Abstract
Background
Smoking tobacco is the most preventable cause of gastrointestinal (GI) cancer disease in Germany. The more and the longer you smoke, the higher your risk of GI cancer. About 28% of 18–64 year-old Germans are current smokers; in addition, 11% of the population is regularly exposed to secondhand tobacco smoke.
Summary
Tobacco use is causally associated with esophageal, gastric, pancreatic, biliary, hepatocellular, colorectal, and anal cancers. Combining smoking with alcohol use, excess body weight, diabetes, or chronic infections synergistically enhances GI cancer risk. Smoking cessation effectively reduces tobacco-associated GI cancer risk.
Key Messages
Smokers should be encouraged to stop smoking tobacco and join programs of risk-adaptive cancer screening.
Keywords: Colorectal cancer, Anal cancer, Pancreatic cancer, Esophageal cancer, Gastric cancer, Hepatocellular cancer, Biliary cancer, Neoplasm, Tumor, Carcinoma, Tobacco, Smoking
Introduction
Cancer is the major cause of death among adults aged 35–70 years in high-income countries. Among 35–70 year olds of high-income countries, deaths from cancer outnumber those from cardiovascular disease more than twice [1]. In many industrialized countries, lifetime cancer risk of the average population has risen to 35% and higher.
Smoking is the most important and preventable cause of cancer deaths. Tobacco acts on multiple stages of carcinogenesis; it delivers carcinogens directly to tissues, causes irritation and inflammation, and interferes with the body's natural protective barriers and defense mechanisms. Up to 30% of cancer deaths both in the USA and in Europe are due to tobacco use [2, 3, 4]. Tobacco smoking is causally associated with esophageal, gastric, pancreatic, biliary, hepatocellular, colorectal, and anal cancers. Depending on sex and site 8–52% of those malignancies are caused by smoking [3, 4]. In Korea, 51% of esophageal cancer deaths, 19% of liver, 21% of stomach, and 15% of pancreas cancer deaths are attributable to tobacco smoking [5].
A low-risk lifestyle can reduce overall gastrointestinal (GI) cancer risk by about 50% [6]. Stopping the use of tobacco yields remarkable health benefits. In particular smoking cessation reduces tobacco-associated excess GI cancer risk [7].
About 28% of 18–64 year-old Germans are current smokers. In addition, 11% of the population IS regularly exposed to secondhand tobacco smoke. Another 23–27% of German adults are former smokers [8, 9, 10]. Thus, about half of the population is still at risk of tobacco-associated cancers. Therefore risk-adaptive cancer screening strategies are being evaluated not only for lung cancer but also for the detection of early asymptomatic GI cancers [11, 12]. Special attention should be paid to synergistic carcinogenic effects of coincident risk factors such as tobacco plus alcohol. Patients exposed to various, synergistically acting carcinogens can have an up to 100-fold increased risk for certain GI cancers [13, 14, 15].
Esophageal Squamous Cell Cancer
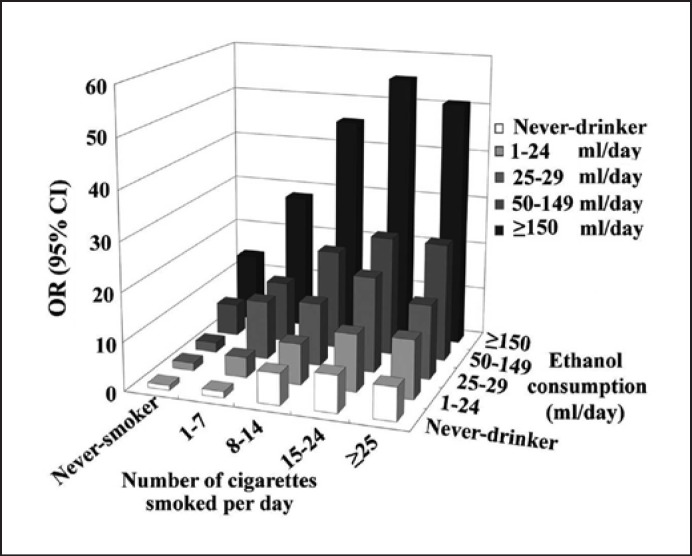
The use of tobacco, including cigarettes, cigars, pipes, and chewing tobacco, is a major risk factor for esophageal squamous cell cancer (ESCC). The more and the longer a person smokes, the higher the ESCC risk. When tobacco use goes along with alcohol consumption, ESCC risk rises synergistically [15, 16], see (Fig. 1). The majority of drinkers do smoke. Smoking cessation time-dependently decreases ESCC risk, particularly in Western populations [17].
