Abstract
Objective
The purpose of this study was to establish within-day intrarater reliability values of ultrasound measurements (excursion and resting thickness).
Methods
Seventeen volunteers met the inclusion criteria for this preliminary study. The right and left hemidiaphragm excursion and resting thickness were compared between 2 measurement sessions using M-mode and B-mode real-time ultrasound, respectively (30 min apart). Intraclass coefficients, coefficients of variation, standard errors of measurement, and minimal detectable changes were calculated to determine intrarater reliability.
Results
The intraclass coefficients of right hemidiaphragm excursion were 0.91 and 0.94 during quiet and deep breathing, respectively. The intraclass coefficient of left hemidiaphragm excursion was 0.95 during quiet breathing. The intraclass coefficients of diaphragm resting thickness were 0.99 and 0.97 in the right and left hemidiaphragm, respectively, which showed high intrarater reliability for ultrasound measurements of both sides of the diaphragm.
Conclusion
This preliminary study suggests that diagnostic ultrasonography could be used as a potential method for measuring the resting thickness and excursion of the right and left hemidiaphragm in people with chronic low back pain. Future research with a larger sample size is needed to confirm these findings.
Key Indexing Terms: Diaphragm, Ultrasonography
Introduction
The diaphragm is the principal muscle of active inspiration. If diaphragm function is impaired, accessory muscles perform this role, but not efficiently, and this results in shortened breath along with diaphragm dysfunction.1, 2, 3 Besides its respiratory function, the diaphragm also is an important functional unit for dynamic spinal stabilization during balancing and loading tasks. Previous studies have shown that individuals with chronic low back pain (CLBP) and sacroiliac joint pain exhibit postural control deficits and abnormal diaphragmatic excursion during tidal breathing while loading tasks.4, 5, 6 Although the diaphragm is involved in respiration and spinal stability, data on its resting thickness and excursion during quiet breathing (QB) and deep breathing (DB) are scarce. In order to confirm diaphragm dysfunction, a reliable and quantifiable measurement tool is necessary for evaluating diaphragm function.7
There are several techniques for evaluating diaphragm function, including fluoroscopy,8 radiography,9 electromyography,2,10,11 dynamic magnetic resonance imaging,4 and high-resolution ultrasound.12 Ultrasound (US) is superior to other measurements because it is safer, cheaper, more readily available, and noninvasive, and can be used to diagnose unilateral diaphragm dysfunction in people with musculoskeletal disorders.1,5,13,14 Several studies have investigated the reliability of ultrasound for assessing diaphragmatic excursion and thickness in both healthy and nonhealthy individuals in different clinical settings.12,15, 16, 17, 18, 19 However, there is a paucity of studies stating the reliability of diaphragmatic resting thickness or excursion during QB and DB in individuals with LBP.15 In addition, few studies have reported the existence of differences between right and left hemidiaphragm measurements (excursion and resting thickness). Based on an earlier study, reliability is dependent on the population studied and the clinical setting used.7 Moreover, to identify true meaningful findings, the standard error of measurement (SEM), minimum detectible change (MDC), and coefficient of variation (CV) as an absolute reliability should also be reported. Understanding these values helps therapists differentiate between measurement error and real change when diaphragm thickness and excursion are measured in different sessions. However, to the best of our knowledge, there are no accuracy and acceptable ranges for absolute reliability (SEM, MDC, and CV) of both hemidiaphragm measurements in people with LBP.
Therefore, the aim of this study was to measure relative and absolute intrarater reliability of ultrasound measurements (resting thickness and excursion) of both sides of the diaphragm during quiet and deep breathing in people with nonspecific chronic low back pain (NS-CLBP).
Materials and Methods
Design
An observational study was conducted between November 2017 and March 2018 in the radiology laboratory of diagnosis imaging, Shohadae Tajrish University Hospital, Tehran, Iran. The study was approved by the Ethics Committee at the School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran (IR. IUMS. FMD. REC 139609221342205). All participants provided written informed consent before being enrolled in the study.
Subjects
Seventeen participants (10 women and 7 men) with NS-CLBP aged 20 to 55 years took part in this study. The individuals were a sample of convenience made up from the most accessible participants.20 They are composed of individuals who agreed to voluntarily participate. Individuals with LBP were included if they had a history of pain with at least 3 months’ duration.21 For ethical considerations and to avoid pain exacerbation during the assessments, the pain intensity at the time of assessment was lower than 5/10 on a numeric pain scale.22 Exclusion criteria were as follows: history of neuromuscular diseases, cardiopulmonary diseases, spinal deformity (kyphosis or scoliosis), or diastolic dysfunction; current pregnancy or cigarette smoking; being an athlete; fatty liver; history of any type of surgery on the spine or of spinal tumor; and pain severity higher than 5.
Procedures
Within-day intrarater reliability tests were performed in the diagnostic imaging laboratory of diagnosis imaging, Shohadae Tajrish University Hospital, Tehran, Iran. All measurements of the diaphragm (excursion and resting thickness) were taken from the same participants by the same operator at 2 different times (∼30 minutes apart) on the same day in a random fashion using the US protocol described later.
