Background:
Anterior cruciate ligament (ACL) injury is considered a risk factor for osteoarthritis. The primary aim of the present study was to investigate the cumulative risk of, and risk factors associated with, a subsequent knee arthroplasty after an ACL reconstruction at up to 15 years of follow-up. The secondary aim was to compare the relative risk of knee arthroplasty after ACL reconstruction compared with that in the general population.
Methods:
Data were analyzed by combining data from 2 national registries, the Norwegian Knee Ligament Register and the Norwegian Arthroplasty Register. The cumulative risk of knee arthroplasty after undergoing ACL reconstruction was calculated as 1 minus the corresponding Kaplan-Meier estimate, and possible risk factors for knee arthroplasty after ACL reconstruction were assessed in a Cox regression model with hazard ratios (HRs) as estimated effect measurements. The relative risk of knee arthroplasty for patients managed with ACL reconstruction as compared with that in the general population was calculated in stratified age groups.
Results:
From the study population of 27,122 knees, 115 knees underwent knee arthroplasty. We found a 1.1% (95% confidence interval [CI], 0.9 to 1.4) cumulative risk of knee arthroplasty 15 years after ACL reconstruction. Deep cartilage injury, ICRS (International Cartilage Repair Society) grade 3 to 4 (HR, 4.8; 95% CI, 3.1 to 7.6), revision of the ACL (HR, 3.9; 95% CI, 2.2 to 7.1), and a 2-year postoperative KOOS Sport/Recreation subscore of <44 (HR, 3.1; 95% CI, 1.5 to 6.2) were important risk factors for knee arthroplasty. We found a higher risk of knee arthroplasty at the age of 30 to 39 years after a previous ACL reconstruction as compared with the general population (relative risk, 3.3; 95% CI, 1.6 to 6.7).
Conclusions:
Fifteen years after an ACL reconstruction, the overall cumulative risk of knee arthroplasty was 1.1%. Cartilage injury at the time of ACL reconstruction, revision ACL reconstruction, and a KOOS Sport/Recreation subscore of <44 (at 2 years postoperatively) were major risk factors for subsequent knee arthroplasty. We found a 3.3-times higher risk of knee arthroplasty at the age of 30 to 39 years after a previous ACL reconstruction as compared with that in the general population.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
An anterior cruciate ligament (ACL) injury has been considered a risk factor for early onset and accelerated progression of osteoarthritis (OA) at a relatively young age1. The primary goal of ACL reconstruction is to restore knee stability, allowing the patient to resume their preinjury activities2. Because of the lack of randomized controlled trials, it is difficult to investigate whether ACL reconstruction alters the risk of development of OA3,4.
Knee arthroplasty is an effective end-stage treatment of knee OA, restoring function, mobility, and quality of life in the vast majority of patients5. Knee arthroplasty has become the gold standard for the management of disability and persistent pain associated with knee OA6. Abram et al.7 analyzed data on >110,000 ACL reconstructions in the U.K., utilizing the national health-care records for England from 1997 to 2017, and found that 0.97% of patients with ACL reconstruction had knee arthroplasty within 10 years. Two case-control studies have suggested that ACL injury may be associated with up to 7 times greater odds of knee arthroplasty compared with the general population8,9, and a recent review presented concomitant meniscal injury as a risk factor for radiographic OA after 20 years10.
The Norwegian Knee Ligament Register (NKLR) was established in 2004 as the world’s first cruciate ligament register11. Reporting to the NKLR is mandatory, and all hospitals in the country participate. The NKLR holds a more extensive dataset than has been used in previous studies, allowing for a more detailed assessment of risk factors for knee arthroplasty after ACL reconstruction. The number of knee arthroplasties in patients reported to the NKLR is unknown. By linking the NKLR data to the Norwegian Arthroplasty Register (NAR), subsequent knee arthroplasties can be identified.
The primary aim of the present study was to investigate 10 and 15-year cumulative risk of, and possible risk factors associated with, a subsequent knee arthroplasty after an ACL reconstruction. The secondary aim was to compare the relative risk (RR) for knee arthroplasty after ACL reconstruction compared with an age-stratified group from the general population.
Materials and Methods
Study Setting and Population
This manuscript was written in accordance with the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) statement12.
