Abstract
Study Design:
Literature review.
Objectives:
An increasing number of obese patients requires operative care for degenerative spinal disorders. The aim of this review is to analyze the available evidence regarding the role of obesity on outcomes after spine surgery. Peri-operative complications and clinical results are evaluated for both cervical and lumbar surgery. Furthermore, the contribution of MIS techniques for lumbar surgery to play a role in reducing risks has been analyzed.
Methods:
Only articles published in English in the last 10 years were reviewed. Inclusion criteria of the references were based on the scope of this review, according to PRISMA guidelines. Moreover, only paper analyzing obesity-related complications in spine surgery have been selected and thoroughly reviewed. Each article was classified according to its rating of evidence using the Sacket Grading System.
Results:
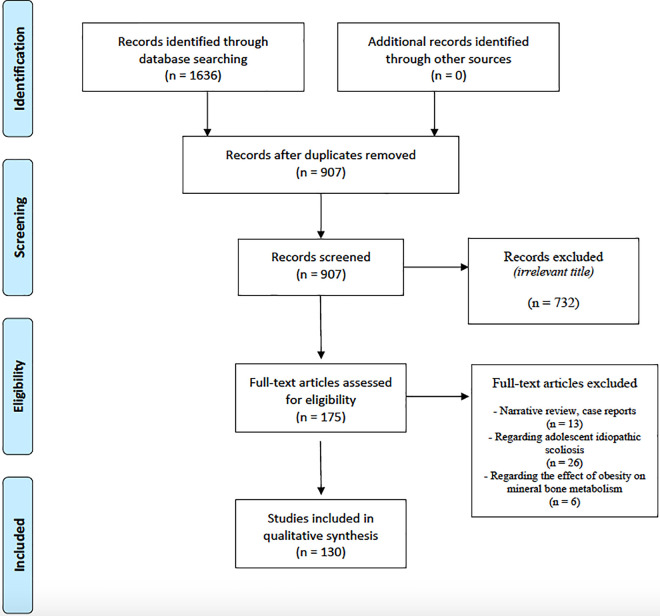
A total number of 1636 articles were found, but only 130 of them were considered to be relevant after thorough evaluation and according to PRISMA checklist. The majority of the included papers were classified according to the Sacket Grading System as Level 2 (Retrospective Studies).
Conclusion:
Evidence suggest that obese patients could benefit from spine surgery and outcomes be satisfactory. A higher rate of peri-operative complications is reported among obese patients, especially in posterior approaches. The use of MIS techniques plays a key role in order to reduce surgical risks. Further studies should evaluate the role of multidisciplinary counseling between spine surgeons, nutritionists and bariatric surgeons, in order to plan proper weight loss before elective spine surgery.
Keywords: obesity, spine, spine surgery, weight loss, minimally-invasive techniques, bariatric surgery, bariatrics
Introduction
Obesity is defined by the WHO as a BMI equal or higher than 30 Kg/m2. However, obese patients are often subdivided in: 1) Class I obese (BMI: 30 34.9 Kg/m2), 2) Class II obese (BMI: 35-39.9 Kg/m2) and 3) Class III obese (also defined as morbidly obese) (BMI ≥ 40 Kg/m2). 1
The strict association between obesity and numerous diseases such as Type 2 diabetes, hypertension, cardiovascular diseases and several types of cancer has been extensively outlined, reporting also a higher mortality rate among these patients. 1 In 2009, a landmark collaborative analysis of 57 prospective studies, including about 900 000 adults, reported significative reduction of life-expectancy for patients exceeding the BMI range of normal weight, being BMI itself a strong predictor of overall mortality both above and below the apparent optimum of about 22.5-25 Kg/m2. In particular, the authors reported a reduction of median survival of 2-4 years in the 30-35 Kg/m2 group and of 8-10 years in the 40-45 Kg/m2. 2
Obesity represents 1 of the most relevant concerns of the modern health systems: approximatively 13% of the world’s adult population resulted to be obese in the 2014 and, consistent with the more recent estimations, 1.9 billion of adult patients resulted obese in the 2016.3-5 In addition to BMI-related increase in mortality, obesity also represents a significant factor influencing the quality of life. Low back pain (LBP), indeed, represents 1 of the main complaints of obese patients, being the fifth most common reason for medical consultations in the United States. 6 As well demonstrated, obesity related diseases and lifestyle restrictions could represent crucial risk factors for musculoskeletal disorders, including degenerative conditions of the spine, namely degenerative disc disease, stenosis and spondylolisthesis.3,7-10
However, albeit the independent high prevalence of both obesity and LBP makes easily expected that they could share coexisting comorbidities in the population, there are some evidences of an existing association between degenerative spine disease and obesity,6,8,11 although the way of this relationship is still not clear. In a meta-analysis by Dario et al, that investigated the influences of genetics and shared environment on the association between obesity and LBP or lumbar degenerative disease (LDD), the authors reported that the risk of having LBP for patients with high levels of BMI was almost twice that of patients with lower BMI values (odds ratio (OR) 1.8). However, analyzing twin studies, the authors did not find a significative causal relationship between obesity and LDD. 12 Hence, a 2 way-relationship could underlie obesity, LDD and LBP, whereby the obesity and reduced mobilization exacerbate the pain increasing the demand on the musculoskeletal system, and the pain burden on QoL could incline obese patients to sedentary lifestyle, a key-factor of the inability to lose weight.13,14
Due to the aging of the population and to the rising prevalence of obesity, an increasing number of obese patients, suffering from LDD, is asking to be evaluated for spine surgery, in order to reduce the impact of pain on their life.6,11,15,16 This phenomenon has led spine surgeons to tackle a challenging problem, namely the effort to balance the patients’ legitimate need for pain relief with the reported increased risk of post-operative complications that is closely related to obesity. Furthermore, surgeons have to face against surgical risk for complications of this patients’ population, due to the high incidence of comorbidities (e.g. diabetes, hypertension, sleep apnea). 17 Notably, indeed, higher risk for wound infections, dural tears, anemia, deep vein thrombosis and pulmonary embolism is usually reported for obese patients undergoing spinal fusion.3,18-20 However, despite several studies—investigating complications rate in gynecological, orthopedic, cardiovascular and general surgeries21-23—carved out the increased peri-operative risk of obese patients undergoing surgery, there is a not negligible amount of literature that did not report significatively higher risk.24,25 Likewise, this specific relationship between post-operative complications in spine surgery for obese patients was not so clear and numerous studies are still investigating this aspect.18,26-28 In a retrospective cohort study analyzing 332 patients undergoing lumbar and / or thoracic spine fusion, Patel et al firstly reported that patients with higher BMI were more likely to experience post-operative complications; the chance of significative complication (event that lengthened hospital stay or delayed recovery) resulted to be 14% with a BMI of 25, 20% with a BMI of 30 and 36% with a BMI of 35. Additionally, although several studies now revealed a higher complication rate, inferior clinical outcomes among obese population have not been consistently demonstrated being the topic still controversial.29-40 Puvanesarajah et al investigated the role of obesity on 90-day complication rates and 30-day readmission rates following 1- to 2-level, primary, lumbar spinal fusion surgery for degenerative pathology in an elderly population. Obese patients resulted to have significantly higher odds of suffering from any 1 major medical complication (odds ratio [OR] 1.79). Moreover, also wound infection and dehiscence rates were increased in obese patients (ORs 3.71 and 3.8 respectively). Additionally, obesity resulted able to significantly increase length of stay and hospital costs ($8000 greater than controls).41,42 On the other hand, during the last years, the surgical evolution has led to even more Minimally Invasive Surgery (MIS) techniques, reporting less blood loss, reduced post-operative pain, shorter length of stay and encouraging long terms outcomes when compared with classical open techniques.43-47
Thus, several studies enrolling obese patients have been performed, with the aim to evaluate the feasibility of MIS techniques among this high-risky population, and to investigate whether the reported good clinical outcomes and lower complication rate could widen the surgical indication for obese patients.4,7,18,28,48-54
The aim of this review is to globally analyze the available evidence regarding the role of obesity on outcomes after spine surgery: after brief metabolic considerations, their impact on peri-operative complications and clinical results is evaluated investigating separately both cervical and lumbar surgery. Furthermore, the contribution of MIS techniques for lumbar surgery to play a role in reducing risks has been analyzed. Finally, starting points for future researches on this topic according to the Literature will be outlined.
Methods
Selection criteria and references for this review were identified by searching PubMed database using the following research strings: “obesity related complications AND degenerative spine fusion surgery”; “obesity AND spine fusion”; “degenerative spine surgery AND obese patients”; “degenerative spine surgery AND obesity related complications”; “obesity related complications AND degenerative spine fusion surgery”; “spine fusion AND obesity related complications”; “spine surgery OR obese patients”; “spine fusion OR obesity morbidity”; “obesity related complications OR spine fusion surgery”; “obesity related complications AND minimally invasive spine surgery”; “obesity related complications AND indirect decompression”; “obesity related complications AND anterior lumbar inter body fusion”; “obesity related complications AND transpsoas access for lumbar fusion; “obesity related complications AND minimally invasive Transforaminal Interbody Fusion.”
Only articles published in English in the last 10 years until January 31, 2021 were reviewed. Inclusion criteria of the references were based on the scope of this review, according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) guidelines. 55
Therefore, only articles analyzing spine fusion for degenerative disease in obese patients have been considered, while narrative review articles and case report have been excluded, as for papers regarding the influence of obesity in spine fusion for adolescent idiopathic scoliosis.
Moreover, according with the first aim of this review, only paper analyzing obesity-related complications in spine surgery have been selected and thoroughly reviewed. Hence, each article was classified according to its rating of evidence using the Sacket Grading System 56 (Table 1).
Table 1.
Review of the Literature With Evidence Levels Classification (According to Sacket Grading System).
