Abstract
Study Design:
Systematic review and meta-analysis.
Objectives:
Indications for surgical decompression of gunshot wounds to the lumbosacral spine are controversial and based on limited data.
Methods:
A systematic review of literature was conducted to identify studies that directly compare neurologic outcomes following operative and non-operative management of gunshot wounds to the lumbosacral spine. Studies were evaluated for degree of neurologic improvement, complications, and antibiotic usage. An odds ratio and 95% confidence interval were calculated for dichotomous outcomes which were then pooled by random-effects model meta-analysis.
Results:
Five studies were included that met inclusion criteria. The total rate of neurologic improvement was 72.3% following surgical intervention and 61.7% following non-operative intervention. A random-effects model meta-analysis was carried out which failed to show a statistically significant difference in the rate of neurologic improvement between surgical and non-operative intervention (OR 1.07; 95% CI 0.45, 2.53; P = 0.88). In civilian only studies, a random-effects model meta-analysis failed to show a statistically significant difference in the rate of neurologic improvement between surgical and non-operative intervention (OR 0.75; 95% CI 0.21, 2.72; P = 0.66). Meta-analysis further failed to show a statistically significant difference in the rate of neurologic improvement between patients with either complete (OR 4.13; 95% CI 0.55, 30.80; P = 0.17) or incomplete (OR 0.38; 95% CI 0.10, 1.52; P = 0.17) neurologic injuries who underwent surgical and non-operative intervention. There were no significant differences in the number of infections and other complications between patients who underwent surgical and non-operative intervention.
Conclusions:
There were no statistically significant differences in the rate of neurologic improvement between those who underwent surgical or non-operative intervention. Further research is necessary to determine if surgical intervention for gunshot wounds to the lumbosacral spine, including in the case of retained bullet within the spinal canal, is efficacious.
Keywords: wounds gunshot, spine, spinal canal, decompression, surgical
Introduction
Gunshot wounds to the spine (Figure 1) account for a rising percentage of spinal injuries each year.1,2 Gun violence has overall seen a paradoxical increase during the Coronavirus Disease 2019 (COVID-19) Pandemic with increasing cases in major United States cities New York, Chicago, and Los Angeles. 3 Low velocity firearms are used more frequently in civilian spinal gunshot wounds. 4 These firearms produce spinal injury by direct mass effect on the spinal cord or by invasion of bullet or osseous fragments into the spinal canal.4,5 High velocity firearm injuries to the spine are seen more commonly in military conflicts and result in significant neurologic and soft tissue damage from penetrating and/or cavitary injury. 4 The lumbosacral spine anatomy includes the termination of the spinal cord in the conus medullaris and presence of the cauda equina; the conus medullaris terminates most commonly at the L1 or L2 vertebral level, however, its anatomic location can vary.6,7 Bullet injuries to the lumbosacral spine can injure the conus medullaris, cauda equina, bone, and exiting nerve roots, causing a variety of neurologic injury patterns.
Figure 1.

Computed tomography (CT) scan of the lumbar spine in sagittal (left) and axial (right) sequences of a patient following a gunshot wound to the lumbar spine. A bullet and multiple osseous fragments are retained within the spinal canal at the L2 vertebral level.
Indications for surgical decompression of gunshot wounds to the lumbosacral spine are not well defined, controversial, and frequently based on limited data, however, surgical intervention has been classically used in cases of spinal instability, progressive neurologic deficits, cases of cerebrospinal fluid leaks, and for patients with incomplete neurologic deficits who have retained bullet or osseous fragments within the spinal canal.1,2,4,8-13 The primary purpose of this study is to compare, through systematic review and meta-analysis, the rate of neurologic improvement following surgical and non-operative intervention for gunshot wounds to the lumbosacral spine. The secondary purpose of this analysis is to compare complication rates, antibiotic usage, and infection in these populations.