This Level-II prospective cohort study combined data from 2 national medical quality registries, the NKLR and NAR. The NKLR is designed to collect information prospectively on all cases of cruciate ligament reconstruction surgery and covers approximately 85% to 90% of all ACL reconstructions performed in Norway13. All subsequent surgical procedures performed on these knees are to be reported to the register. Each year, approximately 2,000 ACL reconstructions are reported to the NKLR. Patients who are included in NKLR report the Knee injury and Osteoarthritis Outcome Score (KOOS)14 preoperatively and at 2, 5, and 10 years postoperatively, and the function in sport and recreation (KOOS Sport/Rec) and knee-related quality of life (KOOS QOL) subscores at 2 years were analyzed. The NAR began recording knee arthroplasties in Norway in 1994. Approximately 6,000 knee arthroplasties are recorded each year, and the completeness of reporting has been reported to be >97%13. Every person in Norway has a unique personal identification number, which allowed us to identify conversions to knee arthroplasty after primary ACL reconstruction from the NAR.
All patients who were reported to the NKLR from its establishment in 2004 to December 31, 2020, were eligible for inclusion. Isolated posterior cruciate ligament reconstructions, multiligament injuries (defined those involving a minimum of 3 ligaments), and knees with missing details from graft, meniscus, and cartilage findings and treatment were excluded.
The following variables were obtained from the NKLR: patient-specific factors, intraoperative findings, surgical details, and KOOS Sport/Rec and QOL subscores at 2 years of follow-up. The following variables were obtained from the NAR on primary knee replacement: date of surgery, surgeon-reported cause of knee arthroplasty, and type of knee arthroplasty.
Statistical Analysis
We used survival analysis with knee arthroplasty as the end point. Survival times of patients with reconstructed ACLs were censored at the date of death (n = 145) or at the end of study (December 31, 2020). Patients who had emigrated were excluded. Cumulative incidences are reported in plots and tables (with point estimates at 10 and 15 years) and were calculated as 1 minus the corresponding Kaplan-Meier estimates. Possible risk factors for knee arthroplasty after ACL reconstruction were assessed in a Cox regression model with hazard ratios (HRs) as estimated effect measurements. The model included adjustment for gender, age group at the time of ACL reconstruction (<20, 20 to 29, 30 to 39, 40 to 49, 50 to 59, ≥60 years), injury (none, International Cartilage Repair Society [ICRS] grade 1 to 2, ICRS grade 3 to 4), meniscal injury (none, no treatment, resection, suture), graft (bone-patellar tendon-bone [BPTB], hamstring, other), graft revision (yes or no), KOOS Sport/Rec subscore (<44 or ≥44), and KOOS knee-related QOL subscore (<44 or ≥44). Since nearly 50% of the included patients had failed to report their KOOS scores at 2 years of follow-up, those KOOS scores were excluded in the model when assessing the other possible risk factors, and the level of 44 points was chosen because of the association between graft failure and KOOS Sport/Rec and knee-related QOL subscores of <4414. Survival times were calculated as the time between primary reconstruction of the ACL and primary knee arthroplasty, with censoring at the time of death (n = 123) or at the end of the study on December 31, 2020.
We compared the risk of undergoing knee arthroplasty after ACL reconstruction with the risk of undergoing knee arthroplasty in the general population. The results are reported as annual rates per 100,000 and as RR estimates stratified by age groups (20 to 79 years at 10-year intervals). The age-stratified estimated risk of knee arthroplasty after ACL was calculated by dividing the number of ipsilateral knee arthroplasties after reconstruction of an ACL (reported to the NAR) by the total number of reconstructed ACLs reported to the NKLR (first knee only). The estimated risk of undergoing knee arthroplasty in the general population (stratified by age group) was calculated by dividing the number of knee arthroplasties reported to the NAR in patients without any previous ligament injury or surgery involving cruciate ligaments (first knee only) between January 1, 2004, and December 31, 2020, by the average number of Norwegian citizens as obtained from Statistics Norway during the same time span.
STATA/SE (version 17.0; StataCorp) was used for statistical analysis. The level of significance was set at p < 0.05.
Ethics
Before enrollment in the NKLR and NAR, patients provided informed consent. The study was approved by the Regional Ethics Committee (reference number 81188).
Source of Funding
The study was funded by the NKLR.
