Abstract
Background
Remote patient monitoring (RPM) interventions are being increasingly implemented in health care environments, given their benefits for different stakeholders. However, the effects of these interventions on the workflow of clinical staff are not always considered in RPM research and practice.
Objective
This review explored how contemporary RPM interventions affect clinical staff and their workflows in perioperative settings.
Methods
We conducted a scoping review of recent articles reporting the impact of RPM interventions implemented in perioperative settings on clinical staff and their workflow. The databases accessed were Embase and PubMed. A qualitative analysis was performed to identify the main problems and advantages that RPM brings to staff, in addition to the approaches taken to evaluate the impact of those interventions. Different themes were identified in terms of the challenges of RPM for clinical staff as well as in terms of benefits, risk-reduction strategies, and methods for measuring the impact of these interventions on the workflow of clinical staff.
Results
A total of 1063 papers were found during the initial search, of which 21 (1.98%) met the inclusion criteria. Of the 21 included papers, 15 (71%) focused on evaluating new RPM systems, 4 (19%) focused on existing systems, and 2 (10%) were reviews.
Conclusions
The reviewed literature shows that the impact on staff work experience is a crucial factor to consider when developing and implementing RPM interventions in perioperative settings. However, we noticed both underdevelopment and lack of standardization in the methods for assessing the impact of these interventions on clinical staff and their workflow. On the basis of the reviewed literature, we recommend the development of more robust methods for evaluating the impact of RPM interventions on staff experience in perioperative care; the adoption of a stronger focus on transition management when introducing these interventions in clinical practice; and the inclusion of longer periods of assessment, including the evaluation of long-term goals.
Keywords: remote patient monitoring, telemonitoring, workflow, nurses, physicians, perioperative care, perioperative medicine, telehealth, mobile phone
Introduction
Background
Remote patient monitoring (RPM) interventions allow patients to be continuously monitored at a distance and beyond the physical borders of the hospital or health care institution [1]. RPM interventions have been used to monitor patients within clinical settings (eg, in intensive care environments) or outside of care facilities (eg, in the patients’ homes). Moreover, RPM has been used for delivering care for multiple health conditions, from heart failure [2] to diabetes [3] and skin problems [4].
RPM interventions can provide 24-hour care as they can collect data continuously and alert specialists when certain parameters are outside the standard thresholds [5]. This can enable real-time adjustments, timely decisions, and improved care. RPM as a field has also enjoyed an unprecedented acceleration as a consequence of the COVID-19 pandemic, which has stimulated the adoption of remote care to minimize face-to-face interactions between patients and staff [6]. In the perioperative setting, RPM can be useful for assessing physical conditions preoperatively or monitoring patients’ recovery after discharge. Although RPM applications in this domain are still relatively novel, encouraging results are driving an increased interest from researchers and practitioners.
An example of the application of RPM technologies to perioperative care was offered by Atilgan et al [7], who evaluated a system comprising monitoring devices collecting several vital signs (including blood pressure, heart rate, oxygen saturation, body temperature, blood glucose, and electrocardiography) and a mobile app providing medication reminders, suggested daily life activities, diet and nutrition plans, and web-based visit capabilities. Vital parameters were measured in patients who had undergone cardiac surgery after discharge and automatically transferred to a telemedicine team for assessment. Overall, the authors reported the RPM intervention to have resulted in high patient satisfaction, prevention of incorrect medications and dosages, prevention of rehospitalization, and early detection of potentially life-threatening complications.
Much of the available research on RPM interventions in the perioperative domain focuses on the effects of RPM on patients [8-11] and describes its advantages, especially in terms of clinical outcomes and efficiency gains [12-14]. Some studies have also addressed the benefits for health care providers, such as hospitals, nursing homes, and other entities. These studies tend to focus on the economic benefits for providers, for instance through reductions in hospitalizations and thus, in the use of resources [15,16]. However, there is limited knowledge of the benefits and limitations of RPM for clinical staff.
Objectives
This research seeks to evaluate the impact of RPM interventions on the workflow of clinical staff in the context of perioperative care. To explain what we mean by workflow, we follow Carayon et al [17], who defined workflow as “the flow of people, equipment, information, and tasks, in different places, at different levels, at different timescales continuously and discontinuously, that are used or required to support the goals of the work domain.” This means that we aimed to evaluate the impact of RPM-related tasks in combination with previously existing activities. In this paper, the words clinical staff will be used when referring to both nurses and specialists. To investigate the impact of RPM on the workflow of clinical staff, a human factor perspective was adopted in this review. As mentioned by Hignett et al [18], human factors help in understanding the interactions between humans and the elements of a system to optimize its performance and human well-being.
This scoping review sought to answer the following overall research question: What is the impact of perioperative RPM interventions on the workflow of clinical staff? To answer this main question, we developed the following subresearch questions: (1) What are the problems and challenges of perioperative RPM interventions for clinical staff from a workflow perspective? (2) What are the benefits of perioperative RPM interventions for clinical staff from a workflow perspective? (3) What strategies are implemented or proposed to overcome the problems that perioperative RPM interventions present to the workflow of clinical staff? (4) How is the impact of perioperative RPM interventions on the workflow of clinical staff evaluated and measured?
Methods
Overview
This scoping review followed the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist [19]. As the review focuses on collecting and comparing workflow-related insights from recent RPM literature rather than on drawing conclusions on specific outcomes, the risk of bias in the results of the included studies was not assessed. Conversely, the risk of bias in the synthesis of the literature review findings was considered. Specifically, the risk of bias owing to missing results was assessed by MAL and VP through the framework for assessing the risk of bias owing to missing results in a synthesis offered in the Cochrane Handbook for Systematic Reviews of Interventions [20]. The results of this assessment are discussed in the Limitations section.
