Abstract
Background
Household air pollution (HAP) from solid fuel use (SFU) for cooking may impact child health in low-resources countries. This study examined the associations between HAP and early childhood development (ECD) outcomes among children under 5 years of age in Bangladesh and explored potential effect modification by sex and urbanicity.
Methods
The study sample consisted of 9395 children aged 36–59 months in the households from the Bangladesh Multiple Indicator Cluster Survey 2019. SFU and levels of exposure to SFU (unexposed, moderately exposed and highly exposed) were used as proxies of HAP exposure. We estimated the covariate-adjusted prevalence ratios (aPRs) and 95% CIs for the associations between HAP and ECD outcomes using multilevel mixed-effects Poisson regression models with a robust variance estimator.
Results
81.4% of children were exposed to SFU, and the prevalence of developmental delay (in Early Childhood Development Index) was 25.3%. Children exposed to SFU were 1.47 times more likely to have developmental delays (95% CI: 1.25, 1.73; p<0.001) compared with children with no SFU exposure. SFU was significantly associated with developmental delay in socioemotional (aPR: 1.17; 95% CI: 1.01, 1.36; p=0.035) and learning-cognitive (aPR: 1.90; 95% CI: 1.39, 2.60; p<0.001) domains. Similarly, children moderately exposed and highly exposed to HAP had higher prevalence of developmental delays than unexposed children. We did not observe effect modification by sex or urbanicity.
Conclusion
Public health policies should promote the use of clean cooking fuels and cookstoves to reduce the high burden of HAP exposure in low-resource countries for helping younger children to meet their developmental milestones.
Keywords: CHILD HEALTH, ENVIRONMENTAL HEALTH, AIR POLLUTION, COGNITION
WHAT IS ALREADY KNOWN ON THIS TOPIC
About 250 million children under 5 years of age in low-income and middle-income countries are at a risk of not reaching their full developmental potential.
Early exposure to household air pollution from solid fuel use may have potential adverse effects on early childhood development.
WHAT THIS STUDY ADDS
This is the first nationally representative study in Bangladesh to suggest that children aged 36–59 months exposed to solid fuel use (SFU) were 47% more likely to have developmental delays in the Early Childhood Development Index compared with those with no SFU exposure.
Delays in socioemotional and learning-cognition subdomainsdrove these associations. In addition, dose–responseassociations between household air pollution and earlychildhood development were observed.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE AND/OR POLICY
Reducing household air pollution exposure can stimulate the healthy brain development of young children and help low-income and middle-income countries achieve sustainable development goals related to early childhood development and clean fuels by 2030.
Background
Household air pollution (HAP) from solid fuel use (SFU) for cooking, a major risk factor for health in low-income and middle-income countries (LMICs), contributed to 1.6–3.2 million cases of premature mortality in 2019, which are disproportionately higher in LMICs.1 2 SFU is highly prevalent in African and Southeast Asian countries.3 In Bangladesh, 87% of households rely on biomass fuels and are at risk of SFU-induced harmful health effects.4
It is well established that HAP from SFU is a major threat to child and adult health.5 6 HAP is associated with higher risks of respiratory diseases,7 8 child mortality, low birth weight,9 10 various cancers and other outcomes such as carboxyhaemoglobin—a reduction of oxygen to the fetus.6 11 Recent animal and human studies also suggest that air pollution can affect brain development.12 For instance, exposure to particulate matter (PM10 and PM2.5), nitrogen oxides (NO×), sulfur oxides (SO×), carbon monoxide (CO) and polycyclic aromatic hydrocarbons from SFU during early stages of life (including perinatal exposures) is associated with damage to the central nervous system (local systematic inflammation, oxidative stress and neurotoxicity),13–15 schizophrenia,16 increased risk of attention-deficit hyperactivity disorder,17 aggressive behaviour,18 changes in white matter19 and damage in brain structure.20 Thus, early exposure to HAP is critically important because the first years of life constitute a critical window for brain development.20 Moreover, exposure to HAP disproportionally affects women and children, who are more likely to be involved in cooking.7 21
However, most studies of air pollution and brain development have been limited to high-income countries.13 20 22 Recent evidence estimates that about 250 million children under 5 years of age in LMICs are at a risk of not reaching their full development potential due to poverty, stunting, nutrient deficiency, violence, heavy metal exposure, social, biological and physiological factors.23–26 Furthermore, early childhood development (ECD) delays are associated with lags in adult productivity and health challenges later in life.3 25 26 Thus, examining the potential effects of HAP on child development in LMICs is essential to address child development delays, which will ultimately help for achieving sustainable development goals (SDGs) related to ECD and clean cooking fuels by 2030.5
The effects of HAP on ECD outcomes are understudied in LMICs. Two studies in Ghana21 27 found a negative association between SFU and ECD outcomes. While the studies carried out in Ghana move our understanding of SFU with ECD forward, these studies did not account for seasonality, cooking place and ventilation, which can influence the levels of exposure to HAP and their ECD outcomes.7 28 Additionally, other studies have assessed how environmental exposures such as arsenic and manganese affect children’s intellectual functions in Bangladesh.29 However, to the best of our knowledge, no study has examined the associations between SFU-induced HAP and ECD outcomes in Bangladesh. This study, therefore, aims to assess the associations between HAP and ECD outcomes—Early Childhood Development Index (ECDI) and its subdomains: literacy–numeracy, physical development, socioemotional and learning-cognition development among children under 5 years of age in Bangladesh. Since HAP could have heterogeneous effects on child’s sex and where they live, we further explore the potential effect modification by sex and urbanicity.
