Abstract
Study Design:
Systematic review.
Objectives:
To summarize the results of clinical studies investigating spinal instrumentation techniques aiming to reduce the postoperative incidence of proximal junctional kyphosis (PJK) and/or failure (PJF) in adult spinal deformity (ASD) patients.
Methods:
EMBASE and Medline® were searched for articles dating from January 2000 onward. Data was extracted by 2 independent authors and methodological quality was assessed using ROBINS-I.
Results:
18 retrospective- and prospective cohort studies with a severe or critical risk of bias were included. Different techniques were applied at the upper instrumented vertebra (UIV): tethers in various configurations, 2-level prophylactic vertebroplasty (2-PVP), transverse process hooks (TPH), flexible rods (FR), sublaminar tapes (ST) and multilevel stabilization screws (MLSS). Compared to a pedicle screw (PS) group, significant differences in PJK incidence were found using tethers in various configurations (18% versus 45%, P = 0.001, 15% versus 38%, P = 0.045), 2-PVP (24% vs 36%, P = 0.020), TPH (0% vs. 30%, P = 0.023) and FR (15% versus 38%, P = 0.045). Differences in revision rates for PJK were found in studies concerning tethers (4% versus 18%, P = 0.002), 2-PVP (0% vs 13%, P = 0.031) and TPH (0% vs 7%, P = n.a.).
Conclusion:
Although the studies are of low quality, the most frequently studied techniques, namely 2-PVP as anterior reinforcement and (tensioned) tethers or TPH as posterior semi-rigid fixation, show promising results. To provide a reliable comparison, more controlled studies need to be performed, including the use of clinical outcome measures and a uniform definition of PJF.
Keywords: long-segment spinal fusion, adult spinal deformity, spine surgery, proximal junctional kyphosis, proximal junctional failure, systematic review, topping-off, transition zone, semi-rigid junctional fixation
Introduction
Over the past decades, the number of surgical procedures for correction and treatment of adult spinal deformity (ASD) has increased enormously. However, long segment spinal fusion constructs are rigid and induce high stresses at the transitional vertebrae, possibly resulting in proximal junctional kyphosis (PJK) and proximal junctional failure (PJF).1-20 PJK is a radiographic observation which often manifests within the first 6 to 8 weeks following surgical correction of ASD, with reported rates ranging from 20%-40%.1,7,11,12,21 PJF is defined in various ways, including: a fracture of the upper instrumented vertebra (UIV) or the vertebra above (UIV+1), the need for proximal extension of the fusion, and/or pullout or failure of the UIV fixation (UIV and UIV defined as in Figure 1A). 11 Incidence rates reported in literature vary widely (1%-35%) due to lack of a standardized definition. 7 Whereas the correlation between the incidence of PJK and clinical outcome has been questioned, PJF has been associated with a worse clinical outcome and a higher need for revision surgery.9,11,19,22 Similar to PJK, PJF is reported to occur early in the postoperative period and often occurs within the first 6 months following surgery. Several authors have suggested that PJF is part of the spectrum of PJK and shares the same multifactorial etiology and surgical-, radiographic-, and patient-specific risk factors.1,7,8,12,21 Both PJK and PJF are a growing challenge with which many spinal surgeons, treating the commonly fragile patient with ASD, are faced nowadays.
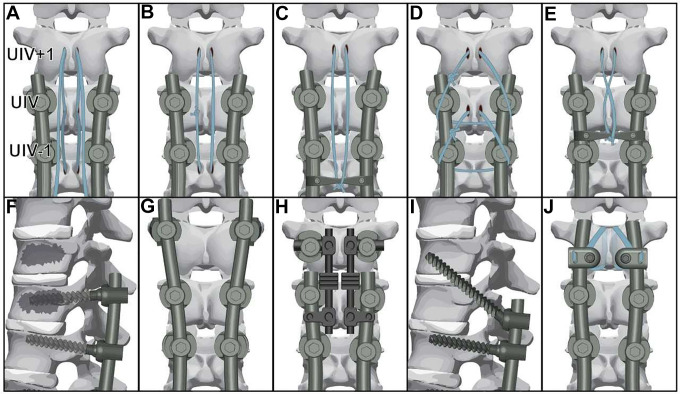
Figure 1.
Surgical prophylactic techniques for PJK and PJF as reported in Table 1, (A) tether-connectors (TO) 28, 33; (B) tether only (TO) 29, 30, 32; (C) tether-crosslink (TC) 29, 30; (D) tether-pedicle loop (TO) 31; (E) tether in a figure 8 way (TO) 34; (F) prophylactic 2-level vertebroplasty (2-PVP) 32, 35-40; (G) transverse process hooks (TPH) 32, 41, 42; (H) flexible rods (FR) 43; (I) multilevel stabilization screw (MLSS) 44; (J) sublaminar tapes (ST) 45.
In the past years, a number of instrumentation techniques aiming to prevent PJK and PJF have been developed.7,8,11 These techniques utilize a semi-rigid fixation at the proximal end of a rigid spinal construct to create a more gradual transition of motion, thereby decreasing peak stresses at junctional levels. This concept has also been referred to as “topping-off.” Alternatively, techniques such as vertebroplasty aim to increase the load carrying capacity of the anterior column.8,11
To date, no systematic comparison on the effectiveness of clinically investigated surgical techniques for the prevention of PJK and PJF in the ASD population exists. Therefore, the purpose of this study is to provide an overview of all clinically investigated instrumentation techniques intended to reduce the incidence of PJK and PJF and to evaluate their effectiveness.
Methods
This systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Statement (PRISMA-statement). 23
Search
A literature search was performed in Medline® and EMBASE for full-text studies, published from January 2000 until April 19th 2021. The search terms and strategy are reported in Supplemental Table 1. Authors of included studies were contacted for any missing full-texts or data if needed. No language restrictions were imposed and the reference lists from the included studies were manually checked for additional eligible studies. Duplicates were removed using the Bramer method in EndNoteX8. 24
Study Selection
Using the Rayyan application (Qatar Computing Research Institute), 25 2 researchers (TV, RD) independently screened the titles and abstracts applying the following inclusion criteria: clinical study, ≥6 months follow up, degenerative/adult (≥18years) spinal deformity, upper instrumented vertebrae in the thoracic spine, >4 segments fused or prophylactic technique for PJK and/or PJF. Exclusion criteria were: case reports, case series with <5 patients, fusion constructs ending proximally in the cervical spine, tuberculous spine, adolescent idiopathic scoliosis (<18 years), spinal trauma, spinal tumor or congenital spinal deformities. Any disagreement was resolved by discussion and consultation of a third reviewer (PW). Full-text analysis was performed using the same criteria.
Data Collection
