Abstract
Purpose
To evaluate whether an anatomic dry shoulder Dexter training model surgical simulator would be effective in augmenting orthopaedic residents’ skills for arthroscopic rotator cuff repair.
Methods
Nine residents, enrolled for this prospective study, watched a video presentation about transosseus equivalent (TOE) double-row, rotator cuff repair technique, repeating the aforementioned technique twice on the simulator. The time to complete all steps to final repair, as well as the quality of the final repair, were measured.
Results
The data for repair completion time showed a statistically significant difference in the total duration time of performing the procedure, when comparing the timing in tests 1 and 2, demonstrating a reduced operative time. The qualitative data collected show an increase in the final score in 100% (9 out of 9) of the participants between the first and second tests, with an improvement in the average score of 16.4% (3.22 points with a standard deviation of 2.64). Hence, there is a statistically significant difference (P = .006) between the total scores obtained by the participants at the end of tests 1 and 2, presenting an improvement of the quality score, shifting from the first (average score 19.7) to the second (average score 22.9) test. Conclusion: The dry simulator may be a valuable device to improve arthroscopic technical skills. This improvement was observed both in the resulting reduced operative time required to carry out the surgical procedure and the increased quality score (established to evaluate the quality of the required tasks).
Clinical Relevance
In order to provide as many training opportunities as possible, an arthroscopy simulator could be used to supplement clinical arthroscopy skills training for orthopaedic residents.
Introduction
The education of residents is an extremely important and demanding mission, particularly in surgical fields. The restricted availability of educators forces societies to search for teaching and training alternatives.1,2
All surgical skills have a learning curve and require dedicated practice to obtain mastery; arthroscopic techniques present additional challenges to the learning curve.3 The master-apprentice approach has dominated surgical training for more than 100 years,4 but specifically regarding minimally invasive surgery, it has been shown that operating during the period of initial skill acquisition can lead to increased rates of complications.5 New methods and new criterion standards for the training of surgeons must be developed. Simulation-based training (SBT) can be used to develop surgeons’ knowledge, skills, and behaviors, e.g., by allowing surgical trainees to develop diagnostic skills with simulated patients (SPs), or learn technical skills on various models, including virtual-reality (VR) simulators, animal tissue, live anesthetized animals, and human cadavers6 without exposing patients to risks.7,8
The overall aim of SBT is to increase patient safety by improving the competency of surgeons.4,9 It has been shown that VR-based training has at least equal value to direct observation, animal and/or cadaver models or videotape learning tools.1,10 To accelerate the learning process, numerous methods can be used to create an arthroscopic experience; within the wide range of possibilities, there are courses involving surgery on a corpse, nonanatomical models, anatomical models, virtual models on electronic platforms, and computer models. However, several anatomic virtual-reality or laboratory-based trainers may be impractical or cost-prohibitive, leading to barriers in implementation.11 Therefore, mid-range price and portable training models may solve important accessibility, flexibility, and financial barriers faced by some orthopaedic trainees and in residency programs.
The purpose of this study was to evaluate whether an anatomic dry shoulder Dexter training model surgical simulator would be effective in augmenting orthopaedic residents’ skills for arthroscopic rotator cuff repair. The hypothesis of this study was that the anatomic dry shoulder Dexter training model would be an effective tool to improve arthroscopic skills of orthopaedic residents.”
Methods
All 9 residents in the department of orthopaedics and tramatology at the authors’ institution were asked to participate in this study. The exclusion criterion was if the resident had previous experience with shoulder arthroscopy simulations or training models.
The study was a prospective trial consisting of a group of residents repeating the assigned tasks twice on the simulator and evaluating the results between the sessions. Four months were necessary to complete all the planned sessions. Before the tutorial session, each participant reviewed the study objectives and scoring system and was informed about the evaluation criteria used. All participants viewed a video presentation (performed by the senior surgeon) clearly explaining the technique to be reproduced with a specific focus on the key surgical steps to address (e.g., anchor positioning, the geometry of the repair, type of knots, knot tension, etc.). Participants were then given 5 minutes of undirected arthroscopy time to become further familiarized with the simulator. The evaluation metric was divided into two main categories: time and quality. The former variable consists of the time measurement of the overall steps completed to accomplish the final repair configuration (surgery start, medial anchor placement, knot, first lateral anchor placement, second lateral anchor placement, and the end of the surgery).
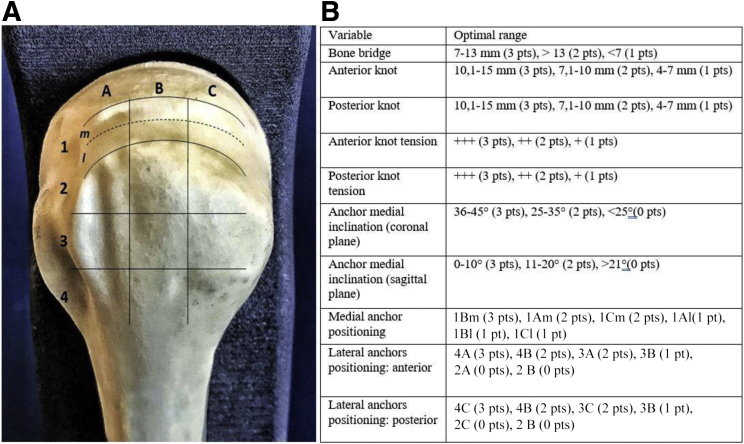
The latter variable (including assessment of the motor tasks at the base of the repair configuration) comprises evaluations about the configuration geometry, the proper anchors’ insertion, the correct suture tension (evaluated qualitatively at the end of the repair by opening the simulator and analyzing the final repair by naked eyes) and the anchors’ placements in the correct areas. To identify the proper anchors’ placement, the proximal humeral head was mapped beforehand onto different areas. The size and position of these areas were geometrically defined (Fig 1A). An appropriate, a predefined score was assigned to every qualitative variable based on the measured value (Fig 1B).
