Abstract
Study Design:
Prospective case series.
Objective:
SSPSS (single step pedicle screw system) was developed for minimally invasive spine surgery. We performed this study to report on safety, workflow, and our initial clinical experience with this novel technique.
Methods:
The prospective study was conducted on patients who underwent pedicle screw fixation between October 2017 and April 2018 using a novel single step 3D navigated pedicle screw system for MIS. Outcome measurements were obtained from intraoperative computerized tomography. The images were evaluated to determine pedicle wall penetration. We used a grading system to assess the severity of the pedicle wall penetration. Breaches were classified as grade 1 (<2 mm), grade 2 (2-4 mm), or grade 3 (<4 mm), 1 and as cranial, caudal, medial, and lateral.
Results:
Our study includes 135 screws in 24 patients. SSPSS eliminated K-wires and multiple steps traditionally necessary for MIS pedicle screw insertion. The median time per screw was 2.45 minutes. 3 screws were corrected intraoperatively. Pedicle wall penetration occurred in 14 screws (10%). Grade 1 breaches occurred in 4 screws (3%) and grade 2 breaches occurred in 10 screws (7%). Lateral breaches were observed more often than medial breaches. The accuracy rate in our study was 90% (Grade 0 breach). No revision surgeries were needed and no complications occurred.
Conclusions:
Our study suggests that SSPSS could be a safe, accurate, and efficient tool. Our accuracy rate is comparable to that found in the literature.
Keywords: accuracy, minimally invasive, screw placement, navigation, 3D-NAV, pedicle screw, thoracolumbosacral pedicle screw system, time, SSPSS, MIS, MISS
Introduction
Minimally invasive spine (MIS) surgery has witnessed rapid progression within the last decade, especially in regard to pedicle screw systems. The benefits are less damage to the soft tissues, less loss of blood, fewer postoperative complications, and a reduced length of hospitalization.1,2 Pedicle screw placement in an open or minimally invasive surgery is a technically demanding procedure. Placing the screws in the pedicles is ideal because it limits paraspinal soft tissue trauma while also giving strength to the screw’s purchase. The incidence of screw misplacement varies from 5 percent to 40 percent in the literature.3,4-6
Malpositioning of pedicle screws can lead to with increased rate of pseudarthrosis, adjacent segment disease, neural injury or irritation, and CSF leaks. Lateral and medial breaches endanger neural elements,7-10 with medial breaches being more likely to encroach on the nerve due to its the proximity to the nerve root in the medial and inferomedial aspects of the pedicle. Lateral breaches occur more often in order to avoid the cranial facet joint. The identification of pedicle screw positioning is better appreciated with CT imaging than fluoroscopy. 11 Traditional MIS pedicle screw systems are cumbersome, requiring multiple steps and instruments including placement of Jamshidi needles, K-wires, power drill, tap, and finally screw placement. In order to facilitate workflow, we previously described a technique that eliminated the use of K-wires and several of these steps by using one navigated guide tube through which the drill, tap, and screw could be used. 12
Companies have developed navigable single step pedicle screw systems (SSPSS) for mini-open or percutaneous placement. Compared to conventional pedicle screw systems, SSPSS eliminates the need for K-wires and combines docking, tapping, and screw placement into one step with a single device that needs to be registered once for intraoperative navigation. Thus, this system even further facilitate the workflow with the navigated guide tube. Furthermore, advances in 3D image guidance allows the surgeon to track the trajectory and anatomic location of the pedicle screw in real time.
Given the relatively recent introduction of SSPSS, studies describing the accuracy of pedicle screw placement do not exist. In this manuscript, we describe our institutional experience with SSPSS and discuss the technical procedure, radiological outcomes, and timing considerations in a series of 135 screw placements.
Methods
Data Collection
A prospective single center study of patients who underwent MIS surgery for lumbar degenerative disease was performed. Indications for surgery included spondylolisthesis with or without neurogenic claudication, foraminal stenosis, or facet arthropathy with degenerative dynamic instability. Patients who were eligible for ALIF, TLIF, LLIF, and PLIF were included. The procedures included thoracolumbar stabilizations.