For each included study, data was extracted independently by 2 authors (TV, RD) and reported using a standardized form. The form included; the applied PJK or PJF prophylactic surgical technique, study design, number of patients, patient population (gender, age, body mass index (BMI)), fusion characteristics (UIV, lower instrumented vertebrae, rod material, levels fused) and concomitant surgical procedures performed.
Quality Assessment
The risk of bias of the included articles was evaluated independently by 2 authors (TV, RD) using the Risk Of Bias In Non-randomized Studies-of Interventions (ROBINS-I) tool. 26
Data Extraction
Studies were classified according to the prophylactic technique used. Throughout this review, PJK was defined as a postoperative proximal junction sagittal Cobb angle (PJA) ≥10° and/or a proximal junction sagittal Cobb angle ≥10° compared to the preoperative measurement, as defined by Glattes et al. 4 Due to inconsistent reporting in the literature, no standardized definition for PJF was used. Incidences of PJK, and incidences and definitions of PJF were extracted. Next, we reported clinical outcomes and complications following surgery, as converted to the classification of Glassman et al. 27 Revision surgery for PJK was not included as a complication, but was categorized separately.
Results
Study Characteristics
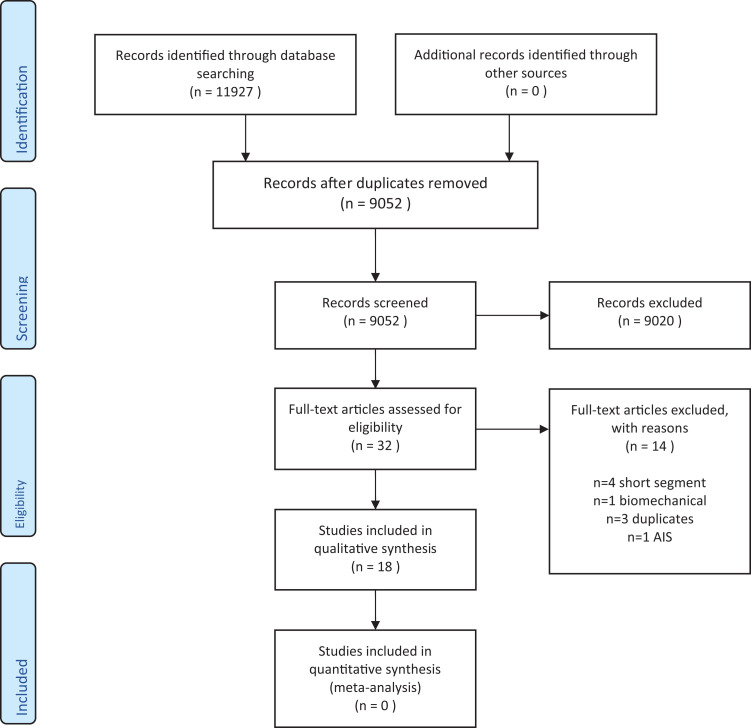
A total of 11,144 unique articles were identified following the search strategy. After preliminary selection based on title and abstract, 32 full text articles were screened for the in- and exclusion criteria. Fourteen articles were excluded and 18 articles, published between 2008-2021, were included (Figure 2). Of the included studies, 4 were prospective- and 14 were retrospective cohort studies. The studies that were included reported on tether fixation,28-34 prophylactic 2-level vertebroplasty (2-PVP),32,35-40 transverse process hooks (TPH),32,41,42 flexible rods (FR), 43 multilevel stabilization screw (MLSS), 44 and sublaminar tapes (ST). 45 These surgical techniques are schematically illustrated in Figure 1. Thirteen of the studies compared the intervention to a control group, consisting of patients treated with pedicle screws at the UIV (PS).28,29,31-37,40-43 The minimal follow-up duration was 12 months. All study characteristics are presented in Table 1.
Figure 2.
PRISMA 2009 flow diagram of the included studies. AIS = adult idiopathic scoliosis.
Table 1.
Study Characteristics.
| Author and study design | Groups and surgical technique description | Follow-up (mo) | Participants | Additional surgery | |
|---|---|---|---|---|---|
| Tether (tether only (TO) + tether and crosslink (TC)) | |||||
| Alluri et al 2020
28
Retrospective, Single center |
PS | 23.4 ± 14.1 | N = 34 | Age 62 ± 9; M/F 13:21 | Ost. n = 30, ACP n = 3 |
| TC: semitendinosus allograft interwoven between spinous processes UIV+1 and a crosslink between the rods at UIV−2. | 18.2 ± 9.4 | N = 49 | Age 64 ± 10; M/F 13:36 | Ost. n = 44, ACP n = 9 | |
| Buell et al 2018
29
Retrospective, Single center |
PS | 28 (12-57)† | N = 64 | Age 66.1 ± 8.5; M/F 22:42 | Ost. n = 18 |
| TO: Hand-tightened 5-mm polyethylene tape through the spinous processes of UIV+1 and UIV−1 | 28 (12-57)† | N = 64 | Age 66.3 ± 10.9; M/F 31:43 | Ost. n = 17 | |
| TC: 5-mm polyethylene tape through the spinous processes of UIV+1 and tensioned by distal displacement of a crosslink between UIV−1 and UIV−2 | 28 (12-57)† | N = 56 | Age 66.6 ± 8.6; M/F 17:39 | Ost. n = 8 | |
| Buell et al 2019
30
Retrospective, Single center |
PS + TO + TC: Pedicle screws at UIV or polyethylene tape tied through the spinous processes of UIV+1 and either tied to UIV−1 or to a standard crosslink between UIV−1 and UIV−2. | 20 (3-56) | N = 120 | Age 67.3 ± 8.2; M/F 43:77 | Ost. n = 22 |
| Iyer et al 2020
31
Retrospective, Single center |
PS | 17.6 ± 6.1 | N = 77 | *Age 51.3 ± 21.4 | *Ost. n = 51, IBF n = 13 |
| TO: 5-mm polyethylene tape through spinous processes of UIV+1 and looped below pedicle screws of UIV. This process was repeated at UIV, tied to UIV−1. | 17.4 ± 6.0 | N = 31 | *Age 64.1 ± 10.4 | *Ost. n = 28, IBF n = 18 |
|
| Line et al 2020
32
Retrospective, Single center |
PS | 31.2 (8-83)† | N = 390 | Age 62.2 (19-86); M/F 121:296 | Unclear |
| TO: Polyethylene tape tied through the spinous processes of UIV+1 (and/or UIV+2) and UIV−1, reference to Buell et al 2019 28 | 31.2 (8-83)† | N = 62 | Age 65.9 (41-84); M/F 15:47 | ||
| Safaee et al 2018
33
Retrospective, Single center |
PS | 12 (6-26)† | N = 100 | *Age 62; M/F 29:71 | *UIV hook n = 18 *Vert. plasty. N = 25 |
| TO: Two soft translaminar cables are passed through the center of the spinous processes at UIV, UIV+1 and UIV−1, then the cable ends are locked to connecters bilaterally between UIV−2 and UIV−3 | 12 (6-26)† | N = 100 | *Age 66 (25-84); M/F 33:67 | Ost. n = 4 *UIV hook n = 42 *Vert.pl. n = 48 |
|
| Rodriguez-Fontan et al 2019
34
Retrospective, Single center |
PS | Minimum 24 | N = 60 | Age 62.1 ± 11.2; M/F 20:40 | Ost. n = 37 Vert.pl. n = 6 |
| TO: 5-mm braded polyethylene tape passed through the spinous process of UIV+1 and looped in a figure 8 way around the infra-adjacent spinous process and eventually tied through a cross-link or to the rods bilaterally. | Minimum 24 | N = 20 | Age 63.2 ± 10.9; M/F 9:11 | Ost. n = 10 Vert.pl. n = 1 |
|
| 2-level prophylactic vertebroplasty (2-PVP) | |||||
| Ghobrial et al 2017
35
Retrospective, Single center |
PS | 27.9 ± 13.4 | N = 47 | *Age 58.3 ± 10.6; *M/F 14:33 | Dec. n = 34, Ost. n = 32 SH n = 15, *ALIF n = 21 |
| 2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 24.2 ± 9.77 | N = 38 | *Age 71.0 ± 6.8; *M/F 23:15 | Dec. n = 5, Ost. n = 28 SH n = 6, *ALIF n = 4 |
|
| Han et al 2019
36
Retrospective, Multi center |
PS | 22.6 ± 11.7 | N = 56 | Age 70.0 ± 5.1; M/F 55:51 | Ost. n = 36, |
| 2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 19.8 ± 13.3 | N = 28 | Age 70.8 ± 7.1 M/F 0:28 | Ost. n = 12 | |
| Hart et al 2008
37
Retrospective, Single center |
PS | 15.5 (13-49) | N = 13 | Age 67.3 (60-77); M/F 0:15 | Unclear |
| 2/3-PVP: Prophylactic vertebroplasty at UIV and UIV+1 and/or UIV−1 | 17.3 (12-44) | N = 15 | Age 73.9 (60-87); M/F 0:13 | ||
| Line et al 2020
