Abstract
Background
Prehospital stroke triage scales help with the decision to transport patients with suspected stroke to suitable hospitals.
Objective
To explore the effect of the region-wide use of the Japan Urgent Stroke Triage (JUST) score, which can predict several types of stroke: large vessel occlusion (LVO), intracranial hemorrhage (ICH), subarachnoid hemorrhage (SAH), and cerebral infarction other than LVO (CI).
Methods
We implemented the JUST score and conducted a retrospective and prospective multicenter cohort study at 13 centers in Hiroshima from April 1, 2018, to March 31, 2020. We investigated the success rate of the first request to the hospital, on-scene time, and transport time to hospital. We evaluated the door-to-puncture time, puncture-to-reperfusion time, and 90-day outcome among patients with final diagnoses of LVO.
Results
The cohort included 5141 patients (2735 before and 2406 after JUST score implementation). Before JUST score implementation, 1269 strokes (46.4%) occurred, including 140 LVO (5.1%), 394 ICH (14.4%), 120 SAH (4.4%), and 615 CI (22.5%). The JUST score was used in 1484 (61.7%) of the 2406 patients after implementation, which included 1267 (52.7%) cases of stroke (186 LVO (7.7%), 405 ICH (16.8%), 109 SAH (4.5%), and 567 CI (23.6%)). Success rate of the first request to the hospital significantly increased after JUST score implementation (76.3% vs 79.7%, p=0.004). JUST score implementation significantly shortened the door-to-puncture time (84 vs 73 min, p=0.03), but the prognosis remained unaltered among patients with acute LVO.
Conclusions
Use of prehospital stroke triage scales improved prehospital management and preparation time of intervention among patients with acute stroke.
Keywords: stroke, hemorrhage, intervention, thrombectomy
Introduction
Patients with acute stroke require timely management and appropriate treatment, including intravenous thrombolysis, endovascular therapy, and neurosurgical interventions. The transportation of patients with suspected stroke to an appropriate hospital is critical because few hospitals are equipped to perform some of these treatments. The American Stroke Association recommends to first recognize the stroke, activate emergency medical services (EMS), triage to appropriate hospital, and designate capable stroke centers.1 It is also recommended that EMS should use a triage tool for patients with suspected stroke, such as the Cincinnati Prehospital Stroke Scale, Los Angeles Prehospital Stroke Screen, or Field Assessment Stroke Triage for Emergency Destination.2 These scales are commonly used and are reported to have good performance in screening patients with suspected acute large vessel occlusion (LVO). Capable hospitals have worked to shorten the door-to-reperfusion time to increase the chance for obtaining a good prognosis in patients with acute LVO.3 The delay in surgical or other interventions for intracranial hemorrhage (ICH) or subarachnoid hemorrhage (SAH) was also associated with poor prognosis.4 Therefore, early triage and transportation of patients with suspected stroke to the appropriate hospitals are crucial for acute LVO and the other types of stroke.5
We devised and reported two prehospital stroke triage scales—namely, the Japan Urgent Stroke Triage (JUST) score and seven-item Japan Urgent Stroke Triage (JUST-7) score, which can simultaneously distinguish between LVO, ICH, SAH, and cerebral infarction other than LVO (CI).6 7 In Japan, the JUST score is currently used by many EMS at the point of patient contact to determine the appropriate hospital for the treatment of the stroke. The impact of prehospital stroke triage scales for LVO and other forms of stroke has not been assessed in clinical practice. Therefore, we explored the effect of the implementation of the JUST score within clinical settings.
Methods
Study design and population
We conducted a prospective cohort study with a retrospective control cohort to assess the management of EMS in patients with suspected stroke at 13 hospitals in Hiroshima City from April 1, 2018, to March 31, 2020. The 13 participating hospitals were certified to conduct comprehensive stroke care and were staffed with qualified stroke physicians. We implemented the JUST score on April 1, 2019, at the Hiroshima City Fire Department. Thereafter, the cohort was investigated prospectively, while the cohort before March 31, 2019 was assessed retrospectively.6 The institutional review boards of all participating hospitals approved the study protocol. The requirement for written informed consent was waived for this study because we used information obtained during routine clinical practice. The institutional review boards approved this waiver in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
We enrolled consecutive patients suspected of having stroke events by EMS and transported to the participating hospitals. There were no age limits. We excluded the patients transferred from one hospital to another hospital because the patients were diagnosed before transportation. We also excluded those who were transported to hospitals other than the 13 participating hospitals.