| Study number | Reference | Type of study | Evidence rate |
|---|---|---|---|
| 1 | Mulvaney G et al, 2021 57 | Retrospective study | 2 |
| 2 | Paranjape CS et al, 2021 58 | Retrospective study | 2 |
| 3 | Chan AK et al, 2020 5 | Retrospective study | 2 |
| 4 | Divi SN et al, 2020 59 | Retrospective study | 2 |
| 5 | Duan PG et al, 2020 60 | Retrospective study | 2 |
| 6 | Fatima N et al, 2020 61 | Retrospective study | 2 |
| 7 | He X et al, 2020 62 | Retrospective cohort study | 3 |
| 8 | Jain D et al, 2020 63 | Retrospective study | 2 |
| 9 | Jenkins NW et al, 2020 64 | Retrospective study | 2 |
| 10 | Khan JM et al, 2020 65 | Retrospective cohort study | 3 |
| 11 | Katsevman GA et al, 2020 66 | Retrospective study | 2 |
| 12 | Othman YA et al, 2020 67 | Meta-analysis | 1 |
| 13 | Malik AT et al, 2020 68 | Retrospective cohort study | 3 |
| 14 | Passias PG et al, 2020 42 | Retrospective study | 2 |
| 15 | Qi M et al, 2020 69 | Retrospective study | 2 |
| 16 | Safaee MM et al, 2020 70 | Retrospective study | 2 |
| 17 | Siccoli A et al, 2020 71 | Retrospective study | 2 |
| 18 | Sridharan M et al, 2020 72 | Retrospective study | 2 |
| 19 | Xi Z et al, 2020 73 | Retrospective study | 2 |
| 20 | Basques et al, 2019 74 | Retrospective cohort study | 3 |
| 21 | Buyuk AF et al, 2019 75 | Retrospective cohort study | 3 |
| 22 | Cheng CW et al, 2019 76 | Retrospective cohort study | 3 |
| 23 | Goh GS et al, 2019 77 | Retrospective study | 2 |
| 24 | Goyal A et al, 2019 78 | Meta-analysis | 1 |
| 25 | Elsamadicy et al, 2019 40 | Retrospective study | 2 |
| 26 | Kashkoush A et al, 2019 79 | Retrospective study | 2 |
| 27 | Kru?ger et al, 2019 4 | Retrospective study | 2 |
| 28 | Linhares D et al, 2019 80 | Prospective study | 1 |
| 29 | Malik AT et al, 2019 81 | Retrospective study | 2 |
| 30 | Mombell KW et al, 2019 82 | Retrospective study | 2 |
| 31 | Villavicencio et al, 2019 83 | Retrospective study | 2 |
| 32 | Yoo JS et al, 2019 84 | Retrospective study | 2 |
| 33 | Zhang G.A. et al, 2019 18 | Meta-analysis | 1 |
| 34 | Zhang Y. et al, 2019 85 | Retrospective study | 2 |
| 35 | Abbasi H et al, 2018 86 | Retrospective cohort study | 3 |
| 36 | Akins et al, 2018 87 | Retrospective cohort study | 3 |
| 37 | Bono OJ et al, 2018 88 | Retrospective study | 2 |
| 38 | Byval’tsev VA et al, 2018 89 | Retrospective cohort study | 3 |
| 39 | Chung AS et al, 2018 90 | Retrospective cohort study | 3 |
| 40 | Jain et al, 2018 91 | Retrospective cohort study | 3 |
| 41 | Lovecchio F et al, 2018 92 | Retrospective cohort study | 3 |
| 42 | Madsbu MA et al, 2018 93 | Retrospective study | 2 |
| 43 | Nahhas CR et al, 2018 94 | Retrospective study | 2 |
| 44 | Narain AS et al, 2018 95 | Retrospective study | 2 |
| 45 | Passias PG et al, 2018 96 | Retrospective study | 2 |
| 46 | Ranson WA et al, 2018 97 | Retrospective cohort study | 3 |
| 47 | Senker et al, 2018 49 | Prospective study | 1 |
| 48 | Tan JH et al, 2018 50 | Meta-analysis | 1 |
| 49 | Vinas-Rios JM et al, 2018 98 | Retrospective study | 2 |
| 50 | Wang T et al, 2018 99 | Meta-analysis | 1 |
| 51 | Xie Q et al, 2018 100 | Meta-analysis | 1 |
| 52 | Flippin M et al, 2017 101 | Retrospective study | 2 |
| 53 | Grover PJ et al, 2017 102 | Retrospective study | 2 |
| 54 | Joseph et al, 2017 6 | Retrospective cohort study | 3 |
| 55 | Onyekwelu et al, 2017 3 | Retrospective study | 2 |
| 56 | Phan, Rogers et al, 2017 103 | Prospective study | 1 |
| 57 | Phan, Kothari et al, 2017 20 | Retrospective study | 2 |
| 58 | Puvanesarajah et al, 2017 104 | Retrospective study | 2 |
| 59 | Wang H et al, 2017 105 | Retrospective study | 2 |
| 60 | Wilson JR et al, 2017 106 | Prospective study | 1 |
| 61 | Adogwa et al, 2016 23 | Retrospective study | 2 |
| 62 | Burgstaller JM et al, 2016 107 | Prospective study | 1 |
| 63 | Chotai et al, 2016 108 | Prospective study | 1 |
| 64 | Elsamadicy AA et al, 2016 109 | Retrospective study | 2 |
| 65 | Higgins DM et al, 2016 110 | Retrospective study | 2 |
| 66 | Huang S et al, 2016 111 | Retrospective study | 2 |
| 67 | Lucas et al, 2016 36 | Retrospective study | 2 |
| 68 | Manson NA et al, 2016 112 | Retrospective study | 2 |
| 69 | McAnany et al, 2016 7 | Retrospective study | 2 |
| 70 | Owens et al, 2016 38 | Retrospective study | 2 |
| 71 | Sielatycki et al, 2016 113 | Retrospective study | 2 |
| 72 | Sielatycki JA et al 114 | Retrospective study | 2 |
| 73 | Sing et al, 2016 115 | Retrospective cohort study | 3 |
| 74 | Sorimachi Y et al, 2016 116 | Prospective study | 1 |
| 75 | Stienen et al, 2016 117 | Prospective study | 1 |
| 76 | Wang H et al, 2016 118 | Retrospective study | 2 |
| 77 | Wang YP et al, 2016 119 | Retrospective study | 2 |
| 78 | Adogwa et al, 2015 120 | Retrospective study | 2 |
| 79 | Burks et al, 2015 121 | Retrospective study | 2 |
| 80 | Cao J et al, 2015 122 | Meta-analysis | 1 |
| 81 | De la Garza Ramos et al, 2015 32 | Retrospective study | 2 |
| 82 | Giannadakis C et al, 2015 123 | Prospective study | 1 |
| 83 | Goldin AN et al, 2015 124 | Retrospective study | 2 |
| 84 | Kukreja et al, 2015 51 | Retrospective study | 2 |
| 85 | Lingutla et al, 2015 30 | Meta-analysis | 1 |
| 86 | Nota SP et al, 2015 125 | Retrospective study | 2 |
| 87 | Ou et al, 2015 10 | Retrospective study | 2 |
| 88 | Planchard RF et al, 2015 126 | Retrospective study | 2 |
| 89 | Yagi et al, 2015 127 | Retrospective study | 2 |
| 90 | Auffinger B et al, 2014 128 | Retrospective study | 2 |
| 91 | Buerba et al, 2014 129 | Retrospective cohort study | 3 |
| 92 | Buerba RA et al, 2014 130 | Retrospective cohort study | 3 |
| 93 | Fu et al, 2014 34 | Retrospective cohort study | 3 |
| 94 | Jiang J et al, 2014 29 | Meta-analysis | 1 |
| 95 | Marquez-Lara A et al, 2014 131 | Retrospective study | 2 |
| 96 | Mcclendon et al, 2014 16 | Retrospective study | 2 |
| 97 | McGuire KJ et al, 2014 132 | Prospective study | 1 |
| 98 | Pereira BJ et al, 2014 133 | Retrospective study | 2 |
| 99 | Quah C et al, 2014 134 | Retrospective study | 2 |
| 100 | Seicean A et al, 2014 135 | Retrospective cohort study | 3 |
| 101 | Srinivasan et al, 2014 136 | Retrospective study | 2 |
| 102 | Terman et al, 2014 28 | Retrospective cohort study | 3 |
| 103 | Wang J et al, 2014 137 | Prospective study | 1 |
| 104 | Lau, Khan et al, 2013 27 | Retrospective study | 2 |
| 105 | Lau, Ziewacz et al, 2013 52 | Retrospective study | 2 |
| 106 | Rihn JA et al, 2013 138 | Retrospective study | 2 |
| 107 | Rosenfeld HE et al, 2013 139 | Case series | 4 |
| 108 | Gaudelli C et al, 2012 140 | Retrospective cohort study | 3 |
| 109 | Kalanithi et al, 2012 17 | Retrospective study | 2 |
| 110 | Mehta AI et al, 2012 141 | Retrospective study | 2 |
| 111 | Mogannam et al, 2012 37 | Retrospective study | 2 |
| 112 | Rihn JA et al, 2012 142 | Retrospective study | 2 |
| 113 | Senker et al, 2011 48 | Retrospective study | 2 |
| 114 | Anderson PA et al, 2010 71 | Meta-analysis | 1 |
| 115 | Rodgers et al, 2010 143 | Retrospective study | 2 |
| 116 | Singh et al, 2010 144 | Retrospective study | 2 |
| 117 | Yadla et al, 2010 145 | Prospective study | 1 |
| 118 | Walid MS et al, 2010 146 | Retrospective study | 3 |
| 119 | Peng et al, 2009 39 | Prospective study | 1 |
| 120 | Shamji MF et al, 2009 147 | Retrospective study | 2 |
| 121 | Vaidya R et al, 2009 148 | Retrospective study | 2 |
| 122 | Djurasovic et al, 2008 53 | Retrospective cohort study | 3 |
| 123 | Park et al, 2016 149 | Retrospective study | 2 |
| 124 | Rosen et al, 2008 150 | Retrospective study | 2 |
| 125 | Patel et al, 2007 19 | Retrospective study | 2 |
| 126 | Sonne-Holm S et al, 2007 151 | Retrospective study | 2 |
| 127 | Gepstein R et al, 2004 26 | Retrospective study | 2 |
| 128 | Epstein, 2003 54 | Case series | 4 |
| 129 | Telfeian AE et al, 2002 152 | Retrospective study | 2 |
| 130 | Andreshak TG et al, 1997 153 | Prospective study | 1 |
Results
Two authors (GDP, FC) independently evaluated the English literature and a total number of 1636 articles were found, but only 130 of them were considered to be relevant after thorough evaluation and according to PRISMA checklist (Figure 1).
Figure 1.
PRISMA flow chart.
Specifically, 729 papers were duplicated, while 732 articles were found to have irrelevant title. Moreover, 45 articles were excluded after reading since they did not meet the inclusion criteria: 13 of them were constituted by narrative review or case report, 26 dealt with adolescent idiopathic scoliosis while 6 papers evaluated the effect of obesity on mineral bone metabolism (Figure 1). The majority of the included papers were classified according to the Sacket Grading System 56 as Level 2 (Retrospective Studies).
Discussion
Obesity-Metabolic Considerations
Albeit not influencing long-term surgical outcomes, obesity is generally considered to exert an adverse effect on major surgeries.104,154 In particular, obesity could prolong operative time and may represent a risk factor for short-term complications. The strict correlation between obesity—especially the visceral one—and insulin resistance could increase the risks for complications.155-157 Specifically, increase in the secretion of some adipokines such as resistin, TNF- and IL-6, was found to have a negative effect on insulin sensitivity.155,157-159 Moreover, the arterial hypertension and atherogenic dyslipidemia—often associated with obesity—contribute to create a prothrombotic and pro-inflammatory general state. 158 Furthermore, a close relationship between the content of skeletal muscle and systemic insulin resistance was demonstrated, since the metabolic lipo-toxicity of diacylglycerol and ceramides, able to create a direct pro-oxidative and inflammatory activity. Lastly, recent evidence shows that ectopic lipids deposition can also compromise the turnover of muscle proteins promoting systemic and muscular oxidative stress.157,160,161 Blood glucose concentrations could also play substantial roles with its opposing effects on immunological/cellular mechanisms. The augmented risk for infections of diabetic patients is well known, together with the consequences of acute, short term hyperglycemia on innate immunity and the ability of the host to combat infections. Although there is still no global consensus and sufficient evidence to support a rigid glycemic control in the peri-operative management beyond common routinely measures, 162 the implications of acute hyperglycemia on neutrophil activity, cytokine patterns and microvascular reactivity are well described. 163
Obesity and Cervical Spine Surgery
Most studies analyzing the association between obesity and outcomes in spine surgery have focused on thoracic and lumbar diseases, while few reports evaluated outcomes and complications following cervical surgery (Table 2).18,95,106,113,122,164
Table 2.
Literature Regarding Cervical Surgery in Obese Patients Grouped Into Anterior and Posterior Cervical Surgery.
| Anterior cervical surgery | ||
|---|---|---|
| Study number | Reference | Type of study |
| 13 | Malik AT et al, 2020 68 | Retrospective cohort study |
| 15 | Qi M et al, 2020 69 | Retrospective study |
| 20 | Basques et al, 2019 74 | Retrospective cohort study |
| 26 | Kashkoush A et al, 2019 79 | Retrospective study |
| 29 | Malik AT et al, 2019 81 | Retrospective study |
| 33 | Zhang G.A. et al, 2019 18 | Meta-analysis |
| 44 | Narain AS et al, 2018 95 | Retrospective study |
| 60 | Wilson JR et al, 2017 106 | Prospective study |
| 63 | Chotai et al, 2016 108 | Prospective study |
| 91 | Auffinger B et al, 2014 128 | Retrospective study |
| 93 | Buerba RA et al, 2014 130 | Retrospective cohort study |
| 94 | Fu et al, 2014 34 | Retrospective cohort study |
| 102 | Srinivasan et al, 2014 136 | Retrospective study |
| Posterior cervical surgery | ||
| Study number | Reference | Type of study |
| 6 | Fatima N et al, 2020 61 | Retrospective study |
| 18 | Sridharan M et al, 2020 72 | Retrospective study |
| 22 | Cheng CW et al, 2019 76 | Retrospective cohort study |
| 57 | Phan, Kothari et al, 2017 20 | Retrospective study |
| 93 | Buerba RA et al, 2014 130 | Retrospective cohort study |
In a multi-centric Japanese study, Wilson et al conducted a quantitative analysis of 1-year clinical outcomes (Neck Disability Index (NDI), modified Japanese Orthopedic Association (mJOA) score, and Short Form-36 (SF-36) scores) in a cohort of 757 patients. NDI scores resulted to be 5.7 points higher for obese patients compared with individuals of normal weight and, albeit strong trends toward reduced SF-36 mental component scores and physical component scores resulted among obese patients, no associations were found between BMI and 1-year mJOA. 106
In 2016, comparing 80 obese with 219 non obese patients, Sielatycki et al observed that despite obesity was associated with worst clinical myelopathy (mJOA score: 10.7 vs 12.2) and higher general physical and mental health impairment (SF-12 mental physical component scale: 28.7 vs 31.8; SF-12 mental component scale score: 38.9 vs 42.3) at the baseline evaluation, all patient-referred outcomes resulted to be significantly improved at 12-months after surgery, and, additionally, the multivariate analysis showed that the pre-operative BMI did not turned out to be a predictor of less improvement in postoperative disability (NDI), neck pain (NRS), general mental and physical health (SF-12 MCS and PCS), and mJOA scale scores. 113
Narain et al retrospectively reviewed 277 obese patients who underwent primary 1-to 2-level anterior cervical discectomy and fusion (ACDF) for degenerative spinal pathology, evaluating clinical outcomes, complications, narcotics consumption and hospital costs after patients’ stratification in the different obesity classes. The authors did not report out significant differences in terms of outcomes (fusion rate and clinical improvement) and also operative time, intraoperative blood loss, length of hospital stay, postoperative narcotics consumption, complication rates, reoperation rates and total direct costs across BMI stratifications. 95 Same results about outcomes were outlined by Auffinger et al in a prospective study. 128
Although many studies did not find global differences in terms of clinical outcomes both in the immediate post-operative period and at long-term follow up comparing obese and non-obese patients 81 —suggesting that cervical spine fusion procedures resulted to be effective for all patients across the entire BMI spectrum—very few studies have critically investigated the rate of complications.74,108
Recently, Zhang et al handled with this aspect, reporting interesting results in a meta-analysis including 7 studies resulting in a total number of 90 740 patients. The results showed that higher BMIs were significatively associated with longer hospital stay (weight mean difference (WMD): 1.61 days), longer surgical time (WMD: 4.55), higher mortality rate (risk ratio (RR) = 3.01) and higher postoperative rates of cardiac complications (RR = 1.30), deep venous thromboembolism (RR = 2.29) and wound complications (RR = 1.69). Conversely, no significant differences were reported between high and normal BMI groups in terms of NDI, SF-36 MC and PC score, overall complications, pulmonary and septic complications. 18
Hence, albeit several limitations could be remarked in this study, such as the fact that no randomized control trials have been conducted and the lack of subgroups analysis, due to the poor data availability, high BMI appeared to be associated with longer surgical time, hospital stay and higher post-operative complication rates.18,95 Buerba et al did not find significative associations analyzing the impact of obesity on 30-day complications following cervical fusions in 2072 patients, while a significative longer operative time was reported among Class III comparing to non-obese patients (138.75 vs 132.21 for anterior cervical spine fusion; 200.24 vs 177.35 for posterior cervical spine fusion). Nonetheless, their study lacked of long-term outcomes assessment. 130 Fatima et al reported more complications in obese vs nonobese patients after posterior cervical fusion in terms of infections and hardware failure. 61 Same results in terms of higher rates of post-surgical complications were reported by other studies. Evidences are stronger for posterior approaches72,76 while for anterior surgery results are controversial.69,79,136
According to the available evidence, then, the topic is still debatable. Surgery seems to be equally of help in obese patients with valuable outcomes if compared to nonobese patients, while a not negligible amount of studies—especially about posterior surgery—describes an higher rate of complications. Therefore, patients with high BMI should be advised concerning the risk of postoperative complications related to cervical spine surgery and, besides, whereby allowed by neurological impairment, a weight loss program with the aim to reduce the pre-operative BMI could be considered.