32
Prospective, Multi center |
PS | 31.2 (8-83)† | N = 390 | Age 62.2 (19-86); M/F 121:296 | Unclear |
| 2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 31.2 (8-83)† | N = 58 | Age 65.0 (41-84); M/F 11:47 | ||
| Martin et al 2013
38
Prospective, Single center |
2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 32.3 (24-48) | N = 41 | Age 64.4 (41-80); M/F 4:34 | Ost. n = 27 |
| Raman et al 2017
39
Prospective, Single center |
2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 67.9 ± 30.9 | N = 39 | Age 65.6 ± 8.8; M/F 5:34 | Unclear |
| Theologis and Burch 2015
40
Retrospective, Single center |
PS | 24.9 ± 15.4 | N = 23 | *Age 59.8 ± 13.0; M/F 9:14 | Ost. n = 9 |
| 1-PVP at UIV or UIV+1/2-PVP at UIV and UIV−1/3-PVP at UIV, UIV+1 and UIV−1 | 20.4 ± 15.6 | N = 9 | *Age 72.4 ± 7.8; M/F 4:5 | Ost. n = 3 | |
| 2-PVP: Prophylactic vertebroplasty at UIV and UIV+1 | 14.8 ± 8.3 | N = 19 | *Age 68.2 ± 6.3; M/F 9:10 | Ost. n = 6 | |
| Transverse process hooks (TPH) | |||||
| Hassanzadeh et al 2013
41
Retrospective, Single center |
PS | 68.4 (44-88) | N = 27 | Age 51 (20-78); M/F 5:22 | Unclear |
| TPH: Transverse process hooks placed directly lateral to the lateral edge of the pedicle | 33,6 (24-69) | N = 20 | Age 46 (22-78); M/F 3:17 | ||
| Line et al 2020
32
Prospective, Multicentre |
PS | 31.2 (8-83)† | N = 390 | *Age 62.2 (19-86); M/F 121:296 | Unclear |
| TPH: Transverse process hooks at UIV | 31.2 (8-83)† | N = 115 | *Age 58.8 (19-84); M/F 37:78 | ||
| Matsumura et al 2018
42
Retrospective, Single center |
PS | 42.9 (24-91)† | N = 22 | Age 65.5(42-83); M/F 2:37† | Ost. n = 10 Sublaminar taping n = 39 |
| TPH: Transverse process hooks at UIV | 42.9 (24-91)† | N = 17 | Age 69.3 (46-81); M/F 2:37† | ||
| Flexible rod (FR) | |||||
| Lee et al 2019
43
Retrospective, Single center |
Unclear / No-FR | 36.7 ± 9.8 | N = 47 |
Age 71.6 ± 5.1; M/F 2:75† |
*L2 Ost. n = 39, *L5-S1 ALIF n = 35 *L5-S1 PLIF n = 10 *Other OLIFn = 5 *Other PLIF n = 28 |
| FR: Flexible (Ti6Al-4 ELI alloy) rod allowing 15° flexion and 10° extension at the proximal junction. |
16.8 ± 4.7 | N = 30 |
Age 71.8 ± 5.2; M/F 2:75† |
*L2 Ost. n = 10 *L5-S1 ALIF n = 9 *L5-S1 PLIF n = 16 *Other OLIFn = 21 *Other PLIF n = 8 |
|
| Multilevel stabilization screw (MLSS) | |||||
| Sandquist et al 2015
44
Retrospective, Single center |
MLSS: PS at UIV is passed in a superior and oblique manner, ending in the vertebral body of UIV+1 | 30.7 (14-45) | N = 15 | Age 66.3 (44-84); M/F 4:11 | Unclear |
| Sublaminar tapes (ST) | |||||
| Viswanathan et al 2018
45
Prospective, Multi center |
ST: Sublaminar tapes at UIV+1 introduced from the inferior to the superior end bilaterally. | 12 (IQR 6-15) | N = 40 | Age 64 (57-70); M/F 16:24 | Laminectomies, Ost. |
Values are presented as “mean value ± Standard Deviation” or “median (range).”
* Indicates that the mentioned study has reported these values as significantly different between groups.
†Indicates that the mentioned study only reported these values for the entire cohort, not per intervention group.
2-PVP: 2-level prophylactic vertebroplasty, ACP: anterior column procedure, Ant.: anterior, A-, P-, O-LIF: anterior-, posterior-, oblique lumbar interbody fusion, BMI: body mass index (kg/m2), FR: flexible rod, IBF: interbody fusion, Dec: Decompression, IQR: Interquartile range, Levels: amount of levels fused, M/F: male/female ratio, MLSS: multilevel stabilization screws, n: number of patients, PS: pedicle screw at the UIV (control group), Ost.: osteotomy, SH: sublaminar hooks, ST: sublaminar tapes, TC: tether attached to crosslink at the UIV, TO: tether only at the UIV, TPH: transverse process hooks, UIV: upper instrumented vertebrae.
The rod-material used for the spinal fusion was not reported in 15 studies,28-31,33-42,44 and for the remaining 3 studies this was cobalt chromium, stainless steel or titanium.32,43,45 Five studies did not mention if other surgical interventions were performed concomitantly.32,37,39,41,44 In the remaining 13 studies, additional interventions were performed (osteotomies, hooks, vertebroplasty, sublaminar taping, additional fusion or decompression).28-31,33-36,38,40,42,43,45 The mean number of fused segments in the included studies ranged between 6.7 and 16.0 levels, and the constructs ended distally in the sacrum for the majority of patients.
Mean age of the included patients was between 46 and 73.5 years, with 2 studies that reported a mean age below 60 years.31,41 All studies reported the gender of the included patients. Typically, the male-female ratio was skewed, with more female patients. BMI was mentioned in 10 studies, ranging from 21.9 to 31.8 kg/m2.29-32,34,35,38,39,44,45 Preoperative radiographic parameters are presented in Supplementary Table 2.
Risk of Bias
Nine of the studies were judged to hold severe risk of bias and 9 studies at critical risk of bias (see ROBINS-1 score in Table 2). Other major risks of bias found, but not included in the ROBINS-1 score, were: 1) Two studies by Buell et al,29,30 both reporting on the use of tethers, were published within the same time period, so patient populations may be overlapping. 2) Safaee et al 33 analyzed the use of tethers at the UIV compared to a PS control group, however, various combinations of tethers and hook fixation or vertebroplasty at the UIV segment were included in the experimental group. 3) Hassanzadeh et al 41 reported on TPH, in which the follow-up duration in the PS control group was twice as long as in the TPH group (68 versus 34 months). 4) Lee et al 43 reported on the use of FR, but again the follow-up duration of the PS control group was twice as long as in the intervention group (37 versus 17 months). Moreover, major significant differences were found for the patient characteristics between groups for “concomitant surgical procedures” (Table 1).
Table 2.
Risk of Bias Measured Using the ROBINS-I Tool.
| Bias due to confounding | Bias in selection of participants | Bias in classifications of interventions | Bias due to deviations from intended interventions | Bias due to missing outcome data | Bias in measurement of the outcome | Bias in selection of the reported results | Overall risk of bias | |
|---|---|---|---|---|---|---|---|---|
| Alluri et al 2020 28 |