Fig 1.
(A) Proximal humerus. Left side. Posterior view. To precisely localize anchor position, the greater tuberosity was divided into 3 equal zones in the sagittal plane (A-C), and four rows (1-4) were defined in the coronal plane. Row 1 consists of the area included from the articular surface to the summit of the greater tuberosity and is subdivided in medial (m) strictly adjacent to the cartilage (A1m, B1m, C1m), and lateral (l) (A1l, B1l, C1l); Row 2 (A2, B2, C2), 0 to 7 mm below the summit; Row 3 (A3, B3, C3), 8 to 14 mm below row; Row 4 (A4, B4,C4), 15 to 21 mm below row. (B) Anchor positioning was scored. Quality variables: For each of the qualitative variables, points were assigned on the basis of a specifically predetermined numerical reference system: for the Bone Bridge from 7 to 13 mm three points were assigned, for more than 13 mm were assigned two points, one point was awarded for less than 7 mm. For the anterior tendon bridge, three points between 10.1 and 15 mm were assigned, between 7.1 and 10 mm, two points were assigned and one point was assigned between 4 and 7 mm. For the posterior tendon bridge, three points between 10 and 15 mm were assigned, two points between 7.1 and 10 mm and one point between 4 and 7 mm. To evaluate the tension of the anterior and posterior knots, 3 points were assigned when the tightness of the knots was optimal, when the tightness was intermediate, two points were assigned, and one point was assigned when the tightness was poor. The evaluation of the inclination of the medial anchor on the coronal plane was made by attributing three points from 36° to 45°, two points between 25° and 35°, and zero points for values less than 25°. The inclination of the medial anchor on the sagittal plane was evaluated by attributing three points from 0° to 10°, attributing two points between 11° and 20° and zero points for values greater than 21°. The positioning of the anchors was evaluated on the basis of the scheme (Table 3A). For the positioning of the medial anchor three points in 1Bm, two points in 1 Am and 1Cm, one point in 1Al, 1Bl, and 1Cl were attributed. For the positioning of the front lateral anchor, three points were attributed in 4C, two points in 4B, 3C, one point in 3B, zero points in 2B, 2C. For the positioning of the rear lateral anchor three points in 4C, two points in 4B and 3C, one point in 3B, zero points in 2C and 2B were attributed.
Training Model
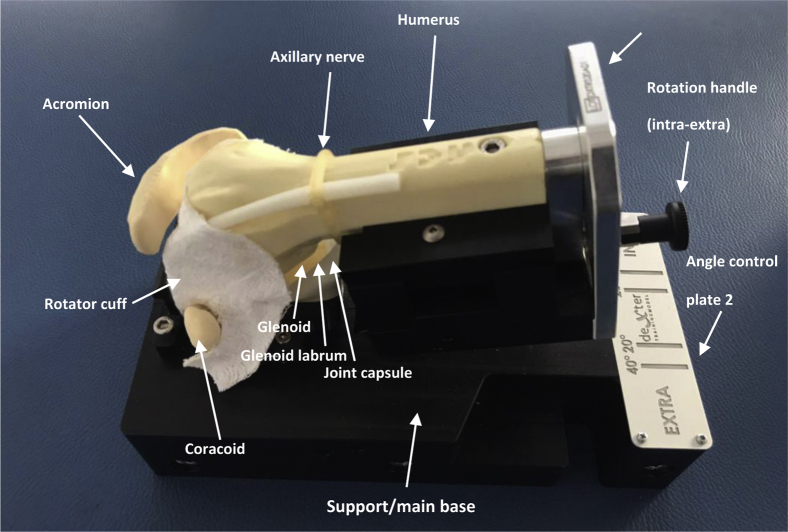
The shoulder simulator used was the Dexter Training Model Surgical Simulator (for brevity named Dexter) (NCS Lab, Carpi, Italy), consisting of a portable system enclosed in a rigid case (Fig 2). It can be used in the beach chair or lateral decubitus position, with the possibility to choose internal and external rotation and abduction/adduction position. Lastly, it is equipped with a 0° arthroscope camera (Teslong) with intensity-adjustable LED lights and with plug-and-play adaptor type USB 2.0/USB mini-B usable with any computer, tablet, or smartphone that supports these USB ports.
Fig 2.
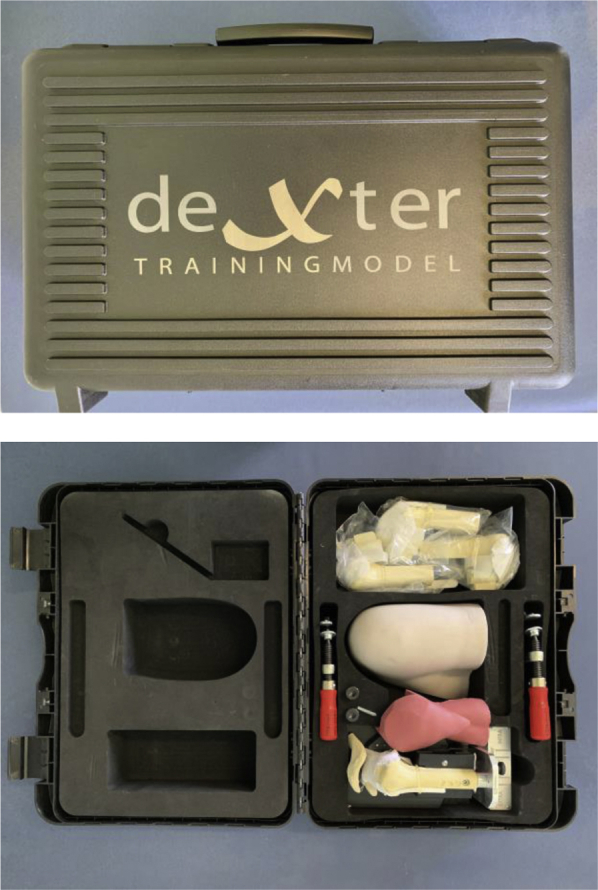
Dexter Training Model Surgical Simulator: modular simulator and spare parts in portable system.