The triage system in Hiroshima City
The JUST score was developed to predict the likelihood of any type of stroke and simultaneously estimates the probabilities of LVO, ICH, SAH, and CI. It comprises 21 items that can be easily evaluated by EMS and its high accuracy and predictive performance have been reported.6 Once patients were assessed at the first contact with the EMS, the EMS entered the items of the JUST score into a mobile device, which displayed the probabilities of any type of stroke as well as each type of stroke on the screen (online supplemental figure 1). Patients were subsequently classified into three groups according to the JUST scores: (1) patients with a high probability of LVO (triage ‘red’), (2) patients with a high probability of other types of stroke besides LVO (triage ‘yellow’), and (3) patients with a low probability of stroke (triage ‘green’). The triage thresholds were set as follows: ‘red’ if the probability of LVO was ≥25%, ‘yellow’ if the probability of LVO was <25% and that of the other types of stroke was ≥10%, and ‘green’ if the probability of any type of stroke was <10% (online supplemental figure 1). The thresholds were clinically determined by discussions among the investigators and EMS.
neurintsurg-2021-017863supp001.pdf (1.1MB, pdf)
Hiroshima City is the capital of Hiroshima Prefecture with a population of 1.2 million and an area spanning 906.68 km2. All EMS belonging to the Hiroshima City Fire Department (online supplemental table 1) and each of the 13 participating hospitals cover stroke care in Hiroshima City. The EMS of Hiroshima City Fire Department transported patients with suspected stroke to one of the 13 participating hospitals. The hospitals were predominantly located at the center of Hiroshima City, with the most distant hospitals within a 1-hour drive (online supplemental figure 2). Ten of the 13 hospitals were thrombectomy-capable and three provided recombinant tissue plasminogen activator (rtPA) only.
The 13 hospitals expressed their acceptance status for patients with stroke and availability of thrombectomy in real time and simultaneously shared the information with the EMS. If thrombectomy was available, the estimated door-to-puncture time (D2P) was displayed at four levels (within 60 min, 75 min, 90 min, and 120 min), based on the time slot (day vs night and weekday vs weekend), stand-by status of thrombectomy-capable physicians, and preparedness or occupation of operating rooms. The global positioning system function of the mobile device estimated the location of the EMS and calculated the transport time to the candidate hospitals. The EMS selected hospitals for ‘red’ triage patients in the order of the shortest total time of transport and D2P and in the order of the closest stroke-capable hospitals for ‘yellow’ triage patients. Patients designated with the ‘green’ triage after the JUST score implementation were generally transported to any of the 13 hospitals but occasionally transported to other hospitals.
Measurements and data collection
Certified EMS providers assessed the 21 items of the JUST score related to medical history, symptoms, and signs.6 We collected data on the number of requests to the hospitals, the on-scene time of EMS contact with patients, and transport time to the hospital. The request to the hospital was defined by when EMS contacted the participating hospital to ask for the transportation of patients who were suspected of having stroke events. The hospital then decided whether it could accept the request for transportation. If the hospital declined the request for reasons such as congestion of emergency rooms or occupation of operating rooms, the EMS made the next request to a different hospital. These data were recorded on paper or the internet and subsequently transferred to the electronic data capture system for further analysis.
The qualified stroke physicians working at the participating hospitals provided standardized care for the patients with suspected stroke and confirmed the diagnosis using CT or MRI. If the final diagnosis differed from the initial diagnosis, the former was considered to be the definitive diagnosis. If the diagnosis was uncertain, the qualified stroke physicians who were not aware of the predictive variables scrutinized the imaging and clinical data to reach a consensus through discussion.