Methods
Study participants and data sources
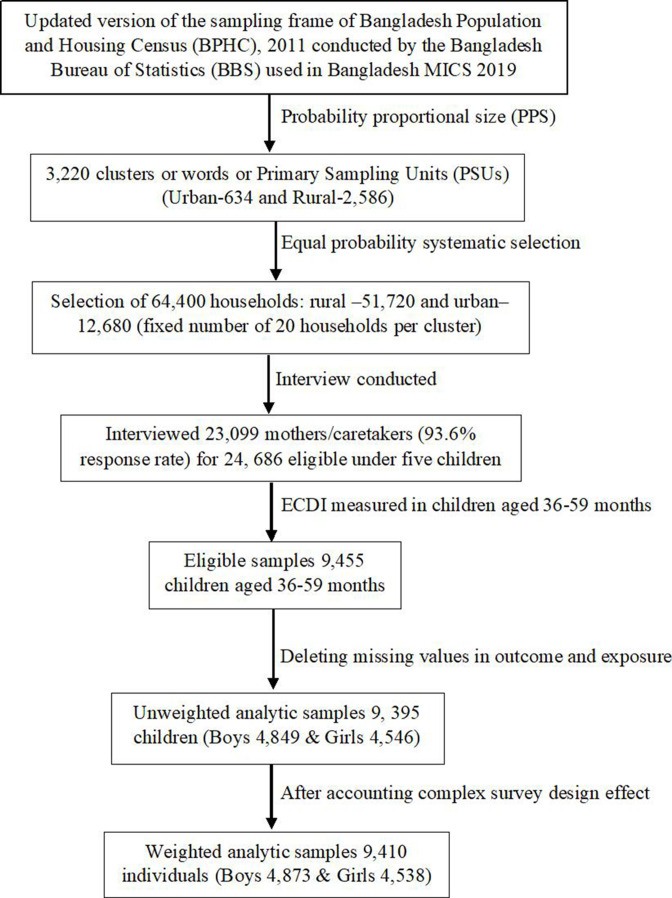
We conducted this cross-sectional study using the most recent round of Bangladesh Multiple Indicator Cluster Survey (MICS) data, collected from 19 January 2019 to 1 June 2019. The MICS is a nationally representative household survey conducted in LMICs that generates reliable and comparable indicators of women’s and children’s health and well-being.30 Data were collected through five face-to-face questionnaires on these, including basic demographic indicators of women (aged 15–49 years), children (aged 5–17 years) and younger children (aged <5 years). The Bangladesh MICS 2019 measured ECD outcomes for 9455 children aged 36–59 months from 8 administrative divisions: Dhaka (at the centre), Chattagram (located near to the Bay of the Bengal), Khulna (at the southwest), Mymensingh (in the north of Dhaka), Rangpur (located in the northern part), Rajshahi (situated in the northwest), Barisal (located in the south-central region) and Sylhet (located in the northeastern) and all 64 districts located in urban and rural areas of Bangladesh. Nine thousand three hundred and ninety five children aged 36–59 months were analytic samples for this study (figure 1).31 Detailed information on the survey is available at http://mics.unicef.org/.30
Figure 1.
Schematic diagram of the analytic study sample. ECDI, Early Childhood Development Index.
Measures of early child development outcomes
The ECD outcomes were measured by ECDI and its four subdomains: literacy–numeracy, physical, socioemotional and learning-cognition development. ECDI, the primary measure of ECD outcomes, is used to assess whether a child is developmentally on track regarding specific milestones.12 31 ECD outcomes were first measured in the fourth round of the MICS Questionnaire for children under 5 years of age and provided the first population-based indicators of ECD comparable at the international level because the selected items were validated in different cultural and socioeconomic contexts. The questionnaire was further customised and translated in a standardised way to ensure validity and high comparability of the data to implement in Bangladesh.31–33 The ECDI consists of 10 different items across 4 developmental domains: literacy–numeracy (3 items), physical (2 items), social-emotional (3 items) and learning-cognitive development (2 items) across the early years of life (36–59 months).31 A child is considered developmentally on track in ECDI if the child is on track in at least three of the four domains:
Literacy–numeracy: a child is considered developmentally on track if they can identify at least 10 letters of the alphabet, read at least 4 simple words and know the name or recognise the symbols of all numbers from 1 to 10.31
Physical: a child is considered developmentally on track if they can pick up a small object with two fingers and if the mother or primary caregiver does not indicate that the child is sometimes too sick to play.31
Socioemotional: a child is considered developmentally on track if they can perform two of the following- if the child gets along with other children; if the child does not kick, bite or hit other children; and if the child does not get distracted easily.31
Learning-cognition: a child is considered developmentally on track if they can follow simple directions to do something and do it independently when asked.31
Measures of HAP exposure
SFU (clean vs solid fuels) and levels of exposure to SFU (unexposed, moderately exposed and highly exposed) were proxy measures of HAP. A child is considered ‘exposed’ to HAP if the household reports the use of coal, charcoal, wood, straw/shrubs, animal dung or agricultural crop residue as a primary source of energy for cooking in the traditional solid fuel cookstove and is considered ‘unexposed’ if the household reports the use of electricity, liquefied petroleum gas, natural gas and/or biogas as a primary source of energy for cooking in the clean cookstove. We developed an augmented Hwhich are more rural divisions andAP exposure index: levels of exposure to HAP accounting for SFU, cooking place and ventilation for solid fuel cookstoves to improve the HAP exposure measurement.7 10 28 Children were categorised as unexposed if household reported clean fuel use (coded 0), moderately exposed if the households reported SFU, separate or outdoor cooking place and chimney or fan for solid fuel cookstove (coded 1) and highly exposed if the households reported SFU, location of cooking inside the house and no chimney or fan for solid fuel cookstove (coded 2).7 10 28
Covariates and potential confounders
Based on the prior literature,7 17 20 21 25 34 35 variables that are known to be associated with ECD or exposure to HAP were included as potential confounders. Models were adjusted for the following covariates: child sex, child age, maternal age, maternal education, household wealth quintiles, iodine status, stunting, attendance to early childhood education (ECE) programme, cooking place, season and urbanicity. Household wealth quintiles (index of available durable and non-durable household assets) generated by MICS included types of cooking fuels; however, to avoid over adjustment in inferential models, household wealth quintiles were reconstructed, excluding the type of cooking fuel used in the household (code is available on request). The Household Wealth Index was then categorised into five quintiles, with the lowest quintile reflecting the poorest households and the highest quintile the wealthiest households.10 31
Statistical analysis
Descriptive statistics were used to provide general characteristics of study samples. The distribution and prevalence of ECDI and its subdomains were calculated by each covariate. We used multilevel mixed-effects Poisson regression models with robust error variance accounting for survey weights to examine the associations between HAP and ECD measures10 21 because ORs from logistic regression can significantly overestimate the relative risk of common outcomes measured in cross-section studies.7 10 36 In addition, we used random subject effects accounting for cluster and stratum.
Results from the multilevel mixed-effects Poisson regression models are presented as prevalence ratios (PRs) with 95% CIs. Additional analyses explored the associations between HAP and ECD by sex (boys/girls) and urbanicity (rural/urban). Differences between estimates for boys and girls and urban and rural areas were tested using a p difference extracted from the Wald test for the interaction term. In addition, we tested for linear trend (p trend) for the dose–response associations between the augmented HAP exposure (treating as a continuous variable) and ECD outcomes. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines to design and report results.37 All analyses were conducted using R V.4.1.2 and Stata V.16.