All the Dexter components are composed of different materials and may be changed (Fig 3).
Fig 3.
Dexter Training Model Surgical Simulator components: left shoulder, lateral decubitus, anterior view. The skin, elastic and soft, is made of polyol and isocyanate. All the bony components (acromion and coracoid tip, glenoid, humerus) are made of polylactic acid (PLA) 3D printed. Labrum and biceps tendon are made of white bioflex. The semi-elastic rotator cuff is made of White Jacquard tissue and the muscle is made of silicone.
Surgical Technique
All participants were required to perform a double-row rotator cuff repair (1 medial anchor and 2 lateral knotless anchors) (Fig 4). To reproduce the surgery, 3 portals were required: standard posterior (for the scope), lateral, and antero-superior (working) portals.12
Fig 4.
Proximal humerus, left side, lateral view. Rotator cuff (RC) repair. Transosseus equivalent configuration. Keep in mind to maintain an 8-10 mm “bone bridge” between lateral anchors (←→) to avoid the risk of cortex cracking
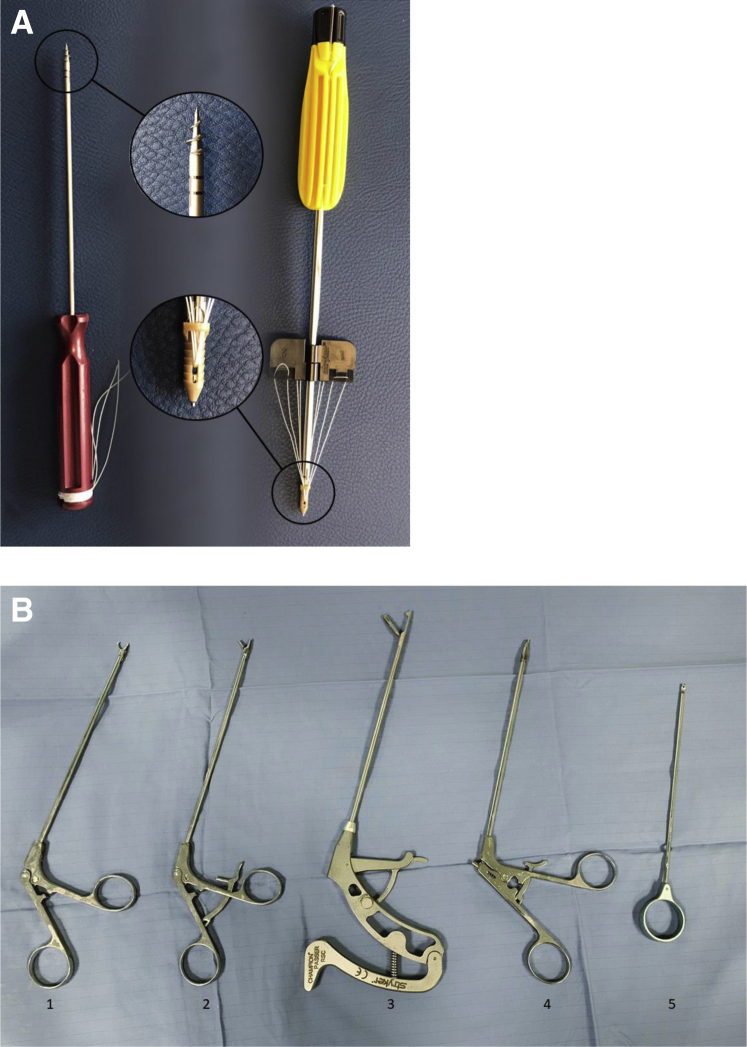
Another percutaneous small accessory supero-lateral portal was performed to correctly place the medial row anchor near the cartilage margin, to avoid the risk of the anchors’ pull-out. Cannulas were not used. The required instrumentation and the anchors employed are reported in Fig 5.
Fig 5.
Rotator cuff repair: anchors tipology. (A) From the left to right titanium IntraLine suture anchors 5.5 mm and The ReelX STT knotless anchor (Stryker, USA). (B) Basic set of arthroscopy instruments for rotator cuff repair: 1, retrievers; 2, grasper; 3, suture passer; 4, cutter; 5, knot pusher.
Medial row
One metal anchor (Titanium IntraLine Suture Anchor, 5 mm; Stryker, Kalamazoo, MI) with 2 sutures of different colors was placed medially. All 4 sutures limbs were then passed through the tendon from posterior to anterior, followed by closure of the medial row with knots in the opposite way. The knot to be used was chosen by each participant among three different types: SMC’s knot13 (sliding), Fisherman’s knot14 (sliding), and Revo’s knot15 (nonsliding). All of the limbs were maintained and employed to close the lateral row
Lateral Row
Two knotless anchors (ReelX STT 4.5 mm, Stryker, USA) were necessary. One limb from each medial knot was crossed over and loaded on the knotless anchors (1 anterior and 1 posterior) and then tensioned in order to compress the tissue to the anatomical footprint. The anchors were positioned through the lateral working portal, as distal as possible to the apex of the greater tuberosity, where a higher pull-out strength has been demonstrated.16 In addition, it is advisable to maintain an 8-10 mm of “bone bridge” between them to avoid the risk of cortex cracking (Fig 4).
