Abstract
Objectives
During the COVID-19 pandemic, excessive workload, a rapidly changing workplace environment, the danger of carrying the virus and transmitting the disease to their families, relatives and those they live with creates stress for the medical workers. In our study, we aimed to evaluate the state and trait anxiety levels of healthcare professionals who encounter patients with suspected COVID-19 infection and related factors.
Method
Data were collected from healthcare professionals working with patients diagnosed or suspected with COVID-19 via online self-report questionnaire between 9–19 April 2020. The state (STAI-S) and trait anxiety (STAI-T) scale was used to measure anxiety.
Results
A total of 291 healthcare professionals, 216 women and 75 men, participated in the study. Women's state and trait anxiety were significantly higher than men's. 11 participants without any lifetime psychiatric illness experienced psychiatric symptoms and consulted to a psychiatrist. The state anxiety of those who have children, nurses and those working in branches directly related to the pandemic (Infectious Diseases, Respiratory Diseases, Emergency Medicine, Internal Medicine, Radiology, Anesthesiology and Reanimation) was higher than others. The state anxiety of those who thought they were not protected with personal protective equipment and those who did not stay in their own home was higher than others.
Conclusions
At the forefront of the fight against COVID-19, there are medical personnel who pay a serious psychological cost. Especially in terms of anxiety, we should pay attention to women, workers with children, nurses and people working in branches that are directly related to pandemics.
Keywords: coronavirus, medical staff, professional experience, behavioral response, isolation measures
Introduction
Anxiety is a feeling of distress, excitement, and fear that something bad will suddenly happen. Anxiety is characterized by physical symptoms such as palpitations, rapid breathing, tremors, excessive sweating, dry mouth, and muscle tension. Anxiety can be inhibitory but sometimes it may help the person adapt to new conditions.1
State anxiety is excessive anxiety when there is an undesirable, dangerous situation, whereas trait anxiety is excessive anxiety for no apparent reason or disproportionate anxiety for that reason.2 Excessive anxiety, which is likely to occur when healthcare professionals encounter an epidemic, may affect their ability of paying attention, understanding and decision-making.3
The new Coronavirus was first detected in Wuhan, China in December 2019 and spread rapidly all over the World. It was named SARS-CoV-2 by the International Virus Taxonomy Board and the disease caused by infection of this virus was named COVID-19 by the World Health Organization (WHO).4 The rapid spread of the disease and the need for hospitalization and/or intensive care units strain the capacity of health systems.5
The Institute of Medicine commenced triple aim for delivery of healthcare services which focused on improving population health, better patient experiences and lower costs. Nevertheless, increasing stress and job dissatisfaction seen in clinicians and other staff brought about a fourth aim ‘improving staff well-being’ making the quadruple aim. Definitely, added stress of Covid-19 and rising burn out in clinical staff highlighted the importance of caring for the carers.6,7
During the pandemic period, all people faced various stress factors (quarantine that prevents people from going out, restrictions on commuting, worrying about getting sick, fear of losing loved ones, friends and family). Healthcare professionals experience the same social changes and try to cope with the same emotions. Despite people who can reduce the risk of catching the virus by being able to lock themselves down at home or work from home, healthcare professionals go to medical institutions-where sick people are excessively found- to do their jobs and take the highest risk of getting infected so the anxiety is most likely to arise. With a rapidly changing and evolving practice environment, very different from what they are familiar with, healthcare workers are under excessive workload and pressure to make the right decision in the dilemmas they face. In the workplace, when their colleagues get sick, they have to treat them and may even witness their death.
The growing number of confirmed and suspected cases, the overwhelming workload, long-term shifts, the necessity of wearing equipment that may cause physical discomfort and breathing difficulties and fear that personal protective equipment may be depleted or insufficient, feeling unprepared to perform clinical interventions for patients, new protocols, isolating themselves from their elementary and extended families, the wide coverage of this issue and negative news in the media, the lack of specific drugs and insufficient support may increase the mental burden of health professionals in this period.5,8,9 Healthcare professionals are generally confident and many do not seek help. This trait may not be beneficial for them at a time when they have to deal with a disease they have not encountered before and where most clinicians are relocated outside of their clinical specialty, with increased workload.10
Researchers investigating the immediate effects of emerging infectious diseases on healthcare staff reported high rates of depression and anxiety during the SARS outbreak.11 Guilt, anger, anxiety, fear, shame, and depression have been shown to lead to resignation and poor job performance in healthcare workers during the SARS epidemic. In a study of healthcare workers struggling with coronavirus pandemic in Wuhan, health providers experienced symptoms of various mental illnesses such as insomnia, fear and irritability, symptoms of anxiety, depression, and denial.12
The front-line healthcare professionals feel emotionally pressured, especially because they have to choose between the responsibilities of their families and the sense of inner duty they feel towards patients. It is common to express emotions that are not expressed verbally by the teams with absenteeism and deficiencies in the work environment.9 Even if adequate beds and ventilators are provided, they will not work without adequate healthcare professionals. During this crisis, maintaining a sufficient workforce in healthcare services is possible not only with a sufficient number of physicians, nurses, and other health personnel but also by maximizing the capacity of each to provide care. Considering the increase in critically ill patients, the epidemic can last for weeks to months, and healthcare professionals have to show full performance over a long period.10 In our study, we aimed to evaluate the anxiety level of healthcare professionals who are in direct contact with patients suspected of having COVID-19 infection and to investigate related factors with anxiety in a sample from our country during the early phase of pandemic to detect more vulnerable healthcare workers and follow them more closely to prevent adverse psychiatric outcomes.
