Abstract
Background:
Racial–ethnic inequity in type 1 diabetes technology use is well documented and contributes to disparities in glycemic and long-term outcomes. However, solutions to address technology inequity remain sparse and lack stakeholder input.
Methods:
We employed user-centered design principles to conduct workshop sessions with multidisciplinary panels of stakeholders, building off of our prior study highlighting patient-identified barriers and proposed solutions. Stakeholders were convened to review our prior findings and co-create interventions to increase technology use among underserved populations with type 1 diabetes. Stakeholders included type 1 diabetes patients who had recently onboarded to technology; endocrinology and primary care physicians; nurses; diabetes educators; psychologists; and community health workers. Sessions were recorded and analyzed iteratively by multiple coders for common themes.
Results:
We convened 7 virtual 2-h workshops for 32 stakeholders from 11 states in the United States. Patients and providers confirmed prior published studies highlighting patient barriers and generated new ideas by co-creating solutions. Common themes of proposed interventions included (1) prioritizing more equitable systems of offering technology, (2) using visual and hands-on approaches to increase accessibility of technology and education, (3) including peer and family support systems more, and (4) assisting with insurance navigation and social needs.
Discussion:
Our study furthers the field by providing stakeholder-endorsed intervention ideas that propose feasible changes at the patient, provider, and system levels to reduce inequity in diabetes technology use in type 1 diabetes. Multidisciplinary stakeholder engagement in disparities research offers unique insight that is impactful and acceptable to the target population.
Keywords: Inequity, Disparities, Race–ethnicity, Minority, Diabetes technology, Type 1 diabetes
Introduction
Mounting evidence from our group and others underscores health inequity between Black and Hispanic versus White people with type 1 diabetes, including nearly two percentage point higher mean glycated hemoglobin (HbA1c) values, twice the risk of diabetic ketoacidosis and hospitalization, and 1.5 times higher risk of mortality.1–3 Advanced diabetes technologies, such as insulin pumps and continuous glucose monitors (CGMs), facilitate diabetes self-management, improve quality of life, and improve HbA1c up to one percentage point—showing clear potential to modify long-term outcomes and reduce disparities.4–8
The proliferation of technological options, increased ease of use, and continued high-quality evidence of glycemic benefit have led professional societies to recommend diabetes technology to become a standard part of care for patients with type 1 diabetes.9,10 However, recent reports demonstrate stark racial–ethnic disparities in technology use, with nearly two to four times higher rates of CGM and insulin pump use in White versus Black and Hispanic people with diabetes.1,11–14 As evidence of inequity in technology use grows,11,12,15–19 there remains a paucity of well-informed interventions to increase use in underserved populations with type 1 diabetes.
Underserved populations have unique health care experiences and social needs that may be limiting diabetes technology use. Challenges from social determinants of health,1,20–28 low social support,29–32 structural racism,33–36 and inequities in health care delivery1,11,12,15,17,18,37 can contribute to fractured care, lost opportunities for building rapport with providers, and inability to follow traditional diabetes care guidelines.
Most studies highlighting racial–ethnic inequity in diabetes technology use cite socioeconomic status (SES) and insurance as main drivers, but emerging evidence has not fully substantiated this long-held belief. We found in a national study of 300 young adults with type 1 diabetes that White young adults were two and four times more likely to use diabetes technology than Hispanic and Black young adults, respectively,21 despite state insurance coverage for technology at the majority of study sites. We further showed that factors related to demographics, insurance, social determinants of health, health care, and diabetes self-management did little to explain large differences in insulin pump and CGM use between White, Black, and Hispanic young adults with type 1 diabetes.11
Our findings were consistent with data from the Type 1 Diabetes Exchange registry of 25,000 people in which Black children and adults were found to use diabetes technology at 50% the rate of White children and adults, regardless of insurance status or income level.12,13 Understanding and addressing unmet patient, provider, and system needs are necessary if we want to address disparities in technology use.