Training Sessions
The surgical simulation was planned in 4 sessions as reported in Table 1. Data were collected in each test session. After the initial testing session (time 0), residents received a video lesson in a webinar format (Time 1) and after that, all subjects were tested twice more (Time 2, Time 3).
Table 1.
Surgical Simulation Sessions
| Time 0 | The first surgical simulation test was performed by all participants without any previous experience with the simulator, neither theoretical nor practical. |
| Time 1 | WATCH AND LEARN – WEBINAR lesson. |
| Time 2 | FREE PRACTICE – Training session performed with the help of the expert surgeon followed by a theoretical study of surgical technique. |
| Time 3 | Second surgical simulation test. |
The WATCH AND LEARN session was an online training webinar carried out by the senior surgeon to elucidate key surgical steps to perform a 3-anchor arthroscopic rotator cuff TOE double row repair on the training model.
Each test session was accomplished following this procedure: The model was secured in the requested orientation (all participants choose the lateral decubitus orientation). The assistants were instructed to act only at the specific direction of the operating surgeon. Prompting and coaching (of technique) were prohibited, and the procedures were monitored by the senior surgeon (the shoulder expert, external observer).
Every surgeon performed the TOE repair according to the technique above reported.
Statistical Analysis
Mathematical means and standard deviations were calculated for continuous variables, and frequencies and proportions were calculated for categorical variables by group and time points (between first and second session). For continuous variables, independent t tests were used to evaluate between-session differences. Dependent t-tests were used to evaluate within-group differences, between preintervention and postintervention, for continuous variables. All statistical analyses were completed using Minitab and a type I error rate of P < .05 was used to assess statistical significance.
Results
All the 9 residents completed the study.
Quality Scores
The quality scores collected for all participants in the first and second tests are shown in Table 2. Bone bridge data showed an improvement in 56% (5 out of 9) of the participants, an unchanged score in 22% (2 out of 9) and a worsening in 22% (2 out of 9). The data on the tightness of the anterior suture showed an improvement in 56% (5 out of 9) of the participants, an unchanged score in 44% (4 out of 9) and a worsening in 0% (0 out of 9). On the posterior knot tension, the data showed an improvement in 11% (1 out of 9) of the participants, an unchanged score in 44, 5% (4 out of 9) and a worsening in 44, 5% (4 out of 9). Data on the amount of tendon tissue sutured anteriorly (for brevity named Tendon bridge) showed an improvement in 44, 5% of the participants, an unchanged score in 44, 5% (4 out of 9), and a worsening in 11% (1 out of 9). Data on the amount of posterior tendon bridge showed an improvement in 78% (7 out of 9) of participants, an unchanged score in 11% (1 out of 9) and a worsening in 11% (1 out of 9). For the coronal inclination of the medial anchor, the data showed an improvement in 33% (3 out of 9) of the participants, an unchanged score in 45% (4 out of 9) and a worsening in 22% (2 out of 9). The data on the sagittal inclination of the medial anchor showed an improvement in 11% (1 out of 9) of the participants, an unchanged score in 67% (6 out of 9), and a worsening in 22% (2 out of 9). The data on the positioning of the medial anchor showed an improvement in 22% (2 out of 9) of participants, an unchanged score in 67% (6 out of 9) and a worsening in 11% (1 out of 9).
Table 2.
Quality Scores of the First and Second Test Session
| 1st Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step | Points for Each Participant |
||||||||
| R#1 | R#2 | R#3 | R#4 | R#5 | R#6 | R#7 | R#8 | R#9 | |
| 1 | 3 | 2 | 2 | 3 | 1 | 1 | 3 | 3 | 2 |
| 2 | 1 | 0 | 2 | 0 | 2 | 3 | 3 | 2 | 3 |
| 3 | 2 | 3 | 3 | 2 | 3 | 3 | 3 | 3 | 3 |
| 4 | 2 | 0 | 2 | 3 | 1 | 2 | 2 | 3 | 1 |
| 5 | 2 | 0 | 2 | 3 | 1 | 1 | 1 | 2 | 0 |
| 6 | 3 | 3 | 2 | 3 | 2 | 2 | 0 | 0 | 3 |
| 7 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 3 | 3 |
| 8 | 3 | 3 | 3 | 0 | 2 | 3 | 1 | 1 | 3 |
| 9 | 2 | 0 | 3 | 2 | 1 | 2 | 2 | 1 | 2 |
| 10 | 3 | 0 | 0 | 3 | 1 | 3 | 0 | 0 | 0 |
| Total | 24 | 14 | 22 | 22 | 17 | 23 | 17 | 18 | 20 |
| 2nd Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Step | Points for Each Participant |
||||||||
| R#1 | R#2 | R#3 | R#4 | R#5 | R#6 | R#7 | R#8 | R#9 | |
| 1 | 3 | 3 | 3 | 1 | 3 | 3 | 1 | 3 | 3 |
| 2 | 2 | 3 | 2 | 3 | 3 | 3 | 3 | 3 | 3 |
| 3 | 0 | 3 | 0 | 3 | 0 | 3 | 1 | 3 | 3 |
| 4 | 3 | 2 | 3 | 3 | 2 | 2 | 2 | 1 | 1 |
| 5 | 3 | 2 | 3 | 3 | 2 | 2 | 2 | 1 | 2 |
| 6 | 3 | 3 | 2 | 2 | 3 | 2 | 3 | 3 | 2 |
| 7 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 2 |
| 8 | 3 | 3 | 3 | 0 | 3 | 3 | 0 | 3 | 3 |
| 9 | 3 | 2 | 3 | 3 | 0 | 2 | 3 | 2 | 2 |
| 10 | 3 | 0 | 2 | 2 | 0 | 3 | 2 | 0 | 2 |
| Total | 26 | 24 | 24 | 23 | 19 | 26 | 20 | 21 | 23 |
1: bone bridge; 2: anterior knot tension; 3: posterior knot tension; 4: anterior edge-knot depth; 5: posterior edge-knot depth; 6: anchor medial inclination (coronal plane); 7: anchor medial inclination (sagittal plane); 8: medial anchor positioning; 9 antero-lateral anchors positioning: anterior; and 10: postero-lateral anchors positioning. R#1,2,3,4…etc: participants.
