Abstract
Study Design:
Systematic review.
Objective:
Providing a comprehensive review of spinal cord injury cost of illness studies to assist health-service planning.
Methods:
We conducted a systematic review of the literature published from Jan. 1990 to Nov. 2020 via Pubmed, EMBASE, and NHS Economic Evaluation Database. Our primary outcomes were overall direct health care costs of SCI during acute care, inpatient rehabilitation, within the first year post-injury, and in the ensuing years.
Results:
Through a 2-phase screening process by independent reviewers, 30 articles out of 6177 identified citations were included. Cost of care varied widely with the mean cost of acute care ranging from $290 to $612,590; inpatient rehabilitation from $19,360 to $443,040; the first year after injury from $32,240 to $1,156,400; and the ensuing years from $4,490 to $251,450. Variations in reported costs were primarily due to neurological level of injury, study location, methodological heterogeneities, cost definitions, study populations, and timeframes. A cervical level of the injury, ASIA grade A and B, concomitant injuries, and in-hospital complications were associated with the greatest incremental effect in cost burden.
Conclusion:
The economic burden of SCI is generally high and cost figures are broadly higher for developed countries. As studies were only available in few countries, the generalizability of the cost estimates to a regional or global level is only limited to countries with similar economic status and health systems. Further investigations with standardized methodologies are required to fill the knowledge gaps in the healthcare economics of SCI.
Keywords: spinal cord injuries, paraplegia, quadriplegia, cost of illness
Introduction
Global Burden of Disease Study estimated that in 2016 the annual global incidence of traumatic spinal cord injury (SCI) was 0.93 million (0.78-1.16 million), with an age-standardized incidence rate of 13 (11-16) per 100,000 population. 1 SCI incidence is relatively low compared with other chronic diseases; however, the consequences are disproportionally high. SCI results in significant physical and psychosocial burdens for individuals, their relatives, and for the health, social, and medico-social systems as a whole. 2 In addition to the physical and psychosocial trauma, the economic burden is substantial, predominantly due to permanent disability, the occurrence of the injury in younger ages, increased health care costs as well as higher rates of morbidity and premature mortality.3,4 In the United States, for example, the national costs attributable to SCI-related hospitalizations in 2009 estimated at approximately $1.7 billion. 5
Given the high economic burden of the disease and with the challenges of budget crises, information on the cost of care is necessary to provide optimal care to individuals with SCI. Cost of illness studies are primarily conducted to raise awareness for the financial burden of diseases, provide evidence for funding for care, and identify potential opportunities to design additional research and more efficient services. 6 Investigations into the economic burden of SCI are inconsistent, often have limited to specific regions, databases, population groups, a subgroup of patients with SCI (specific level of injury, certain etiology), or different periods of care (e.g. acute hospitalization, first year). 7 So there is a need for a comprehensive synthesis of previous research and assessment of the components and drivers of cost variation. This study aims to provide an updated, comprehensive review of previous research on the cost of treating SCI from the payer’s perspective in different countries. In doing so, we considered the variation in reported costs according to country, trauma subgroups, predictors of cost, and the costing methods employed. Finally, we tried to address the existing discrepancies in the literature related to the costs of SCI to be considered in future researches.
Methods
A systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. 8 Using the keywords “costs and cost analysis,” “Economics,” “Spinal Cord Injuries,” “Paraplegia,” “Quadriplegia,” and “Spinal Cord,” a comprehensive literature search was performed in PubMed EMBASE, and NHS Economic Evaluation Database via Cochrane Library for articles published between January 1990 and November 2020. The exact search strategy and keywords for each database are available in Supplementary file 1. There were no restrictions on language or publication status. Additionally, the reference list of each eligible article was screened to find additional articles.
Selection Method and Data Extraction
We searched for all cost of illness studies that reported overall direct costs of care for SCI. Direct costs include medical costs, which are typically associated with medical resource utilization and include in-patient, out-patient, and pharmaceutical services within the health care system, 9 and non-medical costs, which represent the costs associated with non-prescribed supplies and equipment, transportation, meals for patients, and caregivers, etc. Two reviewers independently screened the title and abstract of each paper to identify potentially eligible studies. We then selected studies that met the eligibility criteria for full-text evaluation. Discrepancies regarding the eligibility of studies were resolved through the decision of a third reviewer and group discussion. The required data was then extracted by 2 authors and entered into predefined sheets. The extracted information included the title and first author’s name, year of publication, study duration, design, sample size, setting (hospital/local/national) and location, participant characteristics including the level of SCI (cervical, thoracic, lumbosacral), clinical presentation (tetraplegia, paraplegia), cost currency, and direct costs of care for SCI (Table 1).
Table 1.
Characteristics of Included Studies.
| Study | Country, time-frame | Study type | Participants | Participants data source | Participants identification | Source of cost data | Costing approach | Details on cost items |
|---|---|---|---|---|---|---|---|---|
| New and Jackson 2010 | Australia 2003-2004 |
Retro. Cohort | 564 (170 traumatic and 394 nontraumatic) | Database from public hospitals included in the Victorian Cost Weights Study | ICD-10-AM | Victorian Department of Human Services (VDHS) costing database | Top-down, Diagnosis-Related Group |
Medical, nursing, allied health, and pharmacy |
| Vaikuntam et al, 2019 | Australia 2013-2016 |
Retro. Cohort | 534 ≥ 16 year-olds with acute TSC | NSW Admitted Patient Data Collection (APDC) and Emergency Department Data Collection | ICD-10-AM | NSW Activity-based Funding District Network Return Data | Bottom-up, Activity-based |
Costs incurred by health service providers, except staff salaries and operation costs, for all emergency department (ED) and admitted hospital separations |
| Dryden et al, 2004 | Canada 1992-1994 |
Retro. Cohort | 233 with TSCI | Alberta Health Care Insurance Stakeholder Registry | ICD-9-CM | Cost List for Manitoba Health Services (adjusted for Alberta which provides an average cost per day for each RDRG, and Claims database | Top-down, Diagnosis Related Group, and actual costs of physician services abstracted from the Claims database |
Hospitalizations, physician services, home care services, long-term admissions, and occurrence of secondary complications. The initial hospitalization included acute care hospitalization and inpatient rehabilitation. |
| Bradbury et al, 2008 | Canada NS |
Retro. Cohort | 10 SCI without traumatic brain injury | Spinal Cord Rehabilitation Program of Toronto Rehabilitation Institute | NS | Hospital records | Top-down Resource Utilization Group (RUG) (based on FIM) |
Clinician workload, nursing, physiotherapy, occupational therapy, rehabilitation therapy, and speech language pathology |
| Mac-Thiong et al, 2012 | Canada 2000-2011 |
Retro. Cohort | 477 with TSCI | Quebec Trauma Registry | ICD-9-CM | Quebec Trauma Registry and Niveau Intensité Relative des Ressources Utilisées index (NIRRU1) | Top-down, Diagnosis Related Group (based on NIRRU) |
All resources related to hospitalization. |
| Munce et al, 2013 | Canada 2003-2004 & 2005-2006 |
Retro. Cohort | 559 with TSCI | Rick Hansen Foundation database | ICD-10 | Resource intensity weight and provincial average cost from Ontario Ministry of Health and Long-Term Care (MOHLTC), and patients discharge abstracts | Top-down, Diagnosis Related Group |
Acute inpatient, ED, hospital rehabilitation, complex continuing care1, home health care services, and physician but not medication costs |
| Radhakrishna et al, 2014 | Canada 1997-2007 |
Retro. Cohort | 481 who sustained SCI from motor vehicle accident | Quebec Trauma Registry (RTQ2) | Using the terms spinal cord injury and motor vehicle collisions | Quebec Medical Insurance Agency (RAMQ3), and Quebec Provincial Automobile Insurer (SAAQ4) |