Patient and public involvement
Patients were not involved in this study.
Results
Prevalence of ECD and associated characteristics
The prevalence of ECD outcomes, characteristics of the study children aged 36–59 months, their parental and household information are presented in table 1.
Table 1.
Sample characteristics of children aged 36–59 months in Bangladesh (weighted percentage or mean and n=unweighted)
| Characteristics | Number of children (n=unweighted) | % (weighted) |
| Sex of the child | ||
| Boy | 4849 | 51.8 |
| Girl | 4546 | 48.2 |
| Child age in months (mean±SD) | 9395 | 47.2 (6.9) |
| 36–47 months | 4777 | 51.1 |
| 48–59 months | 4618 | 48.9 |
| Size of the child (information is unavailable for all sample) | ||
| Larger than average | 137 | 1.4 |
| Average | 1086 | 11.3 |
| Smaller than average | 255 | 2.8 |
| Missing | 7917 | 84.5 |
| Child nutritional status | ||
| Height for age (WHO) (mean±SD) | 9394 | 3.0 (20.5) |
| Stunted | 2534 | 26.8 |
| Iodine | 6957 | 74.7 |
| Caregiver’s stimulation | ||
| Poor | 1908 | 18.7 |
| High | 6488 | 71.0 |
| Ever attended ECE | 1771 | 19.3 |
| Maternal age in years (mean±SD) | 9205 | 28.6 (6.0) |
| Maternal age (categories) | ||
| 15–19 years | 224 | 2.5 |
| 20–24 years | 2496 | 26.8 |
| 25–29 years | 2754 | 30.0 |
| 30–34 years | 2132 | 23.3 |
| 35–39 years | 1130 | 12.2 |
| 40–49 years | 469 | 5.2 |
| Maternal education | ||
| None/pre-primary | 1246 | 13.2 |
| Primary | 2325 | 24.3 |
| Secondary | 4553 | 48.1 |
| High secondary+ | 1291 | 14.4 |
| Paternal education | ||
| None/pre-primary | 1847 | 22.9 |
| Primary | 2593 | 30.9 |
| Secondary | 2420 | 30.2 |
| High secondary+ | 1238 | 16.1 |
| Household wealth quintiles | ||
| Poorest | 1879 | 22.3 |
| Poorer | 1879 | 20.0 |
| Middle | 1879 | 18.7 |
| Richer | 1879 | 19.3 |
| Richest | 1879 | 19.8 |
| Region | ||
| Barisal | 823 | 5.6 |
| Chattrogram | 1967 | 21.9 |
| Dhaka | 1802 | 23.1 |
| Khulna | 1309 | 10.4 |
| Mymensingh | 563 | 7.5 |
| Rajshahi | 1030 | 12.6 |
| Rangpur | 1108 | 10.8 |
| Sylhet | 793 | 8.0 |
| Urbanicity | ||
| Rural | 7649 | 79.1 |
| Urban | 1746 | 20.9 |
| Season | ||
| Winter (January–March) | 5085 | 56.2 |
| Summer (April–June) | 4310 | 43.8 |
| Types of cooking fuels | ||
| Clean fuels | 1326 | 18.6 |
| Solid fuels | 8069 | 81.8 |
| Technologies/cookstoves for cooking | ||
| Clean fuel stove | 1326 | 18.6 |
| Solid fuel stove | 8069 | 81.4 |
| Chimney/fan in solid fuel stove | 355 | 4.1 |
| Cooking place | ||
| Indoor | 3257 | 34.4 |
| Separate room | 3582 | 37.4 |
| Outdoor | 2556 | 28.1 |
| Levels of exposure to HAP | ||
| Unexposed | 1326 | 18.6 |
| Moderately exposed | 6017 | 62.6 |
| Highly exposed | 2052 | 18.8 |
| ECD indicators | ||
| Literacy–numeracy (not on track) | 6708 | 71.1 |
| Physical (not on track) | 138 | 1.4 |
| Socioemotional (not on track) | 2589 | 27.2 |
| Learning-cognition (not on track) | 903 | 8.6 |
| ECDI (not on track) | 2516 | 25.3 |
ECD, early childhood development; ECDI, Early Childhood Development Index; ECE, early childhood education; HAP, household air pollution.
The prevalence of children with developmental delay was 25.3% in global ECDI. For the four subdomains, 71.1% of children were delayed developmentally in literacy–numeracy, 27.2% in socioemotional development, 8.6% in learning-cognition and 1.4% in physical development (table 1). On the other hand, the prevalence of SFU as a primary source of energy for cooking and traditional solid fuel cookstoves was 81.4%, only 4.1% of them were equipped with a chimney or a fan and 34.4% of households cooked in the main house. Thus, 62.6% of children were moderately exposed to HAP and 18.8% were highly exposed to HAP (table 1).
The bivariate associations between ECD and sample characteristics are presented in table 2. Younger children (aged 36 months), boys, stunted, those not received sufficient iodine intake, those never attended in ECE programme, received poor caregivers’ stimulation, with parents below primary education, living in rural areas, and poorest/poorer households, exposed to SFU and moderately as well as highly exposed to HAP were more likely to be delayed developmentally in global ECDI (table 2). The highest percentages of children with developmental delay in global ECDI were in Mymensingh (39.1%) and Sylhet divisions (38.1%) (table 2; online supplemental figure S1).
Table 2.