The data on the positioning of the anterior lateral anchor showed an improvement in 56% (5 out of 9) of the participants, an unchanged score in 33% (3 out of 9), and a worsening in 11% (1 out of 9). Finally, the data on the positioning of the lateral posterior anchor showed an improvement in 33% (3 out of 9) of the participants, an unchanged score in 45% (4 out of 9), and a worsening in 22% (2 out of 9).
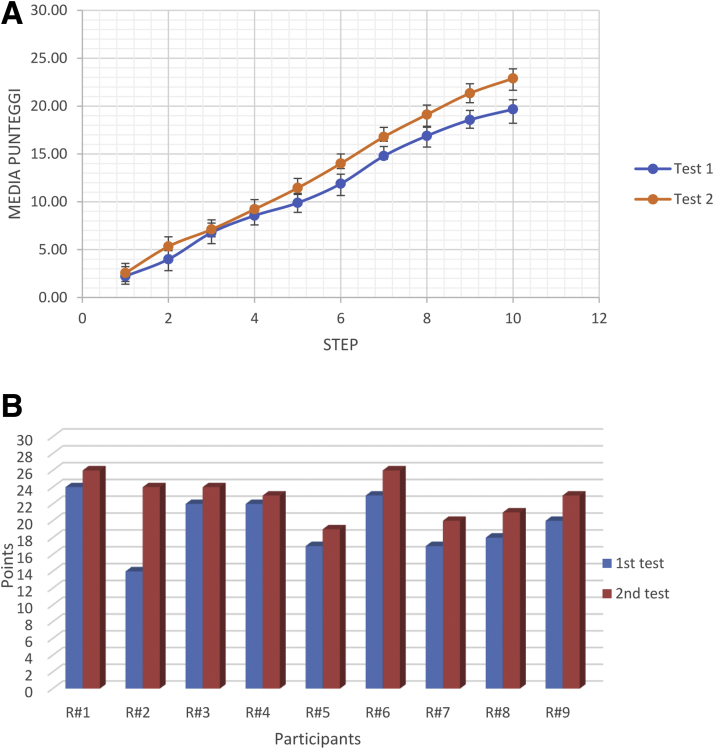
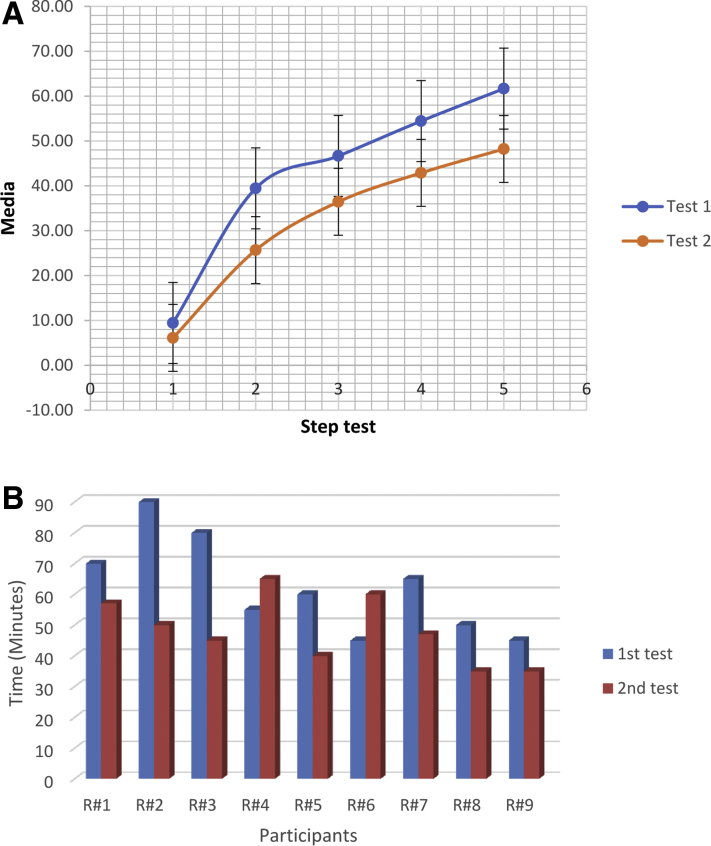
Overall, the qualitative data collected showed an increase in the final score in 100% (9 out of 9) of the participants, between the first and second tests, with an improvement in the average score of 16.4% (3.22 points with standard deviation of 2.64) (Fig 6A). The total of qualitative scores and the difference between the first and second test for every participant are presented in Fig 6B. The two test sessions have been compared on the basis of the total score obtained at the end of the procedure during the various trials. There is a statistically significant difference between the total score obtained in the two trials at the end of the session, showing an increase in quality score comparing the first to the second trial (Table 3).
