Abstract
Introduction
The aim of this study was to evaluate the benefit and tolerability of two dosages of a proprietary flaxseed mucilage (IQP-LU-104) in reducing body weight in overweight and moderately obese individuals.
Methods
In a double-blind, randomized, placebo-controlled, bi-center trial, 108 participants (body mass index [BMI] 25–<35 kg/m<sup>2</sup>) were randomly allocated to receive either IQP-LU-104 high dose (104HD), IQP-LU-104 low dose (104LD), or placebo. Participants were instructed to consume 1 sachet of the investigational product (containing IQP-LU-104 or matching placebo) before or with main meals twice daily and to follow a balanced but hypocaloric diet (20% reduction of individual's daily energy requirements) for 12 weeks. At week 0 (baseline), and weeks 4, 8, and 12 of the intervention periods, the participants' body weight, BMI, body fat composition, and waist and hip circumferences were measured. Blood samples were collected for safety assessment at screening visit (week −2) and at the end of the study. Adverse events were assessed by the investigators through interviewing the participants and were recorded at every visit post screening.
Results
At the end of the 12-week study, body weight reduction was greater in the 104HD group (4.96 ± 1.89 kg, p < 0.001 vs. placebo) and 104LD group (3.70 ± 2.57 kg, p < 0.001 vs. placebo) compared to the placebo group (1.33 ± 2.05 kg). 68% and 46% of participants in the 104HD group (p < 0.001 vs. placebo) and 104LD group (p = 0.002 vs. placebo), respectively, experienced at least 5% weight loss, compared to 9% of participants in the placebo group. Significant decreases in waist and hip circumferences were observed in both the 104HD and 104LD groups compared to the placebo group (each p < 0.001). 104HD group had significantly higher reduction in body fat mass (4.25 ± 5.86 kg) than the placebo group (1.06 ± 3.20 kg) (p = 0.002). Respiratory tract infections and gastrointestinal symptoms were the main adverse events reported and none of the adverse events were related to the intake of IQP-LU-104.
Conclusion
Results demonstrated IQP-LU-104 is safe and efficacious in body weight reduction at both dosages in overweight and moderately obese individuals.
Keywords: Fiber, Obesity, Overweight, Weight loss, Fat
Introduction
The Global Burden Disease Study showed that obesity prevalence doubled in 73 countries between 1980 and 2015, and by 2030, nearly 1 in 2 adults (48.9%) in the USA is predicted to be obese [1, 2]. Obesity, defined as the excess fat accumulation that increases risk to health, is associated with increased risk of chronic diseases including type 2 diabetes, hypertension, and cardiovascular diseases [3, 4]. A weight loss of 5–10% of body weight is the recommended treatment target and a realistic goal for obese patients. This modest reduction in weight is sufficient to reduce most comorbidities' risk significantly [5, 6].
Flaxseed, or linseed (Linum usitatissimum L.), is the seed from the flax plant. It has been cultivated since 5000 BC and is native to the region extending from the eastern Mediterranean to India [7]. The average nutritional composition reported for commercial flaxseed includes 41% fat, 20% protein, 28% total dietary fiber, 7.7% moisture, and 3.4% ash [8]. Health benefits of flaxseed had been researched in various areas including cardiovascular functions [9], gastrointestinal health [10], brain development, immunity, as well as hormonal status in menopausal women [11, 12]. Flaxseed contains both soluble and insoluble fibers in the ratio of 20:80 and 40:60 [7] and the fibers are non-digestible in the small intestine [13]. Cellulose and lignin are the major components in the insoluble fiber fraction, whereas the soluble fiber fraction includes mucilage gums [14]. Flaxseed mucilage consists mainly of water-soluble polysaccharide and makes up about 3–8% of the seed weight [15, 16].
Flaxseed mucilage forms viscous gel when mixed in water and exhibits unique functional properties such as swelling power, foaming capacity, emulsifying activity, as well as fat absorption capacity [13, 15, 17]. The mucilage has large water binding capacity of about 1,600–3,000 g of water/100 g of solids [18], and the hulls containing mucilage has fat absorption capacity of about 1.8 g/g [17]. In food or pharmaceutical applications, mucilage or gums are used as thickening, disintegrating, suspending, stabilizing, and emulsifying agents [19].
The health benefits of flaxseed mucilage had gained interest and have been researched in recent decades. Fibers from flaxseed were found to be associated with body weight regulation via hunger suppression followed by diminished nutrient absorption [7]. The fiber absorbs large quantities of water, swells, and increases stomach distension which mechanically triggers the sensation of fullness or satiety [17]. Soluble fibers from flaxseed mucilage increase the viscosity of intestinal contents, prolong absorption rate of nutrients (e.g., glucose), delay gastric emptying, decrease fat digestibility, and lower blood glucose level [20, 21]. It was suggested that the degree of health benefits (e.g., cholesterol lowering, improved glycemic control, satiety, weight loss) is proportional to the viscosity of the gelling fiber [22].
Meta-analysis of 45 randomized placebo-controlled trials showed that consumption of whole flaxseed, possibly due to high fiber content had led to significant reduction in body weight, BMI, and waist circumference [23]. It was suggested that individual component in flaxseed has greater health potential than the whole flaxseed [24]. Findings from previous research showed the potential of flaxseed mucilage in combating obesity [17, 20, 23, 24]; however, clinical evidence of flaxseed mucilage, especially at a lower dose compared to the whole flaxseed, has not yet been established.
The potential of flaxseed mucilage in weight management is promising, and to the best of our knowledge clinical evidence on weight loss effect of flaxseed mucilage was not available. Thus, in this study, we aimed to determine the efficacy and tolerability of IQP-LU-104, a proprietary flaxseed mucilage composition, in reducing body weight among the overweight and moderately obese populations.
Materials and Methods
Study Design and Participants
The study was designed as a randomized, double-blind, placebo-controlled, three-armed parallel group trial and was conducted at two investigator sites in Berlin, Germany, from March to November 2019. The 14 weeks' study duration consisted of 2 weeks of run-in phase followed by 12 weeks of intervention phase. Individuals were recruited mainly through advertisements in the local press, database of the recruiting center, and on online platforms.