Method
Participants
The research data were collected from healthcare providers who worked with patients considered having COVID-19 by snowballing sampling through an online survey between April 9–19, 2020. Those who are administrative staff, who leave work because of health conditions, pregnancy, child care and similar reasons, those who only work in their own branch without contacting the departments related to COVID-19, remote workers and those who do not work because their department or service is closed were asked not to fill out the questionnaire.
The ethical approval for the study was granted by Bezmialem Vakıf University Non-Interventional Research Ethics Committee with the number 06/111.
Data collection tools
In the questionnaire, the first part included sociodemographic information and questions about how their daily habits changed, the second part included the characteristics of the working environment, the third part included the isolation measures they took at home, and the last part was State-Trait Anxiety Inventory (STAI-S and STAI-T).
Sociodemographic data form: This form was developed by the researchers, comprised questions about the age, gender, marital status of the respondents, the people they live with, if any, additional medical or psychiatric diseases and the medications used to treat medical or psychiatric diseases.
Questions about daily habits: Changes in smoking status, alcohol consumption, the amount of eating, sleeping, and time spent daily on social media since the outbreak was asked.
Features related to the working environment: comprised occupation, work experience, main specialty, whether the participants received training before working in the pandemic, whether or not they found it useful, how much they felt protected with personal protective equipment, how many days they have been working in COVID-19 related fields, weekly working time with COVID-19 patients. If the healthcare worker continues to work in his/her own branch was asked about the subjective anxiety he/she felt there, and whether he/she benefited from the guidelines prepared for patient follow-up.
Isolation precautions: The measures healthcare workers took to protect the households included questions whether he/she went home or stayed somewhere else, how he/she isolated from others at home, what measures were taken, etc.
State Trait Anxiety Inventory (STAI): It is a scale developed by Spielberger et al., inspired by the two-factor anxiety theory to determine state and trait anxiety levels separately.2 The State-Trait Anxiety Inventory (STAI-S and STAI-T) is a self-report questionnaire consisting of brief expressions. It comprises two subscales of 20 items, forty items in total. The Turkish validity and reliability study was conducted by Öner and LeCompte in 1985.13 Direct and inverted statements are added together by weighing separately. The total score obtained on both scales ranges from 20 to 80. The higher scores indicate higher anxiety levels.
Procedure
Healthcare workers from WhatsApp and Facebook applications were directed to the online self-report questionnaire. The informed consent of individuals was asked with a yes or no question before survey confirming willingness to take part in the study. Only those who answered yes for voluntary consent could see the survey and participate in the study. The respondents were able to leave the questionnaire whenever they wanted.
Statistical analysis
The data were analyzed with SPSS 22 program (Statistical Package for Social Sciences, IBM Inc., Chicago, IL, USA). Numbers, percentages, means and standard deviations were used in the descriptive statistics of categorical variables. Normal distribution of data was assessed using the Kolmogorov-Smirnov test and normality plots. Independent samples t-test and the Mann-Whitney U test were used to test the significance of the difference between two independent groups. One-way ANOVA was used for parametric data and Kruskal-Wallis test was used for non-parametric data in groups of three or more. In cases where the ANOVA test was significant, the posthoc Tukey test was used to find out which groups differ. Spearman correlation analysis was performed for nonparametric data. A multiple linear regression analysis was applied to confirm the contribution of relevant predictors on state anxiety. A p-value was considered significant under .05.
Results
A total of 291 healthcare workers, 216 women and 75 men took part in the study. 47.8% of the study participants were doctors, 36.4% were nurses and 15.8% were other health care workers. In the group specified as the other health care workers, there were hospital secretaries, patient caregivers and cleaning staff working in the departments related to COVID-19.
The mean age was 34.8 ± 8.5 years. The total years they worked in the profession varied between the first year and the 38th year (12.1 ± 9.0). They had been on COVID-19 duty for an average of 22.6 ± 16.6 days, and their average weekly working time in this task was 31.2 ± 25.1 hours. Among all participants, 2 people had a positive Coronavirus test, 19 of them were suspected of having the disease, the others had no symptoms.
STAI-S and STAI-T scores according to sociodemographic characteristics of the participants are shown in Table 1.
Table 1.
STAI-S and STAI-T scores according to sociodemographic characteristics.