We investigated the time from the onset of LVO, when the patient was last known to be well, to arrival at the hospital, the onset-to-door time (O2D). Furthermore, we investigated the modified Rankin Scale (mRS) scores before the onset of LVO,8 the National Institutes of Health Stroke Scale (NIHSS) score on admission,9 D2P, puncture to reperfusion time (P2R), the thrombolysis in cerebral infarction (TICI) scale,10 and mRS scores 90 days after the onset of stroke for patients with a final diagnosis of LVO. This information was entered into the electronic medical records and transferred to the electronic data capture system.
Outcomes
The outcomes included whether the first request to the hospital for the transportation of patients with suspected stroke was successful, on-scene time, and transport time. The mRS score of 0–2 or death (mRS score 6) at 90 days was considered as the outcome for patients with LVO. A second transfer to another hospital was also evaluated in patients with LVO. The D2P, P2R, and TICI scale of 2b or 3 were assessed for patients who underwent thrombectomy.
Statistical Analysis
We presented the categorical variables using numbers and percentages, and continuous variables using mean and SD or median and IQR. The variables obtained before and after implementation of the JUST score were presented separately and compared using the χ2 test for categorical variables, and t-test or Wilcoxon rank-sum test for continuous variables.
We compared the rate of use of rtPA and thrombectomy, as well as outcomes before and after implementation of the JUST score. We constructed univariable and multivariable logistic regression models for mRS scores of 0–2 and death at 90 days and estimated the crude and adjusted odds ratios (ORs) and their 95% confidence intervals (95% CIs). The risk-adjusting variables included in the multivariable logistic regression models were age, mRS score before onset, Alberta Stroke Program Early CT Score, occlusion site of the internal carotid artery or M1 segment of the middle cerebral artery, and O2D.
We assessed the difference in patients who were triaged or not triaged with the JUST score after implementation of the JUST score in the same manner as sensitivity analyses. We also compared the success of the first request to hospital by the χ2 test as well as on-scene time, and transport time by Wilcoxon rank-sum test between those triaged as red, yellow, or green.
All statistical analyses were conducted using JMP 15.0 (SAS Institute Inc., Cary, North Carolina, USA). Two-tailed p values of less than 0.05 were considered statistically significant.
Results
Patient characteristics
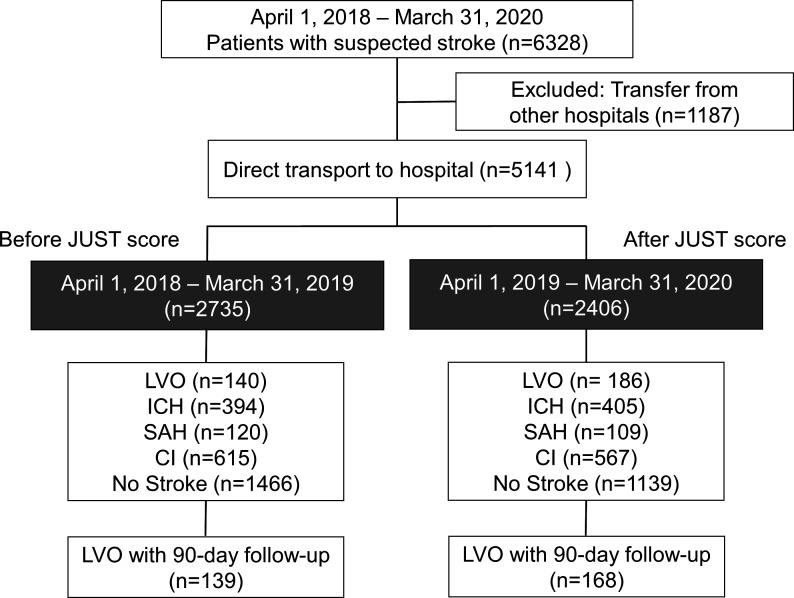
We excluded 1186 of the initially registered 6327 patients who were transferred from other hospitals. 5141 patients were finally enrolled in the study, of whom 2735 and 2406 patients were transported before and after the implementation of the JUST score, respectively (figure 1). The two cohorts were numerically similar before and after JUST score implementation (table 1). After the JUST score was implemented, EMS used the JUST score in 1484 patients (61.7%). The distribution of stroke type was numerically similar before and after JUST score implementation, while the large sample size resulted in statistical significance (p<0.0001). A total of 140 patients (5.1%) experienced LVO before JUST score implementation, which increased to 186 patients (7.7%) after implementation (table 1).