Fig 6.
Rotator cuff repair using a simulator training model performing two test sessions. Quality scores. (A) Average of the quality scores divided by each qualitative target of the first and second test session. 1: bone bridge; 2: anterior knot tension; 3: posterior knot tension; 4: anterior edge-knot depth; 5: posterior edge-knot depth; 6: anchor medial inclination (coronal plane); 7: anchor medial inclination (sagittal plane); 8: medial anchor positioning; 9: antero-lateral anchors positioning: anterior; 10: postero-lateral anchors positioning. (B) Total of quality scores to complete the surgical simulation of every participant in the first and second test session. R#1,2,3,4…etc: participants.
Table 3.
Increasing of the Quality Score Shifting From the First to the Second Trial
| Test 1 |
Test 2 |
P Value |
|---|---|---|
| Average Score | Average Score | |
| 19.7 | 22.9 | 0.006 |
Time Scores
The time scores collected for all participants in the first and second tests are shown in Table 4. Time data were collected and analyzed in 5 consecutive steps for every test session.
Table 4.
Time scores
| 1st Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| STEP | Times of each participant (minutes) |
||||||||
| R#1 | R#2 | R#3 | R#4 | R#5 | R#6 | R#7 | R#8 | R#9 | |
| 1 | 10 | 15 | 15 | 10 | 10 | 10 | 5 | 5 | 5 |
| 2 | 50 | 65 | 45 | 30 | 35 | 25 | 45 | 30 | 30 |
| 3 | 55 | 75 | 60 | 40 | 40 | 35 | 50 | 35 | 35 |
| 4 | 65 | 85 | 70 | 45 | 45 | 40 | 60 | 40 | 40 |
| 5 | 70 | 90 | 80 | 55 | 55 | 45 | 65 | 50 | 45 |
| 2nd Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| STEP | Times of Each Participant (minutes) |
||||||||
| R#1 | R#2 | R#3 | R#4 | R#5 | R#6 | R#7 | R#8 | R#9 | |
| 1 | 5 | 5 | 5 | 10 | 5 | 5 | 5 | 5 | 10 |
| 2 | 30 | 25 | 23 | 46 | 18 | 30 | 24 | 20 | 15 |
| 3 | 40 | 35 | 30 | 56 | 30 | 45 | 35 | 30 | 27 |
| 4 | 50 | 45 | 37 | 61 | 35 | 51 | 43 | 32 | 32 |
| 5 | 57 | 50 | 45 | 65 | 40 | 60 | 47 | 35 | 35 |
To measure the temporal variables, the main surgical steps necessary for the completion of the surgical technique under analysis were taken into consideration in first and second test session. 1: the time for the positioning of the first anchor (medial anchor); 2: the moment in which the suture of the first anchor are tied; 3: the moment in which the first lateral anchor is positioned; 4: the moment in which the second lateral anchor is positioned; 5: the moment of the end of the intervention. R#1,2,3,4 … etc: participants.
The first step corresponds to the time elapsed between the start of the simulation and the moment in which the positioning of the first anchor (medial) takes place: the data showed an improvement (i.e., less time to execute) in 56% (5 out of 9) of participants, an unchanged execution time in 33% (3 out of 9) and a worsening in 11% (1 out of 9). The second step corresponds to the time taken to suture the first stitch of the medial anchor: the data showed an improvement in 78% (7 out of 9) of the participants, an unchanged score in 0% (0 out of 9) and a worsening in 22% (2 out of 9). The third step corresponds to the time taken to place the first lateral anchor: the data showed an improvement in 66% (6 out of 9) of the participants, an unchanged score in 0% (0 out of 9) and a worsening in 44% (4 out of 9). The fourth step corresponds to the time taken to place the last anchor (posterolateral): the data showed an improvement in 78% (7 out of 9) of participants, an unchanged score in 0% (0 out of 9) and a worsening in 22% (2 out of 9). The fifth and last step corresponds to the end of the surgical simulation: the data showed an overall improvement in the total test time in 78% (7 out of 9) of the participants, an unchanged time in 0% (0 out of 9) and a worsening in 22% (2 out of 9).
The average of each single time-score in the first and second tests for each of the participants is represented in Fig 7A. The Total of the time scores and the difference between the first and second test for every participant are presented in Fig 7B. The two test sessions have been compared both in the intermediate steps of the procedure and in the overall length.
Fig 7.
Rotator cuff repair using a simulator training model performing two test sessions. Time scores. (A) Average times to complete each step in the first and second test session. 0: beginning of the intervention; 1: the time for the positioning of the first anchor (medial anchor); 2: the moment in which the suture of the first anchor are tied; 3: the moment in which the first lateral anchor is positioned; 4: the moment in which the second lateral anchor is positioned; 5: the moment of the end of the intervention. (B) Total time to complete the surgical simulation of every participant in the first and second test session. R#1,2,3,4 … etc: participants.
There is a statistically significant difference in the total duration of the accomplished procedure, when comparing the timing in trials 1 and 2, demonstrating a reduction in operative time. There is no significant difference at the intermediate level (Table 5).
Table 5.
