Abstract
Study Design:
Retrospective Study.
Objectives:
Sacroiliac buttress screws (SBS) and S2 alar iliac screws (SAI) are used as distal screws in cases with long fusion to the pelvis. Distal fixation ends, whether exceeding the sacroiliac joint (SIJ), may affect postoperative degenerative changes in the SIJ. The aim of this study was to investigate SIJ degeneration after lumbosacral and lumbopelvic fixation, using SBS and SAI in degenerative spine diseases, respectively.
Methods:
This study included 70 patients aged ≥50 years with lumbosacral fusion (>3 levels). They were divided into 2 groups (SBS 20 and SAI 50 cases) based on the type of distal screws. Radiographical and clinical data were reviewed with a minimum 2-year follow-up. Radiographical SIJ degeneration was analyzed using computed tomography; clinical outcomes were evaluated using visual analog scale (VAS) and Japanese Orthopaedic Association Back Pain Questionnaire (JOABPEQ).
Results:
No significant differences were observed in patients’ preoperative characteristics between the 2 groups. The incidence of SIJ degeneration, including osteophyte formation (30.0% and 8.0%, p = 0.03), intraarticular air (75.0% and 16.0%, p < 0.001), and subchondral cyst (20.0% and 2.0%. p = 0.02) in SBS and SAI groups, respectively, at the follow-up, was significantly higher in the SBS group. Although SIJ degenerative changes were significantly different between the SBS and SAI groups, there was no significant difference in VAS and JOABPEQ scores between the groups at 2 years post-surgery.
Conclusions:
Lumbosacral fusion can cause SIJ degeneration, which is more frequent when SBS are used in fixation to the sacrum.
Keywords: lumbosacral fusion, S2 alar iliac screws, sacroiliac buttress screws, adjacent segment disease, sacroiliac joint
Introduction
Pseudarthrosis and implant failures at the lumbosacral junction have been a concern. Anatomical complex biomechanics, due to dynamic stress, increase the risk of failures in this area, thereby necessitating rigid distal end fixation for the maintenance of proper spinal balance. 1 Solitary fixation, using S1 pedicle screws, is often associated with insufficient outcomes in long adult fusions. 2 Therefore, additional sacral and pelvic fixation techniques to spinal instrumentations have been developed to reduce complications and promote fusion at the lumbosacral junction, 3 including intrasacral rods and screws,4,5 S2 pedicle screws, 6 iliac screws,2,7 and S2 alar iliac screws (SAI).8,9 Although various surgical techniques and instrumentations have been reported, they can be grouped into 2 types, i.e. “fixation to the sacrum” or “fixation across the sacroiliac joint (SIJ) to the iliac bone.”
The intrasacral rod, Jackson technique, is one of the strong distal anchors used for “fixation to the sacrum.” In this technique, rods are inserted into the lateral sacral mass and attached to segmental pedicle screws. 4 These rods are stabilized by the subchondral bone of the sacrum at the SIJ with iliac buttress coverage. However, using intrasacral rods is technically demanding while connecting proximal screws in the lumbar spine. Therefore, Fukuda et al reported sacroiliac buttress screws (SBS) as an alternative for these intrasacral rods. 5 In their technique, polyaxial screws were inserted into the sacrum, instead of the rods, and the polyaxial screw head provides an easier assembly of the rods and screws than intrasacral rods.
Iliac screws and SAI are also useful instruments for distal anchoring, which are used in the “fixation across the SIJ to the iliac bone.”2,7-10 Extending the instrumentation to the iliac bone provides a strong distal foundation to resist the substantial cantilever forces on the sacrum. Several potential advantages of SAI have been reported, such as lower rates of implant failure, screw head prominence, postoperative pain, and wound dehiscence, 11 and they are often used in long spinal instrumentation and fusion.
Although these additional sacral and pelvic fixations provide better stabilization, SIJ arthritis and pain may occur after surgery.12-14 Adjacent segment degeneration could occur in the SIJ in cases with fixation to the sacrum, while SIJ degeneration might be accelerated by partial destruction of the articular cartilage in the SIJ due to SAI insertion. Although the rate of SIJ-related pain after lumbosacral fixation has been reported at 4.2%–31.7%,13,14 the degree of radiographical degenerative changes remains unclear. Moreover, there are few reports comparing the degree of radiographical degenerative changes in the SIJ between “fixation to the sacrum” and “fixation across the SIJ to the iliac bone.”