One hundred and eight male and female individuals aged 18–65 years who fulfilled the eligibility criteria were enrolled in the study: overweight (BMI 25–<30 kg/m2) or moderately obese (BMI 30–<35 kg/m2). Inclusion criteria required participants to be in good health condition, have a desire to lose weight, be accustomed to regular daily consumption of 3 main meals (breakfast, lunch, dinner), have a consistent and stable body weight in the last 3 months prior to screening, agree to take the investigational product (IP) as recommended, adhere to the recommended diet, maintain habitual levels of physical activity, commit to complete the participant diary and study questionnaires, and the use of contraception methods and a negative pregnancy test in women of childbearing potential. Main exclusion criteria were: sensitivity to any of the ingredients in the IP, uncontrolled thyroid gland disorder, uncontrolled hypertension, gastrointestinal disorders, diabetes mellitus type 1, uncontrolled diabetes mellitus type 2, significant surgery within the last 6 months, eating disorders within the last 12 months, significant deviation of safety laboratory parameters, electronic medical implant, any treatment/program that influenced body weight and gastrointestinal functions, smoking cessation within last 6 months, vegetarian/vegan/restrictive diet, pregnancy or nursing, and abuse of drugs and alcohol. Written informed consent was obtained from all participants before the trial was conducted. The clinical investigation was approved by the Ethics Committee of Charité − University Medicine Berlin and was performed in compliance with ISO 14155, the Declaration of Helsinki, and the Guidance for Good Clinical Practice (CPMP/ICH/135/95, ICH E6 [R2]). The study is registered with clinicaltrials.gov, No.: NCT03888911.
Diet and Intervention
Screening of participants was performed during visit 1, followed by a 2-week run-in phase for acclimation to study requirements. Instructions were given to the participants to maintain a nutritionally balanced and hypocaloric diet (providing 30% of energy from fat) according to the calculated individual energy requirement based on gender, age, physical activity, weight, and height, with 20% energy reduction [25]. A recommended diet plan was provided, and a diary was issued to each participant to record food and beverage intake on 2 weekdays and 1 weekend day per week for calorie intake assessment. At visit 2 (baseline), participants were randomly allocated to one of the three groups in a 1:1:1 ratio: IQP-LU-104 high-dose group (herein 104HD group), IQP-LU-104 low-dose group (herein 104LD), or the placebo group.
The IP consists of proprietary flaxseed mucilage (IQP-LU-104) as the functional composition. Other ingredients in the IP are excipients commonly used in manufacturing of pharmaceutical or food products such as bulking agent, anti-caking agent, sweetener, flavoring agent and colorant. IP was prepared in the form of sachets, and each sachet of 104HD and 104LD contained 2,560 mg and 1,280 mg of flaxseed mucilage, respectively. Placebo sachets contained standard excipients matching the taste and color of the product sachets given to the 104HD and 104LD groups. All sachets were identical in size and appearance.
Participants were instructed to take 1 sachet, mixed in a glass of water (∼200 mL) twice daily together with the two heaviest meals (breakfast, lunch, or dinner) of the day. The beverage was to be consumed before or during early stage of the meal, within 10 min of mixing.
Assessments
Body weight, body fat, and fat free mass, as well as the waist and hip circumference of the participants were measured during visit 1 (screening, week −2), visit 2 (baseline, week 0), visit 3 (week 4), visit 4 (week 8), and visit 5 (week 12) of the study. Body weight, body fat, and fat free mass (per bioimpedance) were measured in participants wearing underwear and barefoot using validated electronic weighing scales (Tanita BC-420 MA). Waist circumference (cm) was measured at the level midway between the lateral lower rib margin and the iliac crest, whereas hip circumference (cm) was measured as the maximal circumference over the buttocks using a measuring tape.
Additionally, the overall feelings of hunger, satiety, fullness, and craving were assessed throughout the study via entries in the participants' diaries on 3 days per week (2 weekdays and 1 weekend day of their choice). A visual analogue scale 100 mm in length was used to rate the feelings of hunger, satiety, and fullness, from no feeling at all to very strong feeling. For the feeling of craving, a 5-point Likert scale (0 = “no,” 1 = “slightly,” 2 = “moderate,” 3 = “strong,” 4 = “very strong”) was used for the ratings [26]. The appetite rating of a day was retrospectively evaluated and recorded in the evening after the last meal.
Physical activity was assessed by the International Physical Activity Questionnaire short form [27] and completed by participants during their visits from visit 2 to visit 5. Stool frequency was recorded in the participants' diaries based on the number of bowel movements on 3 days per week (2 weekdays and 1 weekend day of their choice) from visit 2 to visit 5.
Blood samples for assessment of safety and lipid parameters, glycated hemoglobin (HbA1c), and levels of fat-soluble vitamins (A, D, E, K) were collected by the investigator at visit 1 and visit 5. The blood samples were transported on the same day in cooler boxes to a central laboratory for analysis. Safety assessment included the measurement of the blood count, glucose and hemoglobin levels, liver and renal parameters, and thyroid-stimulating hormone level in blood, as well as urine analysis. Measurement for blood pressure and pulse rate was performed during every visit using a standard calibrated oscillometric device. At every post-screening visit, individuals were interviewed by the investigators for the occurrence of any medical events and the respective adverse events were recorded. Information for each of the adverse event, such as the type, intensity, and causal relationship were collected. The global evaluation of benefit and tolerability was rated at the end of the study by both the participants and the investigators.
Compliance with study procedures was evaluated based on the intake of IP and study duration (from visit 2 to visit 5). IP intake compliance (%) was defined as “total number of sachets taken divided by the total number of sachets to be taken multiplied by 100.” Compliance acceptable range was determined at 80–120%. For study duration, the deviation between visit 2 and visit 5 should be within the tolerance range of +5 days to be in compliance.