Fig. 1.
Combined exposure to both cigarette smoking and alcohol use and risk of developing ESCC. Alcohol (ethanol) consumption is given in milliliters of pure alcohol drunk per day. The material has been reproduced from [15]. OR, odds ratio; CI, confidence interval.
Persons exposed to synergistically acting carcinogens for more than 15–20 years may consider going for a screening esophagoscopy as to detect precancerous lesions and asymptomatic early ESCC. Male smokers with risky alcohol use should have access to screening esophagogastroscopy at the age of 50 years. Former smokers surviving a lung or head and neck cancer should be surveilled endoscopically for a second primary ESCC [16]. Risk prediction models for esophageal cancer among the general population and biomarkers for early detection are being evaluated [18, 19].
Gastric Cancer
Gastric cancer (GC) is the third leading cause of cancer deaths worldwide. Smoking tobacco is the most important behavioral risk factor for GC. Several studies have examined the relationship between tobacco use and GC. A meta-analysis estimated that the risk was increased about 1.5-fold and was higher in men. Risks are somewhat higher for cardia than noncardia GC. When tobacco smoking goes along with (CagA-positive) Helicobacter pylori infection, the risk for GC can increase synergistically [20, 21]. About 18% of GC cases and 21% of GC deaths may be attributed to smoking [3, 4]. Important to note, GC risk decreases with increasing time since stopping cigarette smoking and becomes similar to that of never smokers 10 years after quitting [22].
In addition, H. pylori infection, family history, diabetes, dietary (nitroso compounds and a high-salt diet with few vegetables), or lifestyle factors (excess body weight, physical inactivity, and alcohol use) as well as chronic atrophic gastritis are important risk factors of GC. All these risk factors should be taken into account when counseling a smoker whether and at what age to go for a screening esophagogastroduodenoscopy. The Korean National Cancer Screening Program has provided strong evidence that screening gastroscopy offered to the general population − starting at the age of 40 years − effectively reduces both GC and overall mortality [23]. Although early-detection screening is routine in Korea, Japan, and certain areas of China [23, 24, 25], in Western countries, screening esophagogastroscopy is restricted to persons at high risk.
Smokers who show 4 or more risk factors of esophageal and/or GC are at high risk of upper GI cancer and should be advised to go for a screening esophagogastroscopy at the age of 50 years. The aim is to detect early esophageal cancer, early esophagogastric junction adenocarcinoma, early GC, or precancerous lesions. Risk factors of GC are H. pylori infection, dietary (nitroso compounds and high-salt diet with few vegetables), and lifestyle factors (excess body weight, tobacco smoking, and risky alcohol use), family history, age, male sex, diabetes, and autoimmune gastritis/pernicious anemia. Well-known risk factors of (either squamous or glandular cell) esophageal cancer comprise tobacco use, risky alcohol intake, family history, (previous) head and neck cancer, age, male sex, excess body weight, Barrett's esophagus, reflux disease, and diabetes.