Methods
Protocol
This study includes a systematic review of literature conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. 14
Eligibility Criteria, Information Sources, Search
Online databases PubMed, the Cochrane Library, and Scopus, were used to identify clinical studies comparing neurologic outcomes following surgical and non-operative management of gunshot wounds to the lumbosacral spine. Specific MeSH terms and key words including “gunshot wound,” “lumbar spine,” “lumbosacral spine,” and “cauda equina” were used in various combinations to identify studies of interest. Additional manual searches through cited references were performed.
Study Selection
Direct comparative studies including randomized controlled trials, prospective/retrospective cohort and case-control studies were included in further analysis. Non-English publications, editorials, conference abstracts, errata, book chapters, systematic reviews, meta-analyses, case reports, and case series were excluded. Only studies directly comparing neurologic outcomes following operative and non-operative management of gunshot wounds to the lumbosacral spine were included in analysis. Studies that did not include both a surgical and non-operative group were excluded. Studies that did not specifically include the neurologic improvement following lumbosacral gunshot wounds were excluded. Both military and civilian studies including both high and low velocity projectiles were included in further analysis.
Data Collection Process, Data Items
Studies were evaluated for the method of classification of neurologic improvement (Frankel grading, complete versus incomplete, etc.) and for the rate of neurologic improvement in patients following gunshot wounds to the lumbar spine. Studies were further analyzed for complications including infection, hemorrhage, neurologic decline, pseudomeningocele, cerebrospinal fluid leak, and antibiotic usage. Studies were sub-analyzed for the degree of neurologic improvement that occurred after surgical and non-operative intervention in patients following complete and incomplete neurologic injuries and for the degree of neurologic improvement that occurred in civilian only injuries.
Summary Measures, Synthesis of Results, Risk of Bias, Additional Analyses
For the purpose of meta-analysis, an odds ratio and 95% confidence interval were calculated for dichotomous outcomes which were then pooled by random-effects model meta-analysis. All statistical tests were performed using RevMan 5.3 (Copenhagen: The Nordic Cochrane Center, The Cochrane Collaboration, 2014). An I2 test was performed for each comparison to test statistical heterogeneity with I2 values exceeding 25%, 50%, and 75% indicating a low, moderate, and high degree of heterogeneity, respectively. For all meta-analyses, outcomes were pooled with weights calculated by the inverse-variance method. A P-value < 0.05 was used to assess statistical significance. Each study included in meta-analysis was further assessed for risk of bias. Specifically, studies were evaluated for selection bias, performance bias, detection bias, attrition bias, and reporting bias. Each study was assigned a corresponding level of evidence according to the scale adopted by the North American Spine Society, January 2005. 15
Results
In total, 240 abstracts were reviewed, of which 187 were excluded. Fifty-three full text articles were assessed, of which 48 were excluded. Studies were excluded for failing to include both a surgical and non-operative group.5,16-23 Studies were further excluded if they did not include patients with injuries to the lumbosacral spine or if it was not possible to calculate the number of lumbosacral spine patients who showed neurologic improvement in each group.6,12,13,24-34 Simpson et al was excluded from the study as it included the same population of patients included in Robertson and Simpson.35,36 Overall 5 studies were included in quantitative synthesis that directly compared neurologic improvement following surgical and non-operative management of patients who presented after gunshot wounds to the lumbosacral spine.36-40 A flow chart of study inclusion and exclusion is shown in Figure 2.
Figure 2.

A flow chart of study inclusion and exclusion.
All studies included in meta-analysis were retrospective cohort series and were assessed to comprise level III evidence with a high risk of bias (Figure 3). Of the 5 studies included in analysis, 2 studies concerned injuries during military conflict (Table 1). Aarabi et al included patients who sustained injuries during the Iran-Iraq War from 1980 to 1988 whereas Kahraman et al included patients who sustained injuries in military conflict in Turkey between 1994 and 2000. Both studies included mixed projectiles and mixed velocities within the study cohorts. Time from injury to admission to a medical center qualified to care for spinal injuries is longer in military conflict as compared to civilian injury. The mean time from injury to admission was 84 hours in Aarabi et al and 28 hours in Kahraman et al.38,40 The remainder of included studies included injuries sustained in civilian conflict (Table 1). Isiklar and Lindsey included patients with exclusively low velocity bullet injuries, whereas Benzel et al included bullet wounds of mixed or non-specified velocity.37,39 Robertson and Simpson included 33 patients with low velocity injuries to the cauda equina of which 30 were from low velocity bullet injuries and 3 were stab wounds. 36 Three of the 5 included studies included injuries exclusively to the “cauda equina.”36-38 Isiklar and Lindsey included patients with gunshot wounds to the “lumbar spine (L1-L5)” and Kahraman et al included patients with gunshot wounds to the “lumbosacral spine.”39,40
Figure 3.