Statistical Analyses
Primary endpoints of the study were the differences in mean changes of body weight: (1) between 104HD and placebo; and (2) between 104LD and placebo, after 12 weeks of intervention in comparison to baseline. The null hypotheses stated that there were no statistical differences (1) between 104HD and placebo, and (2) between 104LD and placebo on body weight after 12 weeks, respectively. The testing of the second null hypothesis could only be performed if the first null hypothesis was rejected. The nonparametric Mann-Whitney U test for independent samples was applied and performed by determining the rank sum of individual body weight changes. The full analysis set data was analyzed for primary endpoints, other benefit endpoints, and safety endpoints. Sensitivity analysis was performed on individuals who completed the intervention (with data available for visit 5) for the primary endpoints.
Other benefit endpoints, safety endpoints as well as concurrent variables were exploratively and descriptively assessed. For continuous data, the statistical characteristics (number, mean, standard deviation, median, extremes, and quartiles) were analyzed. For ordinal data, the frequency distribution was performed. All variables were evaluated primarily by exact nonparametric procedures. For independent groups, Mann-Whitney U test was applied for comparison of groups or subgroups, whereas Kruskal-Wallis test was applied for comparison of more than two groups. Wilcoxon test was applied for dependent groups for comparison pre-post within groups or subgroups and exact Fisher's test for comparison of percentage.
All statistical analyses were performed using the SPSS software version v22.0 (Statistical Package for the Social Sciences) and level of significance (p < 0.05) was assumed. Multiple tests were performed without correction of significance level in the explorative analysis.
The sample size estimation was determined by the postulated Cohens effect size (group comparison) of 0.8 as well as the previously determined requirements of the significance level of 5.0% (double-sided) and power of 80%. Taking into account the estimated dropout rate of 20% and the block randomization, a total sample size of 36 individuals per study group (total 108 individuals) was recommended.
Results
Baseline Characteristics
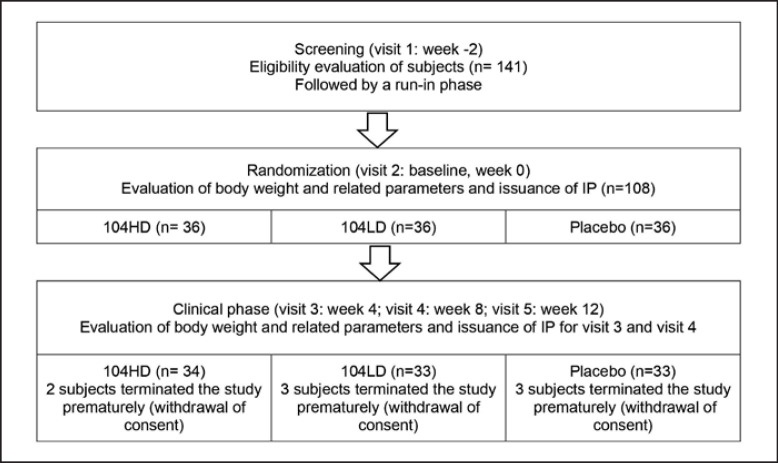
Out of the 108 enrolled participants, 8 were excluded from the full analysis set population as they terminated the study after their baseline visit (as shown in Fig. 1). Baseline characteristics of 100 participants in the FAS population are shown in Table 1. The mean age of the study population was 45.8 ± 13.4 years. Female constituted 66% of the study population. There were no statistical differences in age, gender distribution, blood pressure, pulse, body height, body weight, BMI, waist circumference, hip circumference, body fat mass, fat free mass, and energy intake between 104HD and placebo groups, 104LD and placebo groups, as well as 104HD and 104LD groups at baseline.
Fig. 1.
Study design and population.
Table 1.
Baseline characteristics of the study population
| Parameters | 104HD (n = 34) | 104LD (n = 33) | Placebo (n = 33 |
|---|---|---|---|
| Age | 43.2±13.0 | 46.8±13.2 | 46.2±14.0 |
| Gender, n (%) | |||
| Male | 11 (32.4) | 14 (42.4) | 9 (27.3) |
| Female | 23 (67.6) | 19 (57.6) | 24 (72.7) |
| Systolic blood pressure, mm Hg | 128.4±6.9 | 128.0±10.1 | 127.2±10.2 |
| Diastolic blood pressure, mm Hg | 80.3±5.7 | 79.3±7.1 | 79.5±5.6 |
| Pulse, bpm | 73.3±5.9 | 72.2±8.0 | 70.4±8.8 |
| Body weight, kg | 85.31±12.56 | 89.47±14.28 | 87.42±12.92 |
| Height, cm | 170.1±9.3 | 171.7±8.9 | 169.6±10.5 |
| BMI, kg/m2 | 29.39±2.69 | 30.17±2.84 | 30.28±2.07 |
| Body fat mass, kg | 28.97±8.21 | 30.91±7.20 | 30.62±6.56 |
| Fat free mass, kg | 56.05±10.64 | 58.56±12.57 | 55.56±11.53 |
| Waist circumference, cm | 106.2±10.8 | 108.6±10.0 | 107.9±8.9 |
| Hip circumference, cm | 108.0±8.5 | 112.2±8.4 | 110.5±5.8 |
| Energy intake, kcal | 1,761±281 | 1,832±319 | 1,771±322 |
Data are presented as mean ± SD or n (%) of participants for full analysis set population. No significant differences between groups for all parameters.
Compliance
There were no statistical differences between the groups in study duration from visit 2 to visit 5. The compliance rate of IP intake in the whole study population was 98.6 ± 3.8% and no statistical difference was found between the study groups.