Top-down, Per-diem Quebec hospital cost |
Initial hospitalization (including therapy, imaging, medication, surgery, and the hospitals fixed costs), practitioners fees, medications, environmental modifications, and personal aides |
| Richard-Denis et al 2017 | Canada 2008-2014 |
Retro. Cohort | 116 with motor-complete (AIS A, B) cervical SCI | Individuals admitted to a level I SCI-specialized trauma center | – | Hospital database and Niveau Intensité Relative des Ressources Utilisées index (NIRRU) | Top-down, Diagnosis Related Group (based on NIRRU) |
The NIRRU index includes all resources related to hospitalization. Physician fee and costs related to the spine surgery and tracheostomy placement were not available. |
| Porgo et al, 2019 | Canada 2019 |
Retro. Cohort | 614 ≥ 16-year-olds admitted to adult trauma centers | Quebec trauma registry | – | Hospital financial reports (AS-471) for the 2016 fiscal year | Bottom-up Activity-based |
Non-physician personnel, services and materials costs in ED, medical ward, OR, ICU, imaging, and para-clinical services. drugs, laboratory tests, blood products, and physician fees were not included |
| Li et al, 2011 | China 2002 |
Retro. Cohort | 710 with TSCI | Information Center of Beijing Health Bureau | Using the term paraplegia or tetraplegia in Chinese language | Information Center of Beijing Health Bureau | Top-down | NS |
| Jiménez-Avila et al, 2012 | Mexico 2004-2007 |
Retro. Cohort | 34 ≥ 16-year-olds with complete cervical SCI | Individuals with a diagnosis of complete cervical spinal cord injury | – | Hospital records | Bottom-up (charges) |
The cost calculation was done considering bed days, specialty consultation, laboratory, X-ray, axial computed tomography, MRI, and surgery. |
| Kawu et al, 2011 | Nigeria 2009 |
Pros. Cohort | 34 cases with SCI | Spinal cord injured adults at the University of Abuja Hospital | – | Hospital bills paid on discharge | Bottom-up (charges) |
Nursing/medical care, accommodation, bed fees, drugs, laboratory charges and operative procedures; But not hospital staff and physicians fees, and medical equipment costs |
| Tsai et al, 2005 | Taiwan 1998-2000 |
Retro. Cohort | 184 with cervical SCI | Bureau of National Health Insurance (BNHI) database | ICD-9-CM | Annual in-patient expenses information system of the BNHI | Top-down | Total in-patient and medical order items |
| Yang et al, 2008 | Taiwan 2000-2003 |
Retro. Cohort | 15,510 with acute TSCI | National Health Insurance (NHI) database | ICD-9-CM | National Health Insurance Bureau (NHIB) datasets, including monthly claim summary for inpatient claims, inpatient expenditures by admissions and details of inpatient orders | Top-down | The datasets including details of inpatient orders, monthly claim summary for inpatient claims and inpatient expenditures by admissions were selected. |
| Lessing et al, 2020 | Tanzania 2016-2019 |
Retro. Cohort | 125 > 14 year-olds | Muhimbili Orthopaedic Institute database | – | Hospital records | Bottom-up Activity-based |
The sum of direct costs during admission. For nonoperative patients calculated by adding the cost of initial imaging, LOS, OR fee, surgical implants, and postop. imaging |
| Price et al, 1994 | USA 1989 |
Retro. Cohort | 376 with TSCI | Population-based statewide surveillance system | ICD-9-CM | Estimated or actual charges for acute care and rehabilitation hospitalization | Bottom-up (charges) |
All charges of acute care and rehabilitation except physician services, outpatient rehabilitation, emergency transportation and later admissions |
| Johnson et al, 1996 | USA 1989 |
Retro. Cohort | 115 with TSCI | Colorado Spinal Cord Injury Early Notification System (ENS) | ICD-9 | Participants were asked about the names of all providers and billing information was obtained from providers. | Bottom-up (hospital or outpatient charges) |
Medical services, medical supplies and equipment, in-home care, and the names of providers. Providers are asked for Billing information |
| Chan et al, 1997 | USA 1987-1994 |
Retro. Cohort | NS, discharges from rehab hospitals (non-acute rehab) | Medicare billing records and selected hospital cost reports | – | Records of hospital charges on Medicare | Bottom-up (charges) |
NS |
| Cifu et al, 1999 | USA, 1988-1996 |
Retro. Cohort | 2,099 adults with tetraplegia TSCI | National Model Spinal Cord Injury Systems program | Individuals with paraplegia SCI | Hospital billing records | Bottom-up (estimated or actual hospital bills) |
Acute care and inpatient rehabilitation |
| Cifu et al, 1999 | USA 1988-1996 |
Retro. Cohort | 2,169 adult persons with paraplegia TSCI | National Model Spinal Cord Injury Systems program | Individuals with paraplegia SCI | Hospital billing records | Bottom-up Activity-based (estimated or actual hospital charges) |
Acute care and inpatient rehabilitation |
| McKinley et al, 2001 | USA 1992-1999 |
Retro. Cohort | 172 rehabilitation inpatients (86 with TSCI and 86 nontraumatic SCI) | National Model Spinal Cord Injury Systems program compiled on the NIDRR7 SCI Database | NS | Actual rehabilitation hospital charges for each patient | Bottom-up (charges) |
Nursing, occupational therapy, physiatry and related medical services, physical therapy, psychologic and neurologic assessment, recreational therapy, and social services |
| Seel et al, 2001 | USA 1988-1998 |
Retro. Cohort | 180 adults with paraplegia | National Model Spinal Cord Injury Systems program compiled on the NIDRR5 SCI Database | – | Actual hospital charges for each patient | Bottom-up (charges) |
|
| Smith et al, 2003 | USA 1993-1999 |
Retro. Cohort | 47 with SCI Caused by Gunshot wounds | National Rehabilitation Hospital | Nonacute rehabilitative care recipients | Completed bills for 12 of the 47 persons | Bottom-up (rehabilitation hospital charges) |
NS |
| Webster et al, 2004 | USA 1989-1999 |
Retro. Cohort | 62 with work-related tetraplegia | The workers compensation database | Cross-referencing NCCI codes specific to: body part injured and injury type with relevant word search terms in the accident description | Compensation insurer data source covering 8-10% of the US private workers compensation market | Top-down | Initial hospitalization, acute rehabilitation, subsequent hospital and rehabilitation readmissions, outpatient services (i.e., physician and therapy visits, diagnostic services), pharmacy and medical supplies, vehicle and home modifications, personal care attendants, and ambulance/assisted transportation. |
| French et al, 2007 | USA 2005 |
Retro. Cohort | 675 veterans with SCI | Veterans Health Administration (VHA) administrative database | Non-ventilator dependent wheelchair user veterans with SCI over 2 years | The Decision Support System National Data Extracts (DSS-NDE) | Bottom-up Activity-based (DSS provided costs) |
All outpatient and inpatient care i.e. hospitalization and surgery, medications, radiology, laboratory, nursing care, prosthetics, rehabilitation, and nursing home care |
| Yu et al, 2008 | USA 1999-2001 |
Retro. Cohort | 1,181 veterans with SC | VA National Patient Care Databases (NPCDs) | ICD-9 | VA Health Economics Resource Center Average Cost File (ACF) | Top-down Medicare’s Diagnosis Related Group |
Inpatient and outpatient care at VA facilities |
| DeVivo et al, 2011 | USA 2000-2006 |
Retro. Cohort | 1,676 with SCI | National SCI Statistical Center (NSCISC) database | A random sample of 508 treated from 1973 to 1988 and 227 newly injured in 1989 | Charges reflect the average amount billed to individuals or third parties | Bottom-up | Inpatient acute care and rehabilitation, emergency medical services, nursing home, outpatient services, physician fees, equipment, environmental modifications, medications, supplies, attendant care, vocational rehabilitation |
| Deutsch et al, 2011 | USA 2002-2006 |
Retro. Cohort | 2919 > 64 Medicare fee-for-service cases | Medicare claims and assessment data files | ICD-9-CM | Patient-level Medicare billing (ie, claims) records (Medicare Provider Analysis and Review file) | Top-down (The total amount paid to the rehabilitation hospital) |
Part A services |
| Krause et al, 2019 | USA 2011-2015 |
Retro. Cohort | 303 | State-wide SCI Surveillance System Registry | ICD-9-CM | South Carolina Revenue and Fiscal Affairs, Health and Demographics records | Bottom-up (acute hospital care charges) |
Costs related to health care utilization for ED visits and hospitalizations. |
| Sikka et al, 2019 | USA, 2003-2014 |
Retro. Cohort | 591 with TSCI | Trauma registry data merged with the regional hospital registry database (DFWHC)6 | ICD-9 | DFWHC database | Bottom-up (acute hospital care charges) |
NS |
1 Niveau Intensité Relative des Ressources Utilisées index (NIRRU); relative intensity of resources, 2 Registre des traumatismes du Québec, 3 Régie de l’assurance maladie du Québec, 4 Société de l’assurance automobile du Québec, 5 National Institute on Disability, Independent Living and Rehabilitation Research (NIDRR), 6 Dallas-Fort Worth Hospital Council.