| Socidemographic characteristics | N | % | STAI-SM ± SD | Statistics | STAI-TM ± SD | Statistics |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 216 | 74.2 | 50.9 ± 10.5 | t: 2.54 | 43.0 ± 7.3 | t: 2.78 |
| Male | 75 | 25.8 | 47.2 ± 12.2 | p = .01 | 40.2 ± 8.5 | p = .006 |
| Age groups | ||||||
| 18–35 | 160 | 54.9 | 48.2 ± 11.4 | Z: –3.19 | 42.8 ± 8.3 | Z: –.97 |
| 36–65 | 131 | 45.1 | 52.1 ± 10.2 | p = .001 | 41.4 ± 7.0 | p = .03 |
| Marital status | ||||||
| Married | 178 | 61.2 | 50.4 ± 11.0 | χ2: 3.45 | 42.0 ± 7.3 | χ2 :3.60 |
| Single | 97 | 33.3 | 48.9 ± 11.5 | p = .32 | 43.2 ± 8.3 | p = .30 |
| Divorced | 14 | 4.8 | 53.0 ± 8.2 | 40.1 ± 8.3 | ||
| Widow | 2 | 0.7 | 51.0 ± 5.6 | 36.0 ± 4.2 | ||
| Having a child | ||||||
| No | 143 | 49.1 | 48.6 ± 11.6 | t: –2.10 | 43.3 ± 8.3 | t: –2.09 |
| Yes | 148 | 50.8 | 51.3 ± 10.3 | p = .03 | 41.4 ± 7.0 | p = .03 |
| Household | ||||||
| Spouse and/or children | 167 | 57.4 | 50.7 ± 11.0 | F: 1.15 | 42.1 ± 7.3 | F: 1.77 |
| Parents | 53 | 18.2 | 50.8 ± 11.2 | p = .33 | 44.5 ± 8.5 | p = .13 |
| Roommate | 16 | 5.5 | 46.7 ± 11.7 | 42.8 ± 8.3 | ||
| Dormitory/hotel | 7 | 2.4 | 52.1 ± 6.5 | 41.1 ± 7.3 | ||
| Alone | 48 | 16.5 | 47.7 ± 11.2 | 40.6 ± 7.8 | ||
| Job title | ||||||
| Doctor | 139 | 47.8 | 47.7 ± 11.6 | F: 7.10 | 42,3 ± 8.5 | F: .08 |
| Nurse | 106 | 36.4 | 52.9 ± 10.1a | p = .001 | 42,3 ± 7.0 | p =.99 |
| Assistant (other) personnel | 46 | 15.8 | 50.1 ± 9.7 | 42,2 ± 6.8 | ||
| Branch | ||||||
| Related to pandemic | 100 | 36.7 | 52.2 ± 9.6b | F: 3.36 | 42.8 ± 7.1 | F: .47 |
| Assigned non-surgical | 111 | 40.6 | 48.7 ± 11.7 | p = .03 | 42.5 ± 8.0 | p = .62 |
| Assigned surgical | 62 | 22.7 | 48.7 ± 11.7 | 42.0 ± 7.8 | ||
| Experience | ||||||
| 0–5 years | 93 | 32.0 | 47.7 ± 12,3 | F: 3.27 | 42.2 ± 8.6 | F: .639 |
| 6–15 years | 104 | 35.7 | 49.5 ± 10.0 | p = .02 | 43.0 ± 7.4 | p = .59 |
| 16–25 years | 60 | 20.6 | 52.8 ± 9.7c | 42.0 ± 6.6 | ||
| >25 years | 34 | 11.7 | 52.4 ± 11.4 | 41.0 ± 7.9 | ||
| Chronic disease history | ||||||
| Yes | 68 | 23.3 | 49.9 ± 10.8 | Z: -.14 | 43.6 ± 8.5 | Z: –1.44 |
| No | 223 | 76.6 | 50.0 ± 11.1 | p = .88 | 41.9 ± 7.4 | p = .14 |
| Psychiatric disorder | ||||||
| Yes, newly after pandemic | 11 | 3.8 | 61.4 ± 12.4d | F: 5.14 | 49.4 ± 8.6d | F: 5.94 |
| Yes, in the past, now fine | 31 | 10.7 | 52.5 ± 12.2 | p = .002 | 45.4 ± 7.6 | p = .001 |
| Yes, still under treatment | 10 | 3.4 | 48.7 ± 10.2 | 39.9 ± 10.0 | ||
| Never | 239 | 82.1 | 49.2 ± 10.6 | 41.7 ± 7.3 |
Post hoc Tukey test performed. STAI-S: State Trait Anxiety Inventory-State anxiety; STAI-T: State Trait Anxiety Inventory-Trait anxiety; M ± SD: Mean ± Standard Deviation; independent samples t-test (t); Kruskal Wallis test, Chi-square (χ2); One-way ANOVA (F); Mann-Whitney U test (Z).
aNurses higher than doctors.
bHigher than assigned surgical branches.
cHigher than 0–5 years.
dHigher than who never had a psychiatric disorder and those still receiving treatment.
Women's mean state anxiety score (p = .01) and trait anxiety (p = .006) scores were significantly higher than that of men. Participants aged over 35 years had higher mean STAI-S scores (p = .001) and lower STAI-T (p = .03) scores than younger sample.
State and trait anxiety scores did not show a statistically significant difference according to marital status and household. Being a parent was associated with a higher STAI-S score (p = .03) and lower STAI-T score (p = .03).
There was a significant difference in STAI-S scores between doctors, nurses, and other healthcare workers (p = .001). The mean STAI-S score of nurses was significantly higher than the doctors (post hoc Tukey test, p = .001).
Before the outbreak, there was 273 staff working permanently in certain branches. Although the branches of workers that filled out the questionnaire were not equally distributed in number, 100 workers were in the front line branches directly related to the pandemic (Infectious Diseases, Respiratory Diseases, Emergency Medicine, Internal Medicine, Radiology, Anesthesiology and Reanimationa), 111 were from non-surgical branches temporarily assigned during the COVID-19 pandemic (Pediatrics, Cardiology, Nephrology, Hematology, Gastroenterology, Dermatology, Ophthalmology, Physical Medicine and Rehabilitation, Neurology, Psychiatry, Family Medicine, Nuclear Medicine) and 62 people were working in surgical branches (General Surgery, Orthopedics, Urology, Gynecology, Neurosurgery, Cardiovascular Surgery, Otorhinolaryngology and Plastic and Reconstructive surgery) permanently. The mean state anxiety score showed a significant difference between the branches in ANOVA test (p = .03). Workers in frontline branches had higher STAI-S scores than the other assigned surgical and non-surgical branches. The difference in the posthoc Tukey test was borderline compared to surgical branches (p = .05), but not significant compared to non-surgical branches (p = .08).
When the experience in the profession is classified as 0–5 years, 6–15 years, 16–25 years and over 25 years; The mean STAI-S score of people working between 16–25 years was higher than those working for 0–5 years (p = .02).