The aims of this study were to investigate the radiographical degenerative changes in the SIJ and the clinical symptoms after lumbosacral fixation and to compare them between cases with SBS and SAI with a minimum 2-year follow-up period.
Materials and Methods
We retrospectively reviewed prospectively collected data from a single center between 2010 and 2016. Written informed consent was obtained from all patients. Data were analyzed after obtaining approval from the Ethics Committee. Ethical approval was obtained from the Konan Kosei Hospital institutional ethics committees (IRB approved no., 25-022[0174]). We included patients with lumbosacral fixation using SBS or SAI for degenerative spine diseases. Enrollment criteria were age >50 years, fusion level >3, and a minimum follow-up of >2 years. We excluded cases with syndromic scoliosis, other neurological disorders, or mental disorders because of the difficulty in obtaining the changes in clinical symptoms. Finally, 70 cases (SBS: 20 and SAI: 50 cases) were included. SAI were used at our institution beginning in 2013. We included patients for whom SBS were used between 2010 and 2012 and for whom SAI were used between 2013 and 2016. To minimize selection bias, we selected the surgical instrumentation techniques depending on the date of surgery.
Radiographical Assessment of SIJ
According to the definition described by Ha et al, 15 SIJ degeneration was evaluated by computed tomography (CT) 1 and 2 years after surgery. A 64-line multislice CT (Light Speed VCT; GE Healthcare Bio-Sciences, Piscataway, NJ, USA) was used for the CT examination. The diagnosis of SIJ degeneration was based on the presence of one or more of the following CT findings: increased or new formation of osteophyte, intraarticular air, subchondral cyst, and intraarticular bone fragment.
Clinical Assessments
We evaluated the results of the Japanese Orthopaedic Association Back Pain Evaluation Questionnaire (JOABPEQ) preoperatively and at 2 years post-surgery. The JOABPEQ includes 25 questions covering 5 domains: pain-related disorders, lumbar spine dysfunction, gait disturbance, social life dysfunction, and psychological disorders.16,17 The scores for each domain were calculated according to official guidelines, ranging from 0 to 100 points, with a higher score indicating better health status. The JOABPEQ also incorporates the visual analog scale (VAS) scores for low back pain, pain in the buttocks and lower limbs, and numbness of the buttocks and lower limbs.
Statistical Analysis
Each variable was reported as mean ± standard deviation. Comparisons between the 2 groups were performed using the Mann–Whitney U test or Fisher’s exact test. To analyze the risk factors of SIJ degeneration, we performed stepwise logistic regression. A p value less than 0.05 was considered statistically significant. All analyses were conducted using SPSS version 26 (SPSS, Chicago, IL, USA).
Results
There were no significant differences in the patients’ preoperative characteristics between the 2 groups in terms of age (69.5 ± 5.5 and 73.2 ± 7.3 years), sex (male/female: 13/7 and 35/15), body mass index: BMI (23.0 ± 2.6 and 24.1 ± 3.8), presence of diabetes mellitus (25.0% and 28.0%), smoking history (15.0% and 26.0%), and number of fusion segments (6.2 ± 2.9 and 7.5 ± 3.3 levels) as shown in Table 1. Preoperative SIJ degeneration was found in terms of osteophyte formation (80.0% and 82.0%, p = 1.00), intraarticular air (55.0% and 72.0%, p = 0.26), subchondral cyst (15.0% and 12.0%, p = 0.71), and intraarticular bone fragment (0% and 0%, p = 1.00) in the SBS and SAI groups, respectively, which was not significantly different (Table 1).
Table 1.