Obesity and Lumbar Spine Surgery
In the 1987, Hanigan et al reported 1 of the first experience of lumbar surgery for obese patients. The authors conducted a prospective study, enrolling 110 patients suffering from intractable sciatica, with a total number of 17 obese patients and 6-month follow up, and They concluded that obesity did not result to be a prognostic factor when patients were considered eligible for surgery according to their protocol (clinical condition and similar conservative management). 165
Subsequently, reports from Spine Patient Outcomes Research Trial (SPORT)—one of the largest studies of operative and non-operative are of patients with lumbar degenerative diseases—started to define outcomes and complications after spine surgery in obese patients. One of the analysis derived from the SPORT Trial, analyzing the effects of surgical and non-surgical treatment in 2 subgroups—nonobese vs obese patients—reported significant treatment effects in the surgical arm, both for obese and nonobese patients. However, while obesity did not result to affect surgical outcomes in lumbar stenosis, it was found to be associated with higher risks for infection, re-operation rate and lower improvement in SF-36 physical score, when surgery was performed for degenerative spondylolisthesis 142 ; less improvement in Oswestry Disability Index (ODI) scale and SF-36 physical score was similarly reported for inter-vertebral disc herniation from the Trial. 138
Additionally, McGuire et al reported a sub-group analysis from the SPORT trial highlighting higher rate of wound infections and longer operative time for class II and III obese patients (highly obese) compared to class I obese patients. Moreover, although highly obese patients reported worst outcomes compared with class I obeses, especially when surgery was performed for disc herniation, surgical treatment resulted able to provide better outcomes when compared with non-surgical treatment. 132
In a recent meta-analysis, Jiang et al reported significative increased risk for surgical site infections (OR 2.33), venous thromboembolism (OR 3.15), mortality (OR 2.6), revision rate (OR 1.43), longer operative times (OR 14.55) and higher blood loss (weighted mean difference (WD) 28.89) for obese patients. 29 Nonetheless, the lack of stratification on the basis of the type of surgery performed (fusion/non-fusion; open/MIS) and the involved level, could represent a limit of these aforementioned studies.
Thus, despite several studies described good outcomes following spine fusion in obese patients,5,57 the majority of spine surgeons seems to show a tendency toward favor for non-fusion procedures—a priori considered “less invasive”—since the historically reported higher rate of complications.3,98,103,104,121,134 Recently, Onyekwelu et al conducted an interesting retrospective study aiming to establish differences in clinical outcomes and complication rates between obese and nonobese patients (1181 vs 1266) following decompression alone compared with decompression plus fusion for lumbar spinal stenosis. Specifically, considering 12-month ODI or leg pain improvement evaluation, no differences were found in the decompression plus spine fusion group between obese and non-obese patients. Then, improvement in back pain resulted to be less consistent among the obese group when spine fusion was not performed. Conversely, blood loss and operative times resulted higher in obese patients, despite fusion or non-fusion procedures, if compared to non-obese patients and, also, obese patients who underwent spine fusion needed a longer hospital stay than non-obese patients (4.1 vs 3.3 days). 3 Kalanithi et al conducted a retrospective cross-sectional study of all spinal fusions performed in California from 2003 to 2007 analyzing whether morbid obesity alters rates of complications and charges in patients undergoing spinal fusion, resulting in 1455 were morbidly obese. Higher morbidity rate among the morbidly obese was reported as were average hospital costs ($108 604 vs. $84 861, P < .0001). Morbid obesity was the most significant predictor of complications in posterior lumbar fusion. However, no subgroup analysis was reported in order to evaluated the role of MIS techniques among the posterior lumbar fusion group and this could actually represent a bias. 17
Hence, major trends support valuable clinical outcomes in obese patients, both at short and long-term follow up, surgically treated for LDD 59 and better results were observed with spine fusion. While outcomes are reported to be satisfactory and often comparable among obese and nonobese patients treated with surgery when needed, peri-operative complications rate seems to be higher in most of the analyzed papers with few exceptions (Table 3).60,62,63,65,66,70,73,77,78,80,82,86,88,90,92-94,97,101,102,105,107,109-112,114,116,118,123,125,126,129,131,133,135,139-141,146-148,151-153,166-172
Table 3.
Literature Regarding Lumbar Spine Surgery in Obese Patients.
| Lumbar spine surgery | |||||
|---|---|---|---|---|---|
| Study number | Reference | Type of study | Study number | Reference | Type of study |
| 1 | Mulvaney G et al, 2021 57 | Retrospective study | 72 | Sielatycki et al, 2016 113 | Retrospective study |
| 2 | Paranjape CS et al, 2021 58 | Retrospective study | 73 | Sielatycki JA et al, 114 | Retrospective study |
| 3 | Chan AK et al, 2020 5 | Retrospective study | 75 | Sorimachi Y et al, 2016 116 | Prospective study |
| 4 | Divi SN et al, 2020 59 | Retrospective study | 76 | Stienen et al, 2016 117 | Prospective study |
| 5 | Duan PG et al, 2020 60 | Retrospective study | 77 | Wang H et al, 2016 118 | Retrospective study |
| 7 | He X et al, 2020 62 | Retrospective cohort study | 78 | Wang YP et al, 2016 119 | Retrospective study |
| 8 | Jain D et al, 2020 63 | Retrospective study | 79 | Adogwa et al, 2015 120 | Retrospective study |
| 10 | Khan JM et al, 2020 65 | Retrospective cohort study | 80 | Burks et al, 2015 121 | Retrospective study |
| 16 | Safaee MM et al, 2020 70 | Retrospective study | 81 | Cao J et al, 2015 122 | Meta-analysis |
| 17 | Siccoli A et al, 2020 71 | Retrospective study | 82 | De la Garza Ramos et al, 2015 32 | Retrospective study |
| 19 | Xi Z et al, 2020 73 | Retrospective study | 83 | Giannadakis C et al, 2015 123 | Prospective study |
| 24 | Goyal A et al, 2019 78 | Meta-analysis | 86 | Lingutla et al, 2015 30 | Meta-analysis |
| 25 | Elsamadicy et al, 2019 40 | Retrospective study | 87 | Nota SP et al, 2015 125 | Retrospective study |
| 28 | Linhares D et al, 2019 80 | Prospective study | 88 | Ou et al, 2015 10 | Retrospective study |
| 30 | Mombell KW et al, 2019 82 | Retrospective study | 89 | Planchard RF et al, 2015 126 | Retrospective study |
| 31 | Villavicencio et al, 2019 83 | Retrospective study | 90 | Yagi et al, 2015 127 | Retrospective study |
| 34 | Zhang Y. et al, 2019 85 | Retrospective study | 92 | Buerba et al, 2014 129 | Retrospective cohort study |
| 36 | Akins et al, 2018 87 | Retrospective cohort study | 96 | Marquez-Lara A et al, 2014 131 | Retrospective study |
| 37 | Bono OJ et al, 2018 88 | Retrospective study | 98 | McGuire KJ et al, 2014 132 | Prospective study |
| 39 | Chung AS et al, 2018 90 | Retrospective cohort study | 99 | Pereira BJ et al, 2014 133 | Retrospective study |
| 40 | Jain et al, 2018 91 | Retrospective cohort study | 100 | Quah C et al, 2014 134 | Retrospective study |
| 41 | Lovecchio F et al, 2018 92 | Retrospective cohort study | 107 | Rihn JA et al, 2013 138 | Retrospective study |
| 42 | Madsbu MA et al, 2018 93 | Retrospective study | 108 | Rosenfeld HE et al, 2013 139 | Case series |
| 43 | Nahhas CR et al, 2018 94 | Retrospective study | 109 | Gaudelli C et al, 2012 140 | Retrospective cohort study |
| 46 | Ranson WA et al, 2018 97 | Retrospective cohort study | 110 | Kalanithi et al, 2012 17 | Retrospective study |
| 47 | Senker et al, 2018 49 | Prospective study | 111 | Mehta AI et al, 2012 141 | Retrospective study |
| 49 | Vinas-Rios JM et al, 2018 98 | Retrospective study | 112 | Mogannam et al, 2012 37 | Retrospective study |
| 52 | Flippin M et al, 2017 101 | Retrospective study | 113 | Rihn JA et al, 2012 142 | Retrospective study |
| 53 | Grover PJ et al, 2017 102 | Retrospective study | 114 | Senker et al, 2011 48 | Retrospective study |
| 54 | Joseph et al, 2017 6 | Retrospective cohort study | 115 | Anderson PA et al, 2010 71 | Meta-analysis |
| 55 | Onyekwelu et al, 2017 3 | Retrospective study | 117 | Singh et al, 2010 144 | Retrospective study |
| 56 | Phan, Rogers et al, 2017 103 | Prospective study | 118 | Yadla et al, 2010 145 | Prospective study |
| 58 | Puvanesarajah et al, 2017 104 | Retrospective study | 120 | Peng et al, 2009 39 | Prospective study |
| 59 | Wang H et al, 2017 105 | Retrospective study | 121 | Shamji MF et al, 2009 147 | Retrospective study |
| 62 | Burgstaller JM et al, 2016 107 | Prospective study | 122 | Vaidya R et al, 2009 148 | Retrospective study |
| 66 | Huang S et al, 2016 111 | Retrospective study | 123 | Djurasovic et al, 2008 53 | Retrospective cohort study |
| 67 | Lucas et al, 2016 36 | Retrospective study | 126 | Sonne-Holm S et al, 2007 151 | Retrospective study |
| 68 | Manson NA et al, 2016 112 | Retrospective study | 127 | Gepstein R et al, 2004 26 | Retrospective study |
| 71 | Owens et al, 2016 38 | Retrospective study | 128 | Epstein, 2003 54 | Case series |
| 1 | Mulvaney G et al, 2021 57 | Retrospective study | 129 | Telfeian AE et al, 2002 152 | Retrospective study |
The role of MIS techniques for lumbar spine surgery
In summary, the introduction of MIS techniques represents a great stride in the operative care of obese patients. By reducing surgical related complications and, specifically, the overall higher complications rate that burden on these patients, MIS techniques could represent a feasible solution against the tendence toward favor non-fusion of the spine—even when needed—due to the fear of complications (Table 4). 124 Most of the aforementioned studies reported higher complication rates among obese patients who underwent surgery, especially for spinal fusion.120,149 Similarly, many studies highlighted the benefits, in terms of relief from pain and QoL improvement, obtained with surgery.115,117,127,144,145,150 Therefore, in recent years, several authors focused their research on the need for less invasive procedures capable to guarantee similar outcomes to those reported with the “classic” open surgery.7,27,28,43,45,49,50
Table 4.