Percentage of children aged 36–59 months who are delayed developmentally for indicated domains (weighted percentage and n=unweighted)
| Characteristics | Number of children (unweighted) | ECDI % | P value | Literacy–numeracy % | P value | Physical % | P value | Socioemotional % | P value | Learning % | P value |
| Total | 9395 (100) | 25.3 | – | 71.1 | – | 1.4 | – | 27.2 | – | 8.6 | – |
| Child sex | |||||||||||
| Boy | 4849 | 28.5 | <0.001 | 72.5 | 0.007 | 1.4 | 0.888 | 30.9 | <0.001 | 9.0 | 0.168 |
| Girl | 4546 | 21.6 | 69.7 | 1.4 | 23.1 | 8.1 | |||||
| Child age in months | |||||||||||
| 36–47 months | 4777 | 31.3 | <0.001 | 83.6 | <0.001 | 1.6 | 0.062 | 29.0 | 0.0003 | 10.3 | <0.001 |
| 48–59 months | 4618 | 18.8 | 58.2 | 1.1 | 25.2 | 6.7 | |||||
| Child size | |||||||||||
| Larger than average | 137 | 22.2 | 0.326 | 64.2 | 0.091 | 0.8 | 0.183 | 29.3 | 0.453 | 5.4 | 0.154 |
| Average | 1086 | 28.5 | 71.7 | 0.8 | 31.8 | 10.7 | |||||
| Smaller than average | 255 | 25.6 | 75.8 | 2.2 | 27.5 | 8.9 | |||||
| Child nutritional status (stunting) | |||||||||||
| No | 6860 | 23.5 | <0.001 | 67.5 | <0.001 | 1.3 | 0.191 | 26.8 | 0.289 | 7.7 | <0.001 |
| Yes | 2534 | 29.7 | 81.3 | 1.7 | 28.0 | 10.8 | |||||
| Iodine | |||||||||||
| Yes | 6957 | 24.0 | <0.001 | 68.6 | <0.001 | 1.3 | 0.168 | 26.8 | 0.311 | 8.6 | 0.965 |
| No | 2436 | 28.9 | 79.0 | 1.7 | 28.1 | 8.5 | |||||
| Ever attended ECE | |||||||||||
| No | 7624 | 27.9 | <0.001 | 78.6 | <0.001 | 1.4 | 0.388 | 27.3 | 0.372 | 9.5 | <0.001 |
| Yes | 1771 | 14.1 | 40.4 | 1.1 | 26.1 | 4.6 | |||||
| Caregiver’s stimulation | |||||||||||
| None | 999 | 29.5 | 0.001 | 88.3 | <0.001 | 2.1 | <0.001 | 23.6 | 0.076 | 10 | 0.241 |
| Poor | 1908 | 27.4 | 79.5 | 2.5 | 27.4 | 8.1 | |||||
| Sufficient | 6488 | 24.0 | 66.5 | 0.9 | 27.6 | 8.4 | |||||
| Maternal age | |||||||||||
| 15–19 years | 224 | 31.1 | 0.059 | 80.7 | 0.0001 | 1.5 | 0.796 | 30.9 | 0.476 | 11.3 | 0.193 |
| 20–24 years | 2496 | 24.7 | 69.1 | 1.4 | 28.0 | 7.8 | |||||
| 25–29 years | 2754 | 24.3 | 70.4 | 1.4 | 26.2 | 8.3 | |||||
| 30–34 years | 2132 | 25.1 | 69.9 | 1.1 | 27.0 | 8.7 | |||||
| 35–39 years | 1130 | 25.7 | 73.9 | 1.4 | 26.5 | 8.7 | |||||
| 40–49 years | 469 | 30.6 | 79.2 | 0.8 | 29.8 | 11.1 | |||||
| Maternal education | |||||||||||
| None/pre- primary | 1246 | 31.5 | <0.001 | 85.2 | <0.001 | 2.2 | 0.007 | 27.8 | 0.134 | 12.5 | <0.001 |
| Primary | 2325 | 30.6 | 80.4 | 1.8 | 28.4 | 10.4 | |||||
| Secondary | 4553 | 23.2 | 68.1 | 1.0 | 27.1 | 7.2 | |||||
| Higher secondary+ | 1291 | 17.0 | 53.3 | 1.3 | 24.4 | 6.1 | |||||
| Paternal education | |||||||||||
| None/pre- primary | 1847 | 30.7 | <0.001 | 83.2 | <0.001 | 2.0 | 0.011 | 27.5 | 0.003 | 11.9 | <0.001 |
| Primary | 2593 | 29.4 | 76.3 | 1.5 | 30.1 | 8.8 | |||||
| Secondary | 2420 | 22.7 | 66.9 | 0.8 | 26.6 | 7.4 | |||||
| Higher secondary+ | 1238 | 16.0 | 54.2 | 1.0 | 23.7 | 5.2 | |||||
| Household wealth quintiles | |||||||||||
| Poorest | 1879 | 30.3 | <0.001 | 83.5 | <0.001 | 1.8 | 0.196 | 27.0 | 0.0002 | 11.3 | <0.001 |
| Poorer | 1879 | 30.1 | 78.7 | 1.6 | 28.5 | 10.5 | |||||
| Middle | 1879 | 26.9 | 72.6 | 1.6 | 30.0 | 9.1 | |||||
| Richer | 1879 | 23.8 | 67.7 | 1.2 | 27.9 | 6.9 | |||||
| Richest | 1879 | 17.2 | 57.8 | 0.9 | 22.9 | 6.0 | |||||
| Region | |||||||||||
| Barisal | 823 | 32.1 | <0.001 | 69.3 | <0.001 | 0.8 | <0.001 | 35.3 | <0.001 | 11.3 | <0.001 |
| Chattrogram | 1967 | 21.8 | 68.0 | 1.3 | 27.7 | 9.0 | |||||
| Dhaka | 1802 | 18.3 | 68.1 | 1.2 | 18.1 | 6.4 | |||||
| Khulna | 1309 | 26.9 | 72.2 | 0.6 | 32.3 | 5.9 | |||||
| Mymensingh | 563 | 39.0 | 69.7 | 4.4 | 42.1 | 8,6 | |||||
| Rajshahi | 1030 | 30.4 | 76.2 | 1.1 | 30.0 | 7.6 | |||||
| Rangpur | 1108 | 16.4 | 74.2 | 1.8 | 17.3 | 6.5 | |||||
| Sylhet | 793 | 38.1 | 78.6 | 0.7 | 33.6 | 19.2 | |||||
| Urbanicity | |||||||||||
| Urban | 1746 | 21.8 | 0.002 | 65.2 | <0.001 | 1.1 | 0.303 | 25.6 | 0.182 | 7.4 | 0.124 |
| Rural | 7649 | 26.1 | 72.7 | 1.5 | 27.5 | 8.8 | |||||
| Season | |||||||||||
| Winter | 5085 | 25.4 | 0.640 | 70.5 | 0.144 | 1.3 | 0.590 | 27.3 | 0.694 | 8.8 | 0.503 |
| Summer | 4310 | 24.9 | 72.2 | 1.5 | 26.8 | 8.3 | |||||
| Types of cooking fuels | |||||||||||
| Clean fuels | 1326 | 16.3 | <0.001 | 60.0 | <0.001 | 1.0 | 0.253 | 22.8 | 0.001 | 4.7 | <0.001 |
| Solid fuels | 8069 | 27.2 | 73.8 | 1.5 | 28.1 | 9.4 | |||||
| Cooking place | |||||||||||
| Indoor | 3257 | 23.8 | 0.020 | 67.3 | <0.001 | 1.3 | 0.797 | 25.8 | 0.207 | 8.9 | 0.440 |
| Separate room | 3582 | 24.7 | 71.3 | 1.5 | 28.2 | 8.0 | |||||
| Outdoor | 2556 | 27.5 | 75.7 | 1.4 | 27.2 | 8.8 | |||||
| Technologies/cookstoves for cooking | |||||||||||
| Clean fuel stove | 1326 | 16.3 | <0.001 | 60.0 | <0.001 | 1.0 | 0.253 | 22.8 | 0.001 | 4.7 | <0.001 |
| Solid fuel stove | 8069 | 27.2 | 73.8 | 1.5 | 28.1 | 9.4 | |||||
| Levels of exposure to HAP | |||||||||||
| Unexposed | 1326 | 16.3 | <0.001 | 60.0 | <0.001 | 1.0 | 0.476 | 22.8 | 0.001 | 4.7 | <0.001 |
| Moderately exposed | 6017 | 26.8 | 73.8 | 1.4 | 28.62 | 8.5 | |||||
| Highly exposed | 2052 | 28.7 | 73.6 | 1.6 | 26.3 | 12.5 | |||||
ECE, early childhood education; HAP, household air pollution.