Informed consent was obtained from all patients and 3D-NAV surgical treatment was performed. All patients had an intraoperative CT scan using the AIRO (BrainLAB AG, Munich, Germany) that was then co-registered with 3D navigation software (BrainLAB AG, Munich, Germany). The Viper Prime System (DePuy Spine, Raynham, MA, USA) was the SSPSS used for all surgeries. All surgeries were performed by the senior author between October 2017 and April 2018. Clinical and intraoperative data were collected from the patients’ electronic medical record and radiologic data were collected from intraoperative CT scans. The time per screw was calculated from calibration until insertion. The time was then divided by the numbers of placed screws.
Surgical Technique
After general endotracheal anesthesia and placement of neurophysiologic monitoring needles, patients were positioned prone onto a modified Jackson table. Intraoperative continuous electromyography (EMG) monitoring was routinely used in all cases to avoid potential nerve root injury and neural compression. Excess skin and fat were taped down to ensure stabilization. This was important especially in overweight patients to prevent skin shift during navigation. The patient was prepped and draped in the usual fashion. A reference array was fixed into the iliac crest using Steinmann pins. The intraoperative CT scan was performed and registered with navigation software. The navigation wand was used to identify the optimal trajectory for pedicle screw insertion at each level on each side. The skin was marked over these areas. Typically, one skin incision can be made on each side with separate fascial openings per level. The SSPSS device with navigation star was registered and calibrated. A short stylet was exposed at the tip of the screw and used to dock on the lateral aspect of the superior articulating facet of the level to be instrumented. Gentle malleting ensures that the stylet was engaged in bone. The required trajectory was aligned then the self-tapping screw was inserted. It was critical to hold the SSPSS device in a manner that allows the navigation to be facing the camera of the navigation station to maintain the ideal trajectory. Once the pedicle screw enters the vertebral body, the stylet was retracted. There was no need for extra drilling or taping. At this point, a final intraoperative CT scan was performed to evaluate the placement of all screws. Once confirmed, the navigation software can estimate the length of the rod from the newly acquired CT which is then passed subfascially. Caps were placed and finally tightened. After the screw and rod construct was secured, morselized allograft was packed below the rods for arthrodesis. Autograft from the facet joints (in the case of TLIF) or iliac crest contralateral to the reference array can also be harvested under 3D navigation (Figure 1A-C, Figure 2).
Figure 1.
A, Picture showing a SSPSS navigated screw inserter. B and C, The navigated stylet can be extended to a maximum of 5 mm beyond the tip of the screw.
Figure 2.
Drawing showing the OR setup with patient positioning, intraoperative CT, anesthesia, and navigation unit.
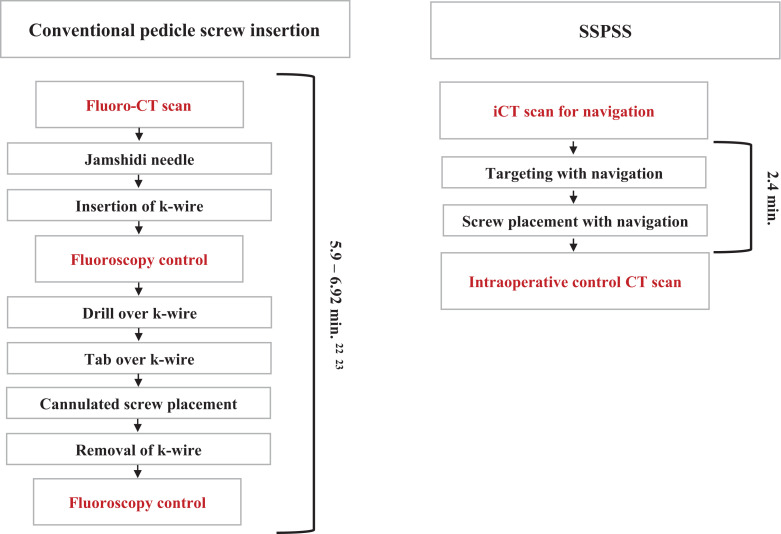
The regular workflow using SSPSS is very straight forward and includes the following steps (Figure 3):
Skin incision is marked using navigation guidance.
Manual verification of navigation accuracy using the BrainLAB pointer by identifying and palpating a transverse process at a distance from the reference array.
The navigated screw with the screw driver are calibrated.