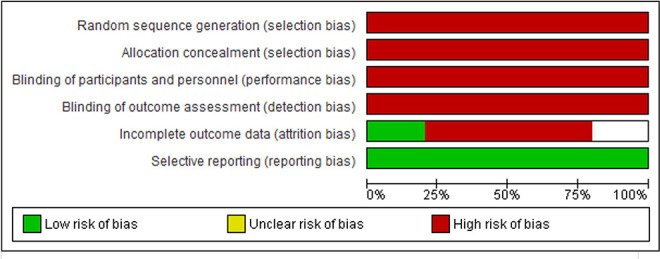
A graphic representation of risk of bias for each included study.
Table 1.
Characteristics of Studies Included in Quantitative Synthesis.
| Study | Year | Military/civilian | Projectile type | Velocity | Description of injury location |
|---|---|---|---|---|---|
| Benzel et al | 1987 | Civilian | Bullet | Mixed | Cauda Equina |
| Robertson and Simpson | 1992 | Civilian | Mixed | Low | Cauda Equina |
| Aarabi et al | 1996 | Military | Mixed | Mixed | Cauda Equina |
| Isiklar and Lindsey | 1997 | Civilian | Bullet | Low | Lumbar Spine |
| Kahraman et al | 2004 | Military | Mixed | Mixed | Lumbosacral |
All patients included in analysis presented with a neurologic deficit on admission. The method of assessment of neurologic status ranged across included studies (Table 2). Three of the 5 included studies assessed neurologic status on admission using Frankel grading and defined neurologic improvement as an improvement in 1 grade.13,38-40 Benzel et al did not specify using a specific grading system, however, defined improvement as an improvement in myelopathic or radicular function. 37 Robertson and Simpson defined deficits as complete if there was a total loss of function below the level of injury and incomplete if any function remained below the level of injury. Robertson and Simpson further defined improvement as the recovery of any motor strength or the regaining of at least a unilateral sensory level. 36 Across all 5 studies, only 3 patients were noted to neurologically worsen during the follow-up period. All 3 patients were treated surgically.36,40 The remainder of patients either showed neurologic improvement or remained at their admission baseline.
Table 2.
Neurologic Outcomes Following Surgical and Non-Operative Management of Patients With Lumbosacral Gunshot Wounds.
| Study | Year | Method of classification of neurologic status | Intervention (# of patients) | Number of patients who neurologically improved | Number of patients who remained at neurologic baseline | Number of patients who neurologically deteriorated | Mean follow-up |
|---|---|---|---|---|---|---|---|
| Benzel et al | 1987 | NR | Surgical (5) Non-operative (1) | 5 1 | 0 0 | 0 0 | NR |
| Robertson and Simpson | 1992 | Complete/Incomplete | Surgical (18) Non-operative (15) | 10 10 | 7 5 | 1 0 | 22 weeks |
| Aarabi et al | 1996 | Frankel Grading | Surgical (26) Non-operative (12) | 21 8 | 5 4 | 0 0 | NR |
| Isiklar and Lindsey | 1997 | Frankel Grading | Surgical (2) Non-operative (11) | 1 4 | 1 7 | 0 0 | NR |
| Kahraman et al | 2004 | Frankel Grading | Surgical (32) Non-operative (8) | 23 6 | 7 2 | 2 0 | 32 months |
Abbreviations: NR (Not reported).