jech-2021-217554supp001.pdf (166.3KB, pdf)
Multivariable associations between HAP and ECD by sex and urbanicity
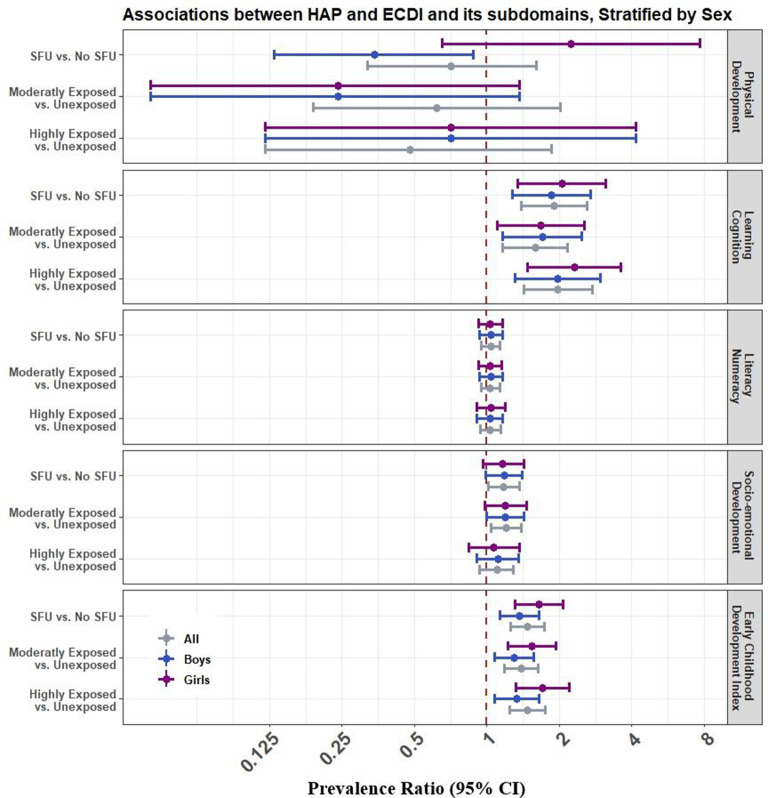
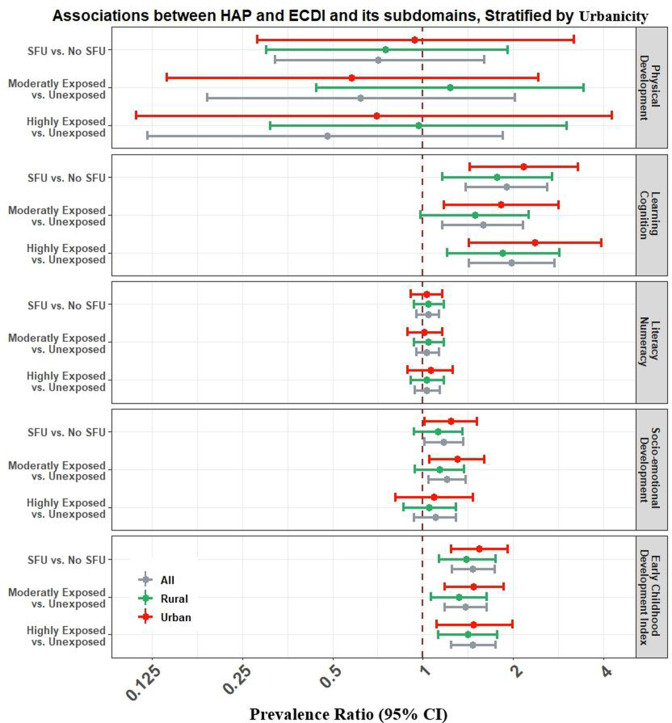
Figures 2 and 3 show the associations between HAP and ECDI and its subdomains by sex and urbanicity after adjusting for potential confounders (online supplemental tables S1-S12).
Figure 2.
Associations between HAP and ECD stratified by sex in Bangladesh. *Models were adjusted for child age, maternal age, maternal education, household wealth quintiles, iodine, stunting, attendance to ECE, urbanicity and season (details of these models are included as online supplemental tables S1, S3, S5, S7, S9 and S11). ECD, early childhood development; ECDI, Early Childhood Development Index; ECE, early childhood education; HAP, household air pollution; SFU, solid fuel use.
Figure 3.
Associations between HAP and ECD stratified by urbanicity in Bangladesh. *Models were adjusted for child age, sex, maternal age, maternal education, household wealth quintiles, iodine, stunting, attendance to ECE, cooking place and season (details of these models are included as online supplemental tables S2, S4, S6, S8, S10, S12). ECE, early childhood education. ECD, early childhood development; ECDI, Early Childhood Development Index; ECE, early childhood education; HAP, household air pollution; SFU, solid fuel use.
Children exposed to SFU were 1.47 times more likely to be developmentally delayed in global ECDI (95% CI: 1.25, 1.73; p<0.001) than unexposed children. We did not observe significant effect modification by sex and results were comparable (p difference=0.210) for boys (adjusted PR (aPR): 1.37; 95% CI: 1.13, 1.65) and girls (aPR: 1.64; 95% CI: 1.31, 2.07) for ECDI (figure 2; online supplemental tables S1-S10). The associations between SFU and developmental delay in socioemotional (aPR: 1.17; 95% CI: 1.01, 1.36; p=0.035) and learning-cognition (aPR: 1.90; 95% CI: 1.39, 2.60; p<0.001) domains were statistically significant. However, literacy–numeracy (aPR: 1.04; 95% CI: 0.95, 1.13) and physical development (aPR: 0.71, 95% CI: 0.32, 1.60) did not show any significant associations with SFU (figure 2; online supplemental tables S1-S10).
