Abstract
Study Design:
Retrospective cohort study.
Objectives:
Vertebral body sliding osteotomy (VBSO) has previously been reported as a technique to decompress ossification of the posterior longitudinal ligament (OPLL) by translating the vertebral body anteriorly. This study aimed to evaluate the radiological and clinical efficacies of VBSO and clarify the surgical indications of VBSO for treating myelopathy caused by OPLL.
Methods:
Ninety-seven patients with symptomatic OPLL-induced cervical myelopathy treated with VBSO or laminoplasty who were followed up for more than 2 years were retrospectively reviewed. Cervical alignment, range of motion, fusion, modified K-line (mK-line) status, and minimum interval between ossified mass and mK-line (INT(min)), and the Japanese Orthopaedic Association (JOA) score were assessed. Patients in the VBSO group were compared with those who underwent laminoplasty.
Results:
Cervical lordosis and INT(min) significantly increased in the VBSO group. All patients in the VBSO group assessed as mK-line (-) preoperatively were assessed as mK-line (+) postoperatively. However, in the LMP group, the mK-line status changed from (+) preoperatively to (−) postoperatively in 3 patients. Final JOA score (p = 0.02) and JOA score improvement (p = 0.01) were significantly higher in the VBSO group. JOA recovery ratio (p = 0.03) and proportion of patients with a recovery rate ≥50% were significantly higher in the VBSO group (p < 0.01).
Conclusions:
VBSO is an effective surgical option for OPLL-induced myelopathy, demonstrating favorable neurological recovery and lordosis restoration with low complication rates. It is best indicated for kyphotic alignment, OPLL with a high space-occupying ratio, and OPLL involving ≤3 segments.
Keywords: anterior cervical corpectomy and fusion, cervical alignment, K-line, laminoplasty, ossification of posterior longitudinal ligament, vertebral body sliding osteotomy
Introduction
Ossification of the posterior longitudinal ligament (OPLL) is a common cause of cervical myelopathy that warrants surgical management. 1 Laminoplasty is a surgical method widely applied for multi-level cervical OPLL for which favorable clinical outcomes have been reported.2,3 However, laminoplasty achieves spinal cord decompression through a posterior shift of the cord, which makes it a poor option for patients with cervical kyphosis and significant compression due to a high OPLL canal-occupying ratio. 4
For multi-level OPLL patients with kyphotic alignment, anterior cervical corpectomy and fusion (ACCF) is superior to laminoplasty. 5 ACCF directly decompresses the spinal cord by removing the OPLL mass, and its success is independent of cervical alignment. 6 However, ACCF for OPLL is demanding and requires perioperative management of troublesome complications, including cerebrospinal leaks and graft-related complications. 7 The authors of this study previously reported a novel technique, vertebral body sliding osteotomy (VBSO), as a replacement for ACCF in the treatment of OPLL myelopathy.8-11 In VBSO, the vertebral body is translated anteriorly to widen the spinal canal, minimizing the need for direct removal of the ossified mass.8-10 It has fewer complications as it minimizes direct separation of OPLL from the dura and has better ability to restore cervical lordosis than ACCF.8-10
Previous studies have reported the safety and efficacy of VBSO. Although the clinical significance and indications of ACCF and laminoplasty have been reported, the significance of VBSO as a surgical strategy to manage OPLL and its indications have not been thoroughly discussed.5,12-17 Therefore, in this study, we aimed to clarify the clinical significance and establish the indications of VBSO for the treatment of OPLL-induced cervical myelopathy by demonstrating clinical and radiographic results.
Methods
Patient Characteristics and Study Design
In total, 118 patients who underwent VBSO or laminoplasty for multi-level OPLL between January 2012 and November 2017 were retrospectively reviewed. Patients who met the following criteria were excluded: underwent surgery for degenerative cervical myelopathy; treated with other surgical procedures such as laminectomy and fusion, or combined anterior/posterior surgery; underwent a revision operation; and followed up for less than 24 months. The study was approved by the institutional review board of our institute. The requirement for informed consent was waived owing to the retrospective nature of this study.
The surgical method was selected based on the number of OPLL-affected segments, cervical alignment, and modified K-line (mK-line) state (Figure 1).5,18-20 VBSO was indicated in the following cases: ≤3 involved segments, kyphotic alignment, mK-line (-), and patients with a neck pain visual analog scale score ≥5 who were not appropriate candidates for laminoplasty (VBSO group). 21 Laminoplasty was indicated in the following cases: involvement of >3 segments, lordotic alignment, mK-line (+); finally, laminoplasty was also performed in patients with borderline mK-line determination and C2–3 segment involvement (laminoplasty (LMP) group). Application of VBSO was limited to cases involving ≤3 segments since anterior interbody fusion of more than 4 levels would increase the risk of pseudarthrosis and retropharyngeal hematoma. 22 Surgical method selection and surgery were performed by a single surgeon.
Figure 1.
Flow diagram of the patient selection process. OPLL, ossification of posterior longitudinal ligament; n. number; ACDF, anterior cervical discectomy and fusion; VBSO, vertebral body sliding osteotomy; mKline, modified K-line.