Reasons for surgical intervention across studies included neurologic decompression, debridement, removal of foreign body, and dural repair. Only 2 studies specified the total follow-up time which ranged from a mean of 22 weeks to 32 months.36,40 Of the 5 studies included in meta-analysis the rate of neurologic improvement ranged from 50% to 100% in the surgical group and 36% to 100% in the non-operative group. The total rate of neurologic improvement was 72.3% following surgical intervention and 61.7% following non-operative intervention. A random-effects model meta-analysis was carried out which failed to show a statistically significant difference in the rate of neurologic improvement between surgical and non-operative intervention (OR 1.07; 95% CI 0.45, 2.53; P = 0.88, I2 = 0) (Figure 4). The rate of neurologic improvement in civilian only studies ranged from 50% to 100% in the surgical group and 36% to 100% in the non-operative group. The total rate of neurologic improvement was 64% following surgical intervention and 56% following non-operative intervention. A random-effects model meta-analysis was carried out which failed to show a statistically significant difference in the rate of neurologic improvement in civilian only studies between surgical and non-operative intervention (OR 0.75; 95% CI 0.21, 2.72; P = 0.66, I2 = 0%) (Figure 5).
Figure 4.
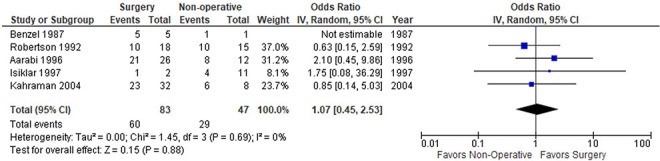
Forest plot comparing neurologic improvement after surgical and non-operative intervention in patients with gunshot wounds to the lumbosacral spine; IV (inverse variance), CI (confidence interval), df (degrees of freedom).
Figure 5.

Forest plot comparing neurologic improvement after surgical and non-operative intervention in civilian patients with gunshot wounds to the lumbosacral spine; IV (inverse variance), CI (confidence interval), df (degrees of freedom).
Only 2 studies were included that calculated the rate of neurologic improvement after surgical and non-operative intervention in patients with complete and incomplete neurologic injuries.36,38 The rate of improvement in patients with complete neurologic injury ranged from 57.1% to 100% in the surgical group compared to 0% to 33.3% in the non-operative group. A random-effects model meta-analysis was carried out which failed to show a statistically significant difference in the rate of neurologic improvement between patients with complete neurologic injuries undergoing surgical and non-operative intervention (OR 4.13; 95% CI 0.55, 30.80; P = 0.17, I2 = 0) (Figure 6). The rate of improvement in patients with incomplete neurologic injury ranged from 46.7% to 89.5% in the surgical group and71.4% to 100% in the non-operative group. A random-effects model meta-analysis was carried out which failed to show a statistically significant difference in the rate of neurologic improvement between patients with incomplete neurologic injuries undergoing surgical and non-operative intervention (OR 0.38; 95% CI 0.10, 1.52; P = 0.17, I2 = 0) (Figure 7).
Figure 6.

Forest plot comparing neurologic improvement after surgical and non-operative intervention in patients with complete neurologic injuries who sustained gunshot wounds to the lumbosacral spine; IV (inverse variance), CI (confidence interval), df (degrees of freedom).
Figure 7.

Forest plot comparing neurologic improvement after surgical and non-operative intervention in patients with incomplete neurologic injuries who sustained gunshot wounds to the lumbosacral spine; IV (inverse variance), CI (confidence interval), df (degrees of freedom).