Figure 1.
Study flowchart. CI, cerebral infarction other than LVO; ICH, intracranial hemorrhage; JUST, Japan Urgent Stroke Triage; LVO, large vessel occlusion; SAH, subarachnoid hemorrhage.
Table 1.
Patient characteristics before and after JUST score implementation
| Variables | Before JUST score (n=2735) |
After JUST score (n=2406) |
P value |
| Age, years, mean (SD) | 70.0 (17.7) | 71.5 (16.7) | 0.002 |
| Men, n (%) | 1426 (52.1) | 1290 (53.6) | 0.29 |
| Systolic blood pressure, mm Hg, mean (SD) | 157.0 (35.0) | 159.6 (34.3) | 0.007 |
| Diastolic blood pressure, mm Hg, mean (SD) | 85.6 (22.5) | 88.2 (21.9) | <0.0001 |
| JUST score use, n (%) | – | 1484 (61.7) | – |
| Final diagnosis | |||
| LVO, n (%) | 140 (5.1) | 186 (7.7) | <0.0001 |
| ICH, n (%) | 394 (14.4) | 405 (16.8) | |
| SAH, n (%) | 120 (4.4) | 109 (4.5) | |
| CI, n (%) | 615 (22.5) | 567 (23.6) | |
| No stroke, n (%) | 1466 (53.6) | 1139 (47.3) | |
| Success of the first request to hospital, n (%) | 2088 (76.3) | 1917 (79.7) | 0.004 |
| On-scene time-min, median (IQR) | 18 (14–23) | 17 (14–23) | 0.69 |
| Transport time-min, median (IQR) | 10 (6–15) | 10 (6–15) | 0.87 |
CI, cerebral infarction other than LVO; ICH, intracranial hemorrhage; IQR, interquartile range; JUST, Japan Urgent Stroke Triage; LVO, large vessel occlusion; SAH, subarachnoid hemorrhage.;
After implementation of the JUST score, the frequency of LVO was high among those who were triaged with the JUST score (10.5%) but for those who were not triaged was 3.3%. The frequency of no stroke was 33.2% among those who were triaged with the JUST score but 70.1% among those who were not triaged (p<0.0001) (online supplemental table 2).
Effect of the prehospital stroke triage scale
The success rate of the first request to the hospital improved significantly from 76.3% to 79.7% (p=0.004) after the implementation of the JUST score (table 1). On the other hand, the on-scene time and transport time did not change after implementation of the score.
The success rate at the first request to the hospital and on-scene time were similar between those who were triaged with and without the JUST score after its implementation, but the transport time was shorter by 1 min for the latter (online supplemental table 2).
The success rate at the first request to the hospital was the highest for ‘red’ triage patients at 84.3%, followed by ‘yellow’ triage patients at 78.9%, and ‘green’ triage patients at 77.2% (p=0.34) among the 1484 patients who were triaged with the JUST score. The on-scene time and transport time were numerically similar among the three triage groups.
Management of large vessel occlusion
After the implementation of the JUST score, the patients with LVO were predominantly women, significantly older, and had higher blood pressure values (table 2) than those without LVO. Although the findings lacked statistical significance, the mRS scores before onset and the severity of LVO were numerically worse after the implementation of the JUST score. The internal carotid artery or M1 segment of the middle cerebral artery was the most dominant site of occlusion after JUST score implementation, but this observation lacked statistical significance.
Table 2.