When we considered the augmented HAP exposure, the prevalence of children with developmental delay was significantly higher among children moderately exposed (aPR: 1.39; 95% CI: 1.18, 1.63; p<0.001) and highly exposed (aPR: 1.47; 95% CI: 1.24, 1.75; p<0.001) to HAP, respectively, compared with unexposed children. Compared with unexposed children, the prevalence of developmental delay in socioemotional domain was higher among children moderately exposed (aPR: 1.20; 95% CI: 1.04, 1.39; p=0.016) and highly exposed (aPR: 1.10; 95% CI: 0.94, 1.29; p=0.259) to HAP, compared with unexposed children. Likewise, the prevalence of developmental delay in the learning-cognition domain was among children moderately exposed (aPR: 1.59; 95% CI: 1.16, 2.16; p=0.016) and highly exposed (aPR: 1.97; 95% CI: 1.42, 2.74; p<0.001) to HAP, compared with unexposed children. However, there were no significant associations of HAP with physical and literacy–numeracy domains (figure 2; online supplemental tables S11-S12). All these associations were not modified by sex (p difference >0.05).
Urbanicity (urban (aPR: 1.54; 95% CI: 1.24, 1.91) and rural (aPR: 1.40; 95% CI: 1.13, 1.74)) did not significantly modify the effect of SFU on global ECDI (p difference=0.450) (figure 3; online supplemental tables S1-S10). We did not observe any modification effects by urbanicity in these associations between SFU and ECDI and its subdomains (p difference >0.05 for all) (figure 3; online supplemental tables S1-S10). Moreover, urbanicity did not modify associations between HAP and ECD outcomes (figure 3; online supplemental tables S11-S12). We observed significant dose–response associations of the augmented HAP exposure with ECDI and learning-cognition for boys (p trend <0.05), girls (p trend <0.05), rural children (p trend <0.05) and urban children (p trend <0.05) (online supplemental tables S11-S12).
Discussion
Our study suggests that Bangladeshi children aged 36–59 months exposed to HAP were more likely to have developmental delays, specifically in global ECDI and its socioemotional and learning-cognition subdomains, compared with unexposed children. Furthermore, dose–response associations were observed between the augmented HAP exposure (categorised into no exposure, moderate exposure and high exposure) and ECDI and learning-cognition. We used nationally representative data from MICS 2019 collected by UNICEF, in which SFU and levels of exposure to SFU were considered as proxy measures for HAP.7 10 21 These results align with a study conducted in Sri Lanka, which found neurotoxic impacts of HAP on child cognitive scores.34 Similar results were observed in many other LMICs in which SFU is highly prevalent.21 34 38 39
In South Asian settings, most households do not have a separate cooking place with sufficient ventilation. Therefore, it is very common for mothers to cook in the same room, where most children’s daily activities occur.7 10 28 Hence, the complex mixture of pollutants emitted from SFU increases the risk of developmental delays in younger children by potentially damaging the central nervous system and affecting brain development.13 19 25 34 35 40 Our study demonstrated that HAP was significantly associated with specific developmental subdomains in boys and girls, corroborated by previous studies.21 22 However, HAP had more pronounced effects on learning-cognition and socioemotional development but null for physical development and literacy–numeracy. One reason could be a non-differential measurement error in the measurements of the physical development and literacy–numeracy subdomains that bias the associations with HAP toward the null. Previous study showed that these two subdomains had low internal consistency, and ECDI items for literacy–numeracy might be advanced for young children, whereas the physical development item is more about the health status of the children.23
Girls exposed to HAP were more likely to be delayed developmentally in ECDI and its subdomain of learning-cognition and physical development compared with boys. However, there was no statistical evidence of sex differences in the associations between HAP and ECD outcomes. Kurata et al 39 observed a significant effect of SFU among Bangladeshi girls’ respiratory illness but null for boys. Another study21 in Ghana found that girls were more likely to have developmental delays than boys. Due to sociocultural factors and gender roles, girls may spend more time indoors, particularly in the kitchen with their mothers in the South Asian countries, and subsequently, be more exposed to HAP.7 21 39
Moreover, gender inequalities in HAP exposure and ECD are prevalent in households for children in LMICs, including in Bangladesh.7 21 39 41 On the contrary, a study showed sex-dependent effects on neuropsychological development at 4–6 years of age, with a greater vulnerability in boys, specifically in domains related to memory, verbal and general cognition.34 However, unlike these studies,34 42 our study did not observe significant effect modification by sex. One of the reasons is the differences in accounting for sex either as a biological variable or a societal construct. In our study, the interaction term would have captured the latter, whereas in the previous studies, especially investigating outdoor air pollutants, sex would represent more the biological construct. However, more studies should be introduced using available biomarkers, particularly for Bangladesh, to understand gender behaviour in the sociocultural context and gender differences in ECD and HAP exposure and greater vulnerability of girls.
This study also observes that urban children exposed to HAP were more likely to be delayed developmentally in ECDI and its subdomains of socioemotional development and learning-cognition compared with rural children, but these differences were not statistically significant. The observed rural–urban differences in ECD outcomes may be because children in rural areas have more mobility and spend more time playing outdoors with other children of joint families, relatives and neighbours. Heissler also showed that it is common for rural children to grow up with other family members, including grandparents, uncles and same-aged children in Bangladesh.43 However, urban children have less opportunity to play with other children and spend time with other family members and relatives who can provide more nurturing.43
Interestingly, the association between HAP and learning-cognition was stronger in urban kids compared with rural kids, maybe because most urban children stay home and have less opportunity for outdoor activities.43 Simultaneously, it is also important to investigate children’s outdoor playing time since this may also limit the effects of indoor pollution areas relatively free of external contamination, especially in rural areas as urban areas in Bangladesh experience high outdoor air pollution levels. Moreover, descriptive results suggest regional variations in global ECDI with higher prevalence in Mymensingh and Sylhet regions, which are more rural divisions and warrant further spatial investigation.
This study contributes to setting specific targets and tracking progress toward meeting SDGs of 4.2: ‘By 2030, ensure that all girls and boys have access to quality ECD, care, and pre-primary education so that we can save the brain of our next generation’.25 31–33 Thus, it is pressing to design interventions and implement strategies to lessen HAP exposure from SFU and improve cooking conditions to reduce the risk of developmental delays among younger children in LMICs, including Bangladesh.