In a qualitative study from our group exploring technology disparities with 50 Black and Hispanic young adults with type 1 diabetes, participants noted a lack of shared decision making and opportunities for discussion of technology with providers. Moreover, these young adults stated that when they felt heard, respected, supported, and helped with social needs, they were more likely to use diabetes technology.15 In another study of 86 adults with type 1 diabetes at federally qualified health centers, similar provider interactions and system-level issues prevented use of technology.19 These findings are consistent with studies that found physicians unconsciously and preferentially prescribed diabetes technology for youth and adult patients with type 1 diabetes who exhibited higher health literacy, SES, and lower HbA1c values.1,12,38,39
Prior qualitative studies in underserved patients with type 1 diabetes have highlighted key solutions to addressing inequity in technology use, by improving patient–provider interactions and removing system-level barriers.15,19 In an effort to include health care providers in both primary and specialty care in intervention development, and to better understand how to implement proposed solutions to increase acceptability, efficacy, and sustainability among all stakeholders, we employed user-centered design to ask stakeholders to co-create solutions and provide more detail on proposed interventions. We leveraged an approach that is interactive, emphasizes collaboration and co-creation among stakeholders, and leverage multiple viewpoints from people to optimize acceptability and implementation.
Methods
Stakeholder participants
Stakeholder characteristics are summarized in Supplementary Table S1. Patient participants were included if they had a clinical diagnosis of type 1 diabetes, were of ages 18–30 years, self-reported non-Hispanic Black or Hispanic race–ethnicity, had ability to participate in collaborative conversation with others, and had recently started on diabetes technology in the past 18 months. The decision was made to engage recent technology users to elicit perspectives of patients while off and on technology, and to ensure that onboarding and new user experiences were recent enough to provide insights relating to decision making about initiation of technology use. A wide variety of potential technologies was included such as CGM only, pump only, and automated insulin delivery (AID).
Patient participants were recruited from the Bronx, NY, which is one of the poorest and most underserved counties in the United States.44 Patients were mainly recruited for the prototyping phase given our and other previously published studies on patient-perceived facilitators and barriers.15,16,18,19,41
Provider participants provided a broad range of expertise in type 1 diabetes, racial–ethnic disparities, and/or social determinants of health. Given large gaps in the literature describing provider barriers, facilitators, and solutions on increasing diabetes technology use in underserved populations, we oversampled providers with a wide variety of experiences and from across the United States. Providers were pediatric or adult endocrine physicians/nurse practitioners, general pediatricians or internal medicine physicians, pediatric or adult psychologists, diabetes educators, or community health workers.
Research team
The multidisciplinary research team from Albert Einstein College of Medicine included expertise in diabetology, internal medicine, type 1 diabetes psychology, social determinants of health, and public health. We employed a health care design firm, Diagram LLC, which included expertise in user-centered design methods, health care design, graphic design, and health care corporations.
User-centered design workshops
Together with Diagram LLC, we developed virtual workshops to convene stakeholders and participate in activities that fostered cross-disciplinary discussion and collaboration of ideas. User-centered design principles were employed, such as empathizing, defining, ideating, and prototyping. The goal of empathizing is to better understand the problem and work through deeper comprehension of its various facets. The goal of defining is to synthesize all of the existing data and define the scope and levels of the problem. For empathizing and defining, our research team and Diagram Inc. reviewed our in-depth qualitative data examining diabetes technology use, facilitators, barriers, and proposed solutions from >50 underserved young adults with type 1 diabetes,15 as well as other available literature.
For ideating and prototyping, we created and ran workshops where stakeholders used the existing data and their own knowledge of the problem to devise solutions where anything was possible. Workshops were offered in Spanish and English; however, no participants preferred Spanish language workshops despite stating they were bilingual. Patient participants were divided by race–ethnicity (Hispanic and non-Hispanic Black) to foster social cohesion, per patient preference. Patient workshops were broken into three activities.
In the first two activities, patients were asked to confirm problems and facilitators along the technology use journey highlighted in the literature and were given the opportunity to add new information. These ideas were synthesized in real time by workshop moderators from the research team for the third activity where patients brainstormed solutions individually and as a group. After solutions were shared, patients voted on the top 2 ideas, the logistics of which were then further fleshed out with a series of implementation-specific questions in the prototyping phase: (1) who delivers the intervention, (2) what content is covered and what barriers/anticipated outcomes are expected, (3) where will the intervention take place (home, clinic, community, or some combination), (4) when should the intervention take place (synchronous or asynchronous with medical appointments and time of day), and (5) how should it be delivered (virtual, in-person, and combination of both)?