Eleven participants without any previous psychiatric disorder had experienced psychiatric symptoms and consulted with a mental health professional. STAI-S and STAI-T scores were higher in these individuals compared to those who never had a psychiatric disorder (For STAI-S, p = .002 and for STAI-T, p = .005) and to those who were receiving psychiatric care before pandemic (For STAI-S, p = .03 and for STAI-T, p = .02).
Correlation analysis of sociodemographic and work-related factors are shown in Table 2.
Table 2.
Correlation analysis of age, number of children and work-related factors with STAI scores.
| STAI-S | |
| r | |
| Age | .117* |
| Weekly working hour | .084 |
| Days in COVID work | .129* |
| Years in the profession | .190** |
| STAI-T | |
| Number of chidren | –.134* |
| STAI-S | .454** |
*Correlation is significant at the 0.05 level (2-tailed).
**Correlation is significant at the 0.01 level (2-tailed).
A mild positive correlation between age and STAI-S score (r = .117, p = .05) was found. There was a weak negative correlation between the number of children and the STAI-T score (r = −.124, p = .05). A statistically significant, weak correlation was found between years of active employment and STAI-S (r = .190, p = .01). There was no significant correlation between working years and STAI-T levels (r = −.27, p = .64). As the number of working days with COVID-19 patients increased, a slight increase was observed in STAI-S (r = .129, p = .05). Hours of COVID-19 work weekly and STAI-S and STAI-T scores did not correlate significantly. STAI-S and STAI-T scores correlated moderately in between (r = .458, p = .01).
STAI-S and STAI-T scores according to daily habits and other factors has been shown in Table 3.
Table 3.
The comparison of STAI-S and STAI-T scores according to working place and daily habits.
| Variables | N | % | STAI-SM ± SD | p | STAI-TM ± SD | p |
|---|---|---|---|---|---|---|
| Anxiety in COVID-19 | ||||||
| work | ||||||
| Less | 0 | 0 | 0 | .000 | 0 | .000 |
| Same amount | 48 | 18.2 | 41.9 ± 10.5 | 38.7 ± 7.9 | ||
| Increased | 238 | 81.8 | 51.6 ± 10.5 | 43.0 ± 7.5 | ||
| Anxiety in usual | ||||||
| work | ||||||
| No | 32 | 11.0 | 50.8 ± 10.5 | .09 | 40.9 ± 6.2 | .34 |
| Yes, some | 137 | 47.1 | 48.3 ± 10.8 | 41.8 ± 7.8 | ||
| Yes, so much | 101 | 34.7 | 51.5 ± 11.3 | 43.1 ± 7.8 | ||
| Full time in COVID-19 | 21 | 7.2 | 52.6 ± 11.1 | 43.4 ± 8.4 | ||
| Cigarette | ||||||
| Not user | 202 | 69.4 | 49.3 ± 11.4 | .13 | 42.7 ± 7.8 | .59 |
| Same amount | 28 | 9.6 | 49.0 ± 10.6 | 41.1 ± 5.1 | ||
| Increased | 33 | 11.3 | 52.9 ± 9.1 | 42.3 ± 7.8 | ||
| Decreased | 8 | 9.6 | 52.5 ± 10.7 | 40.5 ± 9.1 | ||
| Alcohol | ||||||
| Not user | 220 | 75.6 | 50.3 ± 10.7 | .05 | 42.4 ± 7.4 | .93 |
| Same amount | 29 | 10.0 | 46.3 ± 10.6 | 41.8 ± 7.9 | ||
| Increased | 17 | 5.8 | 54.3 ± 12.6 | 41.9 ± 10.2 | ||
| Decreased | 24 | 8.2 | 47.9 ± 12.5 | 42.1 ± 8.6 | ||
| Social media use | ||||||
| Less | 14 | 4.8 | 50.2 ± 10.5 | .39 | 40.9 ± 6.2 | .28 |
| Same amount | 107 | 36.8 | 48.6 ± 10.2 | 41.3 ± 7.4 | ||
| More | 109 | 37.5 | 51.1 ± 11.3 | 43.2 ± 8.0 | ||
| Much more | 61 | 21.0 | 50.3 ± 12.0 | 42.7 ± 7.9 | ||
| Eating | ||||||
| Less | 40 | 13.7 | 49.9 ± 11.0 | .10 | 40.45 ± 6.7 | .09 |
| Same amount | 132 | 45.4 | 48.6 ± 11.3 | 41.7 ± 7.4 | ||
| More | 92 | 31.6 | 50.9 ± 10.7 | 43.6 ± 8.5 | ||
| Much more | 27 | 9.3 | 53.9 ± 9.9 | 43.5 ± 6.8 | ||
| Sleep | ||||||
| Less | 46 | 15.8 | 48.5 ± 10.0 | .07 | 40.3 ± 6.9 | .08 |
| Same amount | 128 | 44.0 | 49.3 ± 10.8 | 42.0 ± 7.7 | ||
| More | 100 | 34.4 | 50.4 ± 11.3 | 43.1 ± 7.8 | ||
| Much more | 17 | 5.8 | 56.3 ± 12.5 | 45.3 ± 8.4 | ||
| Dreams | ||||||
| Less | 23 | 7.9 | 46.0 ± 9.7 | .06 | 40.7 ± 7.6 | .09 |
| Same amount | 123 | 42.3 | 49.0 ± 10.9 | 41.4 ± 7.2 | ||
| More | 101 | 34.7 | 50.8 ± 11.0 | 42.8 ± 7.6 | ||
| More with | 44 | 15.1 | 52.7 ± 11.5 | 44.4 ± 9.0 | ||
| nightmares |
According to their subjective evaluations, 81.8% of the participants stated that their anxiety increased while working in COVID-19 departments. Some healthcare workers continued to work in their own branches when they were not assigned in the COVID-19 departments. In their subjective assessments, 101 people (34.7%) stated that they also had increased anxiety while working in the branch they were accustomed to, 137 people (47.1%) had slightly increased anxiety and 32 (11%) stated that his/her anxiety did not increase when he worked in his/her usual branch.