Characteristics of patients with large vessel occlusion
| Before JUST score (n=140) |
After JUST score (n=186) |
P value | |
| Age, years, mean (SD) | 76.5 (12.8) | 79.8 (11.7) | 0.02 |
| Men, n (%) | 82 (58.6) | 86 (46.2) | 0.03 |
| Systolic blood pressure, mm Hg, mean (SD) | 147.6 (28.7) | 153.9 (27.8) | 0.048 |
| Diastolic blood pressure, mm Hg, mean (SD) | 78.7 (19.3) | 85.3 (21.3) | 0.004 |
| JUST score use, n (%) | – | 156 (83.9) | – |
| mRS score before onset, median (IQR) | 0 (0–1) | 0 (0–2) | 0.16 |
| NIHSS score, median (IQR) | 18 (12–24) | 20 (14–27) | 0.049 |
| ASPECTS (CT or MRI), median (IQR) | 8 (6–9) | 7 (5–9) | 0.46 |
| Occlusion site | |||
| Anterior circulation, n (%) | 128 (91.4) | 174 (93.5) | 0.47 |
| Internal carotid artery or M1 segment of the middle cerebral artery, n (%) | 91 (65.0) | 130 (69.9) | 0.35 |
| Success of the first request to hospital, n (%) | 110 (78.6) | 152 (81.7) | 0.48 |
| On-scene time, min, median (IQR) | 17 (14–22) | 17 (14–22) | 0.66 |
| Transport time, min, median (IQR) | 10 (6–14) | 11 (7–16) | 0.11 |
| Onset-to-door time, min, median (IQR) | 79 (46–200) | 101 (47–378) | 0.13 |
| Second transfer to another hospital, n (%) | 7 (5.0) | 3 (1.6) | 0.08 |
ASPECTS, Alberta Stroke Program Early CT Score; CT, computed tomography; IQR, interquartile range; JUST, Japan Urgent Stroke Triage; MRI, magnetic resonance imaging; mRS, modified Rankin Scale; NIHSS, National Institutes of Health Stroke Scale.;
The success rate of the first request to hospital numerically improved from 78.6% to 81.7%; however, this finding was not statistically significant (p=0.48). No differences were seen between the on-scene time and transport time between before and after the implementation of the JUST score. The O2D increased from a median of 79 min to 101 min after the implementation of the JUST score (p=0.13).
Administration of rtPA and use of thrombectomy were significantly higher before JUST score implementation (table 3), respectively, compared with after implementation. Among those who received thrombectomy, the D2P was significantly shortened after the implementation of the JUST score but the P2R remained the same (table 3). The success rate of thrombectomy defined by a TICI scale of 2b/3 was similar before and after JUST score implementation. The number of patients with mRS scores of 0–2 at 90 days did not increase after JUST score implementation at 90 days (table 3). The crude and adjusted ORs (95% CI) were 0.70 (0.45 to 1.10) and 0.92 (0.49 to 1.75) for mRS sores of 0–2, respectively. The 90-day mortality (mRS score 6) was also similar before and after JUST score implementation. The crude and adjusted ORs (95% CI) for mortality were 1.77 (0.88 to 3.57) and 1.64 (0.55 to 4.92), respectively.
Table 3.
Outcome of the patients with large vessel occlusion
| Before JUST score (n=140) |
After JUST score (n=186) |
P value | |
| rtPA, n (%) | 54 (38.6) | 52 (28.0) | 0.04 |
| Thrombectomy, n (%) | 83 (59.3) | 84 (45.2) | 0.01 |
| D2P, min, median (IQR) | 84 (63–114) | 73 (57–98) | 0.03 |
| P2R, min, median (IQR) | 44 (29–64) | 45 (30–70) | 0.53 |
| TICI score 2b/3, n (%) | 73/83 (88.0) | 72/81 (88.9) | 0.85 |
| mRS score 0–2 at 90 days, n (%) | 62 (44.3) | 63/176 (35.8) | 0.13 |
| Death up to 90 days, n (%) | 13 (9.3) | 27/176 (15.3) | 0.11 |
D2P, door-to-puncture time; JUST, Japan Urgent Stroke Triage; mRS, modified Rankin Scale; P2R, puncture-to-reperfusion time; rtPA, recombinant tissue plasminogen activator; TICI, thrombolysis in cerebral infarction.