Hepatocellular Cancer
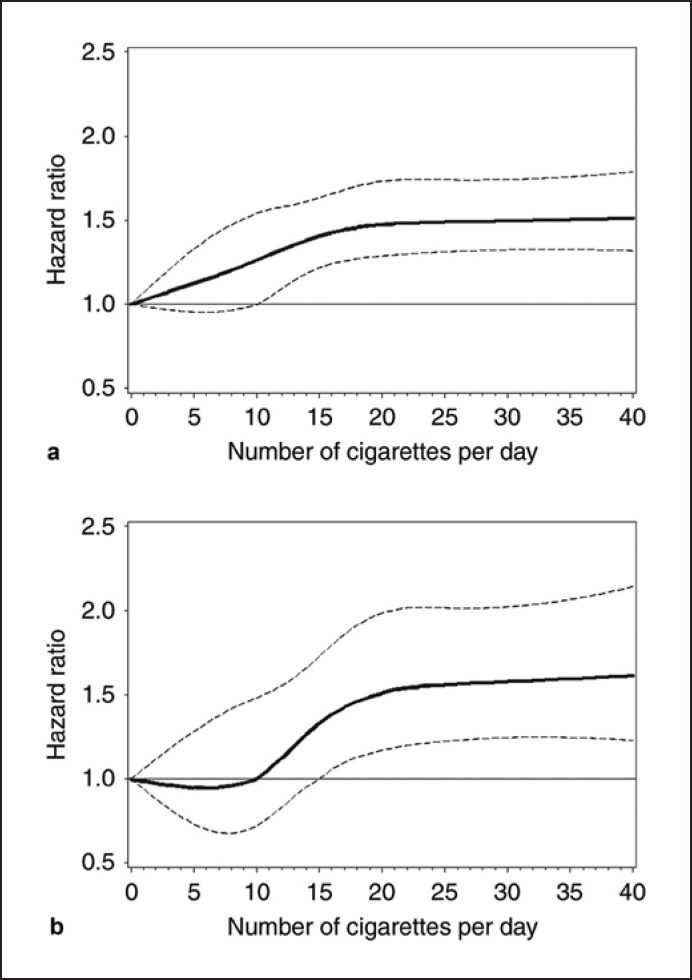
A nested case-control study in Europe showed that smoking tobacco contributed to almost half of all hepatocellular carcinomas (47.6%), whereas 13.2% and 20.9% were attributable to chronic HBV and HCV infection, respectively [26]. Tobacco use increases hepatocellular cancer (HCC) risk dose-dependently (see Fig. 2a). Various carcinogens can interact synergistically to cause HCC. The combination of tobacco smoking with excess body weight, alcohol use, or chronic hepatitis B or C infection can lead to overadditive HCC risks [27, 28, 29, 30]. Thus, obese smokers with concomitant diabetes and chronic hepatitis B or C infection are at a 100-fold increased risk of HCC [14]. Patients at high risk should go for liver ultrasound every 6 months as to detect early HCC. Important to note, HCC risk decreases after quitting smoking [7]. About 22% of liver cancer deaths in the USA could be prevented by not smoking [3].
Fig. 2.
Cubic spline graph of the multivariate-adjusted HR (represented by the solid line) and 95% CI (represented by the dotted lines) for the association between smoking intensity and HCC (a) and ICC risk (b) in the Liver Cancer Pooling Project (knots: 0.5, 10, 15, and 25; referent: 0). This material has been reproduced from [30]. HCC, hepatocellular cancer; ICC, intrahepatic cholangiocarcinoma.
Biliary Tract Cancer
Smokers have increased risk of intrahepatic (hazard ratio [HR] = 2.15; 95% confidence interval [CI] = 1.15–4.00, in case of >40 cigarettes/day) and extrahepatic cholangiocarinoma (HR = 1.69; 95% CI = 1.34–2.13) compared with nonsmokers. While smoking tobacco is associated with both intrahepatic (see Fig. 2b) and extrahepatic bile ducts as well as ampulla of Vater cancers (HR = 2.22; 95% CI = 1.69–2.92), a causal link with gallbladder cancer remains ambiguous [31].
Pancreatic Cancer
Cigarette smoking increases the risk for pancreatic cancer (PC), and the estimated population-attributable fraction of PC deaths to tobacco smoking is 11–32 percent [3, 32]. In multiple cohort and case-control studies, the relative risk for developing PC among smokers was about twice. PC risk increases up to 5-fold with the amount of cigarettes consumed [33]. Important to note, excess PC risk decreases with smoking cessation [7, 32]. It has been estimated that cessation of smoking could eliminate approximately 25 percent of PC cancer deaths in the USA.
Especially for people who have other risk factors like a family history of PC, risky alcohol use, excess body weight, chronic pancreatitis, or diabetes, it is crucial to quit smoking. There are synergistic interactions of tobacco smoking and alcohol use on the risk of PC [13]. Special attention should be paid to the smoking and drinking habits of young adults [34, 35].