Selection Criteria and Search Strategy
The databases used were PubMed and Embase. To define the inclusion criteria, key concepts were selected. For each of them, keywords were defined to guide the search strategy (Textbox 1). For the keywords of each concept, the logical operator OR was included to consider all the possibilities, whereas the logical operator AND was used between concepts. The full queries in both databases are presented in Multimedia Appendix 1. Finally, the search included articles that were written in English between January 2015 and March 2021. This was chosen to obtain a picture of contemporary RPM interventions as this review focuses on current challenges and opportunities. The search was conducted during the last week of March 2021.
Concepts included in the literature search.
-
A keyword can have some variations (plural or singular form or simple or continuous verb form). An asterisk (*) is used for the search algorithm in the database to find all possible variations of a certain word.
Remote patient monitoring: remote monitor*; telemedicine; telemonitoring; telehealth, remote follow-up; eHealth; remote consultation; remote sensing technology; self-monitor*
Workflow: workflow; outcome and process assessment, health care; task performance and analysis; workflow; staffing; attitude of health personnel; alarm fatigue*; alert fatigue; professional burnout, workload; patient care management; nursing process*; clinical competence; caregiver burden; time and motion studies; work simplification; practice patterns, nurses; nursing audit
Perioperative care: surgical procedures, operative; general surgery; perioperative; surgery; post-operative; post-discharge
The articles resulting from this search were screened based on the following inclusion criteria: (1) the inclusion of RPM interventions for perioperative care and (2) the mention of the impact on the workflow of clinical staff.
The criteria were used for 2 iterations of screening: the first was based on the title and abstract of the articles, and the second was based on the full text.
Review Process and Analysis
Our main categories were established (Textbox 2) to analyze the studies, namely challenges and problems, benefits, risk-reduction strategies, and evaluation methods. These were based on the main goals of this research and the research questions.
Categories used for data extraction.
Problems and challenges of remote patient monitoring (RPM) interventions for clinical staff: includes the problems shown regarding RPM interventions for clinical staff.
Benefits of RPM interventions for clinical staff: includes the benefits concerning RPM interventions for clinical staff.
Risk-reduction strategies regarding RPM interventions for clinical staff: includes solutions tested to tackle some of the problems brought by the introduction of RPM interventions and some of the proposals suggested.
Methods to measure and quantify the impact of RPM interventions on clinical staff: includes the methods used to determine the impact of RPM interventions on clinical staff’s tasks and workflow. It entails the variables and measures collected and analyzed.
The articles were reviewed by MAL, who was also responsible for data extraction. Subsequently, the first step of the analysis was performed by classifying the results into the chosen categories. The second step consisted of creating different themes per category. This step required several iterations to obtain the final set of themes.
Results
Overview
A total of 1063 articles were identified after searching both databases, of which 1007 (94.73%) were left after deduplication. Of these 1007 articles, 137 (13.6%) fulfilled the first round of selection, and 21 (2.09%) passed the final round of selection (Figure 1).
Figure 1.
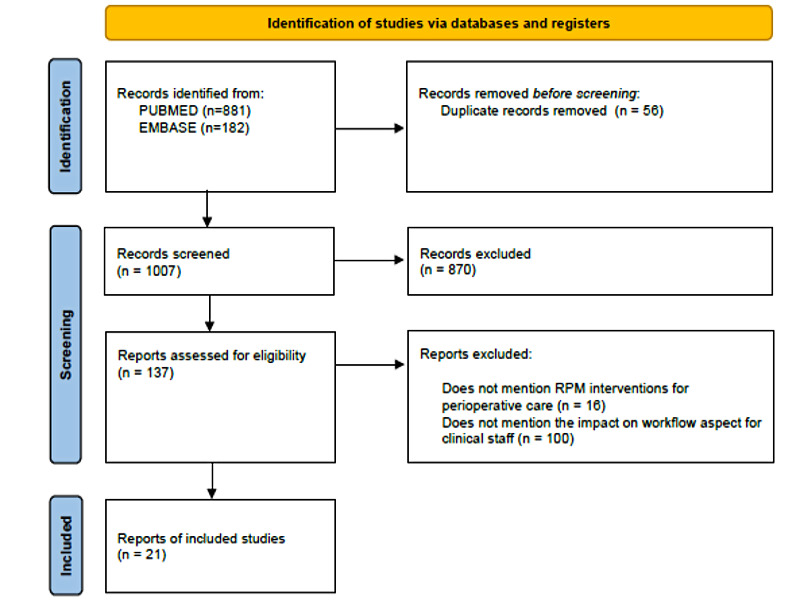
Flowchart of the scoping review process and the inclusion and exclusion criteria. RPM: remote patient monitoring.
In general, the articles included in this review were experimental or observational studies. Of the 21 articles, 15 (71%) involved the evaluation of a design intervention (an RPM model, tool, or service), 4 (19%) consisted of an analysis of already implemented interventions, and the remaining 2 (10%) were reviews. The references and articles analyzed in these 2 reviews did not include any of the other selected articles in this scoping review.
The studies focused on a wide range of patient cohorts and surgical specialties, including orthopedic, bariatric, and oncological surgery. Most of these studies (20/21, 95%) focused on adult patients (aged >18 years). The described RPM interventions ranged from 1 to 45 months of duration.
In addition, the articles presented different types of RPM interventions, ranging from e-tools used only by the clinical staff to services and models that incorporated devices and platforms for both patients and specialists. Moreover, most of the interventions contemplated nursing staff as the main actors responsible for remote care and included physicians for specific tasks or just in case a more detailed and in-depth analysis of the patient’s data was needed.
Not all the included studies contained information on all the categories established. For example, the included reviews hardly mentioned the methodologies used to assess the impact of different RPM interventions on the workflow of the clinical staff.