The O2D was numerically shorter in patients with LVO who were triaged with the JUST score compared with those who were not triaged with (median 96 min vs 426 min) after implementation of the JUST score (online supplemental table 2), although this difference did not attain statistical significance. mRS scores of 0–2 at 90 days were also significantly more prevalent in patients with LVO who were triaged with the JUST score (online supplemental table 2).
Discussion
This study was the first to evaluate the region-wide use of prehospital stroke triage scales in patients with suspected stroke and assess the change in the emergency transportation system, as well as the clinical outcomes in real-world settings. We demonstrated that the request times to hospitals decreased when the JUST score was recommended for EMS to determine the target hospital for transportation. Based on information on the JUST score, physicians at these hospitals could reduce the D2P for patients receiving thrombectomy for LVO. We assumed that the 90-day mRS score would be improved in patients with LVO after implementation of the JUST score because D2P was reported to be an important prognostic factor for patients with LVO;3 however, it was not the case in this study. The importance of prehospital recognition of possible stroke is well documented, but its implementation is challenging in clinical practice. Prehospital recognition of possible strokes by EMS was reported to shorten the door-to-physician and door-to-CT time, as well as increase the likelihood of receiving thrombolysis.11 In addition to the shortened transport time, the American Stroke Association recommends that EMS should transport patients to hospitals that are capable of offering the highest level of stroke care when several options with similar transport time are available.1 Achieving improvements in patient outcomes with prehospital care was a difficult goal despite the improvement in the process indicators. The prehospital management guidelines were associated with survival until hospital admission but not with survival at hospital discharge in patients with traumatic brain injury.12 Although 10 of 13 participating hospitals were capable of thrombectomy, it was not always available owing to the availability of staff or operating rooms. Although a second transportation occurred in a minority of cases and its frequency did not change after implementation of the JUST score, the decrease in the number of requests to hospital and shorter D2P among patients who received the thrombectomy attested to the improved mismatch between EMS and candidate hospitals or the physician in charge.
Only the D2P was significantly shortened after JUST score implementation, whereas other time-related indicators were not shortened among patients with LVO in real-world settings. This implies that although the transport time from the scene to the hospital did not change, the preparedness for conducting thrombectomy improved using the JUST score before transportation, which resulted in a shortened D2P. A simulation study for patients with LVO reported similar findings—that is, the use of a prehospital triage scale substantially decreased the mean time from symptom onset to groin puncture, but did not decrease the mean time from symptom onset to thrombolysis.13
However, we found that the shortened D2P was not associated with improvements in the prognosis measured using the 90-day mRS score. The failure to demonstrate improvements in the prognoses of patients with LVO may be attributed to the difference in the patients’ background. The patients were significantly older and with greater disease severity as measured by the NIHSS score, although we enrolled consecutive patients who were suspected of having stroke events before and after the implementation. Indeed, the performance rates of rtPA and thrombectomy decreased after the implementation, and this observation should reflect that the number of patients with LVO who did not meet the indication criteria for rtPA or thrombectomy increased. We suspected that the unaltered neurological outcome at 90 days reflected these differences in background by chance, but other unmeasured confounding factors may be associated with the 90-day mRS scores in conjunction with potential selection bias. Another explanation is that the improvement of 11 min after implementation of the JUST score was insufficiently large to improve the mRS score. A previous meta-analysis reported that a 1-hour delay was associated with lower functional independence with an OR of 0.81.3