Body Weight and Related Parameters
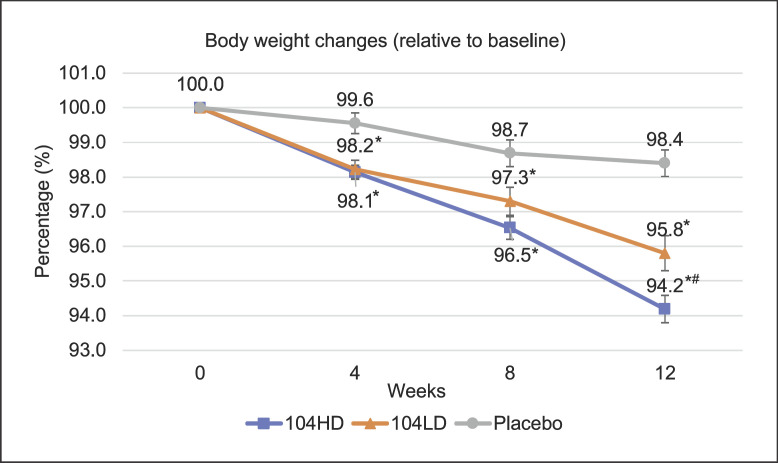
Following the 12-week intervention, both the 104HD and 104LD groups had a significantly greater reduction in mean body weight in comparison to the placebo group (each p < 0.001). Participants in the 104HD and 104LD groups lost additional 3.6 kg and 2.4 kg of body weight, respectively. Sensitivity analysis on individuals who completed the intervention showed that the 104HD (n = 33) and 104LD (n = 31) groups demonstrated the same weight loss effect and were significant compared to the placebo group (each p < 0.001), in comparison to the full analysis set population. The weight reduction effects in both the 104HD and 104LD groups were observed at week 4 and remained statistically significant at every visit until week 12. At week 4, the participants of both groups lost on average up to 4 times more weight compared to the placebo group. The changes in weight and other parameters are shown in Table 2. The body weight reduction (relative to baseline) throughout the study is shown in Figure 2. Relative body weight changes in 104HD and 104LD groups were statistically different compared to the placebo group from week 4 onwards.
Table 2.
Mean changes in body weight and other parameters from baseline to week 4, week 8, and week 12, respectively
| Parameters | 104HD (n = 34) | 104LD (n = 33) | Placebo (n = 33) | p value (104HD vs. placebo) | p value (104LD vs. placebo) |
|---|---|---|---|---|---|
| Body weight change, kg | |||||
| Week 4 | 1.58±1.03 | 1.59±1.37 | 0.39±1.50 | 0.001 | 0.002 |
| Week 8 | 2.96±1.52 | 2.38±2.07 | 1.16±1.87 | <0.001 | 0.018 |
| Week 12 | 4.96±1.89 | 3.70±2.57 | 1.33±2.05 | <0.001 | <0.001 |
| BMI change, kg/m2 | |||||
| Week 4 | 0.55±0.37 | 0.53±0.44 | 0.13±0.50 | 0.001 | 0.003 |
| Week 8 | 1.03±0.55 | 0.80±0.67 | 0.39±0.64 | <0.001 | 0.024 |
| Week 12 | 1.73±0.68 | 1.25±0.85 | 0.45±0.69 | <0.001 | <0.001 |
| Waist circumference change, cm | |||||
| Week 4 | 1.56±1.02 | 1.30±0.85 | 0.27±1.10 | <0.001 | <0.001 |
| Week 8 | 2.91±1.36 | 2.21±1.32 | 0.70±1.16 | <0.001 | <0.001 |
| Week 12 | 4.44±2.48 | 3.55±1.75 | 0.94±1.20 | <0.001 | <0.001 |
| Hip circumference change, cm | |||||
| Week 4 | 1.03±0.90 | 1.36±1.78 | 0.61±1.90 | 0.004 | 0.001 |
| Week 8 | 2.29±1.45 | 2.00±1.80 | 0.64±1.17 | <0.001 | <0.001 |
| Week 12 | 3.53±1.78 | 3.03±2.13 | 0.73±1.21 | <0.001 | <0.001 |
| Body fat mass change, kg | |||||
| Week 4 | 1.96±4.42 | 0.97±1.38 | 0.38±1.85 | 0.057 | 0.129 |
| Week 8 | 2.86±3.58 | 1.53±1.92 | 0.94±3.19 | 0.001 | 0.066 |
| Week 12 | 4.25±5.86 | 2.10±2.59 | 1.06±3.20 | 0.002 | 0.073 |
| Fat free mass change, kg | |||||
| Week 4 | −0.40±4.10 | 0.63±1.64 | 0.06±1.45 | 0.311 | 0.172 |
| Week 8 | 0.13±3.09 | 0.84±1.73 | 0.19±3.23 | 0.792 | 0.479 |
| Week 12 | 0.70±5.50 | 1.60±2.78 | 0.32±2.67 | 0.138 | 0.081 |
Data are presented as mean±SD for full analysis set population. Positive value denotes a reduction and negative value denotes an increase from baseline. p value bolded when significance <0.05.
Fig. 2.
Percentage of body weight reduction from baseline throughout the 12-week study. Error bars denote standard error of mean. *Significant versus placebo. #Significant versus 104LD.
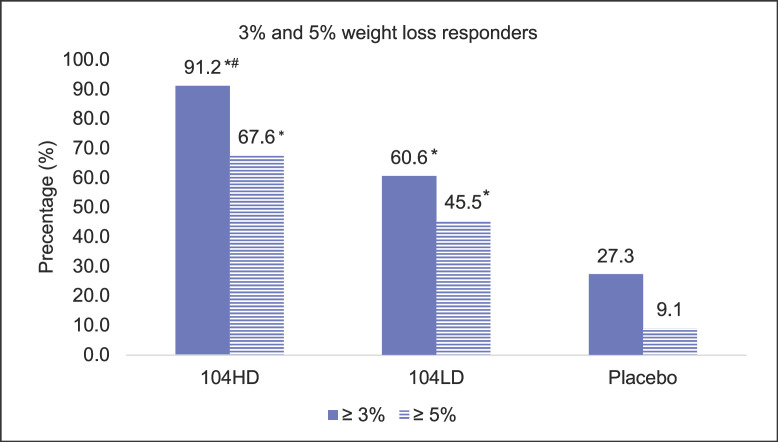
After the 12-week intervention phase, body weight was reduced by 5.84 ± 2.29% and 4.17 ± 3.73% from baseline in the 104HD and 104LD groups, respectively, compared to 1.55 ± 2.24% in the placebo group. In addition, 91.2% of participants in the 104HD group (p < 0.001 vs. placebo) and 60.6% of participants in the 104LD group (p = 0.013 vs. placebo) lost at least 3% baseline body weight, compared to only 27.3% of participants in the placebo group after 12 weeks. Similar trends were observed for participants who lost at least 5% of baseline body weight after 12 weeks, with 67.6% in the 104HD group (p < 0.001 vs. placebo) and 45.5% in 104LD group (p = 0.002 vs. placebo) compared to only 9.1% in the placebo group (shown in Fig. 3). In the subgroup analysis of overweight participants, the proportion of participants who lost at least 5% of baseline body weight was 63.2% in the 104HD group (p = 0.005 vs. placebo) and 52.9% in the 104LD group (p = 0.026 vs. placebo), compared to 12.5% in the placebo group. The proportion of obese participants who lost at least 5% of baseline body weight was 73.5% in the 104HD group (p < 0.001 vs. placebo) and 37.5% in the 104LD group (p = 0.039 vs. placebo), compared to 5.9% in the placebo group.