Once the data were extracted from the articles, they were classified into the 4 categories. To better understand each category, different themes were defined (Figure 2) based on the similarity of the topics addressed in each of the articles. Figure 2 presents an overview of this classification, where each category is labeled with a different color. By means of a gradient in the color’s intensity, it is possible to show the quantity of papers that touch on each of the proposed themes. In this case, more saturated colors represent more papers mentioning information relevant to a specific theme. The results for each category are discussed in detail in the following sections.
Figure 2.
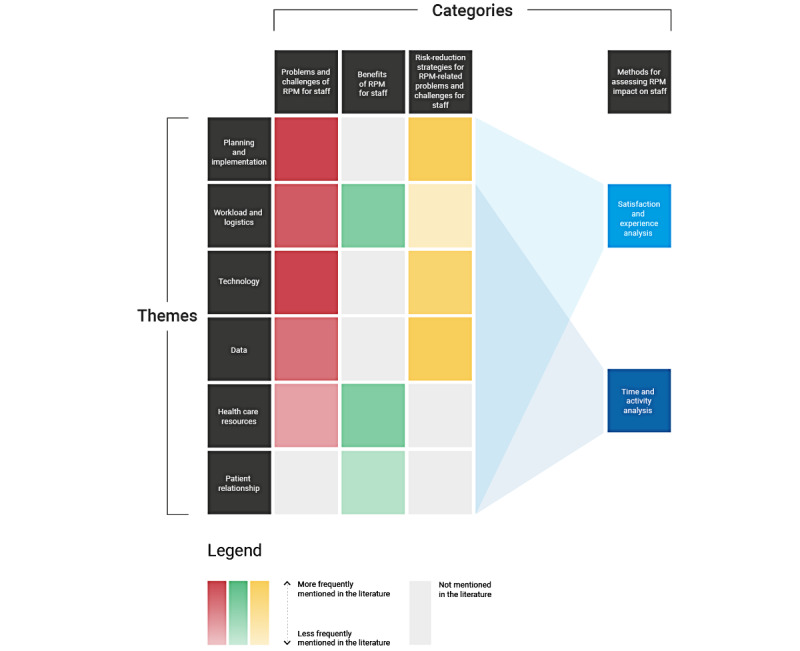
Heat map of the review results organized by categories (each corresponding to a research question) and themes (recurring topics touched on in the included studies). RPM: remote patient monitoring.
Category 1: Problems and Challenges of RPM for Clinical Staff
On the basis of the articles analyzed, 5 main themes regarding RPM challenges from the viewpoint of clinical staff were identified (Table 1). The first theme was planning and implementation. Planning is a complex task in health care given the diversity of the stakeholders involved and their needs. RPM projects do not always involve or consider the complex context in which these interventions have to be implemented. This often leads to ambiguity in tasks and roles and, thus, to lack of clarity and structure in the workflow of the clinical staff.
Table 1.
Overview of problems and challenges of remote patient monitoring (RPM) interventions for clinical staff.
| Theme and description | Studies | |
| Planning and implementation | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Workload and logistics | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Technology | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Data | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Health care resources | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
aEMR: electronic medical record.
bGP: general practitioner.
The second theme was workload and logistics. Some staff members do not feel comfortable with the new behind-the-desk activities, which can result in unpredictable and emergent tasks when RPM systems register values outside the thresholds. Moreover, data analysis may require more than one specialist, making the workflow more complex. In addition, RPM is perceived as bringing more work, which adds to the existing schedule.
The third theme was technology. Systems might not be user-friendly, and different technical malfunctions may arise, which may require extra expertise from clinical staff.
The fourth theme was data, which can produce more informed decisions but also increase time and be burdensome to analyze. Moreover, it can be hard to keep all the data under 1 platform, so the staff may need to analyze multiple fragments of information to provide remote care.
The last theme was health care resources, intended as the new resources that RPM interventions require. Moreover, the aforementioned ambiguity in tasks determines a lack of clarity regarding reimbursement policies.
A detailed overview of the reported challenges for each category is provided in Table 1.
Category 2: Benefits of RPM for Clinical Staff
For the benefits category, 3 main themes were identified as relevant (Table 2). The first theme was the improvement that RPM brings regarding workload and logistics as it allows for the definition of guidelines for more consistent care pathways. This also includes improvements in data management and analysis, which produces timely detection and treatment of conditions.
Table 2.
Overview of benefits of remote patient monitoring interventions for clinical staff.
| Theme and description | Studies | |
| Workload and logistics | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Health care resources | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Patient relationship | ||
|
|
|
|
|
||
The second theme was health care resources, which can be operated more effectively with the reduction of in-hospital visits and stays and the possibility of extending coverage of care.
Finally, patient relationship can be improved by increasing satisfaction and convenience of care.
Category 3: Risk-Reduction Strategies Regarding RPM for Clinical Staff
This category is about strategies to overcome and minimize the challenges that RPM interventions bring about to clinical staff (Table 3). For ease of reference, we refer to risk-reduction strategies related to the introduction of RPM interventions as strategies. First, we listed strategies regarding planning and implementation of RPM interventions. Most of the included studies (14/21, 67%) mentioned the value of involving the relevant stakeholders in these processes to understand their needs and the repercussions of the introduction of the RPM intervention on their workflow. Stakeholders’ involvement and participatory approaches were also deemed useful to assess the resources necessary for RPM interventions, the possible risks associated with them, and the need for possible changes to the implementation plans. Finally, training and establishment of protocols (regarding activities, communication, time, and resources) help in risk reduction during implementation and increase the chances of success and adoption.
Table 3.
Overview of risk-reduction strategies regarding remote patient monitoring (RPM) interventions for clinical staff.
| Theme and description | Studies | ||
| Planning and implementation | |||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
| Workload and logistics | |||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
| Technology | |||
|
|
|
||
|
|
|
|
|
|
|
|
||
|
|
|
||
|
|
|
||
| Data | |||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
|
|
aQoS: quality of service.
bEMR: electronic medical record.
