Agitation in children and adolescents: Diagnostic and treatment considerations. Published June 2019. Accessed October 28, 2021. https://www.mdedge.com/psychiatry/article/201622/pediatrics/agitation‐children‐and‐adolescents‐diagnostic‐and‐treatment
- 3. Haidar‐Elatrache S, Wolf M, Fabie NAV, Sahai S. Approach to children with aggressive behavior for general pediatricians and hospitalists: part 1—epidemiology and etiology. Pediatr Ann. 2018;47(10):e402‐e407. 10.3928/19382359-20180918-02 [DOI] [PubMed] [Google Scholar]
- 4. Gerson R, Malas N, Mroczkowski MM. Crisis in the emergency department: the evaluation and management of acute agitation in children and adolescents. Child Adolesc Psychiatr Clin N Am. 2018;27(3):367‐386. 10.1016/j.chc.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 5. Marzullo LR. Pharmacologic management of the agitated child. Pediatr Emerg Care. 2014;30(4):269‐275. 10.1097/PEC.0000000000000112 [DOI] [PubMed] [Google Scholar]
- 6. Hoffmann JA, Pergjika A, Konicek CE, Reynolds SL. Pharmacologic management of acute agitation in youth in the emergency department. Pediatr Emerg Care. 2021;37(8):417‐422. 10.1097/PEC.0000000000002510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chun TH, Duffy SJ, Grupp‐Phelan J. The increasing burden of psychiatric emergencies: a call to action. Pediatrics. 2019;143(4):e20190251. 10.1542/peds.2019-0251 [DOI] [PubMed] [Google Scholar]
- 8. Rogers SC, Mulvey CH, Divietro S, Sturm J. Escalating mental health care in pediatric emergency departments. Clin Pediatr (Phila). 2017;56(5):488‐491. 10.1177/0009922816684609 [DOI] [PubMed] [Google Scholar]
- 9. McAneney CM, Shaw KN. Violence in the pediatric emergency department. Ann Emerg Med. 1994;23(6):1248‐1251. 10.1016/s0196-0644(94)70349-3 [DOI] [PubMed] [Google Scholar]
- 10. Gillespie GL, Gates DM, Miller M, Howard PK. Violence against healthcare workers in a pediatric emergency department. Adv Emerg Nurs J. 2010;32(1):68‐82. 10.1097/TME.0b013e3181c8b0b4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shaw J. Staff perceptions of workplace violence in a pediatric emergency department. Work. 2015;51(1):39‐49. 10.3233/WOR-141895 [DOI] [PubMed] [Google Scholar]
- 12. Hopper SM, Babl FE, Stewart CE, Woo JW. Aggression management in a children's hospital setting. Med J Aust. 2012;196(3). https://www.mja.com.au/journal/2012/196/3/aggression‐management‐childrens‐hospital‐setting. Accessed November 9, 2021. [DOI] [PubMed] [Google Scholar]
- 13. Malas N, Spital L, Fischer J, Kawai Y, Cruz D, Keefer P. National survey on pediatric acute agitation and behavioral escalation in academic inpatient pediatric care settings. Psychosomatics. 2017;58(3):299‐306. 10.1016/j.psym.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 14. Hoffmann JA, Foster AA. Ready or not, here i come: emergency department readiness for pediatric mental health visits. Pediatrics. 2020;145(6). 10.1542/peds.2019-3542 [DOI] [PubMed] [Google Scholar]
- 15. Roppolo LP, Morris DW, Khan F, et al. Improving the management of acutely agitated patients in the emergency department through implementation of project BETA (best practices in the evaluation and treatment of agitation). J Am Coll Emerg Physicians Open. 2020;1(5):898‐907. 10.1002/emp2.12138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gerson R, Malas N, Feuer V, Silver GH, Prasad R, Mroczkowski MM. Best practices for evaluation and treatment of agitated children and adolescents (BETA) in the emergency department: consensus statement of the American Association for Emergency Psychiatry. West J Emerg Med. 2019;20(2):409‐418. 10.5811/westjem.2019.1.41344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hilt RJ, Woodward TA. Agitation treatment for pediatric emergency patients. J Am Acad Child Adolesc Psychiatry. 2008;47(2):132‐138. 10.1097/chi.0b013e31815d95fd [DOI] [PubMed] [Google Scholar]
- 18. Dorfman DH, Mehta SD. Restraint use for psychiatric patients in the pediatric emergency department. Pediatr Emerg Care. 2006;22(1):7‐12. 10.1097/01.pec.0000195758.12447.69 [DOI] [PubMed] [Google Scholar]