After inserting the screw, the screws were test-stimulated with an extended electrode probe. A threshold of 8 mA is used to consider screw re-positioning.
A final intraoperative CT is done while leaving the navigation reference in place in case further adjustment of the instruments or decompression is needed.
The wound is generously irrigated and washed after meticulous hemostasis is performed. Osteostimulative bone graft is packed under the rod. Local anesthesia is used to infiltrate the muscle and the wound is closed.
Figure 3.
Flow chart illustrating the typical steps of traditional pedicle screw insertion in comparison to SSPSS.
Radiological Evaluation
We performed a double-blinded evaluation of all intraoperative CT scans. The evaluation was performed by a senior spine surgeons and a spine fellow. The 3D-NAV system was used to determine the accuracy of the pedicle screws. The images were reconstructed in the axial, sagittal and coronal planes. The CT scans were evaluated using the grading system described by Mirza et al. 1 previously:
Grade 0: perfect screw placement. The screw is within the cortical margins; grade 1: perforation of 0-2 mm; grade 2: perforation distance between 2 and 4 mm; grade 3: perforation distance greater than 4 mm (Figure 4A and B, Figure 5). The accuracy of each individual screw was graded. Lateral breach is the distance between the lateral cortex of the pedicle and the outer lateral margin of the screw. Medial breach is the distance between the medial cortex of the pedicle and the medial outer margin of the screw (Figure 4A and B). Coronal and caudal breach is the distance of the pedicle to the outer margin of the screw.
Figure 4.
A, Drawing showing the measuring technique of a medial and lateral breach. B, The breach measurement techniques in the axial, coronal and sagittal plane. Axial CT scan: breach grade 2 right T9 screw. Coronal CT scan: breach grade 2 right T10 screw. Sagittal CT scan: without any breach in the sagittal scan.
Figure 5.
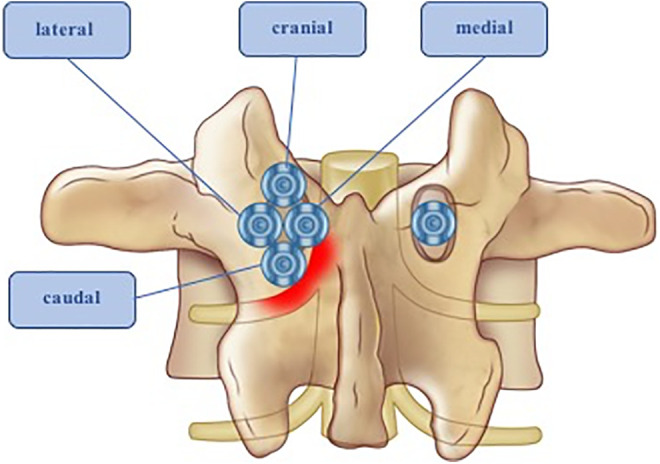
Drawing illustrating the 4 type of breaches (cranial, caudal, medial, and lateral) on the left side. Medial and caudal breaches are more likely to impinge the exiting nerve root. The screw on the ride side is correctly placed.
Statistics
All values are expressed as mean ± SD. All statistical evaluations were performed with SPSS Version 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0, NY: IBM Corp.). Figures were designed using GraphPad Prism (version 5.0 for Mac OS X, GraphPad Software, La Jolla California USA, http://www.graphpad.com).
Results
The median age of our 24 patients was 71 years (range 36–84 years) and the average BMI was 27 kg/m2. Spinal canal stenosis was present in 23 patients (96%), 15 patients (63%) had spondylolisthesis, 8 patients (33%) had degenerative disc disease, and 7 (29%) had previous surgery. Between 1 and 5 levels were treated (1 level: n = 14 (58%), 2 levels: n = 4 (17%), 3 levels: n = 4 (17%), 4 levels: n = 1 (4%), 5 levels: n = 1 (4%)) (Table 1). Patients had pedicle screw placement in conjunction with interbody fusions, of which 5 (21%) were ALIF with posterior fixation, 13 (54%) were TLIF, 4 (17%) were LLIF, 2 (8%) were PLIF (Figure 6). Screws were placed in thoracic and lumbar spine (2 screws in T9, 4 screws in T10, 2 screws in T11, 2 screws in T12, 5 screws in L1, 9 screws in L2, 11 screws in L3, 30 screws in L4, 43 screws in L5, 26 screws in S1, 1 screw in S2). The data was analyzed according to age, sex, BMI, procedure, level, side, breach direction and screw size. We can conclude, that none of the subgroups are predicting factor for breaches.