Data Collection
Patient clinical characteristics and radiological data were collected from medical charts. Japanese Orthopaedic Association (JOA) scores were recorded before surgery and at the final follow-up. JOA score recovery rate (%) was calculated as follows: (postoperative score−preoperative score) × 100/(17−preoperative score). 23
Radiological measurements were performed by 2 spine fellowship–trained independent reviewers. Cervical lordosis was measured in the lateral view in the neutral position on the basis of the angle between the lines passing through the lower margin of the C2 and C6 or C7 vertebrae. Cervical range of motion (ROM) was measured as the change in the angle between the lower margins of C2 and C7 on dynamic (flexion and extension) radiographs. The canal-occupying ratio was measured on preoperative axial computed tomography (CT). The mK-line state was determined on sagittal T1 MRI images by placing a line between the center of C2 and the C7 spinal canal. 20 The mK-line was assessed as (-) when the OPLL mass crossed the mK-line and as (+) when it did not. The minimum interval of the spinal cord (INT(min)) was measured as the minimum interval between the mK-line and the ossified mass causing compression (Figure 2).20,24 Preoperative and postoperative INT(min) were measured at the same level. For patients in the VBSO group, fusion was assessed using the following criteria: interspinous motion (ISM) <1 mm on 150% magnified flexion/extension lateral dynamic radiograph 25 and bone bridging on CT images assessed 12 months postoperatively. 26 Adjacent segments with disc height changes or osteophyte formation at the 1-year follow-up were identified as adjacent segment degeneration. 27
Figure 2.
Radiological measurements. (A) Measurement of the canal-occupying ratio. A, Thickness of ossified mass at the level of greatest canal narrowing. B, Anteroposterior diameter of the spinal canal. (B) Modified K-line (mK-line) was defined as the line connecting the midpoints of the spinal cord at C2 and C7.
Surgical Technique
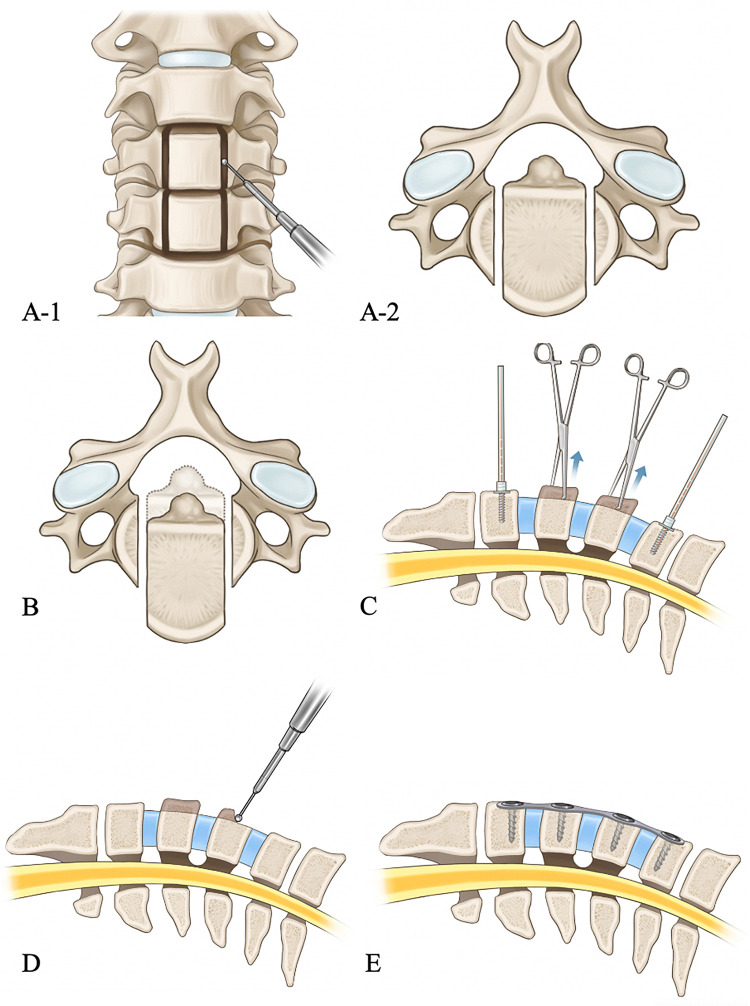
VBSO was performed via the standard Smith-Robinson approach. After exposure of the indicated levels, a multi-level discectomy was performed. The posterior longitudinal ligament was resected at the uppermost and lowermost disc levels. Next, 2 longitudinal 2-mm-wide slits were made using a high-speed burr through the base of the uncinate process. The posterior cortex of each slit was removed using a Kerrison punch. Freely mobilized vertebral bodies were grasped with Allis forceps. Gentle anterior traction forces were applied to the vertebral bodies. After adequate decompression was achieved with anterior sliding, interbody cages packed with local auto bone grafts were inserted into the disc space. An anterior cervical plate was added for reinforcement, and additional anterior translation was induced with screw tightening through mobilized vertebral bodies (Figure 3).8,10
Figure 3.
Technical description of vertebral body sliding osteotomy. (A) Two lateral slits are made using a high-speed burr at the base of the uncinate process. (B) Anterior translation of the vertebral body with ossification of the posterior longitudinal ligament mass with gentle traction. (C) While holding the vertebral body in an anteriorly translated position, interbody cages are inserted. A slight distraction force was applied with a Casper pin distractor to allow control of the vertebral body position. (D) A burr is used to remove the anterior part of the translated vertebral body. (E) The anterior plate is applied for additional stability.