In provider workshops, the first activity included a review of patient priorities and brainstormed solutions, with solicitation of provider barriers and facilitators in the context of patient needs. The second activity consisted of provider-generated intervention ideas elicited through individual and group brainstorming time, followed by the third activity of exploring intervention logistical details. The first two activities covering empathizing, defining, and ideating were heavily focused on for providers given that most of the insights had not been studied before, especially from the viewpoint of primary care, psychologists, educators, or community health workers.
We did not include patients in the provider sessions because of the known power dynamic and our formative study with patients stating they would not feel comfortable ideating with providers present.
Procedures
Workshops were developed iteratively over the course of 2 months with a careful vetting process by our multidisciplinary research team, with initial drafting and edits made by Diagram LLC and subsequent changes made exclusively by the research team in response to preliminary testing (prototyping) with potential participants and scientific experts. Workshops were rehearsed internally in mock sessions to provide additional feedback and refine content and delivery until the research team unanimously decided that workshops were finalized.
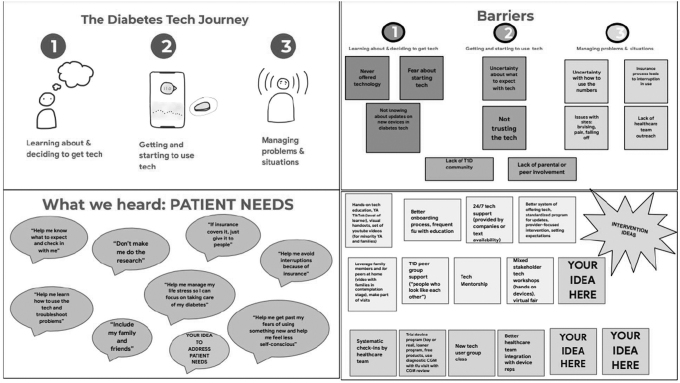
Participants were recruited through phone calls and/or email communication. After introduction of the study, informed consent was obtained. Workshops were held on privacy-protected Zoom and recorded for analysis purposes only. This study was approved by the Albert Einstein College of Medicine Institutional Review Board. All participants were provided compensation for their time. A sample compilation of workshop slides is displayed in Figure 1.
FIG. 1.
Sample workshop slides demonstrating user-centered design principles: empathizing, defining, ideating, and prototyping/co-creation. T1D, type 1 diabetes; YA, young adults.
Analysis
Two members of the Diagram team and two members of the Albert Einstein College of Medicine team performed initial thematic analysis and synthesis of results from all workshops. Coding frameworks were devised according to workshop activity and detailed analysis logs kept by the research team. Analysis was done in parallel between the Diagram and Albert Einstein teams, with the entire research team convening several times throughout the analysis process to discuss results and reconcile coding differences. After this iterative coding process, the principal investigator (S.A.) rewatched all recorded workshop sessions and confirmed that results accurately reflected the participant data.
Results
In all, our team conducted 7 virtual workshops through Zoom including 32 stakeholders: 5 non-Hispanic Black and 7 Hispanic patients with type 1 diabetes, and 20 provider stakeholders from 11 different states. Patients were on a variety of technologies including CGM only (n = 6), insulin pump only (n = 3), and AID systems (n = 3). The workshops were conducted for 7 weeks (from August of 2020 to October 2020).
Empathizing and defining phase results
Patients
Patient stakeholders confirmed much of what has been previously discussed in patient perspective studies on this topic, outlining a linear chronological journey of learning about and getting technology, technology onboarding and starting use, and managing ongoing problems. Barriers included discomfort or fear of new devices as well as needing help with troubleshooting and overall support to sustain technology use, such as education and insurance assistance. Facilitators included family and friend involvement and supportive health care provider teams.
Providers
Providers confirmed similar experiences of their patients. In addition, providers detailed their own possible biases, noting real unconscious bias specifically related to the ability of patients to “handle technology.” They detailed several barriers to traditional self-management in their underserved patients that made them hesitant to prescribe technology, such as education gaps, literacy limitations, inconsistent clinic attendance rates, and management of social determinants. Primary care providers stated that other lack of expertise was associated with lower confidence in prescribing technology even when they perceived benefits for patients.