Second, we listed strategies regarding workload and logistics. Several included studies (8/21, 38%) suggested the creation of new roles for nurses and teams for the remote care of patients, where specialists would be consulted only in special cases. Some strategies to avoid an increase in workload for nursing staff included facilitating collaboration between actors and helping them plan their tasks.
The third theme was technology, which should be user-friendly, interoperable with existing devices and systems, and allow for automatic data collection.
Finally, we identified the theme of data. To avoid the analysis of RPM data being burdensome for staff, smart systems based on customizable alerts were proposed to prevent resource overuse and the incidence of false alarms. These should include measurements from different devices or sources and be presented to the relevant staff in an actionable and understandable way to avoid extra time and burden.
Category 4: Methods to Measure and Quantify the Impact of RPM on Clinical Staff
This category presents the methods used to identify the impact of RPM interventions on clinical staff tasks and workflows. In total, 2 main themes were established (Table 4) based on the kind of measures of the impact of RPM interventions on staff being collected and analyzed using different methods. The first theme was time and activity analysis, which includes methods for measuring clinical staff time expenditure and workload in relation to existing activities and RPM interventions. These methods allow for a comparative analysis between the standard of care and the RPM intervention. Other possible quantifiable measures found in this category are the number of times certain resources are accessed or the time spent on certain tasks.
Table 4.
Overview of methods to measure and quantify the impact of remote patient monitoring (RPM) interventions on clinical staff.
| Theme and description | Studies | ||
| Time and activity analysis | |||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
|
|
| Satisfaction and experience analysis | |||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
||
|
|
|
|
|
The second theme was staff satisfaction and experience, which focuses on how RPM interventions are perceived by the staff and how the new tools and ways of working affect their behaviors. This theme includes subjective measures, such as those gathered through interviews and surveys, and more objective measures, such as measures of adherence to protocols or alert frequency.
Discussion
Principal Findings
RPM is presented as a useful tool to help patients feel safer and more empowered in their self-care during the perioperative period. In addition, health care institutions benefit from it by increasing the efficiency in the use of their resources, both physical (such as beds and monitors) and human (clinical staff). In deciding on the adoption of RPM interventions, considering the impact on and perceptions of clinical staff is crucial as the success of these interventions is based on their cooperation and comprehension. As users and providers of remote perioperative care, clinical staff need to be comfortable and willing to adopt RPM interventions, which should not hinder their other tasks.
Overall, the main RPM-related problems found for clinical staff were related to undesirable changes in their workflow and lack of planning. In several included papers (11/21, 52%), the introduction of RPM led to a higher workload because of unforeseen tasks that emerged when the RPM intervention was implemented in the complex health care environment and not necessarily when the intervention was tested in controlled settings. In particular, tasks such as (remotely monitored) patient data analysis, remote alert response, and remote care reporting and billing were mentioned as sources of increased staff workload and disruptions in the usual care workflow. In addition, the time necessary for activities was often underestimated because of the lack of experience and knowledge of the clinical staff to perform some of the new tasks that RPM interventions created. Furthermore, problems were reported in relation to uncontemplated users as sometimes it was unclear who was in charge of these new tasks, the assigned actor was not the adequate one, or they depended on the assistance of a third party. Problems regarding the difficulty in use and functioning of RPM tools were also described. This was mainly due to lack of knowledge or training, technical malfunctions, or legal issues where the new services conflicted with the current systems. Although it is true that these problems might be temporary and limited to the initial introduction of RPM interventions, it is still important to assess and address them as they do have an impact on the workflow and might cause the intervention implementation to fail before familiarization and adaptation are even possible. Furthermore, it is important to consider initial workflow problems as adaptation strategies and coping mechanisms adopted by staff to overcome these problems might in themselves generate structural issues. For example, when new tasks are introduced by RPM interventions without a clear indication of who is responsible for them, the available actors will feel compelled to take over, adding to their daily workload.
Most of the reported benefits for clinical staff related to the improvement in monitoring and data analysis, resulting in better resource management and clinical outcomes. Even though most staff members agree on the advantages these interventions bring in terms of better follow-up of patients and resource allocation, they are still concerned about the extra workload they face.
Regarding best practices and risk-reduction strategies, most of the included studies (18/21, 86%) mentioned the need to strengthen the implementation process of RPM interventions through better planning and improved stakeholder involvement. This way, clinical staff can provide a better overview of their pre-existing work routines and needs so that the new interventions can be better integrated and adapted to their usual workflow rather than the other way around. Other strategies involved establishing protocols to guide the interventions’ use and operations and providing the necessary training to avoid uncertainty and prepare staff. Finally, several included studies (10/21, 48%) stressed the importance of interoperability and ensuring compatibility between the new RPM interventions and the existing tools and processes used by the staff to prevent double work or the emergence of conflicts in the recorded patient data.
Moreover, it is recommended that RPM-related interfaces be user-friendly and tested in the context to reduce time spent on training and possible technical problems. Enhancing staff’s understanding of and familiarity with the tools can increase their willingness toward their adoption as technology will be perceived as an enhancer and not as an obstacle.
The included studies reported recommendations for best practices and risk-reduction strategies for most of the staff-related problems and challenges mentioned in connection with RPM interventions. It is important to note that these solutions address problems that represent major barriers to RPM implementation in the present. Therefore, adopting them more consistently in RPM research and practice represents a way to maximize the capability of RPM to deliver real-world results in health care services in the future.