Pancreatic adenocarcinoma has shown some of the most troubling signs of increase among young US adults. From 1995 to 2014, the average annual percent change in PC incidence increased with decreasing age from 0.77% (95% CI: 0.57–0.98) for the ages of 45–49 years to 2.47% (1.77–3.8) for the ages of 30–34 years and 4.34% (3.19–5.50) for the ages of 25–29 years [36]. Many experts blame the excess body weight epidemic, while others refer to altered intestinal microbiota, physical inactivity, diabetes mellitus, poor diet, risky alcohol use, and sedentary lifestyle. To what extent the recent smoking and drinking habits of young adults possibly contribute to the observed epidemiological changes still need to be investigated in more detail.
In the average population, there are to date no effective means available for the early detection of asymptomatic early-stage pancreatic adenocarcinoma. For the time being, not smoking and keeping a normal weight are the best options to significantly reduce the burden of PC deaths.
Colorectal Cancer
Cigarette smoking has been associated with increased incidence and mortality from colorectal cancer (CRC). A meta-analysis of 106 observational studies estimated that the risk of developing CRC was increased among cigarette smokers compared with those who never smoked (HR = 1.18, 95% CI = 1.11–1.25). Ever smoking explains about 11% of the CRC burden. The risk of dying from CRC is increased among smokers [37]. CRC risk factor attribution varies by the anatomic site. Thus, history of smoking is associated with left-sided CRC in a positive dose-response relationship [38, 39].
Ever and current smoking goes along with higher risk for certain molecular subtypes of CRC, especially with MSI-high, BRAF-mut, KRAS-wt, and CIMP-high CRC. In addition, tobacco use is associated with higher risk of CRC developing via the traditional or the serrated pathways [40].
Not only smoking but also age, sex, family history, risky alcohol use, diabetes, excess body weight, physical inactivity, poor diet, and ulcerative colitis are risk factors for sporadic CRC and have to be considered in risk-adaptive CRC screening strategies. Studies and models evaluating risk-adapted screening are still rare but suggest that risk-adapted CRC screening is more effective and efficient than conventional screening [11, 12].
Anal Cancer
Smoking increases the risk of anal cancer. The higher a person's pack-year history of smoking, the higher their risk of developing anal cancer. People who currently smoke are more likely to have cancer of the anus compared with people who do not smoke or have quit smoking [41]. Stopping tobacco use reduces the excess risk of developing anal cancer.
Preventive Oncology
A low-risk lifestyle can reduce GI cancer risk by as much as 50% [6]. Therefore, we should pursue a healthy lifestyle that includes following a prudent diet and avoiding excess body weight, pursuing an active exercise program, minimizing alcohol intake, and refraining from smoking tobacco.
It can be hard to quit smoking, but the chances of succeeding are drastically increased with the right support [42, 43, 44]. In several countries, there are comprehensive tobacco cessation programs that use recognized and evidence-based cessation aids. In Ireland, smokers are twice as likely to succeed in ending tobacco addiction with the help of national tobacco cessation programs and 4 times more likely with a combination of cessation programs and medication. Ireland now has more quitters than smokers [42]. The tobacco control measures implemented in Denmark, Norway, Sweden, and Finland have succeeded in lowering the percentage of daily smokers by about 50% [43]. As tobacco use is the most preventable cause of cancer deaths, effective tobacco control does reduce the burden of GI cancer significantly.
Conflict of Interest Statement
The author has no conflicts of interest to declare.
Funding Sources
This work was not funded.
Author Contributions
H.S. designed and wrote the manuscript.