Patients’ Baseline Data.
| SBS | SAI | p | |
|---|---|---|---|
| Number of cases | 20 | 50 | |
| Age (years old) | 69.5 ± 5.5 | 73.2 ± 7.3 | 0.71 |
| Sex (male/ female) | 13/7 | 35/15 | 0.78 |
| BMI | 23.0 ± 2.6 | 24.1 ± 3.8 | 0.23 |
| DM | 25.0% | 28.0% | 1.00 |
| Smoking history | 15.0% | 26.0% | 0.53 |
| Number of fusion segments | 6.2 ± 2.9 | 7.5 ± 3.3 | 0.80 |
| Preoperative radiographical findings | |||
| Osteophyte | 80.0% | 82.0% | 1.00 |
| Intraarticular air | 55.0% | 72.0% | 0.26 |
| Subchondral cyst | 15.0% | 12.0% | 0.71 |
| Intraarticular bone fragment | 0 | 0 | 1.00 |
SBS: sacroiliac buttress screws, SAI: S2 alar iliac screw, BMI: body mass index, DM: diabetes mellitus, statistical analysis: Mann–Whitney U test and Fisher’s exact test
Postoperative increases in, or new formation of, these degenerative changes were detected after 1 and 2 years post-surgery compared with preoperative findings (Figures 1 and 2). The rate of postoperative increases or new formation of intraarticular air was significantly higher in the SBS group than in the SAI group (50.0% and 20.0%, p = 0.04; Table 2) at 1 year post-surgery, although there were no significant differences in osteophyte formation, subchondral cyst, and intraarticular bone fragment (Table 2). Most of these degenerative changes progressed until 2 years post-surgery. Postoperative increases or new formations of osteophyte formation (30.0% and 8.0%, p = 0.03), intraarticular air (75.0% and 16.0%, p < 0.001), and subchondral cyst (20.0% and 2.0%, p = 0.02) were significantly higher in the SBS group, but there was no difference in intraarticular bone fragment (5.0% and 0%, p = 0.29) (Table 2).
Figure 1.
A representative case with postoperative sacroiliac joint (SIJ) degeneration after using sacroiliac buttress screws (SBS). Preoperative X-rays showing scoliosis (Cobb angle: 27°) (A), anterior-posterior combined fusion from T10 to sacrum was performed by using SBS (B), and postoperative CT at 2 years showing a subchondral cyst (white arrow) (C).
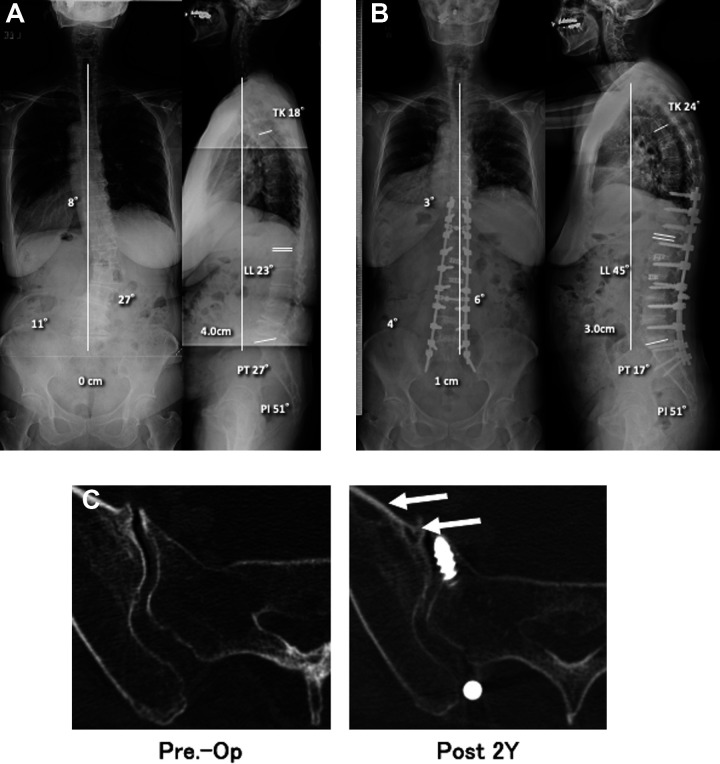
Figure 2.
A representative case with postoperative sacroiliac joint (SIJ) degeneration after using S2 alar iliac screws (SAI). Preoperative X-rays showing scoliosis (Cobb angle: 31°) (A), anterior-posterior combined fusion from T10 to pelvis was performed by using SAI (B), and postoperative CT at 2 years showing a subchondral cyst (white arrow) (C).
Table 2.