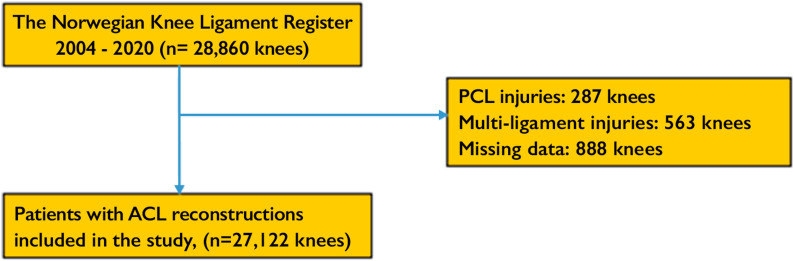
Results
Of the 28,860 knees in the NKLR that had been treated with ACL reconstruction from 2004 to 2020, 1,738 were excluded (Fig. 1). We included 27,122 knees in the study, of which 115 had a knee replacement (including 112 total knee arthroplasties [TKAs] and 3 unicompartmental knee arthroplasties). The mean age (and standard deviation) at the time of ACL reconstruction was 29 ± 11 years, 56% of the knees were in male patients, and the median duration of follow-up was 8 years.
Fig. 1.
Flowchart. PCL = posterior cruciate ligament.
Fifteen-Year Cumulative Risk of Knee Arthroplasty
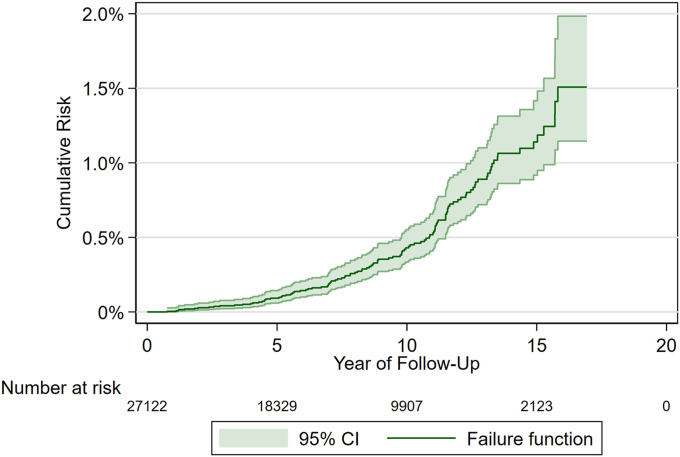
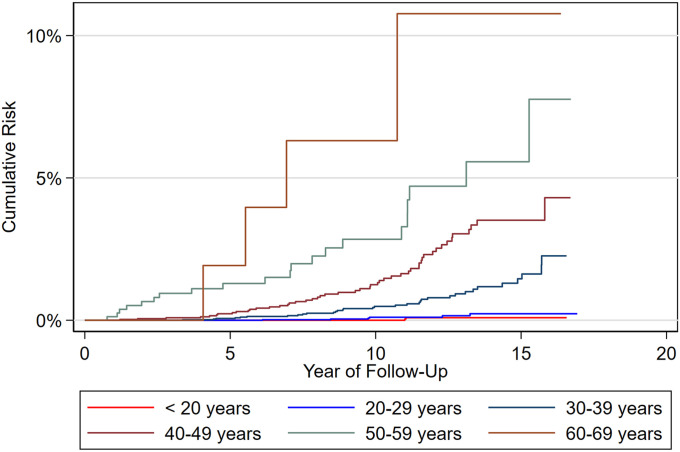
We found that the 15-year cumulative risk of knee arthroplasty after ACL reconstruction was 1.1% (95% confidence interval [CI], 0.9 to 1.4) (Fig. 2). The cumulative risk of knee replacement was significantly higher in patients who were older at the time of the index ACL reconstruction (Fig. 3, Table I).
Fig. 2.
Cumulative risk of knee arthroplasty following ACL reconstruction.
Fig. 3.
Cumulative risk of knee arthroplasty according to age at the time of the index ACL reconstruction.
TABLE I.