The mean state anxiety score of those who increased alcohol use was higher than other alcohol usage groups but the statistical difference was at the edge (p = .05). Although the mean state anxiety scores of the participants who ate more food (p = .12) and slept too much (p = .13) than usual were higher, the difference was not statistically significant.
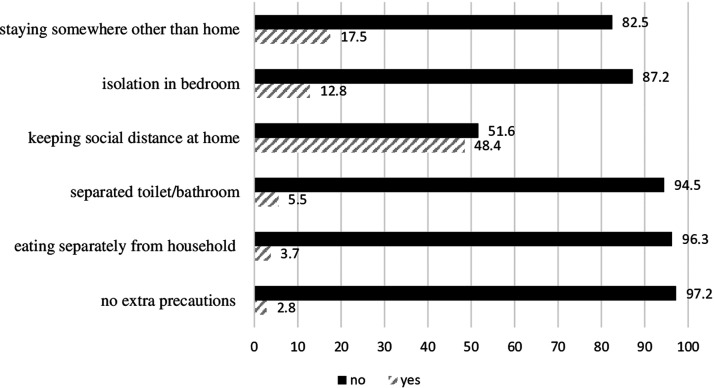
Isolation precautions taken at home have been presented in Figure 1.
Figure 1.
Isolation precautions taken at home.
The STAI-S score of those who stated that they stayed somewhere other than their home was significantly higher than those who continued to stay at their home (N = 50, p = .03). The mean STAI-S score of those who ate their meals separately from household was found to be lower than those who ate with household (N = 10, p = .001). Also the mean STAI-S (p = .10) and STAI-T (p = .40) scores were lower for healthcare workers who self-isolate themselves after bath in their bedroom. Of the participants, 29.6% (N = 86) hold on with a mask in the house, but the STAI-S (p = .63) and STAI-T (p = .10) scores were not different from those who did not wear a mask at home.
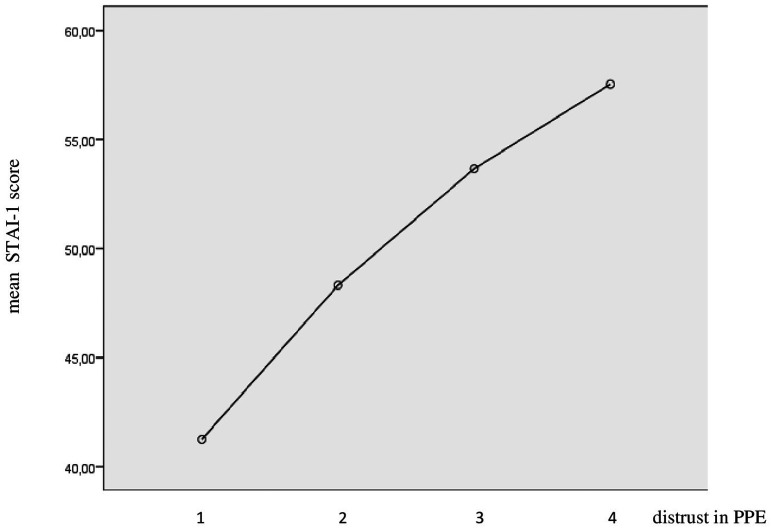
Only 2.7% (N = 8) felt completely safe while in personal protective equipment (PPE). 64% (N = 188) thought that PPE greatly reduced the virus transmission, 28.9% (N = 84) thought it did not reduce the risk of transmission enough, and 3.8% (N = 11) thought that it did not reduce the transmission at all. Those who thought that PPE did not reduce the risk of virus contamination at all had a higher mean STAI-S score than those who felt completely safe with PPE (p = .006) and those who thought it greatly reduced transmission (p = .02). The average STAI-T score of those who thought that PPEs did not reduce the risk of virus transmission was higher than those who thought it greatly reduced (p = .002). Means plot for STAI-S scores according to trust in personal protective equipment is shown in Figure 2.
Figure 2.
STAI-1 scores according to trust in personal protective equipment (PPE).
The statistical tests were not significant for the questions of training and guideline use. One-third of the participants (N = 97, 33.3%) pointed out that they were assigned to the COVID-19 department without training. In the rest percentage of those who received training and found it very useful (N = 120, 41.2%) were more than those who thought it was not very useful (N = 73, 25.2%). The guideline prepared by the Ministry of Health to standardize the approach to patients with suspected COVID-19 was found very useful by 32.3% of participants in reducing anxiety, 41.9% found it somewhat useful, 24.4% thought it was not helpful, and 1% thought the consultation of other colleagues or resources they have read themselves were more useful.
Analysis of variables that can predict state anxiety level is presented in Table 4.
Table 4.
Multiple regression analysis of STAI-S scores.
| B | SE | β | t | p | 95% CI | ||
|---|---|---|---|---|---|---|---|
| (Constant) | 40.818 | 4.683 | 8.717 | .000 | 31.598 | 50.038 | |
| Age | 2.940 | 1.538 | .132 | 1.911 | .057 | –.089 | 5.969 |
| Gender | –1.539 | 1.522 | –.061 | –1.011 | .313 | –4.535 | 1.457 |
| Having a child | 1.440 | 1.522 | .065 | . 946 | .345 | –1.557 | 4.437 |
| Lifetime psychiatric disorder | –1.418 | .534 | –.149 | –2.657 | .008 | –2.546 | –.367 |
| Job title | .515 | .245 | .129 | 2.104 | .036 | .033 | .998 |
| Branch | –1.210 | .825 | –.085 | –1.467 | .144 | –2.835 | .415 |
| Confidence in personal protective equipment | 4.983 | 1.076 | .262 | 4.630 | .000 | 2.864 | 7.102 |
F(8.233) = 849.642; p ≤ 001; Adjusted R2: 0.157.