Ultrasound Imaging Technique
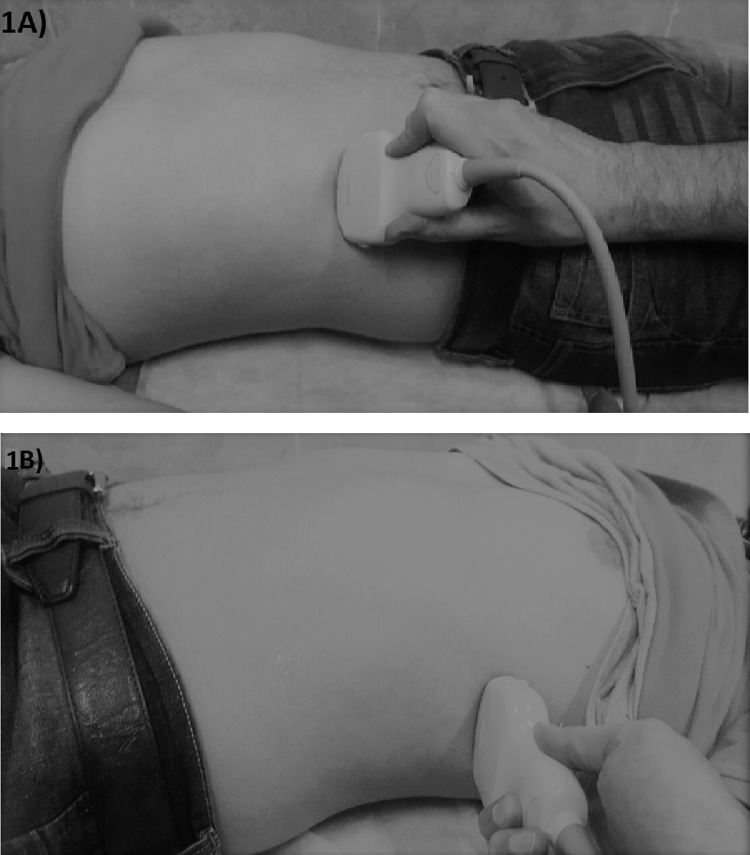
A single experienced radiologist performed the evaluation of the diaphragm using a high-resolution real-time ultrasound apparatus (Toshiba Aplio 300, Tokyo, Japan). The diaphragm excursion and resting thickness were assessed according to previous methods.16,18,19,23 Briefly, for assessment of diaphragmatic excursion, a 3.5 MHz curvilinear transducer was placed on the lower intercostal area between the midclavicular and anterior axillary lines for the right hemidiaphragm and between the anterior and midaxillary lines for the left hemidiaphragm. (Fig 1). For assessment of diaphragm resting thickness, a 7.5 MHz linear array transducer was maneuvered perpendicularly to the chest wall between the mid- and anterior axillary lines on the right and left sides, typically between the 8th and 10th intercostal spaces. This was done in order to have the clearest image of the zone of apposition of the diaphragm, with the transducer spanning 2 ribs, while the individual was breathing comfortably in the supine position.19
Fig 1.
Position of M-mode ultrasound transducers on the lower intercostal area between the midclavicular and anterior axillary lines for the right hemidiaphragm (A) and between the anterior and midaxillary lines for the left hemidiaphragm (B).
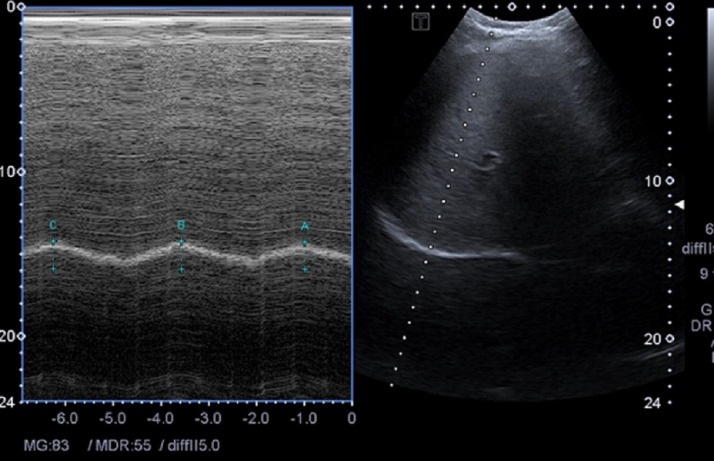
For assessment of diaphragmatic excursion, 2-dimensional B-mode was used to identify the best imaging view of the posterior one-third of the diaphragm, followed by an M-mode recording of consecutive breaths to detect the exact point of end-inspiration and end-expiration, as depicted in Figure 2.24 As shown, the liver was used as a sonic window for the right hemidiaphragm, and the spleen represented the anatomic limit for the left hemidiaphragm.25,26 The transducer was maneuvered medially, cranially, and dorsally to gain the clearest view of both sides of diaphragmatic excursion.16 After confirmation that the individual was breathing regularly, the sonogram and recorded images were frozen. The movement of each side was measured in millimeters in the craniocaudal axis.25,26 As explained by earlier studies, the amplitudes were specified by putting the caliper at the baseline of the diaphragm echoic line and a second caliper at the apex of the diaphragm echoic line (Fig 2).16 The normal resting thickness of the diaphragm was identified in B-mode as the 2 outer echogenic layers of pleura and peritoneum margins where the fibers were parallel.24 All measurements were made by the same operator and the same US machine at 2 different times (∼30 minutes apart). Each time, 3 successive M-mode and B-mode measurements were logged, and the average value was the basis for the statistical analysis.16 The area of measurement on the participant's chest was cleaned between sessions (ie, there were no marks or US gel residue on the individual's skin to show the previous location of the US probe).