All included studies except for Isiklar and Lindsey included antibiotic prophylaxis for all patients. Benzel et al and Aarabi et al specified antibiotic regimens of Nafcillin/Chloramphenicol and Penicillin/Chloramphenicol/Gentamicin, respectively.37,38 Robertson and Simpson reported that all patients received prophylactic antibiotics, however, did not report the type. They reported that there was at least one postoperative infection in the surgical group and none in the non-operative group. 36 Isiklar and Lindsey reported that 9 of 13 patients with injuries to the lumbar spine received prophylactic antibiotics of varying type. There was one patient who had received prophylactic antibiotics who developed a paraspinal infection. The patient had an associated colonic injury however whether or not the patient had undergone surgical intervention was not specified. 39
In terms of complications, only one study specified the number of complications that occurred in both the surgical and non-operative group of patients that presented with injuries to the lumbosacral spine. Robertson and Simpson reported that 28% of patients in the surgical group suffered a complication (cerebrospinal fluid leak, pseudomeningocele, wound infection) compared to 0% in the non-operative group. 36 Only 3 patients in the included studies were shown to neurologically decline. All 3 patients were part of the surgical intervention group.36,40
Discussion
The study of ballistic injury to the spine is inherently challenging. There is substantial heterogeneity in injury type and insufficient sample size to reach meaningful conclusion. There is significant heterogeneity in treatment philosophy and no consensus on indication for surgical intervention. Gunshot wounds to the lumbosacral spine represent a distinct pathology from gunshot wounds to the cervical or thoracic spine. This is not only related to the unique anatomy of the lumbosacral spine which includes the conus medullaris and cauda equina, however, is also related to the abdominal viscera which are in proximity and represent a possible risk factor for infectious complications.
This study includes a systematic review and meta-analysis of studies that directly compare neurologic outcomes following surgical and non-operative intervention for gunshot wounds to the lumbosacral spine. Overall, 5 studies were included in analysis.36-40 There was significant heterogeneity within the included studies, as studies included a mix of injury type (civilian, military), projectile type (bullet, knife, shrapnel), and projectile velocity (Table 1). All studies included primarily gunshot wounds isolated to the lumbosacral spine with 3 studies further isolating analysis to injuries to the cauda equina. The total rate of neurologic improvement was 72.3% following surgical intervention and 61.7% following non-operative intervention. Although the rate of neurologic improvement favored surgical intervention, the relationship was not observed to be statistically significantly different in meta-analysis (Figure 4). The rate of neurologic improvement in patients with complete (Figure 6) and incomplete neurologic injury (Figure 7) favored surgical and non-operative intervention respectively, however, was not observed to be statistically significant in either case.
When only civilian injuries were analyzed the rate of neurologic improvement favored non-operative intervention over surgical intervention, however, it was not statistically significant (Figure 5). Civilian injuries may favor non-operative intervention as compared to military injuries which may favor surgical intervention. This may be related to differences in projectile type and velocity that are encountered in the different populations. 5 High velocity injuries from military weapons are known to cause a higher degree of damage to non-nervous tissue including bone, disc, and muscle. 40 Surgical intervention may aid to a greater extent in these injuries by treating or preventing secondary injuries not caused by the projectile itself, such as compression related to osseous fragments or epidural hemorrhage. Unfortunately, this conclusion is limited by the rarity of comparative studies in civilian and military literature.
Although few studies have examined the differences in outcomes that occur after surgical and non-operative intervention for patients with gunshot wounds to the lumbosacral spine, several reviews have recommended for surgical intervention especially in the case of progressive neurologic decline or in the case of a retained bullet within the spinal canal.4,8-11,13 These recommendations are based on limited data as few previous studies have examined surgical intervention for patients with gunshot wounds to the lumbosacral spine as compared to non-operative management. Cybulski et al recommended surgical exploration/debridement for any patient who sustained a gunshot wound to the lumbar spine. 5 The analysis in the study was limited as patients with gunshot wounds to the lumbar spine who underwent surgical intervention were compared only with patients who underwent surgical intervention after gunshot wounds to the cervical or thoracic spine. There was no comparison to a non-operative group. Conversely, Kihtir et al recommended against surgical exploration/debridement of gunshot wounds to the thoracolumbar spine in patients with complete or non-progressive injuries, however, did not include a surgical comparison group in analysis. 21 Waters and Adkins, which is frequently cited as evidence in recommending for surgical intervention, analyzed 20 patients who sustained civilian gunshot wounds from T12 to L4 and had a bullet or major fragment retained in the spinal canal, and found that patients who had the fragment removed to have a statistically significant improvement in the American Spinal Injury Association (ASIA) motor score at follow-up compared to non-operative patients. 6 The study was unable to be included in this meta-analysis as the number of patients with neurologic improvement was not described.