All providers endorsed that their practice and health system structures were not amenable to patient-centered care. Their limited time with patients during appointments prevented them from having the in-depth conversations they knew they needed to fully introduce technology. They further mentioned that they had little to no support with insurance paperwork that prevented them from pursuing technology for many patients. Lastly, they mentioned that the perceived extra outreach they would need to provide to underserved patients to use technology was also a major barrier to prescribing.
Psychologists mentioned the need for peer support and involvement of family. Having safety nets for diabetes support helped with continued use of technology despite hassles. Social workers and community health workers all noted that underserved patients needed extra clinical and administrative support that was not available, especially in adult health care systems. Importantly, most health care providers did not feel equipped to screen for or manage social needs necessary for underserved patients to successfully initiate or continue use of technology.
Ideating and prototyping phase results
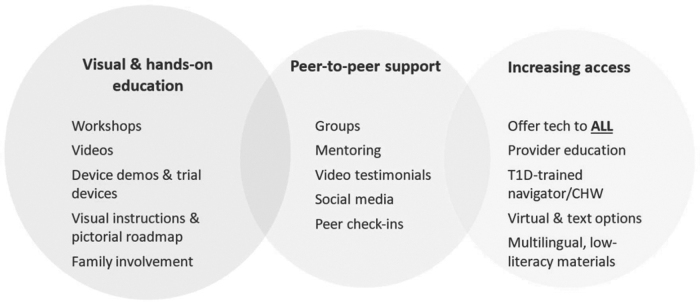
Stakeholders co-created and discussed many solutions to increase technology use in underserved populations with type 1 diabetes, displayed in Figure 2. Interventions fell into several categories, including (1) visual and hands-on education (helping people to understand how everything works and what to expect), (2) peer support (offering practical tips and advice along with emotional support from people with similar lived experiences), and (3) increased access to devices (clearing administrative/insurance and social barriers, meeting people where they are).
FIG. 2.
Key elements of a diabetes technology equity intervention discussed by multidisciplinary stakeholders. CHW, Community Health Worker.
For (1) education, stakeholders focused on demystifying technology devices by employing hands-on visual aids in conversations, such as dummy devices or other pictorial representations of products, as well as trial devices. For (2) peer support, stakeholders suggested peer-led workshops, “peer technology mentors,” use of social media campaigns, and inclusion of family members in conversations surrounding technology even when not present for medical visits. For (3) increased access to devices, stakeholders suggested instituting more equitable systems of offering technology, such as removing the provider from having to offer information on devices and instead relying on waiting room marketing materials or creating a specialized front office role for a “technology specialist/consultant.” Stakeholders also suggested a checklist in the electronic medical record to keep track of whether providers had offered technology information to all eligible patients.
In addition, provider stakeholders discussed needing a new role in clinic to implement the technology intervention instead of tasking an existing staff member. Arguments in favor of a new role described benefits of preventing burnout in clinical staff, prime focus on technology, and the opportunity to hire a staff member of color who had shared lived experiences with patients. Arguments against a new role included risk to continuity and consistency, and concerns with integration into the health care team.
Community Health Workers (CHWs) offered themselves as the best interventionists, citing several advantages over other care team members, including (1) not being part of the “system” of care, (2) having direct community experience and firsthand understanding of patient culture and values, (3) ability to make home visits if needed, (4) having more time for outreach and social support, and (5) expertise in social needs screening and social service linkage to remove barriers to technology use. Community health workers also mentioned that recent increased comfort with mobile health strategies and documentation in the electronic medical record due to the COVID-19 pandemic gave them confidence that they could conduct the intervention virtually and become diabetes technology experts.
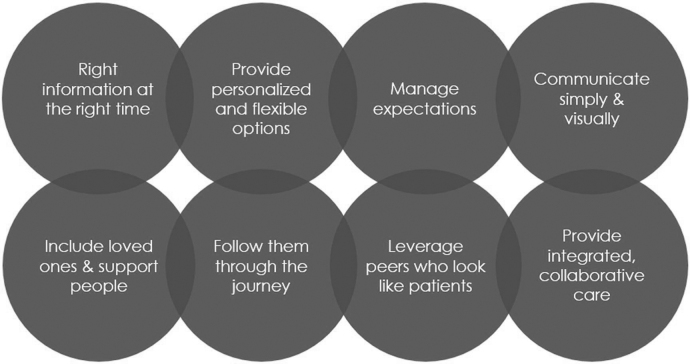
Lastly, stakeholders discussed program principles of interventions that would enable success, displayed in Figure 3. These included giving the right information at the right time, providing accessible information including managing expectations, leveraging support networks, creating collaborative technology care, and supporting patients throughout the journey of technology use.