|

|

|

|

|

|

|

|
| Buell et al 2018 29 |

|

|

|

|

|

|

|

|
| Buell et al 2019 30 |

|

|

|

|

|

|

|

|
| Ghobrial et al 2017 35 |

|

|

|

|

|

|

|

|
| Han et al 2019 36 |

|

|

|

|

|

|

|

|
| Hart et al 2008 37 |

|

|

|

|

|

|

|

|
| Hassanzadeh et al 2013 41 |

|

|

|

|

|

|

|

|
| Iyer et al 31 |

|

|

|

|

|

|

|

|
| Lee et al 2019 43 |

|

|

|

|

|

|

|

|
| Line et al 2020 32 |

|

|

|

|

|

|

|

|
| Matsumura et al 2018 42 |

|

|

|

|

|

|

|

|
| Martin et al 2013 38 |

|

|

|

|

|

|

|

|
| Raman et al 2017 39 |

|

|

|

|

|

|

|

|
| Rodriguez-Fontan et al 2019 34 |

|

|

|

|

|

|

|

|
| Safaee et al 2018 33 |

|

|

|

|

|

|

|

|
| Sandquist et al 2015 44 |

|

|

|

|
? |

|

|

|
| Theologis and Burch 2015 40 |

|

|

|

|

|

|

|

|
| Viswanathan et al 2018 45 |

|

|

|

|

|

|

|

|
| Overall risk of bias criteria: Low: low in all domains Moderate: low or moderate in all domains Severe: severe in ≥ 1 domain Critical: critical in ≥ 1 domain |
||||||||
Outcomes
For each study, PJK incidence, Revision Rate for PJK (RR), PJF incidence, reported clinical outcomes and complications were reported in Table 3. Twelve of the included studies reported on PJK incidence,28-31,33-36,38,39,41,43 10 on revision rate for PJK,28-31,33,35,36,38,39,41 13 on PJF incidence,29,32,34-40,42-45 5 on any clinical outcome measure28,38,40,41,45 and 10 on complications.28-30,35-39,41,45 Four studies28-30,37,45 did not elaborate on the type of complications, and could thus not be converted to the classification of Glassman et al. 27 If reported, the clinical outcome measures were further elucidated in Table 4.
Table 3.
Primary and Secondary Outcomes.
| Title | Definition of PJK used in study | Definition of PJF used in study | Group | PJK | RR | PJF incidence | Clinical outcome | Complications |
|---|---|---|---|---|---|---|---|---|
| Tether (tether only (TO) + tether and crosslink (TC)) | ||||||||
| Alluri et al 2020 28 | Postoperative PJA ≥ 20° | PJK necessitating revision surgery | PS | 32% | 18% | NR | ODI*, | All 62% |
| TC | 33% | 0% | NR | ODI*, | All 49% | |||
| Buell et al 2018 29 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | Mechanical failure at UIV or just above and/or proximal junctional posterior discoligamentous failure | PS | 45%* | 5% | 5% | NR | NR |
| TO | 34% | 9% | 9% | NR | “None related to tether” | |||
| TC | 18%* | 4% | 4% | NR | “None related to tether” | |||
| Buell et al 2019 30 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | None, although revision surgery for PJK is mentioned | PS | 55% | 6% | NR | NR | NR |
| TO + TC | 32% | 5% | NR | NR | “None related to tether” | |||
| Iyer et al 2020 31 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | PJF not reported | PS | 29% | 5% | NR | NR | NR |
| TO | 27% | 0% | NR | NR | NR | |||
| Line et al 2020 32 | PJK not reported | PJA ≥ 28.0° and change PJA ≥ 21.6° OR Upper thoracic PJF: proximal junctional anterolisthesis ≥8 mm and change in proximal junctional anterolisthesis ≥8 mm Lower thoracic PJF: proximal junctional anterolisthesis ≥3 mm and change in proximal junctional anterolisthesis ≥3mm |
PS | NR | NR | 20% | NR | NR |
| TO | NR | NR | 16% | NR | NR | |||
| Safaee et al 2018 33 | PJA change ≥ 10° postoperative compared to preoperative value | PJK requiring surgical revision | PS | NR | 18%* | NR | NR | NR |
| TO | 16% | 4%* | NR | NR | NR | |||
| Rodriguez-Fontan et al 34 | PJA change ≥ 10° than pre-op | Symptomatic PJK with or without instrumentation failure and or vertebral fracture at UIV+2 | PS | #38% | NR | #38% | NR | NR |
| TO | #15% | NR | #15% | NR | NR | |||
| 2 level prophylactic vertebroplasty (2-PVP) | ||||||||
| Ghobrial et al 2017 35 | Postoperative PJA ≥ 10° | Revision surgery as a consequence of PJK (Proximal extension of fusion), or refractory pain | PS | 36%* | 13%* | 16% | NR | Major: 16†, Minor: 6† |
| 2-PVP | 24%* | 0%* | 0% | NR | Major: 16†, Minor: 6† | |||
| Han et al 2019 36 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | Bony failure, ligamentous failure, instrument failure (implant breakage and pullout of UIV fixation). | PS | 46% | 14% | 32% | NR | Major 7, Minor 2 |
| 2-PVP | 46% | 4% | 39% | NR | Major 1, Minor 2 | |||
| Hart et al 2008 37 | PJK not reported | Proximal junctional acute collapse requiring extension of instrumented fusion | PS | NR | NR | 15% | NR | NR |
| 2-PVP / 3-PVP | NR | NR | 0 | NR | “None related to 2-PVP” | |||
| Line et al 2020 32 | (see Line et al 2020 above) | (see Line et al 2020 above) | PS | NR | NR | 20% | NR | NR |
| 2-PVP | NR | NR | 12% | NR | NR | |||
| Martin et al 2013 38 | PJA change ≥ 10° postoperative compared to preoperative value | acute proximal junctional fracture/fixation failure or substantial PJK that required revision or extension of the fusion proximally | 2-PVP | 8% | 5% | 5% | ‡ODI, ‡SF-36, ‡SRS-24 | Major 6, Minor 13 |
| Raman et al 2017 39 | PJA change ≥ 10° postoperative compared to preoperative value | Proximal junctional fracture, fixation failure or kyphosis requiring extension of fusion within 6 months of surgery | 2-PVP | 28% | 5% | 5% | NR | Major 21, Minor 19 |
| Theologis and Burch 2015 40 | PJK not reported | Proximal junctional fracture | PS | NR | NR | 21% | ODI*, ‡VAS leg pain | NR |
| PVP | NR | NR | 22% | ‡ODI*, ‡VAS back pain, ‡VAS leg pain | NR | |||
| 2-PVP | NR | NR | 5% | ‡ODI*, ‡EQ-5D, ‡EQ-Vas, ‡VAS back pain, ‡VAS leg pain | NR | |||
| Transverse process hooks (TPH) | ||||||||
| Hassanzadeh et al 2013 41 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | PJF not reported | PS | 30%* | 7%* | NR | ODI*, ‡SRS-22* | Major 7, Minor 15 |
| TPH | 0%* | 0%* | NR | ODI*, ‡SRS-22* | Major 3, Minor 13 | |||
| Line et al 2020 32 | (see Line et al 2020 above) | (see Line et al 2020 above) | PS | NR | NR | 20% | NR | NR |
| TPH | NR | NR | 7% | NR | NR | |||
| Matsumura et al 2018 42 | PJK not reported | Fracture at UIV (Fx) or PJA > 20° (PJA) | PS | NR | NR | 27% (27%PJFx, 0% PJA > 20°) |
NR | NR |
| TPH | NR | NR | 18% (12% PJFx, 6% PJA > 20°) | NR | NR | |||
| Flexible rods (FR) | ||||||||
| Lee et al 2019 43 | Postoperative PJA ≥ 10° and ≥ 10° change than pre-op | Classified as progressive PJK or PJFx | PS | 53%* | NR | 15% | NR | NR |
| 38% | NR | NR | ||||||
| FR | 10%* | NR | 0 | NR | NR | |||
| 0% | NR | NR | ||||||
| Multilevel stabilization screws (MLSS) | ||||||||
| Sandquist et al 2015 44 | PJK not reported | None, although revision surgery for fractures or instrumentation failure at the proximal junction is reported | MLSS | 0% | NR | 0% | NR | NR |
| Sublaminar Tapes (ST) | ||||||||
| Viswanathan et al 2018 45 | PJK not reported | Unclear | SLB | 8% | NR | 0% | ‡ODI, ‡VAS pain,, ‡VAS back pain, ‡SF-36 | Major 9, Minor 27 |
Data is presented as relative value (%).
*Indicates that the mentioned study has reported these values as significantly different between groups.
‡Indicates that the mentioned study reported a significant improvement from pre-operative to final follow-up.
#Indicates that the mentioned study reported PJK and PJF combined, and did not report separate values.
2-PVP: 2-level prophylactic vertebroplasty, FR: flexible rod, MLSS: multilevel stabilization screws, PJA: proximal junctional angle, PJFx: proximal junctional fracture, PS: pedicle screw at the UIV (control group), RR: revision rate for PJK, ST: sublaminar tapes, TC: tether attached to crosslink at the UIV, TO: tether only at the UIV, TPH: transverse process hooks, UIV: upper instrumented vertebrae.
Table 4.
Clinical Outcome Data Presented per Study.
| Author | Clinical outcome measure | Preoperative value | Final follow-up value | Delta | ||
|---|---|---|---|---|---|---|
| Tether (tether only (TO) + tether and crosslink (TC)) | ||||||
| Alluri et al 2020 28 | ODI | PS | 61 | 55* | 6* | |
| TC | 58 | 42* | 16* | |||
| 2 level prophylactic vertebroplasty (2-PVP) | ||||||
| Martin et al 2013 38 | ODI | 82.88 | 25.04‡ | 57.84 | ||
| SF-36 | Physical health | 45.83 | 41.46‡ | 4.37 | ||
| Mental health | 70.2 | 51.21‡ | 18.99 | |||
| SRS-24 | Function/activity | 54.22 | 64.74‡ | 10.52 | ||
| Pain | 44.31 | 70.61‡ | 26.3 | |||
| Mental health | 54.90 | 58.71‡ | 3.81 | |||
| Satisfaction | 53.05 | 74.75‡ | 21.70 | |||
| Theologis and Burch 2015 40 | EQ | VAS | PS | 71 ± 19 (n = 18) | 61 ± 22 (n = 22) | 10 |