STAI-S: State Trait Anxiety Inventory-State anxiety; B: Unstandardized Beta coefficient, SE: Standard error, β: Standardized beta coefficient, CI: Confidence Interval.
Being a nurse, having a lifetime psychiatric disorder and intrust to personal protective equipment was associated with higher STAI-S scores.
Discussion
In our study, the state anxiety levels of women, aged over 35 years, those who have children, nurses and those working in branches directly related to the pandemic were found to be higher than others. As the age of employees, years in the profession and the number of days they worked in the COVID-19 related departments increased, a slight increase was observed in the STAI-S scores. Those who thought they were not protected with personal protective equipment and those who did not stay in their own homes had higher state anxiety scores.
In the early rapid expansion phase of the SARS epidemic, similar to the current course of the COVID-19 pandemic, healthcare workers reported feelings of hypersensitivity, uncertainty, somatic and cognitive anxiety symptoms and life threats.14 During the H1N1 epidemic in 2009, more than half of the healthcare workers in a tertiary hospital in Greece reported moderately high anxiety and subsequent psychological distress.15 During epidemics, the disruption of routine clinical practice, a sense of loss of control, and the fear of subsequent healthcare becoming unstable trigger the ‘overflowing' anxiety and depression among healthcare workers.3,16
Among the healthcare professionals who participated in our study, 11 people without any previous psychiatric disorder sought professional psychological care during the pandemic. While planning where the workforce will be employed during the pandemic, only medical diseases are taken into consideration by hospital administrations. The evaluation of personnel with a known psychiatric illness or continuing psychiatric treatment will play an important role in preventing the health worker suicides reported during the pandemic.17
Similar to our results in terms of gender, studies conducted with healthcare professionals in China found anxiety scores higher in women compared to men.4,5,18 The anxiety scale we used examines the state and trait anxiety separately and can bring out a unique perspective. Women's both constant anxiety and situational anxiety about the pandemic were higher than men.
A study of doctors in Pakistan (60% working in hospitals where COVID-19 was not treated) found the fear of doctors infecting their family as high as 79.7%.19 In our study, all of the healthcare workers were working in hospitals where COVID-19 was treated, so the fear of infecting their families can be expected to be even higher.
The mean state anxiety score of those staying somewhere other than their home found to be high in our study. Providing places to stay for healthcare professionals who think they should stay away from home to protect their family seems one of the best favors for them. State anxiety scores found to be lower in people living alone, as there is no risk of infecting anyone at home. It has been accounted that the post-epidemic prevention period may take one or two years and the number of healthcare workers leaving their parents’ home and living alone may increase.20 Although people who live alone can meet their need for socialization by communicating with their relatives or friends online or by phone, determining the effects of long social isolation on mental health may be a subject of a separate study.21
The state anxiety levels of those who had children were higher than those who did not have children and there were healthcare professionals who avoided to see their children to prevent transmission of infection to their children. Especially for a person with a large family, staying away from this social support system can increase anxiety. In a study conducted with nurses working in COVID-19 pandemic in China, it was shown that having a child and work stress were factors that increase anxiety.22
During this pandemic, many healthcare professionals are employed out of their familiar branches and work in a different order from their usual duties. In our study, we observed that the branches directly related to the pandemic (Infectious Diseases, Respiratory Diseases, Emergency Medicine, Internal Medicine, Radiology, Anesthesiology and Reanimation) had higher state anxiety scores than other assigned branches. The excess amount of information to be learned about the disease and the pressure of expectations from them may have increased their anxiety levels. There is no study comparing the anxiety levels between medical branches in between but a study in Fujian, China pointed that healthcare personnel who were likely to be in contact with coronavirus pneumonia patients (pulmonary diseases, emergency services, intensive care units and infectious diseases) had more psychological disorders and were almost twice as likely to have anxiety and depression than administrative staff.23
Nurses have always played an important role in infection prevention, infection control, isolation precautions and public health. In our study, nurses were found to have higher anxiety levels than the doctors. 90.6% of the nurses were women, 67% were married and had children, 61.3% had over 15 years of experience in the profession. Nurses treating COVID-19 patients may be anxious because of their close and frequent contact with patients, their longer duration of work, and the high risk of infection. Also, most of the nurses are women, this may have affected the result, cause women report more severe symptoms of depression, anxiety, and distress.5 During the SARS epidemic, frontline nurses treating SARS patients were physically and psychologically overwhelmed while trying to provide high-quality nursing care for their patients.24
It is known that COVID-19 has a more severe course in the elderly and in people with chronic diseases.25 Psychological problems are associated with poor medication compliance and in this way can increase morbidity among elderly healthcare professionals with pre-existing medical conditions.20 Therefore, as the age of the participants and their years in the profession increase, there may be some increase in their worries.
State anxiety was higher in experienced employees than workers in the first 5 years of the profession. With increased professional experience and knowledge, seniors may have greater awareness of risks, or from the other way those in the first 5 years of the profession may see themselves more protected from COVID-19 because of their younger age and stronger immunity. Considering these issues in future research will contribute to our better understanding of the underlying factors for age-anxiety relationship.