Figure 2 shows the connections between themes and categories. Here, we can see how some of the identified themes were not present in all the categories. Notably, there are problems that lack specific recommendations in the literature, such as those related to health care resources. Reimbursement schemes prioritizing in-hospital care constitute a largely unaddressed challenge complicated by the complexity of the context and the different types of stakeholders involved. This affects the commitment and motivation of clinical staff toward RPM interventions as it is not always clear how the extra or new work will be reimbursed. In addition, there are currently few answers on how to increase funding for RPM interventions (Table 1). This is a big challenge, as RPM interventions may not clearly present benefits justifying their relatively high expenses, especially in the short term.
There is still room for improvement in ways to manage incoming alerts so that they do not create interruptions and annoyance among staff while ensuring timely responses. Another open challenge is related to providing a collaborative environment between the different staff members involved in patient care and defining clear roles so as to divide RPM-related tasks effectively and avoid confusion. In addition, there are opportunities to improve the devices and systems that collect, analyze, and communicate patient data. This includes the possibility of using data for more informed or automatized decisions that consider multiple data sources, thus avoiding biases, false positives, and incorrect inputs.
Most of the methods used to assess the impact of RPM interventions on staff-related workflows were qualitative and subjective, including interviews, questionnaires, and observations. Few reported studies (7/21, 33%) included the collection of quantitative measures such as tracking the time invested in using the interventions. This is characterized as an opportunity for improvement in RPM-related research as quantitative impact measures would help assess resource use and, therefore, better evaluate the overall interventions. Furthermore, quantitative measures could unlock the possibility of meaningful comparisons across different interventions and contexts. Some of these more quantitative or objective measures could be anxiety levels using existing scales, as proposed by Jukic et al [42].
However, there is still not enough research on methods to track RPM-related workload quantitatively. Examples of RPM interventions in fields other than perioperative care can be useful in this regard. For example, in tele–intensive care units and the remote monitoring of cardiovascular implantable electronic devices, diverse methods have been deployed to measure staff workload [43-46] by, for example, time-motion studies [47,48]. In these interventions, systems automatically record use time while an observer also tracks the nurses and annotates the duration of RPM-related activities. This has reportedly helped researchers identify the most time-consuming aspects of RPM-related workflow and find bottlenecks and weaknesses to improve designs and implementation plans. These tele–intensive care unit and cardiovascular implantable electronic device remote monitoring research methods could be profitably translated to perioperative care. In general, research on RPM interventions [31,35] helps in understanding possible outcomes and identifying barriers, facilitators, and recommendations [30], which can guide the design and implementation stages of these interventions.
Further research should be dedicated to the quantification of resource use in RPM interventions—to standardize reimbursement policies—and the evaluation of the implementation of these strategies in different settings. Moreover, the time horizon of these studies should be extended to cover longer periods, as many relevant effects of RPM interventions cannot be observed in the short term - partly because of factors such as the staff learning curve.
Limitations
This scoping review has several limitations. The first is the diversity of RPM interventions examined as they might have different objectives, leading to variable results and problems. In addition, the results will be influenced by the initial state and environment in which the RPM intervention was introduced. As mentioned by Herdman [49], intervention benefits depend on the baseline, whereby an initial higher performance may lead to a comparatively smaller advantage. Moreover, these interventions were executed under different circumstances and environments, which might change the dynamics among the clinical staff. Additional limitations are derived from the differences in the methodology used in the included studies as the target variables and outcomes might not be comparable. Finally, most of the included studies (13/21, 62%) only considered short- and midterm impacts, whereas RPM interventions can have long-term effects that are decisive to assess their overall performance.
This review was also susceptible to risk of bias because of missing results. This risk is increased by our exclusive focus on articles in English, our use of 2 databases (PubMed and Embase), and our focus on a limited time frame (January 2015 to March 2021). Nonreporting bias risk is also likely to apply to this review as we noticed that only a small fraction of papers in the RPM domain reported any insight at all on the impact of the introduction of new interventions on staff workflow. Overall, in light of the aforementioned limitations and risks of bias, we recommend interpreting and using our contribution as an initial description of the types of workflow-related implications of RPM described in the current literature and not as an exhaustive overview.
Conclusions
Every day there are more studies that show the impact of RPM interventions given their increasing use in clinical practice and in perioperative care in particular. Most of these studies focus on the patient’s perspective and on clinical outcomes. In our scoping review, we presented an overview of the recent knowledge regarding clinical staff’s perspective, which reveals the possible problems and benefits that remote monitoring can bring. Further research regarding policy making and protocol standardization should be conducted to establish a more trustworthy analysis of RPM interventions.
Studies concerning the impact of RPM strategies on clinical staff workflows and dynamics should be clear about the study objective, the design, and the methods used to test the intervention. This will help future readers in assessing the overall performance of RPM interventions. Moreover, this can enable better comparative research and promote the establishment of valuable benchmarking and auditing systems.
Abbreviations
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews
- RPM
remote patient monitoring
Search strategy.
Footnotes
Conflicts of Interest: None declared.