- 19. Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic restraint use during mental health visits in pediatric emergency departments. J Pediatr. 2021;236:276‐283.e2. 10.1016/j.jpeds.2021.03.027 [DOI] [PubMed] [Google Scholar]
- 20. Choi KR, Omery AK, Watkins AM. An integrative literature review of psychiatric rapid response teams and their implementation for de‐escalating behavioral crises in nonpsychiatric hospital settings. JONA J Nurs Adm. 2019;49(6):297‐302. 10.1097/NNA.0000000000000756 [DOI] [PubMed] [Google Scholar]
- 21. Swift RH, Harrigan EP, Cappelleri JC, Kramer D, Chandler LP. Validation of the behavioural activity rating scale (BARS)™: a novel measure of activity in agitated patients. J Psychiatr Res. 2002;36(2):87‐95. 10.1016/S0022-3956(01)00052-8 [DOI] [PubMed] [Google Scholar]
- 22. Garriga M, Pacchiarotti I, Kasper S, et al. Assessment and management of agitation in psychiatry: expert consensus. World J Biol Psychiatry. 2016;17(2):86‐128. 10.3109/15622975.2015.1132007 [DOI] [PubMed] [Google Scholar]
- 23. Physical Hold vs Restraint or Seclusion | Behavioral Health | Care Treatment and Services CTS | The Joint Commission. Accessed November 24, 2021. https://www.jointcommission.org/standards/standard‐faqs/behavioral‐health/care‐treatment‐and‐services‐cts/000002269/
- 24. Warren MB, Campbell RL, Nestler DM, et al. Prolonged length of stay in ED psychiatric patients: a multivariable predictive model. Am J Emerg Med. 2016;34(2):133‐139. 10.1016/j.ajem.2015.09.044 [DOI] [PubMed] [Google Scholar]
- 25. Richmond JS, Berlin JS, Fishkind AB, et al. Verbal de‐escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA De‐escalation Workgroup. West J Emerg Med. 2012;13(1):17‐25. 10.5811/westjem.2011.9.6864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dorfman DH, Kastner B. The use of restraint for pediatric psychiatric patients in emergency departments. Pediatr Emerg Care. 2004;20(3):151‐156. 10.1097/01.pec.0000117921.65522.fd [DOI] [PubMed] [Google Scholar]
- 27. Rudolf F, Hollenbach K, Carstairs KL, Carstairs SD. A retrospective review of antipsychotic medications administered to psychiatric patients in a tertiary care pediatric emergency department. J Pediatr Pharmacol Ther JPPT. 2019;24(3):234‐237. 10.5863/1551-6776-24.3.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vande Voort JL, Croarkin PE. Benchmarking and optimizing pharmacologic restraint for agitated youth in the emergency medicine department. J Pediatr. 2021;236:8‐9. 10.1016/j.jpeds.2021.04.039 [DOI] [PubMed] [Google Scholar]
- 29. Kalb LG, Stapp EK, Ballard ED, Holingue C, Keefer A, Riley A. Trends in psychiatric emergency department visits among youth and young adults in the US. Pediatrics. 2019;143(4). 10.1542/peds.2018-2192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hoffmann JA, Stack AM, Samnaliev M, Monuteaux MC, Lee LK. Trends in visits and costs for mental health emergencies in a pediatric emergency department. Acad Pediatr. 2019;19(4):386‐393. 10.1016/j.acap.2019.02.006 [DOI] [PubMed] [Google Scholar]
- 31. Sheridan DC, Spiro DM, Fu R, et al. Mental health utilization in a. pediatric emergency department. Pediatr Emerg Care. 2015;31(8):555‐559. 10.1097/PEC.0000000000000343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hoffmann JA, Stack AM, Monuteaux MC, Levin R, Lee LK. Factors associated with boarding and length of stay for pediatric mental health emergency visits. Am J Emerg Med. 2019;37(10):1829‐1835. 10.1016/j.ajem.2018.12.041 [DOI] [PubMed] [Google Scholar]
- 33. Yip L, Aeng E, Elbe D. Management of acute agitation and aggression in children and adolescents with Pro Re Nata Oral Immediate Release Antipsychotics in the pediatric emergency department. J Child Adolesc Psychopharmacol. 2020;30(9):534‐541. 10.1089/cap.2019.0171 [DOI] [PubMed] [Google Scholar]
- 34. Kendrick JG, Goldman RD, Carr RR. Pharmacologic management of agitation and aggression in a pediatric emergency department – a retrospective cohort study. J Pediatr Pharmacol Ther JPPT. 2018;23(6):455‐459. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Information