| 2-PVP | 63 ± 25 (n = 19) | 74 ± 23 (n = 18) | 11* | |||
| 5-D Utility | PS | 0.44 ± 0.21 (n = 18) | 0.50 ± 0.22 (n = 22) | 0.06 | ||
| 2-PVP | 0.51 ± 0.18 (n = 19) | 0.65 ± 0.22 (n = 18) | 0.14* | |||
| ODI | PS | 52 ± 20 (n = 18) | 47 ± 18 (n = 22)‡ | 5 | ||
| 2-level vertebroplasty | 47 ± 14 (n = 13) | 32 ± 17 (n = 17)‡ | 15* | |||
| VAS | Back pain | PS | 5.9 ± 3.0 (n = 14) | 5.2 ± 1.9 (n = 12) | 0.7 | |
| 2-PVP | 6.8 ± 2.6 (n = 5) | 3.4 ± 3.4 (n = 10) | 3.4* | |||
| Leg pain | PS | 6.0 ± 3.4 (n = 14) | 2.4 ± 2.7 (n = 12) | 3.6* | ||
| 2-PVP | 4.0 ± 3.4 (n = 7) | 1.2 ± 2.0 (n = 10) | 2.8* | |||
| Transverse process hooks (TPH) | ||||||
| Hassanzadeh et al 2013 41 | ODI | PS | 72 (48-90) | 32 (0-54‡ | 40 | |
| TPH | 76 (52-90) | 18 (8-38)‡ | 58 | |||
| SRS-22 | Function | PS | 2.4 (1.7-3) | 3.1 (2.5-3.7)‡ | 0.7* | |
| TPH | 2.4 (1-3.3) | 3.6 (3-4.1)‡ | 1.2* | |||
| Pain | PS | 1.7 (0.3-3.1) | 3.2 (2.6-4.3)‡ | 1.5* | ||
| TPH | 1.8 (0.9-2.4) | 4.3 (3.4-4.8)‡ | 2.5* | |||
| Self-image | PS | 2.1 (0.9-3) | 2.4 (1.2-3.6)‡ | 0.3* | ||
| TPH | 1.8 (0.5-3.4) | 4.2 (2.6-5.3)‡ | 2.4* | |||
| Mental Health | PS | 1.8 (1.1-2.5) | 3 (2.3-3.3)‡ | 1.2* | ||
| TPH | 1.7 (1.2-2.6) | 3.8 (3.2-4.1)‡ | 2.1* | |||
| Satisfaction | PS | 1.2 (0.1-4.5) | 3.4 (2.3-4.6)‡ | 2.2* | ||
| TPH | 1.6 (0-4.1) | 4.3 (3.5-5.5)‡ | 3.2* | |||
| Sublaminar tapes (ST) | ||||||
| Viswanathan 2018 45 |
ODI | 56.0 (45.0-64.0) | 46.0 (22.2-54.0) | 10.0* | ||
| VAS | Pain | 12.5 (0.0-22.5) | 45.0 (22.5-67.5) | 32.5* | ||
| Back pain | 8.0 (6.0-10.0) | 2.0 (0.0-6.0) | 6.0* | |||
| Leg pain | 8.0 (6.0-10.0) | 0.5 (0.0-5.0) | 7.5 | |||
| SF-36 | Physical | 20.0 (5.0-30.0) | 32.5 (17.5-53.8) | 12.5* | ||
| Social functioning | 37.5 (12.5-50.0) | 56.3 (37.5-96.9) | 18.8* | |||
Data is presented as “mean value ± Standard Deviation” or “median (range).”
* Indicates that the mentioned study has reported these values as significantly different between groups.
‡Indicates that the mentioned study reported a significant improvement from pre-operative to final follow-up.
2-PVP: 2-level prophylactic vertebroplasty, PS: pedicle screw at the UIV (control group), ST: sublaminar tapes, TPH: transverse process hooks.
Tether
Seven studies investigated the use of tethers at the proximal junction in various configurations (Figure 1A-E). Alluri et al 28 (n = 83) applied a semitendinosus allograft in an interwoven manner between the spinous processes of the UIV+1 and a crosslink at UIV−2, and compared this to a PS control group (Figure 1A). No differences were found in PJK incidence (33% versus 32% resp., P = 0.766), but the reoperation rate for PJK was found to be significantly higher for PS group (18% versus 0%, P = 0.01). Moreover, the postoperative ODI (42% versus 55%, P = 0.02) and preoperative versus postoperative difference in ODI (+16 versus +6%, P = 0.007) were significantly in favor of the tether group. There was no significant difference in post-operative complication incidence.
Buell et al 29 (n = 184) compared 2 different Mersilene tape configurations to a PS control group (Figure 1B and C). Hand-tightening Mersilene tape threaded through the spinous processes of UIV+1 and UIV−1, compared to a PS control group, provided no significant differences. However, Mersilene tape threaded through the spinous process of UIV+1 and tensioned by caudal displacement of a crosslink fixated between UIV−1 and UIV−2, led to a significant decrease in PJK incidence (18% versus 45%, P = 0.001). No effect on the revision rate for PJK was observed when compared to the PS control group. Another study by Buell et al 30 (n = 120) used similar groups and found no significant effect on PJK and revision rate. Moreover, Line et al 32 (n = 452) used the same technique as Buell et al, 29 hand-tightening Mersilene tape through the spinous processes of UIV+1 and UIV−1, and found no significant beneficial effect on PJF incidence.
In a retrospective single surgeon series (n = 108), Iyer et al 31 instrumented 31 patients with Mersilene tape passed through the spinous processes of UIV+1 and looped below the pedicle screws of the UIV as a tether construct. This tether was repeated between the spinous processes of UIV and the pedicle screws of UIV−1 (Figure 1D). No significant difference in PJK incidence at final follow-up was found between the intervention group (28.6%) and the control group (27.3%).
Safaee et al 33 (n = 200) described another tether configuration, in which 2 cables are passed through the center of the spinous process at UIV, UIV+1 and UIV−1. The individual cable ends were bilaterally locked between UIV−2 and UIV−3 (Figure 1A). A significantly lower revision rate was found when compared to a PS control group, (4% versus 18%, P = 0.002). Unfortunately, the PJK incidence was only mentioned for the tether group (16%) and not for the PS control group. The majority of the included subjects was additionally instrumented with hooks or vertebroplasty at the UIV, with a significantly higher proportion in the tether group.
Lastly, Rodriguez-Fontan et al 34 (n = 80) passed Mersilene tape through the spinous process of UIV+1 and looped this in a figure-8 manner around the infra-adjacent spinous process (Figure 1E). The authors combined the PJK and PJF incidence as their outcome, and found a significant decrease in incidence following their technique (15% versus 38%, P = 0.045).
2-Level Prophylactic Vertebroplasty
Seven studies investigated 2-PVP at UIV and UIV+1 (Figure 1F). Ghobrial et al 35 (n = 85) reported a significantly higher PJK incidence (24% vs 36%, P = 0.020) and revision rate (0 vs 13%, P = 0.031) compared to a PS control group. However, the age was significantly higher in the 2-PVP group and significantly more anterior lumbar interbody fusions had been performed in the PS control group. Another controlled study 36 (n = 84) showed no significant differences between groups, and 2 uncontrolled studies showed an incidence of 8% (n = 41) and 28% (n = 39).38,39 PJF is reported in 5 controlled studies (Ghobrial et al, 35 Han et al, 36 Hart et al 37 (n = 28), Line et al 32 (n = 448) and Theologis and Burch 40 (n = 32)), and 2 uncontrolled studies (Martin et al, 38 Raman et al). In all of these studies, no significant differences were found for PJF incidence between groups.32,35-40
Theologis and Burch 40 reported a significantly better outcome on ODI scale following 2-PVP placement versus the PS control group (P = 0.04) at final follow-up. The other studies did not address clinical outcome. Two studies showed no significant differences in the number of complications between groups,35,36 and an uncontrolled study by Raman et al, 39 which included patients with severe sagittal imbalance, reported relatively high complication rates.
Application of PVP at 1- or 3 levels was investigated in a small group of 9 patients by Theologis and Burch, 40 and showed a similar PJK incidence compared to the PS control group (22% versus 21%). This study with a low number of subjects and significantly younger patients in the PS control group, also reported a significantly higher ODI score for the PVP group (1-PVP and 3-PVP).
Transverse Process Hooks
TPHs at the UIV were investigated in 3 of the included studies (Figure 1G). Hassanzadeh et al 41 (n = 47) found that the PJK incidence and revision rate were significantly lower compared to a PS control group (0 vs. 30%, P = 0.023 and 0 vs 7%, P = n.a. respectively). Moreover, significantly higher ODI and SRS-22 scores were found in the TPH group. The follow-up duration was twice as long for the PS control group and the mean age of the subject in both groups was relatively low (46-51 years). Two other studies on TPH (Line et al 32 (n = 505) and Matsumura et al 42 (n = 39)), found no significant difference with regard to PJF incidence.
Flexible Rods
Lee et al 43 (n = 77) investigated the use of a flexible (Ti6Al-4 ELI alloy) rod allowing 15° flexion and 10° extension at the proximal junction (Figure 1H). Following FR placement, PJK incidence was significantly lower compared to the PS control group (15% versus 38%, P = 0.045). However, follow-up duration of the PS control group was twice as long as in the FR group, and various other surgical interventions were applied with significant differences between the groups. Moreover, based on the preoperative radiographic measurements, the study subjects were relatively sagittally imbalanced compared to the measurements of other studies.