Table 1.
Summary of Characteristics and Demographics
| Characteristics | Value |
|---|---|
| Female : male | 8:16 |
| Median age in years (range) | 71 (36-84) |
| BMI (kg/m2) | 27 |
| Treated levels | |
| 1 level | 14 (58 %) |
| 2 levels | 4 (17 %) |
| 3 levels | 4 (17 %) |
| 4 levels | 1 (4 %) |
| 5 levels | 1 (4 %) |
| Primary diagnosis | |
| Stenosis | 23 (96 %) |
| Listhesis | 15 (63 %) |
| DDD | 8 (33 %) |
| Previous surgery | 7 (29 %) |
Figure 6.
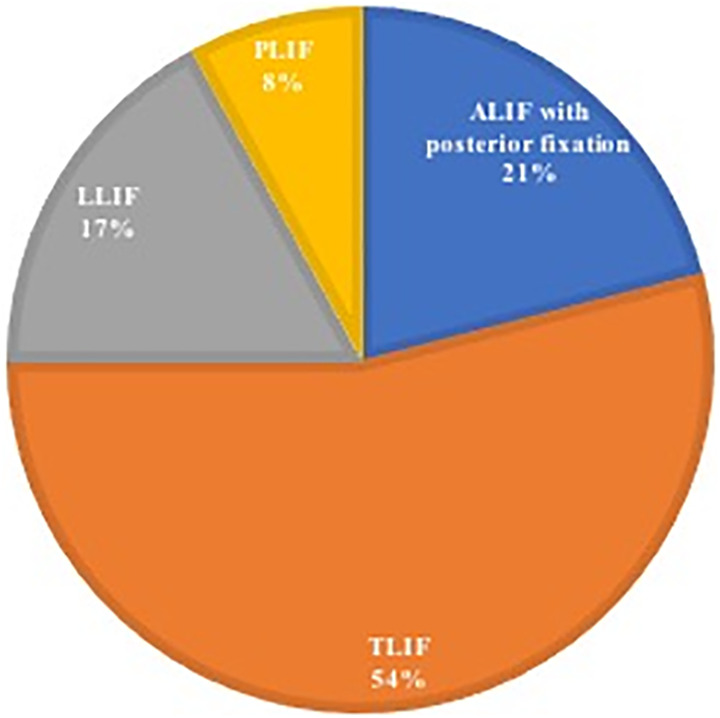
The approaches performed by the senior author in percent.
Three screws out of 135 screws were repositioned intraoperatively. No revision surgeries were needed and no complications occurred. None of the patients reported complications in the 2 weeks postop visit. The median time per screw was 2.45 minutes (range 1.34 to 4.85 minutes). The time per screw was measured from calibration until finishing of the screw insertion (Table 2).
Table 2.
Type and Direction of Pedicle Breaches.
| Breach | Lateral | |||
|---|---|---|---|---|
| Medial | Cranial | Caudal | Total | |
| Grade 0 | - | - | - | 121 |
| Grade 1 | 2 | 0 | 2 | 4 |
| Grade 2 | 2 | 0 | 8 | 10 |
| Grade 3 | 0 | 0 | 0 | 0 |
| Time per screw (from calibration until finishing screw insertion) | 2.4 min | |||
Radiological Outcome
The 135 pedicle screws in our 24 patients were visualized on CT scans with the Dicom viewer (BrainLAB AG, Munich, Germany) to enable an accuracy assessment. Based on the grading system described by Mirza et al. 1 121 (90%) were considered grade 0, 4 (3%) were grade 1, and 10 (7%) were grade 2. No grade 3 breach occurred in our study. For screws grades 1 and 2, we differentiated between medial and lateral breaches. Screw perforation occurred most frequently in the lateral direction, with 10 screws (7%) demonstrating a lateral breach and 4 screws (3%) demonstrating a medial breach. All lateral breaches were caudal. No cranial breach occurred. Lateral breaches were usually accepted in order to prevent violation of the facet joint. Misplacement rates were correlated to the spinal level and there was no statistical significance found.