FIG. 3.
Program principles of interventions to increase diabetes technology use in underserved populations with type 1 diabetes.
Discussion
Our study highlights stakeholder-created multilevel solutions to increase use of diabetes technology for underserved populations with type 1 diabetes. Through our innovative approach, we were able to leverage the breadth and depth of new stakeholder views. Top intervention ideas included developing more accessible education using low-literacy visual and interactive materials, instituting equity in offering technology, leveraging peer and family support for initiating technology, and providing more insurance support to practices. User-centered design methodology is a unique and efficient tool in disparities research to elicit stakeholder lived experiences and to develop new collaborative ideas on solutions to address disparities.
Multiple studies in populations with type 1 diabetes have highlighted the role of the health care provider as the “gateway” to diabetes technology.15,18,19 Some studies suggest that overt or unconscious bias may be occurring and manifesting itself as lack of shared decision making and microaggressive language during medical encounters.18,33,42 Unconscious bias may degrade the patient–provider relationship and trust necessary for patients to accept new treatments, such that patients may be rejecting diabetes technology when offered.43–45 In our prior published study with patients, provider behaviors that instilled confidence in new technology use included optimism, tailoring of information, and clinical expertise.
Stakeholders commented that provider bias had to be addressed, but that bias training would not suffice. One study of an intervention to change provider-level biases in diabetes care using cultural competency training and race-stratified performance reports demonstrated that although clinicians acknowledged disparities in their patients' diabetes control, this knowledge alone did not empower them to address the complex root causes of disparities.53 Stakeholders discussed that the approach to educate and discuss technology had to be changed dramatically to include more hands-on and visual instructions and demos to bypass bias. Partnering with device companies to obtain demos and device trials has potential to demystify technology for patients and enhance practice ability to make technology feel more accessible. If there is a way to avoid marketing influence, partnerships with industry could provide practices with staff training and onboarding onto devices, and enhance provider ability to offer and support technology use.
In addition, training opportunities are needed to allow providers to role play technology introductory conversations to catch any language that inadvertently promotes implicit bias. Low-literacy visual educational aids on diabetes technology devices are available, some in English and Spanish, but are used sparingly in practice currently.46–48 Thus, simple low-touch interventions using readily available resources may be within reach for many practices and could be highly effective.49
While health care provider behavior is a key factor in technology use among underserved populations and needs to be a focused part of any intervention,50–52 it may not be enough. Stakeholders mentioned that system-level interventions were needed to eliminate current practices that make providers prone to prescribing biases. They discussed that instituting a mission of equity into practices was needed that both standardized care approaches and offered specialized tailoring to underserved populations.
It is also well known that patients struggling with social determinants of health require extra support, but receive lower quality care and suffer from worse health outcomes.54,55 Provider stakeholders noted specifically that they lacked the expertise to assess or help manage social needs that act as barriers to technology use. CHW stakeholders noted that they would be optimal in helping to assess social needs and introduce technology in a culturally responsive and less time-pressured way. Thus, the most effective solutions may require practice transformations and inclusion of other team members besides health care providers who are skilled in assessing and managing social needs.
Lastly, stakeholders emphasized the positive influence on technology use of extra support from friends and family. Multiple studies across diabetes and in other fields have demonstrated that inclusion of diabetes support networks in medical care results in higher engagement, improved medical and psychological outcomes, and better cultural competency.56,57 Thus, across the lifespan, it may be imperative to include family members and other support systems for diabetes technology initiation and management, especially given the real-time and complex self-management demands a new technological treatment may require.
Practices can develop informal peer-to-peer mentorship programs or connect patients with social media communities that are connected to technology to normalize and contextualize the use of devices for diabetes management, especially if patients can see others “like them.” Nevertheless, such platforms can provide misinformation, and any clinical advice should be directed to the health care provider.