Fig 2.
Two-dimensional B-mode was used for identification of the diaphragm, followed by an M-mode scan.
Statistical Analysis
Statistical analyses were performed using SPSS software (version 21, IBM Corp., Armonk, NY), with α = 0.05 and a test power of 0.80. All data are expressed as mean ± SD or 95% confidence interval (CI) for continuous variables. The intraclass coefficient (ICC) 2-way mixed-effect model and corresponding 95% confidence interval was used to assess relative intrarater reliability of the measurements. Relative reliability is defined as the degree to which repeated measurements provide similar results.27
In this study, we used the ICC as described by Shrout and Fleiss,28 since only 1 radiologist assessed the same population. Relative reliability values such as ICC are not enough to explain the outcomes in the context of an individual score. The precision of measurement was assessed by determining the CV, SEM, and MDC for all measurements. Bland-Altman plots were determined for quiet- and deep-breathing excursion of the diaphragm. The CV, SEM, and MDC were calculated manually as described by previous methods.27 The absolute reliability (SEM) is defined as the difference (error) between frequent measurements.29 An MDC represents the smallest change necessary to achieve 95% confidence that a variation is not the result of random change or measurement error.30,31 The CV, which is a measure of dispersion, was used to assess the precision of trials.27,32
Bland-Altman plotting was used to assess the intratester agreement (intrarater reproducibility) for the variables measured by comparing the differences between recurrent scores against their means.33
Results
The demographic data for participants are summarized in Table 1. The distribution of all diaphragm excursions and resting thicknesses are showed as mean ± SD (in mm) for the right and left hemidiaphragm. Approximately no significant differences were present between the observed distributions and normal distributions of excursion and thickness variables.
Table 1.
Demographic Data of the Participants (10 Women, 7 Men)
| Variable | Value |
|---|---|
| Age (y) | 38.7 ± 11.23 |
| Weight (kg) | 66.7 ± 9.14 |
| Height (cm) | 165 ± 9.12 |
| BMI (kg/m2) | 24.5 ± 3.26 |
| Pain (VAS) | 2.3 ± 1.64 |
Values are given as mean ± SD.
BMI, body mass index; SD, standard deviation; VAS, visual analog scale.
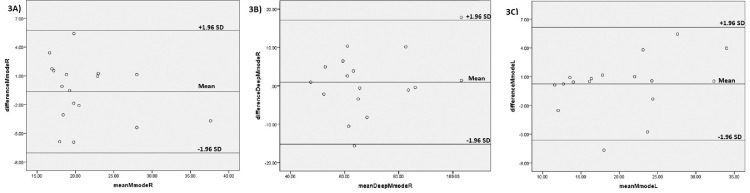
The mean excursion and resting thickness of the right and left hemidiaphragm are presented in Table 2. The mean excursion of the right hemidiaphragm is slightly greater than that of the left hemidiaphragm, and the mean thickness of the left hemidiaphragm is slightly greater than that of the right hemidiaphragm Table 3. presents the ICC3,1, SEM, CV (SEM as % mean), and MDC for within-day reliability of US measurements of the diaphragm that were taken during QB and DB. In the analysis of relative intrarater reliability, the correlation between 2 measurement sessions was highly significant for right hemidiaphragm excursion during QB and DB—respectively, ICC3,1 =0.91; 95% CI, 0.75-0.96; P < .001; and ICC3,1 = 0.94; 95% CI, 0.83-0.97; P < .001—and for left hemidiaphragm excursion during QB (ICC3,1 = 0.95; 95% CI, 0.87-0.98; P < 0.001). The results indicate excellent intrarater reliability for the US measurements (excursion and resting thickness) of the right and left hemidiaphragm in all participants. Within-day reliability assessment demonstrated that during QB, the SEM of right hemidiaphragm excursion (1.5) was slightly larger than that of left hemidiaphragm excursion (1.4). Likewise, the MDC and CV of diaphragm excursion during QB were slightly higher in the right hemidiaphragm than the left hemidiaphragm. The SEM of left hemidiaphragm resting thicknesses (0.16) was slightly higher than that of right hemidiaphragm resting thickness (0.08). Similarly, the MDC and CV of diaphragm resting thicknesses were slightly higher in the left hemidiaphragm than the right hemidiaphragm. The Bland-Altman plots of agreement in US measurements of the right and left hemidiaphragm excursion between 2 sessions are given in Figure 3. They indicate that the difference between the excursion measurements in 2 different sessions did not correlate with the score of the excursion measurements in the right hemidiaphragm. However, in the left hemidiaphragm, this difference (y-axis) was larger in the higher excursion score (x-axis) and smaller in the lower excursion score.