Ten and 15-Year Cumulative Risk of, and Risk Factors Associated with, Knee Arthroplasty After ACL Reconstruction (2004 to 2020)
| No. of ACL Reconstructions | No. of Knee Arthroplasties* | Cumulative Risk, 1 – Kaplan-Meier† (%) | Crude HR†‡ | Adjusted HR†§ | ||
|---|---|---|---|---|---|---|
| 10 Years | 15 Years | |||||
| Total | 27,122 (100%) | 115 (4.2%) | 0.43 (0.34-0.55) | 1.14 (0.92-1.42) | — | — |
| Age at time of ACL reconstruction | ||||||
| <20 yr | 7,337 (27.1%) | 2 (0%) | 0.00 | 0.09 (0.02-0.36) | 0.4 (0.1-2.0) | 0.4 (0.1-1.8) |
| 20-29 yr | 8,845 (32.6%) | 6 (0.1%) | 0.11 (0.04-0.29) | 0.23 (0.09-0.55) | 1 | 1 |
| 30-39 yr | 6,161 (22.7%) | 33 (0.5%) | 0.49 (0.3-0.79) | 1.46 (0.95-2.22) | 7.0 (2.9-16.6) | 6.5 (2.7-15.7) |
| 40-49 yr | 3,869 (14.3%) | 49 (1.3%) | 1.25 (0.85-1.84) | 3.51 (2.57-4.79) | 18.7 (8.0-43.6) | 15.2 (6.5-35.9) |
| 50-59 yr | 836 (3.1%) | 21 (2.5%) | 2.84 (1.68-4.8) | 5.57 (3.32-9.25) | 41.9 (16.9-103.8) | 29.9 (11.9-75.5) |
| ≥60 yr | 74 (0.3%) | 4 (5.4%) | 6.31 (2.07-18.39) | 10.77 (3.86-28.07) | 89.1 (25.1-315.9) | 53.9 (14.9-194.7) |
| Sex | ||||||
| Male | 15,105 (55.7%) | 57 (0.4%) | 0.39 (0.27-0.55) | 0.95 (0.7-1.28) | 1 | 1 |
| Female | 12,017 (44.3%) | 58 (0.5%) | 0.49 (0.34-0.69) | 1.40 (1.02-1.91) | 1.3 (0.9-1.9) | 1.6 (1.1-2.3) |
| Graft | ||||||
| BPTB | 11,808 (43.5%) | 43 (0.4%) | 0.56 (0.37-0.83) | 1.31 (0.92-1.87) | 1 | 1 |
| Hamstring | 14,600 (53.8%) | 72 (0.5%) | 0.39 (0.28-0.53) | 1.06 (0.81-1.38) | 0.8 (0.6-1.2) | 0.9 (0.6-1.3) |
| Other | 714 (2.6%) | 0 (0.0%) | 0.00 | 0.00 | — | — |
| Graft revision | ||||||
| No | 25,707 (94.8%) | 103 (0.4%) | 0.40 (0.31-0.53) | 1.10 (0.87-1.39) | 1 | 1 |
| Yes | 1,415 (5.2%) | 12 (0.8%) | 0.78 (0.39-1.57) | 1.65 (0.89-3.05) | 1.7 (0.9-3.0) | 3.9 (2.2-7.1) |
| Meniscal injury | ||||||
| No | 12,360 (45.6%) | 53 (0.4%) | 0.41 (0.29-0.58) | 0.89 (0.66-1.20) | 1 | 1 |
| No treatment | 1,587 (5.9%) | 11 (0.7%) | 0.50 (0.20-1.23) | 2.31 (1.15-4.60) | 1.8 (1.0-3.5) | 1.4 (0.7-2.7) |
| Resection | 7,760 (28.6%) | 46 (0.6%) | 0.61 (0.42-0.89) | 1.39 (0.98-1.96) | 1.4 (0.9-2.0) | 1.0 (0.7-1.5) |
| Suture | 5,415 (20.0%) | 5 (0.1%) | 0.00 | 1.09 (0.44-2.65) | 0.4 (0.2-1.1) | 0.7 (0.3-1.8) |
| Cartilage injury | ||||||
| No | 20,762 (76.6%) | 44 (0.2%) | 0.21 (0.14-0.32) | 0.54 (0.39-0.76) | 1 | 1 |
| ICRS grade 1-2 | 4,447 (16.4%) | 32 (0.7%) | 0.72 (0.45-1.13) | 1.69 (1.15-2.49) | 3.2 (2.1-5.1) | 2.1 (1.5-3.4) |
| ICRS grade 3-4 | 1,913 (7.1%) | 39 (2.0%) | 2.15 (1.43-3.25) | 5.93 (4.05-8.64) | 9.5(6.1-14.6) | 4.8 (3.1-7.6) |
| KOOS Sport/Rec subscore | ||||||
| <44 | 3,092 (20.5%) of 15,099 | 49 (1.6%) | 1.39 (0.96-2.02) | 3.32 (2.43-4.54) | 7.9 (4.8-13.0) | 3.1 (1.5-6.2)# |
| ≥44 | 12,007 (79.5%) of 15,099 | 23 (0.2%) | 0.15 (0.08-0.27) | 0.52 (0.31-0.87) | 1 | 1 |
| KOOS QOL subscore | ||||||
| <44 | 3,366 (22.3%) of 15,120 | 46 (1.4%) | 1.31 (0.91-1.9) | 3.02 (2.15-4.22) | 6.0 (3.7-9.6) | 2.5 (1.3-5.0)# |
| ≥44 | 11,754 (77.7%) of 15,120 | 27 (0.2%) | 0.17 (0.09-0.3) | 0.59 (0.37-0.93) | 1 | 1 |
The percentages in this column are based on the number of total knee arthroplasties as shown in the previous column.