References
- 1.Dagenais GR, Leong DP, Rangarajan S, Lanas F, Lopez-Jaramillo P, Gupta R, et al. Variations in common diseases, hospital admissions, and deaths in middle-aged adults in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2020;395((10226)):785–94. doi: 10.1016/S0140-6736(19)32007-0. [DOI] [PubMed] [Google Scholar]
- 2.Henley SJ, Thomas CC, Sharapova SR, Momin B, Massetti GM, Winn DM, et al. Vital signs: disparities in tobacco-related cancer incidence and mortality − United States, 2004–2013. MMWR Morb Mortal Wkly Rep. 2016;65:1212. doi: 10.15585/mmwr.mm6544a3. [DOI] [PubMed] [Google Scholar]
- 3.Islami F, Goding Sauer A, Miller KD, Siegel RL, Fedewa SA, Jacobs EJ, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018 Jan;68((1)):31–54. doi: 10.3322/caac.21440. [DOI] [PubMed] [Google Scholar]
- 4.Agudo A, Bonet C, Travier N, González CA, Vineis P, Bueno-de-Mesquita HB, et al. Impact of cigarette smoking on cancer risk in the European prospective investigation into cancer and nutrition study. J Clin Oncol. 2012 Dec 20;30((36)):4550–7. doi: 10.1200/JCO.2011.41.0183. [DOI] [PubMed] [Google Scholar]
- 5.Park S, Jee SH, Shin HR, Park EH, Shin A, Jung KW, et al. Attributable fraction of tobacco smoking on cancer using population-based nationwide cancer incidence and mortality data in Korea. BMC Cancer. 2014;14:406. doi: 10.1186/1471-2407-14-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Y, Li Y, Giovannucci E. Potential impact of time trend of lifestyle risk factors on burden of major gastrointestinal cancers in China. Gastroenterology. 2021 Dec;161((6)):1830–e8. doi: 10.1053/j.gastro.2021.08.006. [DOI] [PubMed] [Google Scholar]
- 7. Available from: https://www.cancer.org/healthy/stay-away-from-tobacco/benefits-of-quitting-smoking-over-time.html (accessed February 4, 2022)
- 8. Available from: https://www.dhs.de/suechte/tabak/zahlen-daten-fakten (accessed February 4, 2022)
- 9.Seitz NN, John L, Atzendorf J, Rauschert C, Kraus L. Kurzbericht Epidemiologischer Suchtsurvey 2018. Tabellenband: Tabakkonsum und Hinweise auf Konsumabhängigkeit nach Geschlecht und Alter im Jahr 2018. München: IFT Institut für Therapieforschung; 2019. [Google Scholar]
- 10.Kuntz B, Starker A. Deutsche Hauptstelle für Suchtfragen (Hrsg.): DHS Jahrbuch Sucht 2021. Lengerich: Pabst Science Publishers; 2021. Tabak − Zahlen und Fakten zum Konsum. [Google Scholar]
- 11.Chen H, Lu M, Liu C, Zou S, Du L, Liao X, et al. Comparative evaluation of participation and diagnostic yield of colonoscopy versus fecal immunochemical test versus risk-adapted screening in colorectal cancer screening: interim analysis of a multicenter randomized controlled trial (TARGET-C) Am J Gastroenterol. 2020 Aug;115((8)):1264–74. doi: 10.14309/ajg.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 12.Wang K, Ma W, Wu K, Ogino S, Giovannucci EL, Chan AT, et al. Long-term colorectal cancer incidence and mortality after colonoscopy screening according to individuals' risk profiles. J Natl Cancer Inst. 2021 Sep 4;113((9)):1177–85. doi: 10.1093/jnci/djab041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.La Torre G, Sferrazza A, Gualano MR, de Waure C, Clemente G, De Rose AM, et al. Investigating the synergistic interaction of diabetes, tobacco smoking, alcohol consumption, and hypercholesterolemia on the risk of pancreatic cancer: a case-control study in Italy. Biomed Res Int. 2014;2014:481019. doi: 10.1155/2014/481019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen CL, Yang HI, Yang WS, Liu CJ, Chen PJ, You SL, et al. Metabolic factors and risk of hepatocellular carcinoma by chronic hepatitis B/C infection: a follow-up study in Taiwan. Gastroenterology. 2008 Jul;135((1)):111–21. doi: 10.1053/j.gastro.2008.03.073. [DOI] [PubMed] [Google Scholar]