Table 2.
Measurements for Right and Left Hemidiaphragm Excursion and Resting Thickness
| Hemidiaphragm | Excursion (QB) |
Excursion (DB) |
Resting Thickness |
|||
|---|---|---|---|---|---|---|
| Session 1 (mm) | Session 2 (mm) | Session 1 (mm) | Session 2 (mm) | Session 1 (mm) | Session 2 (mm) | |
| Right | 21.6 ± 6.03 | 21 ± 5.1 | 69.9 ± 18.25 | 68.9 ± 15.6 | 2.6 ± 0.84 | 2.5 ± 0.84 |
| Left | 20.32 ± 7.5 | 20.08 ± 6.5 | — | — | 2.8 ± 1.1 | 2.6 ± 0.98 |
Values are given as mean ± SD.
DB, deep breathing; QB, quiet breathing; SD, standard deviation.
Table 3.
Intrarater Reliability Values for Right and Left Hemidiaphragm Excursion and Resting Thickness
| Measurement | ICC3,1 (95% CI) | SEM (mm) | MDC (mm) | CV (%) |
|---|---|---|---|---|
| Right hemidiaphragm excursion, quiet breathing | 0.91 (0.75-0.97) | 1.5 | 4.3 | 7.4 |
| Right hemidiaphragm excursion, deep breathing | 0.94 (0.83-0.98) | 3.8 | 10.6 | 5.5 |
| Left hemidiaphragm excursion, quiet breathing | 0.95 (0.87-0.98) | 1.4 | 4.02 | 7.2 |
| Right hemidiaphragm resting thickness | 0.99 (0.98-0.99) | 0.08 | 0.2 | 3.3 |
| Left hemidiaphragm resting thickness | 0.97 (0.93-0.99) | 0.16 | 0.4 | 6.5 |
CI, confidence interval; CV, coefficient of variation; ICC, intraclass correlation coefficient; MDC, minimal detectable change; SEM, standard error of measurement.
Fig 3.
Bland-Altman plots representing mean differences and 95% confidence limits between 2 measurement sessions (measurements of excursion) during quiet and deep breathing in the right and left hemidiaphragms: Quiet breathing in the right hemidiaphragm (A), deep breathing in the right hemidiaphragm (B), quiet breathing in the left hemidiaphragm (C).
Discussion
The present study evaluated the absolute and relative reliability of diaphragmatic excursion and resting thickness on both sides using US in individuals with NS-CLBP in the supine position.
Like any other measurement, it is necessary to assess the reliability of ultrasound measurements before evaluating the function of the diaphragm. Based on earlier studies,7 reliability was not a fixed feature but was dependent on the studied population and clinical setting. Recent studies have focused on the thickness and excursion of the diaphragm in healthy individuals and in pathological states such as chronic obstructive pulmonary disease.12,16,34,35 Based on previous studies, LBP is commonly associated with respiratory dysfunction.36, 37, 38, 39 According to previous studies, mechanical and neural differences exist between the right and left hemidiaphragms.40, 41, 42 Thus, understanding the function and structural integrity of each hemidiaphragm in individuals with NS-CLBP could possibly provide an alternative approach for enhancing examination and treatment of NS-CLBP. The reliability method using an average of 3 trials produced good to excellent reliability scores (0.83-0.94) for measuring excursion and resting thickness of both sides of the diaphragm. This is contrary to the results of some other studies that have found it difficult to consistently visualize and measure the thickness and excursion of the left diaphragm. In the present study, the left hemidiaphragm was always seen, and measurements showed slightly better reliability than measurements of the right hemidiaphragm.
It should be considered that results obtained in this study suggest that US might be used as a reliable technique for assessing right and left hemidiaphragm dysfunction in individuals with LBP, but further research with a larger sample size is needed to confirm it.
This is important, because right or left hemidiaphragm dysfunction can be involved in various clinical situations, including pain.5 Based on earlier studies, dysfunction in either hemidiaphragm (right or left) may lead to altered motor control strategies and alterations of movement patterns and challenge the stability of the spine, resulting in chronic pain.5,43 It should be noted that testing positions and clinical settings applied in this study were different from those used in other studies.12,15, 16, 17, 18 There is evidence that the supine position is the best posture for showing diaphragmatic impairment.44 Therefore, we established intrarater reliability values of ultrasound measurements (resting thickness and excursion) of both sides of the diaphragm in the supine position during QB and DB in individuals with NS-CLBP.