Discussion
Previous studies confirmed that non-navigated screws were more likely to require intraoperative correction than navigated screws. 13 In 2012, a meta-analysis of 20 studies showed that in 8539 screws the overall pedicle screw perforation risk for navigation was 6% compared to 15% for conventional insertion. The meta-analysis did not reveal a significant difference in total operative time and estimated blood loss when comparing the 2 modalities. 14
A worldwide survey in 2013 on the use of navigation in spine surgery revealed that 3D navigation implementation into clinical practice is difficult. The main concerns of the respondents were safety, time and workflow disturbance, and costs. 15
The use of intraoperative CT has a significant advantage because malpositioned screws can be identified and replaced before concluding the operation. Otherwise, postoperative neurologic symptoms and imaging findings would require a second, revision operation. The development and the widespread availability of 3D navigation software technology and MIS surgery within the last decade have increased the precision of hardware implantation while decreasing the amount of radiation to surgical staff.14-16 These advances have improved the safety of MIS surgery through efficient and reproducible workflows. 17
We performed this study to evaluate the accuracy of minimally invasive lumbar pedicle screw placement using SSPSS and CT based computer-assisted navigation. Our hypothesis was that SSPSS would show equal accuracy compared to values published in the literature while decreasing the time taken per screw placement. Ninety percent of our screws were grade 0 meaning no breach occurred. If patients with grade 1 breaches (breaches less than 2 mm) are included, then the accuracy rate increases to 93%. These results are comparable to a previous meta-analysis which described a median accuracy rate of navigated pedicle screw placement of 95.2%. 12 Also, a meta-analysis from our center revealed that navigated pedicle screws were less likely to breach compared to conventional insertion. 14 Our accuracy rate was similar to the rate we found in recent studies.12,17-19 No revision surgery was necessary and no neurologic or vascular complications occurred. No pain related to Steinman pins occurred.
Screw perforation occurs most frequently in the lateral direction which happens in order to avoid the cranial facet joint. This finding correlates with other previous studies. 20
The median time per screw was 2.45 minutes. Other studies in the literature report average time per screw in navigated pedicle screws ranging from 2.6 (navigated guide tubes) to 6.92 minutes (perc screw) per screw 4,12,21,22 (Table 3). Compared to these studies, SSPSS needs less time per screw.
Table 3.
Summary of the Time per Pedicle Screw in MISS.
| Journal | No. of patients | No. of screws | Time per screw | Measurement information | Accuracy rate | Instrumentation | Navigation |
|---|---|---|---|---|---|---|---|
| Biomed Res Int. | 33 | 144 | 2.6 min. | NR | 0.986 | navigated guide tube, MIS-TLIF | yes |
| Spine | 72 | 300 | 5.9 min. | NR | 0.95 | perc pedicle screws with k-wire, LLIF, OLIF | no |
| World Neurosurgery | 117 | 390 | 3.1 min. | time was measured from “pointing” (pedicle identification through the navigated guide tube) to pedicle screw stimulation | 0.99 | navigated guide tube | yes |
| JNS Spne | 28 | 100 | 6.92 min. | calculated from initial skin incision to final screw positioning | 0.967 | MIS k-wireless percutaneous screw system: probe, dilator, screw insertion |
no |
| NR = not recorded |
Another advantage for the surgical team is the reduced radiation exposure with SSPSS. Conventional fluoroscopy is associated with significant radiation exposure to the patient, the team, and the surgeon.22-26 Yet, one significant factor is the cost for an intraoperative O-arm or CT scanner. However, this needs to be weighed against the cost reduction from earlier hospital discharges, decreased surgical duration, hospital readmissions and lower likelihood for a second surgery.
Another advantage of SSPSS is the elimination of K-wires used with traditional MIS approaches, K-wires pose a risk of visceral or vascular injury as well as unintended migration. Multiple instruments such as drill guide, awl and before, tap, screw placement are needed. This can cause disruption in the workflow and also time consuming.27-33
The primary downside of this system is that the sharpness of the stylet which can traumatize tissue when being docked initially or potentially cause injuries to surrounding structures if the screw placement deviates from ideal trajectory. Another downside is that since there are no intermediate steps, redirecting or replacing a screw after it has been placed in its initiate trajectory may be challenging because a screw tract has already been made. However, we illustrated a case of a successful replacement of a screw proving it can be done.