The JUST score can distinguish simultaneously between LVO, ICH, SAH, and other types of stroke. Thus, its usefulness in predicting several types of stroke extends beyond merely assisting with the transportation of patients with suspected stroke.6 However, 38% of patients with suspected stroke were not triaged with the JUST score after its implementation in the EMS. The proportion of patients who were determined not to have a stroke at the final diagnosis was significantly higher among those who were not triaged with the JUST score after its implementation. We supposed that these patients were intuitively judged to have a low probability of stroke by the EMS. However, 3.3% of patients were determined to have LVO at the final diagnosis. These patients were less likely to undergo thrombectomy and had a lower probability of regaining physical independence (defined as an mRS score of 0–2) despite the similarities in the success rate at the first request to the hospital, on-scene time, and transport time. Therefore, it is important for EMS to use the JUST score as much as possible and transport the patient to the appropriate hospital based on the established transportation rules for patients with suspected stroke. Hiroshima City started to use the JUST-7 score after completion of this study, which is a simplified prehospital stroke triage scale with only seven items.7
This study had several limitations. The most important risk of bias was the selection of patients enrolled, who were triaged by EMS. The only inclusion criterion for this study was a suspected stroke judged by the EMS and subsequent transport to the participating hospital. Because we developed the JUST score for use in a wide range of patients, we did not limit the symptoms or signs of the candidate patients in the study during its development and daily clinical use. Second, we introduced a real-time information system which provided the availability of thrombectomy and the predicted D2P of the candidate hospitals when the JUST score was implemented. Although the information of predicted type of stokes and likelihood of LVO was necessarily based on the JUST score, the introduction of the information system partially contributed to the shorter D2P in patients with LVO. Third, we did not follow-up the patients, apart from those with LVO. Because the motivation for the development of JUST scores was the optimization of prehospital care for all types of stroke, future studies should investigate the prognosis of such patients with other types of stroke (ie, besides LVO) or even those without stroke. These investigations could attest to the effectiveness of the region-wide implementation of the JUST score and its generalizability outside Japan. Finally, the success rate of the first request to the hospital increased moderately (from 76.3% to 79.7%), although we developed the application of a real-time information sharing system. This moderate improvement was limited by the congestion of emergency rooms or occupation of operation rooms for thrombectomy and these situations were not reflected on the application in real time. However, the 3.4% improvement would be still relevant because one of 29 (1/0.034) patients with suspected stroke would be transported without unnecessary delay. Therefore, the implementation of prehospital stroke triage scale should be conducted in conjunction with improvement of in-hospital emergency care.
Conclusions
The region-wide use of the prehospital stroke triage scale by EMS improved the success rate at the first request to the hospital for patients with suspected stroke. The prehospital stroke triage scale was also associated with a shortened D2P for patients who underwent thrombectomy for acute LVO, although 11 min reduction was insufficient to improve their disability at 90 days. Further efforts to make substantial reduction in time from onset to door or reperfusion should be investigated with prehospital management to improve the clinical outcomes in patients with acute stroke.
neurintsurg-2021-017863supp002.pdf (103.3KB, pdf)
Acknowledgments
We are indebted to the EMSs who participated in this study. We thank Dr Saujanya Rajbhandari for his comments. We are grateful to Drs Toshinori Nakahara, Masaaki Shibukawa, Yoshihiro Kiura, Ryo Ogami, Satoshi Usui, Ryo Nosaka, Hidekazu Chikuie, Koji Shimonaga, Yuichiro Ota, Naoto Kinoshita, Yuji Shiga, and Seiji Umemoto for giving helpful advice and data collection. We also thank the following for their involvement in the construction and operation of the triage system: Tomiji Kubo, Masaomi Kishida, Yuichi Yamamoto, Hideo Nishioka, Toru Nakata, and Maya Miyoshi from Hiroshima City Fire Department; Kazumi Matsui, Naoko Daimaru, Masatsugu Ashida, Hiroko Imai, Michi Mimori, Ikuya Toyama, and Yuko Tsuda from Hiroshima City Hall; Drs Makoto Matsumura, Shiro Nakai, Toshiyuki Itamoto, Tsuneo Okumichi, and Katsunari Miyamoto from Hiroshima City Medical Association.
Footnotes
Correction notice: Since this article was first published online the supplementary material has been updated.