Postoperative Increased or New Formation of Osteophyte, Intraarticular Bone Fragment, Intraarticular Air, and Subchondral Cyst Compared With Preoperative Findings.
| SBS | SAI | p | |
|---|---|---|---|
| 1-year post surgery | |||
| Osteophyte | 5.0% | 0% | 0.29 |
| Intraarticular air | 50.0% | 22.0% | 0.04 |
| Subchondral cyst | 5.0% | 2.0% | 0.49 |
| Intraarticular bone fragment | 0% | 0% | 1.00 |
| 2-year post-surgery | |||
| Osteophyte | 30.0% | 8.0% | 0.03 |
| Intraarticular air | 75.0% | 16.0% | <0.001 |
| Subchondral cyst | 20.0% | 2.0% | 0.02 |
| Intraarticular bone fragment | 5.0% | 0% | 0.29 |
SBS: sacroiliac buttress screws, SAI: S2 alar iliac screw, statistical analysis: Fisher’s exact test
Patients that exhibited any SIJ degenerative changes, including the formation of osteophyte, subchondral cyst, or intraarticular bone fragment, were diagnosed with SIJ degeneration. A total of 14 cases had SIJ degeneration (20.0%). There were no significant differences in age (70.6 ± 7.0 and 72.6 ± 7.0, p = 0.35), male sex (21.4% and 33.9%, p = 0.37), fixation level number (5.6 ± 2.8 and 7.5 ± 3.2, p = 0.06), or smoking (14.3% and 25.0%, p = 0.39) in cases with and without SIJ degeneration, respectively; however, SBS was significantly more utilized (9/20 and 5/50 cases with SBS and SAI respectively, p = 0.001) in cases with SIJ degeneration. Logistic regression analysis showed that SBS was the only significant factor associated with SIJ degeneration (OR 7.36, 95% CI: 2.05-26.39, p = 0.002).
Regarding the clinical symptoms, assessed using JOABPEQ, there was no preoperative significant difference in all 5 domains of the JOABPEQ and the 3 areas of VAS (Table 3). Significant clinical improvements were achieved in both groups in all domains and all VAS assessments at 2 years post-surgery. Although degenerative changes in the SIJ were significantly different between the SBS and SAI groups, there was no significant difference in all 5 domains of the JOABPEQ and the 3 areas of VAS between the 2 groups at 2 years post-surgery (Table 3).
Table 3.
Preoperative and Postoperative JOABPEQ.
| SBS | SAI | p | |
|---|---|---|---|
| Preoperative | |||
| Low back pain domain | 27.7 ± 25.4 | 27.2 ± 25.4 | 0.82 |
| Lumbar function domain | 30.6 ± 29.2 | 40.9 ± 23.5 | 0.13 |
| Walking ability domain | 22.9 ± 25.5 | 23.1 ± 23.2 | 0.86 |
| Social life function domain | 32.7 ± 23.3 | 28.3 ± 19.4 | 0.42 |
| Mental health domain | 32.4 ± 17.6 | 33.8 ± 20.8 | 0.89 |
| VAS: Low back pain | 64.7 ± 32.6 | 70.0 ± 28.0 | 0.63 |
| VAS: pain in buttocks and lower limbs | 69.1 ± 22.5 | 66.7 ± 29.6 | 0.84 |
| VAS: numbness in buttocks and lower limbs | 62.5 ± 30.2 | 64.9 ± 33.0 | 0.62 |
| 2-year post surgery | |||
| Low back pain domain | 64.9 ± 34.0 | 48.3 ± 38.1 | 0.12 |
| Lumbar function domain | 38.4 ± 27.6 | 31.1 ± 26.2 | 0.37 |
| Walking ability domain | 40.4 ± 21.7 | 30.6 ± 25.5 | 0.10 |
| Social life function domain | 43.8 ± 20.9 | 40.2 ± 22.9 | 0.41 |
| Mental health domain | 45.9 ± 14.0 | 41.0 ± 19.1 | 0.19 |
| VAS: Low back pain | 31.4 ± 21.6 | 40.3 ± 30.7 | 0.35 |
| VAS: pain in buttocks and lower limbs | 34.4 ± 29.6 | 38.4 ± 33.8 | 0.71 |
| VAS: numbness in buttocks and lower limbs | 55.1 ± 32.5 | 41.8 ± 31.6 | 0.17 |
JOABPEQ: Japanese Orthopaedic Association Back Pain Evaluation Questionnaire, SBS: sacroiliac buttress screws, S2 alar iliac screw: SAI, VAS: visual analog scale, statistical analysis: Mann–Whitney U test
Discussion
This study showed that degenerative changes in the SIJ, occurring after lumbosacral fixation, were significantly more frequent with SBS usage than SAI usage in terms of postoperative increases or new formations of osteophyte formation, intraarticular air, and subchondral cyst. Although there was no significant difference in the clinical symptoms assessed by the JOABPEQ at a short-term follow-up of 2 years post-surgery, lumbosacral fixation to the sacrum accelerated the degenerative changes in the SIJ, which might be a cause of long-term SIJ-related pain after surgery.