This study measured the complete motion of the right hemidiaphragm in all participants during QB, but the expanding lung obstructed measurement of the whole diaphragm motion in some participants in DB. In these conditions, the probe could be maneuvered caudally to improve the recording of the complete motion of the right hemidiaphragm. It is believed that visualizing the left hemidiaphragm is not an easy task, since the window of the spleen is smaller than the liver window.35 However, the excursion of the left hemidiaphragm was measured only during QB; we were not able to measure it during DB, for reasons including the descending of the lung and difficulties in adjusting the probe position. We found mean hemidiaphragm excursions of 21 ± 5.1 mm and 20.08 ± 6.5 mm for the right and left hemidiaphragm, respectively, in QB, and of 68.9 ± 15.6 mm for the right hemidiaphragm in DB. These values are slightly higher than those obtained in other studies.12,15,45,46 Moreover, preceding studies have shown that the inspired volume and testing position are related in the sense that hemidiaphragm excursion is greater in the supine position than in either sitting or standing.23,45,46 The results of the current study are in line with this finding. In our study, the mean resting thicknesses of the right and left hemidiaphragms (2.6 ± 0.84 mm and 2.8 ± 1.1 mm, respectively) were less than those reported in other studies.35,47 It seems that the mean hemidiaphragm resting thickness in studies that recruit participants with LBP are not similar to those from studies that recruited participants without LBP. Investigations on the reproducibility of measurements of diaphragm excursion report that relative reliability (ICC) ranges from 0.79 to 0.92 in adults.12,15,16,48 The reliability of those measurements in the present study (0.91-0.95) is consistent with previous studies, which report good to excellent ICC values. The reliability of measurements for resting thickness of the right and left hemidiaphragms were 0.99 and 0.97, respectively. Our findings confirm values previously outlined in the literature, finding excellent ICC scores when measuring diaphragm thickness in healthy individuals or volunteer patients.35,47 The excellent reliability of hemidiaphragm measurements in the present study can be influenced by several factors, such as an experienced rater (in this case an experienced radiologist), accurate identification of anatomic landmarks, 3 replications of each measurement, and participant familiarity with the testing processes. In a study by Dankaerts et al,49 familiarity improved reliability.
Practically, the SEM gives more suitable information than the ICC,50 and the CV is a good option for comparing the relative measurement error of variables with different measurement units.27,32 It is important to consider that no sufficient normative data are available for hemidiaphragm measurements (SEM, MDC, and CV) in the literature that could enable us to compare the results. Only 1 study has determined the SEM, MDC, and CV of right hemidiaphragm excursion,15 two others have determined SEM or CV alone.17,51 The SEM in this study (1.5) was consistent with that in the study by Blaney et al,17 which reports SEMs of right diaphragmatic excursion between 1.3 and 1.6 mm for different breathing, and lower than that in a study by Mohan et al (2.56 mm).15 The low SEM of hemidiaphragm excursion could be considered acceptable for diaphragm excursion using US. In the present study, the SEMs for resting thickness were 0.08 and 0.16—less than 1 mm (mostly less than 0.5 mm)—and the corresponding MDCs were 0.2 and 0.4 mm for the right and left diaphragm, respectively (Table 3). This means that the measurement error is around 0.08 to 0.16 and the 0.2 to 0.4 mm change in muscle thickness seems necessary to be sure that a true change occurred. The MDC can be particularly applied to interpret the relevance of any changes recorded after an intervention.30,31 The MDC of right hemidiaphragm excursion (4.3 mm) was lower than that in the Mohan et al study (7.09 mm).15 Clinically, according to the MDC values, changes of 4.3 and 4.02 mm are required for right and left hemidiaphragm excursion, respectively, because of changes in any sort of intervention measures. Although the SEM and MDC would need to be assessed in each experimental situation, there is no consensus on acceptable data for them in the literature. Therefore, we believe that MDC values of less than 1 mm for diaphragm resting thickness and around 4 mm for diaphragm excursion are sufficiently low and clinically acceptable to detect changes over time.
The CV values of right and left hemidiaphragm excursion were almost similar. Therefore, the measurements of excursion in both hemidiaphragms display approximately the same level of precision. The CV results in this study are lower than in a previous study that reported 12% to 13%.51 However, the sample size in the present study was lower, suggesting that caution is needed when comparing the results of the 2 studies.
According to the Bland-Altman plots (Fig 3A and 3B), US measurements of the right hemidiaphragm excursion demonstrated no systematic pattern of variability in measurement differences between 2 sessions (test and retest). But in excursion of the left hemidiaphragm, the Bland-Altman plot (Fig 3C) shows higher differences between measurements from the 2 sessions, suggesting that SEM and MDC might be greater in the higher excursion scores than in the lower excursion scores. This result may be due to the difficulty of viewing the left hemidiaphragm.35 However, there was not enough power to discover this alteration between different measurement scores.