The first case with COVID-19 in our country was recorded on 11.03.2020. Our study was conducted between 9–19 April 2020. Participants have been on a COVID-19-related task for an average of 22 days, so our study has covered the first month of the outbreak. State anxiety scores increased as the number of days worked in COVID-19 departments increased. While pandemic response arises, the unpredictability of work patterns can be immense. Healthcare professionals are trained to deal with change and stressful scenarios in the short term, but encountering these conditions over and over is unfamiliar to most of us. This poses a notable problem, especially considering how long the rise in sick people who need care will last and when the peak in new cases and deaths will be reached is uncertain.26
Another important issue was the information overload, and also incompatibility of different levels or resources. For example, in the USA there were guidelines provided by relevant specialists in each sub-specialty (eg, anesthesiology, intensive care medicine, respiratory therapy, nursing, and others), as well as guidelines developed by hospitals. However, holistic efforts for compliance were largely lacking at the system level, causing problems, confusion and frustration in teamwork.27 In our study, a single guideline use was found helpful by 74% of the employees in eliminating the concerns.
Ultimately, our findings are compatible with the results of coinciding studies about healthcare workers in Turkey. Women and nurses are the most frequently reported vulnerable groups for mental health risks.28–30 Despite the study of Elbay et al., supporting being married and being a parent as protective factors, we found that being married had no significant effect on anxiety and having a child was associated with higher anxiety.28 Hacımusalar et al. used also STAI to assess anxiety and reported that having difficulty in childcare was associated with higher anxiety.29 And like Şahin et al., we found having a lifetime psychiatric disorder and receiving psychiatric consultation during COVID-19 were associated with higher anxiety.30
A study in Pakistan found that greater exhaustion, greater family strain, and reduced feelings of protection impacted on levels of anxiety among physicians.31 Definitely, reduced protection involves the PPE. Our study found that when the trust in PPE is lower, healthcare worker anxiety is higher. How safe healthcare workers feel with PPE regimen of their hospital has been rarely investigated in the literature. It may be related with the completeness, quality and availability of PPE and risk perception of individuals.32
Healthcare professionals are just human beings. We are experiencing the same COVID-19 related fear and anxiety as everyone else. This may be the fear that we, our friends or family will get sick, and we will have to isolate or quarantine ourselves. Some of us may also experience fear of caring for patients with COVID-19 who will die. To call healthcare professionals superheroes is to give a status. While this adds value, on the other hand, it can cause additional pressure, because superheroes don't fail, give up, or get sick.9 Managing the ventilators in intensive care or providing palliative care for patients with poor pulmonary conditions due to COVID-19 may involve a sense of defeat. When a patient is at his last breath, not his relatives, but a doctor or nurse is present, and he has to say goodbye to his relatives via a video call. These can cause indirect or secondary traumatization in healthcare workers.33
This study has some limitations. The first is the small sample size. The number of non-responders is unknown due to the method. Selection bias is possible because it is unclear whether those who did not respond avoided the questions about anxiety or they were not interested in it. The second is the cross-sectional design of the study. The survey was conducted for 10 days and there was no longitudinal follow-up. The level of anxiety of healthcare workers in the first, middle and last stages of the epidemic may be different and is an issue that deserves further investigation. Third is the use of self-report scales and online application. Fourth is the absence of a control group. As employees in COVID-19 departments and those on the frontline experience more anxiety and mental distress, this was considered to be ‘a priori' and no comparisons were done with lower risk groups.4,23,26
Providing pre-work training to employees, enough resting time with a short-term, frequent shift system, meeting their critical personal needs (such as the care of an elderly family member), identifying and getting answers to psychological problems will help maintain team performance in the long term. It is useful to talk about isolation measures in the training however, there is a need to strike a balance as these ideas can increase anxiety among people who have already overworked in the hospital. Additional home arrangements and extra house cleaning can be a significant challenge after long working hours. Team leaders should emphasize the importance of personal self-care in the challenges that can be encountered with the long duration of the pandemic.34
With regular professional updates, the feeling of uncertainty and fear should be alleviated, emotional and behavioral responses to extraordinary stress should be handled with psychotherapy techniques based on stress adaptation models, psychological counseling can be provided using tele services and applications, and psychotropic drugs should be used when necessary.16
Conclusion
This bio-threat is one of the most serious global crises of our generation. In terms of anxiety, women, nurses, workers with children and people working in branches that are directly related to pandemic are vulnerable segments. It is important to understand the specific sources of anxiety and fears in healthcare professionals before moving on to psychiatric treatment, and the simplest way is to ask them.
In our country, during the peaks of COVID-19 the right to resign and all non-emergency leaves of healthcare workers was cancelled. Staff from surgical and other branches assigned to frontline. Healthcare workers had to get back to work after 7 days of rest if they caught infection. Hostels were provided by some hospitals. Public transport was free for healthcare workers in some cities. Childcare was an important issue, especially when the schools are closed and it has not been resolved yet. The care of patients needs care of providers. For the increasing psychological pressure felt by frontline healthcare personnel, psychological support and interventions to protect their mental health should be implemented immediately.
The working order of psychiatrists in each institution may differ and in hospitals where psychiatrists also work on COVID-19 wards out of their specialty, reaching them can be difficult even for healthcare personnel.34,35 Many countries shifted to telepsychiatry practice for delivery of mental health services.36 Psychiatric Association of Turkey created a telephone line and provided free telepsychiatric consultations to health workers during the first peak of pandemic in our country.37 Turkish Psychological Association, universities and other private mental health clinics had similar smaller initiatives. The Kordep telephone support project of the Ministry of Health has been put into practice which is a platform both the patients and healthcare workers can call.
At the forefront of the fight against COVID-19, there are medical personnel who pay a serious psychological cost. Governments and health institutions are responsible for ensuring the psychological well-being of the health community worldwide.