- 15.Peng Q, Chen H, Huo JR. Alcohol consumption and corresponding factors: a novel perspective on the risk factors of esophageal cancer. Oncol Lett. 2016;11:3231–9. doi: 10.3892/ol.2016.4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scherübl H, Cataldegirmen G, Eick J, Ring W, Schwertner C, Steinberg J, et al. Field cancerization of the upper aerodigestive tract: screening for second primary esophageal cancers in cancer survivors. EMJ Oncol. 2015;3((1)):21–8. [Google Scholar]
- 17.Wang QL, Xie SH, Li WT, Lagergren J. Smoking cessation and risk of esophageal cancer by histological type: systematic review and meta-analysis. J Natl Cancer Inst. 2017 Dec;109((12)):djx115. doi: 10.1093/jnci/djx115. [DOI] [PubMed] [Google Scholar]
- 18.Chen R, Zheng R, Zhou J, Li M, Shao D, Li X, et al. Risk prediction model for esophageal cancer among general population: a systematic review. Front Public Health. 2021 Dec 1;9:680967. doi: 10.3389/fpubh.2021.680967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chu LY, Peng YH, Weng XF, Xie JJ, Xu YW. Blood-based biomarkers for early detection of esophageal squamous cell carcinoma. World J Gastroenterol. 2020;26((15)):1708–25. doi: 10.3748/wjg.v26.i15.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang XQ, Yan H, Terry PD, Wang JS, Cheng L, Wu WA, et al. Interactions between CagA and smoking in gastric cancer. World J Gastroenterol. 2011 Jul 28;17((28)):3330–4. doi: 10.3748/wjg.v17.i28.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brenner H, Arndt V, Bode G, Stegmaier C, Ziegler H, Stümer T. Risk of gastric cancer among smokers infected with Helicobacter pylori. Int J Cancer. 2002 Mar 20;98((3)):446–9. doi: 10.1002/ijc.10201. [DOI] [PubMed] [Google Scholar]
- 22.Praud D, Rota M, Pelucchi C, Bertuccio P, Rosso T, Galeone C, et al. Cigarette smoking and gastric cancer in the Stomach Cancer Pooling (StoP) project. Eur J Cancer Prev. 2018 Mar;27((2)):124–33. doi: 10.1097/CEJ.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 23.Jun JK, Choi KS, Lee HY, Suh M, Park B, Song SH, et al. Effectiveness of the Korean national cancer screening program in reducing gastric cancer mortality. Gastroenterology. 2017;152((6)):1319–28.e7. doi: 10.1053/j.gastro.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 24.Huang HL, Leung CY, Saito E, Katanoda K, Hur C, Kong CY, et al. Effect and cost-effectiveness of national gastric cancer screening in Japan: a microsimulation modeling study. BMC Med. 2020 Sep 14;18((1)):257. doi: 10.1186/s12916-020-01729-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen R, Liu Y, Song G, Li B, Zhao D, Hua Z, et al. Effectiveness of one-time endoscopic screening programme in prevention of upper gastrointestinal cancer in China: a multicentre population-based cohort study. Gut. 2021 Feb;70((2)):251–60. doi: 10.1136/gutjnl-2019-320200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trichopoulos D, Bamia C, Lagiou P, Fedirko V, Trepo E, Jenab M, et al. Hepatocellular carcinoma risk factors and disease burden in a European cohort: a nested case-control study. J Natl Cancer Inst. 2011 Nov 16;103((22)):1686–95. doi: 10.1093/jnci/djr395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meyer J, Rohrmann S, Bopp M, Faeh D, Swiss National Cohort Study Group Impact of smoking and excess body weight on overall and site-specific cancer mortality risk. Cancer Epidemiol Biomarkers Prev. 2015;24((10)):1516–22. doi: 10.1158/1055-9965.EPI-15-0415. [DOI] [PubMed] [Google Scholar]