Eligibility Criteria and Risk of Bias
Our primary outcome was to determine health care costs of SCI during 1) acute care, from index admission to the first discharge to any location other than transfer to acute care in another hospital, 2) inpatient rehabilitation 3) the first year post-injury, and 4) ensuing years; both regardless and stratified by the extent of neurological deficit. Secondary outcomes were to determine components and drivers of cost. All studies with at least 10 cases that reported either any of the primary outcomes were included in the study. Studies reporting indirect costs, a subcategory of costs, costs through modeling/extrapolation methods, and studies from a common database except for the latest one were not included. Furthermore, studies with a population of mainly vertebral column injuries without concomitant SCI and those that were only pediatric were excluded. All currencies were converted to US dollars (USD) using foreign exchange rates provided by the Federal Reserve System, the Central bank of the United States 10 and were adjusted to Nov. 2020 values using the Consumer Price Index by the U.S. Bureau of Labor Statistics. 11 Global Domestic Products (GDP) per capita from the year of the currency for each study were obtained from the World Bank website. 12 For critical appraisal, We used a slightly adjusted form of the checklist developed by Public Health Wales Observatory Evidence Service 13 based on a study by Larg A and Moss J. 14 The final statement had 13 items relating to analytical framework, methodology, analysis, and reporting (Supplementary file2). Each item in the checklist was given a score of −1, 0, or 1, with a score of 1 if the item was appropriately fulfilled.
Results
General Findings
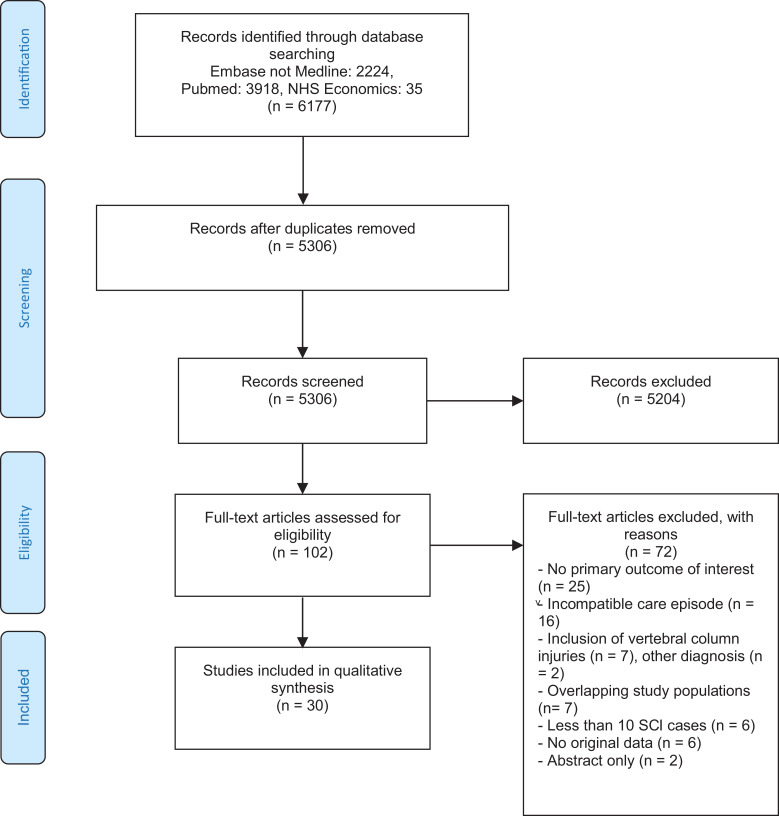
The search identified 6,177 studies, which was reduced to 5,306 after the removal of duplicates. An evaluation of titles and abstracts resulted in the removal of 5,204 articles. The remaining 102 studies underwent full-text assessment for eligibility. Seventy-two studies were excluded based on various reasons, mainly due to a lack of data on our primary outcomes, incompatible care period, inclusion of vertebral column injuries without concomitant SCI, and absence of original data (Figure 1). The list of excluded articles at full-text assessment and Reasons of exclusion are presented in Supplementary file 2. Finally, the remaining 30 studies were included here. Most studies originated in North America (the U.S.: 15 studies,15-29 and Canada: 730-36); and the rest were conducted in Australia,37,38 China, 39 Mexico, 40 Nigeria, 41 Taiwan,42,43 and Tanzania. 44 Sample sizes ranged from 34 to 15,510, and settings varied from hospital-based to nationwide. The methodologies, cost perspectives, and sources of cost data varied considerably among studies; with 13 studies took a top-down approach, and the rest including most of the U.S. studies used bottom-up approaches. The characteristics of the included articles are summarized in Table 1.
Figure 1.
PRISMA 2009 flow diagram.
The cost of care varied widely with the mean cost of acute care ranging from $290 41 to $612,590, 26 inpatient rehabilitation from $19,536 17 to $443,044, 22 the first year after index injury costs from $32,238 30 to $1,156,406, 26 and the ensuing years following the first year from $4,392 17 to $200,810 26 (Table 1). Scores for critical appraisal ranged from −4 to 11 points with a median score of 5. Results of the quality assessment of each study are presented in Supplementary file 2.
Acute Care
A total of 21 studies reported the mean cost of hospital acute care in 8 countries. The lowest costs were found in Nigeria, 41 Tanzania, 44 China, 39 and Taiwan42,43 ($290 to $4,860). A study from Mexico reported the mean cost of acute care for complete cervical SCI to be $29,940. 40 In Australia, the cost of acute care varied from $42,600 for cases with paraplegia to $63,134 for quadriplegia. 38 The costs in Canada ranged from $39,330 for incomplete paraplegia to $138,620 for complete quadriplegia.30,34 Richard-Denis et al showed the mean cost of acute care in a specialized SCI center for individuals with motor-complete SCI was $10,120 for early transfer and $15,443 if transferred after surgery, but omitted all costs related to the spine surgery and tracheostomy as well as physician fees. 35 Although the highest figures were reported in the U.S., which ranged from $73,850 for Asia Impairment Score (AIS) group D, E to $612,590 for C1-C4 AIS A, B, C cases,15,17-19,21,26,29 these figures were charges rather than actual costs (Table 2). The average charges for acute care of SCI regardless of the neurologic category was reported from $92,220 to $337,400 in the U.S.17,26,29 The corresponding costs were $29,550 to $61,180 in Australia37,38 and $9,980 to $34,202 in Canada.32,33,36 The acute care costs as a percentage of the GDP per capita were variable from 68% to 110% for Australia, 47% to 73% for Canada, 281% to 590% for the US, and from 12% to 123% for low-to-middle income countries (LMIC) (Table 3).
Table 2.