Multilevel Stabilization Screws
In an uncontrolled study by Sandquist et al 44 with a low number of patients (n = 15), MLSS was applied at the UIV. For this technique, the multi-level screws were passed in a superior and oblique manner from UIV to the vertebral body of UIV+1. A PJK and PJF incidence of 0% was found (Figure 1I).
Sublaminar Tapes
Viswanathan et al 45 (n = 40) investigated ST at UIV+1, bilaterally placed in a caudal to cranial fashion, and found a PJK incidence of 8% and a PJF incidence of 0% (Figure 1J). The authors found a significant increase of ODI, VAS pain, VAS back pain and SF-36 scores at the final follow-up, with 9 reported major- and 27 minor complications.
Discussion
This systematic review showed that a variety of PJK and PJF prophylactic spinal instrumentation techniques have been clinically investigated. The most frequently evaluated techniques were posterior tether application (varying configurations) or 2-PVP at the UIV. TPH, FR, MLSS and ST have also been clinically assessed.
Tethers have been applied in multiple studies in various attachment methods, as a means to reinforce the posterior ligamentous complex (PLC). Tethers often seemed to provide a beneficial effect on the occurrence of PJK and the need for revision surgery for PJK. Interestingly, Buell et al 29 reported a beneficial effect on PJK incidence after using a crosslink between UIV−1 and UIV−2 as distal fixation for the tether, instead of fixation to the spinous process of UIV−2. Presumably, the added tension induced by distally moving the crosslink compared to hand tensioned tethers, resulted in a beneficial effect on PJK incidence. This finding is supported by Cho et al, 46 who found significant reductions in flexion range of motion with pretension of 250 N and 350 N in an ex vivo biomechanical test (42% and 57% of native condition respectively). A finite-element analysis by Bess et al 47 reported more gradual transitions in kinematics and lower stresses on the posterior elements after using tethers at UIV+1 in comparison to PS. In the same study, applying tethers at multiple levels further improved these results compared to constructs with TPH or PS at UIV. Additional in vitro biomechanical research is required to determine the optimal magnitude of pretension of the tether at the proximal segment. Moreover, controlled studies assessing the optimal configuration of the tethers are needed.
2-PVP provided a significantly lower revision rate and PJK incidence in comparison to PS fixation in one study, 35 and lower overall PJF incidences were seen compared to the PS group. 1-PVP and 3-PVP were also assessed in a very small sub-group, but no difference in PJF incidence was observed in comparison to the PS control group. 40 Although the clinical evidence is meager, the authors speculated that 1-PVP is likely to increase stress on the proximal segment, and 2-PVP may provide a larger transitional zone for axial forces. 48 One of the studies found a beneficial effect on PJK incidence and revision rate after 2-PVP in elderly patients compared to PS in younger patients, suggesting a protective effect in patients with lower BMD. 35 Moreover, 2-PVP could prevent progressive vertebral height loss in case a proximal junctional fracture (PJFx) would occur, and seemed to limit the post-operative kyphotic progression of the proximal junction, possibly also contributing to the lower revision rate for PJK. 36 Nevertheless, this was not reflected in the clinical outcome. Only one of the studies found a significant beneficial effect of 2-PVP on any of the reported HRQoL scores (ODI). Due to the uncontrolled designs of the included studies, controlled trials incorporating 2-PVP as PJK and PJF prophylactic method are needed to support these promising findings.
TPH was shown to achieve a lower incidence of PJK, revision rates, and PJF. In a single study with a small patient population with a relatively low mean age, and major differences in follow-up duration between groups, it was found that application of TPH demonstrated a 0% PJK incidence and 0% revision rates for PJK. 41 However, 2 other studies found no significant difference in PJF incidence compared to the PS group. Finally, Matsumura et al 42 found that if a PJFx occurred, the vertebral body collapse and PJA increase was less severe following TPH compared to pedicle screws. For future research, it is important to consider the bone mineral density (BMD), and its effect on the success rate of TPH. It is known that in the adult patient, BMD in the transverse process is lowest and highest in the lamina. 49 Despite lacking a control group, one of the included studies assessing ST found promising results expressed by a lower PJK incidence. 45 We therefore recommend future clinical studies assessing TPH and ST to report the incidence of instrumentation breakout in their analysis, especially in patients presenting with osteopenia or osteoporosis.
A single low quality study analyzing MLSS found a PJK and PJF incidence of 0%. Sandquist et al 44 argue that placement of MLSS is safe in the upper thoracic spine and minimizes dissection and disruption of the cephalad posterior elements. Similarly, flexible rods were found to lower incidences of PJK (10%) compared to PS fixation (53%) in a low quality study with major risk of bias. Moreover, if PJK occurred, it seemed to be of less progressive nature. 43 Further research is needed for more reliable outcome data on both techniques.
Although most studies reported a favorable effect of the investigated technique on PJK and PJF incidence, few studies reported on clinical outcome and only 2 studies (on TPH and 2-PVP) found a significantly better clinical outcome compared to the control group.40,41 Previous studies have shown that clinical outcome in PJK and non-PJK patients is similar.19,20 However, unlike PJK, multiple studies show that the occurrence of PJF correlates with a worse clinical outcome.7,11 For this reason, the clinical relevance of assessing the success of PJK and PJF prophylactic techniques based on radiographic measurements seems questionable. Future studies should consider clinical outcome measures in the evaluation of prophylaxis success.
Most of the techniques addressed in this review have also been assessed biomechanically.50,51 However, to determine the optimal PJK and PJF prophylactic technique, the relationship between biomechanical findings and clinical performance must be further elucidated. Also, patient demographics such as a higher age (>60 years), low BMD, and pre-existing comorbidities, and surgical characteristics such as a higher number of fused levels, use of bilateral pedicle screws at UIV, fusion to S1, revision surgery, anterior or combined anteroposterior approaches, additional osteotomies and UIV in the lower thoracic spine must be carefully controlled in clinical trials. The large number of possible confounding factors warrant the design of large multi-center trials. Likewise, it is advised to carefully report radiographic parameters indicating the extend of pre- and postoperative sagittal imbalance, and incorporate the amount of sagittal correction in the decision making process of the surgeon.17,18,52-54 Furthermore, some low-quality studies suggest that a combination of tethers, hooks and/or vertebroplasty may provide further reduction of PJK and revision rates for PJK.32,33 However, we advise to first assess the effect per technique in, for example, a matched-cohort study.
Strengths and Limitations