- 28.Matsuura T, Ohfuji S, Enomoto M, Tamori A, Kubo S, Kioka K, et al. Risk factors for hepatocellular carcinoma in treated chronic hepatitis C patients-relationship to smoking and alcohol. JGH Open. 2020 Apr 16;4((5)):867–75. doi: 10.1002/jgh3.12331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. Alcohol, tobacco and obesity are synergistic risk factors for hepatocellular carcinoma. J Hepatol. 2005 Feb;42((2)):218–24. doi: 10.1016/j.jhep.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Petrick JL, Campbell PT, Koshiol J, Thistle JE, Andreotti G, Beane-Freeman LE, et al. Tobacco, alcohol use and risk of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: the liver cancer pooling project. Br J Cancer. 2018;118:1005–12. doi: 10.1038/s41416-018-0007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGee EE, Jackson SS, Petrick JL, Van Dyke AL, Adami HO, Albanes D, et al. Smoking, alcohol, and biliary tract cancer risk: a pooling project of 26 prospective studies. J Natl Cancer Inst. 2019 Dec;111((12)):1263–78. doi: 10.1093/jnci/djz103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Molina-Montes E, Van Hoogstraten L, Gomez-Rubio P, Löhr M, Sharp L, Molero X, et al. Pancreatic cancer risk in relation to lifetime smoking patterns, tobacco type, and dose-response relationships. Cancer Epidemiol Biomarkers Prev. 2020 May;29((5)):1009–18. doi: 10.1158/1055-9965.EPI-19-1027. [DOI] [PubMed] [Google Scholar]
- 33.Larsson SC, Permert J, Håkansson N, Näslund I, Bergkvist L, Wolk A. Overall obesity, abdominal adiposity, diabetes and cigarette smoking in relation to the risk of pancreatic cancer in two Swedish population-based cohorts. Br J Cancer. 2005 Nov 28;93((11)):1310–5. doi: 10.1038/sj.bjc.6602868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barrington-Trimis JL, Braymiller JL, Unger JB, McConnell R, Stokes A, Leventhal AM, et al. Trends in the age of cigarette smoking initiation among young adults in the US from 2002 to 2018. JAMA Netw Open. 2020;3((10)):e2019022. doi: 10.1001/jamanetworkopen.2020.19022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017 Sep;74((9)):911–23. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sung H, Siegel R, Rosenberg P, Jemal A. Emerging cancer trends among young adults in the USA: analysis of a populationbased cancer registry. Lancet Public Health. 2019;4:e137–47. doi: 10.1016/S2468-2667(18)30267-6. [DOI] [PubMed] [Google Scholar]
- 37.Vajdic CM, MacInnis RJ, Canfell K, Hull P, Arriaga ME, Hirani V, et al. The future colorectal cancer burden attributable to modifiable behaviors: a pooled cohort study. JNCI Cancer Spectr. 2018 July;2((3)):pky033. doi: 10.1093/jncics/pky033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Demb J, Earles A, Martínez ME, Bustamante R, Bryant AK, Murphy JD, et al. Risk factors for colorectal cancer significantly vary by anatomic site. BMJ Open Gastroenterol. 2019 Aug 24;6((1)):e000313. doi: 10.1136/bmjgast-2019-000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang LP, Wang ZX, Zhang R, Zhou N, Wang AM, Liang W, et al. Association between cigarette smoking and colorectal cancer sidedness: a multi-center big-data platform-based analysis. J Transl Med. 2021 Apr 15;19((1)):150. doi: 10.1186/s12967-021-02815-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Amitay EL, Carr PR, Jansen L, Roth W, Alwers E, Herpel E, et al. Smoking, alcohol consumption and colorectal cancer risk by molecular pathological subtypes and pathways. Br J Cancer. 2020;122:1604–10. doi: 10.1038/s41416-020-0803-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Umutoni V, Schabath MB, Nyitray AG, Wilkin T, Villa L, Lazcano-Ponce E, et al. The association between smoking and anal human papillomavirus in the HPV infection in Men Study. medRxiv. 2021 doi: 10.1158/1055-9965.EPI-21-1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Available from: https://www.euro.who.int/en/countries/ireland/news2/news/2021/5/ireland-leads-the-way-on-tobacco-cessation-programmes (accessed February 4, 2022)
- 43. Available from: https://nordicwelfare.org/wp-content/uploads/2018/03/eng-180307_lankar.pdf (accessed February 4, 2022)
- 44. Available from: https://www.aerzteblatt.de/archiv/221166/Aerztliche-Tabakentwoehnung-Wirksamkeit-und-Potenziale (accessed February 4, 2022)