In our observation the use of SPSS in MIS surgery is faster, safer, easier, and reduces radiation exposure to the OR staff. Successful screw placement can even be achieved in challenging cases with narrow pedicles due to bone erosion or in densely sclerotic bone. This makes SSPSS usable for a wide spectrum of instrumented MIS surgeries.
However, we encountered 3 challenging cases related to either hard cortical bone that the screw system could not penetrate or bony anatomy so delicate that we decided to modify the insertion technique in order to maximize screw accuracy. Below we present the 3 cases:
Challenging Case Presentation 1
History and presentation
66-year-old female who presents with a large L3-4 schwannoma with severe compression of the thecal sac. The patient was offered resection and stabilization. The tumor has eroded the bony anatomy which resulted in scalloping of the bone and thinning of the pedicle. This made placement of the MIS screws challenging.
Surgical procedure
The reference array for the navigation system was placed on the spinous process of L4. On the right side, the L3 pedicle was thinned out with very little bone and low margin of error. In order to maximize accuracy, the pedicle trajectory was drilled using a navigated 3 mm BrainLAB drill guide and stored in the navigation system (Figure 7A and B). This was then followed using the SSPSS. After screw placement, the tumor was resected successfully and the fusion was performed.
Figure 7.
A, Intraoperative CT scan of 66-year-old female patient with very slim L3 pedicle on the right side due to tumor growth. B, Postoperative X-ray showing correct placement of instrumentation.
Challenging Case Presentation 2
History and presentation
66-year-old male patient who presents with degenerative scoliosis, post-laminectomy loss of lordosis and foraminal narrowing.
Surgical procedure
Due to extensive bony overgrowth, the pedicle could not be penetrated. The navigated awl-tip tap was used to break the cortex of this very hard sclerotic bone and the trajectory is stored in the Brainlab system (Figure 8). After this procedure, we were able to insert the navigated screw. All screws were placed and an intraoperative CT scan showed good placement of all screws and bilateral rods.
Figure 8.
Navigated awl-tip tap penetrate hard sclerotic bone.
Challenging Case Presentation 3
History and presentation
83-year-old female patient who had a previous L4-S1 TLIF and presents with lumbar spinal stenosis and post-laminectomy syndrome with severe disc degeneration and deformity in the lumbar spine.
Surgical procedure
We performed an L1-2, L2-3, L3-4 lateral transpsoas discectomy with cage placement followed by an extension of the pedicle screw implementation from L1-S1 using SSPSS.
In case a screw is misplaced, it is sometimes advantageous to leave it in place until a new trajectory is drilled for the corrected screw. With the use of the navigated awl-tip tap a new trajectory is drilled and stored in the BrainLAB system. Then the misplaced screw is removed and the new screw is placed (Figure 9 A-E).
Figure 9.
A, Intraoperative revision of misplaces SSPSS pedicle screw: Intraoperative control CT scan showed laterally misplaces right L1 pedicle screw. Decision was made to revise screw. The image shows planning of correct screw trajectory. B, Correct medial trajectory has been planned (blue screw). The navigated awl-tip tap is used to prepare screw hole. C, The placement of correct SSPSS screw. D and E, Control CT showing correctly placed screw in L1. The misplaced lateral screw has been removed.
Limitation
The primary limitations of our study is that this is the experience of a single institution and it is the experience of one single surgeon. The navigation set-up time was not measured. We do not have long term outcome results and can therefore not report about fusion rates. A comprehensive cohort study with more patients to determine screw accuracy will be needed. However, our findings are comparable to the previously published studies.
Conclusion
In our case series Single Step Pedicle Screw System results in very low rates of pedicle screw breaches. Furthermore our investigation suggests that the placement time per screw is reduced. There were no complications in the 135 screws that were placed. In our study the workflow of SSPSS seems more efficient than traditional MIS pedicle screw insertion. SSPSS was also used safely for our challenging cases. We suspect that SSPSS greatly expands navigation toward the era of “Total Navigation.”