Fig. 3.
Responders with at least 3% and 5% weight loss after 12 weeks from baseline. *Significant versus placebo. #Significant versus 104LD.
Further subgroup analysis was performed on the weight loss effect in overweight (BMI 25–<30 kg/m2) and moderately obese participants (BMI 30–<35 kg/m2) after 12 weeks. Comparing to the placebo group, overweight participants in 104HD group and 104LD group lost additional 3.62 kg (p < 0.001) and 2.65 kg (p = 0.002) of weight, respectively, whereas the moderately obese participants in 104HD group and 104LD group lost additional 3.72 kg (p < 0.001) and 2.10 kg (p = 0.052) of weight, respectively.
The results of body fat mass reduction are shown in Table 2. While 104LD group showed a trend for fat mass reduction, statistical significance was observed in the 104HD group after 8 and 12 weeks. In the subgroup analysis, a statistically significant reduction was observed in the overweight participants in 104HD group (3.71 ± 3.57 kg, p = 0.008 vs. placebo) and in the 104LD group (2.63 ± 1.64 kg, p = 0.018 vs. placebo). No significant differences were found between the study groups on the changes of the fat free mass.
Results of other parameters associated with weight loss, i.e., BMI, waist circumference, and hip circumference are presented in Table 2. Participants in 104HD and 104LD groups had a significant mean reduction of 4.44 ± 2.48 cm and 3.55 ± 1.75 cm, respectively in waist circumference compared to the placebo group at only 0.94 ± 1.20 cm at the end of the study. The significant mean reduction in hip circumference was 3.53 ± 1.78 cm in the 104HD group and 3.03 ± 2.13 cm in the 104LD group compared to the placebo group (0.73 ± 1.21 cm). Participants in 104HD group and 104LD groups experienced significant reduction in BMI, waist circumference, and hip circumference from week 4 onwards in comparison to the placebo group.
Other Parameters
Feelings of hunger, fullness, satiety, and cravings were assessed as secondary parameters. At the end of study, no significant differences were found between the study groups.
Total cholesterol levels were reduced by 0.23 ± 0.82 mmol/L and 0.20 ± 0.83 mmol/L in both the 104HD and 104LD groups respectively, while the levels were increased by 0.14 ± 0.92 mmol/L in the placebo group at the end of the study. The difference between the 104LD and placebo groups was statistically significant (p = 0.038) while the difference between the 104HD and placebo groups was not significant. Statistically significant reduction of 0.11 ± 0.41 mmol/L (p = 0.040) in triglycerides level was observed in the 104HD group compared to the placebo group with an increase of 0.29 ± 1.03 mmol/L, but not in the 104LD group. There were no significant differences between the 104HD group or 104LD group versus placebo group in the changes of LDL-cholesterol, HDL-cholesterol, glucose, and HbA1c.
There were no significant differences in levels of fat-soluble vitamins (A, D, E, K, K2-4, K2-7) or in changes in mean daily bowel movements reported from baseline across all visits for both the 104HD and 104LD groups versus the placebo group after 12 weeks. Evaluation of the IPAQ-SF data showed that there were no significant differences for the change in time in vigorous and moderate intensity exercise, walking time, and calculated metabolic equivalent from baseline to the end of study between each of the 104HD group and 104LD group versus placebo group. Furthermore, there were no relevant differences between both the 104HD and 104LD groups versus placebo group on calorie intake.
At the end of the study, 97.0% and 80.6% of participants in the 104HD and 104LD groups rated good or very good for the benefits of the treatment, respectively, compared to 19.3% in the placebo group. The investigators rated good or very good for 97.0% and 77.4% of participants in the 104HD and 104LD groups, respectively, compared to 19.3% in the placebo group.
Safety Assessment
All participants, as well as the investigators for all participants, rated the tolerability of 104HD, 104LD, and placebo as good or very good. There were no clinically significant differences for the changes in blood pressure, pulse rate, laboratory values (hemoglobin, hematocrit, erythrocytes, platelets, leucocytes, alanine-aminotransferase, aspartate-aminotransferase, alkaline phosphatase, gamma-glutamyl transferase, bilirubin, creatine, urea, uric acid, and thyroid-stimulating hormone) between the study groups. There were no clinically significant findings for any participant in the urinalysis examination conducted at the end of the study. Sixteen participants reported at least 1 adverse event during the study (5 from 104HD group, 8 from 104LD group, and 3 from placebo group); however, there were no statistically significant differences between the three study groups in the percentage of participants with adverse events. Respiratory tract infections and gastrointestinal symptoms were the main adverse events reported. For all adverse events, the causal relationship to the intake of IQP-LU-104 was regarded as unlikely. No serious adverse event was reported.
Discussion
Results from the present study demonstrated the dose-dependent weight loss effect of IQP-LU-104, consisting of flaxseed mucilage as the functional ingredient. Daily dose of 5,120 mg (104HD) and 2,560 mg (104LD) flaxseed mucilage resulted in significant 4.96 ± 1.89 kg and 3.70 ± 2.57 kg of body weight reduction after 12 weeks, respectively, compared to 1.33 ± 2.05 kg in the placebo group. The 104HD group experienced an additional 1.26 kg of weight loss compared to the 104LD group; however, the difference was not statistically significant. The significant weight loss effect of both groups was observed after 4 weeks of intervention and was increasing significantly until the end of the study. Our study showed that 67.6% participants and 45.5% participants in the 104HD group and 104LD group, respectively, lost at least 5% of their baseline weight after 3 months. The results achieved were in line with the recommended target according to the European Practical and Patient-Centred Guidelines for Adult Obesity Management in Primary Care for obese patients [5, 28].