References
- 1.de Farias FA, Dagostini CC, de Assunção Bicca Y, Falavigna VF, Falavigna A. Remote patient monitoring: a systematic review. Telemed J E Health. 2020 May;26(5):576–83. doi: 10.1089/tmj.2019.0066. [DOI] [PubMed] [Google Scholar]
- 2.Seto E. Cost comparison between telemonitoring and usual care of heart failure: a systematic review. Telemed J E Health. 2008 Sep;14(7):679–86. doi: 10.1089/tmj.2007.0114. [DOI] [PubMed] [Google Scholar]
- 3.Koopman RJ, Wakefield BJ, Johanning JL, Keplinger LE, Kruse RL, Bomar M, Bernt B, Wakefield DS, Mehr DR. Implementing home blood glucose and blood pressure telemonitoring in primary care practices for patients with diabetes: lessons learned. Telemed J E Health. 2014 Mar;20(3):253–60. doi: 10.1089/tmj.2013.0188. http://europepmc.org/abstract/MED/24350806 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Os-Medendorp H, Koffijberg H, Eland-de Kok PC, van der Zalm A, de Bruin-Weller MS, Pasmans SG, Ros WJ, Thio HB, Knol MJ, Bruijnzeel-Koomen CA. E-health in caring for patients with atopic dermatitis: a randomized controlled cost-effectiveness study of Internet-guided monitoring and online self-management training. Br J Dermatol. 2012 May;166(5):1060–8. doi: 10.1111/j.1365-2133.2012.10829.x. [DOI] [PubMed] [Google Scholar]
- 5.Ricci RP, Morichelli L, Santini M. Remote control of implanted devices through Home Monitoring technology improves detection and clinical management of atrial fibrillation. Europace. 2009 Jan;11(1):54–61. doi: 10.1093/europace/eun303.eun303 [DOI] [PubMed] [Google Scholar]
- 6.Anthony Jnr B. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. J Med Syst. 2020 Jun 15;44(7):132. doi: 10.1007/s10916-020-01596-5. http://europepmc.org/abstract/MED/32542571 .10.1007/s10916-020-01596-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atilgan K, Onuk BE, Köksal Coşkun P, Yeşi LG, Aslan C, Çolak A, Çelebi AS, Bozbaş H. Remote patient monitoring after cardiac surgery: the utility of a novel telemedicine system. J Card Surg. 2021 Nov;36(11):4226–34. doi: 10.1111/jocs.15962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belarmino A, Walsh R, Alshak M, Patel N, Wu R, Hu J. Feasibility of a mobile health application to monitor recovery and patient-reported outcomes after robot-assisted radical prostatectomy. Eur Urol Oncol. 2019 Jul;2(4):425–8. doi: 10.1016/j.euo.2018.08.016.S2588-9311(18)30135-4 [DOI] [PubMed] [Google Scholar]
- 9.Dirnberger J, Waisbren S. Efficacy of telehealth visits for postoperative care at the Minneapolis VA. Am J Surg. 2020 Sep;220(3):721–4. doi: 10.1016/j.amjsurg.2020.01.015.S0002-9610(20)30016-7 [DOI] [PubMed] [Google Scholar]
- 10.Symer MM, Abelson JS, Milsom J, McClure B, Yeo HL. A mobile health application to track patients after gastrointestinal surgery: results from a pilot study. J Gastrointest Surg. 2017 Sep;21(9):1500–5. doi: 10.1007/s11605-017-3482-2.10.1007/s11605-017-3482-2 [DOI] [PubMed] [Google Scholar]
- 11.van der Meij E, Huirne JA, Ten Cate AD, Stockmann HB, Scholten PC, Davids PH, Bonjer HJ, Anema JR. A perioperative eHealth program to enhance postoperative recovery after abdominal surgery: process evaluation of a randomized controlled trial. J Med Internet Res. 2018 Jan 02;20(1):e1. doi: 10.2196/jmir.8338. https://www.jmir.org/2018/1/e1/ v20i1e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baniasadi T, Ghazisaeedi M, Hassaniazad M, Niakan Kalhori SR, Shahi M, Esmaeili M. Surgical patients follow-up by smartphone-based applications: a systematic literature review. Stud Health Technol Inform. 2020 Jun 23;271:85–92. doi: 10.3233/SHTI200079.SHTI200079 [DOI] [PubMed] [Google Scholar]
- 13.Mehta SJ, Hume E, Troxel AB, Reitz C, Norton L, Lacko H, McDonald C, Freeman J, Marcus N, Volpp KG, Asch DA. Effect of remote monitoring on discharge to home, return to activity, and rehospitalization after hip and knee arthroplasty: a randomized clinical trial. JAMA Netw Open. 2020 Dec 01;3(12):e2028328. doi: 10.1001/jamanetworkopen.2020.28328. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.28328 .2774354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shah M, Douglas J, Carey R, Daftari M, Smink T, Paisley A, Cannady S, Newman J, Rajasekaran K. Reducing ER visits and readmissions after head and neck surgery through a phone-based quality improvement program. Ann Otol Rhinol Laryngol. 2021 Jan;130(1):24–31. doi: 10.1177/0003489420937044. [DOI] [PubMed] [Google Scholar]
- 15.Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, Thompson RH, O'Neil DA, Hamilton RL, Gardner MR, Bundrick M, Jenkins SM, Pruthi S, Frank I, Gettman MT. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015 Oct;68(4):729–35. doi: 10.1016/j.eururo.2015.04.002.S0302-2838(15)00304-8 [DOI] [PubMed] [Google Scholar]
- 16.Forbes RC, Rybacki DB, Johnson TB, Hannah-Gillis A, Shaffer D, Hale DA. A cost comparison for telehealth utilization in the kidney transplant waitlist evaluation process. Transplantation. 2018 Feb;102(2):279–83. doi: 10.1097/TP.0000000000001903. [DOI] [PubMed] [Google Scholar]
- 17.Carayon P, Cartmill R, Hoonakker P, Hundt AS, Karsh BT, Krueger D, Snellman ML, Thuemling TN, Wetterneck TB. Human factors analysis of Work™ow in health information technology implementation. In: Carayon P, editor. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety. 2nd ed. Boca Raton, FL, USA: CRC Press; 2016. pp. 536–51. [Google Scholar]