The present study reports high reliability of US measurements for individuals with NS-CLBP. Reliable diaphragm assessment is a screening tool to discover the left and right hemidiaphragm thickness and excursion, before and after diaphragm training, to determine the effect of each hemidiaphragm's function on postural stability and disability in individuals with NS-CLBP. Thus, our results provide novel information that may be useful in both clinical and research settings.
In our study, all the SEMs, MDCs, and CVs were relatively small, which makes them favorable measures for further studies to determine normative SEM, MDC, and CV values that can guide the evaluation of each variable for diaphragmatic measurement.
Limitations
There are some limitations to this study. First, the sample size was not big enough. Thus, future studies with a larger sample size are suggested. Second, the study was limited to only intrarater reliability. We suggest assessing the interrater reliability as well. Third, the reliability of the measurements was within-day with a relatively short time between sessions; it is possible that there was some recall bias. Fourth, the sample size was not calculated, and sampling was done according to the most accessible participants. To improve the generalizability of the results, we suggest the same study but considering a longer time interval, a larger sample size, and comparison of the results between individuals with and without LBP.
Conclusion
This preliminary study suggests that diagnostic ultrasonography could possibly be used when measuring the resting thickness and excursion of the right and left hemidiaphragms in people with chronic LBP.
Acknowledgments
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): M.Z., S.N.D., J.S., A.M.A., A.Z.J.
Design (planned the methods to generate the results): M.Z., S.N.D., H.R.H., J.S., A.M.A.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): M.Z., S.N.D., H.R.H., A.M.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): M.Z., H.R.H.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): M.Z., S.N.D., A.M.A.
Literature search (performed the literature search): M.Z.
Writing (responsible for writing a substantive part of the manuscript): M.Z., A.Z.J.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): M.Z., S.N.D., H.R.H., J.S., A.M.A., A.Z.J.
Practical Applications.
-
•
Measurements of diaphragm excursion and resting thickness using ultrasonography exhibited excellent reliability.
-
•
Reported absolute reliability parameters guide the interpretation of clinical and research data.
-
•
A reliable and easily applicable tool for assessing diaphragm function was provided.
Alt-text: Unlabelled box
References
- 1.Hodges PW, Gandevia SC. Activation of the human diaphragm during a repetitive postural task. J Physiol. 2000;1:165–175. doi: 10.1111/j.1469-7793.2000.t01-1-00165.xm. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hodges PW, Butler JE, McKenzie DK, Gandevia SC. Contraction of the human diaphragm during rapid postural adjustments. J Physiol. 1997;505(2):539–548. doi: 10.1111/j.1469-7793.1997.539bb.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodges P, Kaigle Holm A, et al. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine (Phila Pa 1976) 1976;28(23):2594–2601. doi: 10.1097/01.BRS.0000096676.14323.25. [DOI] [PubMed] [Google Scholar]
- 4.Kolar P, Sulc J, Kyncl M, et al. Postural function of the diaphragm in persons with and without chronic low back pain. J Orthop Sports Phys Ther. 2012;42(4):352–362. doi: 10.2519/jospt.2012.3830. [DOI] [PubMed] [Google Scholar]
- 5.O'Sullivan PB, Beales DJ, Beetham JA, et al. Altered motor control strategies in subjects with sacroiliac joint pain during the active straight-leg-raise test. Spine (Phila Pa 1976) 2002;27(1):E1–E8. doi: 10.1097/00007632-200201010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Vostatek P, Novak D, Rychnovsky T, Rychnovska S. Diaphragm postural function analysis using magnetic resonance imaging. PLoS One. 2013;8(3):14. doi: 10.1371/journal.pone.0056724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carter RE, Lubinsky J. Elsevier Health Sciences; St Louis, MO: 2015. Rehabilitation Research: Principles and Applications. [Google Scholar]
- 8.Sanchez de Toledo J, Munoz R, Landsittel D, et al. Diagnosis of abnormal diaphragm motion after cardiothoracic surgery: ultrasound performed by a cardiac intensivist vs. fluoroscopy. Congenit Heart Dis. 2010;5(6):565–572. doi: 10.1111/j.1747-0803.2010.00431.x. [DOI] [PubMed] [Google Scholar]
- 9.Saltiel RV, Grams ST, Pedrini A, Paulin E. High reliability of measure of diaphragmatic mobility by radiographic method in healthy individuals. Braz J Phys Ther. 2013;17(2):128–136. doi: 10.1590/S1413-35552012005000076. [DOI] [PubMed] [Google Scholar]