Average Direct Health Care Costs/Charges* Per Case Stratified by Neurologic Level of SCI.
| Ref. | Study, year | Country | Tetraplegia (C1-C8) | Paraplegia (T1-S5) | AIS D | ||
|---|---|---|---|---|---|---|---|
| Incomplete | Complete | Incomplete | Complete | ||||
| Mean ± SD (median) costs per case in 2020 USD | |||||||
| Acute hospital care | |||||||
| 37 | Vaikuntam et al, 2019 | Australia | 63,134 ± 80,609 (36,706) | T1-T12: 71,030 ± 80,722 (51,238) L1-L5: 42,601 ± 70,059 (24,558) |
– | ||
| 29 | Dryden et al§, 2004 | Canada | 39,330 | 133,192 | T1-T12: 30,395 | T1-T12: 91,835 | - |
| Lumbar/CES: 41,173 | |||||||
| 33 | Radhakrishna et al, 2014 | Canada | 46,714 | 138,621 | C8-T6: 49,504 T7-L1: 40,201 |
C8-T6: 67,319 T7-L1: 44,257 |
- |
| L2-S5: 55,588 | |||||||
| 34 | Richard-Denis et al, 2017 | Canada | – | SCI center: (10,120) NS center: (15,443) |
– | – | – |
| 39 | Jiménez-Ávila, 2012 | Mexico | – | 29,941 | – | – | – |
| 41 | Tsai et al, 2005 | Taiwan | C1-C4: 2,765 ± 4,442 SD | – | – | – | |
| 14 | Price et al, 1994 | USA | (35,594)* | (145,226)* | (37,743)* | (67,808)* | – |
| 16 | Johnson et al, 1996 | USA | C1-C4 AIS A-C: 206,643 (152,275)* C5-C8 AIS A-C: 230,937 (154,844)* |
AIS A-C: 150,895 (122,864)* | 73,847 (39,503)* (AIS D, E) |
||
| 17 | Cifu et al, 1999 | USA | 131,450* | – | – | – | |
| 18 | Cifu et al, 1999 | USA | – | – | 100,030* | – | |
| 20 | Seel et al, 2001 | USA | – | – | 81,840 to 108,876 | – | |
| 25 | DeVivo et al, 2011 | USA | C1-C4 AIS A-C: 612,590* C5-C8 AIS A-C: 437,922* |
AIS A-C: 311,726* | 207,316* | ||
| 28 | Sikka et al, 2019 | USA | (84,002)* | (111,922)* | |||
| Rehabilitation | |||||||
| 14 | Price et al, 1994 | USA | (57,048) | (43,930) | (39,439) | (38,306) | – |
| 16 | Johnson et al, 1996 | USA | C1-C4 AIS A-C: 240,848 (184,491)* C5-C8 AIS A-C: 264,932 (223,351)* |
AIS A-C AIS A-C: 127,124 (107,152)* | 19,536 (0)* (AIS D, E) |
||
| 17 | Cifu et al, 1999 | USA | 159,610* | – | – | – | |
| 18 | Cifu et al, 1999 | USA | – | – | 98,176* | – | |
| 20 | Seel et al, 2001 | USA | – | – | 85,514 to 102,734 | – | |
| 21 | Smith et al, 2003 | USA | 443,044* | T1-T12: 109,116* L1-L5: 77,329* |
– | ||
| 25 | DeVivo et al, 2011 | USA | C1-C4 AIS A-C: 347,215* C5-C8 AIS A-C: 261,155* |
T1-S1 AIS A-C: 161,690* | 119,363* | ||
| First year | |||||||
| 29 | Dryden et al, 2004 | Canada | 42,093 | 138,996 | T1-12: 32,238 | T1-12: 96,348 | - |
| L1-L5/CES: 43,476 | |||||||
| 33 | Radhakrishna et al, 2014 | Canada | 60,058 | 167,637 | C8-T6: 61,334 T7-L1: 47,326 |
C8-T6: 102,534 T7-L1: 75,425 |
- |
| L2-S5: 73,248 | |||||||
| 16 | Johnson et al, 1996 | USA | C1-C4 AIS A-C: 689,091 (577,669)* C5-C8 AIS A-C: 643,908 (447,814)* |
AIS A-C: 344,808 (276,569)* | 111,783 (78,456)* (AIS D, E) |
||
| 22 | Webster et al, 2004 | USA | C1-C4 AIS A-C: 847,784 (859,873)* C5-C8 AIS A-C: 651,328 (583,324)* |
– | – | 268,993 (252,370)* | |
| 25 | DeVivo et al, 2011 | USA | C1-C4 AIS A-C: 1,156,406* C5-C8 AIS A-C: 835,604* |
T1-S1 AIS A-C: 563,590* | 377,407* | ||
| Ensuing years | |||||||
| 29 | Dryden et al, 2004 | Canada | 14,553 | 49,371 | T1-T12: 14,737 | T1-T12: 22,750 | - |
| L1-L5/CES: 6,263 | |||||||
| 33 | Radhakrishna et al, 2014 | Canada | 17,514 | 86,719 | C8-T6: 10,260 T7-L1: 7,201 |
C8-T6: 53,923 T7-L1: 35,478 |
- |
| L2-S5: 14,861 | |||||||
| 16 | Johnson et al, 1996 | USA | C1-C4 AIS A-C: 251,452 (95,518)* C5-C8 AIS A-C: 131,535 (40,716)* |
AIS A-C: 39,761 (33,512)* | 4,492 (1,763)* (AIS D, E) |
||
| 22 | Webster et al, 2004 | USA | C1-C4 AIS A-C: 197,967 (202,501)* C5-C8 AIS A-C: 194,945 (157,165)* |
– | – | 51,380 (42,313)* | |
| 23 | French et al, 2007 | USA | 29,492 | 37,753 | T1-T12: 22,374 L1-L5: 23,400 |
T1-T12: 27,881 L1-L5: 30,857 |
– |
| 24 | Yu et al, 2008 | USA | Last year: 106,240 (67,700) The year before: 45,490 (15,720) |
Last year: 99,130 (55,160) The year before: 45,490 (17,380) |
|||
| 25 | DeVivo et al, 2011 | USA | C1-C4 AIS A-C: 200,810* C5-C8 AIS A-C: 123,190* |
AIS A-C: 74,658* | 45,840* | ||
Numbers are presented as Mean ± SD when available, numbers inside parenthesis represent Medians instead of mean, e.g. Mean (Median).
* Charges instead of costs, § included both the initial acute care and inpatient rehabilitation.
§ included both the initial acute care and inpatient rehabilitation.
Table 3.
Average Direct Health Care Costs/charges* Per Case.
| Ref. | Study | country | Cost of care. Mean (Median) Mean ± SD (median) costs per case in 2020 USD |
Mean cost / GDP per capita (%) |
|---|---|---|---|---|
| Acute hospital care | ||||
| 36 | New and Jackson, 2010 | Australia | Traumatic: $54,718 (24,254) Nontraumatic: $18,700 (10,066) All: $29,555 (11,300) |
126 43 68 |
| 37 | Vaikuntam et al, 2019 | Australia | $61,187 ± 79,992 (36,706) | 110 |
| 31 | Mac-Thiong, 2012 | Canada | ALL: $28,682 ± 20,475 < 24 h surgical delay: 24,370 ± 16,375 > 24 h surgical delay: 29,727 ± 21,237 |
47 40 49 |
| 32 | Munce, 2013 | Canada | $35,457 ± 45,760 | 73 |
| 35 | Porgo et al, 2019 | Canada | ($9,980) IQR: (6,096-17,633) | – |
| 38 | Li, 2011 | China | $4,860 | 123 |
| 40 | Kawu et al, 2011 | Nigeria | $290 | 13 |
| 42 | Yang et al, 2008 | Taiwan | $2,485 ± 4,661 | 12 |
| 43 | Lessing et, al 2020 | Tanzania | Operative: $757 Nonoperative: $219 |
69 20 |
| 16 | Johnson et al, 1996 | USA | $132,525 (86,480)* | 281 |
| 25 | DeVivo et al, 2011 | USA | $337,400* | 59 |
| 28 | Sikka et al, 2019 | USA | ($92,220)* IQR: 43,390-171,750 | – |
| Rehabilitation | ||||
| 32 | Munce, 2013 | Canada | $106,895 ± 74,088 | 273 |
| 30 | Bradbury et al, 2008 | Canada | $180,464 ± 125,067 | 353 |
| 15 | Chan et al, 1997 | USA | $78,969* | 156 |
| 16 | Johnson et al, 1996 | USA | $105,972 (54,727)* | 224 |
| 19 | McKinley et al, 2001 | USA | Nontraumatic: $38,029* Traumatic: $99,916* |
77 201 |
| 25 | DeVivo et al, 2011 | USA | $190,620* | 333 |
| 26 | Deutsch et al, 2011 | USA | $32,222 ± 21,317 (28,814) | 55 |
| First Year | ||||
| 32 | Munce et al, 2013 | Canada | $119,867 | 248 |
| 16 | Johnson et al, 1996 | USA | $300,875 (216,963)* | 638 |
| 25 | DeVivo et al, 2011 | USA | $634,496* | 1101 |
| Ensuing years | ||||
| 16 | Johnson et al, 1994 | USA | $52,758 (7,066)* | 743 |
| 23 | French et al, 2007 | USA | $28,581 | 49 |
| 24 | Yu et al, 2008 | USA | Last year: 93,543 (59,541) The year before: 37,628 (12,240) |
– |
| 25 | DeVivo et al, 2011 | USA | $96,746* | 169 |
| 27 | Krause et al, 2019 | USA | $17,953* | 29 |
* Charges instead of costs.