The 95% CI is given in parentheses.
HR = hazard rate ratio from Cox analysis.
Cox analysis adjusted for all other variables except the KOOS subscores Sport/Rec and QOL.
Sport/Rec and QOL: adjusted for all other variables. Some patients reported one score and not the other; as such, 12,023 cases were excluded because of unreported KOOS scores.
Risk Factors for Knee Arthroplasty
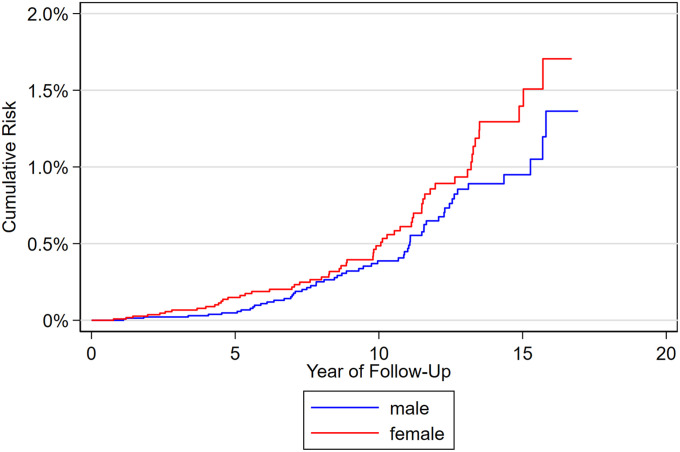
Patients who had ACL reconstruction at the age of 50 to 59 years (HR, 29.9; 95% CI, 11.9 to 75.5) were significantly more likely to have undergone subsequent knee arthroplasty within the previous 15 years in comparison with patients who had undergone ACL reconstruction at the age of 20 to 29 years. Figure 4 presents the cumulative risk of knee arthroplasty following ACL reconstruction by sex. Female patients with ACL reconstruction had a higher risk of knee arthroplasty compared with males (HR, 1.6; 95% CI, 1.1 to 2.3) (Table I).
Fig. 4.
Cumulative risk of knee arthroplasty following ACL reconstruction by sex.
Deep cartilage injury (ICRS 3 to 4) was an important risk factor for knee replacement surgery and was associated with an HR of 4.8 (95% CI, 3.1 to 7.6). Patients who had undergone revision of the ACL (HR, 3.9; 95% CI, 2.2 to 7.1) were more likely to undergo knee arthroplasty as compared with those who had not. The 2-year postoperative KOOS data showed that low function (Sport/Rec subscore, <44) was a risk factor for subsequent knee arthroplasty. Meniscal injury and graft choice (BPTB, hamstring, or other grafts) were not found to be risk factors for subsequent knee arthroplasty (Table I).
Risk of Knee Arthroplasty Compared with General Population
The annual rates and relative risks of knee arthroplasty after ACL reconstruction as compared with the general population are described in Table II. The risk of knee arthroplasty compared with the general population varied between the age groups, and the RR for a knee arthroplasty at the age 30 to 39 years was 3.3 (95% CI, 1.6 to 6.7) for patients with a previous ACL reconstruction compared to the general population. However, among patients aged 60 to 69 years, the RR was 0.5 (95% CI, 0.3 to 0.8).
TABLE II.