Abbreviation
- DDD
degenerative disc disease
- ALIF
anterior lumbar interbody fusion
- TLIF
transforaminal lumbar interbody fusion
- LLIF
lateral lumbar interbody fusion
- PLIF
posterior lumbar interbody fusion
- CSF
cerebral spinal fluid
- MISS
minimally invasive spine surgery
- SSPSS
Single step pedicle screw system
Footnotes
Authors’ Note: IRB/ethics committee approval: Protocol number 0806009851.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Louis Chang received financial from Zimmer, Biomet; Roger Härtl received financial from Brainlab, Nuvasive.
ORCID iD: Franziska A. Schmidt, MD  https://orcid.org/0000-0002-4237-0910
https://orcid.org/0000-0002-4237-0910
Rodrigo Navarro-Ramirez, MD  https://orcid.org/0000-0003-2543-9063
https://orcid.org/0000-0003-2543-9063
Christoph Wipplinger, MD  https://orcid.org/0000-0002-9001-6932
https://orcid.org/0000-0002-9001-6932
References
- 1.Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurgical Focus. 2009;27(3):E9. [DOI] [PubMed] [Google Scholar]
- 2.McAfee PC, Phillips FM, Andersson G, et al. Minimally invasive spine surgery. Spine. 2010;35(26 Suppl): S271–S273. [DOI] [PubMed] [Google Scholar]
- 3.Mirza SK, Wiggins GC, Kuntz CT, et al. Accuracy of thoracic vertebral body screw placement using standard fluoroscopy, fluoroscopic image guidance, and computed tomographic image guidance: a cadaver study. Spine. 2003;28(4):402–413. [DOI] [PubMed] [Google Scholar]
- 4.Navarro-Ramirez R, Lang G, Lian X, et al. Total navigation in spine surgery; a concise guide to eliminate fluoroscopy using a portable intraoperative computed tomography 3-dimensional navigation system. World Neurosurgery. 2017;100:325–335. [DOI] [PubMed] [Google Scholar]
- 5.Shin BJ, Njoku IU, Tsiouris AJ, Hartl R. Navigated guide tube for the placement of mini-open pedicle screws using stereotactic 3D navigation without the use of K-wires: technical note. J Neurosurg Spine. 2013;18(2):178–183. [DOI] [PubMed] [Google Scholar]
- 6.Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine. 1996;21(11):1320–1324. [DOI] [PubMed] [Google Scholar]
- 7.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15(1):11–14. [DOI] [PubMed] [Google Scholar]
- 8.Laine T, Makitalo K, Schlenzka D, Tallroth K, Poussa M, Alho A. Accuracy of pedicle screw insertion: a prospective CT study in 30 low back patients. Eur Spine J. 1997;6(6):402–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verma R, Krishan S, Haendlmayer K, Mohsen A. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J. 2010;19(3):370–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ahmadian A, Deukmedjian AR, Abel N, Dakwar E, Uribe JS. Analysis of lumbar plexopathies and nerve injury after lateral retroperitoneal transpsoas approach: diagnostic standardization. J Neurosurg Spine. 2013;18(3):289–297. [DOI] [PubMed] [Google Scholar]
- 11.Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR. Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res. 2014;472(6):1727–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lian X, Navarro-Ramirez R, Berlin C, et al. Total 3D Airo(R) navigation for minimally invasive transforaminal lumbar interbody fusion. BioMed Res Int. 2016;5027340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Learch TJ, Massie JB, Pathria MN, Ahlgren BA, Garfin SR. Assessment of pedicle screw placement utilizing conventional radiography and computed tomography: a proposed systematic approach to improve accuracy of interpretation. Spine. 2004;29(7):767–773. [DOI] [PubMed] [Google Scholar]
- 14.Shin BJ, James AR, Njoku IU, Hartl R. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. J Neurosurg Spine. 2012;17(2):113–122. [DOI] [PubMed] [Google Scholar]
- 15.Hartl R, Lam KS, Wang J, Korge A, Kandziora F, Audige L. Worldwide survey on the use of navigation in spine surgery. World Neurosurgery. 2013;79(1):162–172. [DOI] [PubMed] [Google Scholar]