All included studies except for one included antibiotic prophylaxis for all patients with most studies using broad spectrum antibiotics, however, there was insufficient data to make a meaningful conclusion regarding the efficacy of antibiotic prophylaxis and the effect of surgery vs non-operative management on the risk of infection. Several previous studies and reviews have recommended broad spectrum antibiotics for patients who sustain gunshot wounds to the spine for at least 48 hours with consideration of longer durations with bowel, specifically colonic, injury.2,9-12,41,42
Only one included study specified the number of complications that occurred in both the surgical and non-operative group, therefore again there was insufficient data to make a meaningful conclusion regarding the risks of complications following surgical and non-operative management of gunshot wounds to the lumbosacral spine. Bumpass et al found, in a study of patients who presented with gunshot wounds to the spine (including cervical and thoracic), that patients who underwent operative management had a significantly increased risk of suffering a complication compared to patients treated non-operatively. Of 3 patients in the study who underwent surgical intervention after gunshot wounds to the lumbar spine, 2 had at least one postoperative complication including a revision for misplaced hardware.
Limitations
There are several limitations to this study. Following systematic review only 5 studies were included that met inclusion/exclusion criteria. Although all studies were directly comparative in nature, outcomes of interest were not included in each study which greatly limited the ability to perform meta-analyses. There was significant heterogeneity between the studies in terms of injury/projectile type, projectile velocity, and method of neurologic assessment. The included studies were further limited by short overall follow-up or unclear follow-up periods. All studies that were included in analysis were graded as class III in terms of level of evidence and further characterized as having a high risk of bias.
Conclusions
Despite significant limitations, this study represents the only systematic review and meta-analysis of studies that directly compared neurologic outcomes following surgical and non-operative intervention for gunshot wounds to the lumbosacral spine. We did not observe any statistically significant differences in the rate of neurologic improvement between those who underwent surgical or non-operative intervention. These limited results contradict several previously written reviews.4,9,11,13 Further research, including large comparative studies with sufficient power, is necessary to determine if surgical intervention for gunshot wounds to the lumbosacral spine, including in the case of retained bullet within the spinal canal, is efficacious.
Footnotes
Authors’ Note: Portions of this paper have been previously presented at the Lumbar Spine Research Society, annual meeting, 2020.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Andrew Platt, MD  https://orcid.org/0000-0002-2514-2705
https://orcid.org/0000-0002-2514-2705
References
- 1.Jaiswal M, Mittal RS. Concept of gunshot wound spine. Asian Spine J. 2013;7(4):359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heary RF, Mammis A. Gunshot injuries to the thoracolumbar spine. Semin Spine Surgs. 2010;22(2):73–77. [Google Scholar]