Relative Risk (RR) of Undergoing Knee Arthroplasty with a History of ACL Reconstruction Compared with the General Population without ACL Reconstruction
| Age at Knee Arthroplasty | Total No. of Knee Arthroplasties | Mean Annual Rate of Knee Arthroplasty in 2004-2020, per 100,000 | RR | 95% CI | |
|---|---|---|---|---|---|
| Patients with Prior ACL Reconstruction | General Population | ||||
| 30-39 yr | 8 | 6.1 | 1.9 | 3.29 | 1.63-6.66 |
| 40-49 yr | 35 | 36.8 | 17.1 | 2.15 | 1.54-3.00 |
| 50-59 yr | 57 | 97.7 | 91.1 | 1.07 | 0.83-1.39 |
| 60-69 yr | 14 | 117.3 | 251.1 | 0.47 | 0.28-0.79 |
| 70-79 yr | 1 | 82.9 | 409.2 | 0.20 | 0.03-1.42 |
Discussion
The main finding of the present study was that, 15 years after ACL reconstruction, the cumulative risk of knee arthroplasty was 1.1%. Deep cartilage injury (ICRS grade 3 to 4) at the time of ACL reconstruction, revision ACL reconstruction, and a KOOS Sport/Rec subscore of <44 at 2 years postoperatively were major risk factors for subsequent knee arthroplasty. Patients with ACL reconstruction had a more than threefold higher risk of knee arthroplasty at the age of 30 to 39 years than the general population.
Fifteen-Year Cumulative Risk of Knee Arthroplasty
Abram et al.7, in a U.K. study, found a cumulative 10-year risk of knee arthroplasty (0.97%). Leroux et al.9 identified all patients who had undergone cruciate ligament reconstruction in Ontario, Canada from 1993 to 2008, and matched them to individuals without previous knee surgery. After 15 years, the cumulative incidence of knee arthroplasty was 1.4% following cruciate ligament reconstruction and 0.2% in the matched control patients from the general population. Grassi et al.10, in a systematic review involving 1,771 patients who had been followed for at least 20 years after ACL reconstruction, reported that TKA was performed in 1.1% of patients. Khan et al.8, in a 20-year follow-up study involving 49,723 individuals who had undergone TKA and 104,353 controls, found that 153 (0.31%) of the patients in the TKA group had sustained an ACL injury, compared with 41 (0.04%) of the controls.
Our study had 2,123 knees at risk after 15 years, and therefore we are able to present robust 15-year cumulative risk estimates15. The incidence of knee arthroplasty may depend on different indications for knee arthroplasty in different countries; Ackerman et al.16 found that, in 2013, Norwegians had a lower lifetime risk of TKA (10% for females and 6% for males) than Australians (21% for females and 15% for males). The use of physiotherapy that includes education and supervised exercise may reduce the need for knee arthroplasty17.
Risk Factors for Knee Arthroplasty
We found that deep cartilage injury (ICRS grade 3 to 4) was a strong risk factor for, and was associated with the high risk of, knee arthroplasty. ACL revision was a major risk factor for subsequent knee arthroplasty, and one associated factor could be subsequent knee trauma, possibly with a new cartilage injury. Focal cartilage defects in the knee seem to impair quality of life as much as severe OA does18. To date, no surgical treatment of focal cartilage lesions has been shown to reduce the risk of later development of OA19. In the present study, a KOOS Sport/Rec subscore of <44 at 2 years postoperatively was associated with later knee arthroplasty. However, the rate of reporting of KOOS scores at 2 years was only 56%, and therefore the adjusted HR for the other variables could not be adjusted for the Sport/Rec subscore. Granan et al.20 investigated KOOS data at 2 years postoperatively, comparing patients who went on to have a revision with those who did not, and observed an increased risk of failure in patients who had KOOS QOL and Sport/Rec subscores of <44 at 2 years after the index ACL reconstruction. We did not find meniscal injury to be an independent risk factor for subsequent knee arthroplasty, independent of treatment of the lesion. We also performed a subanalysis regarding treatment strategy, but this factor did not influence the result. Abram et al.7 surprisingly observed reduced rates of knee arthroplasty in patients who had undergone ACL reconstruction and simultaneous meniscal surgery (partial meniscectomy or repair). In contrast, on the basis of 20-year longitudinal data, Khan et al.8 found that meniscal injury was associated with approximately 15-fold increased odds of TKA for OA. Papalia et al.21, in a systematic review of OA after total or partial meniscectomy, found an overall mean prevalence of OA of 53% in the operatively treated knee, compared with a range of 0% to 44% in the contralateral, non-operatively treated knee, after a mean follow-up of 13.3 years. Our findings may be explained by the relatively short follow-up and the young age of the patients. The peak age of knee arthroplasty is 68 years, and, for patients who were 20 years of age at the time of ACL surgery, we would need up to 50 years of follow-up to have robust estimates.