Our study has several limitations. Given the intensive resources used in this methodology, it was not possible to increase our number of participants. To balance potential biases, we chose to leverage prior published qualitative results that represented >100 underserved patients with T1D to prioritize enrollment of a larger number and variety of providers who have largely been missing in the literature thus far. We also amplified views from stakeholders by encouraging collaborative real-time intervention development in our workshops, which provided unique and in-depth insights that have not been offered as of yet. We added rigor to our analytic approach by standardizing our analysis and by performing multiple cycles using multiple coding experts from a health care design company and our research team.
This study used a new approach to elicit unique cross-disciplinary solutions to increase diabetes technology use among underserved populations with type 1 diabetes. With our methodology, we provide researchers and clinicians with a suite of well-informed interventions that have been voted on by stakeholders as highly acceptable and impactful. Regardless of intervention, stakeholders emphasized the importance of changing the system and not only relying on the provider to change practice behaviors in a system that does not facilitate change. With the current wave of diversity, equity, and inclusion initiatives sweeping across academic medical centers in the United States,52,58 there is potential to use this study's data to transform the way we care for our underserved type 1 diabetes populations.
Supplementary Material
Acknowledgments
We thank all the stakeholders for their time and willingness to participate in this study.
Authors' Contributions
S.A. conceptualized, conducted, and analyzed the study, and wrote and edited the article. G.C.R., S.L.L., and M.F. conducted and analyzed the study, and edited the article. T.P. and K.M. conceptualized, conducted, and analyzed the study, and edited the article. J.S.G. edited the article. J.A.L. conceptualized and analyzed the study and edited the article. S.A. is the guarantor of this study and takes full responsibility for the contents of this article.
Author Disclosure Statement
S.A. is a health disparities advisor to Medtronic Inc. and Beta Bionics Inc. The other authors have nothing to disclose.
Funding Information
NIH-NIDDK K23DK115896-04, NIH-NIDDK P30DK111022-07.
Supplementary Material
References
- 1. Agarwal S, Kanapka LG, Raymond JK, et al. : Racial-ethnic inequity in young adults with type 1 diabetes. J Clin Endocrinol Metab 2020;105:e2960–e2969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Livingstone SJ, Levin D, Looker HC, et al. : Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008–2010. JAMA 2015;313:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saydah S, Imperatore G, Cheng Y, et al. : Disparities in diabetes deaths among children and adolescents—United States, 2000–2014. MMWR Morb Mortal Wkly Rep 2017;66:502–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chamberlain JJ, Dopita D, Gilgen E, Neuman A: Impact of frequent and persistent use of continuous glucose monitoring (CGM) on hypoglycemia fear, frequency of emergency medical treatment, and SMBG frequency after one year. J Diabetes Sci Technol. Published online 2015;10:383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gilbert T, Noar A, Blalock O, Polonsky W: Change in HbA1c and quality of life with real-time CGM use by people with insulin-treated diabetes in the landmark study. Diabetes Technol Ther 2021;23:S35–S39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Polonsky WH, Fortmann AL: Impact of real-time continuous glucose monitoring data sharing on quality of life and health outcomes in adults with type 1 diabetes. Diabetes Technol Ther 2020;23:195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Prahalad P, Tanenbaum M, Hood K, Maahs DM: Diabetes technology: improving care, improving patient-reported outcomes and preventing complications in young people with Type 1 diabetes. Diabet Med 2018;35:419–429. [DOI] [PubMed] [Google Scholar]
- 8. Tauschmann M: Technology in the management of type 1 diabetes mellitus—current status and future prospects. Nat Rev Endocrinol 2018;14:464–475. [DOI] [PubMed] [Google Scholar]
- 9. American Diabetes Association: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021;44(Suppl. 1):S1–S232.33298409 [Google Scholar]
- 10. Danne T, Nimri R, Battelino T, et al. : International consensus on use of continuous glucose monitoring. Diabetes Care 2017;40:1631–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agarwal S, Schechter C, Gonzalez J, Long JA: Racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther 2021;23:306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Willi S, Miller K, DiMeglio L, et al. : Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135:424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Foster NC, Beck RW, Miller KM, et al. : State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McKergow E, Parkin L, Barson DJ, et al. : Demographic and regional disparities in insulin pump utilization in a setting of universal funding: a New Zealand nationwide study. Acta Diabetol 2017;54:63–71. [DOI] [PubMed] [Google Scholar]
- 15. Agarwal S, Crespo-Ramos G, Long JA, Miller VA: “I didn't really have a choice”: qualitative analysis of racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther 2021;23:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lai CW, Lipman TH, Willi SM, Hawkes CP: Racial and ethnic disparities in rates of continuous glucose monitor initiation and continued use in children with type 1 diabetes. Diabetes Care 2021;44:255–257. [DOI] [PubMed] [Google Scholar]
- 17. Addala A, Auzanneau M, Miller K, et al. : A decade of disparities in diabetes technology use and HbA(1c) in pediatric type 1 diabetes: a transatlantic comparison. Diabetes Care 2021;44:133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Addala A, Hanes S, Naranjo D, et al. : Provider implicit bias impacts pediatric type 1 diabetes technology recommendations in the United States: findings from The Gatekeeper Study. J Diabetes Sci Technol 2021;15:1027–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walker AF, Hood KK, Gurka MJ, et al. : Barriers to technology use and endocrinology care for underserved communities with type 1 diabetes. Diabetes Care 2021;44:1480–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. World Health Organization: Healthy people 2020: social determinants of health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health (accessed April 1, 2018).