- 3.Sutherland M, McKenney M, Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med. 2021;39:225–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sidhu GS, Ghag A, Prokuski V, Vaccaro AR, Radcliff KE. Civilian gunshot injuries of the spinal cord: a systematic review of the current literature. Clin Orthop Relat Res. 2013;471(12):3945–3955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cybulski GR, Stone JL, Kant R. Outcome of laminectomy for civilian gunshot injuries of the terminal spinal cord and cauda equina: review of 88 cases. Neurosurgery. 1989;24(3):392–397. [DOI] [PubMed] [Google Scholar]
- 6.Waters RL, Adkins RH. The effects of removal of bullet fragments retained in the spinal canal. A collaborative study by the National Spinal Cord Injury Model Systems. Spine (Phila Pa 1976). 1991;16(8):934–939. [DOI] [PubMed] [Google Scholar]
- 7.Harrop JS, Naroji S, Maltenfort MG, et al. Neurologic improvement after thoracic, thoracolumbar, and lumbar spinal cord (conus medullaris) injuries. Spine (Phila Pa 1976). 2011;36(1):21–25. [DOI] [PubMed] [Google Scholar]
- 8.Nwosu K, Eftekhary N, McCoy E, Bhalla A, Fukunaga D, Rolfe K.Surgical management of civilian gunshot-induced spinal cord injury: is it overutilized? Spine (Phila Pa 1976). 2017;42(2):E117–E124. [DOI] [PubMed] [Google Scholar]
- 9.Rosenfeld JV, Bell RS, Armonda R. Current concepts in penetrating and blast injury to the central nervous system. World J Surg. 2015;39(6):1352–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klimo P, Jr, Ragel BT, Rosner M, Gluf W, McCafferty R. Can surgery improve neurological function in penetrating spinal injury? A review of the military and civilian literature and treatment recommendations for military neurosurgeons. Neurosurg Focus. 2010;28(5):E4. [DOI] [PubMed] [Google Scholar]
- 11.Bono CM, Heary RF. Gunshot wounds to the spine. Spine J. 2004;4(2):230–240. [DOI] [PubMed] [Google Scholar]
- 12.Heary RF, Vaccaro AR, Mesa JJ, Balderston RA. Thoracolumbar infections in penetrating injuries to the spine. Orthop Clin North Am. 1996;27(1):69–81. [PubMed] [Google Scholar]
- 13.Bumpass DB, Buchowski JM, Park A, et al. An update on civilian spinal gunshot wounds: treatment, neurological recovery, and complications. Spine (Phila Pa 1976). 2015;40(7):450–461. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levels of evidence for primary research question as adopted by the North American Spine Society. Published 2005. Updated 2005. Accessed October 24, 2020. https://www.spine.org/Portals/0/Assets/Downloads/ResearchClinicalCare/LevelsofEvidence.pdf
- 16.Aryan HE, Amar AP, Ozgur BM, Levy ML. Gunshot wounds to the spine in adolescents. Neurosurgery. 2005;57(4):748–752; discussion 748-752. [DOI] [PubMed] [Google Scholar]
- 17.le Roux JC, Dunn RN. Gunshot injuries of the spine—a review of 49 cases managed at the Groote Schuur Acute Spinal Cord Injury Unit. S Afr J Surg. 2005;43(4):165–168. [PubMed] [Google Scholar]
- 18.Six E, Alexander E, Jr, Kelly DL, Jr, Davis CH, Jr, McWhorter JM. Gunshot wounds to the spinal cord. South Med J. 1979;72(6):699–702. [DOI] [PubMed] [Google Scholar]
- 19.Formby PM, Wagner SC, Kang DG, Van Blarcum GS, Pisano AJ, Lehman RA, Jr. Reoperation after in-theater combat spine surgery. Spine J. 2016;16(3):329–334. [DOI] [PubMed] [Google Scholar]
- 20.Splavski B, Vrankovic D, Saric G, Blagus G, Mursic B, Rukovanjski M. Early management of war missile spine and spinal cord injuries: experience with 21 cases. Injury. 1996;27(10):699–702. [DOI] [PubMed] [Google Scholar]
- 21.Kihtir T, Ivatury RR, Simon R, Stahl WM. Management of transperitoneal gunshot wounds of the spine. J Trauma. 1991;31(12):1579–1583. [DOI] [PubMed] [Google Scholar]
- 22.Rukovansjki M. Spinal cord injuries caused by missile weapons in the Croatian war. J Trauma. 1996;40(3 suppl):S189–S192. [DOI] [PubMed] [Google Scholar]
- 23.Turgut M, Ozcan OE, Gucay O, Saglam S. Civilian penetrating spinal firearm injuries of the spine. Results of surgical treatment with special attention to factors determining prognosis. Arch Orthop Trauma Surg. 1994;113(5):290–293. [DOI] [PubMed] [Google Scholar]