Comparison of Total Time Duration of Steps 1-5
| Test 1 |
Test 2 |
||||
|---|---|---|---|---|---|
| STEP | Standard Deviation | Average | Standard Deviation | Average | P Value |
| 1 | 3.9 | 9.4 | 2.2 | 6.1 | 0.081 |
| 2 | 12.9 | 39.4 | 9.1 | 25.7 | 0.066 |
| 3 | 14.4 | 46.7 | 9.3 | 36.4 | 0.095 |
| 4 | 16.3 | 54.4 | 9.9 | 42.9 | 0.081 |
| 5 | 15.8 | 61.7 | 10.8 | 48.2 | 0.160 |
| Total Timing | 0.050 | ||||
Statistically significant difference is shown between the total duration to accomplish the procedure by comparing the timing in trials 1 and 2, showing a reduction in operative time. There is no significant difference at the intermediate level
Discussion
The hypothesis of this study was verified and the anatomic dry shoulder Dexter training model revealed to be an effective tool to improve arthroscopic skills of orthopaedic residents. Moreover, it is possible to assume that an arthroscopic rotator cuff repair can be deconstructed into the essential steps necessary for the effective completion of the repair.
The effectiveness of training models and arthroscopic surgical simulators is validated by studies tested on other joints.3,17,18,19,20,21 Considering that, these models have proved principally effective for trainees with a low or intermediate level of experience. This study revealed that training on an arthroscopic simulator improves performance on the simulator, which, in turn, may be beneficial for performance in the operating room, keeping in mind what was reported by R. M. Frank et al.17 on the degree of transferability of the acquired skills. For this reason, it is always very important to use the same scoring system and standardize procedures. Time to perform a task was the most commonly reported skill-evaluating outcome of simulation18 in this study; not only the time to perform every single task were reported, but even the quality of every accomplished task.
In this study, the training model (DEXTER) has been used for an arthroscopic rotator cuffs repair, and data suggest that the training model accelerates the learning process. Moreover, the indisputable advantages of this simulator are the possibility of training 24 hours a day, 365 days a year, in addition to the opportunity to practice anywhere, even in a domestic environment, allowing immediate and objective feedback, as well as self-assessment of progress,1 discarding risks associated with cadaver lab. Furthermore, the prospect of practicing many times on the Dexter could lead to a greater level of safety for the patient, not only because of the acquisition of the current surgical technique, but also for the improvement of simple surgical arthroscopic gestures, such as visualization, triangulation, and knot-tying tasks. Each type of surgical simulator has pros and cons. The main ones are summarized in Table 6.
Table 6.
Main Advantages and Limitations of Each Type of Arthroscopy Simulator
| Arthroscopy Simulators | Advantages | Limitations |
|---|---|---|
| Cadaver lab (Gold standard for training) | Real anatomy, every kind of tasks and complete simulation | High prices, requires travel, legal restrictions in different countries, days off, check of the surgical technique only after anatomical dissection, risk of disease transmission |
| Robotic simulator | Anatomical very realistic simulation; advanced tasks | High prices and cost-effectiveness; not portable |
| Nonanatomic simulator | Very low prices; “at home” simulator | Only basic skills; not realistic |
| Anatomic training model | Anatomical realistic simulation; advanced tasks; easy and immediate check of the surgical technique; portable | Camera 0°, need for spare parts |
The surgical technique chosen for this training was a transosseus equivalent (TOE) double-row rotator cuff repair. With this technique (TOE), the rotator cuff tissue is compressed to the anatomical footprint mainly by the help of bridging sutures,22 decreasing tissue strangulation and better preserving tendon vascularity.23
Limitations
This investigation has some limitations. First, although our sample size in this study is comparable to those reported in the current body of literature, the sample size and the impact of the study were limited by the number of residents tested. At the beginning of the study, only 9 M.D. Residents in orthopaedics and traumatology were assigned from Sapienza University of Rome to this Institute. Moreover, the study was conducted using a single training model, and thus, assumptions cannot be made on the effectiveness of similar models. Finally, as another training model, Dexter lacks some key elements, which could modify operator surgical performance “in vivo”; in fact, it is dry and blood-free. Another intrinsic limitation of the training model adopted in this study was the 0° arthroscope, with the Dexter, equipped only with this camera.
Conclusion
The dry simulator may be a valuable device to improve arthroscopic technical skills. This improvement was observed both in the resulting reduced operative time required to carry out the surgical procedure and the increased quality score (established to evaluate the quality of the required tasks).