For patients in the LMP group, a single-door laminoplasty with centerpiece mini-plate fixation (Medtronic, Minneapolis, MN, USA) was performed. The laminae were opened in the direction of the main symptoms.
Statistical Analyses
Categorical variables were analyzed using chi-square test, while continuous variables were analyzed using Student’s t-test. Paired t-test was used to analyze changes in postoperative values from the preoperative values. Logistic regression and Pearson’s correlation analyses were performed to identify factors associated with neurological recovery. Interobserver and intraobserver agreements were assessed using intraclass correlation coefficient (ICC) and Kappa coefficient. All data management and analyses were performed using SPSS version 21.0 software (SPSS, Inc., Chicago, IL, USA). P-values < 0.05 were considered significant.
Results
Of the 48 patients who underwent VBSO, 40 were followed up for more than 24 months and included in the VBSO group (29 [72.5%] men; mean age, 58.6 ± 10.9 years; follow-up rate, 83.3%). Of the 70 patients who underwent laminoplasty, 57 were followed up for more than 24 months and included in the LMP group (44 men [77.2%]; mean age, 62.2 ± 9.9 years; follow-up rate, 81.4%) (Table 1).
Table 1.
Patient Characteristics.
| VBSO | LMP | P value | |
|---|---|---|---|
| Number | 40 | 57 | |
| Follow-up (m) | 35.56 ± 12.4 | 32.6 ± 11.3 | 0.23 |
| Age | 58.6 ± 10.9 | 62.2 ± 9.9 | 0.10 |
| Sex | 0.64 | ||
| Male | 29 (72.5%) | 44 (77.2%) | |
| Female | 11 (27.5%) | 13 (28.8%) | |
| DM | 8 (20.0%) | 11 (19.3%) | 1.00 |
| HTN | 13 (32.5%) | 19 (33.3%) | 1.00 |
| Malignancy | 2 (5.0%) | 0 (0%) | 0.17 |
| BMI | 25.9 ± 6.9 | 25.6 ± 2.7 | 0.70 |
| Current smokers | 7 (17.5%) | 7 (12.3%) | 0.56 |
| Operative factors | |||
| Operation time | 212.4 ± 34.7 | 157.7 ± 28.7 | <0.01* |
| Number of OPLL-involved levels | 2.6 ± 0.7 | 3.9 ± 1.3 | <0.01* |
| Canal occupying ratio (%) | 46.6 ± 11.3 | 40.6 ± 0.12 | 0.01* |
| Complications | |||
| Dural tear | 1 (2.5%) | 0 (0%) | 0.35 |
| Neurologic deterioration | 0 (0%) | 0 (0%) | - |
| Infection | 0 (0%) | 1 (1.7%) | 1.00 |
| Readmission | 0 (0%) | 1 (1.7%) | 1.00 |
| Reoperation | 0 (0%) | 0 (0%) | - |
BMI, body mass index; DM, diabetes mellitus; HTN, hypertension; LMP, laminoplasty; m, months.
OPLL, ossification of posterior longitudinal ligament; VBSO, vertebral body sliding osteotomy.
Age, BMI, and operative factors were analyzed by Student’s t-test; DM, HTN, malignancy, current smokers, and complications were analyzed by the chi-square test.
* P value < 0.05.
Age, sex, underlying disease, BMI, and smoking status did not significantly differ between the 2 groups. However, operation time was significantly longer in the VBSO group (p < 0.01), and a significantly higher number of OPLL-involved segments were involved in the LMP group (p < 0.01). The canal-occupying ratio was significantly higher in the VBSO group (p = 0.01). One patient in the VBSO group suffered a dural tear (2.5%), and 1 patient in the LMP group had a superficial wound infection treated with intravenous antibiotics (1.7%) (Table 1). A single case of dural tear occurred in the VBSO group during resection of the posterior longitudinal ligament and was managed by inserting a lumbar drain. Graft migration or dislodgement was not observed in the VBSO group. Fusion rates assessed by ISM were 67.5% 6 months postoperatively, 92.5% 12 months postoperatively, and 92.5% at the final follow-up in the VBSO group. The fusion rate assessed by bone bridging was 92.5%. Adjacent segmental degeneration was identified in 1 patient (2.5%) in the VBSO group.
The Kappa coefficients for intraobserver and interobserver reliability for mK-line status were 0.983 and 0.947, respectively. The ICCs of intraobserver and interobserver reliability for measurement of cervical lordosis and ROM were 0.968 and 0.945, respectively. The ICCs of intraobserver and interobserver reliability for measurement of canal-occupying ratio were 0.951 and 0.881, respectively.
Radiographic Results
Preoperative cervical lordosis was significantly lesser in the VBSO than in the LMP group (p = 0.02). However, cervical lordosis significantly increased in the VBSO group postoperatively (p < 0.01) but decreased in the LMP group (p < 0.01). Cervical lordosis was significantly greater in the VBSO group 12 months postoperatively (p < 0.01) and at the final follow-up (p < 0.01).
Preoperative ROM did not differ between groups (p = 0.29). The VBSO group exhibited greater ROM loss than the LMP group at all postoperative time points. Postoperative ROM was significantly higher in the LMP group at 12 months postoperatively (p < 0.01), although there was no significant difference at the final follow-up (p = 0.14) (Table 2).
Table 2.