Literature Regarding MIS Technique in Obese Patients Undergoing Spine Surgery.
| Minimally invasive spine techniques lumbar surgery | ||
|---|---|---|
| Study number | Reference | Type of study |
| 9 | Jenkins NW et al, 2020 64 | Retrospective study |
| 12 | Othman YA et al, 2020 67 | Meta-analysis |
| 21 | Buyuk AF et al, 2019 75 | Retrospective cohort study |
| 23 | Goh GS et al, 2019 77 | Retrospective study |
| 27 | Kru?ger et al, 2019 4 | Retrospective study |
| 32 | Yoo JS et al, 2019 84 | Retrospective study |
| 35 | Abbasi H et al, 2018 86 | Retrospective cohort study |
| 38 | Byval’tsev VA et al, 2018 89 | Retrospective cohort study |
| 45 | Passias PG et al, 2018 96 | Retrospective study |
| 48 | Tan JH et al, 2018 50 | Meta-analysis |
| 50 | Wang T et al, 2018 99 | Meta-analysis |
| 51 | Xie Q et al, 2018 100 | Meta-analysis |
| 61 | Adogwa et al, 2016 23 | Retrospective study |
| 69 | McAnany et al, 2016 7 | Retrospective study |
| 84 | Goldin AN et al, 2015 124 | Retrospective study |
| 85 | Kukreja et al, 2015 51 | Retrospective study |
| 103 | Terman et al, 2014 28 | Retrospective cohort study |
| 104 | Wang J et al, 2014 137 | Prospective study |
| 105 | Lau, Khan et al, 2013 27 | Retrospective study |
| 106 | Lau, Ziewacz et al, 2013 52 | Retrospective study |
| 116 | Rodgers et al, 2010 143 | Retrospective study |
| 125 | Patel et al, 2007 19 | Retrospective study |
MIS Trans-Foraminal Interbody Fusion (TLIF) have been described for the first time by Foley et al in 2003 and showed encouraging results, namely reduced operative times, length of stay, blood loss and wound problems, due to the minimal muscles retraction and to the smaller incision, when compared with open techniques.64,173 Interesting studies analyzing the peak muscles pressure due to the retractors and/or evaluating post-operative muscles edema with MRI or post-operative values of muscles disruption enzymes, indeed, showed significative less retraction and less muscles damage with MIS techniques when compared with open techniques.49,174,175
Lau et al reported in 2013 a retrospective analysis that compared MIS-TLIF with open TLIF in 127 obese patients—stratified for obesity classes—reporting significative less blood loss and shorter hospital stay and, above all, reduced total and intra-operative complication rate (respectively 11.5% vs 28.6% and 3.8% vs 16.3%) in the MIS-TLIF cohort. Besides, when stratified by obesity class, this effect on total complication rate was more evident and statistically significant in patients with Class III obesity (7.1% vs 42.9%). 27
In a prospective study, Senker et al assessed the perioperative and postoperative complications of MIS techniques in a large population of 187 patients. The authors evaluated peri-operative and post-operative complication rates in obese and normal-weight patients and no infection or severe wound healing disorder were reported. Moreover, no significant differences in terms of cerebrospinal fluid leakage, blood loss or length of hospital stay and major complications (i.e. venous thrombo-embolism, strokes, cardiac infarction) was found, while more clinically insignificant hematomas and urinary infections were encountered in the obese groups than in the normal-weight patients. 49
Terman et al retrospectively compared the clinical benefit of open and MIS-TLIF in 74 obese patients with a mean follow up of 30 months, measuring post-operative improvement in visual analog scale (VAS), ODI, blood loss and length of stay. No differences were found between MIS-TLIF and open cohorts when mean VAS score improvement (2.4 vs 2.8) and mean ODI improvement (15 vs 13) were compared, even after stratification according to obesity classes. However, complications and blood loss were significatively greater for the open group than for the MIS-TLIF group (overall complication rate: 52% vs 17%; durotomy rate: 14% vs 4%). 28
McAnany et al reported interesting results analyzing the interaction between obesity status and the change in SF-12 results, concluding that patients undergoing MIS TLIF sustain meaningful and significant gains in SF-12 (mental and physical components) that is not affected by obesity (no interactions between SF-12 changes and obesity status (p .33). 7 Reasons to promote the use of MIS TLIF vs open-TLIF are also related to other complications rate that could affect the perioperative outcomes of obese patients, as reported by 2 meta-analysis: less blood loss, shorter hospital stay and less risk of dural tears.50,67,75,84,89,99,100,137
Indirect decompression of the spinal canal, then without the need for artrectomy and laminectomy could be considered as a powerful weapon in obese patients because of the reduced need for muscle dissection, surgical trauma and, subsequently, blood loss.83,86
In these terms, the Lateral Transpsoas Access for Lumbar Fusion (LLIF) has gained popularity for the treatment of spinal stenosis or instability in obese patients during the last 2 decades. Spinal interbody cages for LLIF, with their large footprint, are able to span both lateral cortical rims while preserving the anterior longitudinal ligament, restoring then a proper disc height while achieving stability in addition to posterior percutaneous fixation from upper lumbar segments to the L4-L5 level. 176 In this way, this technique is able to perform indirect decompression enlarging the neuroforamen and the spinal canal, reducing the bulging/prolapse of the disk and stretching the yellow ligament. Rodgers et al (2010) retrospectively compared obese and non-obese patients who underwent LLIF procedures, focusing on early complications rate—defined as any adverse event observed within 3 months after surgery—and, unlike traditional open lumbar fusion procedures, no greater risk of complication in the obese patients was found. 143
Nevertheless, although commonly accepted as a proper strategy in obese patients, no studies have compared since now open posterior vs lateral approaches in these patients. The anterior retroperitoneal access for fusion (ALIF) represented another effective way to gain indirect decompression with a minimally invasive approach for L5-S1 level. 177 Phan et al aimed to compare complication risks, functional outcomes, and subsidence rates in a group of 137 patients who underwent ALIF, categorizing them into 3 groups according to their BMI: normal-weight, overweight, and obese. There was no difference in operative duration, blood loss, or hospital stay and no difference was found in terms of total complications. Despite fusion rates resulted to be lower for obese patients, obesity should not be considered a contraindication for anterior approaches. 103
Another mini-open technique potentially able to reduce surgical impact on the patient is represented by the use of Cortical Bone trajectory screws for posterior fusion. This approach requires less posterior exposure because of the more medial entry point of screws, then preserving from dissection a larger amount of Multifidus muscle and respecting its innervation.45,47,178 No studies, however, have been conducted to verify benefits of this technique in obese patients if compared to standard open approaches. Together with percutaneous fixation, posterior focal decompression with tubular retractors and/or the use of the endoscope could constitute other effective strategies to reduce complications in obese patients.119,179
Future Perspectives
Future researches should probably concentrate their effort to evaluate the effects of a proper weight loss before spine surgery instead of verifying the risk of complications of surgery in obese patients (Table 5). Jain et al published a retrospective evaluation of the use of bariatric surgery before elective posterior lumbar surgery. 91 Given the limits of a retrospective evaluation, they showed how bariatric surgery was able to mitigate the risk of post-operative complications, with lower rates of respiratory failure (odds ratio [OR] 0.59, P = .019), urinary tract infection (OR 0.64, P = .031), acute renal failure (OR 0.39, P = .007), overall medical complications (OR 0.59, P < .001), and infection (OR 0.65, P = .025). This effort could be justified also because, from the opposite point of view, obese patients who benefit from spine surgery seem to show a valid trend of weight loss after surgery. In a cohort analysis of 7303 patients obese and extremely obese patients were more likely to lose a clinically significant amount of weight 1 year after surgery (BMI 3039: OR1.42, 95% CI 1.22 1.65; BMI 40: OR1.73, 95% CI 1.212.47) compared with nonobese patients. 87 Recently, Malik et al reported interesting results assessing the impact of prior bariatric surgery on 90-day outcomes following ACDF. Patients were divided into 2 groups- obese ACDF patients who underwent bariatric surgery within 2 years before an ACDF and obese patients with no history of a bariatric surgery within the last 2 years. Multivariate regression analyzes revealed that undergoing BS before an elective ACDF was associated with a significantly reduced risk of pulmonary, renal and cardiac complications, sepsis and 90-day readmissions. 68 Other papers supported these results58,91,180 although some results questioned the real measured effect of a proper weight loss.71,96 These results, together with the presented literature, suggest that a multidisciplinary strategy could play a key role in obese patients. The use of a proper diet plan before elective surgery, in order to reduce the fat mass while preserving/reinforcing the lean mass, while reserving bariatric surgery for severely obese patients, could be a powerful strategy to reduce surgical related complications, to increase the chances of functional recovery from spinal diseases and to encourage further and valid post-operative weight loss.
Table 5.
Literature Regarding Future Perspective to Achieve the Best Management of Obese Patients Who Underwent Spine Surgery.
| Future perspectives | ||
|---|---|---|
| Study number | Reference | Type of study |
| 2 | Paranjape CS et al, 2021 58 | Retrospective study |
| 17 | Siccoli A et al, 2020 71 | Retrospective study |
| 29 | Malik AT et al, 2019 81 | Retrospective study |
| 40 | Jain et al, 2018 91 | Retrospective cohort study |
| 45 | Passias PG et al, 2018 96 | Retrospective study |
| 115 | Anderson PA et al, 2010 71 | Meta-analysis |
Conclusions
In cervical and lumbar spine surgery Evidence suggest that obese patients could benefit from spine surgery and outcomes be satisfactory. Given this, the majority of the analyzed studies reported higher rates of peri-operative complications among obese patients, especially in posterior approaches. The use of MIS techniques plays a key role in order to reduce surgical risks. According to preliminary evidence, further studies should evaluate and encourage the role of multidisciplinary counseling between spine surgeons, nutritionists and, in selected cases, bariatric surgeons, in order to plan proper weight loss before elective spine surgery.
Abbreviations
- WHO
World Health Organization
- BMI
Body Mass Index
- QoL
Quality of Life
- MIS
Minimally Invasive Surgery
- LBP
Low Back Pain
- LDD
Lumbar Degenerative Disease
- OR
Odds Ratio
- NDI
Neck Disability Index
- mJOA
modified Japanese Orthopedic Association
- SF-36
Short Form-36; SF-36 MC; Mental Component and SF-36 PC, Physical Component
- SF-12
Short Form-12; SF-12 MC; Mental Component and SF-12 PC, Physical Component
- ACDF
Anterior Cervical Discectomy and Fusion
- WMD
Weight Mean Difference
- SPORT
Spine Patient Outcomes Research Trial
- RR
Risk Ratio
- ODI
Oswestry Disability Index
- TLIF
Trans-Foraminal Interbody Fusion
- LLIF
Lateral Lumbar Interbody Fusion
- ALIF
Anterior Lumbar Interbody Fusion.
Footnotes
Authors’ Note: Fabio Cofano, MD and Giuseppe Di Perna, MD contributed equally to this article. FC conceptualization and writing; GD writing, reviewing and review of the literature; DB conceptualization and writing; VR writing; BB review of the literature; SP reviewing; FT reviewing; DG conceptualization and supervision; MB conceptualization and supervision
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Ministero dell’Istruzione, dell’Università e della Ricerca—MIUR project “Dipartimenti di eccellenza 2018-2022.”