Inpatient Rehabilitation
In Canada, the average reported cost of inpatient rehabilitation for all injury categories was reported as $106,890 33 and $180,460. 31 The corresponding charges in the U.S. were reported to range from $19,540 for people with AIS D, E injuries to $433,044 for people with quadriplegia,17,22 and from $32,220 to $190,620 for inpatient charges regardless of neurologic category.26,27
First-Year After Index Injury
Similar to inpatient rehabilitation, studies reporting costs of the first year after injury were confined to Canada and the U.S. In Canada, the mean first-year costs ranged from $32,240 for incomplete paraplegia to $167,640 for complete quadriplegia.30,34 Another study reported a mean total cost of $119,870 for all neurologic injury levels. 33 However, in the U.S., mean first-year total charges ranged from $111,780 for AIS D, E patients to $1,156,410 for AIS A, B, C injuries of C1-C4 level.17,23,26 The mean charges of the first year without considering injury level were $119,870 in Canada 33 and between $300,880 and $634,500 in the U.S.17,26
Ensuing Years
Two studies from Canada and 6 from the U.S. reported the cost of care for the years following the first year. In Canada, average annual costs varied from $6,260 for lumbar lesions to $86,720 for complete cervical SCI.30,34 In the U.S., annual charges varied from $4,490 for AIS D, E injuries to $251,450 for AIS A, B, C injuries of C1-C4 (Table 2).17,23,26 The mean annual charges regardless of the neurologic level of injury varied widely, from $17,950 to $96,750 (Table 3).17,26,28 Using data from the Veterans Health Administration (VA), French et al 24 reported mean annual costs of all outpatient and inpatient care were $28,540 while Yu et al 25 obtained $37,630 for the second year before the end of life and $93,540 for the final year. It should be pointed out that the former study only included the cost of services provided by the VA. Consequently, the cost for attendant care, which was shown to be the single largest long-term cost item for persons with SCI, was not included. Additionally, ventilator-dependent cases were not included in the former study; therefore the average annual costs were possibly underestimated.
Components and Determinants of the Cost of Care
Several studies provided additional information on demographic and clinical factors that were associated with reported acute care costs. Four of these studies were conducted in Australia35,38 and Canada32,33 and one in Taiwan. 42 We summarized statistically significant predictors of higher treatment costs in Table 4. In the developed setting, after adjustment for other factors, a cervical level of the injury, ASIA grade A and B, concomitant injuries, and complication development showed the greatest incremental effect in costs. Both surgical delay (>24 h) and delayed transfer to a specialized SCI center were associated with incremental costs of 6300$ and 6093$, respectively. Other factors that showed significant relation to higher costs were age (continuous and age >70), female sex, and higher injury severity scores. Nevertheless gender,32,38 age groups, 38 and charlston index 33 were not reported to have a significant effect on total costs in some of these analyses. Among studies from LMIC, Tsai et al 42 showed a male sex and medical center compared to metropolitan hospitals as control were associated with higher costs.
Table 4.
Predictors of Higher Treatment Costs.
| Ref. | Variables | Incremental cost in 2020 USD |
|---|---|---|
| Age | ||
| 31 | continuous | 142$ (41-243) |
| 32 | > 70 | 2,532$ (751-4,630) |
| Gender | ||
| 32 | Female | 1,252$ (119-2,243) |
| 41 | Female | −1285.2 |
| 31 | Neurological level cervical | 11,327$ (7,484-15,170) |
| 37 | Charlson Index | 2,979$ (833-5,724) |
| 31 | Injury Severity Score | 582$ (385-780) |
| 31 | ASIA grade | |
| A | 9,865$ (4,851-14,878) | |
| B | 11,764$ (6,538-16,991) | |
| C | 4,419$ (−939-9777) | |
| D | 0 | |
| 32 | Traumatic brain injury | 1,805$ (233-5,778) |
| 37 | Additional injury | |
| one | 6,300 | |
| 2 or more | 27,524 | |
| 34 | Care pathway; | |
| admission to SCI center ≥24 h | 6,093$ (1,370-10,816) | |
| 31 | Surgical delay | |
| Continuous | 17.8$ (6.1-29.3) | |
| > 24 h | 6,300$ (10,460-2,140) | |
| 32 | Complication development | 4,995$ (108-9,881) |
| 34 | 6,518$ (4,525-8,801) | |
| 41 | Accreditation | |
| Medical centers | 3,681.1 | |
| Community hospitals | −312.5 |
* Statistically significant factors associated with an increase/decrease in.
Costs that were identified by a multiple regression analysis.
The most important contributors to health spending in the first year were initial hospitalization (range: 30% to 53%) followed by inpatient rehabilitation (range: 30% to 58%). After inpatient acute care and rehabilitation, inpatient readmission constituted the greatest proportion of total health care costs. Attendant care, followed by re-hospitalization, were the 2 most substantial drivers of recurring total costs after postoperative year one.
Discussion
We systematically reviewed the direct cost of illness for individuals with SCI from countries with different socioeconomic development levels. This review included 30 studies, most of which were conducted in North America. There is a paucity of literature in Europe and LMICs. The current research has considerable variation in methodology, cost descriptions, and study timeframes, providing a wide array of cost of illness estimates. Despite these differences in cost estimates, we found that health care costs for patients with SCI are substantial. Since the currently published data is not available in most countries, any generalizability of the results to a regional or global level can only be limited to states with similar economic status and health care systems. Our results demonstrated that cost figures were broadly higher for the developed countries compared with the rest of the world. Of note, we only included studies that reported direct costs of care in the SCI population.
In a review article on the health economics of the SCI conducted among war veterans, Furlan et al 45 reported that the cost of care varied from $30,770 to $62,563 in 2016 USD, which in general was greater than the health care costs for other chronic diseases. The authors found the ratio of costs of inpatient care to total health care (50.6% to 80.4%) was greater than the ratio of outpatient care costs (13% to 43.5%), and outpatient pharmacy costs (2.1% to 10.3%) to total health care. The most significant determinants of the cost of care were the presence of pressure ulcers, cervical level of injury, period time (i.e. first-year post-injury and end-of-life year), and more severe SCI. Likewise, our results demonstrated severity, level of injury, and development of in-hospital complications were the main origins of costs.
The disparities in reported health care costs between articles included in our review can be partially explained by different study objectives that possibly contributed to variations in study participants and clinical heterogeneity. They can also be attributed to the major methodological differences in cost calculation methods. Research has shown that approaches used for estimating health care costs including per diem, diagnosis-related (case-mix) groups, and activity-based costing (micro-costing) methods particularly in countries with a single-payer health care system such as Australia and Canada, can remarkably under or overestimate real costs in cases with major injuries.46-48 Furthermore, differences in cost items considered in the cost calculation can be another potential driver of disparities in reported figures (Table 1).
The highest health care costs for patients with SCI were found in studies from the US that reported charges instead of actual costs. How hospitals in the U.S. set their prices and how they are paid by different third-party payers or self-paying individuals are covered in layers of complex negotiation and accounting. U.S. hospitals are often paid by several distinct third-party payers, each with a distinct set of rules for payment contracted independently with each insurer. 49 Accordingly, hospitals in the U.S. were paid only around 35% of the total bill charged to a patient and billed charges are generally higher than true costs. DeVivo et al 26 highlighted the wide disparity between estimates of charges and costs. Charges were 3 times greater than estimated costs for acute care and 2 times greater for inpatient rehabilitation and first-year costs. Moreover, medical care expenditures in the U.S. are approximately twice as much as in other high-income countries. Higher prices for workforce, goods, pharmaceuticals, and administrative costs account for the major differences in overall health spending between the U.S. and other high-income countries. 50 Conversely, the lowest health spending was reported in studies from the developing world, likely due to lower prices and treatment intensity resulting in lower resource utilization. Although acute care costs as a percentage of GDP per capita were considerable for all countries, there was a trend toward higher costs in developed countries. This can be partially explained by different care strategies such as a lower rate of surgical treatment and implementing conservative treatment in low-income countries.