Radiographic Results.
| VBSO | LMP | P value† | ||
|---|---|---|---|---|
| Cervical lordosis | Preoperative | |||
| Degrees | 5.7 ± 13.8 | 11.2 ± 8.0 | 0.02* | |
| Post op 12M | ||||
| Degrees | 12.0 ± 8.3 | 6.9 ± 8.5 | <0.01* | |
| Change | 6.3 ± 10.3 | -4.2 ± 7.2 | <0.01* | |
| P value‡ | <0.01* | <0.01* | ||
| Final follow-up | ||||
| Degrees | 11.6 ± 9.0 | 7.0 ± 7.4 | <0.01* | |
| Change | 5.6 ± 10.5 | -4.2 ± 7.9 | <0.01* | |
| P value‡ | <0.01* | <0.01* | ||
| Range of motion | Preoperative | |||
| Degrees | 38.5 ± 10.7 | 35.7 ± 14.2 | 0.29 | |
| Post op 12M | ||||
| Degrees | 19.9 ± 7.8 | 25.5 ± 12.2 | 0.01* | |
| Change | -18.6 ± 7.8 | -10.2 ± 9.8 | <0.01* | |
| P value‡ | <0.01* | <0.01* | ||
| Final follow-up | ||||
| Degrees | 20.2 ± 7.6 | 23.4 ± 12.2 | 0.14 | |
| Change | -18.8 ± 12.2 | -12.3 ± 10.3 | <0.01* | |
| P value‡ | <0.01* | <0.01* | ||
| INT(min) | Preoperative | |||
| Interval (mm) | 0.5 ± 2.6 | 2.6 ± 2.7 | <0.01* | |
| Post op 12M | ||||
| Interval (mm) | 6.1 ± 3.3 | 2.4 ± 2.8 | <0.01* | |
| Change | 5.6 ± 3.7 | -0.2 ± 1.4 | <0.01* | |
| P value‡ | <0.01* | <0.01* |
INT(min), minimum interval; LMP, laminoplasty; M, months; VBSO, vertebral body sliding osteotomy.
† Student’s t-test was used to compare 2 groups.
‡Paired t-test was used to compare preoperative and postoperative measurements.
* P value < 0.05.
In the VBSO group, 16 (40.0%) patients were assessed as mK-line (+) and 24 (60.0%) as mK-line (-) preoperatively. However, all patients were assessed as mK-line (+) 12 months postoperatively. In the LMP group, 51 (89.5%) patients were assessed as mK-line (+) and 6 (10.5%) as mK-line (-). Among the 51 patients who were assessed as mK-line (+) preoperatively, 3 (5.9%) were assessed as mK-line (-) postoperatively. All patients assessed as mK-line (-) preoperatively were also assessed as mK-line (-) postoperatively. The distribution of mK-line state demonstrated significant difference between the 2 groups both preoperatively (p < 0.01) and postoperatively (p < 0.01) (Table 3).
Table 3.
Assessment of mK-Line Status by Group.
| Preoperative | Postoperative | |||
|---|---|---|---|---|
| VBSO | (+) | 16 (40.0%) | (+) | 16 (40.0%) |
| (-) | 0 (0.0%) | |||
| (-) | 24 (60.0%) | (+) | 24 (60.0%) | |
| (-) | 0 (0.0%) | |||
| LMP | (+) | 51 (89.5%) | (+) | 48 (84.2%) |
| (-) | 3 (5.2%) | |||
| (-) | 6 (10.5%) | (+) | 0 (0.0%) | |
| (-) | 6 (10.5%) | |||
| P value | <0.01* | <0.01* | ||
LMP, laminoplasty; mK-line, modified kyphosis line; VBSO, vertebral body sliding osteotomy.
The chi-square test was used for analysis.
* P value < 0.05.
INT(min) was significantly smaller in the VBSO group preoperatively (p < 0.01). However, INT(min) increased significantly in the VBSO group and was significantly greater than that of the LMP group postoperatively (p < 0.01) (Table 2).
The canal-occupying ratio significantly improved from 46.6% ± 11.3% preoperatively to 13.3% ± 10.2% (range 0%–22.2%) postoperatively in the VBSO group (p < 0.01). Twenty-nine (72.5%) patients achieved complete canal decompression postoperatively, and 3 patients had a postoperative canal-occupying ratio higher than 20%.
JOA Score
The preoperative JOA scores did not differ significantly between the VBSO and LMP groups (p = 0.42). The JOA score significantly improved in the both groups. The JOA score at the final follow-up (p = 0.02) and JOA score improvements (p = 0.01) were significantly higher in the VBSO group (Table 4).
Table 4.
Comparison of JOA Score by Group.
| VBSO | LMP | P value† | ||
|---|---|---|---|---|
| JOA | Preoperative | |||
| Score | 13.4 ± 2.0 | 12.9 ± 3.1 | 0.42 | |
| Final follow-up | ||||
| Score | 15.1 ± 1.8 | 13.8 ± 1.9 | 0.02* | |
| Change | 1.7 ± 1.8 | 0.9 ± 1.3 | 0.01* | |
| P value‡ | <0.01* | <0.01* | ||
| Recovery rate (%) | 60.1 ± 38.4 | 42.4 ± 35.7 | 0.03* |
JOA, Japanese Orthopaedic Association; LMP, laminoplasty; VBSO, vertebral body sliding osteotomy.