ORCID iD: Fabio Cofano, MD  https://orcid.org/0000-0002-5100-7478
https://orcid.org/0000-0002-5100-7478
Giuseppe Di Perna, MD  https://orcid.org/0000-0002-7381-9194
https://orcid.org/0000-0002-7381-9194
Vittoria Roscigno, RD  https://orcid.org/0000-0002-0282-4279
https://orcid.org/0000-0002-0282-4279
Salvatore Petrone, MD  https://orcid.org/0000-0002-9921-3879
https://orcid.org/0000-0002-9921-3879
References
- 1.Haslam DW, James WPT. Obesity. Lancet. 2005. doi:10.1016/S0140-6736(05)67483 -1 [DOI] [PubMed] [Google Scholar]
- 2.MacMahon S, Baigent C, Duffy S, et al. Body-mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studies. The Lancet. 2009;373(9669):1083–1096. doi:10.1016/S0140-6736(09)60318-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onyekwelu I, Glassman SD, Asher AL, Shaffrey CI, Mummaneni PV, Carreon LY. Impact of obesity on complications and outcomes: a comparison of fusion and nonfusion lumbar spine surgery. J Neurosurg Spine. 2017;26(2):158–162. doi:10.3171/2016.7.SPINE16448 [DOI] [PubMed] [Google Scholar]
- 4.Krüger MT, Naseri Y, Hohenhaus M, Hubbe U, Scholz C, Klingler JH. Impact of morbid obesity (BMI > 40 kg/m 2) on complication rate and outcome following minimally invasive Transforaminal Lumbar Interbody Fusion (MIS TLIF). Clin Neurol Neurosurg. 2019;178(2018):82–85. doi:10.1016/j.clineuro.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 5.Chan AK, Bisson EF, Bydon M, et al. Obese patients benefit, but do not fare as well as nonobese patients, following lumbar spondylolisthesis surgery: an analysis of the quality outcomes database. Neurosurgery. 2020;86(1):80–87. doi:10.1093/neuros/nyy589 [DOI] [PubMed] [Google Scholar]
- 6.Joseph JR, Farooqui Z, Smith BW, et al. Does clinical improvement of symptomatic degenerative lumbar disease impact obesity? J Neurosurg Spine. 2017;26(6):705–708. doi:10.3171/2016.11.SPINE16973 [DOI] [PubMed] [Google Scholar]
- 7.McAnany SJ, Patterson DC, Overley S, Alicea D, Guzman J, Qureshi SA. The effect of obesity on the improvement in health state outcomes following minimally invasive transforaminal interbody fusion. Global Spine J. 2016;6(8):744–748. doi:10.1055/s-0036-1579747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L. The impact of obesity on the musculoskeletal system. Int J Obes. 2008;32(2):211–222. doi:10.1038/sj.ijo.0803715 [DOI] [PubMed] [Google Scholar]
- 9.Bjerke BT, Saiyed R, Cheung ZB, Uppstrom TJ, Shifflett GD, Cunningham ME. Does adolescent obesity affect surgical presentation and radiographic outcome for patients with adolescent idiopathic scoliosis? J Pediatr Orthopaed B. 2017;26(1):53–58. doi:10.1097/BPB.0000000000000351 [DOI] [PubMed] [Google Scholar]
- 10.Ou CY, Lee TC, Lee TH, Huang YH. Impact of body mass index on adjacent segment disease after lumbar fusion for degenerative spine disease. Neurosurgery. 2015;76(4):396–401. doi:10.1227/NEU.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 11.Fanuele JC, Abdu WA, Hanscom B, Weinstein JN. Association between obesity and functional status in patients with spine disease. Spine. 2002;27(3):306–312. doi:10.1097/00007632-200202010-00021 [DOI] [PubMed] [Google Scholar]
- 12.Dario AB, Ferreira ML, Refshauge KM, Lima TS, Ordoñana JR, Ferreira PH. The relationship between obesity, low back pain, and lumbar disc degeneration when genetics and the environment are considered: a systematic review of twin studies. Spine J. 2015;15(5):1106–1117. doi:10.1016/j.spinee.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 13.Masheb RM, Lutes LD, Kim HM, et al. Weight loss outcomes in patients with pain. Obesity. 2015;23(9):1778–1784. doi:10.1002/oby.21160 [DOI] [PubMed] [Google Scholar]
- 14.Evers Larsson U, Mattsson E. Perceived disability and observed functional limitations in obese women. Int J Obes. 2001;25(11):1705–1712. doi:10.1038/sj.ijo.0801805 [DOI] [PubMed] [Google Scholar]
- 15.Copay AG, Subach BR, Glassman SD, Polly DW, Schuler TC. Understanding the minimum clinically important difference: a review of concepts and methods. Spine J. 2007;7(5):541–546. doi:10.1016/j.spinee.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 16.McClendon J, Smith TR, Thompson SE, et al. The impact of body mass index on hospital stay and complications after spinal fusion. Neurosurgery. 2014;74(1):42–50. doi:10.1227/NEU.0000000000000195 [DOI] [PubMed] [Google Scholar]
- 17.Kalanithi PA, Arrigo R, Boakye M. Morbid obesity increases cost and complication rates in spinal arthrodesis. Spine. 2012;37(11):982–988. doi:10.1097/BRS.0b013e31823bbeef [DOI] [PubMed] [Google Scholar]
- 18.Zhang GA, Zhang WP, Chen YC, Hou Y, Qu W, Ding LX. Impact of elevated body mass index on surgical outcomes for patients undergoing cervical fusion procedures: a systematic review and meta-analysis. Orthop Surg. 2020;12(1):3–15. doi:10.1111/os.12572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6(4):291–297. doi:10.3171/spi.2007.6.4.1 [DOI] [PubMed] [Google Scholar]
- 20.Phan K, Kothari P, Lee NJ, Virk S, Kim JS, Cho SK. Impact of obesity on outcomes in adults undergoing elective posterior cervical fusion. Spine. 2017;42(4):261–266. doi:10.1097/BRS.0000000000001711 [DOI] [PubMed] [Google Scholar]
- 21.Chapman GW, Mailhes JB, Thompson HE. Morbidity in obese and nonobese patients following gynecologic surgery for cancer. J Natl Med Assoc. 1988;80(4):417–420. [PMC free article] [PubMed] [Google Scholar]
- 22.Karunakar MA, Shah SN, Jerabek S. Body mass index as a predictor of complications after operative treatment of acetabular fractures. J Bone Joint Surg Am. 2005;87(7):1498–1502. doi:10.2106/JBJS.D.02258 [DOI] [PubMed] [Google Scholar]
- 23.Adogwa O, Farber SH, Fatemi P, et al. Do obese patients have worse outcomes after direct lateral interbody fusion compared to non-obese patients? J Clin Neurosci. 2016;25:54–57. doi:10.1016/j.jocn.2015.05.056 [DOI] [PubMed] [Google Scholar]
- 24.Moulton MJ, Creswell LL, Mackey ME, Cox JL, Rosenbloom M. Obesity is not a risk factor for significant adverse outcomes after cardiac surgery. Circulation. 1996;94(9 Suppl):II87–92. [PubMed] [Google Scholar]
- 25.Dindo D, Muller MK, Weber M, Clavien PA. Obesity in general elective surgery. Lancet. 2003;361(9374):2032–2035. doi:10.1016/S0140-6736(03)13640-9 [DOI] [PubMed] [Google Scholar]
- 26.Gepstein R, Shabat S, Arinzon ZH, Berner F, Catz A, Folman F. Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clin Orthop Relat Res. 2004;(426):138–144. doi:10.1097/01.blo.0000141901.23322.98 [DOI] [PubMed] [Google Scholar]
- 27.Lau D, Khan A, Terman SW, Yee T, Marca FL, Park P. Comparison of perioperative outcomes following open versus minimally invasive transforaminal lumbar interbody fusion in obese patients. Neurosurg Focus. 2013;35(2):1–9. doi:10.3171/2013.5.FOCUS13154 [DOI] [PubMed] [Google Scholar]
- 28.Terman SW, Yee TJ, Lau D, Khan AA, la Marca F, Park P.Minimally invasive versus open transforaminal lumbar interbody fusion: comparison of clinical outcomes among obese patients. J Neurosurg Spine. 2014;20(6):644–652. doi:10.3171/2014.2.SPINE13794 [DOI] [PubMed] [Google Scholar]
- 29.Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res. 2014;472(3):968–975. doi:10.1007/s11999-013-3346-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lingutla KK, Pollock R, Benomran E, et al. Outcome of lumbar spinal fusion surgery in obese patients: a systematic review and meta-analysis. Bone Joint J. 2015;97-B(10):1395–1404. doi:10.1302/0301-620X.97B10.35724 [DOI] [PubMed] [Google Scholar]
- 31.Soroceanu A, Burton DC, Diebo BG, et al. Impact of obesity on complications, infection, and patient-reported outcomes in adult spinal deformity surgery. J Neurosurg Spine. 2015;23(5):656–664. doi:10.3171/2015.3.SPINE14743 [DOI] [PubMed] [Google Scholar]
- 32.de La Garza-Ramos R, Bydon M, Abt NB, et al. The impact of obesity on short- and long-term outcomes after lumbar fusion. Spine. 2015;40(1):56–61. doi:10.1097/BRS.0000000000000655 [DOI] [PubMed] [Google Scholar]
- 33.Ding JZ, Kong C, Sun XY, Lu SB. Perioperative complications and risk factors in degenerative lumbar scoliosis surgery for patients older than 70 years of age. Clin Interv Aging. 2019;14:2195–2203. doi:10.2147/CIA.S218204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fu L, Chang MS, Crandall DG, Revella J. Does obesity affect surgical outcomes in degenerative scoliosis? Spine. 2014;39(24):2049–2055. doi:10.1097/BRS.0000000000000600 [DOI] [PubMed] [Google Scholar]
- 35.Fu L, Chang MS, Crandall DG, Revella J. Associations between body mass and revision surgical outcomes in adult scoliosis. Clin Spine Surg. 2016;29(8):352–357. doi:10.1097/BSD.0000000000000148 [DOI] [PubMed] [Google Scholar]
- 36.Lucas F, Emery E, Dudoit T, Berger L. Influence of obesity on access-related complications during anterior lumbar spine interbody fusion. World Neurosurg. 2016;92:229–233. doi:10.1016/j.wneu.2015.12.104 [DOI] [PubMed] [Google Scholar]
- 37.Mogannam A, Bianchi C, Chiriano J, et al. Effects of prior abdominal surgery, obesity, and lumbar spine level on anterior retroperitoneal exposure of the lumbar spine. Arch Surg. 2012;147(12):1130–1134. doi:10.1001/archsurg.2012.1148 [DOI] [PubMed] [Google Scholar]
- 38.Owens RK, Djurasovic M, Onyekwelu I, Bratcher KR, McGraw KE, Carreon LY. Outcomes and revision rates in normal, overweight, and obese patients 5 years after lumbar fusion. Spine J. 2016;16(10):1178–1183. doi:10.1016/j.spinee.2016.06.005 [DOI] [PubMed] [Google Scholar]
- 39.Peng CWB, Bendo JA, Goldstein JA, Nalbandian MM. Perioperative outcomes of anterior lumbar surgery in obese versus non-obese patients. Spine J. 2009;9(9):715–720. doi:10.1016/j.spinee.2009.04.023 [DOI] [PubMed] [Google Scholar]
- 40.Elsamadicy AA, Camara-Quintana J, Kundishora AJ, et al. Reduced impact of obesity on short-term surgical outcomes, patient-reported pain scores, and 30-day readmission rates after complex spinal fusion (≥7 levels) for adult deformity correction. World Neurosurg. 2019;127:e108–e113. doi:10.1016/j.wneu.2019.02.165 [DOI] [PubMed] [Google Scholar]
- 41.Puvanesarajah V, Nourbakhsh A, Hassanzadeh H, Shimer AL, Shen FH, Singla A. Readmission rates, reasons, and risk factors in elderly patients treated with lumbar fusion for degenerative pathology. Spine (Phila Pa 1976). 2016;41(24):1933–1938. doi:10.1097/BRS.0000000000001631. PMID: 27275579. [DOI] [PubMed] [Google Scholar]
- 42.Passias PG, Brown AE, Lebovic J, et al. Metabolic syndrome has a negative impact on cost utility following spine surgery. World Neurosurg. 2020;135:e500–e504. doi:10.1016/j.wneu.2019.12.053 [DOI] [PubMed] [Google Scholar]
- 43.Rodríguez-Vela J, Lobo-Escolar A, Joven E, Muñoz-Marín J, Herrera A, Velilla J. Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Eur Spine J. 2013;22(12):2857–2863. doi:10.1007/s00586-013-2853-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up: clinical article. J Neurosurg Spine. 2008;9(6):560–565. doi:10.3171/SPI.2008.9.08142 [DOI] [PubMed] [Google Scholar]
- 45.Marengo N, Ajello M, Cofano F, et al. A tailored approach to cortical bone track for spine fixation surgery: 3-dimensional printed custom made guides for screws placement: 2-dimensional operative video. Oper Neurosurg. 2020. doi:10.1093/ons/opaa219 [DOI] [PubMed] [Google Scholar]
- 46.Marengo N, Matsukawa K, Monticelli M, et al. Cortical bone trajectory screw placement accuracy with a patient-matched 3-dimensional printed guide in lumbar spinal surgery: a clinical study. World Neurosurg. 2019;130:e98–e104. doi:10.1016/j.wneu.2019.05.241 [DOI] [PubMed] [Google Scholar]