Reduction in body fat mass was observed in both groups, however statistically significant only in the 104HD group. There were no significant differences in changes in fat free mass, demonstrating that the weight reduction effect was primarily based on body fat reduction. Although stool samples in this study were not analyzed for fat excretion, the observed body fat reduction effects may be associated with the increase in fecal fat excretion as reported in previous studies [20, 29]. Kristensen et al. [30] demonstrated that a greater weight of fecal fat (4.96 ± 0.31 g) was excreted with daily intake of 5.2 g of soluble fibers from flaxseed mucilage drinks for 7 days compared to the placebo group (3.20 ± 0.30 g, p < 0.05).
In an acute appetite suppression study conducted by Ibrügger et al. [31], oral administration of 2.5 g flaxseed soluble fibers in drinks increased sensation of satiety and fullness, and decreased energy intake in the subsequent meal significantly compared to the control group. Similar appetite ratings were exhibited by the same dose in tablet format [31]. Vuksan et al. [32] reported that the intake of 31.5 g of ground flaxseed (equivalent to 2.5 g soluble fibers) had significantly reduced desire to eat, hunger, fullness, and overall appetite compared to the control group. Despite the positive findings from other research on the effect of flaxseed mucilage or flaxseed fiber on appetite suppression [31, 33], this effect has not been prominently shown in the present study. This could be explained by differences in study methodology. For studies that showed significant results, appetite sensations were assessed at specific intervals within a defined period following a standardized meal; thereafter, an ad libitum meal was provided followed by the measurement and calculation of energy intake. The present study was primarily designed for the assessment of weight loss, while the subjective evaluation of satiety, hunger, and fullness sensations based on recall was only explorative and may not be specific for evaluation of appetite suppression post-meal. Furthermore, the study may not be sufficiently powered for evaluation of appetite and related sensations in the given setting. Nevertheless, the effects of flaxseed mucilage or flaxseed fiber on appetite suppression (e.g., increased sensation of satiety and fullness, lower ratings of hunger) have been demonstrated in appetite suppression clinical studies [29, 30] and provide an explanation to the mechanism of action of IQP-LU-104 in weight loss.
In this study, there was a slight but statistically significant reduction in total cholesterol and triglycerides levels. There was no significant reduction in blood glucose and HbA1c levels. This was not beyond our expectations as the recruitment was not targeted on individuals with high baseline values that required reduction. It was reported that viscous fiber has no significant effect on individuals with normal cholesterol level as its cholesterol lowering property was highly influenced by the baseline level [22]. Positive findings were reported in other studies on flaxseed fibers (providing 5.2 g of fibers), defatted or milled flaxseed with higher dosages [30, 34, 35].
A positive impact of IQP-LU-104 on body weight and body fat reduction in the longer term (beyond 12 weeks) may lead to beneficial effects on attenuating the risk of metabolic syndrome traits including improvement in lipid profile, reduction in blood pressure level and risk of developing type 2 diabetes [6, 36]. Moreover, decrease in waist circumference has become an important treatment target for reducing cardiovascular health risk in both men and women due to the increase in abdominal obesity. Waist circumference was proposed by the Consensus Statement from the International Atherosclerosis Society and International Chair on Cardiometabolic Risk Working Group as a measurement for health management [37]. An increase in waist circumference of >5 cm over approximately 4 years, with little weight gain is significantly associated with higher total mortality in both men and women [38]. In our study with a duration of 12 weeks, participants in the 104HD and 104LD groups had a mean reduction of 4.44 ± 2.48 cm and 3.55 ± 1.75 cm, respectively, in waist circumference compared to those in the placebo group at only 0.94 ± 1.20 cm.
IQP-LU-104 was well tolerated in the 12 weeks' trial with no major adverse events reported. These observations were consistent with the wide consumption of flaxseed as functional food and dietary supplement. One of the limitations of the present study is that the trial was only performed for a period of 12 weeks with no further follow-up after the intervention period, whereby weight maintenance effect and feedback from participants after weight loss were not investigated. Thus, the results of the study may need to be further investigated. For example, a long-term weight loss-weight maintenance study would be useful to ascertain the health benefits of the product in achieving and in maintaining healthy weight. Second, for appetite and related assessments, standardized assessments, including, e.g., an ad-libitum meal with actual measurement of energy intake should be considered instead of using recall-based records. Considering future studies, it would be worthwhile to investigate the efficacy of IQP-LU-104 in long-term weight management or integrating IQP-LU-104 into the diet via newer strategies, such as nutritional coaching [39], practice of mindful eating [40], lifestyle intervention, and personalized diet plans, which have been recommended as effective approaches for sustainable weight loss [41, 42].
In conclusion, this is the first clinical evidence of the effect of flaxseed mucilage (IQP-LU-104) in reducing body weight in overweight and moderately obese individuals. Throughout the 12-week intervention period, compliance with IP intake was very good, as was tolerability since no adverse effects related to the intake of IQP-LU-104 were reported. IQP-LU-104 can be conveniently incorporated into a person's daily meal as an effective lifestyle approach in combating obesity.
Statement of Ethics
The clinical study was performed in accordance with the principles of the World Medical Association (Declaration of Helsinki), the Guidance for Good Clinical Practice (CPMP/ICH/135/95, ICH E6 [R2]), and ISO 14155:2011. The trial was approved by the Ethics Committee of Charité −University Medicine Berlin and registered with clinicaltrials.gov (no.: NCT03888911). Written consent was obtained from all the participants before the trial was conducted.
Conflict of Interest Statement
Udo Bongartz, Uwe Hochmann, and Felix Alt are the employees; Constantin Erlenbeck is a former employee; and Ralf Uebelhack is the medical adviser of analyze & realize GmbH − clinical research organization that conducted the study. Pee Win Chong, Patricia De Costa, and Li Vern Peng are the employees of InQpharm Group that funded the study.