† Student’s t-test was used to compare 2 groups.
‡Paired t-test was used to compare preoperative and postoperative measurements.
* P value < 0.05.
The recovery rate of JOA score was 60.1 ± 38.4% in the VBSO group and 42.4 ± 35.7% in the LMP group (p = 0.03) (Table 4). A significantly higher number of patients in the VBSO group had a recovery ratio ≥50% (52.5% vs 21.1%, p < 0.01). Multivariate logistic regression analysis demonstrated that a change in mK-line status from (-) to (+) (p < 0.01) and preoperative JOA score (p = 0.01) were significantly associated with a JOA recovery ratio ≥50% (Table 5). Correlation analysis demonstrated that the preoperative canal-occupying ratio was significantly negatively related with the final JOA score (r = -0.25, p = 0.01). No factors demonstrated a significant correlation with the JOA recovery rate.
Table 5.
Results of Logistic Regression Analysis.
| Univariate analysis | P value† |
|---|---|
| Age | 0.16 |
| Sex | 0.43 |
| BMI (kg/m2) | 0.06* |
| Preoperative JOA score | <0.01* |
| Smoking status | 0.26 |
| Preoperative lordosis | 0.65 |
| Preoperative ROM | 0.65 |
| Number of OPLL involved segments | 0.35 |
| Canal occupying ratio | 0.89 |
| mK-line conversion from (-) to (+) | <0.01* |
| Multivariate analysis | P value‡ |
| Preoperative JOA score | 0.01* |
| BMI | 0.43 |
| mK-line conversion from (-) to (+) | <0.01* |
BMI, body mass index; JOA, Japanese Orthopaedic Association; mK-line, modified kyphosis line; OPLL, ossification of posterior longitudinal ligament; ROM, range of motion.
† P value < 0.10 was considered statistically significant.
‡P value < 0.05 was considered statistically significant.
Subgroup Analysis With mK-Line (-) Patients
A subgroup analysis was performed for preoperatively mK-line (-) patients to further clarify the clinical impact of VBSO. Cervical lordosis significantly improved in the VBSO group (p < 0.01), but not in the LMP group (p = 0.14). Cervical lordosis at the final follow-up was significantly greater in the VBSO group (11.5 ± 6.5°) than in the LMP group (5.2 ± 8.2°; p = 0.04). ROM was significantly greater in the LMP group at the final follow-up (VBSO group, 20.3 ± 7.9; LMP group, 33.7 ± 12.3; p < 0.01).
The JOA score at the final follow-up was significantly higher in the VBSO group (15.4 ± 1.7°) than in the LMP group (11.8 ± 3.3°; p < 0.01). The JOA recovery ratio was higher in the VBSO group (51.5 ± 36.1%) than in the LMP group (21.7 ± 24.2%), although the result did not reach statistical significance (p = 0.07).
Discussion
Studies regarding surgical strategies for managing OPLL-induced cervical myelopathy demonstrated the advantages and disadvantages of anterior and posterior approaches.13-17 Cervical alignment, OPLL shape, and the canal-occupying ratio are factors considered in determining surgical approach.8,10,13 The anterior approach is usually preferred in kyphotic alignment with a high occupying ratio of OPLL of ≥60%.16,17
The K-line is a concept that includes both cervical alignment and the OPLL size. 18 It was originally reported to assess the feasibility of laminoplasty, and a K-line (-) status is reportedly a poor prognostic factor after laminoplasty. 18 The mK-line is a K-line measured on sagittal MRI that enables a more accurate visualization of pathologic segments and measures the minimum interval from the pathologic foci to the mK-line.20,24 The results of the present study demonstrated that VBSO, by translating the ossified mass anteriorly and restoring cervical lordosis, can switch an mK-line (-) status to an mK-line (+) status. Since VBSO involves multi-level anterior cervical discectomy and fusion, multiple lordotic shape interbody cages are inserted into the disc space. This would help restore the cervical lordosis and switch the mK-line status.8,9 However, laminoplasty is known to be associated with aggravation rather than improvement of kyphosis, which is also demonstrated in this study. 28 Considering previous studies that have demonstrated the importance of appropriate cervical lordosis in neurologic recovery, VBSO creates a more favorable environment for neurologic recovery than laminoplasty does (Figure 4).29,30
Figure 4.
Transition of mK-line status in vertebral body sliding osteotomy and laminoplasty. (A) Vertebral body sliding osteotomy shifted mK-line (−) status into (+) by increasing cervical lordosis and shifting the ossified mass anteriorly. (B) mK-line (+) status changed into (−) after laminoplasty due to postoperative kyphosis.
In this study, the canal-occupying ratio significantly improved in the VBSO group, with 72.5% (29/40) patients achieving complete canal decompression. JOA score improvement, recovery rate, and the proportion of patients achieving a recovery rate ≥50% were significantly higher in the VBSO group. Better neurological improvements in the VBSO group can be explained in 2 ways. First, although VBSO does not directly remove the OPLL mass, it more effectively separates the spinal cord from the OPLL mass as demonstrated by the increased INT(min). This is achieved by restoring cervical lordosis, conversion of mK-line (-) status to (+) and translating the ossified mass anteriorly. Koda et al. reported that K-line conversion from negative to positive is associated with better neurological outcomes. 31 Likewise, the results of the present study showed that conversion of mK-line status is associated with a recovery rate ≥50%. Second, since VBSO is a fusion procedure, ROM is eliminated at the pathologic segments. Segmental motion at the peak of the ossified mass is reportedly a poor prognostic factor of OPLL-induced myelopathy. 32 Eliminating movement at the pathologic segments has a protective effect on the spinal cord.5,13,16
The VBSO group demonstrated better JOA score recovery despite a higher space-occupying ratio and significant negative correlation between the final JOA score and the canal-occupying ratio. Many studies reported that anterior surgery is preferred to laminoplasty when the canal-occupying ratio is high, especially at an occupying ratio of ≥60%.13,14,17 The results of this study coincide with those of previous reports in that anterior decompression by VBSO is feasible in cases of OPLL with a high canal-occupying ratio.