Although lumbosacral fixation with long spinal instrumentation is performed in spinal deformity and revision surgery, this presents a challenge due to the frequent mechanical complications and pseudarthrosis, despite additional sacral and pelvic fixations to spinal instrumentations.8,18,19 Furthermore, SIJ arthrosis and the related pain after surgery have been underestimated, but it is a clinically important issue. Adjacent segment degeneration is a well-known sequela after spinal fusion surgery, 20 and similar biomechanical responses could be a cause of SIJ arthrosis and pain after surgery. Baria et al conducted a human cadaveric study to analyze the effects of lower lumbar arthrodesis and sacroiliac screws on SIJ biomechanics. 21 They found that flexion-extension loading on the SIJ increased significantly after 1- or 2-level lumbosacral spine arthrodesis, and this overloading could accelerate SIJ degeneration as in adjacent segment degeneration of the spine.
In terms of radiographical changes in the SIJ after lumbar fusion surgery, various reports have indicated an association with clinical symptoms. Froning and Frohman 22 first pointed out a possible association between persistent lumbar pain and SIJ, and increased uptake in bone scintigraphy has been reported in other studies.23,24 Ha et al 15 investigated SIJ degeneration by CT, as done in our study, and reported that the rate of SIJ degeneration in cases with lumbar/lumbosacral fusion was significantly higher (75.0% of 32 cases) than it was in the control group (38.2% of 34 cases). In addition, they reported that the incidence of radiographical SIJ degeneration was higher in patients with fusion down to S1 (100% of 10 cases) than in those with fusion down to L5 (64% of 14 cases), although there was no significant difference in their clinical symptoms, assessed by the Oswestry Disability Index and VAS. Another study 25 also reported a higher incidence of degenerative changes in cases with fusion to S1 than cases with fusion to L5, indicating that lumbosacral fusion could be associated with SIJ degeneration.
Regarding SIJ degeneration after the fixation across the SIJ to the iliac bone, a couple of studies have addressed a lower incidence of SIJ degeneration. Unoki et al investigated SIJ-related pain after multisegmented spinal fusion in 77 patients by comparing the lower fixation end of L5 (30 cases), sacrum (23 cases), and pelvis (24 cases) with a minimum 2-year follow-up. 14 SIJ-related pain was diagnosed using a diagnostic scoring system, 26 and its incidence rates were found to be 16.7%, 26.1%, and 4.2% in the lower fixation end of L5, sacrum, and pelvis, respectively, which were the highest in cases at lower end of the sacrum. Ohtori et al also reported favorable outcomes after lumbosacral fixation with iliac screws. 12 They reported no cases with SIJ-related pain and degeneration in 20 cases with a minimum 3 years of follow-up. In contrast to their report, SIJ degeneration was recognized even by fixation to the pelvis in the current study using SAI; however, the differences in 1) types of lower end screws (SAI 14 and iliac screws 12 ) and 2) the criteria of SIJ degeneration (intraarticular air and subchondral cyst were not assessed in previous reports12,14) might affect the results. SAI penetrate the SIJ, unlike iliac screws; hence, according to the strict evaluation criteria, SIJ degeneration might be induced by SAI due to partial destruction of the articular cartilage. Therefore, a future comparative study is required to compare SIJ degeneration between SAI and iliac screw usage.