- 10.Hodges PW, Eriksson AE, Shirley D, Gandevia SC. Intra-abdominal pressure increases stiffness of the lumbar spine. J Biomech. 2005;38(9):1873–1880. doi: 10.1016/j.jbiomech.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Hodges PW, Heijnen I, Gandevia SC. Postural activity of the diaphragm is reduced in humans when respiratory demand increases. J Physiol. 2001;537(3):999–1008. doi: 10.1111/j.1469-7793.2001.00999.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scarlata S, Mancini D, Laudisio A, Benigni A, Antonelli Incalzi R. Reproducibility and clinical correlates of supine diaphragmatic motion measured by M-mode ultrasonography in healthy volunteers. Respiration. 2018;96:259–266. doi: 10.1159/000489229. [DOI] [PubMed] [Google Scholar]
- 13.Cohen E, Mier A, Heywood P, Murphy K, Boultbee J, Guz A. Diaphragmatic movement in hemiplegic patients measured by ultrasonography. Thorax. 1994;49(9):890–895. doi: 10.1136/thx.49.9.890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Sullivan PB, Beales DJ. Changes in pelvic floor and diaphragm kinematics and respiratory patterns in subjects with sacroiliac joint pain following a motor learning intervention: a case series. Man Ther. 2007;12(3):209–218. doi: 10.1016/j.math.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Mohan V, Hashim UF, Dom SM, Sitilerpisan P, Paungmali A. Reliability of diaphragmatic mobility assessment using a real time ultrasound among non-specific low back pain. Bangladesh J Med Sci. 2017;16(3):443–447. [Google Scholar]
- 16.Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by M-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135(2):391–400. doi: 10.1378/chest.08-1541. [DOI] [PubMed] [Google Scholar]
- 17.Blaney F, English CS, Sawyer T. Sonographic measurement of diaphragmatic displacement during tidal breathing manoeuvres—a reliability study. Aust J Physiother. 1999;45(1):41–43. [PubMed] [Google Scholar]
- 18.Noh DK, Koh JH, You JS. Inter- and intratester reliability values of ultrasound imaging measurements of diaphragm movement in the thoracic and thoracolumbar curves in adolescent idiopathic scoliosis. Physiother Theory Pract. 2016;32(2):139–143. doi: 10.3109/09593985.2015.1091871. [DOI] [PubMed] [Google Scholar]
- 19.Sarwal A, Walker FO, Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013;47(3):319–329. doi: 10.1002/mus.23671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bujang MA, Baharum N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review. Arch Orofac Sci. 2017;12(1):1–11. [Google Scholar]
- 21.Rubin DI. Epidemiology and risk factors for spine pain. Neurol Clin. 2007;25(2):353–371. doi: 10.1016/j.ncl.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 22.Johnson C. Measuring pain—visual analog scale versus numeric pain scale: what is the difference? J Chiropr Med. 2005;4(1):43–44. doi: 10.1016/S0899-3467(07)60112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Houston JG, Angus RM, Cowan MD, McMillan NC, Thomson NC. Ultrasound assessment of normal hemidiaphragmatic movement: relation to inspiratory volume. Thorax. 1994;49(5):500–503. doi: 10.1136/thx.49.5.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Thoracic Society, European Respiratory Society ATS/ERS statement on respiratory muscle testing. Am J Resp Crit Care Med. 2002;166(4):518–624. doi: 10.1164/rccm.166.4.518. [DOI] [PubMed] [Google Scholar]
- 25.Epelman M, Navarro OM, Daneman A, Miller SF. M-mode sonography of diaphragmatic motion: description of technique and experience in 278 pediatric patients. Pediatr Radiol. 2005;35(7):661–667. doi: 10.1007/s00247-005-1433-7. [DOI] [PubMed] [Google Scholar]
- 26.Urvoas E, Pariente D, Fausser C, Lipsich J, Taleb R, Devictor D. Diaphragmatic paralysis in children: diagnosis by TM-mode ultrasound. Pediatr Radiol. 1994;24(8):564–568. doi: 10.1007/BF02012733. [DOI] [PubMed] [Google Scholar]
- 27.Portney LG, Watkins MP. Vol 892: Pearson/Prentice Hall; Upper Saddle River, NJ: 2009. Foundations of clinical research: applications to practice. [Google Scholar]
- 28.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 29.Bueno-Gracia E, Malo-Urries M, Ruiz-de-Escudero-Zapico A, et al. Reliability of measurement of the carpal tunnel and median nerve in asymptomatic subjects with ultrasound. Musculoskelet Sci Pract. 2017;32:17–22. doi: 10.1016/j.msksp.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 30.Haley SM, Fragala-Pinkham MA. Interpreting change scores of tests and measures used in physical therapy. Phys Ther. 2006;86(5):735–743. [PubMed] [Google Scholar]