- 47.Penner F, Marengo N, Ajello M, et al. Preoperative 3D CT planning for cortical bone trajectory screws: a retrospective radiological cohort study. World Neurosurg. 2019;126:e1468–e1474. doi:10.1016/j.wneu.2019.03.121 [DOI] [PubMed] [Google Scholar]
- 48.Senker W, Meznik C, Avian A, Berghold A. Perioperative morbidity and complications in minimal access surgery techniques in obese patients with degenerative lumbar disease. Eur Spine J. 2011;20(7):1182–1187. doi:10.1007/s00586-011-1689-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Senker W, Stefanits H, Gmeiner M, Trutschnig W, Weinfurter I, Gruber A. Does obesity affect perioperative and postoperative morbidity and complication rates after minimal access spinal technologies in surgery for lumbar degenerative disc disease. World Neurosurg. 2018;111(2018):e374–e385. doi:10.1016/j.wneu.2017.12.075 [DOI] [PubMed] [Google Scholar]
- 50.Tan JH, Liu G, Ng R, Kumar N, Wong HK, Liu G. Is MIS-TLIF superior to open TLIF in obese patients?: a systematic review and meta-analysis. Eur Spine J. 2018;27(8):1877–1886. doi:10.1007/s00586-018-5630-0 [DOI] [PubMed] [Google Scholar]
- 51.Kukreja S, Haydel J, Nanda A, Sin AH. Impact of body habitus on fluoroscopic radiation emission during minimally invasive spine surgery. J Neurosurg Spine. 2014;22(2):211–218. doi:10.3171/2014.10.spine14163 [DOI] [PubMed] [Google Scholar]
- 52.Lau D, Ziewacz J, Park P. Minimally invasive transforaminal lumbar interbody fusion for spondylolisthesis in patients with significant obesity. J Clin Neurosci. 2013;20(1):80–83. doi:10.1016/j.jocn.2012.07.004 [DOI] [PubMed] [Google Scholar]
- 53.Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine. 2008;33(16):1789–1792. doi:10.1097/BRS.0b013e31817b8f6f [DOI] [PubMed] [Google Scholar]
- 54.Epstein NE. Posterior cervical fusion failure in three morbidly obese patients following circumferential surgery. Surg Neurol. 2003;60(3):205–210. doi:10.1016/S0090-3019(03)00295-7 [DOI] [PubMed] [Google Scholar]
- 55.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi:10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Jt Surg A. 2003;85(1):1–3. doi:10.2106/00004623-200301000-00001 [PubMed] [Google Scholar]
- 57.Mulvaney G, Rice OM, Rossi V, et al. Mild and severe obesity reduce the effectiveness of lumbar fusions: 1-year patient-reported outcomes in 8171 patients. Neurosurgery. 2021;88(2):285–294. doi:10.1093/neuros/nyaa414 [DOI] [PubMed] [Google Scholar]
- 58.Paranjape CS, Gentry RD, Regan CM. Cost-effectiveness of bariatric surgery prior to posterior lumbar decompression and fusion in an obese population with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2021. doi:10.1097/BRS.0000000000003940 [DOI] [PubMed] [Google Scholar]
- 59.Divi SN, Goyal DKC, Galetta MS, et al. How does body mass index influence outcomes in patients after lumbar fusion? Spine (Phila Pa 1976). 2020;45(8):555–561. doi:10.1097/BRS.0000000000003313. PMID: 31770335. [DOI] [PubMed] [Google Scholar]
- 60.Duan PG, Mummaneni PV, Wang M, et al. Obesity may be associated with adjacent-segment degeneration after single-level transforaminal lumbar interbody fusion in spinopelvic-mismatched patients with a minimum 2-year follow-up. J Neurosurg Spine. 2020:1–6. doi:10.3171/2020.6.SPINE20159. PMID: 33035999. [DOI] [PubMed] [Google Scholar]
- 61.Fatima N, Massaad E, Alvarez-Breckenridge C, et al. Does obesity correlate with postoperative complications after elective posterior cervical spine fusion? World Neurosurg. 2020;141:e231–e238. doi:10.1016/j.wneu.2020.05.083 [DOI] [PubMed] [Google Scholar]
- 62.He X, Fei Q, Sun T. Metabolic syndrome increases risk for perioperative outcomes following posterior lumbar interbody fusion. Medicine (Baltimore). 2020;99(38):e21786. doi:10.1097/MD.0000000000021786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jain D, Durand W, Shaw JD, Burch S, Deviren V, Berven S. The Impact of obesity on risk factors for adverse outcomes in patients undergoing elective posterior lumbar spine fusion. Spine (Phila Pa 1976). 2021;46(7):457–463. doi:10.1097/BRS.0000000000003812 [DOI] [PubMed] [Google Scholar]
- 64.Jenkins NW, Parrish JM, Hrynewycz NM, Brundage TS, Singh K. Complications following minimally invasive transforaminal lumbar interbody fusion: incidence, independent risk factors, and clinical impact. Clin Spine Surg. 2020;33(5):E236–E240. doi:10.1097/BSD.0000000000000933 [DOI] [PubMed] [Google Scholar]
- 65.Khan JM, Basques BA, Kunze KN, et al. Does obesity impact lumbar sagittal alignment and clinical outcomes after a posterior lumbar spine fusion? Eur Spine J. 2020;29(2):340–348. doi:10.1007/s00586-019-06094-y. PMID: 31420726. [DOI] [PubMed] [Google Scholar]
- 66.Katsevman GA, Daffner SD, Brandmeir NJ, Emery SE, France JC, Sedney CL. Complications of spine surgery in “super obese” patients. Global Spine J. 2020. doi:10.1177/2192568220953393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Othman YA, Alhammoud A, Aldahamsheh O, Vaishnav AS, Gang CH, Qureshi SA. Minimally invasive spine lumbar surgery in obese patients: a systematic review and meta-analysis. HSS J. 2020;16(2):168–176. doi:10.1007/s11420-019-09735-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Malik AT, Noria S, Xu W, Retchin S, Yu ES, Khan SN. Bariatric surgery before elective Anterior Cervical Discectomy and Fusion (ACDF) in obese patients is associated with reduced risk of 90-day postoperative complications and readmissions. Clin Spine Surg. 2020. doi:10.1097/BSD.0000000000001120 [DOI] [PubMed] [Google Scholar]
- 69.Qi M, Xu C, Cao P, et al. Does obesity affect outcomes of multilevel ACDF as a treatment for multilevel cervical spondylosis?: a retrospective study. Clin Spine Surg. 2020;33(10):E460–E465. doi:10.1097/BSD.0000000000000964. PMID: 32149743. [DOI] [PubMed] [Google Scholar]
- 70.Safaee MM, Tenorio A, Osorio JA, et al. The impact of obesity on perioperative complications in patients undergoing anterior lumbar interbody fusion. J Neurosurg Spine. 2020:1–10. doi:10.3171/2020.2.SPINE191418 [DOI] [PubMed] [Google Scholar]
- 71.Anderson PA, Dettori JR, Hermsmeyer JT. Does lumbar decompression in overweight patients assist in postoperative weight loss? Evid Based Spine Care J. 2010;1(2):34–38. doi:10.1055/s-0028-1100912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sridharan M, Malik AT, Kim J, Khan SN, Yu E. Does increasing body mass index correlate with adverse outcomes following posterior cervical fusions? World Neurosurg. 2020;133:e789–e795. doi:10.1016/j.wneu.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 73.Xi Z, Burch S, Mummaneni PV, Mayer RR, Eichler C, Chou D. The effect of obesity on perioperative morbidity in oblique lumbar interbody fusion. J Neurosurg Spine. 2020:1–8. doi:10.3171/2020.1.SPINE191131 [DOI] [PubMed] [Google Scholar]
- 74.Basques BA, Khan JM, Louie PK, et al. Obesity does not impact clinical outcome but affects cervical sagittal alignment and adjacent segment degeneration in short term follow-up after an anterior cervical decompression and fusion. Spine J. 2019;19(7):1146–1153. doi:10.1016/j.spinee.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 75.Buyuk AF, Shafa E, Dawson JM, Schwender JD. Complications with minimally invasive transforaminal lumbar interbody fusion for degenerative spondylolisthesis in the obese population. Spine (Phila Pa 1976). 2019;44(23):E1401–E1408. doi:10.1097/BRS.0000000000003160 [DOI] [PubMed] [Google Scholar]
- 76.Cheng CW, Cizik AM, Dagal AHC, et al. Body mass index and the risk of deep surgical site infection following posterior cervical instrumented fusion. Spine J. 2019;19(4):602–609. doi:10.1016/j.spinee.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 77.Goh GS, Liow MHL, Yeo W, et al. The influence of body mass index on functional outcomes, satisfaction, and return to work after single-level minimally-invasive transforaminal lumbar interbody fusion: a five-year follow-up study. Spine (Phila Pa 1976). 2019;44(11):809–817. doi:10.1097/BRS.0000000000002943 [DOI] [PubMed] [Google Scholar]
- 78.Goyal A, Elminawy M, Kerezoudis P, et al. Impact of obesity on outcomes following lumbar spine surgery: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2019;177:27–36. doi:10.1016/j.clineuro.2018.12.012 [DOI] [PubMed] [Google Scholar]
- 79.Kashkoush A, Mehta A, Agarwal N, et al. Perioperative neurological complications following anterior cervical discectomy and fusion: clinical impact on 317,789 patients from the National inpatient sample. World Neurosurg. 2019;128:e107–e115. doi:10.1016/j.wneu.2019.04.037 [DOI] [PubMed] [Google Scholar]
- 80.Linhares D, Cacho Rodrigues P, Ribeiro da Silva M, et al. Minimum of 10-year follow-up of V-rod technique in lumbar spondylolysis. Eur Spine J. 2019;28(7):1743–1749. doi:10.1007/s00586-018-5833-4 [DOI] [PubMed] [Google Scholar]
- 81.Malik AT, Jain N, Kim J, Yu E, Khan SN. The impact of metabolic syndrome on 30-day outcomes following elective anterior cervical discectomy and fusions. Spine (Phila Pa 1976). 2019;44(5):E282–E287. doi:10.1097/BRS.0000000000002824. [DOI] [PubMed] [Google Scholar]
- 82.Mombell KW, Waldron JE, Morrissey PB, Saldua NS. Percutaneous pedicle screws in the obese: should the skin incision be more lateral? Cureus. 2019;11(6):e4966. doi:10.7759/cureus.4966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Villavicencio A, Lee Nelson E, Rajpal S, Vivek N, Burneikiene S. The impact of BMI on operating room time, blood loss, and hospital stay in patients undergoing spinal fusion. Clin Neurol Neurosurg. 2019;179:19–22. doi:10.1016/j.clineuro.2019.02.012 [DOI] [PubMed] [Google Scholar]
- 84.Yoo JS, Hrynewycz NM, Brundage TS, Singh K. The use of patient-reported outcome measurement information system physical function to predict outcomes based on body mass index following minimally invasive transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2019;44(23):E1388–E1395. doi:10.1097/BRS.0000000000003137 [DOI] [PubMed] [Google Scholar]
- 85.Zhang Y, Zhang J, Liu H, et al. Impact of obesity on restoration of sagittal balance and clinical efficacy after posterior lumbar interbody fusion. J Clin Neurosci. 2019;69:170–174. doi:10.1016/j.jocn.2019.07.074 [DOI] [PubMed] [Google Scholar]
- 86.Abbasi H, Grant A. Effect of body mass index on perioperative outcomes in minimally invasive oblique lateral lumbar interbody fusion versus open fusions: a multivariant analysis. Cureus. 2018;10(3):e2288. doi:10.7759/cureus.2288. PMID: 29770280; PMCID: PMC5953510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Akins PT, Inacio MCS, Bernbeck JA, et al. Do obese and extremely obese patients lose weight after lumbar spine fusions? Analysis of a cohort of 7303 patients from the Kaiser National Spine Registry. Spine. 2018;43(1):22–27. doi:10.1097/BRS.0000000000002456 [DOI] [PubMed] [Google Scholar]
- 88.Bono OJ, Poorman GW, Foster N, et al. Body mass index predicts risk of complications in lumbar spine surgery based on surgical invasiveness. Spine J. 2018;18(7):1204–1210. doi:10.1016/j.spinee.2017.11.015 [DOI] [PubMed] [Google Scholar]
- 89.Byval’tsev VA, Kalinin AA. Vozmozhnosti primeneniia minimal’no invazivnykh dorsal’nykh dekompressivno-stabiliziruiushchikh vmeshatel’stv u patsientov s izbytochnoĭ massoĭ tela i ozhireniem. Minimally invasive dorsal decompression-stabilization surgery in patients with overweight and obesity. Zh Vopr Neirokhir Im N N Burdenko. 2018;82(5):69–80. doi:10.17116/neiro20188205169 [DOI] [PubMed] [Google Scholar]