- 18.Hignett S, Jones EL, Miller D, Wolf L, Modi C, Shahzad MW, Buckle P, Banerjee J, Catchpole K. Human factors and ergonomics and quality improvement science: integrating approaches for safety in healthcare. BMJ Qual Saf. 2015 Apr;24(4):250–4. doi: 10.1136/bmjqs-2014-003623. http://qualitysafety.bmj.com/lookup/pmidlookup?view=long&pmid=25715799 .bmjqs-2014-003623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 20.Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas JA, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 6.3. London, UK: Cochrane; 2022. [Google Scholar]
- 21.Harsha P, Paul JE, Chong MA, Buckley N, Tidy A, Clarke A, Buckley D, Sirko Z, Vanniyasingam T, Walsh J, McGillion M, Thabane L. Challenges with continuous pulse oximetry monitoring and wireless clinician notification systems after surgery: reactive analysis of a randomized controlled trial. JMIR Med Inform. 2019 Oct 28;7(4):e14603. doi: 10.2196/14603. https://medinform.jmir.org/2019/4/e14603/ v7i4e14603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Das A, Faxvaag A, Svanæs D. The impact of an eHealth portal on health care professionals' interaction with patients: qualitative study. J Med Internet Res. 2015 Nov 24;17(11):e267. doi: 10.2196/jmir.4950. https://www.jmir.org/2015/11/e267/ v17i11e267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davoody N, Hägglund M. Care Professionals' perceived usefulness of eHealth for post-discharge stroke patients. In: Hoerbst A, Hackl WO, de Keizer N, Prokosch HU, Hercigonja-Szekeres M, de Lusignan S, editors. Exploring Complexity in Health: An Interdisciplinary Systems Approach. Amsterdam, The Netherlands: IOS Press; 2016. pp. 589–93. [Google Scholar]
- 24.Ke JX, George RB, Wozney L, Chorney JL. Patient-centred perioperative mobile application in cesarean delivery: needs assessment and development. Obstet Anesth Dig. 2020 Dec;40(4):185–6. doi: 10.1097/01.aoa.0000719500.35419.e1. doi: 10.1097/01.aoa.0000719500.35419.e1. [DOI] [PubMed] [Google Scholar]
- 25.Leppla L, Mielke J, Kunze M, Mauthner O, Teynor A, Valenta S, Vanhoof J, Dobbels F, Berben L, Zeiser R, Engelhardt M, De Geest S, SMILe study team Clinicians and patients perspectives on follow-up care and eHealth support after allogeneic hematopoietic stem cell transplantation: a mixed-methods contextual analysis as part of the SMILe study. Eur J Oncol Nurs. 2020 Apr;45:101723. doi: 10.1016/j.ejon.2020.101723.S1462-3889(20)30003-X [DOI] [PubMed] [Google Scholar]
- 26.Sanger PC, Hartzler A, Lordon RJ, Armstrong CA, Lober WB, Evans HL, Pratt W. A patient-centered system in a provider-centered world: challenges of incorporating post-discharge wound data into practice. J Am Med Inform Assoc. 2016 May;23(3):514–25. doi: 10.1093/jamia/ocv183. http://europepmc.org/abstract/MED/26977103 .ocv183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Timmerman JG, Dekker-van Weering MG, Stuiver MM, Groen WG, Wouters MW, Tönis TM, Hermens HJ, Vollenbroek-Hutten MM. Ambulant monitoring and Web-accessible home-based exercise program during outpatient follow-up for resected lung cancer survivors: actual use and feasibility in clinical practice. J Cancer Surviv. 2017 Dec;11(6):720–31. doi: 10.1007/s11764-017-0611-6. http://europepmc.org/abstract/MED/28396993 .10.1007/s11764-017-0611-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wiadji E, Mackenzie L, Reeder P, Gani JS, Carroll R, Smith S, Frydenberg M, O'Neill CJ. Utilization of telehealth by surgeons during the COVID 19 pandemic in Australia: lessons learnt. ANZ J Surg. 2021 Apr;91(4):507–14. doi: 10.1111/ans.16693. http://europepmc.org/abstract/MED/33634949 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parkes RJ, Palmer J, Wingham J, Williams DH. Is virtual clinic follow-up of hip and knee joint replacement acceptable to patients and clinicians? A sequential mixed methods evaluation. BMJ Open Qual. 2019 Mar 1;8(1):e000502. doi: 10.1136/bmjoq-2018-000502.bmjoq-2018-000502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothgangel A, Kanera I, van den Heuvel R, Wientgen M, Jamin G, Lenssen T, Braun S. Physiotherapists' clinical use and acceptance of a telemonitoring platform during anterior cruciate ligament rehabilitation: a prospective clinical study. Disabil Rehabil Assist Technol. 2022 Feb;17(2):184–91. doi: 10.1080/17483107.2020.1774810. [DOI] [PubMed] [Google Scholar]
- 31.Makhni MC, Riew GJ, Sumathipala MG. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020 Jul 01;102(13):1109–15. doi: 10.2106/JBJS.20.00452.00004623-202007010-00002 [DOI] [PubMed] [Google Scholar]
- 32.Downey CL, Croft J, Buckley H, Randell R, Brown JM, Jayne DG. Trial of Remote Continuous versus Intermittent NEWS monitoring after major surgery (TRaCINg): protocol for a feasibility randomised controlled trial. Pilot Feasibility Stud. 2018 Jun 11;4:112. doi: 10.1186/s40814-018-0299-z. https://pilotfeasibilitystudies.biomedcentral.com/articles/10.1186/s40814-018-0299-z .299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McMullen C, Nielsen M, Firemark A, Price PM, Nakatani D, Tuthill J, McMyn R, Odisho A, Meyers M, Shibata D, Gilbert S. Designing for impact: identifying stakeholder-driven interventions to support recovery after major cancer surgery. Support Care Cancer. 2018 Dec;26(12):4067–76. doi: 10.1007/s00520-018-4276-0. http://europepmc.org/abstract/MED/29876832 .10.1007/s00520-018-4276-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sharif F, Rahman A, Tonner E, Ahmed H, Haq I, Abbass R, Asinger S, Sbai M. Can technology optimise the pre-operative pathway for elective hip and knee replacement surgery: a qualitative study. Perioper Med (Lond) 2020 Nov 16;9(1):33. doi: 10.1186/s13741-020-00166-0. https://perioperativemedicinejournal.biomedcentral.com/articles/10.1186/s13741-020-00166-0 .10.1186/s13741-020-00166-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brophy PD. Overview on the challenges and benefits of using telehealth tools in a pediatric population. Adv Chronic Kidney Dis. 2017 Jan;24(1):17–21. doi: 10.1053/j.ackd.2016.12.003.S1548-5595(16)30153-7 [DOI] [PubMed] [Google Scholar]