Acknowledgment
The authors wish to thank NCS Lab (Carpi, Modena, Italy) and Stryker (Formello, Italy) for providing free and disinterested materials, respectively: the Dexter training model with spare parts and the anchors used during the study tests, and Ms. Benedetta Zimbalatti (B.A., University of Dublin–Trinity College, Dublin, Ireland) for reviewing the English.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Material
References
- 1.Rahm S., Germann M., Hingsammer A., Wieser K., Gerber C. Validation of a virtual reality-based simulator for shoulder arthroscopy. Knee Surg Sport Traumatol Arthrosc. 2016;24:1730–1737. doi: 10.1007/s00167-016-4022-4. [DOI] [PubMed] [Google Scholar]
- 2.Redondo M.L., Christian D.R., Gowd A.K., et al. The effect of triangulation simulator training on arthroscopy skills: A prospective randomized controlled trial. Arthrosc Sport Med Rehabil. 2020;2:e59–e70. doi: 10.1016/j.asmr.2019.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hauschild J., Rivera J.C., Johnson A.E., Burns T.C., Roach C.J. Shoulder arthroscopy simulator training improves surgical procedure performance: A controlled laboratory study. Orthop J Sports Med. 2021;9 doi: 10.1177/23259671211003873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bjerrum F., Thomsen A.S.S., Nayahangan L.J., Konge L. Surgical simulation: Current practices and future perspectives for technical skills training. Med Teach. 2018;40:668–675. doi: 10.1080/0142159X.2018.1472754. [DOI] [PubMed] [Google Scholar]
- 5.Luzzi A., Hellwinkel J., O’Connor M., Crutchfield C., Lynch T.S. The efficacy of arthroscopic simulation training on clinical ability: A systematic review. Arthroscopy. 2021;37:1000–1007.e1. doi: 10.1016/j.arthro.2020.09.018. [DOI] [PubMed] [Google Scholar]
- 6.Hasan L.K., Haratian A., Kim M., Bolia I.K., Frank A.E.W., Petrigliano A. Virtual reality in orthopedic surgery training. Adv Med Educ Pract. 2021;12:1295–1301. doi: 10.2147/AMEP.S321885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahm S., Wieser K., Bauer D.E., et al. Efficacy of standardized training on a virtual reality simulator to advance knee and shoulder arthroscopic motor skills. Musculoskelet Disord. 2018;19:150. doi: 10.1186/s12891-018-2072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Srivastava A., Gibson M., Patel A. Low-fidelity arthroscopic simulation training in trauma and orthopaedic surgery: A systematic review of experimental studies. Arthroscopy. 2022;38:190–199.e1. doi: 10.1016/j.arthro.2021.05.065. [DOI] [PubMed] [Google Scholar]
- 9.Cullinan D.R., Schill M.R., DeClue A., et al. Fundamentals of laparoscopic surgery: Not only for senior residents. Surg Educ. 2017;74:e51–e54. doi: 10.1016/j.jsurg.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahmood T., Scaffidi M.A., Khan R., Grover S.C. Virtual reality simulation in endoscopy training: Current evidence and future directions. World J Gastroenterol. 2018;24:5439–5445. doi: 10.3748/wjg.v24.i48.5439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yiasemidou M., Glassman D., Khan K., et al. Validation of a cost-effective appendicectomy model for surgical training. Scottish Med J. 2021;0:1–6. doi: 10.1177/0036933019900340. [DOI] [PubMed] [Google Scholar]
- 12.Chillemi C., Guerrisi M., Polizzotti G., Paglialunga C., et al. Arthroscopic rotator cuff repair: Advancements in techniques and technology. Adv Tech Musculoskel Surg. 2021;5:59–65. doi: 10.36959/765/399. [DOI] [Google Scholar]
- 13.Kim S.H., Ha K.I. The SMC knot—A new slip knot with locking mechanism. Arthroscopy. 2000;16:563–565. doi: 10.1053/jars.2000.4821. [DOI] [PubMed] [Google Scholar]
- 14.Ramirez O.M., Tezel E., Ersoy B. The Peruvian fishermans knot: A new, simple, and versatile self-locking sliding knot. Ann Plast Surg. 2009;62:114–117. doi: 10.1097/SAP.0b013e31817e2c9e. [DOI] [PubMed] [Google Scholar]
- 15.Snyder S.J. Technique of arthroscopic rotator cuff repair using implantable 4-mm revo suture anchors, suture shuttle relays, and no. 2 nonabsorbable mattress sutures. Orthop Clin North Am. 1997;28(2):267–275. doi: 10.1016/S0030-5898(05)70285-6. [DOI] [PubMed] [Google Scholar]
- 16.Zumstein M.A., Raniga S., Labrinidis A., Eng K., Bain G.I., Moor B.K. Optimal lateral row anchor positioning in posterior-superior transosseous equivalent rotator cuff repair: A micro-computed tomography study. Orthop J Sport Med. 2016;4:1–8. doi: 10.1177/2325967116671305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frank R.M., Wang K.C., Davey A., et al. Utility of modern arthroscopic simulator training models: A meta-analysis and updated systematic review. Arthrosc J Arthrosc Relat Surg. 2018;34:1650–1677. doi: 10.1016/j.arthro.2017.10.048. [DOI] [PubMed] [Google Scholar]
- 18.Hetaimish B., Elbadawi H., Ayeni O.R. Evaluating simulation in training for arthroscopic knee surgery: A systematic review of the literature. Arthrosc J Arthrosc Relat Surg. 2016;32:1207–1220.e1. doi: 10.1016/j.arthro.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 19.Waterman B.R., Martin K.D., Cameron K.L., et al. Simulation training improves surgical proficiency and safety during diagnostic shoulder arthroscopy performed by residents. Orthopedics. 2016;39:e479–e485. doi: 10.3928/01477447-20160427-02. [DOI] [PubMed] [Google Scholar]
- 20.Johnson J.D., Cheng C., Schmidtberg B., Cote M., Geaney L.E. Assessment of basic ankle arthroscopy skills in orthopedic trainees. Foot Ankle Int. 2020;41:193–199. doi: 10.1177/1071100719891418. [DOI] [PubMed] [Google Scholar]
- 21.Cychosz C., Khazi Z.M., Karam M., Duchman K., Willey M., Westermann R. Validation of a novel hip arthroscopy simulator: establishing construct validity. J Hip Preserv Surg. 2019;6:385–389. doi: 10.1093/jhps/hnz059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aydin N., Karaismailoglu B., Gurcan M., Ozsahin M.K. Arthroscopic double-row rotator cuff repair: A comprehensive review of the literature. SICOT J. 2018;4:57. doi: 10.1051/sicotj/2018048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Christoforetti J.J., Krupp R.J., Singleton S.B., Kissenberth M.J., Cook C., Hawkins R.J. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg. 2012;21:523–530. doi: 10.1016/j.jse.2011.02.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.