- 31.Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, Magel JS. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90(1):87–94. doi: 10.1016/j.apmr.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 32.Mohallem DF., Tavares M., Silva P., Guimarães E., Freitas RJABdMVeZ. Avaliação do coeficiente de variação como medida da precisão em experimentos com. frangos de corte. 2008;60(2):449–453. [Google Scholar]
- 33.Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–310. [PubMed] [Google Scholar]
- 34.Carrillo-Esper R, Perez-Calatayud AA, Arch-Tirado E, et al. Standardization of sonographic diaphragm thickness evaluations in healthy volunteers. Respir Care. 2016;61(7):920–924. doi: 10.4187/respcare.03999. [DOI] [PubMed] [Google Scholar]
- 35.Goligher EC, Laghi F, Detsky ME, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity. J Intensive Care Med. 2015;41(4):734. doi: 10.1007/s00134-015-3724-2. [DOI] [PubMed] [Google Scholar]
- 36.Mohan V, Paungmali A, Sitilerpisan P, Hashim UF, Mazlan MB, Nasuha TN. Respiratory characteristics of individuals with non-specific low back pain: a cross-sectional study. Nurs Health Sci. 2018;20(2):224–230. doi: 10.1111/nhs.12406. [DOI] [PubMed] [Google Scholar]
- 37.Janssens L, Brumagne S, McConnell AK, Hermans G, Troosters T, Gayan-Ramirez G. Greater diaphragm fatigability in individuals with recurrent low back pain. Respir Physiol Neurobiol. 2013;188(2):119–123. doi: 10.1016/j.resp.2013.05.028. [DOI] [PubMed] [Google Scholar]
- 38.Smith MD, Russell A, Hodges PW. The relationship between incontinence, breathing disorders, gastrointestinal symptoms, and back pain in women: a longitudinal cohort study. Clin J Pain. 2014;30(2):162–167. doi: 10.1097/AJP.0b013e31828b10fe. [DOI] [PubMed] [Google Scholar]
- 39.Smith MD, Russell A, Hodges PW. Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust J Physiother. 2006;52(1):11–16. doi: 10.1016/s0004-9514(06)70057-5. [DOI] [PubMed] [Google Scholar]
- 40.Hruska RJ., Jr. Influences of dysfunctional respiratory mechanics on orofacial pain. Dent Clin North Am. 1997;41(2):211–227. [PubMed] [Google Scholar]
- 41.Reddy V, Sharma S, Cobanoglu A. What dictates the position of the diaphragm—the heart or the liver? a review of sixty-five cases. J Thorac Cardiovasc Surg. 1994;108(4):687–691. [PubMed] [Google Scholar]
- 42.Boyle KL, Olinick J, Lewis C. The value of blowing up a balloon. N Am J Sports Phys Ther. 2010;5(3):179–188. [PMC free article] [PubMed] [Google Scholar]
- 43.Terada M, Kosik KB, McCann RS, Gribble PA. Diaphragm contractility in individuals with chronic ankle instability. Med Sci Sports Exerc. 2016;48(10):2040–2045. doi: 10.1249/MSS.0000000000000994. [DOI] [PubMed] [Google Scholar]
- 44.Fromageot C, Lofaso F, Annane D, et al. Supine fall in lung volumes in the assessment of diaphragmatic weakness in neuromuscular disorders. Arch Phys Med Rehabil. 2001;82(1):123–128. doi: 10.1053/apmr.2001.18053. [DOI] [PubMed] [Google Scholar]
- 45.Leal BE, Goncalves MA, Lisboa LG, et al. Validity and reliability of fluoroscopy for digital radiography: a new way to evaluate diaphragmatic mobility. BMC Pulm Med. 2017;17(1):62. doi: 10.1186/s12890-017-0402-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takazakura R, Takahashi M, Nitta N, Murata K. Diaphragmatic motion in the sitting and supine positions: healthy subject study using a vertically open magnetic resonance system. Journal Magn Reson Imaging. 2004;19(5):605–609. doi: 10.1002/jmri.20051. [DOI] [PubMed] [Google Scholar]
- 47.Boon AJ, Harper CJ, Ghahfarokhi LS, Strommen JA, Watson JC, Sorenson EJ. Two-dimensional ultrasound imaging of the diaphragm: quantitative values in normal subjects. Muscle Nerve. 2013;47(6):884–889. doi: 10.1002/mus.23702. [DOI] [PubMed] [Google Scholar]
- 48.Grams ST, von Saltiel R, Mayer AF, et al. Assessment of the reproducibility of the indirect ultrasound method of measuring diaphragm mobility. Clin Physiol Funct Imaging. 2014;34(1):18–25. doi: 10.1111/cpf.12058. [DOI] [PubMed] [Google Scholar]
- 49.Dankaerts W, O'Sullivan P, Straker L, Burnett A, Skouen J. The inter-examiner reliability of a classification method for non-specific chronic low back pain patients with motor control impairment. Man Ther. 2006;11(1):28–39. doi: 10.1016/j.math.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 50.Rankin G, Stokes M. Reliability of assessment tools in rehabilitation: an illustration of appropriate statistical analyses. Clin Rehabil. 1998;12(3):187–199. doi: 10.1191/026921598672178340. [DOI] [PubMed] [Google Scholar]
- 51.Houston JG, Morris AD, Howie CA, Reid JL, McMillan N. Technical report: quantitative assessment of diaphragmatic movement—a reproducible method using ultrasound. Clin Radiol. 1992;46(6):405–407. doi: 10.1016/s0009-9260(05)80688-9. [DOI] [PubMed] [Google Scholar]