Funding Sources
The study was funded by InQpharm Group. InQpharm Group had no involvement in the conduct of the trial, collection of data, trial management, data analysis, and reporting of the results.
Author Contributions
Udo Bongartz, Uwe Hochmann, Barbara Grube, and Ralf Uebelhack were the investigators of the clinical trial. Felix Alt and Constantin Erlenbeck were involved in the study design, study management, and interpretation of results. Authors from InQpharm Group contributed to the design of the study and interpretation of data and results. Li Vern Peng wrote the manuscript and Pee Win Chong and Patricia De Costa critically revised and contributed to the final content of the manuscript. All authors reviewed and approved the manuscript.
Data Availability Statement
Further enquiries on the data generated or analyzed during this study can be directed to the corresponding author.
Acknowledgments
The authors thank Dr. Norman Bitterlich for the support in statistical analysis and Amel Ghouili and Lynne Baxter for the participation in the review and editing of the manuscript.
References
- 1.Inoue Y, Qin B, Poti J, Sokol R, Gordon-Larsen P. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018 Dec;7((4)):276–88. doi: 10.1007/s13679-018-0317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019 Dec;381((25)):2440–50. doi: 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 3.Purnell JQ. Definitions, classification, and epidemiology of obesity. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al., editors. Endotext. South Dartmouth (MA): MDText com; 2018. Apr, [PubMed] [Google Scholar]
- 4.Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: pathophysiology and management. J Am Coll Cardiol. 2018 Jan;71((1)):69–84. doi: 10.1016/j.jacc.2017.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Durrer Schutz D, Busetto L, Dicker D, Farpour-Lambert N, Pryke R, Toplak H, et al. European practical and patient-centred guidelines for adult obesity management in primary care. Obes Facts. 2019 Jan;12((1)):40–66. doi: 10.1159/000496183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of cardiology/American Heart Association task force on practice guidelines and the obesity society. Circulation. 2014 Jun;129((25 Suppl 1)):S102–38. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bernacchia R, Preti R, Vinci G. Chemical composition and health benefits of flaxseed. Austin J Nutr Food Sci. 2014 Oct;2((8)):1045. [Google Scholar]
- 8.Shim YY, Gui B, Arnison PG, Wang Y, Reaney MJT. Flaxseed (Linum usitatissimum L.) bioactive compounds and peptide nomenclature: a review. Trends Food Sci Technol. 2014 Jul;38((1)):5–20. [Google Scholar]
- 9.Parikh M, Netticadan T, Pierce GN. Flaxseed: its bioactive components and their cardiovascular benefits. Am J Physiol Heart Circ Physiol. 2018 Feb;314((2)):H146–59. doi: 10.1152/ajpheart.00400.2017. [DOI] [PubMed] [Google Scholar]
- 10.Hanif Palla A, Gilani AH. Dual effectiveness of flaxseed in constipation and diarrhea: possible mechanism. J Ethnopharmacol. 2015 Jul;169:60–8. doi: 10.1016/j.jep.2015.03.064. [DOI] [PubMed] [Google Scholar]
- 11.Parikh M, Maddaford TG, Austria JA, Aliani M, Netticadan T, Pierce GN. Dietary flaxseed as a strategy for improving human health. Nutrients. 2019 May;11((5)):1171. doi: 10.3390/nu11051171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Singh KK, Mridula D, Rehal J, Barnwal P. Flaxseed: a potential source of food, feed and fiber. Crit Rev Food Sci Nutr. 2011 Mar;51((3)):210–22. doi: 10.1080/10408390903537241. [DOI] [PubMed] [Google Scholar]
- 13.Gray J. International Life Science Institue Europe Concise Monograph Series. Brussels: ILSI Europe; 2006. Dietary fibre definition, analysis, physiology health. [Google Scholar]
- 14.Fedeniuk RW, Biliaderis CG. Composition and physicochemical properties of linseed (Linum usitatissimum L.) mucilage. J Agric Food Chem. 1994 Feb;42((2)):240–7. [Google Scholar]
- 15.Kaewmanee T, Bagnasco L, Benjakul S, Lanteri S, Morelli CF, Speranza G, et al. Characterisation of mucilages extracted from seven Italian cultivars of flax. Food Chem. 2014 Apr;148:60–9. doi: 10.1016/j.foodchem.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Oomah BD, Kenaschuk EO, Cui W, Mazza G. Variation in the composition of water-soluble polysaccharides in flaxseed. J Agric Food Chem. 1995 Jun;43((6)):1484–8. [Google Scholar]
- 17.Kristensen M, Jensen MG. Dietary fibres in the regulation of appetite and food intake. Importance of viscosity. Appetite. 2011 Feb;56((1)):65–70. doi: 10.1016/j.appet.2010.11.147. [DOI] [PubMed] [Google Scholar]
- 18.Kajla P, Sharma A, Sood DR. Flaxseed-a potential functional food source. J Food Sci Technol. 2015 Apr;52((4)):1857–71. doi: 10.1007/s13197-014-1293-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amiri MS, Mohammadzadeh V, Yazdi MET, Barani M, Rahdar A, Kyzas GZ. Plant-based gums and mucilages applications in pharmacology and nanomedicine: a review. Molecules. 2021 Mar;26((6)):1770. doi: 10.3390/molecules26061770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kristensen M, Damgaard TW, Sørensen AD, Raben A, Lindeløv TS, Thomsen AD, et al. Whole flaxseeds but not sunflower seeds in rye bread reduce apparent digestibility of fat in healthy volunteers. Eur J Clin Nutr. 2008 Aug;62:961–7. doi: 10.1038/sj.ejcn.1602813. [DOI] [PubMed] [Google Scholar]
- 21.Repin N, Kay BA, Cui SW, Wright AJ, Duncan AM, Goff HD. Investigation of mechanisms involved in postprandial glycemia and insulinemia attenuation with dietary fibre consumption. Food Funct. 2017 Jun;8((6)):2142–54. doi: 10.1039/c7fo00331e. [DOI] [PubMed] [Google Scholar]