The present study did not demonstrate any difference in the risk of knee arthroplasty according to graft choice. Since 2012, the most popular graft choice in Norway has changed from hamstring grafts to BPTB grafts. A previous study based on data from the NKLR showed that patients with hamstring grafts had twice the risk of revision compared with patients with patellar tendon grafts22, and the same results were also found in another Scandinavian study23.
The Risk of Knee Arthroplasty Compared with the General Population
In the present study, the risk of a subsequent knee arthroplasty increased with age. Although the patients in the youngest age group had the lowest risk, they had a significantly higher risk than the general population (Table II). The risk of knee arthroplasty at the age of 30 to 39 years was 3 times higher among patients who had had a previous ACL reconstruction as compared with the general population. The oldest patients who had ACL reconstruction at the age of ≥60 years had a lower risk of knee arthroplasty compared with the general population. This may be explained by the selection of the candidates of ACL reconstruction at relative old age in Norway. They are probably also a group of well-functioning adults, which may explain their reduced risk of knee arthroplasty compared with the general population. When the follow-up time from the NKLR increases, these estimates may change.
The present registry study had limitations. Approximately 85% to 90% of ACL reconstructions are reported in the NKLR, compared with >97% of knee arthroplasties in the NAR. The registry data are limited to information that can be readily and reliably collected at the time of surgery; therefore, some important information that may affect the risk of knee arthroplasty is not available. Most studies have included radiographic OA data, but the NKLR has no such data. However, using knee arthroplasty as an end point for OA will help to distinguish between severe disease and minor disability. As the NKLR was started in 2004, the maximum follow-up time in the present study was 17 years. The strength of the registries lies in the number of patients who can be evaluated24 and the almost-complete records of knee replacements (>97% completeness of reporting in the study period13).
Conclusions
The main finding of the present study was that, at 15 years after ACL reconstruction, the cumulative risk of knee arthroplasty was 1.1%. Cartilage injury at the time of ACL reconstruction, revision ACL reconstruction, and a KOOS Sport/Rec subscore of <44 at 2 years postoperatively were major risk factors for subsequent knee arthroplasty. We found a 3.3-times higher risk of knee arthroplasty at the age of 30 to 39 years after a previous ACL reconstruction compared with the general population.
Footnotes
Investigation performed at the Norwegian Knee Ligament Register, Department of Orthopedic Surgery, Haukeland University Hospital, Bergen, Norway
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A396).
References
- 1.Lie MM, Risberg MA, Storheim K, Engebretsen L, Øiestad BE. What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med. 2019. Sep;53(18):1162-7. [DOI] [PubMed] [Google Scholar]
- 2.Friel NA, Chu CR. The role of ACL injury in the development of posttraumatic knee osteoarthritis. Clin Sports Med. 2013. Jan;32(1):1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, Davies A. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014. Sep;42(9):2242-52. [DOI] [PubMed] [Google Scholar]
- 4.Lien-Iversen T, Morgan DB, Jensen C, Risberg MA, Engebretsen L, Viberg B. Does surgery reduce knee osteoarthritis, meniscal injury and subsequent complications compared with non-surgery after ACL rupture with at least 10 years follow-up? A systematic review and meta-analysis. Br J Sports Med. 2020. May;54(10):592-8. [DOI] [PubMed] [Google Scholar]
- 5.Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ. Knee replacement. Lancet. 2012. Apr 7;379(9823):1331-40. [DOI] [PubMed] [Google Scholar]
- 6.Skou ST, Roos EM, Laursen MB, Rathleff MS, Arendt-Nielsen L, Simonsen O, Rasmussen S. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med. 2015. Oct 22;373(17):1597-606. [DOI] [PubMed] [Google Scholar]