Several limitations should be considered when interpreting the results of the current review. Major differences in reported outcomes were found between different studies that investigated similar interventions. We were only able to include nonrandomized cohort studies, with severe or critical risk of bias. Moreover, the included studies were heterogeneous with regard to the investigated intervention, study design, patient characteristics, follow-up duration and reported outcomes. The effect of differences in follow-up duration on the reported PJK and PJF incidence rates could be limited, since only studies with >12 months of follow-up duration were included, and both PJK and PJF typically present within the first 3 months after surgery. Furthermore, we have included studies that involved constructs ending proximally at the higher thoracic spine and the thoracolumbar junction. However, it seems that the mode of failure in the thoracic spine differs between the upper- and the lower-region. Generally, a higher incidence of PJK is found if the UIV is in the lower thoracic spine or thoracolumbar region compared to the upper thoracic spine. 6 Our goal was to provide a clear overview of the and clinically investigated techniques. Unfortunately, due to the heterogeneity of the studies and used techniques, quantitative comparison of the data was not considered feasible.
Conclusion
Although the clinical relevance of preventing PJK and PJF in the ASD population is eminent, the exact etiology of PJK and PJF remain unclear. The prophylactic techniques identified, focus on creating a semi-rigid transition proximal to the instrumented vertebrae in an effort to reduce junctional level stresses, or reinforcement of the anterior column to increase the fracture resistance of vertebrae. Although the studies included in this review are of low quality, current literature provides insight into the potential effectiveness of these interventions. The most frequently studied techniques, namely 2-PVP as anterior reinforcement and tethers or TPH as posterior semi-rigid fixation, show promising results. More controlled studies are required to provide a reliable comparison, including the use of clinical outcome measures and a uniform definition of PJF.
Supplemental Material
Supplemental Material, sj-docx-1-gsj-10.1177_21925682211034500 for Instrumentation Techniques to Prevent Proximal Junctional Kyphosis and Proximal Junctional Failure in Adult Spinal Deformity Correction: A Systematic Review of Clinical Studies by Timon F. G. Vercoulen, Remco J. P. Doodkorte, Alex Roth, Rob de Bie and Paul C. Willems in Global Spine Journal
Footnotes
Authors’ Note: This research was performed within the Chemelot InSciTe framework and the authors have no financial or competing interests related to this work. The devices that are subject in the included studies of this manuscript may be investigational or products not FDA-approved for the indication. Moreover, not all products are commercially available in the United States.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Timon F. G. Vercoulen, MD  https://orcid.org/0000-0002-0181-7907
https://orcid.org/0000-0002-0181-7907
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Arlet V, Aebi M. Junctional spinal disorders in operated adult spinal deformities: present understanding and future perspectives. Eur Spine J. 2013;22(suppl 2):S276–S295. doi:10.1007/s00586-013-2676-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bridwell KH, Lenke LG, Cho SK, et al. Proximal junctional kyphosis in primary adult deformity surgery: evaluation of 20 degrees as a critical angle. Neurosurgery. 2013;72(6):899–906 doi:10.1227/NEU.0b013e31828bacd8 [DOI] [PubMed] [Google Scholar]
- 3.Faundez AA, Richards J, Maxy P, Price R, Léglise A, Le Huec JC. The mechanism in junctional failure of thoraco-lumbar fusions. Part II: analysis of a series of PJK after thoraco-lumbar fusion to determine parameters allowing to predict the risk of junctional breakdown. Eur Spine J. 2018;27(suppl 1):139–148. doi:10.1007/s00586-017-5426-7 [DOI] [PubMed] [Google Scholar]
- 4.Glattes RC, Bridwell KH, Lenke LG, Kim YJ, Rinella A, Edwards C. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976). 2005;30(14):1643–1649. doi:10.1097/01.brs.0000169451.76359.49 [DOI] [PubMed] [Google Scholar]
- 5.Hart RA, McCarthy I, Ames CP, Shaffrey CI, Hamilton DK, Hostin R. Proximal junctional kyphosis and proximal junctional failure. Neurosurg Clin N Am. 2013;24(2):213–218. doi:10.1016/j.nec.2013.01.001 [DOI] [PubMed] [Google Scholar]
- 6.Hostin R, McCarthy I, O’Brien M, et al. International Spine Study Group. Incidence, mode, and location of acute proximal junctional failures after surgical treatment of adult spinal deformity. Spine (Phila Pa 1976). 2013;38(12):1008–1015. doi:10.1097/BRS.0b013e318271319c [DOI] [PubMed] [Google Scholar]
- 7.Hyun SJ, Lee BH, Park JH, Kim KJ, Jahng TA, Kim HJ. Proximal junctional kyphosis and proximal junctional failure following adult spinal deformity surgery. Korean J Spine. 2017;14(4):126–132. doi:10.14245/kjs.2017.14.4.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim HJ, Iyer S. Proximal junctional kyphosis. J Am Acad Orthop Surg. 2016;24(5):318–326. doi:10.5435/jaaos-d-14-00393 [DOI] [PubMed] [Google Scholar]
- 9.Kim HJ, Lenke LG, Shaffrey CI, Van Alstyne EM, Skelly AC. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: a systematic review. Spine (Phila Pa 1976). 2012;37(22 suppl):S144–S164. doi:10.1097/BRS.0b013e31826d611b [DOI] [PubMed] [Google Scholar]
- 10.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008;33(20):2179–2184. doi:10.1097/BRS.0b013e31817c0428 [DOI] [PubMed] [Google Scholar]
- 11.Lau D, Clark AJ, Scheer JK, et al. SRS Adult Spinal Deformity Committee. Proximal junctional kyphosis and failure after spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014;39(25):2093–2102. doi:10.1097/brs.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 12.Lee J, Park YS. Proximal junctional kyphosis: diagnosis, pathogenesis, and treatment. Asian Spine J. 2016;10(3):593–600. doi:10.4184/asj.2016.10.3.593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JH, Kim JU, Jang JS, Lee SH. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: minimum 2-year follow-up. Br J Neurosurg. 2014;28(2):252–258. doi:10.3109/02688697.2013.835369 [DOI] [PubMed] [Google Scholar]
- 14.Liu FY, Yang SD, Huo LS, Wang T, Yang DL, Ding WY. Incidence and risk factors for proximal junctional kyphosis: a meta-analysis. Eur Spine J. 2016;25(8):2376–2383. doi:10.1007/s00586-016-4534-0 [DOI] [PubMed] [Google Scholar]
- 15.Nguyen N-LM, Kong CY, Hart RA. Proximal junctional kyphosis and failure-diagnosis, prevention, and treatment. Curr Rev Musculoskelet Med. 2016;9(3):299–308. doi:10.1007/s12178-016-9353-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Segreto FA, Passias PG, Lafage R, et al. Incidence of acute, progressive, and delayed proximal junctional kyphosis over an 8-year period in adult spinal deformity patients. Oper Neurosurg (Hagerstown). 2020;18(1):75–82. doi:10.1093/ons/opz128 [DOI] [PubMed] [Google Scholar]
- 17.Smith MW, Annis P, Lawrence BD, Daubs MD, Brodke DS. Early proximal junctional failure in patients with preoperative sagittal imbalance. Evid Based Spine Care J. 2013;4(2):163–164. doi:10.1055/s-0033-1357366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith MW, Annis P, Lawrence BD, Daubs MD, Brodke DS. Acute proximal junctional failure in patients with preoperative sagittal imbalance. Spine J. 2015;15(10):2142–2148. doi:10.1016/j.spinee.2015.05.028 [DOI] [PubMed] [Google Scholar]
- 19.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36(1):E60–E68. doi:10.1097/BRS.0b013e3181eeaee2 [DOI] [PubMed] [Google Scholar]
- 20.Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 2012;37(17):1479–1489. doi:10.1097/BRS.0b013e31824e4888 [DOI] [PubMed] [Google Scholar]
- 21.Diebo BG, Shah NV, Stroud SG, Paulino CB, Schwab FJ, Lafage V. Realignment surgery in adult spinal deformity: prevalence and risk factors for proximal junctional kyphosis. Orthopade. 2018;47(4):301–309. doi:10.1007/s00132-018-3536-5 [DOI] [PubMed] [Google Scholar]
- 22.Park SJ, Lee CS, Chung SS, Lee JY, Kang SS, Park SH. Different risk factors of proximal junctional kyphosis and proximal junctional failure following long instrumented fusion to the sacrum for adult spinal deformity: survivorship analysis of 160 patients. Neurosurgery. 2017;80(2):279–286. doi:10.1227/neu.0000000000001240 [DOI] [PubMed] [Google Scholar]
- 23.Shamseer L, Moher D, Clarke M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. doi:10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 24.Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104(3):240–243. doi:10.3163/1536-5050.104.3.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid AK. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi:10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi:10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976). 2007;32(24) 2764–2770. doi:10.1097/BRS.0b013e31815a7644 [DOI] [PubMed] [Google Scholar]