- 21. Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE: Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine 2014;47:29–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in type 2 diabetes. Gen Hosp Psychiatry 2014;36:662–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE: Quantifying direct effects of social determinants of health on glycemic control in adults with type 2 diabetes. Diabetes Technol Ther 2015;17:80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Berkowitz SA, Meigs JB, DeWalt D, et al. : Material need insecurities, control of diabetes mellitus, and use of health care resources. JAMA Intern Med 2015;175:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Berkowitz SA, Kalkhoran S, Edwards ST, et al. : Unstable housing and diabetes-related emergency department visits and hospitalization: a nationally representative study of safety-net clinic patients. Diabetes Care 2018;41:933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hill-Briggs F, Adler NE, Berkowitz SA, et al. : Social determinants of health and diabetes: a scientific review. Diabetes Care 2020;44:258–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Butler AM, Weller BE, Rodgers CR, Teasdale AE: Type 1 diabetes self-management behaviors among emerging adults: racial/ethnic differences. Pediatr Diabetes 2020;21:979–986. [DOI] [PubMed] [Google Scholar]
- 28. Syed M, Mitchell L: Race, ethnicity, and emerging adulthood: retrospect and prospects. Emerg Adulthood 2013;1:83–95. [Google Scholar]
- 29. Walker AF, Schatz DA, Johnson C, Silverstein HJRH: Disparities in social support systems for youths with type 1 diabetes. Clin Diabetes 2015;33:62–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Karb RA, Elliott MR, Dowd JB, Morenoff JD: Neighborhood-level stressors, social support, and diurnal patterns of cortisol: the Chicago Community Adult Health Study. Soc Sci Med 2012;75:1038–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hessler D, Bowyer V, Gold R, et al. : Bringing social context into diabetes care: intervening on social risks versus providing contextualized care. Curr Diab Rep 2019;19:30. [DOI] [PubMed] [Google Scholar]
- 32. Mani N, Caiola E, Fortuna RJ: The influence of social networks on patients' attitudes toward type II diabetes. J Community Health 2011;36:728–732. [DOI] [PubMed] [Google Scholar]
- 33. Hall WJ, Chapman MV, Lee KM, et al. : Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health 2015;105:e60–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hagiwara N, Elston Lafata J, Mezuk B, et al. : Detecting implicit racial bias in provider communication behaviors to reduce disparities in healthcare: challenges, solutions, and future directions for provider communication training. Patient Educ Couns 2019;102:1738–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Barajas CB, Jones SCT, Milam AJ, et al. : Coping, discrimination, and physical health conditions among predominantly poor, urban African Americans: implications for community-level health services. J Community Health 2019;44:954–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pugh M Jr, Perrin PB, Rybarczyk B, Tan J: Racism, mental health, healthcare provider trust, and medication adherence among black patients in safety-net primary care. J Clin Psychol Med Settings 2021;28:181–190. [DOI] [PubMed] [Google Scholar]
- 37. Addala A, Maahs DM, Scheinker D, et al. : Uninterrupted continuous glucose monitoring access is associated with a decrease in HbA1c in youth with type 1 diabetes and public insurance. Pediatr Diabetes 2020;21:1301–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Clements MA, Schwandt A, Donaghue KC, Miller K, Lück U, Couper JJ, Foster N, Schröder C, Phelan H, Maahs D, Prinz N, Craig ME; on behalf of the Australasian Diabetes Data Network (ADDN) Study Group, the T1D Exch and the GD (DPV) initiative. Five heterogeneous HbA1c trajectories from childhood to adulthood in youth with type 1 diabetes from three different continents: a group-based modeling approach. Pediatr Diabetes 2019;20:920–931. [DOI] [PubMed] [Google Scholar]
- 39. Kahkoska AR, Shay CM, Crandell J, et al. : Association of race and ethnicity with glycemic control and hemoglobin A1c levels in youth with type 1 diabetes. JAMA Netw Open 2018;1:e181851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The United States Census Bureau: QuickFacts: Bronx County. 2019. https://www.census.gov/quickfacts/bronxcountybronxboroughnewyork (accessed June 13, 2020).