- 90.Chung AS, Campbell D, Waldrop R, Crandall D. Metabolic syndrome and 30-day outcomes in elective lumbar spinal fusion. Spine (Phila Pa 1976). 2018;43(9):661–666. doi:10.1097/BRS.0000000000002397 [DOI] [PubMed] [Google Scholar]
- 91.Jain D, Berven SH, Carter J, Zhang AL, Deviren V. Bariatric surgery before elective posterior lumbar fusion is associated with reduced medical complications and infection. Spine J. 2018;18(9):1526–1532. doi:10.1016/j.spinee.2018.01.023 [DOI] [PubMed] [Google Scholar]
- 92.Lovecchio F, Fu MC, Iyer S, Steinhaus M, Albert T. Does obesity explain the effect of the metabolic syndrome on complications following elective lumbar fusion? A propensity score matched analysis. Global Spine J. 2018;8(7):683–689. doi:10.1177/2192568218765149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Madsbu MA, Øie LR, Salvesen Ø, et al. Lumbar microdiscectomy in obese patients: a multicenter observational study. World Neurosurg. 2018;110:e1004–e1010. doi:10.1016/j.wneu.2017.11.156 [DOI] [PubMed] [Google Scholar]
- 94.Nahhas CR, Hu K, Mehta AI. Incidence and risk factors of wound complications in long segment instrumented thoracolumbar spinal fusions: a retrospective study. J Spine Surg. 2018;4(2):233–240. doi:10.21037/jss.2018.05.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Narain AS, Hijji FY, Haws BE, et al. Impact of body mass index on surgical outcomes, narcotics consumption, and hospital costs following anterior cervical discectomy and fusion. J Neurosurg Spine. 2018;28(2):160–166. doi:10.3171/2017.6.SPINE17288 [DOI] [PubMed] [Google Scholar]
- 96.Siccoli A, Schröder ML, Staartjes VE. Influence of dynamic preoperative body mass index changes on patient-reported outcomes after surgery for degenerative lumbar spine disease. Neurosurg Rev. 2020. doi:10.1007/s10143-020-01454-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ranson WA, Cheung ZB, Di Capua J, et al. Risk factors for perioperative complications in morbidly obese patients undergoing elective posterior lumbar fusion. Global Spine J. 2018;8(8):795–802. doi:10.1177/2192568218771363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Vinas-Rios JM, Sanchez-Aguilar M, Medina Govea FA, Von Beeg-Moreno V, Meyer F; DWG Registry-group. Incidence of early postoperative complications requiring surgical revision for recurrent lumbar disc herniation after spinal surgery: a retrospective observational study of 9,310 patients from the German Spine Register. Patient Saf Surg. 2018;12:9. PMID: 29942349; PMCID: PMC5961485. doi:10.1186/s13037-018-0157 -1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Wang T, Han C, Jiang H, Tian P. The effect of obesity on clinical outcomes after minimally invasive surgery of the spine: a systematic review and meta-analysis. World Neurosurg. 2018;110:e438–e449. PMID: 29138076. doi:10.1016/j.wneu.2017.11.010 [DOI] [PubMed] [Google Scholar]
- 100.Xie Q, Zhang J, Lu F, Wu H, Chen Z, Jian F. Minimally invasive versus open transforaminal lumbar interbody fusion in obese patients: a meta-analysis. BMC Musculoskelet Disord. 2018;19(1):15. doi:10.1186/s12891-018-1937-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Flippin M, Harris J, Paxton EW, et al. Effect of body mass index on patient outcomes of surgical intervention for the lumbar spine. J Spine Surg. 2017;3(3):349–357. doi:10.21037/jss.2017.06.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Grover PJ, Pushpananthan S, Samarage HM, Mendoza ND. Obesity and posterior spinal fat content: impact on complications in non-complex lumbar spine surgery. Br J Neurosurg. 2017;31(1):58–62. doi:10.1080/02688697.2016.1220502 [DOI] [PubMed] [Google Scholar]
- 103.Phan K, Rogers P, Rao PJ, Mobbs RJ. Influence of obesity on complications, clinical outcome, and subsidence after Anterior Lumbar Interbody Fusion (ALIF): prospective observational study. World Neurosurg. 2017;107:334–341. doi:10.1016/j.wneu.2017.08.014 [DOI] [PubMed] [Google Scholar]
- 104.Puvanesarajah V, Werner BC, Cancienne JM, et al. Morbid obesity and lumbar fusion in patients older than 65 years: complications, readmissions, costs, and length of stay. Spine. 2017;42(2):122–127. doi:10.1097/BRS.0000000000001692 [DOI] [PubMed] [Google Scholar]
- 105.Wang H, Ma L, Yang D, et al. Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine (Baltimore). 2017;96(5):e6032. doi:10.1097/MD.0000000000006032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wilson JR, Tetreault LA, Schroeder G, et al. Impact of elevated body mass index and obesity on long-term surgical outcomes for patients with degenerative cervical myelopathy: analysis of a combined prospective dataset. Spine. 2017;42(3):195–201. doi:10.1097/BRS.0000000000001859 [DOI] [PubMed] [Google Scholar]
- 107.Burgstaller JM, Held U, Brunner F, et al. The impact of obesity on the outcome of decompression surgery in degenerative lumbar spinal canal stenosis: analysis of the Lumbar Spinal Outcome Study (LSOS): a swiss prospective multicenter cohort study. Spine (Phila Pa 1976). 2016;41(1):82–89. doi:10.1097/BRS.0000000000001128 [DOI] [PubMed] [Google Scholar]
- 108.Chotai S, Sielatycki JA, Parker SL, et al. Effect of obesity on cost per quality-adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. Spine J. 2016;16(11):1342–1350. doi:10.1016/j.spinee.2016.06.023 [DOI] [PubMed] [Google Scholar]
- 109.Elsamadicy AA, Adogwa O, Vuong VD, et al. Patient body mass index is an independent predictor of 30-day hospital readmission after elective spine surgery. World Neurosurg. 2016;96:148–151. doi:10.1016/j.wneu.2016.08.097. PMID: 27593714. [DOI] [PubMed] [Google Scholar]
- 110.Higgins DM, Mallory GW, Planchard RF, et al. Understanding the impact of obesity on short-term outcomes and in-hospital costs after instrumented spinal fusion. Neurosurgery. 2016;78(1):127–132. doi:10.1227/NEU.0000000000001018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Huang S, Luo J, Li L, et al. Effect of body mass index on outcome of posterior 360 degrees fusion for single-level lumbar degenerative diseases. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2016;30(2):197–201. [PubMed] [Google Scholar]
- 112.Manson NA, Green AJ, Abraham EP. Elevated patient body mass index does not negatively affect self-reported outcomes of thoracolumbar surgery: results of a comparative observational study with minimum 1-year follow-up. Global Spine J. 2016;6(2):108–117. doi:10.1055/s-0035-1556585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sielatycki JA, Chotai S, Kay H, Stonko D, Mcgirt M, Devin CJ. Does obesity correlate with worse patient-reported outcomes following elective anterior cervical discectomy and fusion? Neurosurgery. 2016;79(1):69–74. doi:10.1227/NEU.0000000000001252 [DOI] [PubMed] [Google Scholar]
- 114.Sielatycki JA, Chotai S, Stonko D, et al. Is obesity associated with worse patient-reported outcomes following lumbar surgery for degenerative conditions? Eur Spine J. 2016;25(5):1627–1633. doi:10.1007/s00586-016-4460 -1 [DOI] [PubMed] [Google Scholar]
- 115.Sing DC, Yue JK, Metz LN, et al. Obesity is an independent risk factor of early complications after revision spine surgery. Spine. 2016;41(10):E632–640. doi:10.1097/BRS.0000000000001327 [DOI] [PubMed] [Google Scholar]
- 116.Sorimachi Y, Neva MH, Vihtonen K, et al. Effect of obesity and being overweight on disability and pain after lumbar fusion: an analysis of 805 patients. Spine (Phila Pa 1976). 2016;41(9):772–777. doi:10.1097/BRS.0000000000001356 [DOI] [PubMed] [Google Scholar]
- 117.Stienen MN, Joswig H, Smoll NR, et al. Influence of body mass index on subjective and objective measures of pain, functional impairment, and health-related quality of life in lumbar degenerative disc disease. World Neurosurg. 2016;96:570–577.e1. doi:10.1016/j.wneu.2016.09.070 [DOI] [PubMed] [Google Scholar]
- 118.Wang H, Ma L, Yang D, et al. Incidence and risk factors for the progression of proximal junctional kyphosis in degenerative lumbar scoliosis following long instrumented posterior spinal fusion. Medicine (Baltimore). 2016;95(32):e4443. doi:10.1097/MD.0000000000004443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang YP, Zhang W, An JL, Zhang J, Bai JY, Sun YP. Evaluation of transforaminal endoscopic discectomy in treatment of obese patients with lumbar disc herniation. Med Sci Monit. 2016;22:2513–2519. doi:10.12659/msm.899510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Adogwa O, Carr K, Thompson P, et al. A prospective, multi-institutional comparative effectiveness study of lumbar spine surgery in morbidly obese patients: does minimally invasive transforaminal lumbar interbody fusion result in superior outcomes? World Neurosurg. 2015;83(5):860–866. doi:10.1016/j.wneu.2014.12.034 [DOI] [PubMed] [Google Scholar]
- 121.Burks CA, Werner BC, Yang S, Shimer AL. Obesity is associated with an increased rate of incidental durotomy in lumbar spine surgery. Spine. 2015;40(7):500–504. doi:10.1097/BRS.0000000000000784 [DOI] [PubMed] [Google Scholar]
- 122.Cao J, Kong L, Meng F, Zhang Y, Shen Y. Impact of obesity on lumbar spinal surgery outcomes. J Clin Neurosci. 2016;28:1–6. doi:10.1016/j.jocn.2015.10.034 [DOI] [PubMed] [Google Scholar]
- 123.Giannadakis C, Nerland US, Solheim O, et al. Does obesity affect outcomes after decompressive surgery for lumbar spinal stenosis? A multicenter, observational, registry-based study. World Neurosurg. 2015;84(5):1227–1234. [DOI] [PubMed] [Google Scholar]
- 124.Goldin AN, Alander DH. Effect of body mass index on early outcomes of minimally invasive degenerative lumbar surgery. J Surg Orthop Adv. 2015;24(1):12–17. [PubMed] [Google Scholar]
- 125.Nota SP, Braun Y, Ring D, Schwab JH. Incidence of surgical site infection after spine surgery: what is the impact of the definition of infection? Clin Orthop Relat Res. 2015;473(5):1612–1619. doi:10.1007/s11999-014-3933-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Planchard RF, Higgins DM, Mallory GW, et al. The impact of obesity on perioperative resource utilization after elective spine surgery for degenerative disease. Global Spine J. 2015;5(4):287–293. doi:10.1055/s-0035-1546819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yagi M, Patel R, Boachie-Adjei O. Complications and unfavorable clinical outcomes in obese and overweight patients treated for adult lumbar or thoracolumbar scoliosis with combined anterior/posterior surgery. J Spinal Disord Tech. 2015;28(6):E368–376. doi:10.1097/BSD.0b013e3182999526 [DOI] [PubMed] [Google Scholar]
- 128.Auffinger B, Lam S, Kraninger J, Shen J, Roitberg BZ. The impact of obesity on surgeon ratings and patient-reported outcome measures after degenerative cervical spine disease surgery. World Neurosurg. 2014;82(1-2):e345–352. doi:10.1016/j.wneu.2013.09.053 [DOI] [PubMed] [Google Scholar]
- 129.Buerba RA, Fu MC, Gruskay JA, Long WD III, Grauer JN. Obese class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J. 2014;14(9):2008–2018. doi:10.1016/j.spinee.2013.11.047 [DOI] [PubMed] [Google Scholar]
- 130.Buerba RA, Fu MC, Grauer JN. Anterior and posterior cervical fusion in patients with high body mass index are not associated with greater complications. Spine J. 2014;14(8):1643–1653. doi:10.1016/j.spinee.2013.09.054 [DOI] [PubMed] [Google Scholar]
- 131.Marquez-Lara A, Nandyala SV, Sankaranarayanan S, Noureldin M, Singh K. Body mass index as a predictor of complications and mortality after lumbar spine surgery. Spine (Phila Pa 1976). 2014;39(10):798–804. doi:10.1097/BRS.0000000000000232 [DOI] [PubMed] [Google Scholar]