Therefore, the advantages of VBSO demonstrated in this study are: effective restoration of cervical lordosis, favorable neurologic recovery, and feasibility in kyphotic alignment and OPLL mass with high canal-occupying ratio. ACCF is also a valuable option for treating OPLL in cases of kyphotic alignment and a K-line (-) status since it restores lordosis.5,10,11,16,33 It can also result in better neurologic recovery than laminoplasty, especially in cases with a canal-occupying ratio of ≥60%.13,14,16 Nevertheless, ACCF is associated with high complication rates of durotomy, cerebrospinal fluid leakage, dysphagia, pseudarthrosis, and graft migration.34,35 It is an especially challenging procedure in the presence of adhesions between the OPLL mass and the dura. 13 Although the “floating method” was introduced, wherein the OPLLs were thinned without direct detachment from the dura, dural tears remain relatively common in ACCF, and their incidence is reported to be up to 8-10%, significantly higher than that in laminoplasty.8,14,36 In contrast, because the VBSO technique minimizes the need for direct manipulation of the interspace between the OPLL and the dura mater or the complete removal of the involved vertebral bodies, it can significantly reduce the risk of dural tears.8-11 In this study, although VBSO was more extensive than laminoplasty as demonstrated by its longer operation time, only 1 case of dural tear and no cases of graft migration or extrusion were identified. The complication rate was not significantly different from that of laminoplasty. Furthermore, VBSO demonstrated a high fusion rate.
With advantages similar to that of ACCF and lower complication rates, surgeons can perform VBSO in the following indications: kyphotic alignment, a high canal-occupying ratio, and the involvement of 2-3 segments (Figure 5).7-13,16,17,37 Therefore, the clinical significance of VBSO for managing OPLL-induced myelopathy is that while it retains the previously known strength of anterior approach, it is much safer than the classic ACCF to thoroughly decompress the canal.8-11 Since VBSO demonstrates several similar advantages over laminoplasty with ACCF, it seems that advantages of anterior approach is not necessarily demonstrated by direct removal of the ossified mass, but also can be achieved by canal widening and restoration of lordosis.
Figure 5.
Illustrative case of a 60-year-old woman who underwent vertebral body sliding osteotomy, C4, C5. (A) Preoperative lateral radiograph demonstrating kyphotic alignment. (B) At 2 years after VBSO, alignment had changed to lordosis. Translation of the vertebral body of C4 and C5 were confirmed by comparing the location of the posterior cortex of the vertebral body. (C) The mK-line status was assessed as (-) preoperatively. (D) With restoration of lordosis and anterior translation of the ossified mass, the mK-line status was assessed as (+) at 1 year after VBSO. (E) Preoperative axial CT images demonstrating canal compromise caused by OPLL with a canal-occupying ratio of 61%. (F) Successful decompression identified on an axial CT image taken at 1 year postoperatively. Solid bone union identified on coronal (G) and sagittal (H) CT images taken at 1 year postoperatively. Japanese Orthopaedic Association score improved from 12 to 16.
OPLL progression is related to segmental motion.38-40 OPLL continually progress after laminoplasty, which is a motion-preserving operation. 38 As VBSO is a fusion procedure that eliminates segmental motion, OPLL progression would less likely cause narrowing of the spinal canal in long-term follow-up. 40 However, data regarding the long-term consequences of VBSO for more than 2 years are lacking; thus, further clarification is required.
This study has limitations. First, the indications of VBSO and laminoplasty were different and preoperative cervical lordosis, canal-occupying ratio, and number of involved segments were not identical between the 2 groups. The comparison with laminoplasty should only be considered as a reference because the results of this study are not sufficient to demonstrate the superiority of each procedure. However, the advantages and disadvantages of the anterior and posterior approaches are known, and we judged that it would be unethical to randomize the selection of operative procedures without considering which approach is suitable for each patient.17,22,36 Second, a subgroup analysis of those with a space-occupying ratio ≥60% was not performed. This is because 10 of 11 patients with a space-occupying ratio ≥60% were included in the VBSO group and only 1 patient was included in the LMP group. Although the space-occupying ratio was not a criterion for surgical method selection, OPLL with a high space-occupying ratio tended to be assessed as mK-line (-) status. Finally, the inherent bias of a retrospective study cannot be excluded.
Conclusions
The clinical impact of VBSO include low complication rates and the classically reported advantages of the anterior approach, including effectively restoring lordosis, inducing mK-line positivity, and facilitating favorable neurological recovery. VBSO is best indicated in cases of kyphotic sagittal alignment, high space-occupying ratios, and those involving ≤3 segments.