This study had a couple of limitations. First, the sample size was only 70 cases, which was insufficient. In addition, since the minimum follow-up was 2 years, a future large-scale study is necessary to validate the current result. Second, regarding the clinical symptoms, it was difficult to diagnose SIJ-related pain accurately due to a lack of established diagnostic criteria.25,27 Several studies used an injection test or their original scoring system based on clinical symptoms, but we used LBP-related quality of life questionnaire and VAS scores. Although there was no significant difference in clinical symptoms in the current study, a prospective study, including objective evaluation tests, should be performed to clarify the relationship between SIJ degeneration and pain. Third, although JOABPEQ was used in this study, it is not a traditionally used method of evaluation, such as Oswestry Disability Index (ODI). JOABPEQ was developed by the Japanese Orthopaedic Association in 2007 as patient-reported outcomes evaluating low back pain more comprehensively. However, JOABPEQ is not an internationally recognized method, and this can be a limitation of this study. Finally, although our objective was >50 years old, the progress of SIJ degeneration in young adults is more important with respect to clinical prognoses. The results obtained in the present study should be reinvestigated whether these are consistent for cases <50 years of age.
Conclusion
Degenerative changes in the SIJ, occurring after lumbosacral fixation, were significantly frequent with SBS usage compared to those with SAI usage. Lumbosacral fixation to the sacrum using SBS may accelerate degenerative changes in the SIJ compared with fixation to the iliac bone using SAI; therefore, careful long-term follow-up is required.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Tokumi Kanemura is a consultant for Medtronic and NUVASIVE.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Hiroaki Nakashima, MD, PhD  https://orcid.org/0000-0002-0039-9678
https://orcid.org/0000-0002-0039-9678
Kotaro Satake, MD, PhD  https://orcid.org/0000-0003-0892-5713
https://orcid.org/0000-0003-0892-5713
Naoki Segi, MD  https://orcid.org/0000-0001-9681-2422
https://orcid.org/0000-0001-9681-2422
Kei Ando, MD, PhD  https://orcid.org/0000-0002-1088-2903
https://orcid.org/0000-0002-1088-2903
Shiro Imagama, MD, PhD  https://orcid.org/0000-0003-1721-9626
https://orcid.org/0000-0003-1721-9626
References
- 1.Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329–2336. [DOI] [PubMed] [Google Scholar]
- 2.Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303–308. [DOI] [PubMed] [Google Scholar]
- 3.Jain A, Hassanzadeh H, Strike SA, Menga EN, Sponseller PD, Kebaish KM. Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques: AAOS exhibit selection. J Bone Joint Surg Am. 2015;97(18):1521–1528. [DOI] [PubMed] [Google Scholar]
- 4.Jackson RP, McManus AC. The iliac buttress. A computed tomographic study of sacral anatomy. Spine (Phila Pa 1976). 1993;18(10):1318–1328. [PubMed] [Google Scholar]
- 5.Fukuda K, Takemitsu M, Machida M, Asazuma T. Lumbosacral fixation using sacroiliac buttress screws: a modification to the Jackson technique with intrasacral rods. Scoliosis. 2014;9(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alegre GM, Gupta MC, Bay BK, Smith TS, Laubach JE. S1 screw bending moment with posterior spinal instrumentation across the lumbosacral junction after unilateral iliac crest harvest. Spine. 2001;26(18):1950–1955. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen JH, Buell TJ, Wang TR, et al. Low rates of complications after spinopelvic fixation with iliac screws in 260 adult patients with a minimum 2-year follow-up. J Neurosurg Spine. 2019;30(5):1–9. [DOI] [PubMed] [Google Scholar]
- 8.Kebaish KM. Sacropelvic fixation: techniques and complications. Spine (Phila Pa 1976). 2010;35(25):2245–2251. [DOI] [PubMed] [Google Scholar]
- 9.Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine (Phila Pa 1976). 2010;35(20):1887–1892. [DOI] [PubMed] [Google Scholar]