Strengths and limitations
The primary strength of this study is that it is the first study with a large representative sample of children aged 35–59 months from all districts of Bangladesh. Another strength is our robust analysis, with an appropriate statistical method and adjustment for potential confounders, including child sex and age, maternal age and education, household wealth and attendance to ECE, and lifestyle variables, which makes our findings reliable and valid for policymaking.
Our study has the following limitations. First, measurement error in exposure is very likely due to the use of proxy measures of HAP. However, SFU and levels of exposure to SFU are the available robust and established measurements of HAP,10 although it would be beneficial if MICS may collect the cooking duration and proximity to the kitchen. Moreover, we could not control for outdoor air pollution as the location (GPS) to estimate air pollutants concentrations from satellite data are unavailable in MICS. Nevertheless, particles from SFU are important contributors to outdoor air pollution in countries with ubiquitous SFU. This limitation could be addressed in future studies controlling for modelled outdoor air pollution in countries with location data.
Second, the cross-sectional and observational nature of the study may not allow us to identify how SFU directly affects ECDI and establish any specific causal link at this time. Further longitudinal studies are needed to confirm the causal effects of SFU on ECD. Third, some questions of the ECDI were retrospective, which might introduce recall biases. However, mothers rarely report incorrect information about the developmental activities of their young children because mothers/primary caregivers in Bangladesh are excited about each developmental milestone and keep detailed records. Unfortunately, we did not have comparable data from neighbouring countries that investigated SFU and its impact on ECD. Future studies should contrast these results with neighbouring countries to better assess their validity and generalisability.
Conclusion
The study showed that children exposed to HAP have significant developmental delays compared with unexposed children, regardless of their sex or urbanicity. Specifically, moderate and higher levels of HAP exposure were associated with an increased prevalence of developmental delays in ECDI and its two subdomains in Bangladesh. This is a double burden for most disadvantaged kids struggling to reach their full developmental potentials in low-resources countries like Bangladesh.23 24 Therefore, interventions to promote the use of clean cooking fuels and cookstoves could reduce HAP exposure, nurture healthy and productive early brain development of next generations, and achieve SDGs related to ECD and clean cooking fuels by 2030.
Acknowledgments
The authors are grateful to BBS and UNICEF for granting access to the Bangladesh Multiple Indicator Cluster Survey 2019 data. We thank Jasleen Arneja, as well as the editor and two anonymous referees of this journal for valuable comments.
Footnotes
Twitter: @juwelranasoc, @aynumazi
Contributors: JR and YO conceptualised and designed the study. JR, JIN-M and DKM carried out the analyses. JR, SEH and PLG drafted the initial manuscript. YO supervised the study and revised the manuscript. All authors met the conditions for authorship: substantial contributions to the conception or design of the work, or the acquisition, analysis or interpretation of data; drafting the work or revising it critically for important intellectual content; final approval of the version published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JR is the study guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. All data files are publicly available and can be downloaded upon request from the MICS program database: https://mics.unicef.org/surveys. Codes are also available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The technical committee of the Government of Bangladesh, led by BBS, approved the MICS 2019 survey protocol. Informed consent was obtained from each participant, and adult consent was obtained for the child’s assent before the enrolment. Approval to use this publicly available de-identified data from MICS online archive was obtained from UNICEF in March 2020.
References
- 1. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1223–49. 10.1016/S0140-6736(20)30752-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet 2017;389:1907–18. 10.1016/S0140-6736(17)30505-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bonjour S, Adair-Rohani H, Wolf J, et al. Solid fuel use for household cooking: country and regional estimates for 1980-2010. Environ Health Perspect 2013;121:784–90. 10.1289/ehp.1205987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Baul TK, Datta D, Alam A. A comparative study on household level energy consumption and related emissions from renewable (biomass) and non-renewable energy sources in Bangladesh. Energy Policy 2018;114:598–608. 10.1016/j.enpol.2017.12.037 [DOI] [Google Scholar]
- 5. Fullerton DG, Bruce N, Gordon SB. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans R Soc Trop Med Hyg 2008;102:843–51. 10.1016/j.trstmh.2008.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lee KK, Bing R, Kiang J, et al. Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob Health 2020;8:e1427–34. 10.1016/S2214-109X(20)30343-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rana J, Uddin J, Peltier R, et al. Associations between indoor air pollution and acute respiratory infections among Under-Five children in Afghanistan: do Ses and sex matter? Int J Environ Res Public Health 2019;16:2910. 10.3390/ijerph16162910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gordon SB, Bruce NG, Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med 2014;2:823–60. 10.1016/S2213-2600(14)70168-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khan MN, B Nurs CZ, Mofizul Islam M, et al. Household air pollution from cooking and risk of adverse health and birth outcomes in Bangladesh: a nationwide population-based study. Environ Health 2017;16:57. 10.1186/s12940-017-0272-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rana J, Islam RM, Khan MN, et al. Association between household air pollution and child mortality in Myanmar using a multilevel mixed-effects poisson regression with robust variance. Sci Rep 2021;11:1–10. 10.1038/s41598-021-92193-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim K-H, Jahan SA, Kabir E. A review of diseases associated with household air pollution due to the use of biomass fuels. J Hazard Mater 2011;192:425–31. 10.1016/j.jhazmat.2011.05.087 [DOI] [PubMed] [Google Scholar]
- 12. Tran TD, Luchters S, Fisher J. Early childhood development: impact of national human development, family poverty, parenting practices and access to early childhood education. Child Care Health Dev 2017;43:415–26. 10.1111/cch.12395 [DOI] [PubMed] [Google Scholar]
- 13. Block ML, Calderón-Garcidueñas L. Air pollution: mechanisms of neuroinflammation and CNS disease. Trends Neurosci 2009;32:506–16. 10.1016/j.tins.2009.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lai AM, Carter E, Shan M, et al. Chemical composition and source apportionment of ambient, household, and personal exposures to PM2.5 in communities using biomass stoves in rural China. Sci Total Environ 2019;646:309–19. 10.1016/j.scitotenv.2018.07.322 [DOI] [PubMed] [Google Scholar]