Footnotes
Authors’ Note: The submitted manuscript does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
No relevant financial activities outside the submitted work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sehan Park, MD  https://orcid.org/0000-0001-8959-8579
https://orcid.org/0000-0001-8959-8579
References
- 1.Matsunaga S, Sakou T, Taketomi E, Komiya S. Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg. 2004;100(3 Suppl Spine):245–248. [DOI] [PubMed] [Google Scholar]
- 2.Matsumoto M, Chiba K, Toyama Y. Surgical treatment of ossification of the posterior longitudinal ligament and its outcomes: posterior surgery by laminoplasty. Spine (Phila Pa 1976). 2012;37(5):E303–E308. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa Y, Chiba K, Matsumoto M, et al. Long-term results after expansive open-door laminoplasty for the segmental-type of ossification of the posterior longitudinal ligament of the cervical spine: a comparison with nonsegmental-type lesions. J Neurosurg Spine. 2005;3(3):198–204. [DOI] [PubMed] [Google Scholar]
- 4.Sodeyama T, Goto S, Mochizuki M, Takahashi J, Moriya H. Effect of decompression enlargement laminoplasty for posterior shifting of the spinal cord. Spine (Phila Pa 1976). 1999;24(15):1527–1531; discussion 1531-1522. [DOI] [PubMed] [Google Scholar]
- 5.Koda M, Mochizuki M, Konishi H, et al. Comparison of clinical outcomes between laminoplasty, posterior decompression with instrumented fusion, and anterior decompression with fusion for K-line (-) cervical ossification of the posterior longitudinal ligament. Eur Spine J. 2016;25(7):2294–2301. [DOI] [PubMed] [Google Scholar]
- 6.Liu H, Li Y, Chen Y, Wu W, Zou D. Cervical curvature, spinal cord MRIT2 signal, and occupying ratio impact surgical approach selection in patients with ossification of the posterior longitudinal ligament. Eur Spine J. 2013;22(7):1480–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li H, Dai LY. A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J. 2011;11(11):1049–1057. [DOI] [PubMed] [Google Scholar]
- 8.Lee DH, Riew KD, Choi SH, et al. Safety and efficacy of a novel anterior decompression technique for ossification of posterior longitudinal ligament of the cervical spine. J Am Acad Orthop Surg. 2020;28(8):332–341. [DOI] [PubMed] [Google Scholar]
- 9.Lee DH, Lee CS, Hwang CJ, Cho JH, Park JW, Park KB. Improvement in cervical lordosis and sagittal alignment after vertebral body sliding osteotomy in patients with cervical spondylotic myelopathy and kyphosis. J Neurosurg Spine. 2020;1–9. [DOI] [PubMed] [Google Scholar]
- 10.Lee DH, Cho JH, Lee CS, Hwang CJ, Choi SH, Hong CG. A novel anterior decompression technique (vertebral body sliding osteotomy) for ossification of posterior longitudinal ligament of the cervical spine. Spine J. 2018;18(6):1099–1105. [DOI] [PubMed] [Google Scholar]
- 11.Lee DH, Park S, Hong CG. A novel anterior decompression technique for kyphosis line (K-line) ossification of posterior longitudinal ligament (OPLL): vertebral body sliding osteotomy. J Spine Surg. 2020;6(1):196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Edwards CC, 2nd, Heller JG, Murakami H. Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine (Phila Pa 1976). 2002;27(11):1168–1175. [DOI] [PubMed] [Google Scholar]
- 13.Chen Z, Liu B, Dong J, et al. Comparison of anterior corpectomy and fusion versus laminoplasty for the treatment of cervical ossification of posterior longitudinal ligament: a meta-analysis. Neurosurg Focus. 2016;40(6):E8. [DOI] [PubMed] [Google Scholar]
- 14.Qin R, Chen X, Zhou P, Li M, Hao J, Zhang F. Anterior cervical corpectomy and fusion versus posterior laminoplasty for the treatment of oppressive myelopathy owing to cervical ossification of posterior longitudinal ligament: a meta-analysis. Eur Spine J. 2018;27(6):1375–1387. [DOI] [PubMed] [Google Scholar]
- 15.Liu X, Min S, Zhang H, Zhou Z, Wang H, Jin A. Anterior corpectomy versus posterior laminoplasty for multilevel cervical myelopathy: a systematic review and meta-analysis. Eur Spine J. 2014;23(2):362–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament. Part 2: advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976). 2007;32(6):654–660. [DOI] [PubMed] [Google Scholar]
- 17.Iwasaki M, Okuda S, Miyauchi A, et al. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament. Part 1: clinical results and limitations of laminoplasty. Spine (Phila Pa 1976). 2007;32(6):647–653. [DOI] [PubMed] [Google Scholar]
- 18.Fujiyoshi T, Yamazaki M, Kawabe J, et al. A new concept for making decisions regarding the surgical approach for cervical ossification of the posterior longitudinal ligament: the K-line. Spine (Phila Pa 1976). 2008;33(26):E990–E993. [DOI] [PubMed] [Google Scholar]
- 19.Yamazaki A, Homma T, Uchiyama S, Katsumi Y, Okumura H. Morphologic limitations of posterior decompression by midsagittal splitting method for myelopathy caused by ossification of the posterior longitudinal ligament in the cervical spine. Spine (Phila Pa 1976). 1999;24(1):32–34. [DOI] [PubMed] [Google Scholar]