- 10.Nakashima H, Kanemura T, Satake K, et al. The prevalence and risk factors for S2 alar-Iliac screw loosening with a minimum 2-year follow-up. Asian Spine J. 2020;14(2):177–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ishida W, Elder BD, Holmes C, et al. S2-Alar-Iliac screws are associated with lower rate of symptomatic screw prominence than iliac screws: radiographic analysis of minimal distance from screw head to skin. World Neurosurg. 2016;93:253–260. [DOI] [PubMed] [Google Scholar]
- 12.Ohtori S, Sainoh T, Takaso M, et al. Clinical incidence of sacroiliac joint arthritis and pain after sacropelvic fixation for spinal deformity. Yonsei Med J. 2012;53(2):416–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finger T, Bayerl S, Bertog M, Czabanka M, Woitzik J, Vajkoczy P. Impact of sacropelvic fixation on the development of postoperative sacroiliac joint pain following multilevel stabilization for degenerative spine disease. Clin Neurol Neurosurg. 2016;150:18–22. [DOI] [PubMed] [Google Scholar]
- 14.Unoki E, Miyakoshi N, Abe E, et al. Sacropelvic fixation with S2 alar iliac screws may prevent sacroiliac joint pain after multisegment spinal fusion. Spine (Phila Pa 1976). 2019;44(17):E1024–e1030. [DOI] [PubMed] [Google Scholar]
- 15.Ha K-Y, Lee J-S, Kim K-W. Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up. Spine. 2008;33(11):1192–1198. [DOI] [PubMed] [Google Scholar]
- 16.Fukui M, Chiba K, Kawakami M, et al. Japanese Orthopaedic Association Back Pain Evaluation Questionnaire. Part 3. Validity study and establishment of the measurement scale: subcommittee on low back pain and cervical myelopathy evaluation of the clinical outcome committee of the Japanese Orthopaedic Association, Japan. J Orthop Sci. 2008;13(3):173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fukui M, Chiba K, Kawakami M, et al. JOA Back Pain Evaluation Questionnaire (JOABPEQ)/JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). The report on the development of revised versions. April 16, 2007. The subcommittee of the clinical outcome committee of the Japanese Orthopaedic Association on Low Back Pain and Cervical Myelopathy Evaluation. J Orthop Sci. 2009;14(3):348–365. [DOI] [PubMed] [Google Scholar]
- 18.Elder BD, Ishida W, Lo SL, et al. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976). 2017;42(3): E142–E149. [DOI] [PubMed] [Google Scholar]
- 19.Yasuda T, Hasegawa T, Yamato Y, et al. Lumbosacral junctional failures after long spinal fusion for adult spinal deformity-which vertebra is the preferred distal instrumented vertebra? Spine Deform. 2016;4(5):378–384. [DOI] [PubMed] [Google Scholar]
- 20.Nakashima H, Kawakami N, Tsuji T, et al. Adjacent segment disease after posterior lumbar interbody fusion: based on cases with a minimum of 10 years of follow-up. Spine (Phila Pa 1976). 2015;40(14):E831–841. [DOI] [PubMed] [Google Scholar]
- 21.Baria D, Lindsey RW, Milne EL, Kaimrajh DN, Latta LL. Effects of lumbosacral arthrodesis on the biomechanics of the sacroiliac joint. JB JS Open Access. 2020;5(1):e0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Froning EC, Frohman B. Motion of the lumbosacral spine after laminectomy and spine fusion. Correlation of motion with the result. J Bone Joint Surg Am. 1968;50(5):897–918. [PubMed] [Google Scholar]
- 23.Gates GF, McDonald RJ. Bone SPECT of the back after lumbar surgery. Clin Nucl Med. 1999;24(6):395–403. [DOI] [PubMed] [Google Scholar]
- 24.Onsel C, Collier BD, Kir KM, et al. Increased sacroiliac joint uptake after lumbar fusion and/or laminectomy. Clin Nucl Med. 1992;17(4):283–287. [DOI] [PubMed] [Google Scholar]
- 25.Unoki E, Abe E, Murai H, Kobayashi T, Abe T. Fusion of multiple segments can increase the incidence of sacroiliac joint pain after lumbar or lumbosacral fusion. Spine (Phila Pa 1976). 2016;41(12):999–1005. [DOI] [PubMed] [Google Scholar]
- 26.Kurosawa D, Murakami E, Ozawa H, et al. A diagnostic scoring system for sacroiliac joint pain originating from the posterior ligament. Pain Med. 2017;18(2):228–238. [DOI] [PubMed] [Google Scholar]
- 27.Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis, and treatment. Anesth Analg. 2005;101(5):1440–1453. [DOI] [PubMed] [Google Scholar]