Contributors: TMo had full access to all the data in the study and takes responsibility for the integrity and accuracy of the data analysis. Study concept and design: HA, KU, SY, and TMo. Acquisition of data: HA, KU, SS, SA, NI, YoK, AT, HN, TMi, MS, NH, EN, TM, JK, YuK, YuKaw, and KazK. Analysis and interpretation of data: HA, KU, SY, KaoK, NS, SS, SA, NI, YoK, AT, HN, TMi, MS, NH, EN, TM, JK, YuKat, YuKaw, KazK, and TMo. Drafting of the manuscript: HA, KU, and TMo. Critical revision of the manuscript for important intellectual content: SY, KaoK, NS, SS, SA, NI, YoK, AT, HN, TMi, MS, NH, EN, TM, JK, YuKat, YoKaw, and KazK. Statistical analysis: KU and YMo. Administrative, technical, or material support: SY, KaoK, and SS. Study supervision: SY and TMo.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The institutional review boards of all participating hospitals approved the study protocol.
References
- 1. Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update. Stroke 2019;50:e187–210. 10.1161/STR.0000000000000173 [DOI] [PubMed] [Google Scholar]
- 2. Koster GT, Nguyen TTM, van Zwet EW, et al. Clinical prediction of thrombectomy eligibility: a systematic review and 4-item decision tree. Int J Stroke 2019;14:530–9. 10.1177/1747493018801225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 2016;316:1279–88. 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 4. Kowalski RG, Claassen J, Kreiter KT, et al. Initial misdiagnosis and outcome after subarachnoid hemorrhage. JAMA 2004;291:866–9. 10.1001/jama.291.7.866 [DOI] [PubMed] [Google Scholar]
- 5. Oostema JA, Chassee T, Baer W, et al. Accuracy and implications of hemorrhagic stroke recognition by emergency medical services. Prehosp Emerg Care 2020:1–6. 10.1080/10903127.2020.1831669 [DOI] [PubMed] [Google Scholar]
- 6. Uchida K, Yoshimura S, Hiyama N, et al. Clinical prediction rules to classify types of stroke at prehospital stage. Stroke 2018;49:1820–7. 10.1161/STROKEAHA.118.021794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Uchida K, Yoshimura S, Sakakibara F, et al. Simplified prehospital prediction rule to estimate the likelihood of 4 types of stroke: the 7-Item Japan Urgent Stroke Triage (JUST-7) score. Prehosp Emerg Care 2021;25:465–74. 10.1080/10903127.2020.1800877 [DOI] [PubMed] [Google Scholar]
- 8. van Swieten JC, Koudstaal PJ, Visser MC, et al. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988;19:604–7. 10.1161/01.STR.19.5.604 [DOI] [PubMed] [Google Scholar]
- 9. Lyden P, Brott T, Tilley B, et al. Improved reliability of the NIH Stroke Scale using video training. NINDS TPA Stroke Study Group. Stroke 1994;25:2220–6. 10.1161/01.STR.25.11.2220 [DOI] [PubMed] [Google Scholar]
- 10. Tomsick T. Timi, TIBI, TICI: I came, I saw, I got confused. AJNR Am J Neuroradiol 2007;28:382–4. [PMC free article] [PubMed] [Google Scholar]
- 11. Abboud ME, Band R, Jia J, et al. Recognition of stroke by EMS is associated with improvement in emergency department quality measures. Prehosp Emerg Care 2016;20:729–36. 10.1080/10903127.2016.1182602 [DOI] [PubMed] [Google Scholar]
- 12. Spaite DW, Bobrow BJ, Keim SM, et al. Association of statewide implementation of the prehospital traumatic brain injury treatment guidelines with patient survival following traumatic brain injury: the Excellence in Prehospital Injury Care (EPIC) study. JAMA Surg 2019;154:e191152. 10.1001/jamasurg.2019.1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schlemm L, Ebinger M, Nolte CH, et al. Impact of prehospital triage scales to detect large vessel occlusion on resource utilization and time to treatment. Stroke 2018;49:439–46. 10.1161/STROKEAHA.117.019431 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
neurintsurg-2021-017863supp001.pdf (1.1MB, pdf)
neurintsurg-2021-017863supp002.pdf (103.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data that support the findings of this study are available from the corresponding author upon reasonable request.