- 24.Kupcha PC, An HS, Cotler JM. Gunshot wounds to the cervical spine. Spine (Phila Pa 1976). 1990;15(10):1058–1063. [DOI] [PubMed] [Google Scholar]
- 25.Heiden JS, Weiss MH, Rosenberg AW, Kurze T, Apuzzo ML. Penetrating gunshot wounds of the cervical spine in civilians. Review of 38 cases. J Neurosurg. 1975;42(5):575–579. [DOI] [PubMed] [Google Scholar]
- 26.Venger BH, Simpson RK, Narayan RK. Neurosurgical intervention in penetrating spinal trauma with associated visceral injury. J Neurosurg. 1989;70(4):514–518. [DOI] [PubMed] [Google Scholar]
- 27.Duz B, Cansever T, Secer HI, Kahraman S, Daneyemez MK, Gonul E. Evaluation of spinal missile injuries with respect to bullet trajectory, surgical indications and timing of surgical intervention: a new guideline. Spine (Phila Pa 1976). 2008;33(20):E746–E753. [DOI] [PubMed] [Google Scholar]
- 28.Heary RF, Vaccaro AR, Mesa JJ, et al. Steroids and gunshot wounds to the spine. Neurosurgery. 1997;41(3):576–583; discussion 583-584. [DOI] [PubMed] [Google Scholar]
- 29.Levy ML, Gans W, Wijesinghe HS, SooHoo WE, Adkins RH, Stillerman CB. Use of methylprednisolone as an adjunct in the management of patients with penetrating spinal cord injury: outcome analysis. Neurosurgery. 1996;39(6):1141–1148; discussion 1148-1149. [DOI] [PubMed] [Google Scholar]
- 30.Stauffer ES, Wood RW, Kelly EG. Gunshot wounds of the spine: the effects of laminectomy. J Bone Joint Surg Am. 1979;61(3):389–392. [PubMed] [Google Scholar]
- 31.Yashon D, Jane JA, White RJ. Prognosis and management of spinal cord and cauda equina bullet injuries in sixty-five civilians. J Neurosurg. 1970;32(2):163–170. [DOI] [PubMed] [Google Scholar]
- 32.Hammoud MA, Haddad FS, Moufarrij NA. Spinal cord missile injuries during the Lebanese civil war. Surg Neurol. 1995;43(5):432–437; discussion 437-442. [DOI] [PubMed] [Google Scholar]
- 33.Morrow KD, Podet AG, Spinelli CP, et al. A case series of penetrating spinal trauma: comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019;46(3):E4. [DOI] [PubMed] [Google Scholar]
- 34.Gutierrez A, Su YS, Vaughan KA, et al. Penetrating spinal column injuries (pSI): an institutional experience with 100 consecutive cases in an urban trauma center. World Neurosurg. 2020;138:e551–e556. [DOI] [PubMed] [Google Scholar]
- 35.Simpson RK, Jr, Venger BH, Narayan RK. Treatment of acute penetrating injuries of the spine: a retrospective analysis. J Trauma. 1989;29(1):42–46. [PubMed] [Google Scholar]
- 36.Robertson DP, Simpson RK. Penetrating injuries restricted to the cauda equina: a retrospective review. Neurosurgery. 1992;31(2):265–269; discussion 269-270. [DOI] [PubMed] [Google Scholar]
- 37.Benzel EC, Hadden TA, Coleman JE. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20(2):281–285. [DOI] [PubMed] [Google Scholar]
- 38.Aarabi B, Alibaii E, Taghipur M, Kamgarpur A. Comparative study of functional recovery for surgically explored and conservatively managed spinal cord missile injuries. Neurosurgery. 1996;39(6):1133–1140. [DOI] [PubMed] [Google Scholar]
- 39.Isiklar ZU, Lindsey RW. Low-velocity civilian gunshot wounds of the spine. Orthopedics. 1997;20(10):967–972. [DOI] [PubMed] [Google Scholar]
- 40.Kahraman S, Gonul E, Kayali H, et al. Retrospective analysis of spinal missile injuries. Neurosurg Rev. 2004;27(1):42–45. [DOI] [PubMed] [Google Scholar]
- 41.Romanick PC, Smith TK, Kopaniky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg Am. 1985;67(8):1195–1201. [PubMed] [Google Scholar]
- 42.Gjolaj JP, Eismont FJ. Gunshot injuries to the spine. JBJS Rev. 2015;3(11):01874474–201511000-00001. [DOI] [PubMed] [Google Scholar]