- 36.Dunphy E, Hamilton FL, Spasić I, Button K. Acceptability of a digital health intervention alongside physiotherapy to support patients following anterior cruciate ligament reconstruction. BMC Musculoskelet Disord. 2017 Nov 21;18(1):471. doi: 10.1186/s12891-017-1846-0. https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-017-1846-0 .10.1186/s12891-017-1846-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sousa P, OLiveira M, Sousa J. Impact of computerized information systems in the global nurses’ workload: nurses’ perceptions and real-time. Proceedings of the 3rd IPLeiria's International Health Congress; IPLeiria-IHC '16; May 6-7, 2016; Leiria, Portugal. 2016. p. 27. [Google Scholar]
- 38.Augestad KM, Sneve AM, Lindsetmo RO. Telemedicine in postoperative follow-up of STOMa PAtients: a randomized clinical trial (the STOMPA trial) Br J Surg. 2020 Apr;107(5):509–18. doi: 10.1002/bjs.11491. [DOI] [PubMed] [Google Scholar]
- 39.Richards HS, Blazeby JM, Portal A, Harding R, Reed T, Lander T, Chalmers KA, Carter R, Singhal R, Absolom K, Velikova G, Avery KN. A real-time electronic symptom monitoring system for patients after discharge following surgery: a pilot study in cancer-related surgery. BMC Cancer. 2020 Jun 10;20(1):543. doi: 10.1186/s12885-020-07027-5. https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07027-5 .10.1186/s12885-020-07027-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Semple JL, Evans HL, Lober WB, Lavallee DC. Implementing mobile health interventions to capture post-operative patient-generated health data. Surg Infect (Larchmt) 2019 Oct;20(7):566–70. doi: 10.1089/sur.2019.151. [DOI] [PubMed] [Google Scholar]
- 41.Jansson MM, Harjumaa M, Puhto AP, Pikkarainen M. Healthcare professionals' proposed eHealth needs in elective primary fast-track hip and knee arthroplasty journey: a qualitative interview study. J Clin Nurs. 2019 Dec;28(23-24):4434–46. doi: 10.1111/jocn.15028. [DOI] [PubMed] [Google Scholar]
- 42.Jukic T, Ihan A, Petek Šter M, Strojnik V, Stubljar D, Starc A. Adherence of female health care workers to the use a Web-based tool for improving and modifying lifestyle: prospective target group pilot study. J Med Internet Res. 2020 Aug 14;22(8):e19500. doi: 10.2196/19500. https://www.jmir.org/2020/8/e19500/ v22i8e19500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cady R, Finkelstein S, Lindgren B, Robiner W, Lindquist R, VanWormer A, Harrington K. Exploring the translational impact of a home telemonitoring intervention using time-motion study. Telemed J E Health. 2010 Jun;16(5):576–84. doi: 10.1089/tmj.2009.0148. http://europepmc.org/abstract/MED/20575725 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Papavasileiou LP, Forleo GB, Panattoni G, Schirripa V, Minni V, Magliano G, Bellos K, Santini L, Romeo F. Work burden with remote monitoring of implantable cardioverter defibrillator: is it time for reimbursement policies? J Cardiovasc Med (Hagerstown) 2013 Feb;14(2):114–9. doi: 10.2459/JCM.0b013e328354e3e1. [DOI] [PubMed] [Google Scholar]
- 45.Ricci RP, Morichelli L, D'Onofrio A, Calò L, Vaccari D, Zanotto G, Curnis A, Buja G, Rovai N, Gargaro A. Manpower and outpatient clinic workload for remote monitoring of patients with cardiac implantable electronic devices: data from the HomeGuide Registry. J Cardiovasc Electrophysiol. 2014 Nov;25(11):1216–23. doi: 10.1111/jce.12482. [DOI] [PubMed] [Google Scholar]
- 46.Ricci RP, Morichelli L, D'Onofrio A, Calò L, Vaccari D, Zanotto G, Curnis A, Buja G, Rovai N, Gargaro A. Effectiveness of remote monitoring of CIEDs in detection and treatment of clinical and device-related cardiovascular events in daily practice: the HomeGuide Registry. Europace. 2013 Jul;15(7):970–7. doi: 10.1093/europace/eus440. http://europepmc.org/abstract/MED/23362021 .eus440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang Z, Mazabob J, Weavind L, Thomas E, Johnson TR. A time-motion study of registered nurses' workflow in intensive care unit remote monitoring. AMIA Annu Symp Proc. 2006;2006:759–63. http://europepmc.org/abstract/MED/17238443 .86310 [PMC free article] [PubMed] [Google Scholar]
- 48.Tang Z, Weavind L, Mazabob J, Thomas EJ, Chu-Weininger MY, Johnson TR. Workflow in intensive care unit remote monitoring: a time-and-motion study. Crit Care Med. 2007 Sep;35(9):2057–63. doi: 10.1097/01.ccm.0000281516.84767.96. [DOI] [PubMed] [Google Scholar]
- 49.Herdman TH, Burgess LP, Ebright PR, Paulson SS, Powell-Cope G, Hancock H, Wada E, Cadman EC. Impact of continuous vigilance monitoring on nursing workflow. J Nurs Adm. 2009 Mar;39(3):123–9. doi: 10.1097/NNA.0b013e31819894c8.00005110-200903000-00007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.