The different time spans between studies also contributed to variations in reported health care costs for patients with SCI. Using data from the National Spinal Cord Injury Statistical Center (NSCISC), Fiedler et al reported that yearly charges for acute care increased from $34,072 to $89,615 and total charges increased from $125,176 to $177,415 in 1997 USD from 1973 to 1997. 51 Asemota et al also presented recent evidence showing increasing trends in total charges in older-adults with cervical SCI analyzing The Nationwide Inpatient Sample (NIS) from 2001 to 2010. 52 Since advances in medicine and rehabilitation have improved survival among patients with extreme injuries, 53 health expenditures have increased substantially over the past few decades. Advances in surgical technology and improvement in internal fixation devices have increased the number of surgical procedures involving surgical decompression of the spine and have partially caused increasing costs. 54 This does not include incentives to reduce total care spending and rehabilitation utilization and reimbursement in the U.S. Therefore, it is unjustified to compare health spending in different timeframes. Hospital-associated factors (e.g. level of the trauma center, specified centers, volume, indirect or delayed transfer, and treatment protocols) and major epidemiological and demographic differences in SCI populations between the studies could also be potential sources of difference in healthcare spending.
For the predictors of higher treatment costs, level and severity of the injury and in-hospital complications were major determinants of cost. Urinary-related secondary complications followed by respiratory complications and pressure injuries were the major secondary complications during acute care treatment. 38 Pressure ulcer in individuals with SCI remains a common yet preventable complication. The average monthly cost of pressure ulcer management in a community-dwelling SCI population was $4,745 (2011 Canadian dollars). 55 Hospitalization costs were also related to a surgical delay of >24 h. Furthermore, acute care costs were comparatively less expensive if patients admitted to a specialized SCI center within 24 h from injury. Previous studies have suggested that early decompression of the spinal cord and early inpatient rehabilitation are cost-effective, and are associated with favorable outcomes.56,57 Early recognition, appropriate prehospital care, and timely transfer to an SCI center are essential to receive specialist care and reduce preventable complications. 58
Healthcare costs in the first year post-injury were higher than the following years. The largest proportion of total healthcare costs in the first year post-injury involved initial hospitalization, inpatient rehabilitation, and inpatient readmission. 33 During the following years after the first year, attendant care followed by re-hospitalization was the most substantial driver of recurring total costs. Samsa et al 59 , in a study of the patterns of inpatient admissions among a cohort of veterans with SCI, found that the incidence of re-hospitalization decreased more in years 2 to 5 after injury but more slowly thereafter. Another study of VA patients showed that among the SCI population, one-half of the recurring costs after the first year post-injury were associated with inpatient care. 24 Jaglal et al 60 showed that the main causes of secondary complications after index discharge were musculoskeletal, respiratory, gastrointestinal, and urological disorders. Although the inpatient and attendant service costs are an important part, durable medical equipment, and home modification costs are also major constituents of the total costs during the years following the first postoperative year.
Limitations
Our review had some inherent limitations. Firstly, data was not available in most parts of the world. Secondly, our review showed considerable variability in the costs and cost calculations of SCI cases. There was no unified definition for the cost of care, and literature consisted of different methods of cost calculation. Furthermore, methodological and reporting heterogeneities were common, which complicated the comparison of the results between publications. Moreover, it was not practical to extract the results and conduct a meta-analysis.
Conclusion
Healthcare costs associated with SCI have broad heterogeneity among different countries due to the definition of cost of care, different time horizons, level and severity of the injury, and health system structure. Therefore, generalizing these health care costs to a regional or global level requires careful consideration. However, the life-long economic cost of SCI is extremely high. Since inconsistencies in the method of conducting studies and limited reporting detail have complicated interpretation and limited studies usefulness, future investigations should follow standard guides for methodology. Published standards on conducting cost of illness studies are available to encourage uniformity.14,61,62 A methodology guide designed particularly for SCI studies based on these publications could make the best use of a cost of illness studies for SCI. Further studies on the cost of care for individuals with SCI are needed to assist patients, healthcare providers, administrators, and policymakers in making better decisions concerning resource allocation based on the anticipated costs. Moreover, cost-effectiveness studies are essential to identify the efficacy of different interventions and care pathways when planning for optimal care for SCI cases.
Supplemental Material
Supplemental Material, sj-doc-1-gsj-10.1177_21925682211031190 for Direct Cost of Illness for Spinal Cord Injury: A Systematic Review by Hamid Malekzadeh, Mahdi Golpayegani, Zahra Ghodsi, Mohsen Sadeghi-Naini, Mohammadhossein Asgardoon, Vali Baigi, Alexander R. Vaccaro and Vafa Rahimi-Movaghar in Global Spine Journal
Supplemental Material, sj-doc-2-gsj-10.1177_21925682211031190 for Direct Cost of Illness for Spinal Cord Injury: A Systematic Review by Hamid Malekzadeh, Mahdi Golpayegani, Zahra Ghodsi, Mohsen Sadeghi-Naini, Mohammadhossein Asgardoon, Vali Baigi, Alexander R. Vaccaro and Vafa Rahimi-Movaghar in Global Spine Journal
Acknowledgments
The authors would like to thank Dr. Farnam Mohebbi, MD for her cooperation in conducting the search strategy. We also thank Dr. Kasra Molooghi, MD for his help in editing the manuscript.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: None declared except Alexander R. Vaccaro—receipt of royalty payments: Medtronics, Stryker Spine, Globus, Aesculap, Thieme, Jaypee, Elseviere, Taylor Francis/Hodder and Stoughton, SpineWave, Atlas Spine; stock/stock option ownership interests: Replication Medica, Globus, Paradigm Spine, Stout Medical, Progressive Spinal Technologies, Advanced Spinal Intellectual Properties, Spine Medica, Computational Biodynamics, Spinology, Flagship Surgical, Cytonics, Bonovo Orthopaedics, Electrocore, Insight Therapeutics, FlowPharma, Rothman Institute and Related Properties, Innovative Surgical Design, Orthobullets, Vertiflex, Avaz Surgical, Dimension Orthotics, LLC, Nuvasive Parvizi Surgical Innovation, Franklin Bioscience, Deep Health; member in good standing/independent contractor: AO Spine, expert testimony.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by Sina Trauma and Surgery Research Center, Tehran University of Medical Sciences (grant number is 96-01-38-34334).
ORCID iD: Hamid Malekzadeh, MD  https://orcid.org/0000-0003-1309-0757
https://orcid.org/0000-0003-1309-0757
Vali Baigi, PhD  https://orcid.org/0000-0003-1882-7340
https://orcid.org/0000-0003-1882-7340
Alexander R. Vaccaro, MD, PhD  https://orcid.org/0000-0002-8073-0796
https://orcid.org/0000-0002-8073-0796
Vafa Rahimi-Movaghar, MD  https://orcid.org/0000-0001-7347-8767
https://orcid.org/0000-0001-7347-8767
Supplemental Material: Supplemental material for this article is available online.