- 20.Taniyama T, Hirai T, Yamada T, et al. Modified K-line in magnetic resonance imaging predicts insufficient decompression of cervical laminoplasty. Spine (Phila Pa 1976). 2013;38(6):496–501. [DOI] [PubMed] [Google Scholar]
- 21.Lau D, Winkler EA, Than KD, Chou D, Mummaneni PV. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: influence of cervical alignment on outcomes. J Neurosurg Spine. 2017;27(5):508–517. [DOI] [PubMed] [Google Scholar]
- 22.Lee HC, Chen CH, Wu CY, Guo JH, Chen YS. Comparison of radiological outcomes and complications between single-level and multilevel anterior cervical discectomy and fusion (ACDF) by using a polyetheretherketone (PEEK) cage-plate fusion system. Medicine (Baltimore). 2019;98(5):e14277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976). 2001;26(17):1890–1894; discussion 1895. [DOI] [PubMed] [Google Scholar]
- 24.Taniyama T, Hirai T, Yoshii T, et al. Modified K-line in magnetic resonance imaging predicts clinical outcome in patients with nonlordotic alignment after laminoplasty for cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2014;39(21):E1261–E1268. [DOI] [PubMed] [Google Scholar]
- 25.Song KS, Piyaskulkaew C, Chuntarapas T, et al. Dynamic radiographic criteria for detecting pseudarthrosis following anterior cervical arthrodesis. J Bone Joint Surg Am. 2014;96(7):557–563. [DOI] [PubMed] [Google Scholar]
- 26.Song KS, Chaiwat P, Kim HJ, Mesfin A, Park SM, Riew KD. Anterior cervical fusion assessment using reconstructed computed tomographic scans: surgical confirmation of 254 segments. Spine (Phila Pa 1976). 2013;38(25):2171–2177. [DOI] [PubMed] [Google Scholar]
- 27.Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17(2):79–85. [DOI] [PubMed] [Google Scholar]
- 28.Sakai K, Okawa A, Takahashi M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine (Phila Pa 1976). 2012;37(5):367–376. [DOI] [PubMed] [Google Scholar]
- 29.Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S149–S160. [DOI] [PubMed] [Google Scholar]
- 30.Smith JS, Lafage V, Ryan DJ, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: analysis of 56 preoperative cases from the AOSpine North America Myelopathy study. Spine (Phila Pa 1976). 2013;38(22 Suppl 1):S161–S170. [DOI] [PubMed] [Google Scholar]
- 31.Koda M, Furuya T, Saito J, et al. Postoperative K-line conversion from negative to positive is independently associated with a better surgical outcome after posterior decompression with instrumented fusion for K-line negative cervical ossification of the posterior ligament. Eur Spine J. 2018;27(6):1393–1400. [DOI] [PubMed] [Google Scholar]
- 32.Masaki Y, Yamazaki M, Okawa A, et al. An analysis of factors causing poor surgical outcome in patients with cervical myelopathy due to ossification of the posterior longitudinal ligament: anterior decompression with spinal fusion versus laminoplasty. J Spinal Disord Tech. 2007;20(1):7–13. [DOI] [PubMed] [Google Scholar]
- 33.Kim B, Yoon DH, Shin HC, et al. Surgical outcome and prognostic factors of anterior decompression and fusion for cervical compressive myelopathy due to ossification of the posterior longitudinal ligament. Spine J. 2015;15(5):875–884. [DOI] [PubMed] [Google Scholar]
- 34.Kimura A, Seichi A, Hoshino Y, et al. Perioperative complications of anterior cervical decompression with fusion in patients with ossification of the posterior longitudinal ligament: a retrospective, multi-institutional study. J Orthop Sci. 2012;17(6):667–672. [DOI] [PubMed] [Google Scholar]
- 35.Mizuno J, Nakagawa H. Outcome analysis of anterior decompressive surgery and fusion for cervical ossification of the posterior longitudinal ligament: report of 107 cases and review of the literature. Neurosurg Focus. 2001;10(4):E6. [DOI] [PubMed] [Google Scholar]
- 36.An HS, Al-Shihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg. 2014;22(7):420–429. [DOI] [PubMed] [Google Scholar]
- 37.Huang D, Du X, Liang H, Hu W, Hu H, Cheng X.Anterior corpectomy versus posterior laminoplasty for the treatment of multilevel cervical myelopathy: a meta-analysis. Int J Surg. 2016;35:21–27. [DOI] [PubMed] [Google Scholar]
- 38.Lee DH, Cho JH, Kim NH, et al. Radiological risk factors for progression of ossification of posterior longitudinal ligament following laminoplasty. Spine J. 2018;18(7):1116–1121. [DOI] [PubMed] [Google Scholar]
- 39.Park S, Lee DH, Ahn J, et al. How does ossification of posterior longitudinal ligament progress in conservatively managed patients? Spine (Phila Pa 1976). 2020;45(4):234–243. [DOI] [PubMed] [Google Scholar]
- 40.Lee CH, Sohn MJ, Lee CH, Choi CY, Han SR, Choi BW. Are there differences in the progression of ossification of the posterior longitudinal ligament following laminoplasty versus Fusion? A meta-analysis. Spine (Phila Pa 1976). 2017;42(12):887–894. [DOI] [PubMed] [Google Scholar]