- 16.Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM. Computed tomography-guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine. 2012;37(8): E473–478. [DOI] [PubMed] [Google Scholar]
- 17.Schlenzka D, Laine T, Lund T. Computer-assisted spine surgery: principles, technique, results and perspectives [in German]. Der Orthopade. 2000;29(7):658–669. [DOI] [PubMed] [Google Scholar]
- 18.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine. 2007;32(3): E111–120. [DOI] [PubMed] [Google Scholar]
- 19.Fraser J, Gebhard H, Irie D, Parikh K, Hartl R. Iso-C/3-dimensional neuronavigation versus conventional fluoroscopy for minimally invasive pedicle screw placement in lumbar fusion. Minim Invasive Neurosurg. 2010;53(4):184–190. [DOI] [PubMed] [Google Scholar]
- 20.Torres J, James AR, Alimi M, Tsiouris AJ, Geannette C, Hartl R. Screw placement accuracy for minimally invasive transforaminal lumbar interbody fusion surgery: a study on 3-D neuronavigation-guided surgery. Global Spine J. 2012;2(3):143–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blizzard DJ, Thomas JA. MIS single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: feasibility and perioperative results. Spine. 2018;43(6):440–446. [DOI] [PubMed] [Google Scholar]
- 22.Spitz SM, Sandhu FA, Voyadzis JM. Percutaneous “K-wireless” pedicle screw fixation technique: an evaluation of the initial experience of 100 screws with assessment of accuracy, radiation exposure, and procedure time. J Neurosurg Spine. 2015;22(4):422–431. [DOI] [PubMed] [Google Scholar]
- 23.Lee K, Lee KM, Park MS, Lee B, Kwon DG, Chung CY. Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine. 2012;37(14):1240–1244. [DOI] [PubMed] [Google Scholar]
- 24.Bandela JR, Jacob RP, Arreola M, Griglock TM, Bova F, Yang M. Use of CT-based intraoperative spinal navigation: management of radiation exposure to operator, staff, and patients. World Neurosurg. 2013;79(2):390–394. [DOI] [PubMed] [Google Scholar]
- 25.Wood MJ, Mannion RJ. Improving accuracy and reducing radiation exposure in minimally invasive lumbar interbody fusion. J Neurosurg Spine. 2010;12(5):533–539. [DOI] [PubMed] [Google Scholar]
- 26.Abdullah KG, Bishop FS, Lubelski D, Steinmetz MP, Benzel EC, Mroz TE. Radiation exposure to the spine surgeon in lumbar and thoracolumbar fusions with the use of an intraoperative computed tomographic 3-dimensional imaging system. Spine. 2012;37(17): E1074–E1078. [DOI] [PubMed] [Google Scholar]
- 27.Myles RT, Fong B, Esses SI, Hipp JA. Radiographic verification of pedicle screw pilot hole placement using Kirshner wires versus beaded wires. Spine. 1999;24(5):476–480. [DOI] [PubMed] [Google Scholar]
- 28.Fomekong E, Pierrard J, Danse E, Tombal B, Raftopoulos C. An unusual case of ureteral perforation in minimally invasive pedicle screw instrumentation: case report and review of the literature. World Neurosurgery. 2018;111:28–35. [DOI] [PubMed] [Google Scholar]
- 29.Minic L, Lepic M, Novakovic N, Mandic-Rajcevic S. Symptomatic migration of a Kirschner wire into the spinal canal without spinal cord injury: case report. J Neurosurg Spine. 2016;24(2):291–294. [DOI] [PubMed] [Google Scholar]
- 30.Chung T, Thien C, Wang YY. A rare cause of postoperative paraplegia in minimally invasive spine surgery. Spine. 2014;39(3): E228–E230. [DOI] [PubMed] [Google Scholar]
- 31.Tubbax H, Hendzel P, Sergeant P. Cardiac perforation after Kirschner wire migration. Acta Chir Belg. 1989;89(6):309–311. [PubMed] [Google Scholar]
- 32.Hargreaves DG, Drew SJ, Eckersley R. Kirschner wire pin tract infection rates: a randomized controlled trial between percutaneous and buried wires. J Hand Surg (Edinburgh, Scotland). 2004;29(4):374–376. [DOI] [PubMed] [Google Scholar]
- 33.Bezer M, Aydin N, Erol B, Lacin T, Guven O. Unusual migration of K-wire following fixation of clavicle fracture: a case report [in Turkish]. Ulus Travma Acil Cerrahi Derg. 2009;15(3):298–300. [PubMed] [Google Scholar]