References
- 1.GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(1):56–87. doi:10.1016/s1474-4422(18)30415-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hall OT, McGrath RP, Peterson MD, et al. The burden of traumatic spinal cord injury in the United States: disability-adjusted life years. Arch Phys Med Rehabil. 2019;100(1):95–100. doi:10.1016/j.apmr.2018.08.179 [DOI] [PubMed] [Google Scholar]
- 3.Economics A. The economic cost of spinal cord injury and traumatic brain injury in Australia. Report by Access Economics Pty Limited for The Victorian Neurotrauma Initiative. 2009. January 28, 2015. [Google Scholar]
- 4.Polinder S, Meerding WJ, Mulder S, Petridou E, van Beeck E; EUROCOST Reference Group. Assessing the burden of injury in six European countries. Bull World Health Organ. 2007;85(1):27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahabaleshwarkar R, Khanna R. National inpatient burden associated with spinal cord injuries in the United States. Conference Abstract. Value Health. 2012;15(4):A80. doi:10.1016/j.jval.2012.03.440 [DOI] [PubMed] [Google Scholar]
- 6.Hoffman J. Linking Economic Research and Policy Making: The Role of AERC. African Economic Research Consortium; 1995. [Google Scholar]
- 7.Lo J, Chan L, Flynn S. A systematic review of the incidence, prevalence, costs, and activity/work limitations of amputation, osteoarthritis, rheumatoid arthritis, back pain, multiple sclerosis, spinal cord injury, stroke, and traumatic brain injury in the United States: a 2019 update. Arch Phys Med Rehabil. 2021;102(1):115–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi:10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boccuzzi SJ. Indirect health care costs. In: Weintraub WS, ed Cardiovascular health care economics. Springer; 2003:63–79. [Google Scholar]
- 10.Board of Governors of the Federal Reserve System. Foreign Exchange Rates—G.5A. Published 4, 2021. Updated February 12, 2021. Accessed February 2021. https://www.federalreserve.gov/releases/g5a/default.htm
- 11.U.S. Bureau of Labor Statistics. CPI Inflation Calculator. Accessed February 2021. https://www.bls.gov/data/inflation_calculator.htm
- 12.The World Bank Group. GDP per capita. Published 2021. Accessed 2021. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD
- 13.Public Health Wales Observatory Evidence Service. Questions to assist with the critical appraisal of a cost of illness/ risk factor analysis. Published December 2014. Accessed February 2021. http://www2.nphs.wales.nhs.uk:8080/PubHObservatoryProjDocs.nsf/($All)/3F7F34D64C70747180257DBD00411C39/$File/Cost%20of%20illness%20studies%20critical%20appraisal%20checklist.docx?OpenElement
- 14.Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011;29(8):653–671. doi:10.2165/11588380-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15.Price C, Makintubee S, Herndon W, Istre GR. Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988-1990. Am J Epidemiol. 1994;139(1):37–47. doi:10.1093/oxfordjournals.aje.a116933 [DOI] [PubMed] [Google Scholar]
- 16.Chan L, Koepsell TD, Deyo RA, et al. The effect of Medicare’s payment system for rehabilitation hospitals on length of stay, charges, and total payments. New Engl J Med. 1997;337(14):978–985. doi:10.1056/nejm199710023371406 [DOI] [PubMed] [Google Scholar]
- 17.Johnson RL, Brooks CA, Whiteneck GG. Cost of traumatic spinal cord injury in a population-based registry. Spinal Cord. 1996;34(8):470–480. doi:10.1038/sc.1996.81 [DOI] [PubMed] [Google Scholar]
- 18.Cifu DX, Seel RT, Kreutzer JS, Marwitz J, McKinley WO, Wisor D.Age, outcome, and rehabilitation costs after tetraplegia spinal cord injury. NeuroRehabilitation. 1999;12(3):177–185. doi:10.3233/nre-1999-12304 [Google Scholar]
- 19.Cifu DX, Huang ME, Kolakowsky-Hayner SA, Seel RT. Age, outcome, and rehabilitation costs after paraplegia caused by traumatic injury of the thoracic spinal cord, conus medullaris, and cauda equina. J Neurotrauma. 1999;16(9):805–815. doi:10.1089/neu.1999.16.805 [DOI] [PubMed] [Google Scholar]
- 20.McKinley WO, Seel RT, Gadi RK, Tewksbury MA. Nontraumatic vs. traumatic spinal cord injury: a rehabilitation outcome comparison. Am J Phys Med Rehabil. 2001;80(9):693–699. [DOI] [PubMed] [Google Scholar]
- 21.Seel RT, Huang ME, Cifu DX, Kolakowsky-Hayner SA, McKinley WO. Age-related differences in length of stays, hospitalization costs, and outcomes for an injury-matched sample of adults with paraplegia. J Spinal Cord Med. 2001;24(4):241–250. doi:10.1080/10790268.2001.11753581 [DOI] [PubMed] [Google Scholar]
- 22.Smith W, Simmonds JO, Alam ZS, Grant RE. Spinal cord injury caused by gunshot wounds: the cost of rehabilitation. Clin Orthop Relat Res. 2003;(408):145–151. doi:10.1097/00003086-200303000-00017 [DOI] [PubMed] [Google Scholar]
- 23.Webster B, Giunti G, Young A, Pransky G, Nesathurai S. Work-related tetraplegia: cause of injury and annual medical costs. Spinal Cord. 2004;42(4):240–247. doi:10.1038/sj.sc.3101526 [DOI] [PubMed] [Google Scholar]
- 24.French DD, Campbell RR, Sabharwal S, Nelson AL, Palacios PA, Gavin-Dreschnack D. Health care costs for patients with chronic spinal cord injury in the Veterans health administration. J Spinal Cord Med. 2007;30(5):477–481. doi:10.1080/10790268.2007.11754581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu W, Smith B, Kim S, Chow A, Weaver FM. Major medical conditions and VA healthcare costs near end of life for veterans with spinal cord injuries and disorders. J Rehabil Res Dev. 2008;45(6):831–839. doi:10.1682/jrrd.2006.08.0102 [DOI] [PubMed] [Google Scholar]
- 26.DeVivo MJ, Chen Y, Mennemeyer ST, Deutsch A.Costs of care following spinal cord injury. Topic Spinal Cord Injury Rehabil. 2011;16(4):1–9. doi:10.1310/sci1604-1 [Google Scholar]
- 27.Deutsch A, Almagor O, Rowles DM, Pucci D, Chen D. Characteristics and outcomes of aged Medicare beneficiaries with a traumatic spinal cord injury: 2002-2005. Topics Spinal Cord Injury Rehabil. 2011;16(4):17–26. doi:10.1310/sci1604-17 [Google Scholar]
- 28.Krause JS, Murday D, Corley EH, DiPiro ND. Concentration of costs among high utilizers of health care services over the first 10 years after spinal cord injury rehabilitation: a population-based study. Arch Phys Med Rehabil. 2019;100(5):938–944. doi:10.1016/j.apmr.2018.10.020 [DOI] [PubMed] [Google Scholar]
- 29.Sikka S, Callender L, Driver S, et al. Healthcare utilization following spinal cord injury: objective findings from a regional hospital registry. J Spinal Cord Med. 2019;42(2):194–200. doi:10.1080/10790268.2018.1505330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dryden DM, Saunders LD, Jacobs P, et al. Direct health care costs after traumatic spinal cord injury. J Trauma. 2005;59(2):464–467. doi:10.1097/01.ta.0000174732.90517.df [DOI] [PubMed] [Google Scholar]
- 31.Bradbury CL, Wodchis WP, Mikulis DJ, et al. Traumatic brain injury in patients with traumatic spinal cord injury: clinical and economic consequences. Arch Phys Med Rehabil. 2008;89(12 suppl):S77–S84. doi:10.1016/j.apmr.2008.07.008 [DOI] [PubMed] [Google Scholar]
- 32.Mac-Thiong JM, Feldman DE, Thompson C, Bourassa-Moreau E, Parent S. Does timing of surgery affect hospitalization costs and length of stay for acute care following a traumatic spinal cord injury? J Neurotrauma. 2012;29(18):2816–2822. doi:10.1089/neu.2012.2503 [DOI] [PubMed] [Google Scholar]
- 33.Munce SE, Wodchis WP, Guilcher SJ, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51(1):64–69. doi:10.1038/sc.2012.81 [DOI] [PubMed] [Google Scholar]