- 28.Alluri R, Kim A, Ton A, Kang H, Acosta F, Hah R. Semitendinosus tendon augmentation for prevention of proximal junctional failure. Spine (Phila Pa 1976). 2021;46(4):241–248. doi:10.1097/brs.0000000000003765 [DOI] [PubMed] [Google Scholar]
- 29.Buell TJ, Buchholz AL, Quinn JC, et al. A pilot study on posterior polyethylene tethers to prevent proximal junctional kyphosis after multilevel spinal instrumentation for adult spinal deformity. Oper Neurosurg (Hagerstown). 2019;16(2):256–266. doi:10.1093/ons/opy065 [DOI] [PubMed] [Google Scholar]
- 30.Buell TJ, Chen CJ, Quinn JC, et al. Alignment risk factors for proximal junctional kyphosis and the effect of lower thoracic junctional tethers for adult spinal deformity. World Neurosurg. 2019;121:e96–e103. doi:10.1016/j.wneu.2018.08.242 [DOI] [PubMed] [Google Scholar]
- 31.Iyer S, Lovecchio F, Elysée JC, et al. Posterior ligamentous reinforcement of the upper instrumented vertebrae +1 does not decrease proximal junctional kyphosis in adult spinal deformity. Global Spine J. 2020;10(6):692–699. doi:10.1177/2192568219868472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Line BG, Bess S, Lafage R, et al. International Spine Study Group. Effective prevention of proximal junctional failure in adult spinal deformity surgery requires a combination of surgical implant prophylaxis and avoidance of sagittal alignment overcorrection. Spine (Phila Pa 1976). 2020;45(4):258–267. doi:10.1097/BRS.0000000000003249 [DOI] [PubMed] [Google Scholar]
- 33.Safaee MM, Deviren V, Dalle Ore C, et al. Ligament augmentation for prevention of proximal junctional kyphosis and proximal junctional failure in adult spinal deformity. J Neurosurg Spine. 2018;28(5):512–519. doi:10.3171/2017.9.SPINE1710 [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez-Fontan F, Reeves BJ, Noshchenko A, et al. Strap stabilization for proximal junctional kyphosis prevention in instrumented posterior spinal fusion. Eur Spine J. 2020;29(6):1287–1296 doi:10.1007/s00586-020-06291-0 [DOI] [PubMed] [Google Scholar]
- 35.Ghobrial GM, Eichberg DG, Kolcun JPG, et al. Prophylactic vertebral cement augmentation at the uppermost instrumented vertebra and rostral adjacent vertebra for the prevention of proximal junctional kyphosis and failure following long-segment fusion for adult spinal deformity. Spine J. 2017;17(10):1499–1505. doi:10.1016/j.spinee.2017.05.015 [DOI] [PubMed] [Google Scholar]
- 36.Han S, Hyun SJ, Kim KJ, et al. Effect of vertebroplasty at the upper instrumented vertebra and upper instrumented vertebra +1 for prevention of proximal junctional failure in adult spinal deformity surgery: a comparative matched-cohort study. World Neurosurg. 2019;S1878–S8750(18)32936–X. doi:10.1016/j.wneu.2018.12.113 [DOI] [PubMed] [Google Scholar]
- 37.Hart RA, Prendergast MA, Roberts WG, Nesbit GM, Barnwell SL. Proximal junctional acute collapse cranial to multi-level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J. 2008;8(6):875–881. doi:10.1016/j.spinee.2008.01.015 [DOI] [PubMed] [Google Scholar]
- 38.Martin CT, Skolasky RL, Mohamed AS, Kebaish KM. Preliminary results of the effect of prophylactic vertebroplasty on the incidence of proximal junctional complications after posterior spinal fusion to the low thoracic spine. Spine Deform. 2013;1(2):132–138. doi:10.1016/j.jspd.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 39.Raman T, Miller E, Martin CT, Kebaish KM. The effect of prophylactic vertebroplasty on the incidence of proximal junctional kyphosis and proximal junctional failure following posterior spinal fusion in adult spinal deformity: a 5-year follow-up study. Spine J. 2017;17(10):1489–1498. doi:10.1016/j.spinee.2017.05.017 [DOI] [PubMed] [Google Scholar]
- 40.Theologis AA, Burch S. Prevention of acute proximal junctional fractures after long thoracolumbar posterior fusions for adult spinal deformity using 2-level cement augmentation at the upper instrumented vertebra and the vertebra 1 level proximal to the upper instrumented vertebra. Spine (Phila Pa 1976). 2015;40(19):1516–1526. doi:10.1097/brs.0000000000001043 [DOI] [PubMed] [Google Scholar]
- 41.Hassanzadeh H, Gupta S, Jain A, El Dafrawy MH, Skolasky RL, Kebaish KM. Type of anchor at the proximal fusion level has a significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform. 2013;1(4):299–305. doi:10.1016/j.jspd.2013.05.008 [DOI] [PubMed] [Google Scholar]
- 42.Matsumura A, Namikawa T, Kato M, et al. Effect of different types of upper instrumented vertebrae instruments on proximal junctional kyphosis following adult spinal deformity surgery: pedicle screw versus transverse process hook. Asian Spine J. 2018;12(4):622–631. doi:10.31616/asj.2018.12.4.622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee KY, Lee JH, Kang KC, Shin WJ, Im SK, Cho SJ. Preliminary report on the flexible rod technique for prevention of proximal junctional kyphosis following long-segment fusion to the sacrum in adult spinal deformity. J Neurosurg Spine. 2019:1–8. doi:10.3171/2019.4.SPINE1915 [DOI] [PubMed] [Google Scholar]
- 44.Sandquist L, Carr D, Tong D, Gonda R, Soo TM. Preventing proximal junctional failure in long segmental instrumented cases of adult degenerative scoliosis using a multilevel stabilization screw technique. Surg Neurol Int. 2015;6:112. doi:10.4103/2152-7806.159383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Viswanathan VK, Kukreja S, Minnema AJ, Farhadi HF. Prospective assessment of the safety and early outcomes of sublaminar band placement for the prevention of proximal junctional kyphosis. J Neurosurg Spine. 2018;28(5):520–531. doi:10.3171/2017.8.Spine17672 [DOI] [PubMed] [Google Scholar]
- 46.Cho SK, Caridi J, Kim JS, Cheung ZB, Gandhi A, Inzana J. Attenuation of proximal junctional kyphosis using sublaminar polyester tension bands: a biomechanical study. World Neurosurg. 2018;120:e1136–e1142. doi:10.1016/j.wneu.2018.08.244 [DOI] [PubMed] [Google Scholar]
- 47.Bess S, Harris JE, Turner AW, et al. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine. 2017;26(1):125–133. doi:10.3171/2016.6.SPINE151477 [DOI] [PubMed] [Google Scholar]
- 48.Kebaish KM, Martin CT, O’Brien JR, LaMotta IE, Voros GD, Belkoff SM. Use of vertebroplasty to prevent proximal junctional fractures in adult deformity surgery: a biomechanical cadaveric study. Spine J. 2013;13(12):1897–1903. doi:10.1016/j.spinee.2013.06.039 [DOI] [PubMed] [Google Scholar]
- 49.Hohn EA, Chu B, Martin A, et al. The pedicles are not the densest regions of the lumbar vertebrae: implications for bone quality assessment and surgical treatment strategy. Global Spine J. 2017;7(6):567–571. doi:10.1177/2192568217694141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shay B, Jeffrey EH, Alexander WLT, et al. The effect of posterior polyester tethers on the biomechanics of proximal junctional kyphosis: a finite element analysis. J Neurosurg Spine. 2017;26(1):125–133. doi:10.3171/2016.6.SPINE151477 [DOI] [PubMed] [Google Scholar]
- 51.Doodkorte RJP, Roth AK, Arts JJ, Lataster LMA, van Rhijn LW, Willems PC. Instrumentation techniques to prevent proximal junctional kyphosis and proximal junctional failure in adult spinal deformity correction—a systematic review of biomechanical studies. Spine J. 2021;21(5):855–864. doi:10.1016/j.spinee.2021.01.011 [DOI] [PubMed] [Google Scholar]
- 52.Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 2014;39(9):E576–E580. doi:10.1097/brs.0000000000000246 [DOI] [PubMed] [Google Scholar]
- 53.Watanabe K, Lenke LG, Bridwell KH, Kim YJ, Koester L, Hensley M. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine (Phila Pa 1976). 2010;35(2):138–145. doi:10.1097/BRS.0b013e3181c8f35d [DOI] [PubMed] [Google Scholar]
- 54.Yagi M, Rahm M, Gaines R, et al. Complex Spine Study Group. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976). 2014;39(10):E607–614. doi:10.1097/brs.0000000000000266 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-gsj-10.1177_21925682211034500 for Instrumentation Techniques to Prevent Proximal Junctional Kyphosis and Proximal Junctional Failure in Adult Spinal Deformity Correction: A Systematic Review of Clinical Studies by Timon F. G. Vercoulen, Remco J. P. Doodkorte, Alex Roth, Rob de Bie and Paul C. Willems in Global Spine Journal