- 132.McGuire KJ, Khaleel MA, Rihn JA, Lurie JD, Zhao W, Weinstein JN. The effect of high obesity on outcomes of treatment for lumbar spinal conditions: subgroup analysis of the Spine Patient Outcomes Research Trial. Spine. 2014;39(23):1975–1980. doi:10.1097/BRS.0000000000000577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pereira BJ, de Holanda CV, Ribeiro CA, et al. Impact of body mass index in spinal surgery for degenerative lumbar spine disease. Clin Neurol Neurosurg. 2014;127:112–115. doi:10.1016/j.clineuro.2014.09.016 [DOI] [PubMed] [Google Scholar]
- 134.Quah C, Syme G, Swamy GN, Nanjayan S, Fowler A, Calthorpe D. Obesity and recurrent intervertebral disc prolapse after lumbar microdiscectomy. Ann R Coll Surg Engl. 2014;96(2):140–143. doi:10.1308/003588414X13814021676873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Seicean A, Alan N, Seicean S, et al. Impact of increased body mass index on outcomes of elective spinal surgery. Spine (Phila Pa 1976). 2014;39(18):1520–1530. doi:10.1097/BRS.0000000000000435 [DOI] [PubMed] [Google Scholar]
- 136.Srinivasan D, La Marca F, Than KD, Patel RD, Park P. Perioperative characteristics and complications in obese patients undergoing anterior cervical fusion surgery. J Clin Neurosci. 2014;21(7):1159–1162. doi:10.1016/j.jocn.2013.11.017 [DOI] [PubMed] [Google Scholar]
- 137.Wang J, Zhou Y, Feng Zhang Z, Qing Li C, Jie Zheng W, Liu J. Comparison of the clinical outcome in overweight or obese patients after minimally invasive versus open transforaminal lumbar interbody fusion. J Spinal Disord Tech. 2014;27(4):202–206. doi:10.1097/BSD.0b013e31825d68 ac [DOI] [PubMed] [Google Scholar]
- 138.Rihn JA, Kurd M, Hilibrand AS, et al. The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Jt Surg Am. 2013;95(1):1–8. doi:10.2106/JBJS.K.01558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Rosenfeld HE, Limb R, Chan P, Fitzgerald M, Bradley WP, Rosenfeld JV. Challenges in the surgical management of spine trauma in the morbidly obese patient: a case series. J Neurosurg Spine. 2013;19(1):101–109. doi:10.3171/2013.4.SPINE12876 [DOI] [PubMed] [Google Scholar]
- 140.Gaudelli C, Thomas K. Obesity and early reoperation rate after elective lumbar spine surgery: a population-based study. Evid Based Spine Care J. 2012;3(2):11–16. doi:10.1055/s-0031-1298613. PMID: 23230413; PMCID: PMC3516454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mehta AI, Babu R, Karikari IO, et al. 2012 young investigator award winner: the distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine (Phila Pa 1976). 2012;37(19):1652–1656. doi:10.1097/BRS.0b013e318241b186 [DOI] [PubMed] [Google Scholar]
- 142.Rihn JA, Radcliff K, Hilibrand AS, et al. Does obesity affect outcomes of treatment for lumbar stenosis and degenerative spondylolisthesis? Analysis of the Spine Patient Outcomes Research Trial (SPORT). Spine. 2012;37(23):1933–1946. doi:10.1097/BRS.0b013e31825e21b2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rodgers WB, Cox CS, Gerber EJ. Early complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech. 2010;23(6):393–397. doi:10.1097/BSD.0b013e3181b31729 [DOI] [PubMed] [Google Scholar]
- 144.Singh AK, Ramappa M, Bhatia CK, Krishna M.Less invasive posterior lumbar interbody fusion and obesity: clinical outcomes and return to work. Spine. 2010;35(24):2116–2120. doi:10.1097/BRS.0b013e3181cf0980 [DOI] [PubMed] [Google Scholar]
- 145.Yadla S, Malone J, Campbell PG, et al. Obesity and spine surgery: reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J. 2010;10(7):581–587. doi:10.1016/j.spinee.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 146.Walid MS, Robinson JS III, Robinson ER, Brannick BB, Ajjan M, Robinson JS, Jr. Comparison of outpatient and inpatient spine surgery patients with regards to obesity, comorbidities and readmission for infection. J Clin Neurosci. 2010;17(12):1497–1498. doi:10.1016/j.jocn.2010.03.037 [DOI] [PubMed] [Google Scholar]
- 147.Shamji MF, Parker S, Cook C, Pietrobon R, Brown C, Isaacs RE. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009;65(3):490–498. Discussion 498. doi:10.1227/01.NEU.0000350863.69524.8E [DOI] [PubMed] [Google Scholar]
- 148.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976). 2009;34(5):495–500. doi:10.1097/BRS.0b013e318198c5f2 [DOI] [PubMed] [Google Scholar]
- 149.Park P, Wang MY, Nguyen S, et al. Comparison of complications and clinical and radiographic outcomes between nonobese and obese patients with adult spinal deformity undergoing minimally invasive surgery. World Neurosurg. 2016;87:55–60. doi:10.1016/j.wneu.2015.12.024 [DOI] [PubMed] [Google Scholar]
- 150.Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG. Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery. 2008;63(5):956–960. doi:10.1227/01.NEU.0000313626.23194.3F [DOI] [PubMed] [Google Scholar]
- 151.Sonne-Holm S, Jacobsen S, Rovsing HC, Monrad H, Gebuhr P. Lumbar spondylolysis: a life long dynamic condition? A cross sectional survey of 4.151 adults. Eur Spine J. 2007;16(6):821–828. doi:10.1007/s00586-006-0250-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Telfeian AE, Reiter GT, Durham SR, Marcotte P. Spine surgery in morbidly obese patients. J Neurosurg. 2002;97(1 Suppl):20–24. doi:10.3171/spi.2002.97.1.0020 [DOI] [PubMed] [Google Scholar]
- 153.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997;10(5):376–379. [PubMed] [Google Scholar]
- 154.Ramos RD la G, Nakhla J, Nasser R, et al. Effect of body mass index on surgical outcomes after posterior spinal fusion for adolescent idiopathic scoliosis. Neurosurg Focus. 2017;43(4):E5. doi:10.3171/2017.7.FOCUS17342 [DOI] [PubMed] [Google Scholar]
- 155.McLaughlin T, Sherman A, Tsao P, et al. Enhanced proportion of small adipose cells in insulin-resistant vs insulin-sensitive obese individuals implicates impaired adipogenesis. Diabetologia. 2007;50(8):1707–1715. doi:10.1007/s00125-007-0708-y [DOI] [PubMed] [Google Scholar]
- 156.Wang Y, Rimm EB, Stampfer MJ, Willett WC, Hu FB. Comparison of abdominal adiposity and overall obesity in predicting risk of type 2 diabetes among men. Am J Clin Nutr. 2005;81(3):555–563. doi:10.1093/ajcn/81.3.555 [DOI] [PubMed] [Google Scholar]
- 157.Laviola L, Perrini S, Cignarelli A, et al. Insulin signaling in human visceral and subcutaneous adipose tissue in vivo. Diabetes. 2006;55(4):952–961. doi:10.2337/diabetes.55.04.06.db05-1414 [DOI] [PubMed] [Google Scholar]
- 158.Kershaw EE, Flier JS. Adipose tissue as an endocrine organ. J Clin Endocrinol Metab. 2004;89(6):2548–2556. [DOI] [PubMed] [Google Scholar]
- 159.Reaven GM.The insulin resistance syndrome: definition and dietary approaches to treatment. Ann Rev Nutr. 2005;25:391–406. doi:10.1146/annurev.nutr.24.012003.132155 [DOI] [PubMed] [Google Scholar]
- 160.Polyzos SA, Margioris AN. Sarcopenic obesity. Hormones. 2018;17(3):321–331. doi:10.1007/s42000-018-0049-x [DOI] [PubMed] [Google Scholar]
- 161.Barazzoni R, Bischoff S, Boirie Y, et al. Sarcopenic obesity: time to meet the challenge. Obesity Facts. 2018;11(4):294–305. doi:10.1159/000490361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kao LS, Meeks D, Moyer VA, Lally KP. Peri-operative glycaemic control regimens for preventing surgical site infections in adults. Cochrane Database Syst Rev. 2009;(3):CD006806. doi:10.1002/14651858.CD006806.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Turina M, Fry DE, Polk HC, Jr. Acute hyperglycemia and the innate immune system: clinical, cellular, and molecular aspects. Crit Care Med. 2005;33(7):1624–1633. doi:10.1097/01.ccm.0000170106.61978.d8. PMID: 16003073. [DOI] [PubMed] [Google Scholar]
- 164.Witek AM, Benzel EC. Obesity in cervical spine surgery. World Neurosurg. 2014;82(1-2):e147–e148. doi:10.1016/j.wneu.2014.02.014 [DOI] [PubMed] [Google Scholar]
- 165.Hanigan WC, Elwood PW, Henderson JP, Lister JR. Surgical results in obese patients with sciatica. Neurosurgery. 1987;20(6):896–899. doi:10.1227/00006123-198706000-00012 [DOI] [PubMed] [Google Scholar]
- 166.Jain D, Berven S. Effect of obesity on the development, management, and outcomes of spinal disorders. J Am Acad Orthop Surg. 2019;27(11):e499–e506. doi:10.5435/JAAOS-D-17-00837 [DOI] [PubMed] [Google Scholar]
- 167.Pierce KE, Kapadia BH, Bortz C, et al. Operative fusion of patients with metabolic syndrome increases risk for perioperative complications. J Clin Neurosci. 2020;72:142–145. doi:10.1016/j.jocn.2019.12.043 [DOI] [PubMed] [Google Scholar]
- 168.Snowden RD, Prusick VW, Oeffinger DJ, Iwinski HJ, Muchow RD. Increased acute postoperative wound problems following spinal fusion in overweight patients with adolescent idiopathic scoliosis. J Pediatr Orthop B. 2019;28(4):374–379. doi:10.1097/BPB.0000000000000610 [DOI] [PubMed] [Google Scholar]
- 169.Childs BR, Nahm NJ, Dolenc AJ, Vallier HA. Obesity is associated with more complications and longer hospital stays after orthopaedic trauma. J Orthop Trauma. 2015;29(11):504–509. doi:10.1097/BOT.0000000000000324 [DOI] [PubMed] [Google Scholar]
- 170.Koreckij T, Park DK, Fischgrund J. Minimally invasive spine surgery in the treatment of thoracolumbar and lumbar spine trauma. Neurosurg Focus. 2014;37(1):E11. doi:10.3171/2014.5.FOCUS1494 [DOI] [PubMed] [Google Scholar]
- 171.Yamada K, Abe Y, Satoh S, Yanagibashi Y, Hyakumachi T, Masuda T. Large increase in blood pressure after extubation and high body mass index elevate the risk of spinal epidural hematoma after spinal surgery. Spine. 2015;40(13):1046–1052. doi:10.1097/BRS.0000000000000876 [DOI] [PubMed] [Google Scholar]
- 172.Bohl DD, Ahn J, Mayo BC, et al. Does greater body mass index increase the risk for revision procedures following a single-level minimally invasive lumbar discectomy? Spine. 2016;41(9):816–821. doi:10.1097/BRS.0000000000001340145 [DOI] [PubMed] [Google Scholar]
- 173.Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003;28(15 Suppl):S26–35. doi:10.1097/01.brs.0000076895.52418.5e [DOI] [PubMed] [Google Scholar]
- 174.Stevens KJ, Spenciner DB, Griffiths KL, et al. Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech. 2006;19(2):77–86. doi:10.1097/01.bsd.0000193820.42522.d9 [DOI] [PubMed] [Google Scholar]
- 175.Kim KT, Lee SH, Suk KS, Bae SC. The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine. 2006;31(6):712–716. doi:10.1097/01.brs.0000202533.05906.ea [DOI] [PubMed] [Google Scholar]
- 176.Nomura H, Yamashita A, Watanabe T, Shirasawa K. Quantitative analysis of indirect decompression in extreme lateral interbody fusion and posterior spinal fusion with a percutaneous pedicle screw system for lumbar spinal stenosis. J Spine Surg. 2019;5(2):266–272. doi:10.21037/jss.2019.06.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yoshihara H. Indirect decompression in spinal surgery. J Clin Neurosci. 2017;44:63–68. doi:10.1016/j.jocn.2017.06.061 [DOI] [PubMed] [Google Scholar]
- 178.Cofano F, Marengo N, Ajello M, et al. The Era of cortical bone trajectory screws in spine surgery: a qualitative review with rating of evidence. World Neurosurg. 2020;134:14–24. doi:10.1016/j.wneu.2019.10.079 [DOI] [PubMed] [Google Scholar]
- 179.Boukebir MA, Berlin CD, Navarro-Ramirez R, et al. Ten-step minimally invasive spine lumbar decompression and dural repair through tubular retractors. Oper Neurosurg. 2017;13(2):232–245. doi:10.1227/NEU.0000000000001407 [DOI] [PubMed] [Google Scholar]
- 180.Passias PG, Horn SR, Vasquez-Montes D, et al. Prior bariatric surgery lowers complication rates following spine surgery in obese patients. Acta Neurochir (Wien). 2018;160(12):2459–2465. doi:10.1007/s00701-018-3722-6 [DOI] [PubMed] [Google Scholar]