- 7.Abram SGF, Judge A, Khan T, Beard DJ, Price AJ. Rates of knee arthroplasty in anterior cruciate ligament reconstructed patients: a longitudinal cohort study of 111,212 procedures over 20 years. Acta Orthop. 2019. Dec;90(6):568-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khan T, Alvand A, Prieto-Alhambra D, Culliford DJ, Judge A, Jackson WF, Scammell BE, Arden NK, Price AJ. ACL and meniscal injuries increase the risk of primary total knee replacement for osteoarthritis: a matched case-control study using the Clinical Practice Research Datalink (CPRD). Br J Sports Med. 2019. Aug;53(15):965-8. [DOI] [PubMed] [Google Scholar]
- 9.Leroux T, Ogilvie-Harris D, Dwyer T, Chahal J, Gandhi R, Mahomed N, Wasserstein D. The risk of knee arthroplasty following cruciate ligament reconstruction: a population-based matched cohort study. J Bone Joint Surg Am. 2014. Jan 1;96(1):2-10. [DOI] [PubMed] [Google Scholar]
- 10.Grassi A, Pizza N, Al-Zu’bi BBH, Fabbro GD, Lucidi GA, Zaffagnini S. Clinical Outcomes and Osteoarthritis at Very Long-term Follow-up After ACL Reconstruction: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2022. Jan 7;10(1):23259671211062238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008. Feb;36(2):308-15. [DOI] [PubMed] [Google Scholar]
- 12.Benchimol EI Smeeth L Guttmann A Harron K Moher D Petersen I Sørensen HT von Elm E Langan SM; Working Committee RECORD. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015. Oct 6;12(10):e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furnes O, Gjertsen JE, Hallan G, Visnes H, Gundersen T, Kvinnesland I, et al. Norwegian National Advisory Unit on Arthroplasty and Hip Fractures: Annual Report 2020. 2020. https://helse-bergen.no/seksjon/Nasjonal_kompetansetjeneste_leddproteser_hoftebrudd/Share%20point%20Documents/Rapport/Report%202020_english.pdf [Google Scholar]
- 14.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998. Aug;28(2):88-96. [DOI] [PubMed] [Google Scholar]
- 15.Sainani KL. Introduction to Survival Analysis. PM R. 2016. Jun;8(6):580-5. [DOI] [PubMed] [Google Scholar]
- 16.Ackerman IN, Bohensky MA, de Steiger R, Brand CA, Eskelinen A, Fenstad AM, Furnes O, Garellick G, Graves SE, Haapakoski J, Havelin LI, Mäkelä K, Mehnert F, Pedersen AB, Robertsson O. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003 to 2013: an international, population-level analysis. Osteoarthritis Cartilage. 2017. Apr;25(4):455-61. [DOI] [PubMed] [Google Scholar]
- 17.Skou ST, Roos EM. Good Life with osteoArthritis in Denmark (GLA:D™): evidence-based education and supervised neuromuscular exercise delivered by certified physiotherapists nationwide. BMC Musculoskelet Disord. 2017. Feb 7;18(1):72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heir S, Nerhus TK, Røtterud JH, Løken S, Ekeland A, Engebretsen L, Arøen A. Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of Knee injury and Osteoarthritis Outcome Score in 4 patient categories scheduled for knee surgery. Am J Sports Med. 2010. Feb;38(2):231-7. [DOI] [PubMed] [Google Scholar]
- 19.Hunziker EB, Lippuner K, Keel MJ, Shintani N. An educational review of cartilage repair: precepts & practice—myths & misconceptions—progress & prospects. Osteoarthritis Cartilage. 2015. Mar;23(3):334-50. [DOI] [PubMed] [Google Scholar]
- 20.Granan LP, Baste V, Engebretsen L, Inacio MC. Associations between inadequate knee function detected by KOOS and prospective graft failure in an anterior cruciate ligament-reconstructed knee. Knee Surg Sports Traumatol Arthrosc. 2015. Apr;23(4):1135-40. [DOI] [PubMed] [Google Scholar]
- 21.Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N. Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull. 2011;99:89-106. [DOI] [PubMed] [Google Scholar]
- 22.Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014. Feb;42(2):285-91. [DOI] [PubMed] [Google Scholar]
- 23.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014. Oct;42(10):2319-28. [DOI] [PubMed] [Google Scholar]
- 24.Maletis GB, Granan LP, Inacio MC, Funahashi TT, Engebretsen L. Comparison of community-based ACL reconstruction registries in the U.S. and Norway. J Bone Joint Surg Am. 2011. Dec 21;93(Suppl 3):31-6. [DOI] [PubMed] [Google Scholar]