- 41. Addala A, Suttiratana SC, Wong JJ, et al. : Cost considerations for adoption of diabetes technology are pervasive: a qualitative study of persons living with type 1 diabetes and their families. Diabet Med 2021;38:e14575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sukhera H, Michael W, Milne A, et al. : Implicit bias and the feedback paradox: exploring how health professionals engage with feedback while questioning its credibility. Acad Med 2019;94:1204–1210. [DOI] [PubMed] [Google Scholar]
- 43. Huang ES, Brown SE, Thakur N, et al. : Racial/ethnic differences in concerns about current and future medications among patients with type 2 diabetes. Diabetes Care 2009;32:311–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dang BN, Westbrook RA, Njue SM, Giordano TP: Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study. BMC Med Educ 2017;17:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Pérez-Stable EJ, El-Toukhy S: Communicating with diverse patients: how patient and clinician factors affect disparities. Patient Educ Couns 2018;101:2186–2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ruelas VF, Walker MA, Peters AL: The STEPP-UP Project—Designing low literacy teaching tools for use of devices in a minority population. Diabetes 2018;67(Suppl. 1):2227-PUB.30181160 [Google Scholar]
- 47. Diabetes Wise: Helping you find the right diabetes devices for your life. DiabetesWise.org (accessed October 1, 2021).
- 48. American Diabetes Association: American Diabetes Association Consumer Guide: Products. 2021. https://consumerguide.diabetes.org/
- 49. Mbanda N, Dada S, Bastable K, et al. : A scoping review of the use of visual aids in health education materials for persons with low-literacy levels. Patient Educ Couns 2021;104:998–1017. [DOI] [PubMed] [Google Scholar]
- 50. Berkman ND, Sheridan SL, Donahue KE, et al. : Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- 51. Agency for Healthcare Research and Quality: Consumer assessment of healthcare providers and systems. 2005. https://www.ahrq.gov/cahps/index.html (accessed April 1, 2018).
- 52. Golden SH, Joseph JJ, Hill-Briggs F: Casting a health equity lens on endocrinology and diabetes. J Clin Endocrinol Metab 2021;106:e1909–e1916. [DOI] [PubMed] [Google Scholar]
- 53. Thorlby R, Jorgensen S, Ayanian JZ, Sequist TD: Clinicians' views of an intervention to reduce racial disparities in diabetes outcomes. J Natl Med Assoc 2011;103:968–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Agency for Healthcare Research and Quality: 2019 National Healthcare Quality and Disparities Report. 2019. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr19/index.html (accessed October 1, 2021). [PubMed]
- 55. ATSDR: Agency for Toxic Substances and Disease Registry. CDC/ATSDR Social Vulnerability Index. Centers for Disease Prevention and Control: Place and Health. 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html (accessed July 6, 2021).
- 56. Baig AA, Benitez A, Quinn MT, Burnet DL: Family interventions to improve diabetes outcomes for adults. Ann N Y Acad Sci 2015;1353:89–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hilliard ME, Powell PW, Anderson BJ: Evidence-based behavioral interventions to promote diabetes management in children, adolescents, and families. Am Psychol 2016;71:590–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Roberts BT, Rodgers GP: NIDDK initiatives addressing health disparities in chronic diseases. J Clin Invest 2020;130:5036–5038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.