- 15. Du W, Wang J, Zhuo S, et al. Emissions of particulate PAHs from solid fuel combustion in indoor cookstoves. Sci Total Environ 2021;771:145411. 10.1016/j.scitotenv.2021.145411 [DOI] [PubMed] [Google Scholar]
- 16. Antonsen S, Mok PLH, Webb RT, et al. Exposure to air pollution during childhood and risk of developing schizophrenia: a national cohort study. Lancet Planet Health 2020;4:e64–73. 10.1016/S2542-5196(20)30004-8 [DOI] [PubMed] [Google Scholar]
- 17. Fang X-Y, Strodl E, Wu C-A, et al. Maternal cooking during pregnancy may increase hyperactive behaviors among children aged at around 3 years old. Indoor Air 2020;30:126–36. 10.1111/ina.12614 [DOI] [PubMed] [Google Scholar]
- 18. Jorcano A, Lubczyńska MJ, Pierotti L, et al. Prenatal and postnatal exposure to air pollution and emotional and aggressive symptoms in children from 8 European birth cohorts. Environ Int 2019;131:104927. 10.1016/j.envint.2019.104927 [DOI] [PubMed] [Google Scholar]
- 19. Calderón-Garcidueñas L, Mora-Tiscareño A, Ontiveros E, et al. Air pollution, cognitive deficits and brain abnormalities: a pilot study with children and dogs. Brain Cogn 2008;68:117–27. 10.1016/j.bandc.2008.04.008 [DOI] [PubMed] [Google Scholar]
- 20. Sunyer J, Dadvand P. Pre-Natal brain development as a target for urban air pollution. Basic Clin Pharmacol Toxicol 2019;125 Suppl 3:81–8. 10.1111/bcpt.13226 [DOI] [PubMed] [Google Scholar]
- 21. Nazif-Muñoz JI, Spengler JD, Arku RE, et al. Solid fuel use and early child development disparities in Ghana: analyses by gender and urbanicity. J Expo Sci Environ Epidemiol 2020;30:698–706. 10.1038/s41370-020-0224-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Freire C, Ramos R, Puertas R, et al. Association of traffic-related air pollution with cognitive development in children. J Epidemiol Community Health 2010;64:223–8. 10.1136/jech.2008.084574 [DOI] [PubMed] [Google Scholar]
- 23. McCoy DC, Peet ED, Ezzati M, et al. Early childhood developmental status in low- and middle-income countries: national, regional, and global prevalence estimates using predictive modeling. PLoS Med 2016;13:e1002034–18. 10.1371/journal.pmed.1002034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Walker SP, Wachs TD, Grantham-McGregor S, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet 2011;378:1325–38. 10.1016/S0140-6736(11)60555-2 [DOI] [PubMed] [Google Scholar]
- 25. Black MM, Walker SP, Fernald LC H. Advancing early childhood development: from science to scale 1: early childhood development coming of age: science through the life course early childhood development series Steering Committee HHS public access. Lancet 2017;389:77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Walker SP, Chang SM, Powell CA, et al. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation. J Nutr 2007;137:2464–9. 10.1093/jn/137.11.2464 [DOI] [PubMed] [Google Scholar]
- 27. Karimu A, Asiedu E. Energy poverty and classes missed by a child. Evidence from a developing energy poverty and classes missed by a child. Evidence from a developing country. Univ Ghena Bus Sch 2018. 10.13140/RG.2.2.14996.19845 [DOI] [Google Scholar]
- 28. Naz S, Page A, Agho KE. Household air pollution from use of cooking fuel and under-five mortality: the role of breastfeeding status and kitchen location in Pakistan. PLoS One 2017;12:e0173256. 10.1371/journal.pone.0173256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wasserman GA, Liu X, Parvez F, et al. Child intelligence and reductions in water arsenic and manganese: a two-year follow-up study in Bangladesh. Environ Health Perspect 2016;124:1114–20. 10.1289/ehp.1509974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Khan S, Hancioglu A. Multiple indicator cluster surveys: delivering robust data on children and women across the globe. Stud Fam Plann 2019;50:279–86. 10.1111/sifp.12103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bangladesh Bureau of Statistics (BBS) and UNICEF Bangladesh . Progotir Pathey Bangladesh: multiple indicator cluster survey 2019, survey findings report. Dhaka, 2019. [Google Scholar]
- 32. UNICEF, WHO, World Bank . Advancing early childhood development: from science to scale. Lancet 2016. [Google Scholar]
- 33. UNICEF . The formative years early childhood development: the promise of investing. New York, 2019. Available: https://data.unicef.org/resources/the-formative-years-unicefs-work-on-measuring-ecd/
- 34. Lertxundi A, Andiarena A, Martínez MD, et al. Prenatal exposure to PM2.5 and NO2 and sex-dependent infant cognitive and motor development. Environ Res 2019;174:114–21. 10.1016/j.envres.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 35. Sentís A, Sunyer J, Dalmau-Bueno A, et al. Prenatal and postnatal exposure to NO2 and child attentional function at 4-5years of age. Environ Int 2017;106:170–7. 10.1016/j.envint.2017.05.021 [DOI] [PubMed] [Google Scholar]
- 36. Barros AJD, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 2003;3:1–13. 10.1186/1471-2288-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 2014;12:1495–9. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- 38. Midouhas E, Kokosi T, Flouri E. The quality of air outside and inside the home: associations with emotional and behavioural problem scores in early childhood. BMC Public Health 2019;19:1–10. 10.1186/s12889-019-6733-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kurata M, Takahashi K, Hibiki A. Gender differences in associations of household and ambient air pollution with child health: evidence from household and satellite-based data in Bangladesh. World Dev 2020;128:104779. 10.1016/j.worlddev.2019.104779 [DOI] [Google Scholar]
- 40. Brockmeyer S, D'Angiulli A. How air pollution alters brain development: the role of neuroinflammation. Transl Neurosci 2016;7:24–30. 10.1515/tnsci-2016-0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jo H, Eckel SP, Wang X, et al. Sex-Specific associations of autism spectrum disorder with residential air pollution exposure in a large southern California pregnancy cohort. Environ Pollut 2019;254:113010. 10.1016/j.envpol.2019.113010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Alderman H, Behrman JR, Glewwe P. Evidence of Impact of Interventions on Growth and Development during Early and Middle Childhood. In: Bundy DAP, de SN, Horton S, eds. Child and adolescent health and development. 3rd edition. Washington (dC): the International bank for reconstruction and development / the world bank. Washington (DC), 2017. 10.1596/978-1-4648-0423-6_ch7 [DOI] [PubMed] [Google Scholar]
- 43. Heissler K. Children’s migration for work in Bangladesh: the policy implications of intra-household relations. Dev Pract 2012;22:498–509. 10.1080/09614524.2012.673555 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jech-2021-217554supp001.pdf (166.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request. All data files are publicly available and can be downloaded upon request from the MICS program database: https://mics.unicef.org/surveys. Codes are also available from the corresponding author on reasonable request.