Acknowledgements
We thank Prof. Rumeysa Kazancıoğlu for her support to conduct this study.
Note
Reanimation (also, resuscitation), is a new branch of medicine. It involves the measures taken to revive a person in a state of clinical death and to restore the functions of vital organs suddenly lost or impaired as a result of accident, disease, or complications.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ebru Şahan https://orcid.org/0000-0002-1287-8166
References
- 1.Karamustafalıoğlu O, Akpınar A.Anksiyete bozuklukları. In: Karamustafalıoğlu O. (ed). Aile hekimleri için psikiyatri. İstanbul: MT Uluslararası Yayıncılık, 2010, pp.71–88. [Google Scholar]
- 2.Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, 1983. [Google Scholar]
- 3.Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020; 7: e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom 2020; 89: 242–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020; 3: e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Sinsky C.From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014; 12: 573–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stefanacci RG. Impact of COVID-19 on the quadruple aim. Popul Health Manag. Epub Ahead of Print 5 November 2020. doi.org/10.1089/pop.2020.0263 [DOI] [PubMed]
- 8.Lee SA.Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud 2020; 44: 393–401. [DOI] [PubMed] [Google Scholar]
- 9.Ornell F, Halpern SC, Kessler FHP, et al. The impact of the COVID-19 pandemic on the mental health of healthcare professionals. Cad Saude Publica 2020; 6: e00063520. [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt T, Ripp J, Trockel M.Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020; 323: 2133–2134. [DOI] [PubMed] [Google Scholar]
- 11.McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 2007; 52: 241–247. [DOI] [PubMed] [Google Scholar]
- 12.Zu ZY, Jiang MD, Xu PP, et al. Coronavirus disease 2019 (COVID-19): a perspective from China. Radiology 2020; 296: E15-E25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Öner N, Le Compte A.Durumluk sürekli anksiyete envanteri el kitabı. Istanbul: Boğaziçi Üniversitesi Yayınları, 1985. [Google Scholar]
- 14.Chong MY, Wang WC, Hsieh WC, et al. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br J Psychiatry 2004; 185: 127–133. [DOI] [PubMed] [Google Scholar]
- 15.Goulia P, Mantas C, Dimitroula D, et al. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the a/H1N1 influenza pandemic. BMC Infect Dis 2010; 10: 322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Neto MLR, Almeida HG, Esmeraldo JDA, et al. When health professionals look death in the eye: the mental health of professionals who deal daily with the 2019 coronavirus outbreak. Psychiatry Res 2020; 288: 112972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thakur V, Jain A.COVID 2019-suicides: a global psychological pandemic. Brain Behav Immun 2020; 88: 952–953. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.Huang JZ, Han MF, Luo TD, et al. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2020; 38: E001. [DOI] [PubMed] [Google Scholar]
- 19.Urooj U, Ansari A, Siraj A, et al. Expectations, fears and perceptions of doctors during covid-19 pandemic. Pak J Med Sci 2020; 36: S37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science 2020; 368: 860–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okruszek L, Aniszewska-Stańczuk A, Piejka A, et al. Safe but lonely? Loneliness, mental health symptoms and COVID-19. Front Psychol 2020; 11: 579181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID‐19 epidemic. J Nurs Manag 2020; 28: 1002–1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu W, Wang H, Lin Y, et al. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res 2020; 288: 112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shih FJ, Gau ML, Kao CC, et al. Dying and caring on the edge: Taiwan's surviving nurses' reflections on taking care of patients with severe acute respiratory syndrome. Appl Nurs Res 2007; 20: 171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.CDC COVID-19 Response Team et al. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. Morb Mortal Wkly Rep 2020; 69: 343–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song X, Ni C, Cai W, et al. Psychological status of health care workers during the outbreak of coronavirus disease in China: a cross-sectional study. Research Square 2020; doi.org/10.21203/rs.3.rs-18641/v1. [Google Scholar]
- 27.Sasangohar F, Jones SL, Masud FN, et al. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg 2020; 131: 106–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Elbay RY, Kurtulmuş A, Arpacıoğlu S, et al. Depression, anxiety, stress levels of physicians and associated factors in covid-19 pandemics. Psychiatry Res 2020; 290: 113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hacimusalar Y, Kahve AC, Yasar AB, et al. Anxiety and hopelessness levels in COVID-19 pandemic: a comparative study of healthcare professionals and other community sample in Turkey. J Psychiatr Res 2020; 129: 181–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Şahin MK, Aker S, Şahin G, Karabekiroğlu A.Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J Community Health 2020; 45: 1168–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mahmood QK, Jafree SR, Jalil A, et al. Anxiety amongst physicians during COVID-19: cross-sectional study in Pakistan. BMC Public Health 2021; 21: 118–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fix GM, Reisinger HS, Etchin A, et al. Health care workers' perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control 2019; 47: 1162–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Z, Ge J, Yang M, et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav Immun 2020; 88: 916–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wingfield T, Taegtmeyer M. Healthcare workers and coronavirus: behind the stiff upper lip we are highly vulnerable, https://theconversation.com/uk (2020, accessed 12 June 2020).
- 35.Tsamakis K, Rizos E, Manolis AJ, et al. [Comment] COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med 2020; 19: 3451–3453. [ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shoib S, Gupta AK, Ahmad W, et al. Mental health professionals as ‘silent frontline healthcare workers’: perspectives from three South Asian countries. Open J Psychiatry Allied Sci 2020; 21: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Capraz N, Erim BR, Kucukparlak I, et al. A specific mental health intervention for healthcare workers in Turkey. Asian J Psychiatr 2020; 54: 102315. [DOI] [PMC free article] [PubMed] [Google Scholar]