- 34.Radhakrishna M, Makriyianni I, Marcoux J, Zhang X. Effects of injury level and severity on direct costs of care for acute spinal cord injury. Int J Rehabil Res. 2014;37(4):349–353. doi:10.1097/mrr.0000000000000081 [DOI] [PubMed] [Google Scholar]
- 35.Richard-Denis A, Ehrmann Feldman D, Thompson C, Bourassa-Moreau É, Mac-Thiong JM. Costs and length of stay for the acute care of patients with motor-complete spinal cord injury following cervical trauma: the impact of early transfer to specialized acute SCI center. Am J Phys Med Rehabil. 2017;96(7):449–456. doi:10.1097/phm.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 36.Porgo TV, Moore L, Truchon C, et al. Patient-level resource use for injury admissions in Canada: a multicentre retrospective cohort study. Injury. 2019;50(6):1192–1201. doi:10.1016/j.injury.2019.03.038 [DOI] [PubMed] [Google Scholar]
- 37.New PW, Jackson T.The costs and adverse events associated with hospitalization of patients with spinal cord injury in Victoria, Australia. Spine (Phila Pa 1976). 2010;35(7):796–802. doi:10.1097/BRS.0b013e3181be76f5 [DOI] [PubMed] [Google Scholar]
- 38.Vaikuntam BP, Middleton JW, McElduff P, et al. Identifying predictors of higher acute care costs for patients with traumatic spinal cord injury and modeling acute care pathway redesign: a record linkage study. Spine (Phila Pa 1976). 2019;44(16):E974–E983. doi:10.1097/brs.0000000000003021 [DOI] [PubMed] [Google Scholar]
- 39.Li J, Liu G, Zheng Y, et al. The epidemiological survey of acute traumatic spinal cord injury (ATSCI) of 2002 in Beijing municipality. Spinal Cord. 2011;49(7):777–782. doi:10.1038/sc.2011.8 [DOI] [PubMed] [Google Scholar]
- 40.Jiménez-Avila JM, Alvarez-Garnier JC, Bitar-Alatorre WE. Direct cost of complete cervical spinal cord injury [in Spanish]. Acta Ortop Mex. 2012;26(1):10–14. [PubMed] [Google Scholar]
- 41.Kawu AA, Olawepo A, Salami AO, Kuranga SA, Abdulhameed S, Esenwah VC. A cost analysis of conservative management of spinal cord-injured patients in Nigeria. Spinal Cord. 2011;49(11):1134–1137. doi:10.1038/sc.2011.69 [DOI] [PubMed] [Google Scholar]
- 42.Tsai JC, Chang WY, Hsueh IH, et al. In-patient medical resource utilization for high-level cervical spinal cord injury without bone fracture in Taiwan. Spinal Cord. 2005;43(7):426–433. doi:10.1038/sj.sc.3101733 [DOI] [PubMed] [Google Scholar]
- 43.Yang NP, Deng CY, Lee YH, Lin CH, Kao CH, Chou P. The incidence and characterisation of hospitalised acute spinal trauma in Taiwan—a population-based study. Injury. 2008;39(4):443–450. doi:10.1016/j.injury.2007.12.007 [DOI] [PubMed] [Google Scholar]
- 44.Lessing NL, Zuckerman SL, Lazaro A, et al. Cost-effectiveness of operating on traumatic spinal injuries in low-middle income countries: a preliminary report from a major East African referral center. Global Spine J. 2020;2192568220944888. doi:10.1177/2192568220944888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Furlan JC, Gulasingam S, Craven BC. The Health economics of the spinal cord injury or disease among veterans of war: a systematic review. J Spinal Cord Med. 2017;40(6):649–664. doi:10.1080/10790268.2017.1368267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The Canadian Agency for Drugs and Technologies in Health. Guidance Document for the Costing of Health Care Resources in the Canadian Setting. 2nd ed. Canadian Agency for Drugs and Technologies in Health; 2016. [Google Scholar]
- 47.Curtis K, Mitchell R, Dickson C, Black D, Lam M.Do AR-DRGs adequately describe the trauma patient episode in New South Wales, Australia? Health Inf Manag. 2011;40(1):7–13. doi:10.1177/183335831104000102 [DOI] [PubMed] [Google Scholar]
- 48.Taheri PA, Butz DA, Greenfield LJ. Paying a premium: how patient complexity affects costs and profit margins. Ann Surg. 1999;229(6):807–811; discussion 811-814. doi:10.1097/00000658-199906000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinhardt UE. The pricing of U.S. hospital services: chaos behind a veil of secrecy. Health Aff (Millwood). 2006;25(1):57–69. doi:10.1377/hlthaff.25.1.57 [DOI] [PubMed] [Google Scholar]
- 50.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319(10):1024–1039. doi:10.1001/jama.2018.1150 [DOI] [PubMed] [Google Scholar]
- 51.Fiedler IG, Laud PW, Maiman DJ, Apple DF. Economics of managed care in spinal cord injury. Arch Phys Med Rehabil. 1999;80(11):1441–1449. doi:10.1016/s0003-9993(99)90256-3 [DOI] [PubMed] [Google Scholar]
- 52.Asemota AO, Ahmed AK, Purvis TE, Passias PG, Goodwin CR, Sciubba DM. Analysis of cervical spine injuries in elderly patients from 2001 to 2010 using a nationwide database: increasing incidence, overall mortality, and inpatient hospital charges. World Neurosurg. 2018;120:e114–e130. doi:10.1016/j.wneu.2018.07.228 [DOI] [PubMed] [Google Scholar]
- 53.Vaidyanathan S, Soni BM, Gopalan L, et al. A review of the readmissions of patients with tetraplegia to the regional spinal injuries centre, Southport, United Kingdom, between January 1994 and December 1995. Spinal Cord. 1998;36(12):838–846. doi:10.1038/sj.sc.3100629 [DOI] [PubMed] [Google Scholar]
- 54.Waters RL, Meyer PR, Jr, Adkins RH, Felton D. Emergency, acute, and surgical management of spine trauma. Arch Phys Med Rehabil. 1999;80(11):1383–1390. doi:10.1016/S0003-9993(99)90248-4 [DOI] [PubMed] [Google Scholar]
- 55.Chan BC, Nanwa N, Mittmann N, Bryant D, Coyte PC, Houghton PE. The average cost of pressure ulcer management in a community dwelling spinal cord injury population. Int Wound J. 2013;10(4):431–440. doi:10.1111/j.1742-481X.2012.01002.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Furlan JC, Craven BC, Massicotte EM, Fehlings MG. Early versus delayed surgical decompression of spinal cord after traumatic cervical spinal cord injury: a cost-utility analysis. World Neurosurg. 2016;88:166–174. doi:10.1016/j.wneu.2015.12.072 [DOI] [PubMed] [Google Scholar]
- 57.Scivoletto G, Morganti B, Molinari M. Early versus delayed inpatient spinal cord injury rehabilitation: an Italian study. Arch Phys Med Rehabil. 2005;86(3):512–516. doi:10.1016/j.apmr.2004.05.021 [DOI] [PubMed] [Google Scholar]
- 58.Middleton PM, Davies SR, Anand S, Reinten-Reynolds T, Marial O, Middleton JW. The pre-hospital epidemiology and management of spinal cord injuries in New South Wales: 2004-2008. Injury. 2012;43(4):480–485. doi:10.1016/j.injury.2011.12.010 [DOI] [PubMed] [Google Scholar]
- 59.Samsa GP, Landsman PB, Hamilton B. Inpatient hospital utilization among veterans with traumatic spinal cord injury. Arch Phys Med Rehabil. 1996;77(10):1037–1043. doi:10.1016/s0003-9993(96)90065-9 [DOI] [PubMed] [Google Scholar]
- 60.Jaglal SB, Munce SE, Guilcher SJ, et al. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord. 2009;47(8):604–609. doi:10.1038/sc.2009.9 [DOI] [PubMed] [Google Scholar]
- 61.Hodgson TA, Meiners MR. Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem Fund Q Health Soc. 1982;60(3):429–462. [PubMed] [Google Scholar]
- 62.Rice DP, Hodgson TA, Kopstein AN. The economic costs of illness: a replication and update. Health Care Finan Rev. 1985;7(1):61–80. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-doc-1-gsj-10.1177_21925682211031190 for Direct Cost of Illness for Spinal Cord Injury: A Systematic Review by Hamid Malekzadeh, Mahdi Golpayegani, Zahra Ghodsi, Mohsen Sadeghi-Naini, Mohammadhossein Asgardoon, Vali Baigi, Alexander R. Vaccaro and Vafa Rahimi-Movaghar in Global Spine Journal
Supplemental Material, sj-doc-2-gsj-10.1177_21925682211031190 for Direct Cost of Illness for Spinal Cord Injury: A Systematic Review by Hamid Malekzadeh, Mahdi Golpayegani, Zahra Ghodsi, Mohsen Sadeghi-Naini, Mohammadhossein Asgardoon, Vali Baigi, Alexander R. Vaccaro and Vafa Rahimi-Movaghar in Global Spine Journal