- 22.McRorie JW. Evidence-based approach to fiber supplements and clinically meaningful health benefits, part 1: what to look for and how to recommend an effective fiber therapy. Nutr Today. 2015 Mar;50((2)):82–9. doi: 10.1097/NT.0000000000000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohammadi-Sartang M, Mazloom Z, Raeisi-Dehkordi H, Barati-Boldaji R, Bellissimo N, Totosy de Zepetnek JOJO. The effect of flaxseed supplementation on body weight and body composition: a systematic review and meta-analysis of 45 randomized placebo-controlled trials. Obes Rev. 2017 Sep;18((9)):1096–107. doi: 10.1111/obr.12550. [DOI] [PubMed] [Google Scholar]
- 24.Shafie SR, Wanyonyi S, Panchal SK, Brown L. Linseed components are more effective than whole linseed in reversing diet-induced metabolic syndrome in rats. Nutrients. 2019 Jul;11((7)):1677. doi: 10.3390/nu11071677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trumbo P, Schlicker S, Yates AA, Poos M, Food and Nutrition Board of the Institute of Medicine, The National Academies Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002 Nov;102((11)):1621–30. doi: 10.1016/s0002-8223(02)90346-9. [DOI] [PubMed] [Google Scholar]
- 26.Flint A, Raben A, Blundell JE, Astrup A. Reproducibility, power and validity of visual analogue scales in assessment of appetite sensations in single test meal studies. Int J Obes Relat Metab Disord. 2000 Jan;24((1)):38–48. doi: 10.1038/sj.ijo.0801083. [DOI] [PubMed] [Google Scholar]
- 27.Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. 2011 Oct;8:115. doi: 10.1186/1479-5868-8-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karam J, McFarlane S. Tackling obesity: new therapeutic agents for assisted weight loss. Diabetes Metab Syndr Obes. 2010 Apr;26((3)):95–112. [PMC free article] [PubMed] [Google Scholar]
- 29.Kristensen M, Juul SR, Sørensen KV, Lorenzen JK, Astrup A. Supplementation with dairy calcium and/or flaxseed fibers in conjunction with orlistat augments fecal fat excretion without altering ratings of gastrointestinal comfort. Nutr Metab (Lond) 2017 Feb;14:13. doi: 10.1186/s12986-017-0164-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kristensen M, Jensen MG, Aarestrup J, Petersen KE, Søndergaard L, Mikkelsen MS, et al. Flaxseed dietary fibers lower cholesterol and increase fecal fat excretion, but magnitude of effect depend on food type. Nutr Metab (Lond) 2012 Feb;9:8. doi: 10.1186/1743-7075-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibrügger S, Kristensen M, Mikkelsen MS, Astrup A. Flaxseed dietary fiber supplements for suppression of appetite and food intake. Appetite. 2012 Apr;58((2)):490–5. doi: 10.1016/j.appet.2011.12.024. [DOI] [PubMed] [Google Scholar]
- 32.Vuksan V, Choleva L, Jovanovski E, Jenkins AL, Au-Yeung F, Dias AG, et al. Comparison of flax (Linum usitatissimum) and Salba-chia (Salvia hispanica L.) seeds on postprandial glycemia and satiety in healthy individuals: a randomized, controlled, crossover study. Eur J Clin Nutr. 2017 Feb;71((2)):234–8. doi: 10.1038/ejcn.2016.148. [DOI] [PubMed] [Google Scholar]
- 33.Kristensen M, Savorani F, Christensen S, Engelsen SB, Bügel S, Toubro S, et al. Flaxseed dietary fibers suppress postprandial lipemia and appetite sensation in young men. Nutr Metab Cardiovasc Dis. 2013 Feb;23((2)):136–43. doi: 10.1016/j.numecd.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 34.Jenkins DJ, Kendall CW, Vidgen E, Agarwal S, Rao AV, Rosenberg RS, et al. Health aspects of partially defatted flaxseed, including effects on serum lipids, oxidative measures, and ex vivo androgen and progestin activity: a controlled crossover trial. Am J Clin Nutr. 1999 Mar;69((3)):395–402. doi: 10.1093/ajcn/69.3.395. [DOI] [PubMed] [Google Scholar]
- 35.Yari Z, Rahimlou M, Poustchi H, Hekmatdoost A. Flaxseed supplementation in metabolic syndrome management: a pilot randomized, open-labeled, controlled Study. Phytother Res. 2016 Aug;30((8)):1339–44. doi: 10.1002/ptr.5635. [DOI] [PubMed] [Google Scholar]
- 36.Magkos F, Fraterrigo G, Yoshino J, Luecking C, Kirbach K, Kelly SC, et al. Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity. Cell Metab. 2016 Apr;23((4)):591–601. doi: 10.1016/j.cmet.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. 2020 Mar;16((3)):177–89. doi: 10.1038/s41574-019-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mulligan AA, Lentjes MAH, Luben RN, Wareham NJ, Khaw KT. Changes in waist circumference and risk of all-cause and CVD mortality: results from the European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) cohort study. BMC Cardiovasc Disord. 2019 Oct;19((1)):238. doi: 10.1186/s12872-019-1223-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dayan PH, Sforzo G, Boisseau N, Pereira-Lancha LO, Lancha AH. A new clinical perspective: treating obesity with nutritional coaching versus energy-restricted diets. Nutrition. 2019 Apr;60:147–51. doi: 10.1016/j.nut.2018.09.027. [DOI] [PubMed] [Google Scholar]
- 40.Dunn C, Haubenreiser M, Johnson M, Nordby K, Aggarwal S, Myer S, et al. Mindfulness approaches and weight loss, weight maintenance, and weight regain. Curr Obes Rep. 2018 Mar;7((1)):37–49. doi: 10.1007/s13679-018-0299-6. [DOI] [PubMed] [Google Scholar]
- 41.Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin North Am. 2018 Jan;102((1)):49–63. doi: 10.1016/j.mcna.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 42.Smethers AD, Rolls BJ. Dietary management of obesity: cornerstones of healthy eating patterns. Med Clin North Am. 2018 Jan;102((1)):107–24. doi: 10.1016/j.mcna.2017.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Further enquiries on the data generated or analyzed during this study can be directed to the corresponding author.